Abstract
Background
Surgical (SM) or cloth facemasks (CM) has become mandatory in many public spaces during the COVID-19 pandemic. They may interfere with the participation in physical activities.
Objective
To evaluate how these masks influence dyspnoea (primary outcome), exercise performance and cardiorespiratory response during a 1-min sit-to-stand test (1STST), and to assess masks discomfort sensations.
Methods
A randomized crossover trial was conducted in healthy adults. They performed 3 1STST (with either no mask (NM), a SM, or a CM) separated from each other by 24–72 h. The number of 1STST repetitions and leg rate of perceived exertion (RPE) were measured. Dyspnoea (Borg scale), hearth rate, respiratory rate and SpO2 were recorded before and at the end of 1STST, as well as after a short resting period. Several domains of subjective discomfort perceptions with masks were assessed.
Results
Twenty adults aged 22 ± 2y (11 males) were recruited. Wearing the CM generated significantly higher dyspnoea than NM at all time points, but it only became clinically relevant after the 1STST (median difference, 1 [95%CI 0 to 1]). The SM generated a small but significant higher leg RPE than NM (median difference, 1 [95%CI 0 to 1]). The masks had no impact on 1STST performance nor cardiorespiratory parameters. Both masks were rated similarly for discomfort perceptions except for breathing resistance where CM was rated higher.
Conclusions
In healthy adults, the CM and SM had minimal to no impact on dyspnoea, cardiorespiratory parameters, and exercise performance during a short submaximal exercise test.
Keywords: Surgical mask, Cloth mask, COVID-19, 1-Min sit-to-stand test, Exercise capacity
1. Introduction
The 31st of December 2019, the World Health Organization (WHO) was alerted by several cases of pneumonia emerging from Wuhan (China) from unknown cause. The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was quickly identified as the culprit, causing the coronavirus disease 2019 (COVID-19). Since then, the disease spread rapidly worldwide and evolved into an unprecedented pandemic. To reduce viral transmission among people, different measures were instituted by local health authorities such as lockdown, hand disinfection, physical distancing and personal protective equipment including facemasks.
In a lot of countries, wearing a facemask became widely recommended or even mandatory, particularly during activities in crowded public spaces [1,2] to block emitted respiratory droplets and mitigate person-to-person transmission of SARS-CoV-2 [3,4]. Indeed, virus particles in respiratory droplets can be transmitted during quiet breathing or speaking [[4], [5], [6], [7]], and may be accentuated with increased ventilation like during physical activity, including those of daily living. Among the general community, different types of facemask were observed depending on the situation even if disposable surgical and non-disposable cloth facemasks were the most frequently worn during activities of the daily living [2,8].
Wearing a facemask while performing activities of daily living or during outdoor physical activities quickly appeared to be difficulty tolerated in some people. Medical exemptions to the compulsory use of facemasks have even been applied to respiratory patients in some countries, although such exemption was not evidence-based [9]. However, studies reported that facemask was associated with discomfort and respiratory difficulties [10,11]. Recently, the WHO advises against the wearing of masks during vigorous physical activities because they may reduce the ability to breathe comfortably [12]. There are also concerns that the masks increase breathing resistance and carbon dioxide rebreathing and reduce oxygen uptake during exercising [13]. However, previous studies have shown no physiological impact from wearing a surgical facemask or even a N95 filtering facepiece respirator in healthy subjects exercising on a treadmill for 1 h at low-to-moderate work rate [14,15].
Therefore, the purpose of our study was to evaluate whether dyspnoea sensation, performance, and cardiorespiratory response are altered during a submaximal field test, the 1-min sit-to-stand test (1STST), when wearing masks used in the general community. Our hypothesis was that the resistance of a cloth and surgical facemasks increases the discomfort without impact on physiological parameters.
2. Material and methods
2.1. Participants
Participants were recruited on voluntary basis within the medical staff of the physiotherapy unit from Cliniques universitaires Saint-Luc (Brussels, Belgium) from October to December 2020. The recruitment was performed on simple oral request. As unique inclusion criterion, the subjects had to be aged between 18 and 30 years old. Exclusion criteria were a diagnosis of chronic disease, musculoskeletal disorders, lower-limb muscle soreness, or obesity determined by a body mass index higher than 30 kg/m2. In addition, eligible subjects had to avoid unordinary physical exercise or high alcohol consumption the day before each test. The study was approved by the local Ethics Committee (B4032020000121) and all participants provided written consent before inclusion.
