Abstract
Background:
Yoga is gaining popularity as a multisystem intervention due to its impact on both the physical and mental well-being of children with typical development. However, there is limited empirical evidence to support the use of this approach in school-aged children with Autism Spectrum Disorder (ASD). The current pilot study evaluated the impact of a creative yoga intervention on the joint attention, social communication, and affective states of children with ASD.
Methods:
24 school-aged children with ASD received eight weeks of yoga (e.g., breathing, poses, relaxation) or tabletop play/academic intervention (e.g., reading, arts-crafts, building activities). Children were tested before and after the intervention using a standardized measure of responsive joint attention. Additionally, changes in socially directed verbal communication and affective states of children were assessed three times during the intervention period, i.e. during early, mid, and late intervention sessions.
Results:
Children with ASD showed improvements in responsive joint attention in both groups in the posttest vs. the pretest. Furthermore, children in the yoga group showed improvements in socially directed verbal communication skills across the intervention sessions, i.e. greater spontaneous and responsive communication from early/mid to late intervention sessions compared to the academic group. There were no changes in affective states with the intervention, however, the yoga group showed greater interested and less negative affect compared to the academic group.
Conclusions:
Creative yoga intervention is a promising tool that led to improvements in intervention-related social communication skills and generalized joint attention skills of children with ASD.
Keywords: Autism, yoga, verbal communication, joint attention, affect, children
1. Introduction
Yoga, a mind-body intervention (Wahbeh et al., 2008), is an effective alternative to standard therapeutic tools used to promote physical and mental well-being of children (Barnes et al., 2008). Yoga is becoming increasingly popular in school and therapeutic settings due to its cost-effective and minimalistic nature (i.e., requires a limited number of supplies to implement) (Serwacki & Cook-Cottone, 2012). Moreover, it is a multisystem therapeutic approach due to its varied effects on the perceptuo-motor (e.g., flexibility, strength, and balance) (Galantino et al., 2008; Serwacki & Cook-Cottone, 2012), behavioral (e.g., attention and alertness) (Lawson, 2012; Peck et al., 2005), and social skills of children (e.g., social relationships, speech, and affect) (Beauchemin et al., 2008; Harrison et al., 2004). For these reasons, yoga could be a valuable intervention tool for children with atypical development including those with Autism Spectrum Disorder (ASD). Below, we provide a brief overview of ASD-specific impairments in social communication and affective/behavioral skills, followed by the current evidence on the effects of yoga in individuals with ASD.
Socially directed verbal communication impairments are a primary impairment in children with ASD (American Psychiatric Association, 2013) with children’s communication skills ranging from being completely non-verbal to highly verbal with use of full sentences (Eigsti et al., 2011; Tager-Flusberg & Caronna, 2007). Moreover, many children with ASD have difficulties with socially directed verbalizations, with more difficulties in spontaneous initiation of verbal communication than “responsive” verbalizations that involve responding to questions and comments of others (Condouris et al., 2003; Vismara & Rogers, 2010). Specifically, lower rates and less variety of spontaneous speech is reported in subgroups of children with ASD compared to typically developing children (Tager-Flusberg et al., 2005). Moreover, some children with ASD use echolalic speech (repetition/echoing of words and phrases heard in the past), self-directed speech, and speech monologues instead of engaging in socially directed communication (i.e., spontaneous sharing of information or responding to questions or instructions) (Eigsti et al., 2011).
Children with ASD may also present with non-verbal communication difficulties in initiating and responding to joint attention bids (Bean & Eigsti, 2012; Leekam & Ramsden, 2006; MacDonald et al., 2006; Mundy et al., 2007). Joint attention is the ability to share attention with others about objects or events in the environment, for example, a child directing their parents’ attention to a toy by pointing to it (i.e., spontaneous joint attention) or a child turning their head towards a picture on the wall after the parent pointed to it (i.e., responsive joint attention) (Mundy et al., 2007). Using early childhood joint attention measures such as the Early Social Communication Scales (ESCS), it is known that children with ASD do not follow the eye gaze or pointing gestures of others compared to mentally-age matched children with developmental delays and/or children with typical development (TD) (Bean & Eigsti, 2012; Leekam & Ramsden, 2006; MacDonald et al., 2006; Mundy et al., 2007). Furthermore, using the only standardized test of joint attention for school-aged children i.e., the Joint Attention Test (JTAT), children with ASD between 7 and 17 years respond less frequently to the gestural (i.e. bids initiated using eye contact, pointing) and verbal bids (i.e. bids initiated using verbal labels) initiated by a tester compared to chronologically- and mentally-age matched children with TD (Bean & Eigsti, 2012).
In addition, children with ASD frequently present with comorbid impairments in affective/emotional expression and regulation. They may have odd/flat facial expressions or few variations in emotional expressions while interacting and playing with their peers (Dawson et al., 1990; Reddy et al., 2002; Stagg et al., 2013). This can impact the child’s ability to form social connections with peers, as was evident from the low friendship ratings given to children with ASD by their peers with TD (Stagg et al., 2013). Taken together, children with ASD show varying levels of difficulties in socially directed verbal communication, joint attention, and emotional expression/regulation which could negatively impact their ability to engage in meaningful interactions, build peer relationships, as well as learn new skills from others.
There is some anecdotal evidence for the effects of yoga in reducing maladaptive behaviors (Goldberg, 2004; Koenig et al., 2012; Rosenblatt et al., 2011) and improving social skills of children with ASD (Ehleringer, 2010; Kenny, 2002; Radhakrishna, 2010). In terms of behavioral skills, 16 weeks of class room yoga including breathing, poses, relaxation, and chanting reduced the maladaptive behaviors such as irritability, lethargy, and hyperactivity in children with ASD as measured by a teacher-rated behavior checklist, the Aberrant Behavior Checklist (ABC), with no similar improvements in the control group (Koenig et al., 2012). However, the teachers were not blinded to the grouping of the child which may have contributed to a response bias. Similarly, eight weeks of integrated intervention including yoga, music, and dance in children with ASD indicated positive effects on various subscales of two parent-rated behavior checklists including the Atypicality, Depression, and Irritability subscales (Rosenblatt et al., 2011). In terms of social skills, there is a lack of empirical evidence for the social effects of yoga in children with ASD. However, based on qualitative reports teachers indicated increased socialization attempts such as greater social proximity, smiling, and vocalizations in children with ASD following regular practice of yoga (Ehleringer, 2010; Kenny, 2002; Radhakrishna, 2010).
Although the current yoga literature is limited in children with ASD, evidence from other typical and atypical populations suggests positive effects of yoga on the emotional regulation and attentional focus of children (Daly et al., 2015; Peck et al., 2005). A randomized controlled trial (RCT) involving high-school children showed improvements in emotional regulation such as the ability to identify self and others’ emotional states in adolescents who underwent the yoga intervention compared to the physical education group (Daly et al., 2015). Additionally, neuroimaging and electrophysiological studies have shed light on the impact of yoga on the emotional processing abilities of yogis. For example, prolonged practice of yoga/meditation led to increased activation in the medial/orbitofrontal cortices, i.e. regions important for emotional processing (Hölzel et al., 2007) as well as lower responses to negative emotional stimuli (or lower event-related potentials) (Sobolewski et al., 2011). Similarly, children with attentional deficits between 6 and 10 years increased the percent of eye contact with their teacher as well as increased attentional focus on the class activities after 3 weeks of yoga intervention delivered twice a week (Peck et al., 2005). These improvements in attentional focus of children have been attributed to the changes in the functioning of the autonomic nervous system. To elaborate, regular practice of yoga impacts both the branches of autonomic nervous system by increasing the activation of the parasympathetic and reducing the activation of the sympathetic nervous system (Peck et al., 2005). Specifically, increased parasympathetic nervous system activity during relaxation states conserves energy, reduces heart rate, increases calmness, and improves concentration and attentional focus in children.
