Abstract
Background:
Secondary hypertension has emerged as a major public health problem in China. Early diagnosis and treatment can significantly improve the clinical outcomes. However, data on the current cause composition in China are seldom reported.
Objective:
To describe the trends in cause-related comorbidities in hospitalized patients with secondary hypertension in China from 2013 to 2016.
Methods:
This was a retrospective analysis based on the national Hospital Quality Monitoring System (HQMS) database, which collects information from the front pages of in-hospital medical records. Hospitalized patients with secondary hypertension from 746 tertiary hospitals that consistently uploaded data to the HQMS from 2013 to 2016 were enrolled. All diagnoses were identified using International Classification of Diseases version 10 (ICD-10) diagnostic codes. Descriptive analyses were used to determine the proportions of secondary hypertension causes and changing trends over 4 years.
Result:
The study collected data on 402 371 hospitalized patients with secondary hypertension from the HQMS during 2013–2016. Secondary hypertension caused by renal parenchymal disease ranked first and accounted for more than 50%. Obstructive sleep apnea syndrome (OSAS) followed closely with a rate of approximately 25%. Primary aldosteronism presented the highest proportion among all causes of endocrine hypertension. Regarding longitudinal changes over time, the rates of renal hypertension showed a significant downward trend from 2013 to 2016 (P < 0.001). In contrast, OSAS, endocrine hypertension, renal vascular disease, and aorta diseases maintained a significant upward trend from 2013 to 2016 (P < 0.001). The rates of these diseases in women with common secondary hypertension was higher than that of men, except in patients with OSAS (P < 0.001). In addition, renal parenchymal diseases and renal vascular diseases gradually decreased with age, whereas OSAS and aortic diseases gradually increased with age. The proportion of endocrine hypertension in the middle-aged group was higher than the other two age groups.
Conclusion:
The study provides important information on the changing trends of cause rate of secondary hypertension modified by age and sex in China during 2013–2016. Renal parenchymal disease is still the most common cause of secondary hypertension with a decreasing trend, followed by OSAS with an increasing trend.
Keywords: cause composition, obstructive sleep apnea syndrome, secondary hypertension
INTRODUCTION
Hypertension is a serious challenge for global public health and is recognized as an important factor for increased risk of stroke, cardiovascular disease, peripheral vascular disease, and mortality [1–4]. Secondary hypertension is hypertension with an identifiable cause that may be treatable with an intervention specific to the cause [5]. Approximately 5–10% of patients with elevated blood pressure have secondary hypertension [6]. The causes of secondary hypertension are complex and diverse and involve a wide range of diseases originating from other systems, resulting in high costs owing to secondary hypertension examinations and consumption of medical resources.
In addition to the harm caused by high blood pressure itself, secondary hypertension can be accompanied by other physiological states, such as electrolyte disturbance, endocrine imbalance, and hypoxemia, that can lead to cardiovascular damage independent of blood pressure [7,8]. The proportion of secondary hypertension in young hypertensive patients is extremely high, and the majority of these patients require specific treatment [5,9]. Therefore, early and accurate diagnosis and targeted treatment of secondary hypertension are important. Analysis of the cause and current status of hospitalized patients with secondary hypertension can help toward the development of more effective screening and treatment strategies.
Previous studies based on hospitalized patients with secondary hypertension have shown that renal parenchymal disease was the most common cause of secondary hypertension, and primary aldosteronism accounted for a relatively high proportion of cases [8,10–14]. A single-center study in China reported that obstructive sleep apnea syndrome (OSAS) and primary aldosteronism were the two leading causes of secondary hypertension [15]. However, these studies were limited by their sample size, study population, age span, and detection methods. Additionally, no data have revealed recent changes in the causes among hospitalized patients with secondary hypertension, especially in China. The Hospital Quality Monitoring System (HQMS) [16–19] is a mandatory national patient-level database for hospital accreditation, authorized by the National Health Commission of the People's Republic of China. Use of HQMS data provided us with the opportunity to analyze the causes of patients with secondary hypertension in tertiary hospitals across China. In this study, we aimed to explore the rates and changes in causes among hospitalized patients with secondary hypertension in China from 2013 to 2016.
METHODS
Data source
This was a retrospective analysis based on the HQMS, a national database that contains information from the front page of in-hospital medical records for patients in tertiary hospitals throughout China. Variables mainly include basic demographic information, up to 10 International Classification of Diseases (ICD) discharge diagnostic codes, certain treatment information, in-hospital death, and other discharge outcome information, hospitalization time, and total costs. All variables are encoded by certified professional medical coders in each hospital and then automatically uploaded to the HQMS. All data preprocessing and analysis were performed on a computer dedicated to database storage. For the purpose of our study, we selected the data of HQMS database from 2013 to 2016 for analysis. This study was authorized by the HQMS Committee Board and was approved by the Ethics Committee of Peking University First Hospital.
