Abstract
Lasting immunity will be critical for overcoming COVID-19. However, the factors associated with the development of high titers of anti-SARS-CoV-2 antibodies and how long those antibodies persist remain incompletely defined. In particular, an understanding of the relationship between COVID-19 symptoms and anti-SARS-CoV-2 antibodies is limited. To address these unknowns, we quantified serum anti-SARS-CoV-2 antibodies in clinically diverse COVID-19 convalescent human subjects five weeks (n=113) and three months (n=79) after symptom resolution with three methods: a novel multiplex assay to quantify IgG against four SARS-CoV-2 antigens, a new SARS-CoV-2 receptor binding domain-angiotensin converting enzyme 2 inhibition assay, and a SARS-CoV-2 neutralizing assay. We then identified clinical and demographic factors, including never before assessed COVID-19 symptoms, that consistently correlate with high anti-SARS-CoV-2 antibody levels. We detected anti-SARS-CoV-2 antibodies in 98% of COVID-19 convalescent subjects five weeks after symptom resolution and antibody levels did not decline at three months. Greater disease severity, older age, male sex, higher body mass index, and higher Charlson Comorbidity Index score correlated with increased anti-SARS-CoV-2 antibody levels. Moreover, we report for the first time that COVID-19 symptoms, most consistently fever, body aches, and low appetite, correlate with higher anti-SARS-CoV-2 antibody levels. Our results provide robust and new insights into the development and persistence of anti-SARS-CoV-2 antibodies.
INTRODUCTION
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), isolated January 2020 (1), causes coronavirus disease 2019 (COVID-19), which ranges from no symptoms to a flu-like illness to death (2). As of May 2020, there have been over 157 million cases worldwide and over 3.2 million deaths (3), with devastating effects on health, economies, and societies (4).
Lasting immunity, often estimated by persistent antibodies, will be critical for overcoming the COVID-19 pandemic, but our understanding of the development of persistent anti-SARS-CoV-2 antibodies is still emerging. In severe acute respiratory syndrome (SARS), caused by related SARS-CoV, antibodies typically persist at least three years (5–7). SARS-CoV-2 has not existed for three years yet, but some reports suggest that immunity may last at least three to six months (8–11). However, other reports suggest that anti-SARS-CoV-2 neutralizing and IgG antibodies can decline within a few months, with some patients becoming seronegative (12–21). These discrepant findings may be due to small sample sizes, use of variable or loosely defined time points, differing disease severity (a known correlate of antibody levels and persistence (16, 21–23)), and the use of different antibody detection methods, with neutralizing titers more likely to be low (24, 25). Also, many studies do not evaluate clinical correlates of antibody titers and none have systematically evaluated COVID-19 symptoms. A standardized approach to evaluating anti-SARS-CoV-2 antibodies with uniform time points defined by the resolution of disease, multiple antibody tests, and incorporation of clinical and demographic factors including COVID-19 symptoms would shed light on the development of antibody-based immunity in COVID-19.
Thus, we broadly evaluated the antibody response against SARS-CoV-2 in a clinically diverse COVID-19 convalescent population at five weeks and three months after symptom resolution using three different assays and then correlated antibody levels with clinical and demographic factors including COVID-19 symptoms. We found that greater disease severity, older age, male sex, higher body mass index, and higher Charlson Comorbidity Index score correlate with higher anti-SARS-CoV-2 antibody levels. We also identified fever, body aches, and low appetite as symptoms that consistently correlate with higher anti-SARS-CoV-2 antibody levels and demonstrate antibody persistence three months after symptom resolution.
MATERIALS AND METHODS
Human Subjects
Human studies were performed according to the Declaration of Helsinki and were approved by the University of Wisconsin (UW) Institutional Review Board. All subjects provided written informed consent. COVID-19 convalescent sera and data were obtained from the UW COVID-19 Convalescent Biorepository and control sera collected prior to 2019 were obtained from the UW Rheumatology Biorepository (26) and the NIH clinical protocol VRC200. For the COVID-19 Convalescent Biorepository, all individuals 18+ years old who tested positive for SARS-CoV-2 by PCR at UW Health were invited to participate until 120 subjects were recruited. Clinical and demographic data were collected by survey upon recruitment. Additional data and blood were collected 5 weeks and 3 months +/− 10 days post-symptom resolution. Age, sex, address (for area of deprivation index, ADI (27)), medications, lab values, height and weight (for body mass index, BMI), medical problems, and the date of the most recent primary care appointment were abstracted from the UW Health electronic medical record (EMR). Race, ethnicity, tobacco use, COVID-19 symptoms, and date of symptom resolution were self-reported by questionnaire. Hospitalization and intubation for COVID-19 were obtained by questionnaire and EMR abstraction. COVID-19 severity was scored as critical (4, intubated), severe (3, hospitalized but not intubated), moderate (2, fever defined as temperature >100°F, chills, productive cough, or shortness of breath, but not hospitalized), or mild (1, none of the above). Charlson Comorbidity Index Scores were calculated (28). Subjects were excluded from this study if they received convalescent plasma, if blood was collected >14 days from the intended time point, or if they did not provide consent for all aspects of the study.
IgG binding to coronavirus antigens (multiplex assay)
Plates (96 well) printed with SARS-CoV-2 spike protein, receptor binding domain (RBD) of spike, N terminal domain (NTD) of spike, and nucleocapsid protein, as well as spike from SARS-CoV, HCoV-HKU1, HCoV-OC43, HCoV-NL63, and HCoV-229E, in addition to bovine serum albumin (BSA) were supplied by Meso Scale Discovery (MSD, Rockville, USA). Plates were blocked for 60 minutes with MSD Blocker A (5% BSA) followed by washing. Then, sera were applied to the wells at 4 dilutions (1:100, 1:800, 1:3200 and 1:12,800) and incubated with shaking for 2 hours. Plates were washed and SULFO-TAG labeled anti-IgG (MSD) was applied to the wells for 1 hour. Plates were washed, enhanced chemiluminescence (ECL) substrate (MSD) applied, and light emission (as a measure of bound IgG) read with the MSD Sector instrument. BSA readings were subtracted from CoV antigen readings. Area under the curve values for each sample were used for statistical analysis with zero values (3 samples for anti-NTD) depicted as ten in graphs for optimal visualization using the log scale.
Inhibition assay
Plates (384 well) precoated with RBD were supplied by MSD. Plates were blocked for 30 minutes with MSD Blocker A, washed, sera applied at 1:10 dilution, and incubated with shaking for 1 hour. SULFO-TAG labeled angiotensin converting enzyme (ACE)2 was applied to the wells, incubated for 1 hour, and washed. ECL substrate was applied, and light emission (a measure of RBD-ACE2 complex) was read by the MSD Sector instrument. The amount of light emitted in wells containing no sample (assay diluent only) was considered the maximal binding response. Reduction of ECL response from the maximal binding response was directly proportional to the extent of competitive binding activity.
Neutralization assay
Vero E6/TMPRSS2 cells were grown in Dulbecco’s Modified Eagle Medium supplemented with 5% fetal calf serum, HEPES, amphotericin B, and gentamicin sulfate. Sera (100μl) were diluted in cell culture solution with 2-fold serial dilutions from 5x to 2560x. Virus (SARS-CoV-2/UW-001/Human/2020/Wisconsin) was diluted in cell culture solution to an adjusted titer of 100 plaque-forming units (PFU) per 60μl. Diluted sera (60μl) and diluted virus (60μl) were mixed in wells of 96-well U-bottom plates in duplicate. Plates were incubated at 37°C for 30 minutes. Culture supernatant was aspirated from Vero E6/TMPRSS2 cells plated in 96 well dishes and replaced with the mixtures of serially diluted sera and virus (100μl/well, in duplicate) followed by incubation at 37°C with 5% CO2 for 3 days. Crystal violet stain was added to wells to stain for living cells. Neutralization titers were determined by the maximum fold dilution at which the serum samples could completely prevent cell death as determined by eye. Some duplicates diverged by a single fold dilution in their neutralization titer. In this situation, the lower dilution was used as the neutralization titer. Sera with cell death at all dilutions were assigned a dilution value of 1 for analysis purposes.
Statistical analysis
Antibody levels were compared between COVID-19 convalescent and control sera using a t test or among subsets of COVID-19 convalescent sera by one-way ANOVA with Tukey’s, Dunnett’s, or Dunn’s multiple comparisons tests. Welch’s correction was used for unequal variance. Anti-SARS-CoV-2 antibody levels from different time points in the same subject were compared by paired t test. Correlations between antibody levels from different tests were estimated by Spearman rank correlation. The relationship between clinical and demographic factors and COVID-19 hospitalization or antibody levels were examined using the Pearson’s chi-squared test for categorical variables and Kruskal-Wallis test for non-normally distributed continuous data. Multiple linear regression analysis was performed to determine if the presence of specific symptoms were associated with transformed antibody levels (square root transformed for spike, RBD and nucleocapsid and log transformed for NTD, ACE2 inhibition and neutralizing titers) adjusted for age, BMI, Charlson Comorbidity Index score, and sex. We also modeled the combination of symptoms indicative of moderate disease (severity score 2) and the total number of symptoms to determine their associations with antibody titers. We examined adjusted R2 values to determine if modeling symptoms in these ways explained more of the variability in antibody titer as compared to symptom-specific regressions. Analyses were performed using GraphPad Prism software (San Diego, USA) and STATA version 16 (College Station, USA). For all analyses, p<0.05 was considered statistically significant.