Overall, yoga appears to be a promising adjuvant therapeutic tool for children with ASD, but there is a clear need for rigorous empirical studies investigating the multisystem effects of yoga using standardized clinical outcome measures and reliable video coding of behaviors. Therefore, the primary purpose of this research was to conduct a pilot study examining the effects of a “creative yoga” intervention on the motor, socially-directed verbal communication skills, and affective states of children with ASD compared to a comparison group that received tabletop play activities or an “academic intervention”. We term our approach as “creative yoga” because the key components of yoga (i.e. poses, breathing, relaxation, etc.) were made fun and creative using age-appropriate songs, stories, games, and props. The “academic intervention” involved therapeutic activities that are often offered to children with ASD in standard special education settings including activities to promote fine-motor and communication skills through reading, building, art-craft, etc. The current manuscript discusses the intervention effects on the social communication behaviors including joint attention and socially directed verbalization as well as affective states of children with ASD. The motor/imitation skill effects of yoga or academic interventions for children with ASD have been reported in the Kaur & Bhat, 2019 publication. We hypothesized that children in both the groups will improve their socially directed verbal communication as well as joint attention skills following the intervention because both interventions involve interacting and attending to social partners throughout the sessions. Furthermore, we hypothesized that children in the yoga group will show greater interested/task-appropriate affect or positive (i.e., smiles) affect following the intervention due to its regulatory effects on behaviors and emotions of children in general and those with ASD.
2. Methods
2.1. Participants
Twenty-four children with ASD between 5 and 13 years of age participated in the study (i.e., 12 children in the yoga group and 12 children in the academic group) (Table 1). We estimated our sample size based on our past pilot RCT involving children with ASD who received similar multisystem, movement-based interventions (Srinivasan et al, 2015, 2016a). Previous RCT findings indicated large intervention-related effect using standard mean difference (SMD=0.78) for the primary outcome of socially directed verbalization with an N of 12 children per group (Srinivasan et al., 2016a). We had already enrolled 12 children with ASD in the standard of care, comparison group as part of the previous trial and they served as a comparison group for the present study. In this study, we mainly recruited 12 more children for the yoga group and expected large effects for socially directed verbal communication given the strong effects we reported previously in a similar sized sample. Children were recruited by distributing fliers at the local schools, clinical services, and through online postings with the local parent and family advocacy groups. We had a relatively higher proportion of males in this study (11 males:1 female) compared to the nationally representative proportion (4-5 males: 1 female) (Maenner et al., 2020); however, sex distributions did not differ across the two groups. Children in both groups provided demographic data (i.e. age, sex, socioeconomic status), were assessed for autism severity (i.e. ADOS-2 comparison scores) (Lord et al., 2012), as well as level of cognitive, adaptive functioning, and motor abilities (i.e. IQ scores, adaptive behaviors, motor skills; Table 1) (Bruininks & Bruininks, 2005; Roid, 2003; Sparrow et al., 2005). We ensured that the 12 children in the yoga group were matched on age, autism severity, and level of functioning to the academic, comparison group. The socioeconomic status scores were calculated using the Hollingshead Scale, and majority of the families belonged to upper or upper-middle class, except 1 family was lower-middle and 3 families were middle class (Hollingshead, 1975). In terms of ethnicity, there is a relatively higher proportion of Asian families (5 out of 11) in the yoga group compared to the academic group (1 out of 12, Table 1a). Next, for autism severity, there were no differences between the yoga and the academic group based on ADOS-2 comparison scores (Table 1b). Lastly, in terms of level of functioning, Stanford Binet Intelligence Scale-5th Edition (SBIT) was used to assess the cognitive functioning (Roid, 2003), Vineland Adaptive Behavior Scales-2nd Edition (VABS-II) to assess the adaptive functioning and communication skills (Sparrow et al., 2005), and short form of Bruininks-Oseretsky Test of Motor Proficiency-2nd Edition (BOT-2) to assess the baseline level of motor functioning (Bruininks & Bruininks, 2005). Children in both the groups did not differ in terms of their baseline cognitive, adaptive, communication, and motor functioning and continued to receive standard of care, school-based interventions described in their Individualized Education Plans (Table 1b). All parents signed the consent form approved by the University of Delaware’s Institutional Review Board before participating in the study.
Table 1a.
Group demographics (age, sex, socioeconomic status, ethnicity).
| Characteristic | Yoga | Academic | p a | ||
|---|---|---|---|---|---|
| # of participants |
Mean ± SE | # of participants |
Mean ± SE | ||
| Age | 7.84 + 0.54 | 7.80 + 0.70 | 0.96 | ||
| 5 – 6 yr | 4 | 4 | 1.00 | ||
| 7 – 8 yr | 4 | 5 | |||
| 9 – 10 yr | 2 | 2 | |||
| 11 – 12 yr | 1 | 1 | |||
| Sex | |||||
| Males | 10 | 11 | 0.95 | ||
| Females | 1 | 1 | |||
| Socioeconomic Status (SES) | 56.0 + 2.33 | 52.46 + 2.9 | 0.37 | ||
| Upper | 2 | 1 | 0.65 | ||
| Upper-middle | 8 | 8 | |||
| Middle | 1 | 2 | |||
| Lower-middle | 0 | 1 | |||
| Ethnicity | |||||
| White | 6 | 9 | 0.3 | ||
| Asian | 5 | 1 | |||
| African American | 0 | 1 | |||
| Hispanic | 0 | 1 | |||
p determined by t-test or X2 test.
Table 1b.
Group demographics (level of functioning and yoga experience).
| Characteristic | Yoga | Academic | p a | ||
|---|---|---|---|---|---|
| # of participants |
Mean ± SE | # of participants |
Mean ± SE | ||
| ADOS-2b | 8.27 + 0.49 | 8.67 + 0.53 | 0.73 | ||
| High | 9 | 10 | 1.00 | ||
| Moderate | 2 | 2 | |||
| Low | 0 | 0 | |||
| Minimal to no | 0 | 0 | |||
| SB5c | 86.27 + 5.62 | 82.92 + 8.02 | 0.74 | ||
| High Average | 1 | 4 | 0.11 | ||
| Average | 5 | 0 | |||
| Low Average | 1 | 2 | |||
| Borderline | 1 | 2 | |||
| Extremely Low | 3 | 4 | |||
| VABS-IId (adaptive) | 81.18 + 4.83 | 75.92 + 5.32 | 0.47 | ||
| High | 0 | 0 | 0.95 | ||
| Moderately High | 0 | 0 | |||
| Adequate | 5 | 4 | |||
| Moderately Low | 2 | 4 | |||
| Low | 4 | 4 | |||
| VABS-IId (communication) | 89.55 + 6.0 | 83.5 + 6.28 | 0.49 | ||
| High | 0 | 0 | 0.84 | ||
| Moderately High | 1 | 0 | |||
| Adequate | 6 | 6 | |||
| Moderately Low | 1 | 2 | |||
| Low | 3 | 4 | |||
| BOT-SFe | 37.46 + 2.29 | 39.30 + 3.12 | 0.64 | ||
| Above average | 0 | 0 | 0.61 | ||
| Average | 2 | 4 | |||
| Below Average | 7 | 6 | |||
| Well-below Average | 2 | 2 | |||
| Yoga Experience | 2 | 0 | |||
p determined by t-test or X2 test.
ADOS-2 = Autism Diagnostic Observation Schedule, Second Edition. Comparison scores of ADOS-2 were used to gauge autism severity. The scores range from 0 to 10 with higher score indicating greater autism severity.
SB5 = Stanford-Binet Intelligence Scales, Fifth Edition. Intelligence quotient (IQ) scores were used to assess the cognitive functioning. IQ scores had a normative mean of 100 and an SD of 15.
VABS-II = Vineland Adaptive Behavior Scales, Second Edition (VABS-II). The adaptive scores assess the communication, social, and daily living skills of children. The scores had a normative mean of 100 and an SD of 15.