Case identification
To identify cases, we selected discharge diagnoses according to the ICD diagnostic codes in the HQMS. As the diagnostic codes for hypertension, common secondary hypertension, coronary heart disease, and cerebrovascular disease in the HQMS are numerous and complex, we arranged for two groups of cardiologists with substantial experience in clinical diagnosis to separately review and confirm the codes and criteria. Three sets of codes containing the most detailed diagnostic codes from different editions of the ICD-10 dictionary were used [20]. Regarding the diagnosis of common secondary hypertension, a separate detailed series of codes was established for several major diseases with high incidence reported in previous studies, including renal parenchymal disease, renal vascular disease, endocrine hypertension, diseases of the aorta, and OSAS [6,21]. All patients with hypertension admitted to 746 tertiary hospitals nationwide that had consistently uploaded data to the HQMS database from 1 January 2013 to 31 December 2016 were included, based on the hypertension diagnosis ICD-10 codes. We subsequently enrolled cases of secondary hypertension with a definite diagnosis of renal parenchymal disease, renal vascular disease, endocrine hypertension, aortic diseases, and OSAS, for further analysis.
Statistical analysis
Patient characteristics were presented as mean (SD) for continuous variables, and categorical variables were reported as percentage. We described and compared the changes in demographic data and proportions of various causes in each year for inpatients with hypertension and a diagnosis of secondary hypertension. Comparisons among groups were also stratified by age and sex. Continuous variables were compared using analysis of variance, and categorical variables were compared using the chi-square test. Linear trends over time in the models were also examined and reported as the P value for trend. All analyses were performed using R software version 3.4.3 (http://www.R-project.org). Statistical significance was set to P less than 0.05.
RESULTS
Patient characteristics
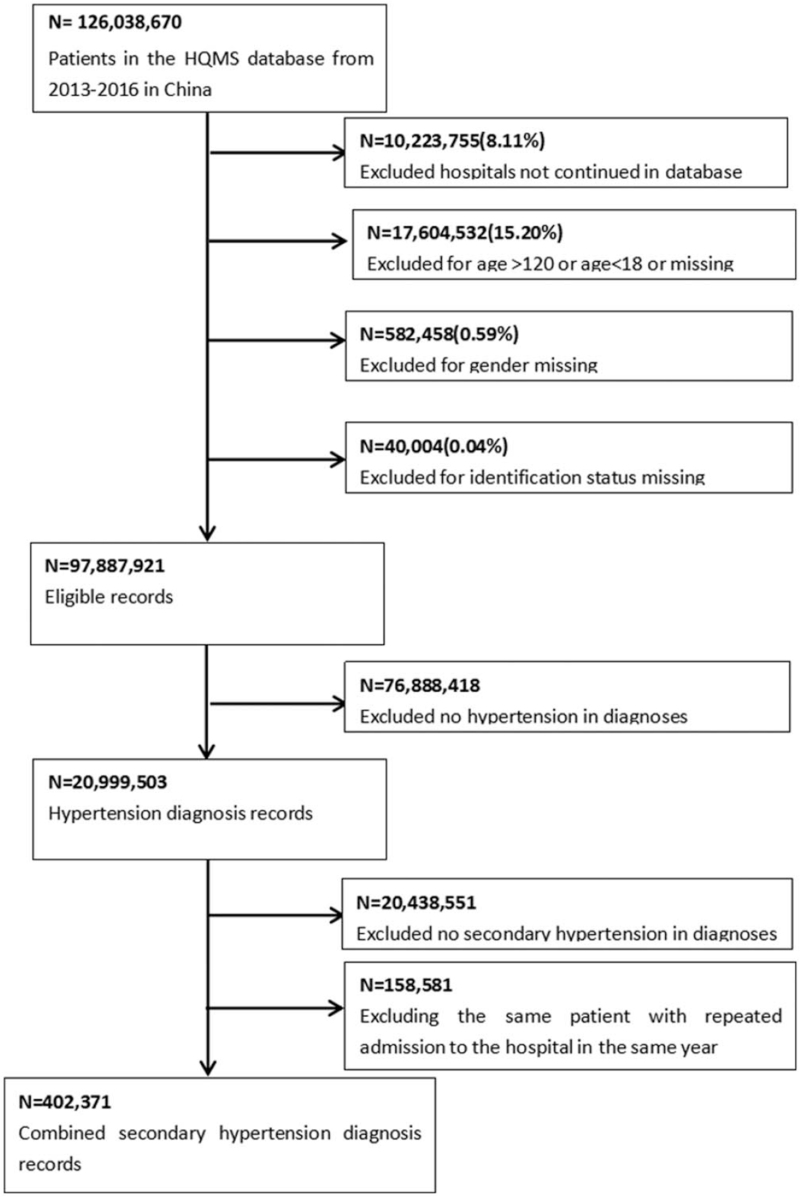
The database contained information for 126 038 670 inpatients from 746 tertiary hospitals in China between 2013 and 2016. We used ICD codes to screen a total of 20 999 503 patients aged more than 18 years who had a diagnosis of hypertension and complete demographic information. We then further screened patients using the ICD codes for common causes of secondary hypertension, to finally enroll a total of 402 371 patients in this study (Fig. 1). We grouped all