RESULTS
We recruited 120 COVID-19 convalescent subjects into the UW COVID-19 Convalescent Biorepository. Seven subjects were excluded from this study due to erroneous blood collection timing (n=1), receipt of convalescent plasma (n=3), or partial consent (n=3). Two additional subjects were excluded from longitudinal evaluation due to a blood draw >14 days from the 3 month time point. Of the included subjects, blood was collected from 113 at 5 weeks (range 29–48 days, median 36 days, IQR 35–39 days) and from 79 at 3 months (range 85–102 days, median 91 days, IQR 90–93 days) post-symptom resolution. Eighty-one percent of COVID-19 convalescent subjects had a primary care appointment within two years of the first blood draw and/or a hospital admission note with past medical history and medications. Subjects ranged in age from 19–83 years and had a variety of COVID-19 manifestations (Supplementary Table 1 and Supplementary Figure 1). One subject was a current smoker. As expected (22, 29), hospitalized subjects were more likely to be older and male with more comorbidities like vascular disease, but less likely to have asthma (Supplementary Table 1). Additionally, hospitalized subjects were more likely to have fever and less likely to have chest tightness, sore throat, or headache than non-hospitalized patients. We detected no correlation between race, ethnicity, ADI, BMI, cancer, immunosuppressing medications, or other COVID-19 symptoms and hospitalization, potentially due to the relative uniformity of race and ethnicity and the low number of subjects with cancer or immunosuppressing medications in our cohort.
We used a multiplex approach to evaluate IgG levels against four SARS-CoV-2 antigens (spike, RBD of spike, NTD of spike, and nucleocapsid) as well as IgG against the spike protein of SARS-CoV and four seasonal coronaviruses HCoV-OC43, HCoV-HKU1, HCoV-NL63, and HCoV-229E) in subjects five weeks post-COVID-19 symptom resolution (Figure 1A). COVID-19 convalescent subjects had higher IgG levels against all four SARS-CoV-2 antigens compared to naive subjects. Further, 98% of convalescent subjects had higher binding than any naive subject in at least one test. Finally, IgG levels against spike from SARS-CoV, HCoV-OC43, and HCoV-HKU1, but not HCoV-NL63 and HCoV-229E, were higher in convalescent subjects compared to controls.
Figure 1. Antibodies against SARS-CoV-2 in COVID-19 convalescent subjects five weeks post-symptom resolution.
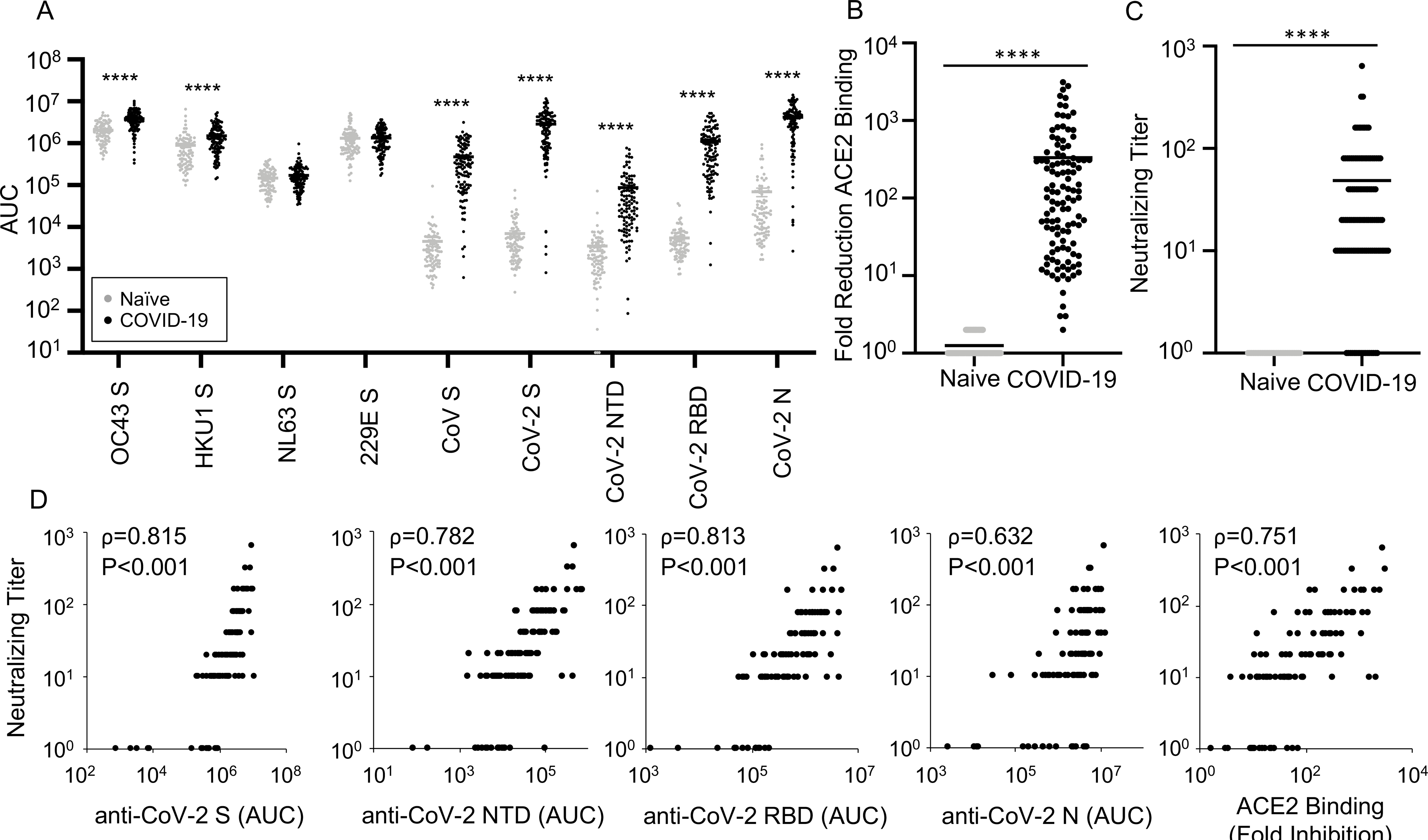
IgG against the spike (S) protein from HCoV-OC43, HCoV-HKU1, HCoV-NL63, HCoV-229E, and SARS-CoV, as well as SARS-CoV-2 S, N terminal domain (NTD) of S, receptor binding domain (RBD) of S, and nucleocapsid (N) protein for convalescent (black, n=113) and naive (gray, n=87) sera (A), fold reduction of angiotensin converting enzyme (ACE)2 binding to RBD for convalescent (n=113) and naive (n=88) sera (B), and neutralizing titers for convalescent (n=113) and naive (n=30) sera (C) were compared by t test with Welch’s correction. Bars represent mean, ****p<0.0001, and AUC: area under the curve. D. Neutralizing titers were compared with anti-SARS-CoV-2 IgG levels and RBD-ACE2 binding inhibition for convalescent subjects (n=113) with Spearman correlation coefficients (ρ) and p values listed.
We then evaluated the antibody response against SARS-CoV-2 in a more functional manner. Since the RBD of spike binds to ACE2, enabling viral entry (30), we quantified the ability of sera to inhibit RBD binding to ACE2. Compared to naive sera, five week convalescent sera demonstrated much higher inhibition of RBD-ACE2 binding (Figure 1B). Further, in a neutralizing assay using live SARS-CoV-2, COVID-19 convalescent sera had higher titers compared to naive sera, although 15% of convalescent subjects did not have neutralizing titers above controls (Figure 1C). Overall, neutralizing titers correlated well with IgG levels against SARS-CoV-2 and RBD-ACE2 binding inhibition (Figure 1D).
Next, we evaluated if antibody titers at five weeks post-symptom resolution varied with disease severity in our cohort. Hospitalized subjects had higher antibody levels than non-hospitalized subjects according to all of our tests, and, in general, antibody titers increased with COVID-19 severity (Figure 2). To determine if clinical and demographic factors apart from severe disease correlate with antibody levels, we analyzed non-hospitalized subjects alone. Older age, male sex, higher BMI and a Charlson Comorbidity Index score >2 correlated with higher antibody titers in non-hospitalized subjects for all or most tests (Table 1). Race, ethnicity, ADI, cancer, diabetes, vascular disease, asthma, immunosuppressive medications and inhaled/intranasal steroids did not correlate with antibody levels in general (Supplementary Table 2).
Figure 2. Patients with more severe COVID-19 have higher antibody levels against SARS-CoV-2.