2.2. Study design
We conducted a prospective randomized crossover trial following the CONSORT statement. Each subject performed three 1STST separated from each other by 24–72 h without any mask (no mask - NM), with a surgical mask (SM), or with a cloth mask (CM). The order of these tests was randomly assigned using the website randomizer.org. The subjects were familiarized with the 1STST procedure by performing a training test at least 24 h before the randomization to account for the learning effect [16].
2.3. 1-Min sit-to-stand test
The 1STST was performed with a standard chair without armrests (height = 46 cm). Hands on the hips, participants had to completely stand up and sit down as many times as possible for 1 min. No encouragements were provided during the test. Subjects were told that rest periods were permitted during the test, with no interruption of the countdown timer. Standardized instructions were given to all participants before the procedure.
2.4. Masks
The SM were a standard 3 ply disposable facemask CE-marked that complied with the European standard EN 14683:2019 + AC:2019, Type II (BruMed, Kontich, Belgium).
The CM were 3-layer ear-loop handmade masks. The outer and middle layers were composed of cotton, the inner layer was made of polyester fabric. The CM conformed to the local Federal Public Health Service template and to the Belgian technical document (NBN/DTD S 65–001:2020). Two models made with the same materials were used repeatedly, and they were washed at 60 °C using a washing machine and completely dried before reusing them for the next subject. Their differential pressure (breathability) was measured (online supplement).
The masks were tightly fitted around the face of each participant using an adjustable plastic mask strap extender.
2.5. Outcomes
The following demographic data were collected the day of the familiarization 1STST: age, gender, height, weight, lower limb length, and smoking status. Participants also performed spirometry the same day using the SpiroScout (Ganshorn, Schiller Group, Germany) according to the American Thoracic Society/European Respiratory Society guidelines [17,18]. Forced vital capacity (FVC), forced expiratory volume in 1 s (FEV1), forced expiratory flow between 25 and 75% of FVC were reported and expressed in percentage of predictive values and z-scores using appropriate reference equations [19]. Finally, all participants filled out the Global Physical Activity Questionnaire (GPAQ), the Multidimensional Fatigue Inventory (MFI-20) and the Nijmegen questionnaire.
The GPAQ comprises 16 questions and collects information on physical activity participation in three domains (activity at work, travel to and from places, and recreational activities) as well as sedentary behaviour [20]. Results were expressed in metabolic equivalents (METs) and as a proportion of participants that were sufficiently active or not according to World Health Organization recommendations [21]. The MFI-20 consists of 20 items assessing fatigue into five subscales: general fatigue, physical fatigue, reduced motivation, reduced activity and mental fatigue. Each subscale ranges from 4 to 20 points. The higher the score, the higher the fatigue [22,23]. The Nijmegen questionnaire includes 16 questions scored each from 0 to 4. A total score ≥23 out of 64 suggests hyperventilation syndrome [24].
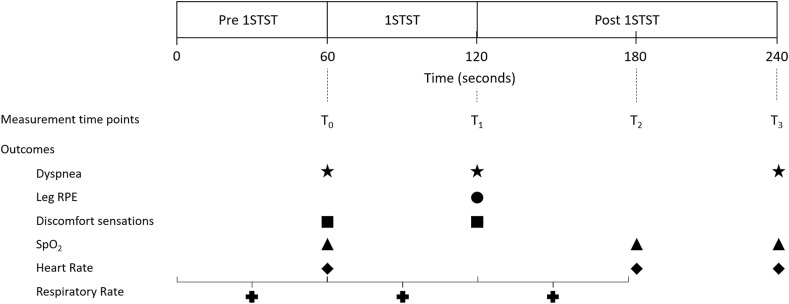
During the 1STSTs, the parameters were recorded at several time points over a 4-min long period (Fig. 1 ). These time points were defined as follows: immediately before the start of 1STST (T0), immediately after the test (T1), and at 60- and 120-s post effort (T2 and T3, respectively). Subjects were asked to rate dyspnoea according to the Borg CR10 scale [25] at T0 (immediate effect of wearing a mask), T1 and T3. The primary outcome was dyspnoea at T1. The rate of perceived exertion for leg (RPE) was also assessed at T1 [25].