enrolled patients by year, to analyze inpatient characteristics and explore the changing trends in conditions over time. Owing to multiple hospitalizations, there were a total of 72 691 patients in 2013, 100 867 patients in 2014, 110 678 patients in 2015, and 118 135 patients in 2016. The demographic characteristics for all patients, which were relatively similar among the 4 years, are presented in Table 1. For example, in 2016, the mean age of 118 135 hospitalized patients with secondary hypertension was 52.08 ± 15.08 years, and 61.30% were men. Among them, 10.70% had cerebrovascular disease and 13.23% had coronary heart disease. We excluded 28 881 patients (7.18%) from further cause-related analysis owing to a lack of detailed cause information for secondary hypertension.
FIGURE 1.
Data processing for identification of patients with secondary hypertension.
TABLE 1.
Characteristics of hospitalized patients with secondary hypertension in China from 2013 to 2016
| Variables | 2013 (72 691) | 2014 (100 867) | 2015 (110 678) | 2016 (118 135) | P value |
| Demographic characteristics | |||||
| Age, mean (SD) (years) | 51.23 (15.41) | 51.63 (15.27) | 51.77 (15.18) | 52.08 (15.08) | <0.001 |
| Male [n (%)] | 43 702 (60.12) | 60 817 (60.29) | 67 319 (60.82) | 72 417 (61.30) | <0.001 |
| Han [n (%)] | 63 549 (94.45) | 89 481 (94.59) | 98 442 (94.23) | 106 523 (94.05) | <0.001 |
| Major comorbid conditions | |||||
| Cerebrovascular disease [n (%)] | 6011 (8.26) | 9352 (9.27) | 11 000 (9.93) | 12 642 (10.70) | <0.001 |
| Coronary heart disease [n (%)] | 8043 (11.06) | 11 868 (11.76) | 13 851 (12.51) | 15 635 (13.23) | <0.001 |
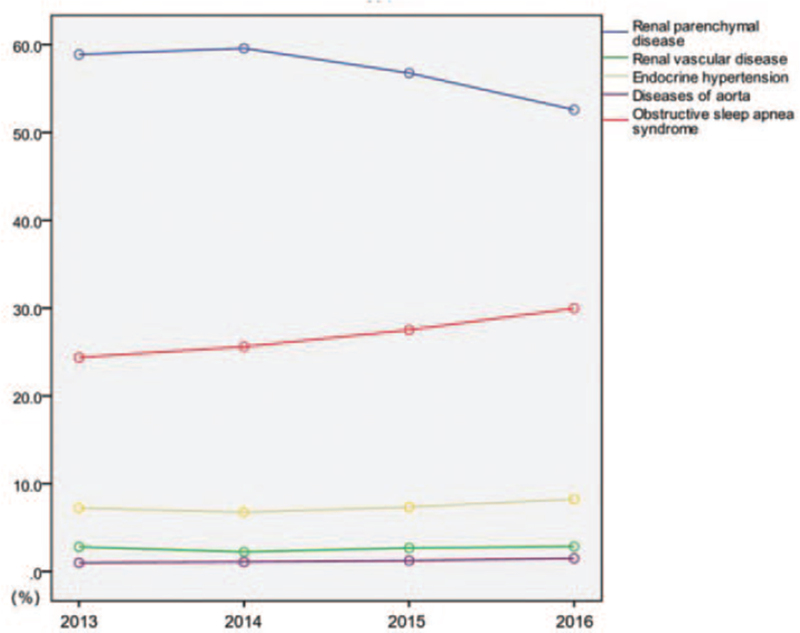
Trends in disease change, by year
Regarding causes (Table 2), secondary hypertension caused by renal parenchymal disease ranked first in each year, accounting for more than 50% of cases. OSAS followed closely, with an unexpected rate of approximately 25%; renal vascular disease and aortic disease accounted for smaller proportions of the overall population. Primary aldosteronism presented the highest proportion among all causes of endocrine hypertension. According to longitudinal changes over time (Fig. 2), the diagnosis rate of renal hypertension showed a significant downward trend from 2013 to 2016 (58.89--52.59%, respectively; P < 0.001). In contrast, endocrine hypertension (7.25% in 2013 to 8.25% in 2016, P < 0.001), particularly primary aldosteronism, increased gradually (5.49% in 2013 to 6.40% in 2016, P < 0.001). Notably, OSAS maintained a significant upward trend between 2013 and 2016 (24.39--29.98%, respectively; P < 0.001).
