Abstract
People bereaved through road traffic accidents (RTAs) are at risk for severe and disabling grief (i.e., pathological grief). Knowledge about needs and use of bereavement care, including psychotherapy, pharmacotherapy, and support groups, is limited. This study charted (correlates of) the needs and use of bereavement care in RTA bereaved people. Furthermore, although online grief treatment seems effective, it is unknown whether it is perceived as acceptable. Accordingly, we examined the acceptability of online treatment. Dutch RTA bereaved adults (N = 273) completed self‐report measures about needs and use of bereavement care, acceptability of online grief treatment, and pathological grief. Regression analyses were used to identify correlates of care needs and use and acceptability of online treatment. The majority (63%) had received help from psychotherapy, pharmacotherapy, and/or support groups. One in five participants had not used bereavement care services, despite reporting elevated pathological grief levels and/or expressing a need for care, pointing to a treatment gap. Use of psychological support before the loss was the strongest predictor of bereavement care needs and use following the loss. A minority (35%) reported being inclined to use online grief treatment if in need of support. More openness towards online services was related to greater acceptability of online treatment. In conclusion, 20% of RTA bereaved people with pathological grief or care needs had not received care. This treatment gap may be reduced by improving accessibility of online treatments. However, as only 35% was open to using online treatments, increasing the acceptability of (online) treatments appears important.
Keywords: bereavement, grief, internet, prolonged grief, therapy, trauma
Key Practitioner Message.
This is the first study examining self‐reported use of psychotherapy, pharmacotherapy, and support groups in traumatically bereaved people.
Psychotherapy was the most frequently used service (55%), followed by pharmacotherapy (30%), and attending support group meetings (23%).
One in five participants had not used bereavement care services, despite reporting elevated pathological grief levels and/or expressing needs for care.
One third of the participants perceived online grief treatment as acceptable.
More openness towards innovative online services and higher pathological grief levels were related to increased acceptability of online grief treatment.
1. INTRODUCTION
Worldwide, road traffic accidents (RTAs) are the leading cause of unnatural death (WHO, 2019). Research has shown that prevalence rates of disturbed grief and comorbid post‐traumatic stress disorder (PTSD) and depression after a sudden or violent loss (i.e., traumatic loss), such as RTAs, are higher than after a death due to illness (Djelantik et al., 2020; Heeke et al., 2019; Kristensen et al., 2012; Lundorff et al., 2017). When these grief reactions persist and cause significant functional impairment, diagnoses of Persistent Complex Bereavement Disorder (PCBD; APA, 2013) or Prolonged Grief Disorder (PGD; WHO, 2018) may apply, and bereavement care may be indicated. Although these two diagnostic criteria sets differ (e.g., in number of symptoms and prevalence rates), they share common core symptoms (Lenferink et al., 2019); we therefore chose to hereafter use the term “pathological grief” to refer to such grief reactions. Bereavement care may be offered in different forms, including (i) psychotherapy, (ii) pharmacotherapy, and (iii) support groups. In a rare prior study on use of bereavement care in parents who lost a child due to cancer, 78% of people reported use of these bereavement services (Lichtenthal et al., 2015).
Psychotherapy is one of the most commonly used services by bereaved people (Aoun et al., 2015; Lichtenthal et al., 2015). Several reviews have shown that individual cognitive behavioural therapy (CBT) targeting grief symptoms is the most effective treatment to alleviate pathological grief (Boelen & Smid, 2017a; Doering & Eisma, 2016; Johannsen et al., 2019). Pharmacotherapy, with, for example, antidepressants and sleep medication, is also frequently obtained. For instance, Lichtenthal et al. (2015) found that about 40% of parents who had lost a child due to cancer have used pharmacotherapy. Pharmacotherapy is safe and effective for targeting bereavement‐related depression, but there is limited support for its effectiveness in reducing pathological grief symptoms (Boelen & Smid, 2017a). Bereavement (peer)support groups are widely available. Yet, this service is less commonly used compared with psychotherapy (Aoun et al., 2015; Lichtenthal et al., 2015). The effectiveness of bereavement support groups is unclear due to the lack of controlled research (Gauthier & Gagliese, 2012; Wilson et al., 2017).
Several scholars have expressed their concerns about a treatment gap in bereavement care, pointing to people who want or need professional bereavement care, but not receive this (Breen & Moullin, 2020; Lichtenthal et al., 2015). For instance, Lichtenthal et al. (2015) observed that 40% of cancer‐bereaved people, who wanted or needed bereavement care, did not receive any support; the two most common barriers to care in this group of bereaved people were that people found it too painful to talk about the loss and too difficult to find support. Furthermore, in a study drawing from the general bereaved population, those who were most in need of support (based on elevated pathological grief levels) were more likely to perceive a lack of support (Aoun et al., 2015). Offering online bereavement care may help to (partly) reduce this treatment gap, because, compared with face‐to‐face, in online care, clients may feel less vulnerable or ashamed and might be less afraid of being judged when disclosing painful thoughts or emotions. Furthermore, for those with difficulties finding support, because of limited availability of a specialized care provider close to home or because of scheduling difficulties, online care could offer the opportunity to receive care from home (or another place where they feel comfortable and safe) at any time of the day (Li et al., 2013).
Several studies have shown that online CBT‐based interventions successfully alleviate pathological grief and PTSD symptoms (Eisma et al., 2015; Kersting et al., 2013; Wagner et al., 2006). However, some of these studies suffered from relatively small sample sizes and/or high drop‐out rates compared with studies examining face‐to‐face grief‐specific CBT (for reviews, see Johannsen et al., 2019; Wagner et al., 2020). The Technology Acceptance Model (Davis, 1989) postulates that motivation of the user predicts technology use. Users' motivation is determined by (i) attitudes towards using the technology, (ii) perceived ease, and (iii) perceived usefulness of the technology. Drawing from this model, the lack of perceived acceptability of online treatment might partly explain why it is difficult to recruit and retain participants in online support (Arjadi et al., 2018; Simblett et al., 2019). Prior research in depression has shown that people who were younger, more highly educated, more depressed, more open to innovative technologies, and who used mental health services before perceived online treatment as more acceptable (Arjadi et al., 2018; Dorow et al., 2018). Insight into factors related to perceived acceptability of online grief treatment may be helpful in recruiting and retaining bereaved people in online treatment.