BOT-SF = Bruininks-Oseretsky Test of Motor Proficiency - 2nd Edition, Short Form
2.2. Inclusion/Exclusion Criteria
The inclusion criteria for the study was: a) ages between 5 and 13 years, b) school/medical record confirming an ASD diagnosis or a social communication delay on the Social Communication Questionnaire, and c) ADOS-2 criteria met for ASD. The exclusion criteria was a) significant behavioral problems such as aggression, non-compliance, inability to stay on task based on pretest performance, b) receptive communication impairments such as inability to follow simple, two-step commands based on pretest performance. Additionally, participation was terminated if the child could not complete 50% of the intervention sessions (i.e., 8 out of 16 expert sessions). Note that four children met the aforementioned exclusion criteria after pretesting; hence, were excluded from the study. One other child was excluded when he did not meet the intervention criteria of completing at least 50% of the intervention sessions (see Figure 1 for number of subjects screened and enrolled in the study).
Figure 1:
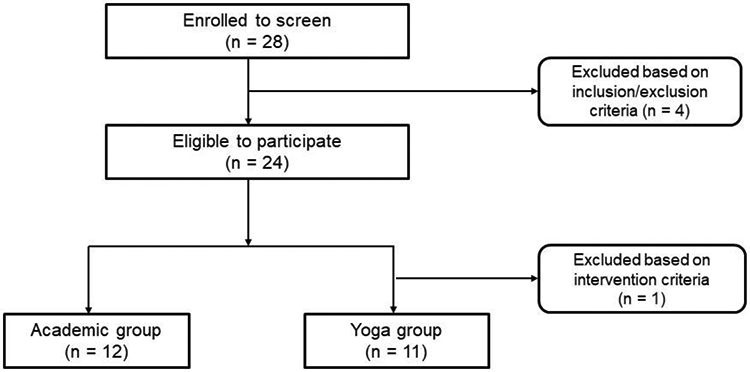
Flow chart indicating the subjects screened and enrolled for study participation.
2.3. Study Procedure
Parents who expressed interest in the study completed an initial screening process to determine eligibility for participation. The initial screening included a parent completing the Social Communication Questionnaire (SCQ), a screening tool for ASD (Rutter et al., 2003) and providing a medical/school record of their child’s diagnosis; however, not all children met criteria for social communication delay on the SCQ. Hence, each child’s eligibility was further confirmed by administering the Autism Diagnostic Observation Schedule-Second Edition (ADOS-2) (Lord et al., 2012). ADOS-2 is a gold standard assessment for autism diagnosis and provides a total algorithm score that can be used to derive a comparison score ranging from 1-10. The ADOS comparison score provides a measure of ASD severity with higher scores indicating greater ASD severity. The ADOS-2 was administered by the last author who is research reliable on the ADOS-2 with the test creator, Dr. Lord’s team. An ASD diagnosis was confirmed for all 24 children using ADOS-2 with comparison scores ranging from 5 to 10 indicating moderate to high autism severity (Table 1).
The study lasted for ten weeks with pre/posttest sessions in the 1st and 10th week, and eight weeks of intervention delivered from 2nd to 9th week of participation. Intervention consisted of two expert-led and two parent-led sessions each week (for a total of 16 expert and 16 parent-led sessions). Expert-led sessions lasted ~45 minutes and were delivered by the first author who is a pediatric physical therapist. Parent sessions lasted ~30 minutes and were delivered by mothers. Pre/Posttest sessions during the 1st and 10th week involved a series of standardized assessments measuring gross/fine motor, imitation, and joint attention skills conducted by doctoral students with a background in physical or occupational therapy who were blinded to group assignment. The results for the motor and imitation assessments for the current study sample are discussed in another manuscript (Kaur & Bhat, 2019). All pre/posttest and expert-led intervention sessions were videotaped for later coding. Behavioral coding was conducted by trained and reliable undergraduate research coders.
2.4. Intervention Procedure
Both yoga and academic intervention included expert and parent sessions. The expert sessions involved a triadic context, i.e. a child with ASD, a trainer, and an adult model (Figure 2). The trainer was responsible for conducting the session and guiding the child through the activities. The adult model acted as a buddy for the child and helped the trainer in delivering the sessions. All trainers and models ensured intervention fidelity by adhering to the standard protocol for majority of the sessions (yoga = 95.51% + 0.41; academic = 91.38% + 0.90; p > 0.05). The parents were provided with instructional videos, manuals, and one-on-one training from the trainer to deliver the two additional sessions at home each week. Using an intervention diary, both trainers and parents logged their intervention days and timeframes. In both the groups, all children completed far more than the 50% cut-off for total intervention sessions completed (yoga = 71.59% + 3.73; academic = 80.21% + 4.41; p > 0.05), except one child in the yoga group who completed only 25% of the total sessions. As mentioned earlier, this child was excluded from the final analysis resulting in 11 children in the yoga group compared to 12 children in the academic group.
Figure 2:
Intervention setup indicating the triadic context during the (a) yoga and (b) academic interventions.
Children practiced different set of activities within the yoga and the academic group (Table 2). The yoga group practiced activities such as breathing, poses, partner poses, and relaxation, as well as activities focused on the needs of children with ASD such as greetings, contact, and looking games (Table 2). A variety of age-appropriate contexts such as songs, stories, and games were used to make the yoga sessions fun and engaging for children. The academic group engaged in several sedentary, tabletop activities typically commonly offered within academic settings such as reading books, building games, and art/craft activities to promote fine-motor and communication skills (Table 2). Similar to the yoga sessions, substantial efforts were made to make the seated play sessions engaging for children by using daily themes such as solar system, people, animals, transport, foods, etc. In both groups, children were frequently offered reinforcement through verbal and gestural praise (e.g., hi-fives, “good job”), choice between activities (e.g., bee breathing or snake breathing), breaks and preferred activities (e.g., iPad break, stickers) to ensure task compliance and behavioral regulation during the sessions. To ensure intervention fidelity, trainers were instructed to follow the standard guidelines for delivering prompts and reinforcements via a fidelity checklist (see Kaur & Bhat, 2019 for details on Intervention Fidelity Checklist). Additionally, common ASD intervention strategies such as session structure through use of same space and materials, consistency in instruction, procedures, and people involved in the intervention, and visual picture schedules were used to provide session structure, repetition and reinforcement, and manual/visual feedback. Note: More information about the intervention protocol, fidelity checklist, and exemplar videos are available in our previous publication (Kaur & Bhat, 2019).
Table 2.
Intervention activities practiced during the yoga and the academic group.
| Yoga group | Academic group |
|---|---|
| Hello: Child sings a song together with the trainer and the model. | Hello: Child greets the model and the trainer. |
| Breathing: Child practices breathing exercises with or without props (eg, sniffing flowers, blowing pinwheels). | Reading: Child reads an age-appropriate book with the trainer and the model, while taking turns with them. |
| Contact & Looking: Child practices social touch (eg, joining hands or feet to form a shape). Child practices eye/head movements towards social and non-social stimuli (eg, looking at bouncing ball). | Building: Child builds various creations using building supplies such as Play-Doh,a LEGO,b and ZOOBc (eg, Lego car, Play-Doh snow man). |
| Poses/Partner poses: Children practices poses on their own and together with the trainer and the model. | Arts & Crafts: Child makes various creations by coloring/painting/drawing, as well as cutting and pasting. |
| Relaxation: Child lies down and remains still while a pre-recorded verbal imagery plays in the background. | Clean up: Child helps the trainer and model to clean up the working station. |
| Bye: Child bids farewell by singing a song together with the trainer and the model. | Bye: Child bids farewell to the trainer and the model. |
Hasbro, Pawtucket, RI, USA.
The LEGO Group, Billund, Denmark.
Alex Brands, Fairfield, CT, USA.
Note: Original Source Kaur & Bhat, 2019
2.5. Study Measures
2.5.1. Joint Attention Test (JTAT).
The JTAT was designed by the middle author’s group to assess changes in responsive joint attention in school-aged children (Bean & Eigsti, 2012). It is the only standardized measure of joint attention available for school-aged children with ASD and is validated for children between 7 and 17 years and has an inter-reliability of 94%. (Bean & Eigsti, 2012). Moreover, JTAT has been successfully used in our past published study in school-aged children with ASD (Srinivasan et al, 2016a). JTAT was administered during the pretest (1st week) and posttest session (10th week). The testers were blinded to group assignments and interacted with the child only during the pre/posttest sessions. During the session, the child was seated across from the tester and the tester initiated 9 different naturalistic bids, including 4 verbal (e.g., Look at that!) and 5 gestural bids (e.g., waving hand to say bye) to evoke a response from the child (see Table 3). If the child did not respond to the tester’s bids, the tester employed different levels of cueing depending on the social bid. The JTAT measure is scored in two ways: a) for the child’s response to the bid (i.e. response score) and b) for any additional cues the tester must provide to obtain a response from the child (i.e., cue level score). Both, the response scores and cue level scores were summed to calculate a total JTAT score.
