Abstract
Patient: Female, 71-year-old
Final Diagnosis: Giant cell carcinoma
Symptoms: Vaginal bleeding
Medication:—
Clinical Procedure: Bilateral salpingo-oophorectomy • hysterectomy • lymph node excision
Specialty: Obstetrics and Gynecology • Pathology
Objective:
Rare disease
Background:
Giant cell carcinoma of the endometrium is one of the rare variants of endometrial carcinoma, with a very limited number of reported cases and limited follow-up data. The purpose of this case report is to present yet another example of endometrial giant cell carcinoma, discuss its differential diagnosis and management course, and review all previously reported cases.
Case Report:
We report a case of a 71-year-old woman who presented with vaginal bleeding. Her laboratory investigations were within normal limits except for her glycated hemoglobin, which was 10%. Ultrasound and computed tomography scans showed an endometrial mass invading the myometrium. Microscopically, the tumor is comprised almost exclusively of multinucleated giant cells. The patient underwent a total robotic hysterectomy with bilateral salpingo-oophorectomy and lymph nodes dissection, and she is currently undergoing adjuvant radiotherapy.
Conclusions:
Giant cell carcinoma of the endometrium is a rare diagnosis that can be established by histopathological examination after excluding the other common giant cell-rich lesions that may occur in the endometrium.
Keywords: Adenocarcinoma; Carcinoma, Giant Cell; Endometrium
Background
Endometrial carcinoma is the sixth most frequently diagnosed cancer in women and the second most common carcinoma of the female genital tract, with an estimated 66 570 new cases and 12 940 deaths in 2021 [1,2]. The current World Health Organization (WHO) classification of tumors of the uterine corpus includes the common types of endometrial carcinoma; however, a few other rare variants have been reported in the literature, like hepatoid carcinoma, glassy cell carcinoma, lymphoepithelioma-like carcinoma, adenocarcinoma with trophoblastic differentiation, and giant cell carcinoma (GCC) [2,3]. Giant cell carcinoma of the endometrium was first described in 1991 by Jones et al, with only 15 cases reported in the literature [4–9]. Herein, we present a case of GCC of the endometrium in a 71-year-old woman. We also review the previously reported cases and discuss the various features of this infrequently reported variant, emphasizing its differential diagnosis and the importance of recognizing this entity to avoid misdiagnosis or improper management.
Case Report
A 71-year-old postmenopausal woman presented with vaginal bleeding. She had a history of diabetes, hypertension, hypothyroidism, and aortic valve stenosis. Her surgical history included a sleeve gastrectomy and a discectomy. Pelvic examination was unremarkable, with no palpable lymph nodes. Her cervical smear was negative; however, an endometrial biopsy showed a high-grade carcinoma with bizarre and multinucleated giant cells. The patient was admitted for further investigations, and her laboratory tests were within normal limits, including tumor markers (CA-125, CA15-3, CA19.9, AFP, and CEA). Her glycated hemoglobin level (HbA1c) was 10%. Transvaginal ultrasound showed a thickened endometrium (17 mm) with some cystic areas and average-sized uterus and adnexa. A computed tomography scan of the chest, abdomen, and pelvis showed an endometrial mass involving more than 50% of the myometrial thickness, without evidence of extension beyond the serosa. There was no evidence of invasion into the adjacent structures, hydronephrosis, or distant metastasis.
The patient underwent a total robotic hysterectomy with bilateral salpingo-oophorectomy and pelvic lymph nodes sampling. The para-aortic lymph nodes were not dissected. Macroscopically, a tan friable mass measuring 2.5×2.0×2.0 cm was seen within the endometrial cavity and invading into the inner half of the myometrium. The cervix, ovaries, and fallopian tubes were grossly unremarkable. Microscopically, the tumor comprised sheets of multinucleated giant cells with abundant dense eosinophilic cytoplasm, marked nuclear pleomorphism, prominent nucleoli, and numerous atypical mitoses (Figure 1). The giant cells comprised around 95% of the tumor volume, with no evidence of other conventional types of endometrial carcinoma. The remainder of the neoplasm showed undifferentiated carcinoma (Figure 2). The tumor infiltrated into the inner half of the myometrium, with no evidence of lymphovascular invasion or cervical involvement. The adnexa were unremarkable, and a total of 4 lymph nodes were negative for meta-static carcinoma.