Accordingly, the aim of the current study was to clarify the needs and use of bereavement care and preferences for online treatment among people confronted with deaths of loved ones through an RTA. We first examined prevalence rates of needs and use of bereavement care, by reporting on how many people (1) did not want to use a specific service (i.e., psychotherapy, pharmacotherapy, or support groups), (2) wanted to use a specific service but did not do so, (3) have used a specific service, but not anymore, and (4) were using a service at the time of study participation (Aim 1). Second, we examined correlates of needs and use of bereavement care (i.e., the latter three groups vs. people who did not want to use services) for each of the three types of services separately. More specifically, we examined background (gender, level of education, age, and preloss psychological support) and loss‐related (time since loss and relationship to the deceased) correlates of bereavement care needs and use, while taking severity of pathological grief levels into account (Aim 2). Third, to define the magnitude of a treatment gap in bereavement care, we calculated how many people did not use any services after the loss but reported clinically relevant pathological grief levels (as defined by scoring above cut‐off on a pathological grief measure) and/or reported that they would like to use a service (Aim 3). Fourth, frequencies of barriers of care were explored in people who did not use any services at the time of study participation (Aim 4). Lastly, in the total sample, we explored to what extent previously described background and loss‐related variables and pathological grief levels plus openness towards use of innovative technologies were related to perceived acceptability of online grief treatment (Aim 5).
2. METHODS
2.1. Procedure and participants
Data were collected between December 2018 and April 2020 among Dutch adults whose spouse, family member, or friend had died due to an RTA. This study was part of a larger research project examining emotional consequences of, and care after, death of a relative or friend due to RTAs (TrafVic‐project). Invitation letters for participation were sent to 1,884 people who had been in contact with Victim Support the Netherlands between December 2013 and December 2017 after a relative or friend died due to an RTA. Victim Support is a non‐governmental organization offering practical, judicial, and emotional support to victims after exposure to potential traumatic events. People could also sign up for the study via a website about the TrafVic‐project. In total, 283 people completed the questionnaire; 264 completed questionnaires online (via Qualtrics), and 19 completed paper questionnaires. Ten people had missing data on all variables of interest for this study (i.e., bereavement care needs and use and perceived acceptability of online grief treatment) and were excluded from the analysis yielding a final sample size of 273. The majority of the sample (N = 221, 81%) was recruited via Victim Support, 22 (8%) via social media, 21 (8%) via a family member or friend, and nine (3%) via other pathways. This study was approved by a local ethics committee. Written consent was obtained from all participants.
2.2. Measures
2.2.1. Bereavement care needs and use
Following prior research (Lichtenthal et al., 2015), bereavement care needs and use among the bereaved after an RTA were assessed by asking: “Have you used any of these services related to your loss?” This question was followed by three services: (1) talking with a psychologist, therapist, or psychiatrist; (2) using pharmacotherapy (e.g., antidepressant, mood stabilizer, tranquilliser, or sleep medication), and (3) participation in support groups or peer support meetings. Participants chose one of four answers for each service type: 1 = No, and I don't want to, 2 = No, but I would like to, 3 = Yes, but currently I don't, and 4 = Yes, I still use this service.
2.2.2. Barriers to bereavement care
People who answered with 1, 2, or 3 on each of the three bereavement care needs and use items (i.e., those currently not receiving any bereavement care) were asked to report to what extent 13 potential barriers to bereavement care (cf., Lichtenthal et al., 2015) applied to them on 4‐point scales (ranging from 1 = does not apply to me at all to 4 = strongly applies to me). An example item is “I currently do not receive help from a psychologist, psychiatrist, or support group, because I believe that no one can help me.” We considered barriers rated with 1 or 2 as “barrier absent” and 3 or 4 as “barrier present.”
2.2.3. Preloss psychological support
Professional support obtained from a mental healthcare professional prior to the loss (referred to as “pre‐loss psychological support”) was assessed with one dichotomously rated (yes/no) item, that is, “Did you ever receive support from a psychologist, therapist, or psychiatrist prior to the death of your loved one due to a traffic accident?”
2.2.4. Acceptability of online grief treatment
Acceptability of online grief treatment was assessed with nine items from the Internet‐based Interventions Acceptability Questionnaire (Rai et al., 2013; cf. Arjadi et al., 2018). We replaced the wording referring to “internet‐based intervention for depression” for “online grief treatment.” In the instruction, we gave a description of online grief treatment (see Appendix A). Three items of this measure assessed Behavioural intentions towards online grief treatment (e.g., “If I have access to online grief treatment, I will use it.”), three other items assessed Acceptability of online grief treatment as a substitute for face‐to‐face treatment (e.g., “I am willing to use online grief treatment for monitoring my grief process instead of visiting a local grief therapist.”), and another three items measured the Acceptability of online grief treatment combined with face‐to‐face treatment (e.g., “I am willing to use online grief treatment for exchanging information about my grief process with healthcare providers in addition to visiting a local grief therapist.”). Participant rated their agreement with each item on 7‐point scales (1 = strongly disagree, 7 = strongly agree). Total scores of ≥12 for each subscale were considered as indicating a positive attitude towards use of online grief treatment. Each subscale's Cronbach's alpha was .99.
2.2.5. Openness towards use of innovative technologies
Following prior research (Arjadi et al., 2018), openness towards use of innovative technologies was assessed with three items (e.g., “I like to experiment with new online services”) rated on 7‐point scales (1 = strongly disagree, 7 = strongly agree). Cronbach's alpha of this measure was .99.