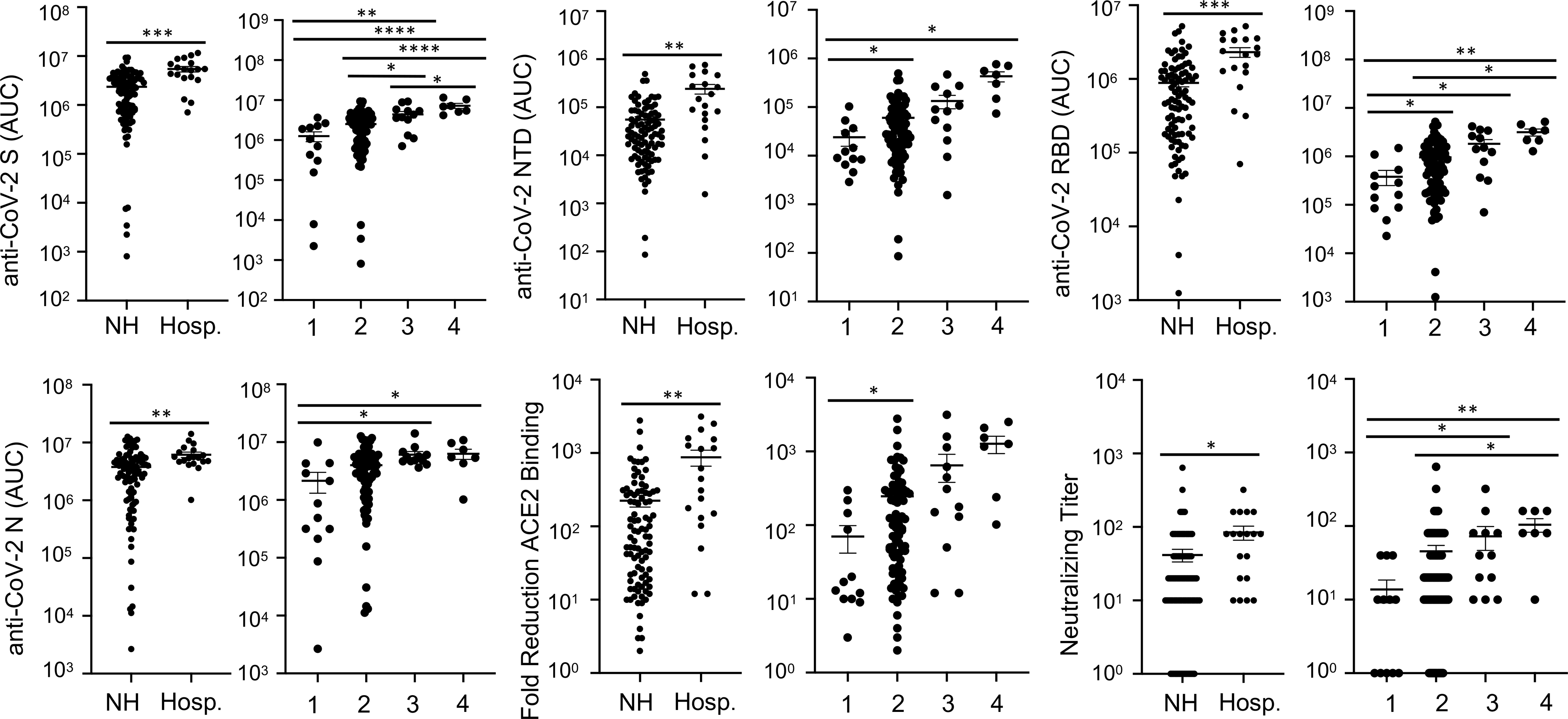
IgG levels against SARS-CoV-2 S, NTD, RBD, and N, as well as fold reduction of RBD-ACE2 binding, and neutralizing antibodies in COVID-19 convalescent sera five weeks post-symptom resolution were compared for non-hospitalized (NH, n=94) versus hospitalized (Hosp., n=19) subjects by t test and among subjects with mild (score 1, n=12), moderate (2, n=82), severe (3, n=12), and critical (4, n=7) COVID-19 severity by ANOVA (anti-NTD, anti-RBD, and RBD-ACE2 binding inhibition by Welch’s ANOVA with Dunnett’s test; anti-S and anti-N by ANOVA with Tukey’s multiple comparisons test, and neutralizing titers by Kruskal-Wallis ANOVA with Dunn’s multiple comparisons test). For all panels: lines indicate mean +/− SEM; *p<0.05, **p<0.01, ***p<0.001, ****p<0.0001.
Table 1.
Median (IQR) IgG levels, fold RBD-ACE2 inhibition, and SARS-CoV-2 neutralization titers five weeks after resolution of COVID-19 symptoms according to clinical and demographic characteristics in non-hospitalized subjects
| N | Anti-Spike a | Anti-NTD a | Anti-RBD a | Anti-N a | ACE-2 Inhib. | Neut. Titer | |
|---|---|---|---|---|---|---|---|
|
| |||||||
| All subjects | 94 | 19 (7.0, 35) | 0.27 (0.10, 0.69) | 5.1 (1.8, 12) | 31 (11, 51) | 73 (20, 287) | 20 (10, 40) |
| Age quartile | p=0.047 | p=0.009 | p=0.028 | p=0.005 | p=0.011 | p=0.230 | |
| 1 (19.2–27.6) | 24 | 10 (3.8, 22) | 0.14 (0.07, 0.42) | 2.2 (1.2, 7.3) | 9.6 (3.2, 35) | 32 (11, 94) | 10 (10, 20) |
| 2 (29.6–42.4) | 23 | 18 (8.4, 28) | 0.25 (0.15, 0.53) | 5.3 (1.8, 9.6) | 29.0 (23, 56) | 85 (50, 203) | 20 (10, 40) |
| 3 (42.5–54.5) 4 (54.8–76.5) |
23 24 |
31 (7.9, 37) 30 (8.8, 46) |
0.51 (0.08, 1.0) 0.37 (0.20, 1.7) |
10 (2.1, 15) 8.4 (3.5, 22) |
37 (19, 51) 44.1 (29, 63) |
119 (15, 311) 216 (36, 555) |
20 (1, 40) 20 (10, 80) |
| Sex | p=0.034 | p=0.039 | p=0.015 | p=0.031 | p=0.023 | p=0.009 | |
| Male | 32 | 29 (7.2, 43) | 0.46 (0.15, 0.89) | 9.6 (2.5, 16) | 44 (23, 66) | 121 (43, 344) | 40 (10, 80) |
| Female | 62 | 17 (7.0, 32) | 0.21 (0.08, 0.47) | 4.1 (1.6, 10) | 29 (8.7, 44) | 51 (15, 219) | 15 (10, 40) |
| BMI b (lb/in2) | p=0.041 | p=0.011 | p=0.020 | p=0.091 | p=0.067 | p=0.027 | |
| 1 (<25) | 22 | 11 (5.0, 20) | 0.16 (0.09, 0.27) | 3.1 (1.3, 6.4) | 22 (10, 40) | 38 (20, 121) | 10 (10, 20) |
| 2 (25–29.99) | 27 | 21 (7.9, 43) | 0.41 (0.12, 1.0) | 6.9 (2.2, 16) | 43 (16, 51) | 72 (17, 328) | 10 (10, 40) |
| 3 (≥30) | 30 | 27 (15, 38) | 0.41 (0.18, 0.86) | 9.1 (4.8, 13) | 43 (23, 85) | 139 (45, 298) | 40 (10, 80) |
| Charlson > 2 |
30 |
p=0.021 33 (8.8, 45) |
p=0.001 0.46 (0.25, 1.4) |
p=0.010 9.8 (4.1, 20) |
p=0.010 45 (30, 63) |
p=0.009 217 (34, 489) |
p=0.072 30 (10, 80) |
Values are x105
Data missing for 15 subjects
We then determined if symptoms might correlate with antibody levels. To this end, we first performed a univariate analysis to determine if any symptoms correlated with age, sex, BMI, or Charlson Comorbidity Index score, i.e. characteristics associated with antibody levels (Table 1). Since some symptoms correlated with hospitalization, again we evaluated only non-hospitalized patients. As shown in detail in Table 2 and in a summarized form in Figure 3, we found that most symptoms did not associate with these characteristics. However, abdominal pain was associated with older age and higher Charlson Comorbidity Index score, diarrhea with higher BMI and male sex, vomiting with higher BMI, fever with higher Charlson Comorbidity Index score, and body aches and productive cough with male sex.
Table 2.
Clinical and demographic features according to clinical symptoms in non-hospitalized subjects
| Symptom | N | Age in years | BMI a in lb/in2 | CCS b | Sex |
|---|---|---|---|---|---|
| Median (IQR) | Median (IQR) | Median (IQR) | % of M - % of F (% of M, % of F) | ||
|
| |||||
| All subjects | 94 | 42.4 (27.6, 54.8) | 27.7 (24.7, 32.4) | 1 (0, 2) | −31.9 (34.0, 66.0) |
| Fever | 59 | 44.3 (29.6, 55.4) | 28.4 (25.2, 32.4) | 1 (0, 2) * | 9.1 (68.8, 59.7) |
| Chills c | 59 | 42.5 (29.6, 54.5) | 29.3 (25.2, 34.1) | 1 (0, 2) | 15.7 (75.0, 59.3) |
| Productive cough | 37 | 43.6 (27.0, 52.9) | 31.3 (25.6, 34.1) | 1 (0, 2) | 25.6 (56.3, 30.7) * |
| Dry cough | 58 | 42.1 (31.4, 54.0) | 28.5 (24.8, 32.5) | 1 (0, 2) | 15.4 (71.9, 56.5) |
| Shortness of breath | 47 | 44.1 (36.3, 54.8) | 29.4 (25.0, 32.5) | 1 (0, 2) | 18.9 (62.5, 43.6) |
| Chest tightness | 60 | 41.2 (29.8, 54.7) | 28.2 (24.7, 32.3) | 1 (0, 2) | 12.2 (71.9, 59.7) |
| Sore throat | 45 | 43.3 (27.6, 54.8) | 29.0 (24.6, 32.9) | 1 (0, 2) | −1.5 (46.9, 48.4) |
| Loss of taste or smell | 58 | 40.4 (26.6, 52.9) | 27.3 (24.2, 32.3) | 0 (0, 2) | 1.2 (62.5, 61.3) |
| Runny or stuffed nose | 54 | 39.3 (26.6, 54.0) | 28.0 (25.0, 33.1) | 0 (0, 2) | −1.8 (56.3, 58.1) |
| Body aches | 69 | 42.4 (27.5, 54.5) | 28.0 (25.1, 32.5) | 1 (0, 2) | 21.4 (87.5, 66.1) * |
| Headaches | 68 | 40.4 (27.2, 54.3) | 27.7 (24.1, 32.4) | 0.5 (0, 2) | −0.7 (71.9, 72.6) |
| Low appetite | 59 | 43.4 (30.1, 54.8) | 28.3 (25.0, 32.5) | 1 (0, 2) | 9.1 (68.8, 59.7) |
| Nausea | 32 | 44.1 (32.5, 55.3) | 27.0 (24.8, 35.4) | 1 (0, 2.5) | 0.5 (34.4, 33.9) |
| Vomiting | 13 | 51.3 (32.3, 54.8) | 32.4 (30.0, 36.0) * | 2 (0, 3) | −2 (12.5, 14.5) |
| Abdominal pain | 17 | 54.8 (42.5, 62.5) ** | 31.2 (26.0, 32.4) | 2 (1, 3) *** | 15.2 (28.1, 12.9) |
| Diarrhea | 42 | 43.8 (36.3, 54.8) | 31.4 (25.4, 34.3) ** | 1 (0, 2) | 27 (62.5, 35.5) * |
BMI data missing for 15 subjects
CCS: Charlson Comorbidity Score
Chills data missing for two subjects
p<0.05
p<0.01
p<0.001
Figure 3. Correlation of COVID-19 symptoms with clinical features and anti-SARS-CoV-2 antibody levels five weeks after symptom resolution.