Figure 1.
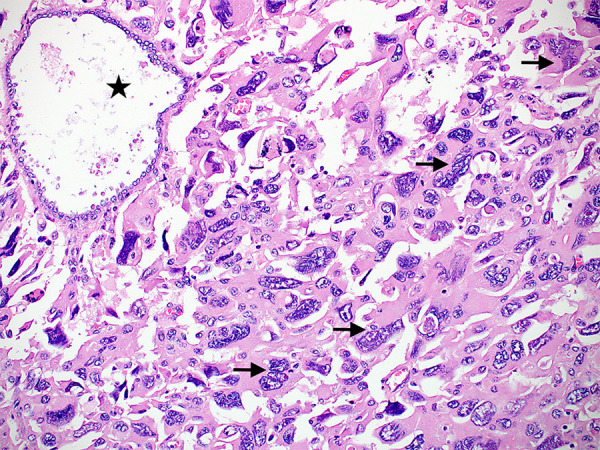
A photomicrograph showing sheets of multinucleated tumor cells (arrows) with abundant dense eosinophilic cytoplasm and marked nuclear pleomorphism, with an entrapped non-neoplastic gland (star). (Hematoxylin and eosin stain, ×200 magnifications) (CellSens Entry 1.18, Olympus).
Figure 2.
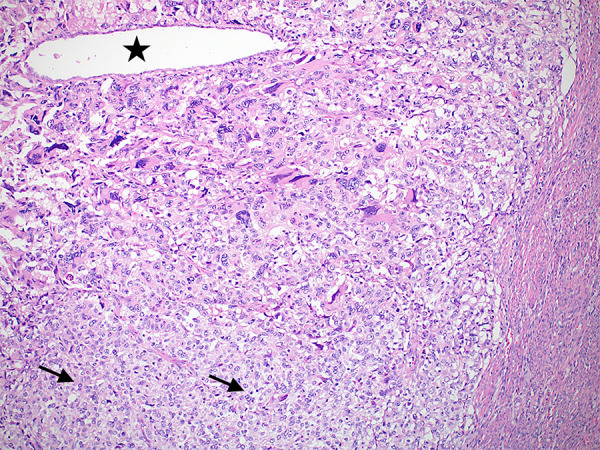
A low-magnification image showing the giant cell carcinoma component and the minor component of undifferentiated carcinoma (arrows). A single entrapped endometrial gland is also noted (star) (Hematoxylin and eosin stain, ×100 magnifications) (CellSens Entry 1.18, Olympus).
A panel of immunohistochemical stains was done and showed tumor cells positivity for vimentin, CAM 5.2 (Figure 3), p16 (Figure 4), and cytokeratin 7 (CK 7). p53 showed a wild-type pattern of staining. Tumor cells were negative for estrogen receptor (ER), desmin, myogenin, β-human chorionic gonadotropin (β-hCG), and CD68. In addition, they showed intact nuclear staining for mismatch repair proteins (MLH1, MSH2, MSH6, and PMS2). The diagnosis rendered was a giant cell carcinoma of the endometrium, International Federation of Gynecology and Obstetrics (FIGO) stage IA. Upon the consensus of a multidisciplinary tumor board, the patient is currently undergoing adjuvant radiotherapy. A written informed consent for patient information and images to be published was obtained from the patient.
Figure 3.