Table 3.
Joint Attention Test (JTAT) bids to evoke responsive joint attention in the participant
| S. No | JTAT Bids |
|---|---|
| Verbal Bids | |
| 1. | Look at the poster on the side |
| 2. | Look at the poster in the back |
| 3. | Look at novel object on the floor |
| 4. | Look at a personal item (e.g. child’s pants, shirt etc.) |
| Gestural Bids | |
| 5. | Shake hands or wave “Hi” |
| 6. | Ask for a. hi-five |
| 7. | Ask for a low-five |
| 8. | Hand a pen |
| 9. | Wave “Bye” |
Response Scores on the JTAT.
The child’s response to 7 of the 9 JTAT bids received a score of 1 to 4 based on the following criteria, a) Correct action received 1 point if the child accurately responded to the bid, e.g., for ‘wave bye’, child raises his/her hand to wave bye to the tester, b) Looking at the face/appropriate direction received 1 point if the child looked in the direction of tester’s attentional focus, e.g., looking at the painting on the wall in response to the tester’s bid, c) Eye contact received 1 point if the child made eye contact with the tester while responding to the bid, and d) Verbal response received 1 point if the child responded to the tester by producing spontaneous verbiage. 2 of the 9 bids (“wave hi” and “wave bye”) also offer an additional point for smiling (Table 3). Therefore, the total response scores could range from 0 (worst performance) to 38 (best performance) i.e., 7*4+2*5=38.
Cue Level Scores.
There were different levels of cueing involved depending on the social bid: a) Level 1 Cue involved the most general social bid with minimal cues, e.g., Saying “Look at that!” and looking in the direction of a poster on the wall, b) Level 2 Cue involved an explicit calling of the child’s name, e.g., “Hey Joey! Look at that!”, c) Level 3 Cue involved even more explicit cues of calling the child’s name and labeling the object of tester’s attentional focus, e.g., “Hey Joey! Look at that poster!” Higher level cueing (Levels 2 or 3) were offered only if the child was unable to respond to lower level cueing in a 10-second period. The cue level at which the child responded to the tester’s bids was recorded, i.e. Level 1, 2, or 3, and scored in reverse by assigning a higher score if a child responded appropriately to a lower cue level (i.e. score of 3 for Level 1, 2 for Level 2, 1 for Level 3, and 0 for no response). While 8 out of the 9 bids had 3 levels of responding, 1 bid was a follow-up question to another bid, and so involved a single level for which the child could receive a single point. Therefore, the total cue scores could range from 0 (worst performance) to 25 (best performance) i.e., 8*3+1.
2.5.2. Socially Directed Verbal Communication.
Socially directed communication included the time the child spent speaking/verbalizing or vocalizing to social partners (i.e. the trainer and the model) for the duration of the intervention session. Datavyu behavioral coding software (http://datavyu.org) was used to code the child’s verbalization/vocalizations from videotaped early (session 1), mid (session 8), and late (session 16) expert sessions. The coders identified the start and stop time of the child’s verbalization (i.e. words, phrases, and sentences) and vocalization bouts (i.e. humming while singing, breath sounds produced in the context of the task, etc.) directed towards the trainer/model. Any instances of echolalia or stereotypical verbalizations/vocalizations produced by the child were not considered within the total duration of child’s socially directed communication. For example, spontaneous, unprovoked repetition of words, phrases, and sounds such as scripting of songs or statements related to favorite TV shows were not considered socially directed communication. Next, coders coded these bouts as spontaneous (initiated by the child) or responsive (in response to questions asked by the trainer/model). The coded files were run through a custom MATLAB program (MATLAB Inc., Natick, MA) to calculate the percent duration of socially directed, spontaneous and responsive verbalizations/vocalizations produced by the child for each intervention session.
2.5.3. Affective/Behavioral States.
The child’s affective/behavioral states were also coded for the early (session 1), mid (session 8), and late (session 16) expert sessions. There were three types of affective/behavioral states: a) positive affect/behavior or periods of smiling, b) negative affect/behavior or period of pouting, frowning, crying, and yelling, etc. and (c) interested or task-appropriate affect/behavior or periods of on-task behaviors while being compliant with the trainer’s requests and without clear positive or negative affect/behaviors. Datavyu software was used to code the start and end times of each behavior and the coded files were run through a custom MATLAB program (MATLAB Inc., Natick, MA) to calculate the percent duration of positive, negative, and interested affect.
3. Statistical Analysis
For the total JTAT score, a repeated measures Analysis of Variance (ANOVA) was conducted with pre/posttest session (pretest, posttest) as the within-subjects factor, and group (yoga, academic) as the between-subjects factor. Similarly, for socially directed verbal communication, a repeated measures ANOVA with behavior type (spontaneous, responsive) and intervention session (early, mid, late) as the within-subjects factors, and group (yoga, academic) as the between-subjects factor was conducted. Finally, for the affective state variable, the repeated measures ANOVA included behavior type (positive, negative, interested) and intervention session (early, mid, late) as the within-subjects factors, and group (yoga, academic) as the between-subjects factor. The data were checked for parametric assumptions using the Mauchly’s Test of Sphericity and Greenhouse-Geisser corrections were applied in case of violations. The significance for the ANOVA model was set at p ≤ 0.05, and main/interaction effects were further analyzed using post-hoc t-tests. If there was a significant main effect and an interaction involving the same factor, t-tests were conducted for the significant interactions only. In case of significant 2-way and 3-way interactions involving the same factors, t-tests were conducted only for the 3-way interactions. For less than three post-hoc comparisons, significance was set at 0.05, with p-values between 0.05 and 0.1 considered statistical trends. In case of 3 or more post-hoc comparisons, Bonferroni corrections were applied to adjust the level of significance and p-values between adjusted p-values and 0.05 are reported as statistical trends because the trends were always similar to the significant differences. The main or interaction effect sizes are reported using partial eta-squared with partial η2 < 0.01 indicating a small effect, partial η2 < 0.06 indicating a medium effect, and partial η2 < 0.14 indicating a large effect. Within or between-group effect sizes are reported using the Cohen’s d, with d > 0.2 indicating a small effect, d > 0.5 indicating a medium effect, and d > 0.8 indicating a large effect. We are also reporting the proportion of children in each group that improved performance more than minimally important difference (MID) = 0.2*pooled baseline SD across both groups.
4. Results
4.1. JTAT
The repeated measures ANOVA for JTAT revealed a significant main effect of pre/posttest session (F1,20 = 16.61, p < 0.05, partial η2 = 0.45 or large effect), with no group interaction. The post-hoc test for the main effect indicated that when JTAT data were pooled across both groups, children improved their total JTAT scores in the posttest session (39.09 ± 1.47) compared to the pretest session (35.23 ± 1.67) following both interventions (p < 0.05, d = 0.51 or a medium effect, % academic group > MID = 45.5% and % yoga > MID = 72.7%). In terms of missing data, one child in the academic group is missing JTAT data due to non-compliance during the session.