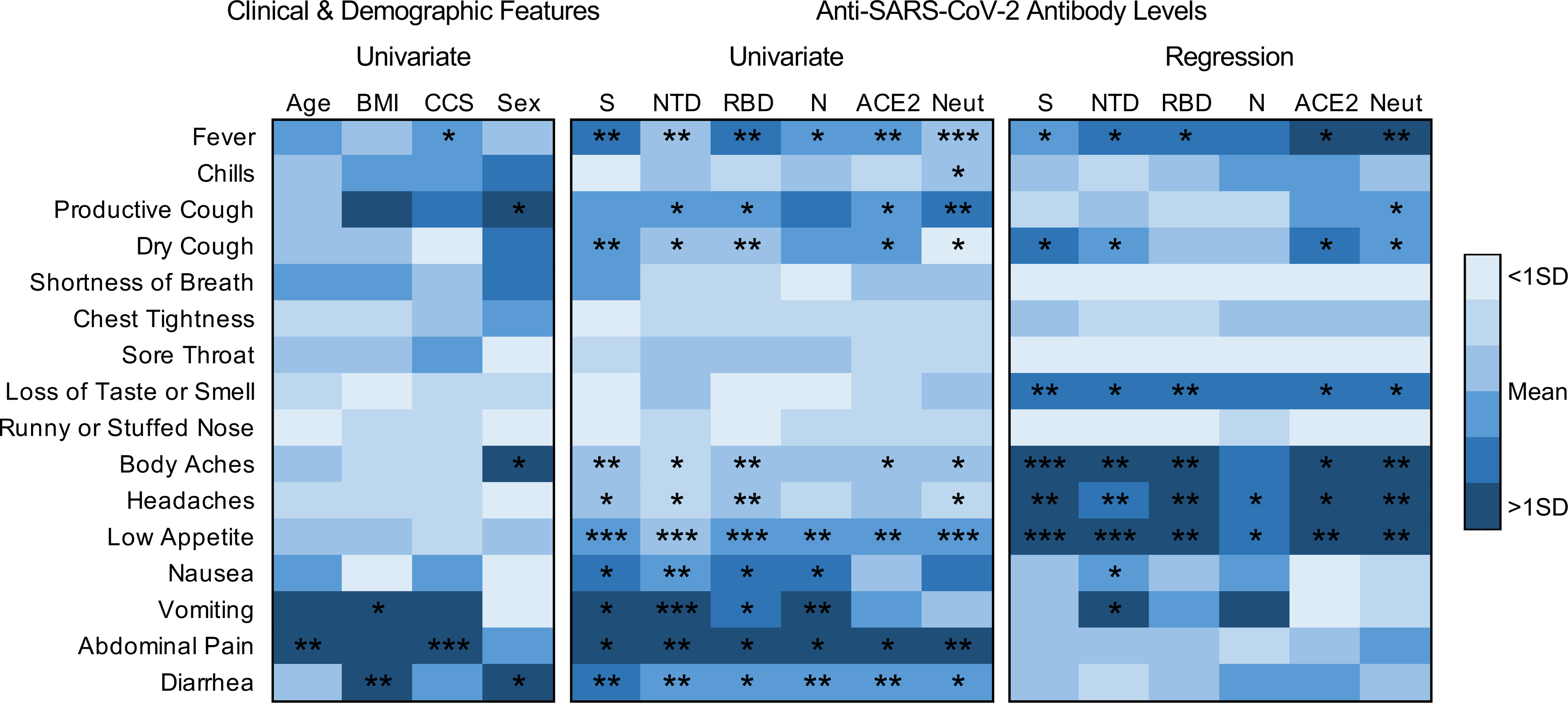
Univariate analysis was performed to identify associations between symptoms and age, BMI, Charlson Comorbidity Index Score (CCS), and sex (left panel) or IgG levels against S, NTD, RBD, or N, fold reduction in ACE2 binding to RBD, and neutralizing antibodies (Neut) (middle panel) by Kruskal-Wallis test or, for sex, by chi-squared test. Color indicates how the median age, BMI, S, NTD, RBD, N, ACE2 or mean neutralizing titer for subjects with the indicated symptom compares to the mean +/− one standard deviation (SD) of all symptoms for that clinical feature or antibody. For sex, the difference in the percent of males minus females with the reported symptom was used to determine color. Multiple linear regression analysis to determine if specific symptoms are associated with antibody levels adjusted for age, BMI, CCS, and sex is represented in the right panel with color corresponding to strength of association of the variables (beta coefficient). Full data for this figure can be found in Tables 2–4 with *p<0.05, **p<0.01 and ***p<0.001.
We then performed a univariate analysis to determine if antibody titers at five weeks post-symptom resolution varied with symptoms in our non-hospitalized subjects. As shown in Figure 3 and Table 3, fever, low appetite, abdominal pain, and diarrhea correlated with higher antibody levels measured by every test. Cough, body aches, headache, nausea, and vomiting correlated with some antibody tests. Chills, shortness of breath, chest tightness, sore throat, loss of taste or smell, and runny or stuffed nose correlated with no or almost no antibody tests.
Table 3.
Median (IQR) IgG levels, fold RBD-ACE2 inhibition, and SARS-CoV-2 neutralization titers five weeks after resolution of COVID-19 symptoms according to clinical symptoms in non-hospitalized subjects
| N | Anti-Spike a | Anti-NTD a | Anti-RBD a | Anti-N a | ACE-2 Inhib. | Neut. Titer | |
|---|---|---|---|---|---|---|---|
|
| |||||||
| All subjects | 94 | 19 (7.0, 35) | 0.27 (0.10, 0.69) | 5.1 (1.8, 12) | 31 (11, 51) | 73 (20, 287) | 20 (10, 40) |
| Fever | 59 | 29 (7.9, 39) ** | 0.41 (0.17, 0.86) ** | 9.2 (2.8, 14) ** | 40 (23, 54) * | 121 (37, 328) ** | 20 (10, 80) *** |
| Chills b | 59 | 21 (7.9, 39) | 0.32 (0.14, 0.82) | 5.9 (2.1, 14) | 38 (16, 53) | 73 (34, 305) | 20 (10, 80) * |
| Productive cough | 37 | 26 (10, 38) | 0.44 (0.18, 0.74) * | 8.7 (3.2, 13) * | 42 (23, 55) | 131 (42, 305) * | 20 (10, 80) ** |
| Dry cough | 58 | 26 (10, 38) ** | 0.32 (0.17, 0.73) * | 7.4 (2.8, 13) ** | 39 (21, 53) | 124 (37, 298) * | 20 (10, 40) * |
| Shortness of breath | 47 | 26 (6.7, 38) | 0.27 (0.12, 0.74) | 5.9 (1.8, 13) | 27 (11, 56) | 85 (22, 305) | 20 (10, 80) |
| Chest tightness | 60 | 21 (7.2, 35) | 0.26 (0.09, 0.71) | 5.8 (1.8, 13) | 36 (12, 56) | 79 (21, 287) | 20 (10, 40) |
| Sore throat | 45 | 22 (8.4, 35) | 0.34 (0.17, 0.68) | 6.9 (2.4, 12) | 38 (14, 53) | 73 (20, 298) | 20 (10, 40) |
| Loss of taste or smell | 58 | 21 (8.0, 36) | 0.33 (0.10, 0.73) | 5.0 (1.8, 13) | 31 (14, 54) | 73 (22, 298) | 20 (10, 40) |
| Runny or stuffed nose | 54 | 20 (6.7, 37) | 0.28 (0.09, 0.69) | 5.5 (1.7, 12) | 35 (16, 53) | 73 (20, 279) | 20 (10, 40) |
| Body aches | 69 | 24 (8.4, 39) ** | 0.29 (0.14, 0.86) * | 6.9 (2.2, 14) ** | 38 (16, 53) | 93 (28, 298) * | 20 (10, 80) * |
| Headaches | 68 | 24 (9.1, 35) * | 0.31 (0.16, 0.71) * | 6.8 (2.9, 13) ** | 36 (18, 53) | 92 (26, 293) | 20 (10, 40) * |
| Low appetite | 59 | 27 (9.8, 43) *** | 0.41 (0.18, 1.0) *** | 8.7 (2.9, 16) *** | 40 (22, 56) ** | 123 (28, 311) ** | 20 (10, 80) *** |
| Nausea | 32 | 29 (9.2, 46) * | 0.45 (0.26, 1.1) ** | 9.1 (3.5, 14) * | 42 (26, 56) * | 95 (19, 332) | 20 (10, 80) |
| Vomiting | 13 | 30 (20, 43) * | 0.93 (0.44, 1.1) *** | 10 (4.8, 20) * | 48 (42, 82) ** | 131 (26, 376) | 40 (10, 80) |
| Abdominal pain | 17 | 35 (17, 47) * | 1.0 (0.28, 1.6) ** | 14 (5.6, 20) * | 48 (29, 69) * | 310 (47, 756) * | 80 (20, 80) ** |
| Diarrhea | 42 | 28 (13, 43) ** | 0.44 (0.23, 0.93) ** | 8.9 (4.1, 14) * | 41 (23, 82) ** | 124 (47, 392) ** | 30 (10, 80) * |
Values are x105
Data missing for three subjects
p<0.05
p<0.01
p<0.001
Concerned that age, sex, BMI, or Charlson Comorbidity Index score, which correlate with anti-SARS-CoV-2 antibodies and some symptoms (Tables 1 and 2), could be confounding our univariate analysis, we performed a multiple linear regression analysis controlling for these variables (Figure 3 and Table 4). We found that fever and low appetite remained strong correlates and that chills, shortness of breath, chest tightness, sore throat, and runny/stuffed nose remained weak correlates of anti-SARS-CoV-2 antibody levels when accounting for these characteristics. However, gastrointestinal symptoms had little correlation with antibody levels in the multivariable analysis. Further, the strength of association between antibody levels and cough, particularly productive cough, was reduced whereas the correlation between body aches and headaches increased. Interestingly, when adjusting for age, BMI, comorbidities, and sex, loss of taste or smell was strongly associated with almost all antibody tests.