2.2.6. Pathological grief
Severity of pathological grief was assessed with the 18‐item Traumatic Grief Inventory‐Self Report (TGI‐SR; Boelen & Smid, 2017b). This measure includes 16 items corresponding to the 16 PCBD symptoms in DSM‐5, plus one item (“feeling stunned/shocked”) assessing a symptom of PGD (as per Prigerson et al., 2009) that is not among the PCBD criteria, and one “functional impairment” item included in both PCBD and PGD criteria. Participants rated the frequency of symptoms (e.g., “I felt strong longing or yearning for the deceased”) during the preceding month on 5‐point scales (1 = never, 5 = always). A total score of >53 is indicative of clinically relevant pathological grief (Boelen et al., 2019). Psychometric properties of TGI‐SR are adequate (Boelen et al., 2019; Boelen & Smid, 2017b). Cronbach's alpha of TGI‐SR was .94.
2.3. Statistical analyses
Descriptive statistics were used to describe needs and use for three bereavement care services separately, including psychotherapy, pharmacotherapy, and support groups (Aim 1). For Aim 2, a series of logistic regression models were built to examine correlates of needs and use (vs. no needs or use) for these three services separately. People who expressed the need for the service under consideration (e.g., psychotherapy) or reported prior or current use of that service were categorized as people needing or using this service. People who reported that they did not use this service and were also not interested in using it were categorized as people not needing or using this service. Next, correlates (i.e., gender, age, educational level, kinship to the deceased, preloss psychological support, and pathological grief levels) of need and use of each of the three services (psychotherapy, pharmacotherapy, and support groups) were examined in three distinct logistical regression models.
People who did not use any of the three services after the loss, while endorsing clinically relevant levels of pathological grief levels (TGI‐SR score of >53) and/or reporting that they would like to use any service (irrespective of grief levels), were categorized as people having unmet care needs; these people were considered to represent the treatment gap (Aim 3). Those who reported that they did not use any service at the time of study completion completed items on barriers to bereavement care. Differences in reported barriers to care between people with and without unmet bereavement care needs were tested using Chi‐square difference tests (Aim 4).
Lastly, with respect to our fifth aim, in three multiple regression models, correlates of acceptability towards online grief treatment were examined, with total scores on the items tapping (1) behavioural intentions, (2) online grief treatment as supplement for face‐to‐face treatment, or (3) online grief treatment as complementary to face‐to‐face treatment from the Internet‐based Interventions Acceptability Questionnaire consecutively treated as dependent variables. The following independent variables were entered simultaneously to the regression models: gender, age, educational level, preloss psychological support, kinship to the deceased, time since loss, openness towards use of innovative technologies, and concurrent pathological grief levels. Tolerance levels were all above .20 and individual variance inflation factors (VIFs) below 10 for the regression models; therefore, there was no reason for concerns about multicollinearity. Analyses were conducted with SPSS version 25 (IBM Corp., 2017).
3. RESULTS
3.1. Participants
Table 1 shows the characteristics of the participants. The sample predominantly consisted of middle‐aged (M = 51.86; SD = 12.95 years) women (76%) who were highly educated (43% obtained a university degree). Ninety‐two percent of the people lost one relative or friend due to an RTA. The majority lost a child (39%) or a partner (22%). The death took place on average 4.73 years (SD = 6.05) ago. Eighty‐nine people (33%) had received support from a psychologist, therapist, or psychiatrist prior to the death of their loved one. About half of the sample (n = 125, 46%) scored above the threshold of >53 for clinically relevant grief on the TGI‐SR.
TABLE 1.
Characteristics of participants (N = 273)
| Gender, N (%) | |
|---|---|
| Male | 67 (24.5) |
| Female | 206 (75.5) |
| Age, M (SD) | 51.86 (12.95) |
| Level of education, N (%) | |
| Lower than university | 156 (57.1) |
| University | 117 (42.9) |
| Preloss psychological support | |
| No | 184 (67.4) |
| Yes | 89 (32.6) |
| Number of people that died due to a road traffic accident, N (%) | |
| 1 | 251 (91.9) |
| 2 | 17 (6.2) |
| 3 | 2 (0.7) |
| 4 | 3 (1.1) |
| Deceased relative is my …, N (%) | |
| Partner/spouse | 59 (21.6) |
| Child | 105 (38.5) |
| Parent | 37 (13.6) |
| Sibling | 47 (17.2) |
| Other | 25 (9.2) |
| Time since loss in years, M (SD) | 4.73 (6.05) |
| IIAQ behavioural intentions, M (SD) | 8.83 (6.00) |
| IIAQ preference to use online as substitute for face‐to‐face grief treatment, M (SD) | 7.40 (5.28) |
| IIAQ preference to use online complementary to face‐to‐face grief treatment, M (SD) | 9.11 (6.43) |
| Personal innovativeness towards online services, M (SD) | 7.11 (4.64) |
| Pathological grief levels, M (SD) | 51.59 (14.83) |
Abbreviation: IIAQ, Internet‐based Interventions Acceptability Questionnaire.
3.2. Aim 1: Bereavement care services needs and use
In total, 172 people (63%) had used (one or more) bereavement care services (i.e., psychotherapy, pharmacotherapy, and/or support group) related to the loss, 74 of whom (27%) were still receiving this care. More specifically, about half of the sample (still) received psychotherapy, one third (still) received pharmacotherapy, and about a quarter (still) participated in support group meetings.
Among people with clinically relevant pathological grief symptoms (N = 125), 87 people (70%) used (one or more) bereavement care services, of which 45 people (36%) still used it. Six out of 10 people (still) received psychotherapy, four out of 10 (still) received pharmacotherapy, and one third (still) participated in support meetings. See Table 2 for an overview.
TABLE 2.