Fig. 1.
Measurement time points and outcome measures during the 1-min sit-to-stand tests.
The number of 1STST repetitions were recorded and expressed in absolute and in percentage of predicted values according to reference data from Stassmann et al. [26]. Heart rate (HR) and pulsed oxygen saturation (SpO2) were recorded with a finger pulse oximeter (Somnolter, Nomics, Belgium) and analysed offline using the APIOS software (Nomics, Belgium). The HR and SpO2 values at specific timing were reported: immediately before the start of 1STST (T0) and at T2 & T3. Respiratory rate (RR) was registered continuously over 3 min using 2 respiratory inductive plethysmography belts (one thoracic and one abdominal) (Somnolter, Nomics, Belgium) and retrieved offline with APIOS. The RR was reported over 1-min before, 1-min during and 1-min after each effort (Fig. 1).
Five domains of comfort/discomfort of wearing a mask were assessed at T0 and T1 using scales published in another study and ranging from 0 (no discomfort at all) to 10 (maximal discomfort) [27]. The evaluated domains were humidity, heat, breathing resistance, fatigue, and overall discomfort.
2.6. Statistical analyses
The sample size was calculated based on an estimated difference (±SD) of 1 ± 1.3 point in dyspnoea between two of the three conditions (NM, SM and CM) [28]. We estimated that 20 participants had to be recruited in this crossover trial to reach a power of 80% with an alpha risk of 0.016 to account for Bonferroni correction for post-hoc comparisons. Data was analysed using SPSS 25.0 (IBM software). Normality of data were verified with the Shapiro-Wilk test. Descriptive analysis was performed for baseline parameters. All data were presented as mean (±SD) or median (interquartile range) according to their distribution. Comparison of STST variables between the 3 conditions were tested with repeated measures ANOVA or Friedman test as appropriate. To assess how each condition influenced and affected the cardiorespiratory parameters (RR, HR, SpO2) and subjective discomfort scores over the different time points, we performed 2-way repeated measures ANOVA with time and condition as within-subject factors. If assumptions to run the latter test were not respected, a Friedman test on difference between time points was realized. The Bonferroni correction was applied for any post-hoc comparisons. Correlations were tested using Pearson's correlation coefficient. A p value ≤ 0.05 was considered as statistically significant.
3. Results
3.1. Demographics
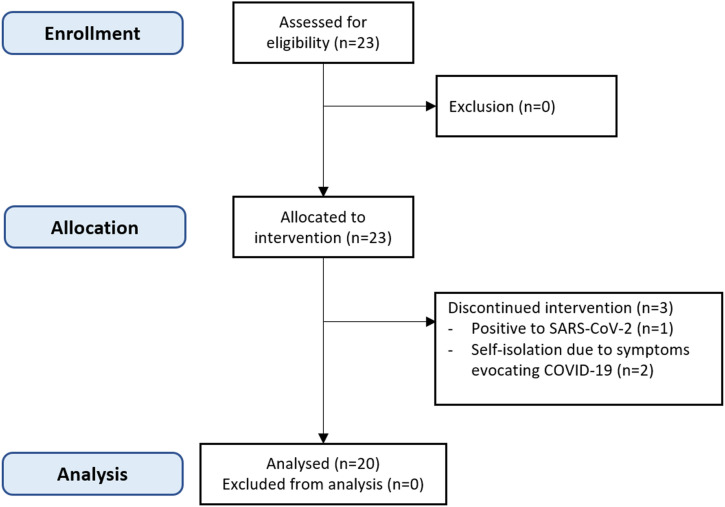
Twenty-three healthy young volunteers had to be recruited in this study. Three of them could not complete the entire experimentation due to SARS-CoV-2 infection (n = 1) or self-isolation due to symptoms suggestive of COVID-19 (n = 2). Therefore, 20 healthy participants completed the experiments (Fig. 2 ). Demographic data and baseline characteristics of these participants are displayed in Table 1 .