TABLE 4.
Multiple linear regression of symptoms associated with antibody levels, ACE-2 inhibition, and viral neutralization titers five weeks after resolution of COVID-19 symptoms in non-hospitalized subjects
| Symptom a | sqrt[IgG(Spike)] | log[IgG(NTD)] | sqrt[IgG(RBD)] | |||||||||
| β | 95% CI | p | Adj. R2 | β | 95% CI | p | Adj. R2 | β | 95% CI | p | Adj. R2 | |
|
| ||||||||||||
| Fever | 314 | 13, 614 | 0.041 | 0.14 | 0.73 | 0.16, 1.29 | 0.012 | 0.19 | 254 | 55, 452 | 0.013 | 0.21 |
| Chills | 207 | −124, 539 | 0.217 | 0.12 | 0.28 | −0.36, 0.91 | 0.385 | 0.13 | 143 | −80, 366 | 0.205 | 0.16 |
| Productive cough | 167 | −152, 487 | 0.300 | 0.10 | 0.49 | −0.11, 1.09 | 0.108 | 0.14 | 82 | −133, 297 | 0.448 | 0.14 |
| Dry cough | 363 | 60, 666 | 0.020 | 0.15 | 0.68 | 0.11, 1.26 | 0.021 | 0.18 | 164 | −44, 371 | 0.120 | 0.16 |
| Shortness of breath | 71 | −229, 372 | 0.637 | 0.09 | −0.02 | −0.59, 0.56 | 0.955 | 0.11 | −2 | −204, 200 | 0.982 | 0.14 |
| Chest tightness | 193 | −117, 503 | 0.219 | 0.11 | 0.11 | −0.48, 0.71 | 0.713 | 0.11 | 87 | −122, 297 | 0.407 | 0.14 |
| Sore throat | 51 | −244, 346 | 0.730 | 0.09 | −0.06 | −0.62, 0.51 | 0.844 | 0.11 | 10 | −188, 208 | 0.922 | 0.14 |
| Loss of taste/smell | 419 | 123, 715 | 0.006 | 0.18 | 0.70 | 0.13, 1.27 | 0.017 | 0.18 | 279 | 81, 478 | 0.007 | 0.22 |
| Runny/stuffed nose | 42 | −263, 347 | 0.786 | 0.09 | −0.03 | −0.61, 0.55 | 0.920 | 0.11 | 26 | −179, 231 | 0.802 | 0.14 |
| Body aches | 638 | 308, 968 | <0.001 | 0.24 | 1.07 | 0.43, 1.71 | 0.001 | 0.23 | 377 | 151, 603 | 0.001 | 0.25 |
| Headaches | 512 | 202, 821 | 0.002 | 0.21 | 0.86 | 0.26, 1.46 | 0.005 | 0.20 | 285 | 73, 497 | 0.009 | 0.21 |
| Low appetite | 527 | 239, 815 | <0.001 | 0.23 | 1.05 | 0.51, 1.59 | <0.001 | 0.26 | 351 | 158, 544 | 0.001 | 0.27 |
| Nausea | 238 | −67, 543 | 0.124 | 0.12 | 0.62 | 0.05, 1.19 | 0.035 | 0.17 | 124 | −82, 330 | 0.235 | 0.15 |
| Vomiting | 205 | −225, 634 | 0.345 | 0.10 | 1.02 | 0.23, 1.80 | 0.012 | 0.19 | 171 | −116, 458 | 0.238 | 0.15 |
| Abdominal pain | 197 | −194, 588 | 0.320 | 0.10 | 0.32 | −0.43, 1.06 | 0.396 | 0.12 | 144 | −118, 406 | 0.276 | 0.15 |
| Diarrhea | 258 | −52, 569 | 0.101 | 0.12 | 0.21 | −0.39, 0.81 | 0.483 | 0.12 | 143 | −66, 352 | 0.177 | 0.16 |
| Moderate disease | 482 | 34, 930 | 0.035 | 0.14 | 0.57 | −0.29, 1.44 | 0.191 | 0.13 | 302 | −0.1, 604 | 0.050 | 0.18 |
| Number of symptoms | 95 | 52, 138 | <0.001 | 0.28 | 0.17 | 0.08, 0.25 | <0.001 | 0.27 | 56 | 27, 86 | <0.001 | 0.28 |
|
| ||||||||||||
| Symptom a | sqrt[IgG(Nucleocapsid)] | log[ACE2 Inhibition] | log[Neut Titer] | |||||||||
| β | 95% CI | p | Adj. R2 | β | 95% CI | p | Adj. R2 | β | 95% CI | p | Adj. R2 | |
|
| ||||||||||||
| Fever | 340 | −40, 721 | 0.079 | 0.15 | 0.80 | 0.13, 1.48 | 0.020 | 0.20 | 1.15 | 0.50, 1.80 | 0.001 | 0.22 |
| Chills | 257 | −162, 676 | 0.226 | 0.14 | 0.47 | −0.27, 1.21 | 0.212 | 0.18 | 0.52 | −0.23, 1.27 | 0.168 | 0.13 |
| Productive cough | 121 | −282, 525 | 0.551 | 0.11 | 0.46 | −0.26, 1.18 | 0.209 | 0.16 | 0.78 | 0.08, 1.48 | 0.029 | 0.15 |
| Dry cough | 150 | −244, 544 | 0.450 | 0.12 | 0.72 | 0.03, 1.41 | 0.040 | 0.19 | 0.71 | 0.02, 1.40 | 0.044 | 0.14 |
| Shortness of breath | −222 | −597, 152 | 0.241 | 0.13 | −0.03 | −0.71, 0.65 | 0.922 | 0.14 | −0.02 | −0.71, 0.66 | 0.947 | 0.09 |
| Chest tightness | 158 | −234, 550 | 0.424 | 0.12 | 0.22 | −0.49, 0.92 | 0.544 | 0.14 | 0.37 | −0.34, 1.07 | 0.304 | 0.11 |
| Sore throat | −111 | −482, 259 | 0.550 | 0.11 | −0.06 | −0.73, 0.60 | 0.855 | 0.14 | −0.03 | −0.70, 0.64 | 0.926 | 0.09 |
| Loss of taste/smell | 380 | −1, 762 | 0.051 | 0.15 | 0.73 | 0.04, 1.41 | 0.037 | 0.19 | 0.87 | 0.18, 1.56 | 0.014 | 0.16 |
| Runny/stuffed nose | 129 | −254, 512 | 0.504 | 0.11 | −0.07 | −0.76, 0.62 | 0.834 | 0.14 | −0.05 | −0.74, 0.63 | 0.879 | 0.09 |
| Body aches | 406 | −39, 850 | 0.073 | 0.15 | 0.88 | 0.10, 1.67 | 0.029 | 0.20 | 1.16 | 0.39, 1.94 | 0.004 | 0.19 |
| Headaches | 423 | 18, 828 | 0.041 | 0.16 | 0.89 | 0.17, 1.61 | 0.016 | 0.21 | 1.10 | 0.41, 1.78 | 0.002 | 0.20 |
| Low appetite | 429 | 49, 809 | 0.028 | 0.17 | 0.99 | 0.33, 1.66 | 0.004 | 0.23 | 1.08 | 0.41, 1.75 | 0.002 | 0.20 |
| Nausea | 328 | −55, 710 | 0.092 | 0.14 | 0.01 | −0.69, 0.71 | 0.981 | 0.14 | 0.34 | −0.36, 1.03 | 0.338 | 0.11 |
| Vomiting | 517 | −12. 1047 | 0.055 | 0.15 | −0.12 | −1.10, 0.85 | 0.799 | 0.14 | 0.16 | −0.83, 1.15 | 0.749 | 0.10 |
| Abdominal pain | 110 | −385, 604 | 0.660 | 0.11 | 0.25 | −0.63, 1.14 | 0.571 | 0.14 | 0.63 | −0.22, 1.47 | 0.144 | 0.12 |
| Diarrhea | 316 | −74, 707 | 0.110 | 0.14 | 0.43 | −0.28, 1.13 | 0.230 | 0.16 | 0.40 | −0.31, 1.10 | 0.269 | 0.11 |
| Moderate disease | 476 | −94, 1047 | 0.100 | 0.14 | 1.35 | 0.36, 2.34 | 0.008 | 0.22 | 1.23 | 0.21, 2.26 | 0.019 | 0.16 |
| Number of symptoms | 77 | 19, 135 | 0.010 | 0.19 | 0.14 | 0.04, 0.25 | 0.007 | 0.22 | 0.19 | 0.09, 0.29 | <0.001 | 0.24 |
All models adjusted for age, sex, BMI, and Charlson Comorbidity Index Score
Since almost all subjects experienced more than one symptom, we also evaluated if the combination of symptoms included in moderate disease (severity score 2: fever, chills, productive cough, or shortness of breath, but not hospitalized) or the total number of symptoms correlated with antibody levels. As shown in Table 4, having a combination of symptoms indicative of moderate disease correlated with some antibody levels, but the explanatory power was not enhanced since the adjusted R2 value fell within the range of adjusted R2 values from symptom-specific regression models. This was unsurprising since most people experienced multiple symptoms. However, there was evidence that number of symptoms experienced had greater explanatory power (i.e., higher adjusted R2 values) of the variability in each of the antibody levels after adjusting for age, sex, BMI, and Charlson Comorbidity Score.
