Health disparities result from distinct but intertwined exposures and social determinants. Work is a critical factor, reflecting and influencing other key health determinants, including socioeconomic status, access to health care, stress, and hazardous exposures. However, the important impact of work has been largely neglected in health disparities research and practice,1 , 2 which is a critical deficit given the potential for workplace exposures and conditions to amplify health disparities. Further, as work and workplace hazards are modifiable, with recognition and understanding there is tremendous opportunity to intervene and thereby promote health equity.1
SARS-CoV-2, an exposure under national and global surveillance and an added workplace hazard, has brought new attention to workplace safety and the complex interactions between work, other determinants of health, and access to medical care. COVID-19 has proved, in part, to be an occupational disease.3 In addition to health care workers, workers at higher risk of exposure have largely included those who (1) are unable to work from home; (2) lack proper personal protective measures; (3) work in shared, densely populated spaces with insufficient environmental controls; and/or (4) commute via shared and/or crowded transit.3 Outbreaks of COVID-19 have occurred in a wide range of industries, including but not limited to cleaning/domestic work, food production, restaurant/hospitality, transportation, public safety, construction, and agricultural work.4 Many of these occupations are lower-income occupations that are disproportionately occupied by ethnic/racial minorities5 (including immigrants) who may also experience worse health outcomes related to reduced access to health care; fear of reprisal or income loss, delaying presentation to care; and language or cultural barriers. These same factors increase susceptibility to other chronic medical diseases and predispose individuals working in the aforesaid occupations to severe, acute COVID-19. Indeed, these vulnerable populations have disproportionate rates of COVID-19 infection and mortality.6
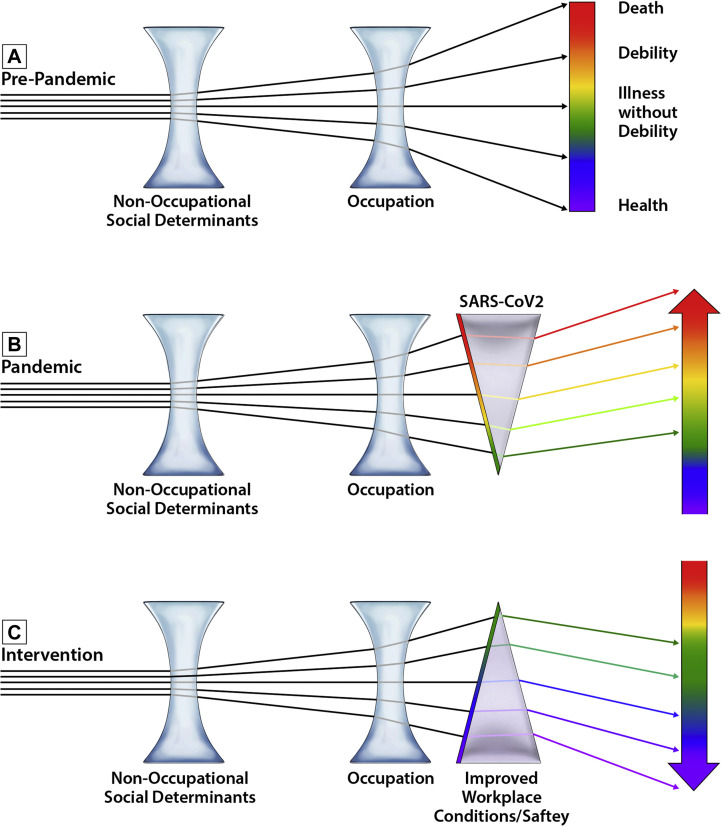
Although the COVID-19 pandemic brought heightened attention to occupational disparities (Fig 1 , A and B), work conditions that contribute to outbreaks, illness, and injury have long been present and linked to health inequity.7 In the United States, which is the focus of this article, understanding the true breadth and burden of work-related illness is limited by reporting systems and available data. Employers are required to report work-related injury or illness events meeting Occupational Safety and Health Administration (OSHA) reporting thresholds, which are almost exclusively work-related injuries and fatalities.1 Although health care providers routinely obtain information about risk factors such as smoking and family history, work is infrequently queried or documented. Thus, medical records rarely contain information about work, and other sources of occupational data are very limited. The National Institute for Occupational Safety and Health oversees several occupational health surveillance programs and data sources to monitor work-related illnesses and injuries and identify modifiable risk factors for intervention. At present, such efforts are underresourced, and broader support for a national, concerted effort is an urgent need. Although frameworks for broader recognition and data collection have been proposed,1 national education and infrastructure for requisite assessment and documentation necessitate greater support.