TABLE 2.
Rates of specific cause-related comorbidities in hospitalized patients with secondary hypertension in China from 2013 to 2016
| 2013 | 2014 | 2015 | 2016 | P for trend | |
| Renal parenchymal disease [n (%)] | 42 812 (58.89) | 60 106 (59.58) | 62 841 (56.77) | 62 129 (52.59) | <0.001 |
| Renal vascular disease [n (%)] | 2053 (2.82) | 2274 (2.25) | 2991 (2.70) | 3388 (2.86) | <0.001 |
| Endocrine hypertension [n (%)] | 5276 (7.25) | 6823 (6.76) | 8147 (7.36) | 9757 (8.25) | <0.001 |
| Cushing's syndrome [n (%)] | 771 (1.06) | 995 (0.98) | 1172 (1.05) | 1349 (1.14) | 0.012 |
| Primary aldosteronism [n (%)] | 3991 (5.49) | 5148 (5.10) | 6293 (5.68) | 7564 (6.40) | <0.001 |
| Pheochromocytoma [n (%)] | 444 (0.61) | 660 (0.65) | 659 (0.59) | 790 (0.66) | 0.313 |
| Diseases of aorta [n (%)] | 739 (1.01) | 1124 (1.11) | 1401 (1.26) | 1798 (1.52) | <0.001 |
| Obstructive sleep apnea syndrome [n (%)] | 17 732 (24.39) | 25 835 (25.61) | 30 467 (27.52) | 35 421 (29.98) | <0.001 |
FIGURE 2.
Trends in cause-related comorbidities among hospitalized patients with secondary hypertension, from 2013 to 2016.
Trends in disease change, by sex
Regardless of sex, the order of the causes and annual change in trends were similar to those in the overall population (Table 3 and Supplementary Table 1). Taking 2016 as an example, the diagnosis rates of renal parenchymal disease (58.72 vs. 48.71%, P < 0.001), renal vascular disease (3.20 vs. 2.65%, P < 0.001), endocrine hypertension (11.12 vs. 6.45%, P < 0.001), and diseases of the aorta (1.72 vs. 1.39%, P < 0.001) were much higher in female than in male patients. Only the rate of OSAS presented diametrically opposite results (18.48% in women vs. 37.24% in men, P < 0.001).
TABLE 3.
Rates of specific cause-related comorbidities in hospitalized patients with secondary hypertension in different sex groups in 2016
| Male | Female | P value | |
| Renal parenchymal disease [n (%)] | 35 280 (48.71) | 26 849 (58.72) | <0.001 |
| Renal vascular disease [n (%)] | 1923 (2.65) | 1465 (3.20) | <0.001 |
| Endocrine hypertension [n (%)] | 4672 (6.45) | 5085 (11.12) | <0.001 |
| Cushing's syndrome [n (%)] | 405 (0.55) | 944 (2.06) | <0.001 |
| Primary aldosteronism [n (%)] | 3898 (5.38) | 3666 (8.01) | <0.001 |
| Pheochromocytoma [n (%)] | 336 (0.46) | 454 (0.99) | <0.001 |
| Diseases of aorta [n (%)] | 1009 (1.39) | 789 (1.72) | <0.001 |
| Obstructive sleep apnea syndrome [n (%)] | 26 970 (37.24) | 8451 (18.48) | <0.001 |
Trends in disease change, by age
Patients were divided into three age groups: young (18–40 years), middle-aged (41–65 years), and older (>65 years). The rates of all diseases were significantly different among age groups (P < 0.001), shown in Table 4 and Supplementary Table 2. Again taking 2016 as an example, in the young age group, the rate of secondary hypertension caused by renal parenchymal disease still ranked first among all causes, reaching 67.19%; this far exceeded the rates in the other two groups (49.70% in the middle-aged group and 43.97% in the older group, P < 0.001). The rate of renal vascular disease in the young group was also higher than those in the other two groups. In contrast, the rate of OSAS was lower in the young group than those in the other two groups (16.41% in young patients, 33.42% in middle-aged patients, and 35.83% in older patients). In the middle-aged group, renal parenchymal diseases accounted for approximately 50% of all secondary hypertension causes. Endocrine hypertension, especially primary aldosteronism, showed the highest diagnosis rate in the middle-aged group. In the older group, renal parenchymal disease, OSAS, and primary aldosteronism remained the three leading causes. The proportion of OSAS in the older group was higher than those in the other two groups.