4.2. Socially directed verbal communication (Figure 3)
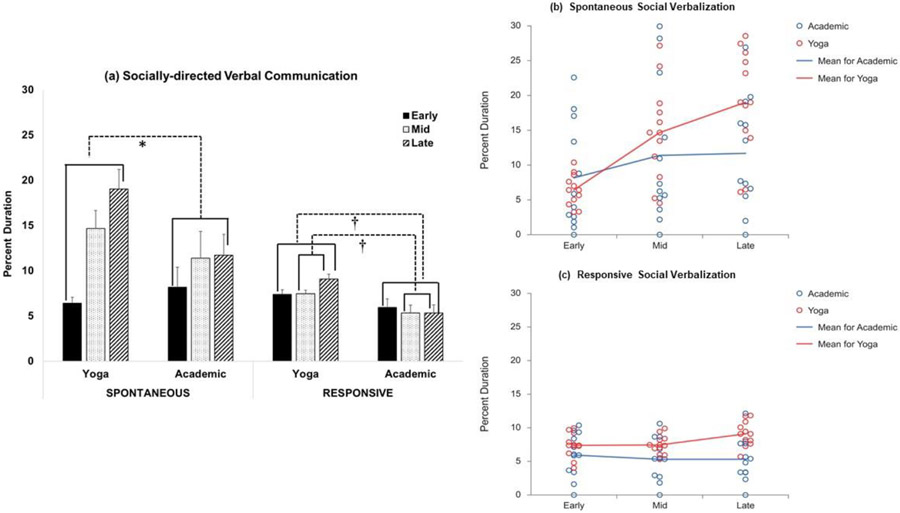
Figure 3:
(a) Bar graphs for percent duration of socially directed verbal communication shown by children in the yoga and the academic group during the early, mid, and late intervention sessions. *indicates significant differences with p-values less than the adjusted p-value thresholds after Bonferroni corrections, †indicates statistical trends with p-values between 0.05 and the adjusted p-value thresholds after Bonferroni corrections. Note that the magnitude of improvement in spontaneous verbalization between early to late session is greater for the yoga group compared to the academic group. Similarly, the magnitude of improvement in responsive verbalization between early to late and mid to late sessions is greater for the yoga compared to the academic group. (b) Scatter plots for percent duration of spontaneous social verbalization and (c) responsive social verbalization for the yoga and the academic groups during the early, mid, and late intervention sessions. The red and blue circles represent the individual data points for the yoga and academic group, respectively.
The repeated measures ANOVA for socially directed verbal communication indicated a significant main effect of intervention session (F2,44 = 22.08, p < 0.01, partial η2 = 0.50) and verbalization type (F1,22 = 17.45, p < 0.01, partial η2 = 0.44 or large effect), 2-way interactions of session x group (F2,44 = 9.49, p < 0.01, partial η2 = 0.30 or large effect) and session x verbalization type (F2,44 = 20.42, p < 0.01, partial η2 = 0.48 or large effect), and lastly 3-way interaction of session x verbalization type x group (F2,88 = 3.76, p = 0.03, partial η2 = 0.15 or large effect). The 3-way session x verbalization type x group interaction was further analyzed to examine between-group changes, i.e. change in socially directed verbalizations from early to mid/late session across the yoga and the academic group. The improvement in spontaneous social verbalization from early to late intervention session was significantly greater in the yoga (12.60 ± 2.11, % intervention-related increase in yoga group > MID = 90%) compared to the academic group (3.53 ± 1.12; p < 0.008 after Bonferroni corrections for 6 comparisons, d = 1.23 or large effect, % intervention-related increase in academic group > MID = 81.8%). Similarly, the improvement in responsive social verbalization from early to late intervention session was greater in the yoga (1.70 ± 0.60, % intervention-related increase in yoga group > MID = 70%) compared to the academic group (−0.63 ± 0.66; p = 0.02, Bonferroni adjusted p < 0.008 for 6 comparisons, d = 0.96 or large effect, % intervention-related increase in the academic group > MID = 45.5%). Additionally, the improvement in responsive social verbalization from mid to late intervention session was greater in the yoga (1.63 ± 0.40; % intervention-related increase in the yoga group > MID = 40%) compared to the academic group (−0.002 ± 0.62; p = 0.04, Bonferroni adjusted p < 0.008 for 6 comparisons, d = 0.84 or large effect, % intervention-related increase in the academic group > MID = 18.2%). In terms of missing data, one child in the yoga group was completely non-verbal and hence, was not included in this analysis.
4.3. Affective/behavioral state (Figure 4)
Figure 4:
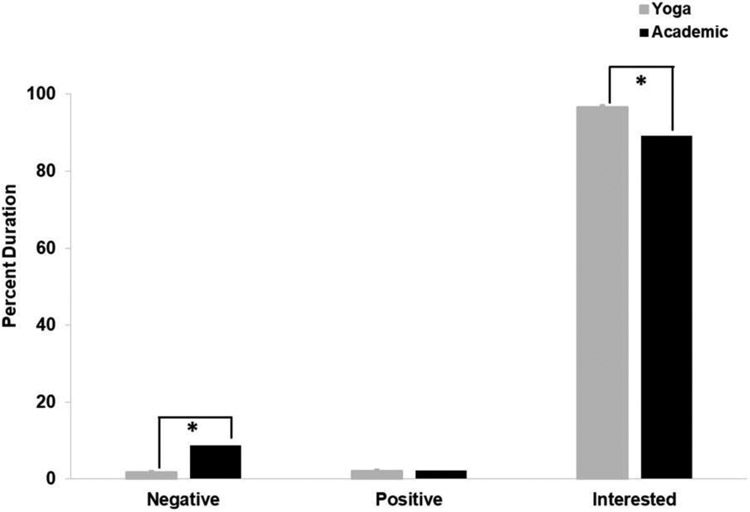
Bar graphs for percent duration of interested, positive, and negative affective states in the yoga and academic groups. *indicates significant differences with p-values less than the adjusted p-value thresholds after Bonferroni corrections.
The repeated measures ANOVA for affect indicated a significant main effect of affective state (F2,44 = 749.81, p < 0.01, partial η2 = 0.97 or large effect), and a significant affective state x group interaction (F2,44 = 3.67, p = 0.03, partial η2 = 0.14 or large effect). We further analyzed the 2-way affect x group interaction to examine the between-group differences in affective states. Children in the yoga group showed less negative affect (Bonferroni adjusted p < 0.02 after 3 comparisons, d = 0.70 or large effect) and greater interested affect (Bonferroni adjusted p < 0.02 after 3 comparisons, d = 0.72 or large effect) compared to the academic group throughout the intervention, with no differences in positive affect. To be clear, there were no significant interactions involving session x group which means that children in both groups did not change their affective states following intervention. However, the yoga intervention evoked more interested and less negative affect compared to the academic group.
5. Discussion
The current study compared the effects of an eight weeks creative yoga intervention to a tabletop play/academic intervention on the responsive joint attention, socially directed verbalizations, and affective states of school-aged children with ASD. In terms of responsive joint attention changes, children in both groups improved their total JTAT scores in the posttest session compared to the pretest session. In terms of socially directed verbal communication changes, the yoga group showed greater improvements in both spontaneous and responsive verbalization compared to the academic group during the late compared to early intervention session. In terms of affective states, there were no intervention-related changes in the affective states for the yoga or the academic group. However, the yoga group had overall less negative affect and greater interested/task-appropriate affect compared to the academic group during the intervention sessions
5.1. Effects on the Joint Attention Skills of Children with ASD
Children with ASD in both groups showed medium effect size improvements in their responsive joint attention skills during the posttest compared to the pretest session. These improvements could be attributed to changes in social monitoring and attentional focus of children following the intervention. Specifically, throughout the intervention, children in both groups were engaged in activities requiring continuous monitoring and responding to the cues of the trainer. Additionally, the looking games practiced during the yoga sessions involved eye movement exercises through isolated eye or head movements as well as following of the trainer’s command to attend to the trainer, model, or objects in the surroundings. Similarly, the building and art-craft games practiced during the seated play sessions required children to look and follow the trainers to complete the tasks. This provided ample opportunities to the children to share their attention and engage in joint attention bids with the trainers during the intervention. It was encouraging to see that children generalized these improvements to a standardized assessment administered by a novel tester during the posttest sessions, which could be related to the inherently engaging, play-based nature of both interventions. A systematic review of the joint attention interventions in children with ASD recommended use of play as a natural context to improve and generalize the joint attention skills of children as these contexts are inherently motivating and offer natural reinforcements to the child (White et al., 2011). Similarly, in the current study, use of several child-appropriate themes and games delivered within a social play-based context helped in generalizing the joint attention skills of children to novel people and assessment during the posttest session.