Needs and use of bereavement care services
| Service type | No, and I don't want to | No, but I would like to | Yes, but not anymore | Yes, I still use this |
|---|---|---|---|---|
| Complete sample (N = 272a) | ||||
| Psychotherapy | 90 (33.1) | 33 (12.1) | 102 (37.5) | 47 (17.3) |
| Pharmacotherapy | 185 (68.0) | 5 (1.8) | 45 (16.5) | 37 (13.6) |
| Support group meetings | 158 (58.1) | 52 (19.1) | 42 (15.4) | 20 (7.4) |
| Subsample with clinically relevant pathological grief levels (N = 125) | ||||
| Psychotherapy | 26 (20.8) | 20 (16.0) | 52 (41.6) | 27 (21.6) |
| Pharmacotherapy | 72 (57.6) | 5 (4.0) | 20 (16.0) | 28 (22.4) |
| Support group meetingsa | 52 (41.9) | 37 (29.8) | 23 (18.5) | 12 (9.7) |
Data were missing for one person.
3.3. Aim 2: Correlates of bereavement care needs and use
People who expressed the need to use one of the three services or reported prior or current use of a service were categorized as people needing or using this service. People who reported that they did not use a service and were also not interested in using it were categorized as people not needing or using this service. Three logistic regression analyses were performed to examine correlates (i.e., gender, age, educational level, kinship to the deceased, preloss psychological support, and pathological grief levels) of self‐reported need for or use of psychotherapy, pharmacotherapy, and support groups, respectively. The category of people not needing or using this service was used as reference category. See Table 3 for results.
TABLE 3.
Correlates of needs for or use of bereavement care services (N = 269a)
| Psychotherapy | Pharmacotherapy | Support group | ||||
|---|---|---|---|---|---|---|
| B (SE) | OR | B (SE) | OR | B (SE) | OR | |
| Gender (0 = male, 1 = female) | −0.51 (0.36) | 0.60 | 0.33 (0.36) | 1.39 | −0.09 (0.33) | 0.91 |
| Age in years | −0.04 (0.01) | 0.96** | −0.02 (0.01) | 0.98 | −0.02 (0.01) | 0.98 |
| Educational level (0 = lower than university, 1 = university) | 0.73 (0.32) | 2.07* | 0.47 (0.31) | 1.59 | 0.34 (0.30) | 1.41 |
| Kinship to the deceased (0 = other than partner/child, 1 = partner/child) | −0.06 (0.34) | 0.95 | 0.54 (0.35) | 1.72 | 0.62 (0.33) | 1.85 |
| Time since loss in years | 0.09 (0.04) | 1.09* | 0.01 (0.02) | 1.01 | 0.05 (0.03) | 1.05 |
| Preloss psychological support (0 = no, 1 = yes) | 1.18 (0.35) | 3.24** | 0.88 (0.29) | 2.40** | 0.63 (0.29) | 1.89* |
| Pathological grief levels | 0.07 (0.01) | 1.07*** | 0.04 (0.01) | 1.04*** | 0.05 (0.01) | 1.05*** |
Abbreviation: OR, odds ratio.
Due to missing data for four people on some of the variables, the total sample is 269 instead of 273.
p < .001.
p < .01.
p < .05.
Being younger, having a higher educational level, having experienced the loss longer ago, having obtained psychological support prior to the loss, and reporting higher pathological grief levels significantly increased the likelihood of the self‐reported need for or use of psychotherapy. The strongest predictor was preloss psychological support; people were three times more likely to report the need for or use of psychotherapy if they had received psychological support prior to the loss than people who had not received such preloss psychological support.
Preloss psychological support and higher pathological grief levels were both significantly related to self‐reported need for, or use of pharmacotherapy and self‐reported need for, or use of support groups. Again, preloss psychological support was the strongest predictor in both these analyses. People who received psychological support prior to the loss were two times more likely to report the need for or use of pharmacotherapy and two times more likely to report the need for or use of support groups.
3.4. Aim 3: Magnitude of treatment gap in bereavement care
The total number of people with clinically relevant pathological grief who did not use any of the three services (N = 38) and/or who reported the need for using one of these services (irrespective of grief severity (N = 36) was 52 (19%); these were participants categorized as having unmet bereavement care needs representing the treatment gap in bereavement care.
3.5. Aim 4: Barriers to bereavement care in people with and without unmet bereavement care needs
Barriers to bereavement care were only assessed among 198 people who reported no current use of bereavement care services. The most commonly reported reason for not receiving bereavement care among these people was “I believe I do not have emotional problems that I need help with,” followed by “I think my problems will naturally disappear,” “I find it difficult to find adequate support,” and “I think no one can help me” (see Figure 1).
FIGURE 1.
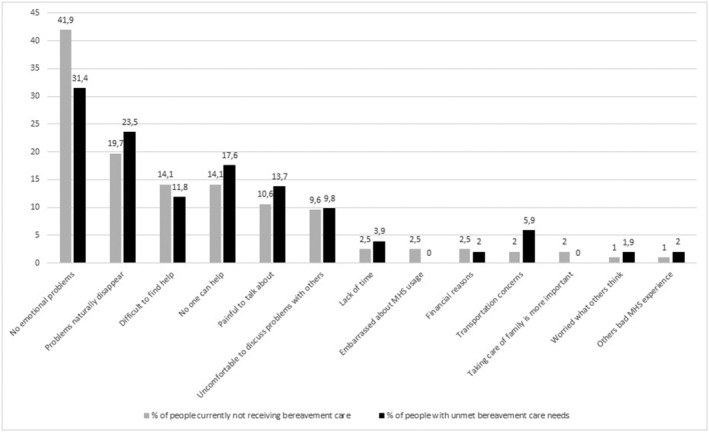
Percentages of reported barriers to bereavement care among people not receiving bereavement care at time of study completion (N = 198) and people with unmet bereavement care needs (N = 52)
The most commonly reported barriers to care for people with unmet bereavement care needs were “I believe I do not have emotional problems that I need help with,” “I think my problems will naturally disappear,” “I think no one can help me,” and “I think is it too painful to talk about the loss” (see Figure 1). Chi‐square difference tests showed that people with unmet bereavement care needs (N = 52) were more likely to report “Transportation concerns” (5.9% vs. 0.7%, χ 2 = 5.18 [1], p = .023) than people without unmet needs (N = 146). No significant differences were found between these groups regarding frequencies of other barriers to care (findings are therefore not reported here).