Finally, we evaluated the antibody response against SARS-CoV-2 and other coronaviruses in COVID-19 convalescent subjects three months post symptom resolution. In our cohort as a whole, anti-SARS-CoV-2 IgG, RBD-ACE2 binding inhibition, and neutralizing titers did not decline from five weeks to three months post-symptom resolution (Figure 4). However, when hospitalized and non-hospitalized subjects were analyzed separately (Figure 4), anti-spike and anti-nucleocapsid IgG rose slightly in hospitalized subjects (area under the curve: 4,525,184 +/− 796,452 versus 5,247,312 +/− 811,346 and 5,765,064 +/− 588,170 versus 7,004,295 +/− 654,857, respectively) and neutralizing titers decreased slightly in non-hospitalized subjects (titers: 49 +/− 11 versus 37 +/−10) over time. Titers against SARS-CoV and seasonal coronaviruses also did not fall regardless of hospitalization status, and rose slightly for seasonal coronaviruses (Supplementary Figure 2).
Figure 4. Antibodies against SARS-CoV-2 persist three months after COVID-19 symptom resolution.
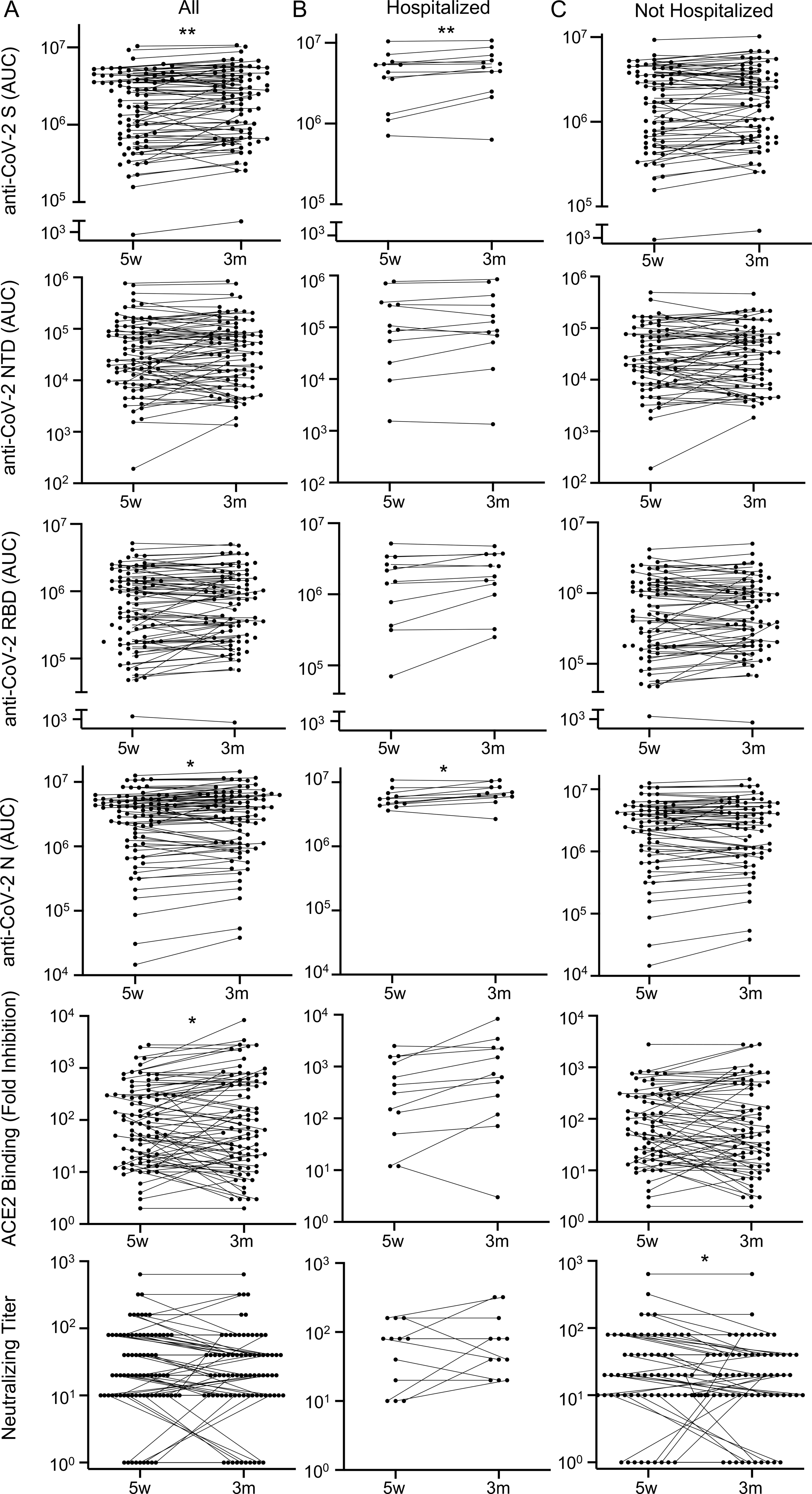
Sera from COVID-19 convalescent subjects collected 5 weeks (w) and 3 months (m) after symptom resolution were subjected to multiplex assay to detect IgG that binds to SARS-CoV-2 S, NTD, RBD and N antigens, to RBD-ACE2 binding inhibition assay, and to SARS-CoV-2 neutralization assay. Dots with lines connecting the two time points for individual subjects are shown for (A) all subjects (n=79), (B) hospitalized subjects (n=12), and (C) non-hospitalized subjects (n=67) with *p<0.05 and **p<0.01 by paired t test.
DISCUSSION
We have demonstrated that the vast majority of COVID-19 convalescent subjects generate antibodies against SARS-CoV-2 that inhibit ACE2 binding, neutralize live SARS-CoV-2, and persist at least three months post-COVID-19 symptom resolution. Further, greater disease severity, older age, male sex, higher BMI, higher Charlson Comorbidity Index score, fever, body aches and low appetite consistently correlate with higher antibody titers.
Although we detected IgG against SARS-CoV-2 in the majority of COVID-19 convalescent subjects, there was variability among tests. IgG levels against spike and RBD, but not NTD or nucleocapsid, showed an impressive difference between COVID-19 convalescent and control sera. Similar strong results were observed for RBD-ACE2 binding inhibition. Of note, two convalescent subjects had similar values to naive subjects in all three tests. It is unknown if these subjects had false positive SARS-CoV-2 PCR tests, if they did not make antibodies, or if our tests were insufficiently sensitive.
All of the antibody tests correlated well with neutralizing titers, a gold standard for protective antibodies. This correlation is encouraging, suggesting that our antibody assays are measuring relevant antibodies without the cost, hazards, time, and expertise needed for neutralizing assays. However, similar to related studies (24, 25), more COVID-19 convalescent subjects had antibody titers no higher than naive controls using the neutralizing assay as compared to other assays. It is unknown if these subjects truly lack protective antibodies (in many cases despite the presence of anti-SARS-CoV-2 IgG) or if the neutralization assay is insufficiently sensitive.
In addition to the development of anti-SARS-CoV-2 antibodies in COVID-19 convalescent sera five weeks post-symptom resolution, we saw a small increase in antibodies against seasonal betacoronaviruses (OC43 and HKU1), but not alphacoronaviruses (NL63 and 229E), likely because SARS-CoV-2 is a betacoronavirus (30). Moreover, antibodies that bind to seasonal coronaviruses rose slightly from five weeks to three months post-symptom resolution. This “back boost” phenomenon (31) could represent cross-reactivity of newly developed anti-SARS-CoV-2 antibodies and/or stimulation of memory B cells originally developed in response to circulating coronaviruses. In contrast, the high anti-SARS-CoV levels seen in COVID-19 convalescent subjects, which did not change over time, are probably due to cross-reactive anti-SARS-CoV-2 antibodies, since the Wisconsin cohort was almost certainly not exposed to SARS-CoV.
Similar to recent reports (21–23, 32–34), we demonstrated that anti-SARS-CoV-2 antibodies were highest in patients with severe disease, perhaps due to different immunophenotypes in COVID-19 patients (35) with a stronger inflammatory response in severe disease driving higher antibody titers. We also found that in non-hospitalized patients, higher antibody levels correlated with older age, male sex, higher BMI, and higher Charlson Comorbidity Index score. These factors all correlated with severe disease in our cohort as measured by hospitalization except for BMI, which others have reported to be associated with severe disease (36). Thus, non-hospitalized subjects with these high-risk characteristics might have had relatively severe disease that our methods could not measure, driving higher antibody levels. Alternatively, these characteristics could contribute directly to increased antibody levels. However, other reports suggest that older age and obesity impair antibody responses (37), and males have no generalizable increased antibody response (38). Of note, the correlation between anti-SARS-CoV-2 antibody titers with age, sex, and obesity has been previously reported (23, 39), but we are the first to report a correlation with the Charlson Comorbidity Index score.
In addition to disease severity, we report for the first time that specific COVID-19 symptoms correlate with higher anti-SARS-CoV-2 antibody levels. Fever, body aches, and low appetite, which consistently correlated with higher antibody levels in both univariate and multivariable analyses, can be signs of a systemic inflammatory response, which is likely key for developing a strong anti-SARS-CoV-2 antibody response. Gastrointestinal symptoms correlated with older age, higher BMI, more comorbidities, and male sex as well as higher antibody levels. Thus, it is difficult to determine if disease severity, one of these clinical factors, or gastrointestinal symptoms might drive antibody development. Diarrhea, typically caused by enteric viral infection and damage, may directly exacerbate inflammation and COVID-19 severity (40) causing higher antibody titers. Alternatively, diarrhea may simply be more common in severe disease, which correlates with age, BMI, Charlson Comorbidity Index score, and male sex, although we did not see increased diarrhea in our hospitalized patients.