Fig. 2.
Study flowchart.
Table 1.
Demographics and baseline characteristics.
| Variables | n = 20 |
|---|---|
| Age, years | 22 ± 1.6 |
| Sex, n (%) | |
| Males | 11 (55) |
| Females | 9 (45) |
| BMI, kg/m2 | 22.1 ± 2.8 |
| GPAQ | |
| Score (MET-minutes/week) | 7246.4 ± 3479.4 |
| Meeting WHO recommendations, n (%) | 20 (100) |
| Nijmegen score | 8.3 ± 6.1, range [[1], [2], [3], [4], [5], [6], [7], [8], [9], [10], [11], [12], [13], [14], [15], [16], [17], [18], [19], [20], [21], [22]] |
| MFI-20 score | |
| General Fatigue | 8.9 ± 2.7 |
| Physical Fatigue | 10.6 ± 1.8 |
| Reduced Activity | 8.6 ± 2.5 |
| Reduced Motivation | 8.2 ± 2.8 |
| Mental Fatigue | 6.8 ± 2.0 |
| Pulmonary function | |
| FEV1, % predicted | 94.01 ± 12.01 |
| FEV1, z-score | −0.47 ± 1.12 |
| FVC, % predicted | 99.48 ± 10.39 |
| FVC, z-score | 0 ± 0.99 |
| FEV1/FVC, % | 80.9 ± 7.7 |
| FEV1/FVC, z-score | −0.72 ± 1.11 |
| FEF25-75, % predicted | 91.35 ± 29.01 |
| FEF25-75, z-score | −0.47 ± 1.34 |
| 1STST (familiarization test) | |
| Number of repetitions | 49.7 ± 10.1 |
| Predicted values (%) | 98 ± 15 |
Data are presented as n (%) or mean ± SD, unless otherwise stated.
1STST – 1-min sit-to-stand test; BMI - body mass index; FEV1 - forced expiratory volume in 1 s; FEF25–75 - forced expiratory flow between 25% and 75% of forced vital capacity; FVC – forced vital capacity; GPAQ – global physical activity questionnaire; MFI-20 – Multidimensional fatigue inventory with 20 items.
3.2. Effects of facemasks on dyspnoea, perceived exercise, and performance
There were significant differences in dyspnoea sensation at T0, T1 and T3 between the three conditions (Table 2 ). Post-hoc analysis revealed that the CM generated significantly higher but not clinically relevant dyspnoea than NM at T0 (median difference, 0 [95%CI 0 to 1]). The difference became clinically relevant at T1 and T3 (median difference, 1 [95%CI 0 to 1]). A similar, although clinically irrelevant difference was also noted between SM and CM at T3 (median difference, 0.5 [95%CI 0 to 1]). There was a significant difference in leg RPE post-effort between the 3 conditions. The SM generated a small but significant higher leg RPE than NM (median difference, 1 [95%CI 0 to 1]). There was no difference in 1STST performance between the 3 conditions (Table 2).
Table 2.
Effects of each condition on outcome measures.
| NM |
SM |
CM |
P value |
Adjusted P value |
|||
|---|---|---|---|---|---|---|---|
| NM vs SM | NM vs CM | SM vs CM | |||||
| Dyspnoea | |||||||
| T0 | 0 [0; 0] | 0 [0; 0.75] | 0 [0; 1] | 0.012a | 0.076 | 0.042 | 0.618 |
| T1 | 3 [1.25; 4] | 3 [2; 4] | 3 [2.5; 4] | 0.004a | 0.076 | 0.007 | 0.855 |
| T3 | 1 [0; 2] | 2 [1; 2] | 2 [1.25; 3] | < 0.001a | 0.100 | 0.004 | 0.005 |
| Leg RPE | 2.5 [1.25; 3] | 3 [2; 4] | 3 [2; 4] | 0.012a | 0.014 | 0.117 | 0.999 |
| 1STST repetitions (n) | 58.5 (9.9) | 58.6 (9.3) | 58.4 (9.3) | 0.986b | |||
Data are presented as mean ± SD or median [interquartile range].