3.6. Aim 5: Correlates of perceived acceptability of online grief treatment
From the total sample (N = 273), 96 people (35%) reported a positive attitude (score of ≥12) towards the intention to use online grief treatment if in current need of support or if they would be in need of support; 68 people (25%) reported a positive attitude towards online grief treatment as a substitute for face‐to‐face grief treatment; and 100 people (37%) a positive attitude towards online grief treatment supplementing face‐to‐face grief treatment. For the subsample with clinically relevant pathological grief levels (N = 125), these numbers were 49 (39%), 39 (31%), and 48 (38%), respectively.
In three multiple regression analyses, correlates of acceptability of online grief treatment were examined in distinct models with the following dependent variables: (1) behavioural intentions towards online grief treatment, (2) acceptability of online grief treatment as a substitute for face‐to‐face grief treatment, and (3) acceptability of online grief treatment combined with face‐to‐face grief treatment (see Table 4). Findings showed that being more highly educated, having received psychological support prior to the loss, more openness towards innovative online services, and higher pathological grief levels were significantly related to stronger behavioural intentions towards online grief treatment when taking all other background and loss‐related characteristics into account. More openness towards innovative online services and higher pathological grief levels were significantly associated with greater acceptability of online grief treatment as a substitute for face‐to‐face treatment. Being younger, being more highly educated, being more open towards innovative online services, and higher pathological grief levels were significantly related to greater acceptability of online grief treatment combined with face‐to‐face treatment.
TABLE 4.
Correlates of perceived acceptability of online grief treatment (N = 269a)
| Behavioural intentions towards online grief treatment | Acceptability of online grief treatment as a substitute for face‐to‐face treatment | Acceptability of online grief treatment combined with face‐to‐face treatment | ||||
|---|---|---|---|---|---|---|
| B (SE) | β | B (SE) | β | B (SE) | β | |
| Gender (0 = male, 1 = female) | 0.64 (0.76) | .05 | 0.54 (0.69) | .04 | −0.38 (0.83) | −.03 |
| Age in years | −0.04 (0.03) | −.08 | −0.04 (0.03) | −.10 | −0.09 (0.03) | −.18** |
| Educational level (0 = lower than university, 1 = university) | 1.61 (0.69) | .13* | −0.02 (0.63) | −.01 | 2.55 (0.76)** | .20** |
| Kinship to the deceased (0 = other than partner/child, 1 = partner/child) | −0.05 (0.76) | .01 | 0.82 (0.69) | .08 | 1.35 (0.83) | .10 |
| Time since loss in years | 0.01 (0.05) | .01 | −0.01 (0.05) | −.01 | −0.10 (0.06) | −.10 |
| Pre‐loss psychological support (0 = no, 1 = yes) | 2.16 (0.69) | .17** | 0.50 (0.62) | .05 | 1.23 (0.75) | .09 |
| Personal innovativeness towards online services | 0.51 (0.07) | .39*** | 0.50 (0.07) | .44*** | 0.44 (0.08) | .32*** |
| Pathological grief levels | 0.09 (0.02) | .21*** | 0.06 (0.02) | .15** | 0.07 (0.03) | .17** |
Due to missing data for four people on some of the variables, the total sample is 269 instead of 273.
p < .001.
p < .01.
p < .05.
4. DISCUSSION
This is one of few studies examining (correlates of) needs and use of bereavement care in a sample of bereaved people and the first examining this in a traumatically bereaved sample. Our sample consisted of 273 people bereaved by an RTA less than 5 years earlier on average. Moreover, this study is, to the best of our knowledge, also the first that examined perceived acceptability of online grief treatment and correlates thereof.
About half our sample experienced clinically relevant pathological grief levels, which correspond with prevalence rates found in other samples confronted with unnatural loss (Djelantik et al., 2020). Regarding our first aim (i.e., examination of prevalence rates of needs and use of bereavement care), six out of 10 of our sample had used psychotherapy, pharmacotherapy, and/or support meetings related to the loss of their loved one(s). About a quarter of the sample still used one of these services at time of study participation. Psychotherapy was the most frequently used service, followed by pharmacotherapy and attending support group meetings. This aligns with prior research demonstrating that psychotherapy was the most commonly used service, followed by pharmacotherapy and support groups in people bereaved through cancer (Lichtenthal et al., 2015).
By examining correlates of needs and use of bereavement care (Aim 2), we found that use of psychological support prior to the loss was the strongest predictor of bereavement care needs and use after loss. In line with prior research (Lichtenthal et al., 2015), people who received psychological support before the loss were more likely to be interested in receiving bereavement care. Speculatively, this could be explained by at least two reasons. First, people who already received support prior to the loss might be more likely to seek help in the future because they were acquainted with using mental health services and therefore less reluctant to seek professional help. Second, people who sought professional help prior to loss may be more vulnerable for developing grief‐related distress and, thus, be more likely to seek help following the traumatic death of someone close. More research is needed to further examine the role of prior mental health service use in bereavement care.
With respect to our third research aim (i.e., calculating the magnitude of a treatment gap), we found that one out of five participants did not use any of these three services, despite reporting elevated pathological grief levels and/or a need to use one of the services. This finding represents a treatment gap for bereaved people that was also found in prior research (Aoun et al., 2015; Lichtenthal et al., 2015). The most frequently mentioned barriers to bereavement care for these people with unmet needs were being convinced that professional support is not needed, that problems will naturally disappear, and believing that no one can offer the right help were (Aim 4). Similar barriers were identified in prior bereavement research (Lichtenthal et al., 2015). This underutilization of bereavement services may partly be explained by the recency of inclusion of a grief disorder in diagnostic classification systems, including DSM‐5 (APA, 2013; APA, 2020) and the 11th edition of the International Classification of Diseases (ICD‐11; WHO, 2018). The general public may not yet be familiar with these novel diagnoses. Therefore, people may not recognize that their experiences are symptoms of disturbed grief reactions, leading to difficulties in seeking and finding appropriate professional care. Relatedly, many service providers may be unfamiliar with diagnosing and treating grief disorders leading to a reduced availability of appropriate care. More generally, our findings are in accordance with research in general populations in the Netherlands, Canada, and the United States showing that attitudinal barriers (e.g., “No one can help me”) are more common than structural/practical barriers (e.g., financial or transportation obstacles) for mental healthcare utilization (Sareen et al., 2007).