TABLE 4.
Rates of specific cause-related comorbidities in hospitalized patients with secondary hypertension in different age groups in 2016
| 18–40 years | 41–65 years | >65 years | P value | |
| Renal parenchymal disease [n (%)] | 18 319 (67.19) | 33 378 (49.70) | 10 432 (43.97) | <0.001 |
| Renal vascular disease [n (%)] | 983 (3.60) | 1783 (2.65) | 622 (2.62) | <0.001 |
| Endocrine hypertension [n (%)] | 1917 (7.03) | 6130 (9.12) | 1710 (7.20) | <0.001 |
| Cushing's syndrome [n (%)] | 421 (1.54) | 770 (1.14) | 158 (0.66) | <0.001 |
| Primary aldosteronism [n (%)] | 1342 (4.92) | 4844 (7.21) | 1378 (5.80) | <0.001 |
| Pheochromocytoma [n (%)] | 137 (0.50) | 491 (0.73) | 162 (0.68) | <0.001 |
| Diseases of aorta [n (%)] | 172 (0.63) | 641 (0.95) | 985 (4.15) | <0.001 |
| Obstructive sleep apnea syndrome [n (%)] | 4475 (16.41) | 22 445 (33.42) | 8501 (35.83) | <0.001 |
DISCUSSION
To the best of our knowledge, this is the most recent and largest national study to examine the causes of hospitalized patients with secondary hypertension and variation over time. This study is the first to establish trends in the rate of hospitalized patients with secondary hypertension from 2013 to 2016 in China. We found that the number of hypertensive inpatients with secondary hypertension increased during the target 4-year period. In addition, although cause-related diseases differed on the basis of age and sex, renal parenchymal disease and OSAS remained the leading two causes in China, with opposite trends by year.
The prevalence and composition ratio of various common diseases that cause secondary hypertension remain unknown. Renal parenchymal disease, one of the most common causes of secondary hypertension, has a prevalence of 1.6–8% in patients with hypertension, according to previous reports [10,12,13,22]. Similar single-center studies in China have shown that renal parenchymal hypertension accounts for approximately 3 and 8% of patients with hypertension and secondary hypertension, respectively [15,23]. The incidence of chronic kidney disease in China is high, and awareness is relatively poor [24]. As the risk of hypertension in patients with chronic kidney disease is close to 70% [25], the status of renal parenchymal disease as a cause of secondary hypertension in China must be taken seriously. According to the results of the present study, renal parenchymal disease reached a maximum of 59.58% in 2014, becoming the main cause of secondary hypertension among hospitalized patients in China. The constituent ratio began to decline after 2014, mainly owing to both the strengthening of prevention and treatment as well as screening for other causes.
OSAS, a cause of secondary hypertension reported in 2003 [26], has been a focus of attention because of its high morbidity and direct damage to target organs. Although the prevalence of OSAS varies widely according to previous investigations, it is persistently high, particularly among patients with resistant hypertension [8,27–29]. In a retrospective study conducted in 2007, OSAS accounted for 42.9% of all hospitalized patients with secondary hypertension in a Chinese hospital over 8 years [23]. As important evidence that can support and supplement this finding, the present study revealed that the diagnosis rate of OSAS was ranked second highest among hospitalized patients with secondary hypertension in China, and the absolute frequency and proportion of the disease increased from 2013 to 2016. Even if these findings are related to increased awareness of the disease and available detection methods, these data are valuable in clinical practice. The recent European guidelines for hypertension recommend routine examination using polysomnography to monitor OSAS in patients with resistant hypertension. For hypertensive patients who have corresponding systemic symptoms or hypertension that is difficult to control with medication, screening for this disease in a timely manner is important.
Primary aldosteronism was considered a rare disease a few decades ago. With continuous improvement in detection techniques, previous studies have shown that the prevalence of primary aldosteronism in patients with hypertension is approximately 5–10% [30,31]. A recent single-center study at Fuwai Hospital in China suggested that the diagnosis rate of primary aldosteronism among hypertensive patients was 5.2% whereas that of secondary hypertension was 16.8% [32]. In the present study, the diagnosis rate of primary aldosteronism among patients with secondary hypertension was 6.40% in 2016, making this the third leading cause of secondary hypertension and the leading cause of endocrine hypertension.