To date, one study with children with ASD has reported improvements in the social gaze of children with ASD following an intensive 20-month yoga intervention (Radhakrishna, 2010). Additionally, the yoga trainers in the same study reported qualitative improvements in the social skills of children with ASD such as increased attempts of social proximity with the trainers following the intervention (Radhakrishna, 2010). Although the evidence is limited in children with ASD, studies in children with attentional deficits show that yoga improved the attentional focus of children (Abadi et al., 2008; Lawson, 2012; Peck et al., 2005). Children with attentional deficits between 6 and 10 years increased the percent of eye contact with their teacher as well as increased focus on the class activities after 3 weeks of yoga intervention delivered twice a week (Peck et al., 2005). Similarly, Lawson (2012) reported improvements in on-task behaviors of children with attentional problems following 5 weeks of yoga therapy compared to the no intervention, control group. Taken together, practice of yoga poses, stretches, and breathing exercises can positively impact the attentional focus of school-aged children with ASD.
5.2. Effects on the Communication Skills of Children with ASD
Children in the yoga group showed a greater increase in their spontaneous and responsive verbalizations compared to the academic group during the mid/late intervention sessions. Our baseline data from the communication subscales of the VABS indicated significant communication challenges in our study participants. Hence, it was encouraging to see that children spent greater time in spontaneous or self-initiated communication during the later yoga sessions which could be attributed to the playful nature of the intervention resulting in high levels of engagement and spontaneous verbalizations. Both the trainers and the coders noted that children would initiate conversations about general topics such as their day at school as well as ask specific questions regarding the different intervention activities practiced during the sessions. Our findings fit with the results from a systematic review comparing the traditional adult-led to the more contemporary, child-led language interventions in ASD suggesting that child-led activities practiced within a play-based setting are effective in improving the language skills of children with ASD (Delprato, 2001). It is also possible that children’s growing familiarity with the trainers could have led to increased levels of socially directed verbalizations in the late compared to early and mid-intervention sessions, however, similar increases would be expected in the academic group as well.
This is the first systematic study reporting the positive effects of yoga intervention on the social communication skills of children with ASD. Greater improvements in the spontaneous and responsive verbalization skills during yoga sessions compared to academic sessions could also be attributed to the nature of activities practiced within both the groups. Firstly, yoga was a novel context for majority of the children (9 out of 11 children in the yoga group had no prior yoga experience, Table 1b) as these activities are usually not included in the standard interventions offered to children with ASD compared to the academic group activities which are often practiced at school and/or home. It is likely that the novelty and engaging nature of the creative yoga themes motivated the children to initiate conversations with the trainers. Secondly, within-group improvements in communication skills of children in the yoga group could be related to the motoric demands of the yoga intervention activities. There is growing evidence of motor impairments such as poor posture and balance, incoordination, and gait difficulties in children with ASD (Bhat et al., 2011; Kaur et al., 2018). Therefore, it is possible that during the initial intervention sessions, children were focused on learning and mastering the yoga poses/partner poses practiced during the sessions, and were unable to perform a dual-task of moving and communicating simultaneously. However, as reported in our earlier publication, with improvements in the imitation of yoga poses and the bilateral motor coordination skills of children following the yoga intervention (Kaur & Bhat, 2019); children may be better equipped to handle the challenge of moving and verbalizing/vocalizing simultaneously. Overall, it is encouraging to see that movement-based interventions using the creative yoga approach could positively impact the socially directed verbal communication skills of children during the intervention sessions.
5.3. Effects on the Affective States of Children with ASD
Children in both groups showed greatest interested affect throughout the intervention sessions suggesting that children were willing to do the activities practiced within both types of sessions (i.e., yoga and academic intervention). As mentioned earlier, all our intervention activities were built around engaging, age-appropriate themes such as stories, songs, and games, which clearly motivated the children to comply with the trainers and complete the activities. There were no changes in the interested affective states of children across both groups perhaps due to a ceiling effect; majority of the children showed high levels of interested affect throughout the intervention sessions, and, hence, did not have much scope for further improvement. Based on trainer’s observations, yoga activities promoted a calm and self-regulated demeanor/ emotional state. For this reason, it is not surprising that the yoga intervention did not evoke many smiles/positive affect. Instead, it encouraged more self-regulation/compliance and few negative behaviors such as running away, tantrums, etc.
Across the two groups, children in the yoga group showed greater interested and lower negative affect compared to children in the academic group. Note that interested affect indicated task compliance (i. e., states without any positive or negative affect). This could be attributed to the enjoyable nature of the creative yoga approach using songs, stories, or games to provide more context to the key components of yoga (i.e., poses, breathing, and relaxation). Additionally, the positive effects of yoga itself may have contributed to the high levels of interested affect in the study participants. Yoga has been implemented in several school curriculums to improve the affective/emotional awareness, regulation, and reactivity of children and adolescents (Daly et al., 2015; Felver et al., 2015; Serwacki & Cook-Cottone, 2012). For example, a randomized controlled trial conducted within a public high school showed improvements in emotional regulation such as the ability to identify self and others’ emotional states in adolescents who underwent the yoga intervention compared to the physical education group (Daly et al., 2015). Similarly, ninth and tenth graders reported reduced negative affect, tension, fatigue, and anger after a single yoga session composed of breathing, poses, and relaxation compared to when they participated in a single physical education session of sports and aerobic activity (Felver et al., 2015). Taken together, yoga-based activities evoked more compliant affective/behavioral state and less negative affect compared to the standard of care academic intervention.
5.4. Clinical Implications
ASD is a multisystem disorder leading to varied levels of impairments in social communication (e.g., poor social eye contact and peer relationships, lack of socially-directed spontaneous or responsive verbalization) and behavioral skills (e.g., repetitive mannerisms) (American Psychiatric Association, 2013; Tager-Flusberg & Caronna, 2007) as well as motor comorbidities (e.g., poor posture and limb and body coordination) (Bhat et al., 2011; Bhat, 2020, 2021; Kaur et al., 2013, 2018). Typically, the verbal and non-verbal communication and behavioral impairments of children with ASD are addressed through intensive, sedentary play contexts. However, results from the current study suggest that movement-based contexts such as creative yoga evoke more compliant affective states and improve both joint attention and socially directed spontaneous and responsive verbal communication skills of children with ASD. Moreover, our previous paper reported improvements in gross motor skills such as bilateral coordination and task-related imitation performance in children with ASD following the yoga intervention (Kaur & Bhat, 2019). Our past work has also reported positive effects of music and movement on the verbal communication, joint attention skills, and affective states of children with ASD following intervention (Srinivasan et al., 2015, 2016a, 2016b; Kaur et al., 2013; Srinivasan et al., 2013a, 2013b). Taken together, clinicians such as physical therapists and occupational therapists should consider using yoga and other creative movement approaches in their clinical practice due to their multisystem effects. Improving motor performance may lead to cascading effects on other affected systems including social communication (verbal communication, positive affect, social attention) and cognitive systems (executive functioning skills of planning, organizing attention, response inhibition). Overall, socially embedded movement games delivered using engaging contexts such as stories, songs, and games offer excellent opportunities for multisystem development in children with ASD.
5.5. Study Limitations and Future Directions
Clinicians and therapists should be cognizant of the preliminary nature of the study and be cautious while interpreting the results due to limitations such as small sample size, wide age range, and lack of random assignment and follow-up tests. Moreover, information about medications, diagnostic history, and comorbidities of children were not collected; which could affect each participant’s intervention responsivity. However, several measures such as demographic information (age, sex, socioeconomic status; see Table 1a for details) and level of functioning (cognitive, adaptive, motor; see Table 1b for details) were collected to better conceptualize the study results.
In the future, we recommend conducting larger randomized controlled trials with better control of confounding factors (e.g., level of functioning, autism severity, etc.) in children with wide-ranging autism-specific symptomology to further evaluate the effects of creative yoga in ASD. Similar to the present study, we recommend use of standardized outcome measures and/or behavioral coding of sessions to further validate use of yoga in other pediatric populations. Lastly, it will be imperative to conduct short-term and long-term follow up to evaluate the maintenance of intervention effects.