Interestingly, loss of taste or smell, a unique feature of COVID-19, is associated with higher antibody levels only in the multiple linear regression analysis, suggesting that it is a predictor of higher antibody titers independent of severe disease correlates, namely BMI, age, Charlson Comorbidity Index score, and male sex. The mechanism for loss of taste or smell remains unclear. It seems unlikely that anti-SARS-CoV-2 antibodies cause this symptom, since only a small percentage of subjects have antibodies early in disease when loss of taste and smell occurs (41). Moreover, a mechanism by which this symptom could drive higher antibody levels is similarly hard to imagine. Thus, the relationship between loss of taste and smell and antibody titers is likely indirect, driven by factors that remain to be discovered.
Finally, many symptoms did not correlate consistently or at all with antibody levels including shortness of breath, which was associated with higher antibody levels in COVID-19 convalescent plasma donors in a previous study (24). However, that study (24) had fewer subjects than our study with plasma donated at various times post-COVID-19 and no other symptoms evaluated. Many symptoms that did not correlate with antibody levels also did not correlate with severe disease and may not be related to the inflammation that drives antibody production.
Finally, we found that antibodies persist at least three months after symptom resolution. Some antibody levels even continued to rise slightly during this time period, although neutralizing titers fell slightly in non-hospitalized subjects. Our findings are discrepant from some studies, which reported falling antibody levels against SARS-CoV-2 within a few months of disease (12–21). However, these studies had smaller sample sizes (particularly at later time points), variable or unclear time points as related to symptom resolution, antibody loss in subjects with mild or asymptomatic disease, or no clinical data. Our findings are consistent with reports of persistent antibody titers at least three to six months after disease (8–11). As time goes on, additional studies will be needed at later time points that use a variety of antibody detection methods, defined collection time points, and extensive clinical data.
There are a few caveats to our studies. First, samples were not collected prior to five weeks post-symptom resolution due to logistical issues such as limited personal protective equipment early in the pandemic when the biorepository was established. Similarly, at the time that this study was performed, samples had not yet been collected later than 3 months from symptom resolution, a task that is currently underway. Also, COVID-19 symptoms were self-reported up to a month after symptom resolution, which could lead to recall error. Additionally, some medical records were incomplete with no recent primary care or admission note for 19% of subjects and incomplete BMI data for 14%. This gap would be biased toward non-hospitalized patients. Also, our population was relatively racially and ethnically homogeneous. However, our study is strong in its wide breadth of COVID-19 severity in 113 subjects with consistent time points and multiple types of antibody tests.
In sum, we report that anti-SARS-CoV-2 antibodies last at least three months post-symptom resolution and that antibody titers consistently correlate with fever, body aches, low appetite, older age, male sex, higher COVID-19 severity, higher BMI, and higher Charlson Comorbidity Index score. Further work is needed to determine protective antibody levels against re-infection, how long protective titers last, and the mechanisms by which COVID-19 symptoms, demographics, and comorbidities may drive higher antibody levels.
Supplementary Material
ACKNOWLEDGEMENTS
We thank the UW Office of Clinical Trials and the UW Carbone Cancer Center Translational Science BioCore as well as the human subjects who participated in this study.
Funding: This work was supported by a COVID-19 Response grant from the Wisconsin Partnership Program [4647] and the Department of Medicine, both at the UW School of Medicine and Public Health to M.A.S. Additional support was provided by the National Institutes of Health’s National Institute on Aging to M.F.A. [T32 AG000213], National Heart, Lung, and Blood Institute [T32 HL007899] to A.M.M., and National Institute of Allergy and Infectious Disease to A.S.H. [T32 AI007414].
REFERENCES
- 1.2020. Novel Coronavirus (2019-nCoV) Situation Report. World Health Organization: 5. [Google Scholar]
- 2.Fu L, Wang B, Yuan T, Chen X, Ao Y, Fitzpatrick T, Li P, Zhou Y, Lin YF, Duan Q, Luo G, Fan S, Lu Y, Feng A, Zhan Y, Liang B, Cai W, Zhang L, Du X, Li L, Shu Y, and Zou H. 2020. Clinical characteristics of coronavirus disease 2019 (COVID-19) in China: A systematic review and meta-analysis. J Infect 80: 656–665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.worldometer. https://www.worldometers.info/coronavirus/.
- 4.Haleem A, Javaid M, and Vaishya R. 2020. Effects of COVID-19 pandemic in daily life. Curr Med Res Pract 10: 78–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chang SC, Wang JT, Huang LM, Chen YC, Fang CT, Sheng WH, Wang JL, Yu CJ, and Yang PC. 2005. Longitudinal analysis of Severe Acute Respiratory Syndrome (SARS) coronavirus-specific antibody in SARS patients. Clin Diagn Lab Immunol 12: 1455–1457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shi Y, Wan Z, Li L, Li P, Li C, Ma Q, and Cao C. 2004. Antibody responses against SARS-coronavirus and its nucleocaspid in SARS patients. J Clin Virol 31: 66–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Liu L, Xie J, Sun J, Han Y, Zhang C, Fan H, Liu Z, Qiu Z, He Y, and Li T. 2011. Longitudinal profiles of immunoglobulin G antibodies against severe acute respiratory syndrome coronavirus components and neutralizing activities in recovered patients. Scand J Infect Dis 43: 515–521. [DOI] [PubMed] [Google Scholar]
- 8.Dan JM, Mateus J, Kato Y, Hastie KM, Yu ED, Faliti CE, Grifoni A, Ramirez SI, Haupt S, Frazier A, Nakao C, Rayaprolu V, Rawlings SA, Peters B, Krammer F, Simon V, Saphire EO, Smith DM, Weiskopf D, Sette A, and Crotty S. 2021. Immunological memory to SARS-CoV-2 assessed for up to 8 months after infection. Science. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wu J, Liang B, Chen C, Wang H, Fang Y, Shen S, Yang X, Wang B, Chen L, Chen Q, Wu Y, Liu J, Yang X, Li W, Zhu B, Zhou W, Wang H, Li S, Lu S, Liu D, Li H, Krawczyk A, Lu M, Yang D, Deng F, Dittmer U, Trilling M, and Zheng X. 2020. SARS-CoV-2 infection induces sustained humoral immune responses in convalescent patients following symptomatic COVID-19. medRxiv. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pradenas E, Trinité B, Urrea V, Marfil S, Ávila-Nieto C, Rodríguez de la Concepción ML, Tarrés-Freixas F, Pérez-Yanes S, Rovirosa C, Ainsua-Enrich E, Rodon J, Vergara-Alert J, Segalés J, Guallar V, Valencia A, Izquierdo-Useros N, Paredes R, Mateu L, Chamorro A, Massanella M, Carrillo J, Clotet B, and Blanco J. 2020. Stable neutralizing antibody levels six months after mild and severe COVID-19 episode. bioRxiv. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rodda LB, Netland J, Shehata L, Pruner KB, Morawski PA, Thouvenel CD, Takehara KK, Eggenberger J, Hemann EA, Waterman HR, Fahning ML, Chen Y, Hale M, Rathe J, Stokes C, Wrenn S, Fiala B, Carter L, Hamerman JA, King NP, Gale M, Campbell DJ, Rawlings DJ, and Pepper M. 2021. Functional SARS-CoV-2-Specific Immune Memory Persists after Mild COVID-19. Cell 184: 169–183.e117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Korte W, Buljan M, Rösslein M, Wick P, Golubov V, Jentsch J, Reut M, Peier K, Nohynek B, Fischer A, Stolz R, Cettuzzi M, and Nolte O. 2020. SARS-CoV-2 IgG and IgA antibody response is gender dependent; and IgG antibodies rapidly decline early on. J Infect. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yin S, Tong X, Huang A, Shen H, Li Y, Liu Y, Wu C, Huang R, and Chen Y. 2020. Longitudinal anti-SARS-CoV-2 antibody profile and neutralization activity of a COVID-19 patient. J Infect. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Röltgen K, Wirz OF, Stevens BA, Powell AE, Hogan CA, Najeeb J, Hunter M, Sahoo MK, Huang C, Yamamoto F, Manalac J, Otrelo-Cardoso AR, Pham TD, Rustagi A, Rogers AJ, Shah NH, Blish CA, Cochran JR, Nadeau KC, Jardetzky TS, Zehnder JL, Wang TT, Kim PS, Gombar S, Tibshirani R, Pinsky BA, and Boyd SD. 2020. SARS-CoV-2 Antibody Responses Correlate with Resolution of RNAemia But Are Short-Lived in Patients with Mild Illness. medRxiv. [Google Scholar]