The proportions of secondary hypertension indicate specific characteristics among different age groups, on the basis of previous research. Our study found that the rate of renal parenchymal disease as a cause of secondary hypertension showed a downward trend with increased age and OSAS showed the opposite trend. Various researchers are in agreement that a principal cause of secondary hypertension among young adults in Western countries is renal parenchymal disease [5,33]. In contrast to past findings [34], in the present study, OSAS surpassed renal vascular disease as the second leading cause among young adults in China. Previous studies among patients with hypertension or resistant hypertension have shown that individuals with OSAS are significantly older than those without OSAS [8,29]. Our results showed that the rate of renal vascular disease in young patients was higher than that in the other two age groups; however, we could not further explore the causes owing to a lack of information. A single-center study from China analyzed the cause among 2047 patients with renal artery stenosis and found that patients under 40 years of age had the highest proportion of fibromuscular dysplasia, whereas those over 40 years of age had the highest proportion of atherosclerosis [35]. In middle-aged adults, OSAS, endocrine hypertension, and renal parenchymal disease predominate, similar to Western countries [5]. In older adults, it was worth noting that the results of previous studies suggest that the proportion of patients with hypertension and OSAS over 60 years of age is lower than this proportion among their counterparts aged 40–59 years [36]. However, the results of our study suggested that among Chinese patients with secondary hypertension over 65 years old, the combined rate of OSAS reached more than 30%, which requires greater attention in clinical screening.
The differences in causes by sex are also worth noting. Men showed a predominance of OSAS prevalence, similar to a previous study [8]. Women accounted for most cases of endocrine diseases, such as primary aldosteronism. Previous studies have not suggested significant sex differences among patients with primary aldosteronism [30,37]. However, studies on ion channel mutations in patients with aldosterone-producing adenoma, the most common cause of primary aldosteronism, have suggested that the proportion of KCNJ5 mutations in women was significantly higher than that in men [38]. These findings can provide guidance on the selection of screening methods for secondary hypertension among patients of different ages and sex.
Limitations
First, this was a retrospective study and the data were obtained from the front page of inpatients’ medical records. Owing to a lack of detailed data regarding patient examinations and treatment, we were unable to collect further information, such as causality, subtypes, severity, and outcomes. Second, we only included inpatients in tertiary hospitals, which may cause overestimation of the overall constituent ratio owing to both the purpose of diagnosis and improved examinations for related diseases. Third, we excluded some patients without a definite cause-related diagnosis, which may have impacts on the constituent ratio of secondary hypertension causes. However, this did not affect our main findings as the rates of both renal parenchymal disease and OSAS were much higher than this unclear rate.
In conclusion, our study provides important information on the changing trends in cause composition of secondary hypertension in China, on the basis of age and sex. Renal parenchymal disease remained the most common cause of secondary hypertension from 2013 to 2016, with a decreasing trend. This was followed by OSAS, which has become an important complicating disease in the cause of secondary hypertension. Screening for OSAS should be considered in patients with hypertension in China.
ACKNOWLEDGEMENTS
The authors would like to thank all members of the China Standard Medical Information Research Center for their help and support throughout the study.
Funding: This work was supported by the China-WHO Biennial Collaborative Projects 2016–2017 (2016/648722-0).
Conflicts of interest
There are no conflicts of interest.
Supplementary Material
Supplementary Material
Footnotes
Abbreviations: HQMS, Hospital Quality Monitoring System; ICD, International Classification of Diseases; OSAS, obstructive sleep apnea syndrome
Supplemental digital content is available for this article.