Abbreviations: CM, cloth facemask; NM, no facemask; RPE, rate of perceived exertion; SM, surgical facemask; 1STST, 1-min sit-to-stand test.
Friedman test was realized.
ANOVArm was realized.
3.3. Effects of facemasks on cardio-respiratory parameters
The influence of time and facemasks, and their interaction on cardio-respiratory parameters are summarized in Table 3 . Only time influenced the cardio-respiratory parameters. The facemasks had no effect on any of these parameters and did not interact with them over time.
Table 3.
Cardiorespiratory parameters among each condition and at different time points.
| p-value |
||||||
|---|---|---|---|---|---|---|
| Cardiorespiratory parameters | NM | SM | CM | Time | Mask | Time x Mask |
| RR (bpm) | ||||||
| 1-min Pre 1STST | 20.9 ± 4.5 | 21.9 ± 7.8 | 21.1 ± 4.6 | < 0.001 | 0.31 | 0.56 |
| 1-min 1STST | 47.9 ± 11.1 | 50.1 ± 8.0 | 51.2 ± 11.2 | |||
| 1-min Post 1STST | 23.0 ± 5.2 | 23.4 ± 6.8 | 23.0 ± 5.7 | |||
| SpO2(%) | ||||||
| T0 | 98 [98–98] | 98 [98–98] | 98 [98–98] | 0.97a | NA | NA |
| T2 | 98 [97–98] | 98 [97–98] | 97 [97–98] | |||
| T3 | 98 [97–98] | 98 [97–98] | 98 [97–98] | |||
| HR (bpm) | ||||||
| T0 | 78.7 ± 13.4 | 78.3 ± 12.3 | 75.6 ± 12.2 | < 0.001 | 0.51 | 0.87 |
| T2 | 103.7 ± 16.5 | 103.3 ± 15.6 | 100.4 ± 13.7 | |||
| T3 |
92.7 ± 15.2 |
92.3 ± 15.6 |
91.2 ± 16.1 |
|||
| Subjective sensations |
||||||
| Humidity | ||||||
| T0 | 2.6 ± 1.9 | 2.3 ± 1.7 | < 0.001 | 0.94 | 0.23 | |
| T1 | 4.1 ± 1.5 | 4.3 ± 1.7 | ||||
| Heat | ||||||
| T0 | 3.1 ± 1.8 | 3.2 ± 2.1 | < 0.001 | 0.52 | 0.63 | |
| T1 | 4.6 ± 1.6 | 4.9 ± 2.3 | ||||
| Resistance | ||||||
| T0 | 1.8 ± 1.5 | 2.5 ± 1.6 | < 0.001 | 0.04 | 0.63 | |
| T1 | 3.1 ± 1.6 | 3.9 ± 1.9 | ||||
| Fatigue | ||||||
| T0 | 1.7 ± 1.4 | 1.8 ± 1.9 | < 0.001 | 0.42 | 0.54 | |
| T1 | 3.6 ± 1.8 | 4.2 ± 2.5 | ||||
| Overall discomfort | ||||||
| T0 | 2.8 ± 1.9 | 2.9 ± 1.6 | < 0.001 | 0.98 | 0.89 | |
| T1 | 4.2 ± 2.5 | 4.2 ± 2.1 | ||||
Data are presented as mean ± SD or median [interquartile range].
Abbreviations: bpm; breathes or beats per minute; CM, cloth facemask; HR, hearth rate; NM, no facemask; RR, respiratory rate; SM, surgical facemask; SpO2, pulsed oxygen saturation.
Default statistical analysis were two-way repeated measures ANOVA in this table.
Indicates that the Friedman test was realized because of violation of assumptions to run a two-way repeated measures ANOVA.
3.4. Mask discomfort sensations
The influence of time and facemasks, and their interaction on subjective ratings of discomfort domains are summarized in Table 3. As shown in this table, the effort (time) influenced the perception of all the evaluated discomfort domains. On the other hand, sensations were not significantly influenced by the type of masks except for the breathing resistance domain where the CM generated higher discomfort than SM. There was no interaction between time and facemasks, meaning that the type of mask did not influence the change of the sensations.