- 15.Seow J, Graham C, Merrick B, Acors S, Pickering S, Steel KJA, Hemmings O, O’Byrne A, Kouphou N, Galao RP, Betancor G, Wilson HD, Signell AW, Winstone H, Kerridge C, Huettner I, Jimenez-Guardeño JM, Lista MJ, Temperton N, Snell LB, Bisnauthsing K, Moore A, Green A, Martinez L, Stokes B, Honey J, Izquierdo-Barras A, Arbane G, Patel A, Tan MKI, O’Connell L, O’Hara G, MacMahon E, Douthwaite S, Nebbia G, Batra R, Martinez-Nunez R, Shankar-Hari M, Edgeworth JD, Neil SJD, Malim MH, and Doores KJ. 2020. Longitudinal observation and decline of neutralizing antibody responses in the three months following SARS-CoV-2 infection in humans. Nat Microbiol 5: 1598–1607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ibarrondo FJ, Fulcher JA, Goodman-Meza D, Elliott J, Hofmann C, Hausner MA, Ferbas KG, Tobin NH, Aldrovandi GM, and Yang OO. 2020. Rapid Decay of Anti-SARS-CoV-2 Antibodies in Persons with Mild Covid-19. N Engl J Med. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Long QX, Tang XJ, Shi QL, Li Q, Deng HJ, Yuan J, Hu JL, Xu W, Zhang Y, Lv FJ, Su K, Zhang F, Gong J, Wu B, Liu XM, Li JJ, Qiu JF, Chen J, and Huang AL. 2020. Clinical and immunological assessment of asymptomatic SARS-CoV-2 infections. Nat Med. [DOI] [PubMed] [Google Scholar]
- 18.Liu A, Li Y, Peng J, Huang Y, and Xu D. 2020. Antibody responses against SARS-CoV-2 in COVID-19 patients. J Med Virol. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Girardin RC, Dupuis AP, Payne AF, Sullivan TJ, Strauss D, Parker MM, and McDonough KA. 2021. Temporal Analysis of Serial Donations Reveals Decrease in Neutralizing Capacity and Justifies Revised Qualifying Criteria for COVID-19 Convalescent Plasma. J Infect Dis. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wajnberg A, Amanat F, Firpo A, Altman DR, Bailey MJ, Mansour M, McMahon M, Meade P, Mendu DR, Muellers K, Stadlbauer D, Stone K, Strohmeier S, Simon V, Aberg J, Reich DL, Krammer F, and Cordon-Cardo C. 2020. Robust neutralizing antibodies to SARS-CoV-2 infection persist for months. Science 370: 1227–1230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bonifacius A, Tischer-Zimmermann S, Dragon AC, Gussarow D, Vogel A, Krettek U, Gödecke N, Yilmaz M, Kraft ARM, Hoeper MM, Pink I, Schmidt JJ, Li Y, Welte T, Maecker-Kolhoff B, Martens J, Berger MM, Lobenwein C, Stankov MV, Cornberg M, David S, Behrens GMN, Witzke O, Blasczyk R, and Eiz-Vesper B. 2021. COVID-19 immune signatures reveal stable antiviral T cell function despite declining humoral responses. Immunity 54: 340–354.e346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Marklund E, Leach S, Axelsson H, Nyström K, Norder H, Bemark M, Angeletti D, Lundgren A, Nilsson S, Andersson LM, Yilmaz A, Lindh M, Liljeqvist J, and Gisslén M. 2020. Serum-IgG responses to SARS-CoV-2 after mild and severe COVID-19 infection and analysis of IgG non-responders. PLoS One 15: e0241104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Klein SL, Pekosz A, Park HS, Ursin RL, Shapiro JR, Benner SE, Littlefield K, Kumar S, Naik HM, Betenbaugh MJ, Shrestha R, Wu AA, Hughes RM, Burgess I, Caturegli P, Laeyendecker O, Quinn TC, Sullivan D, Shoham S, Redd AD, Bloch EM, Casadevall A, and Tobian AA. 2020. Sex, age, and hospitalization drive antibody responses in a COVID-19 convalescent plasma donor population. J Clin Invest 130: 6141–6150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Salazar E, Kuchipudi SV, Christensen PA, Eagar T, Yi X, Zhao P, Jin Z, Long SW, Olsen RJ, Chen J, Castillo B, Leveque C, Towers D, Lavinder JJ, Gollihar J, Cardona JA, Ippolito GC, Nissly RH, Bird I, Greenawalt D, Rossi RM, Gontu A, Srinivasan S, Poojary I, Cattadori IM, Hudson P, Josleyn NM, Prugar L, Huie KE, Herbert AS, Bernard DW, Dye JM, Kapur V, and Musser JM. 2020. Convalescent plasma anti-SARS-CoV-2 spike protein ectodomain and receptor binding domain IgG correlate with virus neutralization. J Clin Invest. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rijkers G, Murk JL, Wintermans B, van Looy B, van den Berge M, Veenemans J, Stohr J, Reusken C, van der Pol P, and Reimerink J. 2020. Differences in antibody kinetics and functionality between severe and mild SARS-CoV-2 infections. J Infect Dis. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Holmes CL, Peyton CG, Bier AM, Donlon TZ, Osman F, Bartels CM, and Shelef MA. 2019. Reduced IgG titers against pertussis in rheumatoid arthritis: Evidence for a citrulline-biased immune response and medication effects. PLoS One 14: e0217221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kind AJH, and Buckingham WR. 2018. Making Neighborhood-Disadvantage Metrics Accessible - The Neighborhood Atlas. N Engl J Med 378: 2456–2458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Charlson ME, Pompei P, Ales KL, and MacKenzie CR. 1987. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40: 373–383. [DOI] [PubMed] [Google Scholar]
- 29.Alkhouli M, Nanjundappa A, Annie F, Bates MC, and Bhatt DL. 2020. Sex Differences in Case Fatality Rate of COVID-19: Insights From a Multinational Registry. Mayo Clin Proc 95: 1613–1620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zhou P, Yang XL, Wang XG, Hu B, Zhang L, Zhang W, Si HR, Zhu Y, Li B, Huang CL, Chen HD, Chen J, Luo Y, Guo H, Jiang RD, Liu MQ, Chen Y, Shen XR, Wang X, Zheng XS, Zhao K, Chen QJ, Deng F, Liu LL, Yan B, Zhan FX, Wang YY, Xiao GF, and Shi ZL. 2020. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature 579: 270–273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fonville JM, Wilks SH, James SL, Fox A, Ventresca M, Aban M, Xue L, Jones TC, Le NMH, Pham QT, Tran ND, Wong Y, Mosterin A, Katzelnick LC, Labonte D, Le TT, van der Net G, Skepner E, Russell CA, Kaplan TD, Rimmelzwaan GF, Masurel N, de Jong JC, Palache A, Beyer WEP, Le QM, Nguyen TH, Wertheim HFL, Hurt AC, Osterhaus ADME, Barr IG, Fouchier RAM, Horby PW, and Smith DJ. 2014. Antibody landscapes after influenza virus infection or vaccination. Science 346: 996–1000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wang P, Liu L, Nair MS, Yin MT, Luo Y, Wang Q, Yuan T, Mori K, Solis AG, Yamashita M, Garg A, Purpura LJ, Laracy JC, Yu J, Joshua-Tor L, Sodroski J, Huang Y, and Ho DD. 2020. SARS-CoV-2 neutralizing antibody responses are more robust in patients with severe disease. Emerg Microbes Infect 9: 2091–2093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chen X, Pan Z, Yue S, Yu F, Zhang J, Yang Y, Li R, Liu B, Yang X, Gao L, Li Z, Lin Y, Huang Q, Xu L, Tang J, Hu L, Zhao J, Liu P, Zhang G, Chen Y, Deng K, and Ye L. 2020. Disease severity dictates SARS-CoV-2-specific neutralizing antibody responses in COVID-19. Signal Transduct Target Ther 5: 180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wang Y, Zhang L, Sang L, Ye F, Ruan S, Zhong B, Song T, Alshukairi AN, Chen R, Zhang Z, Gan M, Zhu A, Huang Y, Luo L, Mok CKP, Al Gethamy MM, Tan H, Li Z, Huang X, Li F, Sun J, Zhang Y, Wen L, Li Y, Chen Z, Zhuang Z, Zhuo J, Chen C, Kuang L, Wang J, Lv H, Jiang Y, Li M, Lin Y, Deng Y, Tang L, Liang J, Huang J, Perlman S, Zhong N, Zhao J, and Malik Peiris JS. 2020. Kinetics of viral load and antibody response in relation to COVID-19 severity. J Clin Invest 130: 5235–5244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mathew D, Giles JR, Baxter AE, Oldridge DA, Greenplate AR, Wu JE, Alanio C, Kuri-Cervantes L, Pampena MB, D’Andrea K, Manne S, Chen Z, Huang YJ, Reilly JP, Weisman AR, Ittner CAG, Kuthuru O, Dougherty J, Nzingha K, Han N, Kim J, Pattekar A, Goodwin EC, Anderson EM, Weirick ME, Gouma S, Arevalo CP, Bolton MJ, Chen F, Lacey SF, Ramage H, Cherry S, Hensley SE, Apostolidis SA, Huang AC, Vella LA, Betts MR, Meyer NJ, Wherry EJ, and Unit UCP. 2020. Deep immune profiling of COVID-19 patients reveals distinct immunotypes with therapeutic implications. Science 369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hussain A, Mahawar K, Xia Z, Yang W, and El-Hasani S. 2020. Obesity and mortality of COVID-19. Meta-analysis. Obes Res Clin Pract 14: 295–300. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 37.Frasca D, Diaz A, Romero M, and Blomberg BB. 2017. Ageing and obesity similarly impair antibody responses. Clin Exp Immunol 187: 64–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kumakura S, Shibata H, Onoda K, Nishimura N, Matsuda C, and Hirose M. 2014. Seroprevalence survey on measles, mumps, rubella and varicella antibodies in healthcare workers in Japan: sex, age, occupational-related differences and vaccine efficacy. Epidemiol Infect 142: 12–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Petersen LR, Sami S, Vuong N, Pathela P, Weiss D, Morgenthau BM, Henseler RA, Daskalakis DC, Atas J, Patel A, Lukacs S, Mackey L, Grohskopf LA, Thornburg N, and Akinbami LJ. 2020. Lack of antibodies to SARS-CoV-2 in a large cohort of previously infected persons. Clin Infect Dis. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wang F, Zheng S, Zheng C, and Sun X. 2020. Attaching clinical significance to COVID-19-associated diarrhea. Life Sci 260: 118312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Long QX, Liu BZ, Deng HJ, Wu GC, Deng K, Chen YK, Liao P, Qiu JF, Lin Y, Cai XF, Wang DQ, Hu Y, Ren JH, Tang N, Xu YY, Yu LH, Mo Z, Gong F, Zhang XL, Tian WG, Hu L, Zhang XX, Xiang JL, Du HX, Liu HW, Lang CH, Luo XH, Wu SB, Cui XP, Zhou Z, Zhu MM, Wang J, Xue CJ, Li XF, Wang L, Li ZJ, Wang K, Niu CC, Yang QJ, Tang XJ, Zhang Y, Liu XM, Li JJ, Zhang DC, Zhang F, Liu P, Yuan J, Li Q, Hu JL, Chen J, and Huang AL. 2020. Antibody responses to SARS-CoV-2 in patients with COVID-19. Nat Med 26: 845–848. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