Fig 1.
Worker health as a modifiable spectrum. A, Nonoccupational factors (including age, race/ethnicity, sex, education, health care access) are associated with disparities in health outcomes. Occupation is related to these factors, but it may also independently affect and further expand the spectrum of outcomes through exposure and income disparities. B, Onset of the COVID-19 pandemic compounded preexisting workplace hazards, shifting the spectrum of outcomes to harm in the absence of compensatory worker protections. C, Shifting the spectrum away from poor outcomes in worker health requires population-level interventions that reduce health disparities and improve workplace conditions and protections. The schematic is intentionally simplistic for conceptual representation, with the greater complexity underlying occupational health disparities noted in this article's text and referenced works.
Workplace interventions, if effective, have the potential to not only prevent work-related illness and injury but also dramatically reduce health disparities and shift the spectrum of health outcomes toward wellness (Fig 1, C). Enforceable standards are the government’s most effective tool for protecting vulnerable workers.8 More than a year after the first cases of COVID-19 were detected in the United States, OSHA has released a rule mandating protections against COVID-19 for health care workers, but not for other high-risk and frontline workers.9 In addition to further practical standards to protect employee health, parallel interdisciplinary research is critical to assess feasibility and impact on employment and industry alongside work-related injury, illness, and health disparities.
Given the limitations of developing and implementing enforceable standards, health care professionals can play a key role in supporting the occupational health and safety of individual, at-risk patients and help identify sentinel cases of work-related illness. Unfortunately, work-related illnesses are vastly underdiagnosed10 for multiple reasons, including similarity to non–work-related disease, lack of information on exposure, and also clinicians’ inexperience or discomfort in addressing occupational health. To establish work-relatedness, workers’ compensation systems in the United States, although quite variable depending on state laws, are based on a standard of it being “more probable than not” (>50% likelihood) that hazards in the workplace were a contributing factor to the onset or worsening of the patient’s condition. Once work-relatedness is established, workers’ compensation provides employer-funded medical insurance for the work-related condition, delivering compensation for lost work time but simultaneously creating separate occupational health care delivery systems that may be suboptimal (eg, restricting provider options). As an example, consider a poultry plant worker with COVID-19 who lives alone and worked in close contact with coworkers who also had COVID-19. Although it is possible that this patient acquired SARS-CoV-2 elsewhere, it is more probable than not that the infection was acquired at the workplace. A diagnosis of work-related COVID-19 provides the worker with some paid sick time and health insurance coverage for the work-related condition, which is especially a concern if this worker is unable to return to his or her prior employment on account of the work-related condition and thus could be at risk of also losing employer-based health insurance, thereby further widening disparities.
Once an injury or illness is suspected to be work-related, or ideally once a hazardous work environment is recognized before the onset of injury or illness, clinicians can take several actions to help reduce hazards and improve outcomes. These include clinician documentation of the following items in the medical record: the employer, job tasks, work conditions, potential exposures, and work-related symptoms. Clinicians can also encourage patients to talk with their employers directly, work with their union representative, anonymously request a workplace evaluation from OSHA or with coworkers, and request a health hazard evaluation from the National Institute for Occupational Safety and Health. With patient permission, clinicians can also contact employers to obtain additional information about work exposures and can advocate to reduce workplace hazards. Although workplace interventions that reduce or eliminate exposures are preferred, personal protective equipment and job transfers and/or restrictions can be effective at reducing an individual worker’s exposures. Caution is warranted to avoid overly restrictive recommendations that might result in job loss, as well as underrestriction, which may enable ongoing harmful exposure. Referral to an occupational health specialist, if available, is recommended, not only to address the complexity of exposure and causality but also to address and/or assist with issues related to work, such as work accommodations or workers' compensation.