The increased risk for pathological grief after a sudden/violent loss (e.g., Heeke et al., 2019) and our finding that one out of five people has unmet care needs highlights the need to close this treatment gap. Scaling up interventions is one of the main strategies of the World Health Organization to address the treatment gap. Offering online grief treatment might be one way of scaling up interventions for bereaved people with unmet care needs (Kazdin, 2017; WHO, 2010). Prior studies have shown promising effects of online grief treatment for the alleviation grief‐related mental health problems (e.g., Eisma et al., 2015; Kersting et al., 2013; Wagner et al., 2006). However, only one third of the total sample, and four out of 10 of the subgroup with elevated pathological grief levels, reported that they intended to use online grief treatment if they were in need of support. Notably, the acceptability of online grief treatment was higher for the online treatment combined with face‐to‐face treatment than for online treatment as substitute for face‐to‐face treatment. Examining correlates of acceptability of online grief treatment showed that more openness towards innovative online services and higher pathological grief levels were related to increased acceptability of online grief treatment (Aim 5), which accords with prior research in people with depression (Arjadi et al., 2018). Prior research in German patients with depression also found low acceptance rates of internet‐based interventions (Ebert et al., 2015). Interestingly, Ebert et al. (2015) found that acceptability of internet invention substantially increased in this patient group after watching a 7‐min video in which information about an internet treatment for depression was provided by an expert and a patient. For instance, acceptance rates were higher among those who reported higher rates of expected ease of use of the intervention and higher rates of usefulness of the intervention, which is in line with theoretical work (Davis, 1989). Accordingly, it might be valuable to explore similar methods for bereaved people, to increase the uptake of online grief treatment. Our findings also suggest that other ways of addressing the treatment gap are needed for bereaved people with unmet care needs, for instance using social media or trained volunteers for delivery of interventions (cf., Kazdin, 2017).
The following limitations should be taken into account when interpreting our findings. First, this study included a voluntary response sample. In general, people with higher grief levels may be more likely to participate, which may have overestimated symptom levels. Furthermore, our sample included people bereaved by an RTA; results may therefore not generalize to people bereaved by other causes. Second, the study was conducted in the Netherlands. The Dutch mental healthcare system may not be comparable with other countries. Costs for psychological support are often (partly) refundable from health insurances for Dutch citizens. Prevalence rates of service use in our study may therefore be higher compared with other countries that do not refund costs. Third, we did not assess what specific type of service (e.g., what type of psychotherapy or pharmacotherapy) people used, for how long they had used it, whether they found it helpful, or why they stopped using it. This information could have provided more insights for clinicians and researchers aiming to reduce barriers to care. Fourth, barriers to care were assessed with a questionnaire that was developed in the context of prior research (Lichtenthal et al., 2015). Although this measure was designed in the context of bereavement research, the psychometric properties of this instrument are unknown. Using a validated generic instrument to assess barriers to care, such as the Barriers to Access to Care Evaluation Scale (Clement et al., 2012), would allow comparisons of findings across studies conducted in diverse contexts. In addition, the questionnaire that we used consisted of a list of predefined barriers of care. Future qualitative research, using open‐ended questions (e.g., “What hindered you the most when seeking bereavement care?”), may enrich our understanding on challenges that bereaved people face while seeking care. Fifth, including intrapersonal factors (e.g., anxious attachment; Lichtenthal et al., 2015; perceived stigma; Eisma et al., 2019), that are susceptible to change, as predictors for use of bereavement care services and acceptability of online grief treatment could have provided more knowledge on factors that could be targeted in interventions to increase the uptake of service use in bereavement care. Lastly, a self‐report questionnaire, instead of a clinical interview, was used to assess pathological grief symptoms, which may have led to an overestimation symptom levels (cf. Lim et al., 2018).
In conclusion, bereavement due to an RTA is a risk factor for pathological grief. The vast majority of our sample was interested in, or had already received, bereavement care of which psychotherapy was the most commonly used service. One in five people with pathological grief and/or a self‐reported need for using bereavement care had not received any bereavement support. This treatment gap could potentially partly be reduced by increasing accessibility of online grief treatment. However, more than half of participants were not open to using online grief treatment, despite preliminary evidence illustrating the effectiveness of such treatment. It therefore seems worthwhile for researchers and clinicians to focus on increasing the acceptability of (online) services that may help to reduce the treatment gap in bereavement care.
ACKNOWLEDGEMENTS
We would like to thank Victim Support the Netherlands for their help with recruitment of participants. Fund Victim Support (in Dutch Fonds Slachtofferhulp) subsidized this work.
APPENDIX A. INTRODUCTION IIAQ
In an online treatment, bereaved people are informed about psychological problems after a death of a loved one due to a road traffic accident and are supported in dealing with these problems. People participating in online treatment are asked to complete assignments online, so that a psychologist could monitor the grief process and could offer you support.
The therapy is focused on people who experience severe and persistent grief complaints after a loss. These people experience impairments in daily life and therefore seek professional psychological support.
We are interested in your opinion about this type of online treatment. When you currently experience few grief complaints, we are still interested in what you would do when you would experience such severe grief complaints that you would like professional support.
Lenferink LIM, de Keijser J, Eisma MC, Smid GE, Boelen PA. Treatment gap in bereavement care: (Online) bereavement support needs and use after traumatic loss. Clin Psychol Psychother. 2021;28:907–916. 10.1002/cpp.2544
DATA AVAILABILITY STATEMENT
The data are not publicly available due to privacy or ethical restrictions.