REFERENCES
- 1.Forouzanfar MH, Liu P, Roth GA, Ng M, Biryukov S, Marczak L, et al. Global burden of hypertension and systolic blood pressure of at least 110 to 115 mmHg, 1990–2015. JAMA 2017; 317:165–182. [DOI] [PubMed] [Google Scholar]
- 2.Olives C, Myerson R, Mokdad AH, Murray CJ, Lim SS. Prevalence, awareness, treatment, and control of hypertension in United States counties, 2001–2009. PLoS One 2013; 8:e60308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fang L, Song J, Ma Z, Zhang L, Jing C, Chen D. Prevalence and characteristics of hypertension in mainland Chinese adults over decades: a systematic review. J Hum Hypertens 2014; 28:649–656. [DOI] [PubMed] [Google Scholar]
- 4.Li Y, Yang L, Wang L, Zhang M, Huang Z, Deng Q, et al. Burden of hypertension in China: a nationally representative survey of 174,621 adults. Int J Cardiol 2017; 227:516–523. [DOI] [PubMed] [Google Scholar]
- 5.Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. the Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens 2018; 36:1953–2041. [DOI] [PubMed] [Google Scholar]
- 6.Rimoldi SF, Scherrer U, Messerli FH. Secondary arterial hypertension: when, who, and how to screen. Eur Heart J 2014; 35:1245–1254. [DOI] [PubMed] [Google Scholar]
- 7.Muiesan ML, Rizzoni D, Salvetti M, Porteri E, Monteduro C, Guelfi D, et al. Structural changes in small resistance arteries and left ventricular geometry in patients with primary and secondary hypertension. J Hypertens 2002; 20:1439–1444. [DOI] [PubMed] [Google Scholar]
- 8.Pedrosa RP, Drager LF, Gonzaga CC, Sousa MG, de Paula LK, Amaro AC, et al. Obstructive sleep apnea: the most common secondary cause of hypertension associated with resistant hypertension. Hypertension 2011; 58:811–817. [DOI] [PubMed] [Google Scholar]
- 9.Streeten DH, Anderson GH, Wagner S. Effect of age on response of secondary hypertension to specific treatment. Am J Hypertens 1990; 3(5 pt 1):360–365. [DOI] [PubMed] [Google Scholar]
- 10.Anderson GH, Blakeman N, Streeten DH. The effect of age on prevalence of secondary forms of hypertension in 4429 consecutively referred patients. J Hypertens 1994; 12:609–615. [DOI] [PubMed] [Google Scholar]
- 11.Kohara K. Clinical characteristic of secondary hypertension in the elderly. Nihon Rinsho 2005; 63:1091–1095. [PubMed] [Google Scholar]
- 12.Omura M, Saito J, Yamaguchi K, Kakuta Y, Nishikawa T. Prospective study on the prevalence of secondary hypertension among hypertensive patients visiting a general outpatient clinic in Japan. Hypertens Res 2004; 27:193–202. [DOI] [PubMed] [Google Scholar]
- 13.Börgel J, Springer S, Ghafoor J, Arndt D, Duchna HW, Barthel A, et al. Unrecognized secondary causes of hypertension in patients with hypertensive urgency/emergency: prevalence and co-prevalence. Clin Res Cardiol 2010; 99:499–506. [DOI] [PubMed] [Google Scholar]
- 14.Peng M, Jiang XJ, Dong H, Zou YB, Zhang HM, Song L, et al. Etiology of renal artery stenosis in 2047 patients: a single-center retrospective analysis during a 15-year period in China. J Hum Hypertens 2016; 30:124–128. [DOI] [PubMed] [Google Scholar]
- 15.Li NF, Lin L, Wang L, Wang XL, Zu FY, Zhang DL, et al. Etiology analysis for hospitalized hypertensive patients: 10 years report from the department of hypertension (1999–2008). Zhonghua Xin Xue Guan Bing Za Zhi 2010; 38:939–942. [PubMed] [Google Scholar]
- 16.Zhang L, Long J, Jiang W, Shi Y, He X, Zhou Z, et al. Trends in chronic kidney disease in China. N Engl J Med 2016; 375:905–906. [DOI] [PubMed] [Google Scholar]
- 17.Zhang L, Wang H, Long J, Shi Y, Bai K, Jiang W, et al. China Kidney Disease Network (CK-NET) 2014 Annual Data Report. Am J Kidney Dis 2017; 69: 6 suppl 2: A4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhang L, Wang H, Li Q, Zhao MH, Zhan QM. Big data and medical research in China. BMJ 2018; 360:j5910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Saran R, Steffick D, Bragg-Gresham J. The China Kidney Disease Network (CK-NET): ‘Big Data-Big Dreams’. Am J Kidney Dis 2017; 69:713–716. [DOI] [PubMed] [Google Scholar]
- 20.Li J, Cui Z, Long JY, Huang W, Wang JW, Wang H, et al. The frequency of ANCA-associated vasculitis in a national database of hospitalized patients in China. Arthritis Res Ther 2018; 20:226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chiong JR, Aronow WS, Khan IA, Nair CK, Vijayaraghavan K, Dart RA, et al. Secondary hypertension: current diagnosis and treatment. Int J Cardiol 2008; 124:6–21. [DOI] [PubMed] [Google Scholar]