Worker health and health disparities are not only national concerns but also worldwide concerns. The COVID-19 pandemic has underscored the fact that workers in the United States and across the globe continue to face preventable occupational hazards. Work-related COVID-19 outbreaks highlight the need for immediate action to address not only pandemic-related hazards but all workplace hazards. Improved occupational health surveillance, data sources, and research funding are also needed to better understand the impact of work and the interactions between work and other health disparities, as well as to inform effective interventions. Enforceable health and safety standards, greater resources to facilitate compliance, mandatory reporting of work-related conditions, improved workers’ compensation insurance systems and delivery of care, and more flexible work accommodations are key to a comprehensive worker health and safety approach. Social responsibility demands protection of the health of the workforce—for the global economy and for the health of individuals sustaining it. COVID-19 has floodlit disparities and deficiencies in workplace protections. This heightened visibility presents opportunity to mobilize support, improve worker health, and reduce health inequities.
Footnotes
Disclosure of potential conflict of interest: The authors declare that they have no relevant conflicts of interest.
References
- 1.Ahonen E.Q., Fujishiro K., Cunningham T., Flynn M. Work as an inclusive part of population health inequities research and prevention. Am J Public Health. 2018;108:306–311. doi: 10.2105/AJPH.2017.304214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Landsbergis P.A., Choi B., Dobson M., Sembajwe G., Slatin C., Delp L. The key role of work in population health inequities. Am J Public Health. 2018;108:296–297. doi: 10.2105/AJPH.2017.304288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Carlsten C., Gulati M., Hines S., Rose C., Scott K., Tarlo S.M. COVID-19 as an occupational disease. Am J Ind Med. 2021;64:227–237. doi: 10.1002/ajim.23222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization Preventing and mitigating COVID-19 at work. https://www.who.int/publications-detail-redirect/WHO-2019-nCoV-workplace-actions-policy-brief-2021-1 Available at:
- 5.Bureau of Labor Statistics Current Population Survey: employed persons by detailed industry, sex, race, and Hispanic or Latino ethnicity. https://www.bls.gov/cps/cpsaat11.htm https://www.bls.gov/cps/cpsaat11.htm Available at:
- 6.Liao T.F., De Maio F. Association of social and economic inequality with coronavirus disease 2019 incidence and mortality across US counties. JAMA Netw Open. 2021;4 doi: 10.1001/jamanetworkopen.2020.34578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Landsbergis P.A. Assessing the contribution of working conditions to socioeconomic disparities in health: a commentary. Am J Ind Med. 2010;53:95–103. doi: 10.1002/ajim.20766. [DOI] [PubMed] [Google Scholar]
- 8.Michaels D., Wagner G.R. Occupational Safety and Health Administration (OSHA) and worker safety during the COVID-19 pandemic. JAMA. 2020;324:1389–1390. doi: 10.1001/jama.2020.16343. [DOI] [PubMed] [Google Scholar]
- 9.Occupational Safety and Health Administration Subpart U — COVID-19 Emergency Temporary Standard. https://www.osha.gov/sites/default/files/covid-19-healthcare-ets-reg-text.pdf Available at:
- 10.Mazurek J.M., White G.E., Moorman J.E., Storey E. Patient-physician communication about work-related asthma: what we do and do not know. Ann Allergy Asthma Immunol. 2015;114:97–102. doi: 10.1016/j.anai.2014.10.022. [DOI] [PMC free article] [PubMed] [Google Scholar]