REFERENCES
- American Psychiatric Association . (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Publishing. 10.1176/appi.books.9780890425596 [DOI] [Google Scholar]
- American Psychiatric Association . (2020). View and comment on recently proposed changes to DSM–5. Retrieved from https://www.psychiatry.org/psychiatrists/practice/dsm/proposed-changes
- Aoun, S. M., Breen, L. J., Howting, D. A., Rumbold, B., McNamara, B., Hegney, D., & Maulik, P. (2015). Who needs bereavement support? A population based survey of bereavement risk and support need. PLoS ONE, 10(3), e0121101. 10.1371/journal.pone.0121101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arjadi, R., Nauta, M. H., & Bockting, C. L. H. (2018). Acceptability of internet‐based interventions for depression in Indonesia. Internet Interventions, 13, 8–15. 10.1016/j.invent.2018.04.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boelen, P. A., Djelantik, A. A. A. M. J., de Keijser, J., Lenferink, L. I. M., & Smid, G. E. (2019). Further validation of the traumatic grief inventory‐self report (TGI‐SR): A measure of persistent complex bereavement disorder and prolonged grief disorder. Death Studies, 43(6), 351–364. 10.1080/07481187.2018.1480546 [DOI] [PubMed] [Google Scholar]
- Boelen, P. A., & Smid, G. E. (2017a). Disturbed grief: Prolonged grief disorder and persistent complex bereavement disorder. BMJ, 357, j2016. [DOI] [PubMed] [Google Scholar]
- Boelen, P. A., & Smid, G. E. (2017b). The Traumatic Grief Inventory Self Report version (TGI‐SR): Introduction and preliminary psychometric evaluation. Journal of Loss and Trauma, 22(3), 196–212. 10.1080/15325024.2017.1284488 [DOI] [Google Scholar]
- Breen, L. J., & Moullin, J. C. (2020). The value of implementation science in bridging the evidence gap in bereavement care. Death Studies, 1–9. 10.1080/07481187.2020.1747572 [DOI] [PubMed] [Google Scholar]
- Clement, S., Brohan, E., Jeffery, D., Henderson, C., Hatch, S. L., & Thornicroft, G. (2012). Development and psychometric properties the barriers to access to care evaluation scale (BACE) related to people with mental ill health. BMC Psychiatry, 12(1). 10.1186/1471-244X-12-36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis, F. D. (1989). Perceived usefulness, perceived ease of use, and user acceptance of information technology. MIS Quartely, 13(3), 319–340. 10.2307/249008 [DOI] [Google Scholar]
- Djelantik, A. A. M. J., Smid, G. E., Mroz, A., Kleber, R. J., & Boelen, P. A. (2020). The prevalence of prolonged grief disorder in bereaved individuals following unnatural losses: Systematic review and meta regression analysis. Journal of Affective Disorders, 265, 146–156. 10.1016/j.jad.2020.01.034 [DOI] [PubMed] [Google Scholar]
- Doering, B. K., & Eisma, M. C. (2016). Treatment for complicated grief: State of the science and ways forward. Current Opinion in Psychiatry, 29(5), 286–291. 10.1097/YCO.0000000000000263 [DOI] [PubMed] [Google Scholar]
- Dorow, M., Löbner, M., Pabst, A., Stein, J., & Riedel‐Heller, S. G. (2018). Preferences for depression treatment including internet‐based interventions: Results from a large sample of primary care patients. Frontiers in Psychiatry, 9. 10.3389/fpsyt.2018.00181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ebert, D. D., Berking, M., Cuijpers, P., Lehr, D., Pörtner, M., & Baumeister, H. (2015). Increasing the acceptance of internet‐based mental health interventions in primary care patients with depressive symptoms. A randomized controlled trial. Journal of Affective Disorders, 176, 9–17. 10.1016/j.jad.2015.01.056 [DOI] [PubMed] [Google Scholar]
- Eisma, M. C., Boelen, P. A., Van den Bout, J., Stroebe, W., Schut, H., Lancee, J., & Stroebe, M. (2015). Internet‐based exposure and behavioral activation for complicated grief and rumination: A randomized controlled trial. Behavior Therapy, 46(6), 729–748. 10.1016/j.beth.2015.05.007 [DOI] [PubMed] [Google Scholar]
- Eisma, M. C., Te Riele, B., Overgaauw, M., & Doering, B. (2019). Does prolonged grief or suicide bereavement cause public stigma? A vignette‐based experiment. Psychiatry Research, 272, 784–789. 10.1016/j.psychres.2018.12.122 [DOI] [PubMed] [Google Scholar]
- Gauthier, L., & Gagliese, L. (2012). Bereavement interventions, end‐of‐life cancer care, and spousal well‐being: A systematic review. Clinical Psychology: Science and Practice, 19(1), 72–92. 10.1111/j.1468-2850.2012.01275.x [DOI] [Google Scholar]
- Heeke, C., Kampisiou, C., Niemeyer, H., & Knaevelsrud, C. (2019). A systematic review and meta‐analysis of correlates of prolonged grief disorder in adults exposed to violent loss. European Journal of Psychotraumatology, 8(sup6), 1583524. 10.1080/20008198.2019.1583524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- IBM Corp . (2017). IBM SPSS statistics for windows, version 25.0. Armonk, NY: IBM Corp. [Google Scholar]
- Johannsen, M., Damholdt, M. F., Zachariae, R., Lundorff, M., Farver‐Vestergaard, I., & O'Connor, M. (2019). Psychological interventions for grief in adults: A systematic review and meta‐analysis of randomized controlled trials. Journal of Affective Disorders, 253, 69–86. 10.1016/j.jad.2019.04.065 [DOI] [PubMed] [Google Scholar]