- 22.Sinclair AM, Isles CG, Brown I, Cameron H, Murray GD, Robertson JW. Secondary hypertension in a blood pressure clinic. Arch Intern Med 1987; 147:1289–1293. [PubMed] [Google Scholar]
- 23.Li NF, Wang L, Zhou KM, Wang XL, Zu FY, Zhang DL, et al. Analysis of etiology of the patients with hypertension from the People's Hospital of Xinjiang Uygur Autonomous Region. Zhonghua Xin Xue Guan Bing Za Zhi 2007; 35:865–868. [PubMed] [Google Scholar]
- 24.Zhang L, Wang F, Wang L, Wang W, Liu B, Liu J, et al. Prevalence of chronic kidney disease in China: a cross-sectional survey. Lancet 2012; 379:815–822. [DOI] [PubMed] [Google Scholar]
- 25.Franklin SS, Jacobs MJ, Wong ND, L’Italien GJ, Lapuerta P. Predominance of isolated systolic hypertension among middle-aged and elderly US hypertensives: analysis based on National Health and Nutrition Examination Survey (NHANES) III. Hypertension 2001; 37:869–874. [DOI] [PubMed] [Google Scholar]
- 26.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, et al. National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure, National High Blood Pressure Education Program Coordinating Committee. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA 2003; 289:2560–2572. [DOI] [PubMed] [Google Scholar]
- 27.Sjöström C, Lindberg E, Elmasry A, Hägg A, Svärdsudd K, Janson C. Prevalence of sleep apnoea and snoring in hypertensive men: a population based study. Thorax 2002; 57:602–607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Logan AG, Perlikowski SM, Mente A, Tisler A, Tkacova R, Niroumand M, et al. High prevalence of unrecognized sleep apnoea in drug-resistant hypertension. J Hypertens 2001; 19:2271–2277. [DOI] [PubMed] [Google Scholar]
- 29.Drager LF, Genta PR, Pedrosa RP, Nerbass FB, Gonzaga CC, Krieger EM, Lorenzi-Filho G. Characteristics and predictors of obstructive sleep apnea in patients with systemic hypertension. Am J Cardiol 2010; 105:1135–1139. [DOI] [PubMed] [Google Scholar]
- 30.Douma S, Petidis K, Doumas M, Papaefthimiou P, Triantafyllou A, Kartali N, et al. Prevalence of primary hyperaldosteronism in resistant hypertension: a retrospective observational study. Lancet 2008; 371:1921–1926. [DOI] [PubMed] [Google Scholar]
- 31.Funder JW, Carey RM, Mantero F, Murad MH, Reincke M, Shibata H, et al. The management of primary aldosteronism: case detection, diagnosis, and treatment: an Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab 2016; 101:1889–1916. [DOI] [PubMed] [Google Scholar]
- 32.Liu XN, Cai J, Ma WJ, Zhou XL, Song L, Zhang HM, et al. Analysis of clinical features of hypertensive patients with primary aldosteronism. Chinese Circ J 2018; 33:836–841. (in Chinese). [Google Scholar]
- 33.Viera AJ, Neutze DM. Diagnosis of secondary hypertension: an age-based approach. Am Fam Physician 2010; 82:1471–1478. [PubMed] [Google Scholar]
- 34.Peng M, Jiang X-j, Dong H, Zou Y-b, Zhang H-m, Song L, et al. Etiology of renal artery stenosis in 2047 patients: a single-center retrospective analysis during a 15-year period in China. J Hum Hypertens 2016; 30:124–128. [DOI] [PubMed] [Google Scholar]
- 35.Charles L, Triscott J, Dobbs B. Secondary hypertension: discovering the underlying cause. Am Fam Physician 2017; 96:453–461. [PubMed] [Google Scholar]
- 36.Haas DC, Foster GL, Nieto FJ, Redline S, Resnick HE, Robbins JA, et al. Age-dependent associations between sleep-disordered breathing and hypertension: importance of discriminating between systolic/diastolic hypertension and isolated systolic hypertension in the Sleep Heart Health Study. Circulation 2005; 111:614–621. [DOI] [PubMed] [Google Scholar]
- 37.Monticone S, Burrello J, Tizzani D, Bertello C, Viola A, Buffolo F, et al. Prevalence and clinical manifestations of primary aldosteronism encountered in primary care practice. J Am Coll Cardiol 2017; 69:1811–1820. [DOI] [PubMed] [Google Scholar]
- 38.Åkerström T, Crona J, Delgado Verdugo A, Starker LF, Cupisti K, Willenberg HS, et al. Comprehensive re-sequencing of adrenal aldosterone producing lesions reveal three somatic mutations near the KCNJ5 potassium channel selectivity filter. PLoS One 2012; 7:e41926. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.