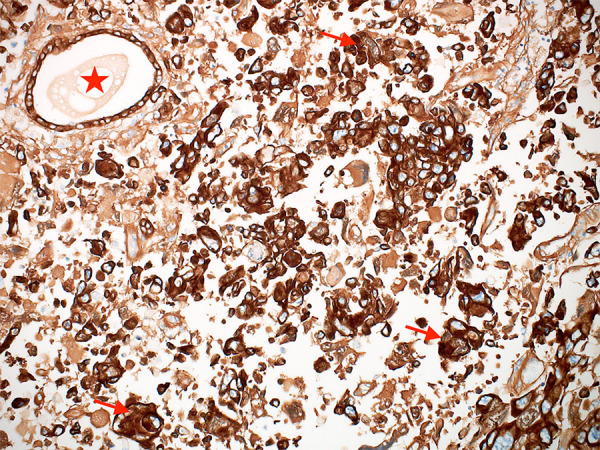
CAM5.2 immunohistochemical stain showing positive staining in both the tumor cells (arrows) and the entrapped non-neoplastic gland (star). (CAM5.2, ×200 magnification) (CellSens Entry 1.18, Olympus).
Figure 4.
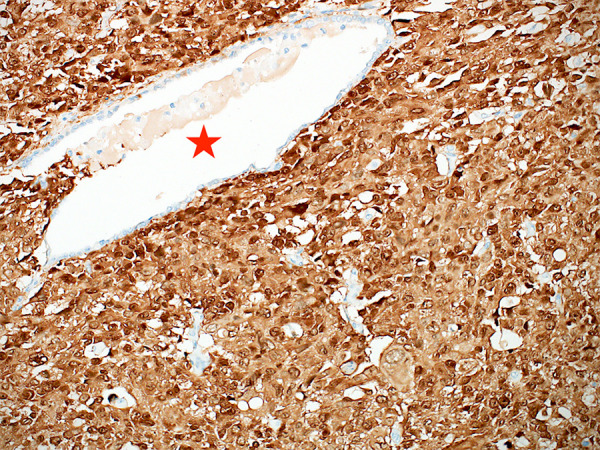
p16 immunohistochemical stain showing nuclear and cytoplasmic staining in tumor cells. An entrapped nonneoplastic gland is shown for comparison (star) (p16, ×200 magnification) (CellSens Entry 1.18, Olympus).
Discussion
Giant cell carcinoma of the endometrium is a rare variant of endometrial carcinoma first reported in 1991 by Jones et al [4]. The defining microscopic feature is the presence of bizarre multinucleated and tumor giant cells accounting for a substantial part of the tumor. The remainder of the tumor usually shows mononuclear undifferentiated carcinoma or a more conventional type of endometrial carcinoma [4]. This entity has not been recognized yet by the WHO as a separate variant of endometrial carcinoma; thus, the exact percentage of giant cells within an endometrial carcinoma qualifying for this diagnosis remains subjective. Nonetheless, the WHO states that any percentage of high-grade carcinoma is sufficient to label the tumor a mixed endometrial carcinoma [2]. Two cases in the original series by Jones et al had a minor giant cell component (15%), one of which presented with advanced disease (FIGO IIIC2) [4]. Similarly, one case in the series reported by Mulligan et al had a 30% giant cell component, and the patient also presented with extrauterine disease [6]. Hence, given the aggressive behavior of endometrial carcinomas containing giant cells, cases with a minor giant cell component are better classified as mixed endometrial carcinomas in agreement with the WHO classification [2,4,6].
Giant cell carcinoma should be differentiated from other endometrial tumors, which may have a prominent giant cell component, including trophoblastic tumors, carcinosarcoma, or primary sarcomas. In uterine choriocarcinoma or endometrial carcinoma with choriocarcinomatous differentiation, patients present with elevated serum β-hCG levels. The multinucleated cells in these tumors are either of a trophoblastic origin or demonstrating trophoblastic immunomorphological features depicted by the positivity of tumor cells to β-hCG [10]. Uterine carcinosarcoma is a biphasic tumor composed of sharply juxtaposed carcinomatous and sarcomatous components [2]. Leiomyosarcoma is a malignant smooth muscle tumor composed of intersecting fascicles of spindle cells with eosinophilic cytoplasm, which may also contain multinucleated giant cells; however, these cells are positive for smooth muscle markers, including desmin, smooth muscle actin (SMA), and h-caldesmon and they are negative for cytokeratin and β-hCG.