- Kazdin, A. E. (2017). Addressing the treatment gap: A key challenge for extending evidence‐based psychosocial interventions. Behaviour Research and Therapy, 88, 7–18. 10.1016/j.brat.2016.06.004 [DOI] [PubMed] [Google Scholar]
- Kersting, A., Dölemeyer, R., Steinig, J., Walter, F., Kroker, K., Baust, K., & Wagner, B. (2013). Brief internet‐based intervention reduces posttraumatic stress and prolonged grief in parents after the loss of a child during pregnancy: A randomized controlled trial. Psychotherapy and Psychosomatics, 82(6), 372–381. 10.1159/000348713 [DOI] [PubMed] [Google Scholar]
- Kristensen, P., Weisæth, L., & Heir, T. (2012). Bereavement and mental health after sudden and violent losses: A review. Psychiatry, 75(1), 76–97. 10.1521/psyc.2012.75.1.76 [DOI] [PubMed] [Google Scholar]
- Lenferink, L. I. M., Boelen, P. A., Smid, G. E., & Paap, M. C. S. (2019). The importance of harmonising diagnostic criteria sets for pathological grief. British Journal of Psychiatry, 1–4. 10.1192/bjp.2019.240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li, L. P., Jaladin, R. A. M., & Abdullah, H. S. (2013). Understanding the two sides of online counseling and their ethical and legal ramifications. Procedia ‐ Social and Behavioral Sciences, 103, 1243–1251. 10.1016/j.sbspro.2013.10.453 [DOI] [Google Scholar]
- Lichtenthal, W. G., Corner, G. W., Sweeney, C. R., Wiener, L., Roberts, K. E., Baser, R. E., Li, Y., Breitbart, W., Kissane, D. W., & Prigerson, H. (2015). Mental health services for parents who lost a child to cancer: If we build them, will they come? Journal of Clinical Oncology, 23(20), 2246–2254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lim, G., Tam, W., Lu, Y., Ho, C., Zhang, M., & Ho, R. (2018). Prevalence of depression in the community from 30 countries between 1994 and 2014. Scientific Reports, 8(1), 2861. 10.1038/s41598-018-21243-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lundorff, M., Holmgren, H., Zachariae, R., Farver‐Vestergaard, I., & O'Connor, M. (2017). Prevalence of prolonged grief disorder in adult bereavement: A systematic review and meta‐analysis. Journal of Affective Disorders, 212, 138–149. 10.1016/j.jad.2017.01.030 [DOI] [PubMed] [Google Scholar]
- Prigerson, H. G., Horowitz, M. J., Jacobs, S. C., Parkes, C. M., Aslan, M., Goodkin, K., Raphael, B., Marwit, S. J., Wortman, C., Neimeyer, R. A., Bonanno, G. A., Block, S. D., Kissane, D., Boelen, P., Maercker, A., Litz, B. T., Johnson, J. G., First, M. B., & Maciejewski, P. K. (2009). Prolonged grief disorder: Psychometric validation of criteria proposed for DSM‐V and ICD‐11. PLoS Medicine, 6(8), e1000121. 10.1371/journal.pmed.1000121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rai, A., Chen, L., Pye, J., & Baird, A. (2013). Understanding determinants of consumer mobile health usage intentions, assimilation, and channel preferences. Journal of Medical Internet Research, 15(8), e149. 10.2196/jmir.2635 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sareen, J., Jagdeo, A., Cox, B. J., Clara, I., Ten, H., Belik, S. L., de Graaf, R., & Stein, M. B. (2007). Perceived barriers to mental health service utilization in the United States, Ontario, and the Netherlands. Psychiatric Services, 58(3), 357–364. 10.1176/ps.2007.58.3.357 [DOI] [PubMed] [Google Scholar]
- Simblett, S., Matcham, F., Siddi, S., Bulgari, V., Barattieri, D., Hortas López, J., Ferrão, J., Polhemus, A., Haro, J. M., de Girolamo, G., Gamble, P., Eriksson, H., Hotopf, M., Wykes, T., & RADAR‐CNS Consortium . (2019). Barriers to and facilitators of engagement with mhealth technology for remote measurement and management of depression: Qualitative analysis. JMIR mHealth and uHealth, 7(1), e11325. 10.2196/11325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagner, B., Knaevelsrud, C., & Maercker, A. (2006). Internet‐based cognitive‐behavioral therapy for complicated grief: A randomized controlled trial. Death Studies, 30(5), 429–453. 10.1080/07481180600614385 [DOI] [PubMed] [Google Scholar]
- Wagner, B., Rosenberg, N., Hofmann, L., & Maass, U. (2020). Web‐based bereavement care: A systematic review and meta‐analysis. Frontiers in Psychiatry, 11. 10.3389/fpsyt.2020.00525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson, D., Dhanji, N., Playfair, R., Nayak, S., Puplampu, G., & Macleod, R. (2017). A scoping review of bereavement service outcomes. Palliative & Supportive Care, 15(2), 242–259. 10.1017/S147895151600047X [DOI] [PubMed] [Google Scholar]
- World Health Organization (WHO) . (2010). Nine Steps for Developing a Scaling‐Up Strategy. Geneva. Accessed on October 7, 2020 via: WHO Press. https://www.google.com/url?sa=t%26rct=j%26q=%26esrc=s%26source=web%26cd=%26ved=2ahUKEwiFvJOb0aLsAhWB2aQKHRUGAxQQFjAAegQIAhAC%26url=https%3A%2F%2Fwww.who.int%2Fimmunization%2Fhpv%2Fdeliver%2Fnine_steps_for_developing_a_scalingup_strategy_who_2010.pdf%26usg=AOvVaw2H24iw-pg8ITR_9OX9vZdm [Google Scholar]
- World Health Organization (WHO) . (2018). ICD‐11. Prolonged Grief Disorder Criteria. Accessed on April 1, 2020 via: https://icd.who.int/browse11/l-m/en#/http://id.who.int/icd/entity/1183832314
- World Health Organization (WHO) . (2019). The top 10 causes of death. Accessed on April 1, 2020 via: https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data are not publicly available due to privacy or ethical restrictions.