6. Conclusions
The primary goal of the pilot study was to compare the effects of a creative yoga intervention with a seated table-top, academic intervention on the social communication, joint attention, and motor skills of school-aged children with ASD. Our results show that yoga intervention leads to generalized and intervention-specific improvements in the joint attention and socially directed verbalizations of children with ASD and is a feasible intervention for school-aged children with ASD. In terms of generalized improvements, both groups improved their responsive joint attention skills when tested using a standardized assessment administered by a novel tester. In terms of intervention-specific improvements, the yoga intervention evoked interested/task-appropriate affect and improved socially directed verbal communication skills of children across sessions compared to the academic intervention. Given the high prevalence and the multisystem impairments of ASD, creative intervention contexts such as yoga could be beneficial for children with ASD due to its positive impact on their social communication and motor performance.
Highlights.
Effects of yoga or academic intervention were compared in school-age children with ASD.
Children in the Yoga group showed greater improvements in spontaneous and responsive socially-directed verbalization compared to the academic group.
Both groups showed improvements in responsive joint attention skills.
Yoga evoked less negative and more task-appropriate affect.
Yoga intervention enhances social verbalization and joint attention skills of children with ASD and should be included within their standard of care.
Acknowledgments
We would like to thank the research assistants at University of Delaware who helped in behavioral coding of the study variables. We would also like to thank all the children and caregivers who participated in the study. The first author’s efforts on this manuscript were supported by the University Graduate Fellows Award from University of Delaware and Research Sundry Funds from MGH Institute of Health Professions. The last author’s efforts on this manuscript were supported by the Institutional Development Award from the National Institute of General Medical Sciences of the National Institutes of Health (Grant #s: U54-GM104941, P20-GM103446) (PI: S. Binder-Macleod, S. Stanhope), the Dana Foundation Clinical Neuroscience Award, and the National Institutes of Mental Health (Grant #: 1R01-MH125823-01, PI: A. Bhat). The funders played no role in the design, conduct, or reporting of this study.
Footnotes
Conflict of Interest
Authors have no conflict of interest to report.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Abadi MS, Madgaonkar J, & Venkatesan S (2008). Effect of yoga on children with attention deficit/hyperactivity disorder. Psychological Studies, 53(2), 154–159. https://psycnet.apa.org/record/2009-02359-012 [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders, 5th Edition: DSM-5 (5th ed.). American Psychiatric Publishing. [Google Scholar]
- Barnes PM, Bloom B, & Nahin RL (2008). Complementary and alternative medicine use among adults and children: United States, 2007. National Health Statistics Reports, 12, 1–23. https://pubmed.ncbi.nlm.nih.gov/19361005/ [PubMed] [Google Scholar]
- Bean JL, & Eigsti I-M (2012). Assessment of joint attention in school-age children and adolescents. Research in Autism Spectrum Disorders, 6(4), 1304–1310. 10.1016/j.rasd.2012.04.003 [DOI] [Google Scholar]
- Beauchemin J, Hutchins TL, & Patterson F (2008). Mindfulness meditation may lessen anxiety, promote social skills, and improve academic performance among adolescents with learning disabilities. Complementary Health Practice Review, 13(1), 34–45. 10.1177/1533210107311624 [DOI] [Google Scholar]
- Bhat AN, Landa RJ, & Galloway JCC (2011). Current Perspectives on Motor Functioning in Infants, Children, and Adults with Autism Spectrum Disorders. Physical Therapy, 91(7), 1116–1129. 10.2522/ptj.20100294 [DOI] [PubMed] [Google Scholar]
- Bhat A (2020) Is Motor Impairment in ASD Distinct from Developmental Coordination Disorder (DCD)? A Report from the SPARK study. Physical Therapy. 100 (4): 633–644. 10.1093/ptj/pzz190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhat A (2021) Motor Impairment Increases in Children With Autism Spectrum Disorder as a Function of Social Communication, Cognitive and Functional Impairment, Repetitive Behavior Severity, and Comorbid Diagnoses: A SPARK Study Report. Autism Research. 14(1):202–219. 10.1002/aur.2453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruininks RH, & Bruininks BD (2005). Bruininks-Oseretsky Test of Motor Proficiency - 2nd Edition. Minneapolis, MN: NCS Pearson. [Google Scholar]
- Capps L, Kehres J, & Sigman M (1998). Conversational abilities among children with autism and children with developmental delays. Autism, 2(4), 325–344. 10.1177/1362361398024002 [DOI] [Google Scholar]
- Condouris K, Meyer E, & Tager-Flusberg H (2003). The relationship between standardized measures of language and measures of spontaneous speech in children with autism. American Journal of Speech-Language Pathology, 12(3), 349–358. 10.1044/1058-0360(2003/080) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daly LA, Haden SC, Hagins M, Papouchis N, & Ramirez PM (2015). Yoga and emotion regulation in high school students: A randomized controlled trial. Evidence-Based Complementary and Alternative Medicine, 2015, 1–8. 10.1155/2015/794928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson G, Hill D, Spencer A, Galpert L, & Watson L (1990). Affective exchanges between young autistic children and their mothers. Journal of Abnormal Child Psychology, 18(3), 335–345. 10.1007/bf00916569 [DOI] [PubMed] [Google Scholar]
- Delprato DJ (2001). Comparisons of discrete-trial and normalized behavioral language intervention for young children with autism. Journal of Autism and Developmental Disorders, 31(3), 315–325. 10.1023/a:1010747303957 [DOI] [PubMed] [Google Scholar]
- Ehleringer J (2010). Yoga for children on the autism spectrum. International Journal of Yoga Therapy, 20(1), 131–139. 10.17761/ijyt.20.1.eu176u2721423510 [DOI] [Google Scholar]
- Eigsti I-M, de Marchena AB, Schuh JM, & Kelley E (2011). Language acquisition in autism spectrum disorders: A developmental review. Research in Autism Spectrum Disorders, 5(2), 681–691. 10.1016/j.rasd.2010.09.001 [DOI] [Google Scholar]
- Felver JC, Butzer B, Olson KJ, Smith IM, & Khalsa SBS (2014). Yoga in public school improves adolescent mood and affect. Contemporary School Psychology, 19(3), 184–192. 10.1007/s40688-014-0031-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galantino ML, Galbavy R, & Quinn L (2008). Therapeutic effects of yoga for children: A systematic review of the literature. Pediatric Physical Therapy, 20(1), 66–80. 10.1097/pep.0b013e31815f1208 [DOI] [PubMed] [Google Scholar]
- Goldberg L (2004). Creative RelaxationSM: A yoga-based program for regular and exceptional student education. International Journal of Yoga Therapy, 14(1), 68–78. 10.17761/ijyt.14.1.50524j511674v292 [DOI] [Google Scholar]
- Harrison LJ, Manocha R, & Rubia K (2004). Sahaja yoga meditation as a family treatment programme for children with Attention Deficit-Hyperactivity Disorder. Clinical Child Psychology and Psychiatry, 9(4), 479–497. 10.1177/1359104504046155 [DOI] [Google Scholar]
- Hollingshead A (1975). Four factor index of social status. New Haven, CT: Yale University. (Unpublished Manuscript). [Google Scholar]
- Hölzel BK, Ott U, Hempel H, Hackl A, Wolf K, Stark R, & Vaitl D (2007). Differential engagement of anterior cingulate and adjacent medial frontal cortex in adept meditators and non-meditators. Neuroscience Letters, 421(1), 16–21. 10.1016/j.neulet.2007.04.074 [DOI] [PubMed] [Google Scholar]