Giant cell carcinoma of the endometrium has been reported in 16 cases (including ours) to date (Table 1) [4–9]. The mean age of the patients was 66 years (range=43 to 83 years), and most of them presented with vaginal bleeding. The giant cell component was admixed with another type of endometrial carcinoma in most cases, including endometrioid adenocarcinoma, serous carcinoma, and clear cell carcinoma (Table 1). In our case and one of the cases reported by Mulligan et al, the tumor was almost exclusively composed of tumor giant cells [6]. Tumor cells were highlighted with cytokeratins (pan-CK, CK AE1/AE3, and CAM5.2) in all cases, and in some, they were also positive for vimentin and ER. When they were performed, β-hCG, CD68, p63, desmin, SMA, and MyoD1 were negative in tumor cells. Most of the reported cases were FIGO stage I, 1 case was stage II, 3 cases were stage III, and 2 cases were stage IV with limited follow-up data (Table 1). The management varied among patients; for example, in the cases reported by Bhattacharyya et al [7] and Sharma et al [8], patients underwent a total hysterectomy and bilateral salpingo-oophorectomy, and their follow-ups were uneventful. In the case reported by Ayık Aydın et al [9], the patient underwent a total abdominal hysterectomy, bilateral salpingo-oophorectomy, and bilateral pelvic and para-aortic lymphadenectomy. Although hormonal therapy is a well-documented treatment modality for primary, metastatic, and recurrent cases of endometrial carcinoma, its role in endometrial GCC remains unknown [9].
Table 1.
Reported cases of giant cell carcinoma of the endometrium.
| Case | Author, year | Age (years) | Presentation | % of giant cell component | Percentage of conventional cell type | FIGO stage | Reference |
|---|---|---|---|---|---|---|---|
| 1 | Jones et al, 1991 | 43 | Vaginal bleeding | 15% | Endometrioid (85%) | IA | [4] |
| 2 | Jones et al, 1991 | 66 | Vaginal bleeding | Predominant | Endometrioid | IA | [4] |
| 3 | Jones et al, 1991 | 64 | Vaginal bleeding | Predominant | Endometrioid | IA | [4] |
| 4 | Jones et al, 1991 | 85 | Vaginal bleeding | Predominant | Endometrioid | IIA | [4] |
| 5 | Jones et al, 1991 | 63 | Vaginal bleeding | 15% | Endometrioid (85%) | IVB | [4] |
| 6 | Jones et al, 1991 | 71 | Vaginal bleeding | Predominant | Endometrioid | IVB | [4] |
| 7 | Mardi et al, 2008 | 70 | Vaginal bleeding | Predominant | Endometrioid | IIIA | [5] |
| 8 | Mulligan et al, 2010 | 53 | Vaginal bleeding | 70% | Clear cell | IA | [6] |
| 9 | Mulligan et al, 2010 | 60 | Anemia | 100% | Not present | IB | [6] |
| 10 | Mulligan et al, 2010 | 58 | Vaginal bleeding | 50% | Endometrioid with spindle cells | IA | [6] |
| 11 | Mulligan et al, 2010 | 83 | Pelvic mass | 30% | Endometrioid | IIIC2 | [6] |
| 12 | Mulligan et al, 2010 | 67 | Vaginal bleeding | 90% | Serous | IA | [6] |
| 13 | Bhattacharyya et al, 2012 | 70 | Vaginal bleeding | 80% | Endometrioid | IB | [7] |
| 14 | Sharma et al, 2016 | 60 | Vaginal bleeding | 60% | Endometrioid | IB | [8] |
| 15 | Ayık Aydın et al, 2019 | 75 | Vaginal bleeding | Not available | Not available | IIIC | [9] |
| 16 | Current case | 71 | Vaginal bleeding | >95% | Not present | IA | Current case |
Information regarding tumor behavior and long-term prognosis is limited. In the original series, 4 patients had tumors with deep myometrial invasion, and they all developed recurrence, and 3 died of disease within 3 years [4]. In another series, 2 patients with a tumor confined to the uterus and extensive lymphovascular invasion developed lung metastasis 4 years after the initial diagnosis [6]. On the other hand, 2 patients, 1 in each of the series mentioned above, had stage 1 disease and remained disease-free at 6 and 14 years of follow-up, respectively [4,6]. Consequently, the prognosis of GCC is still undetermined even though it showed aggressive behavior in some instances.