- Kaur M, & Bhat A (2019). Creative yoga intervention improves motor and imitation skills of children with Autism Spectrum Disorder. Physical Therapy, 99(11), 1520–1534. 10.1093/ptj/pzz115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaur M, Srinivasan SM, & Bhat AN (2018). Comparing motor performance, praxis, coordination, and interpersonal synchrony between children with and without Autism Spectrum Disorder (ASD). Research in Developmental Disabilities, 72, 79–95. 10.1016/j.ridd.2017.10.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaur M, Gifford T, Marsh K, & Bhat A (2013) The effects of robot-child interactions on bilateral coordination skills of typically developing children and one child with autism between 4 to 7 years of age. Journal of Motor Learning and Development, 1(2), 31–37. 10.1123/jmld.1.2.31 [DOI] [Google Scholar]
- Kenny M (2002). Integrated Movement Therapy™: Yoga-based therapy as a viable and effective intervention for autism spectrum and related disorders. International Journal of Yoga Therapy, 12(1), 71–79. 10.17761/ijyt.12.1.r978vxt214683904 [DOI] [Google Scholar]
- Koenig KP, Buckley-Reen A, & Garg S (2012). Efficacy of the Get Ready to Learn Yoga program among children with Autism Spectrum Disorders: A pretest-posttest control group design. American Journal of Occupational Therapy, 66(5), 538–546. 10.5014/ajot.2012.004390 [DOI] [PubMed] [Google Scholar]
- Lawson LM (2012). The effects of yoga on attention of preschool-aged children with attention problems. Annual in Therapeutic Recreation, 20, 36–45. https://www.atra-online.com/page/ATRAPublications [Google Scholar]
- Leekam SR, & Ramsden CAH (2006). Dyadic orienting and joint attention in preschool children with autism. Journal of Autism and Developmental Disorders, 36(2), 185–197. 10.1007/s10803-005-0054-1 [DOI] [PubMed] [Google Scholar]
- Lobo MA, Harbourne RT, Dusing SC, & McCoy SW (2013). Grounding early intervention: Physical Therapy cannot just be about motor skills anymore. Physical Therapy, 93(1), 94–103. 10.2522/ptj.20120158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lord C, Rutter M, DiLavore PC, Risi S, Gotham K, & Bishop S (2012). Autism Diagnostic Observation Schedule, 2nd Edition (ADOS-2). Torrence, CA: Western Psychological Services. [Google Scholar]
- MacDonald R, Anderson J, Dube WV, Geckeler A, Green G, Holcomb W, Mansfield R, & Sanchez J (2006). Behavioral assessment of joint attention: A methodological report. Research in Developmental Disabilities, 27(2), 138–150. 10.1016/j.ridd.2004.09.006 [DOI] [PubMed] [Google Scholar]
- Maenner MJ, Shaw KA, & Baio J (2020). Prevalence of autism spectrum disorder among children aged 8 years—autism and developmental disabilities monitoring network, 11 sites, United States, 2016. MMWR Surveillance Summaries, 69(4), 1. 10.15585/mmwr.ss6904a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mundy P, Block J, Delgado C, Pomares Y, Van Hecke AV, & Parlade MV (2007). Individual differences and the development of joint attention in infancy. Child Development, 78(3), 938–954. 10.1111/j.1467-8624.2007.01042.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peck HL, Kehle TJ, Bray MA, & Theodore LA (2005). Yoga as an intervention for children with attention problems. School Psychology Review, 34(3), 415–424. 10.1080/02796015.2005.12086295 [DOI] [Google Scholar]
- Radhakrishna S (2010). Application of integrated yoga therapy to increase imitation skills in children with autism spectrum disorder. International Journal of Yoga, 3(1), 26. 10.4103/0973-6131.66775 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reddy V, Williams E, & Vaughan A (2002). Sharing humour and laughter in autism and Down’s syndrome. British Journal of Psychology, 93(2), 219–242. 10.1348/000712602162553 [DOI] [PubMed] [Google Scholar]
- Roid GH (2003). Stanford-Binet Intelligence Scales, 5th Edition. Itasca, IL: Riverside Publishing. [Google Scholar]
- Rosenblatt LE, Gorantla S, Torres JA, Yarmush RS, Rao S, Park ER, Denninger JW, Benson H, Fricchione GL, Bernstein B, & Levine JB (2011). Relaxation response-based yoga improves functioning in young children with autism: A pilot study. The Journal of Alternative and Complementary Medicine, 17(11), 1029–1035. 10.1089/acm.2010.0834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rutter M, Bailey A, & Lord C (2003). The Social Communication Questionnaire. Los Angeles: Western Psychological Services. [Google Scholar]
- Serwacki M, & Cook-Cottone C (2012). Yoga in the schools: A systematic review of the literature. International Journal of Yoga Therapy, 22(1), 101–110. 10.17761/ijyt.22.1.7716244t75u4l702 [DOI] [PubMed] [Google Scholar]
- Sobolewski A, Holt E, Kublik E, & Wróbel A (2011). Impact of meditation on emotional processing - A visual ERP study. Neuroscience Research, 71(1), 44–48. 10.1016/j.neures.2011.06.002 [DOI] [PubMed] [Google Scholar]
- Sparrow SS, Cicchetti DV, & Balla DA (2005). Vineland Adaptive Behavior Scales, Second Edition. Toronto, Ontario, Canada: Pearson. [Google Scholar]
- Srinivasan SM, Eigsti I-M, Gifford T, & Bhat AN (2016a). The effects of embodied rhythm and robotic interventions on the spontaneous and responsive verbal communication skills of children with Autism Spectrum Disorder (ASD): A further outcome of a pilot randomized controlled trial. Research in Autism Spectrum Disorders, 27, 73–87. 10.1016/j.rasd.2016.04.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Srinivasan SM, Eigsti I-M, Neelly L, & Bhat AN (2016b). The effects of embodied rhythm and robotic interventions on the spontaneous and responsive social attention patterns of children with autism spectrum disorder (ASD): A pilot randomized controlled trial. Research in Autism Spectrum Disorders, 27, 54–72. 10.1016/j.rasd.2016.01.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Srinivasan SM, Park IK, Neelly LB, & Bhat AN (2015). A comparison of the effects of rhythm and robotic interventions on repetitive behaviors and affective states of children with Autism Spectrum Disorder (ASD). Research in Autism Spectrum Disorders, 18, 51–63. 10.1016/j.rasd.2015.07.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Srinivasan S, Gifford T, Marsh K, & Bhat A (2013a) The effects of robot-child interactions on the attention and verbalization patterns of typically developing children and children with autism between 4 to 8 years of age. Autism Open Access, 3 (2), 1–7. 10.4172/2165-7890.1000111 [DOI] [Google Scholar]
- Srinivasan S, Lynch K, Gifford T Bubela D, & Bhat A (2013b) The effects of robot-child interactions on imitation and praxis skills of children with and without autism between 4 to 7 years of age. Perceptual and Motor Skills, 116 (3), 889–906. 10.2466/15.10.PMS.116.3.885-904 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stagg SD, Slavny R, Hand C, Cardoso A, & Smith P (2013). Does facial expressivity count? How typically developing children respond initially to children with autism. Autism, 18(6), 704–711. 10.1177/1362361313492392 [DOI] [PubMed] [Google Scholar]
- Stone WL, & Caro-Martinez LM (1990). Naturalistic observations of spontaneous communication in autistic children. Journal of Autism and Developmental Disorders, 20(4), 437–453. 10.1007/bf02216051 [DOI] [PubMed] [Google Scholar]
- Tager-Flusberg H, & Caronna E (2007). Language disorders: Autism and other pervasive developmental disorders. Pediatric Clinics of North America, 54(3), 469–481. 10.1016/j.pcl.2007.02.011 [DOI] [PubMed] [Google Scholar]
- Tager-Flusberg H, Paul R, & Lord C (2005). Language and communication in autism. Handbook of Autism and Pervasive Developmental Disorders, 1, 335–364. [Google Scholar]
- Vismara LA, & Rogers SJ (2010). Behavioral treatments in autism spectrum disorder: what do we know? Annual Review of Clinical Psychology, 6, 447–468. [DOI] [PubMed] [Google Scholar]
- Wahbeh H, Elsas S-M, & Oken BS (2008). Mind-body interventions: Applications in neurology. Neurology, 70(24), 2321–2328. 10.1212/01.wnl.0000314667.16386.5e [DOI] [PMC free article] [PubMed] [Google Scholar]
- White PJ, O’Reilly M, Streusand W, Levine A, Sigafoos J, Lancioni G, Fragale C, Pierce N, & Aguilar J (2011). Best practices for teaching joint attention: A systematic review of the intervention literature. Research in Autism Spectrum Disorders, 5(4), 1283–1295. 10.1016/j.rasd.2011.02.003 [DOI] [Google Scholar]