The clinical differences between endometrial GCC and the other more common types of endometrial carcinoma, the appropriate therapeutic approach for endometrial GCC, and its prognosis are still controversial. Therefore, more cases should be collected and studied to highlight the significance of this variant further.
Conclusions
Giant cell carcinoma of the endometrium is a rare diagnosis with a small number of reported cases and limited data on its long-term prognosis. Nevertheless, pathologists should be aware and recognize this variant after excluding other common giant cell-rich lesions to avoid misdiagnosis and improper management.
Footnotes
Conflicti of Interests
None declared.
Declaration of Figures Authenticity
All figures submitted have been created by the authors, who confirm that the images are original with no duplication and have not been previously published in whole or in part.
References:
- 1.National Cancer Institute . SEER Cancer Stat Facts: Uterine Cancer. Bethesda: National Cancer Institute; 2020. SEER Cancer Stat Facts: Uterine Cancer. National Cancer Institute. Bethesda, MD. Available at: https://seer.cancer.gov/statfacts/html/corp.html. [Google Scholar]
- 2.WHO Classification of Tumours Editorial Board . Volume 4: Female Genital Tumours, in: WHO Classification of Tumours. 5th Edition. Geneva: IARC (International Agency for Research on Cancer); 2020. [Google Scholar]
- 3.Rutgers JK. Update on pathology, staging, and molecular pathology of endometrial (uterine corpus) adenocarcinoma. Future Oncol. 2015;11(23):3207–18. doi: 10.2217/fon.15.262. [DOI] [PubMed] [Google Scholar]
- 4.Jones MA, Young RH, Scully RE. Endometrial adenocarcinoma with a component of giant cell carcinoma. Int J Gynecol Pathol. 1991;10(3):260–70. doi: 10.1097/00004347-199107000-00005. [DOI] [PubMed] [Google Scholar]
- 5.Mardi K, Sharma M. Giant cell carcinoma of the endometrium. Internet J Gynecol Obstet [online] 2008;12(1):4545. Available from: https://ispub.com/IJGO/12/1/4545. [Google Scholar]
- 6.Mulligan AM, Plotkin A, Rouzbahman M, et al. Endometrial giant cell carcinoma: A case series and review of the spectrum of endometrial neoplasms containing giant cells. Am J Surg Pathol. 2010;34(8):1132–38. doi: 10.1097/PAS.0b013e3181e6579c. [DOI] [PubMed] [Google Scholar]
- 7.Bhattacharyya A, Gon S, Bandyopadhyay G, et al. Giant cell carcinoma of endometrium: A rare clinical entity. Iran J Pathol. 2012;7(3):197–202. [Google Scholar]
- 8.Sharma P, Ahluwalia C, Kolte S, Mandal AK. Giant cell carcinoma of endometrium: A rare case report and review of literature. Clin Cancer Investig J. 2016;5(1):79–82. [Google Scholar]
- 9.Ayık Aydın H, Tuncer HA, Erdoğan G, Şimşek T. Uterine giant cell carcinoma: A case report and review of the literature. Turk J Obstet Gynecol. 2019;16(1):76–79. doi: 10.4274/tjod.galenos.2018.31855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yamada T, Mori H, Kanemura M, et al. Endometrial carcinoma with choriocarcinomatous differentiation: A case report and review of the literature. Gynecol Oncol. 2009;113(2):291–94. doi: 10.1016/j.ygyno.2009.01.005. [DOI] [PubMed] [Google Scholar]