3.5. Learning effect and correlations with baseline characteristics
There was an important 1STST learning effect between the familiarization test and the NM condition (mean difference 8.8 ± 8.7 repetitions, p < 0.001) (E-Fig. 1). No correlation was found between baseline characteristics (spirometry and questionnaires scores) and the intensity of dyspnoea nor the 1STST performance in any conditions (p > 0.05).
4. Discussion
The main finding of the present study is that the cloth facemask slightly increases dyspnoea sensation in young healthy adults after a short submaximal exercise test. In addition, the surgical facemask had a small effect on the rate of perceived exercise. However, none of the two facemasks used in the general community altered exercise performance or the cardiorespiratory response to effort.
Several studies have demonstrated that facemasks increase the cardio-respiratory stress and elevate perceived exertion during mild to moderate exercise in healthy subject or in patients with COPD [[29], [30], [31], [32]]. Moreover, the protection masks are associated with a significant worsening of FEV1 and FVC due to an increase in airflow resistance, which can impact the perceived exertion for a similar effort [33]. The most significant impacts have been associated with the use of N95 respirators [29,30,34]. Yet, surgical facemasks have also shown to impact these parameters while exercising [14,31,33,34]. Similar to our study, Person et al. have shown that wearing a surgical facemask had no impact on heart rate, SpO2, or walking distance during a 6-min walk test (6MWT) in healthy adults [28]. However, these authors found a significant and clinically relevant impact on dyspnoea, contrarily to our findings with the surgical facemask. Nonetheless, it should be noted that the cardiorespiratory demand is higher with the 6MWT compared to the 1STST [35,36]. The 1STST effort intensity may thus not have been sufficiently high to elicit an increase in dyspnoea sensation compared to NM in our cohort of young healthy adults. In line with this, Mapelli et al. have shown that the increased sensation of dyspnoea with protection masks became progressively apparent at higher exercise intensity [33]. This could explain the small impact on leg RPE we found using facemasks during an exercise of relatively mild intensity. Whether these results also apply in elderly participants or patients with respiratory disease is unknown.
Unlike the SM, the use of a handmade CM was associated with a significant increase in dyspnoea compared to the control condition. Dyspnoea is defined as “a subjective experience of breathing discomfort that consists of qualitatively distinct sensations that vary in intensity” [37]. Therefore, the higher breathing resistance with the CM compared to the SM (online supplement) may have contributed to increase the dyspnoea level at the clinically relevant threshold. It should be noted that the difference became clinically relevant only after the 1STST. This may reflect the greater airflow resistance associated with higher ventilation [38]. At the end of the effort and during the recovery period, the breathing resistance may thus have reached a point susceptible to be perceived by participants.
Another possible hypothesis is that the CM could have increased facial skin temperature and heat or moisture of the inhaled air. Such factors have been postulated to contribute to increased breathing discomfort when wearing a facemask [14,39]. Although we did not objectively assess inhaled temperature and humidity, these sensations were subjectively felt by participants wearing a mask, especially at the end of effort and irrespective of the type of mask. Alone, the facial microclimate changes due to exhaled breath and facial sweat accumulation [39] seem insufficient to amplify dyspnoea. Combined with a higher breathing resistance, however, these sensations could exaggerate breathing difficulties and explain the higher dyspnoea felt with the CM.
Some authors postulated that covering mouth and nose with facemasks will increase work of breathing by imposing a supplemental resistance to respiration [39]. However, the similar cardiorespiratory demand and performance with or without facemask found in this study does not support this hypothesis. The pressure drop associated with an exercise ventilation corresponding to a moderate-vigorous physical activity was found to be around 1 cmH2O or less with surgical and cloth facemasks [38]. It is only at very high intensity exercise that the minute ventilation needed to trigger a noticeable impact in work of breathing may be achieved, which is far beyond the ventilatory demand of the 1STST [38]. Consistent with this, facemasks with resistances similar to those found with surgical or cloth masks did not influence the cardiorespiratory response of the wearer at low-to-moderate work rates over 1 h [40]. Altogether, the increased respiratory resistance due to facemasks seems clinically meaningless in healthy adults at low-to-moderate exercise intensity, but further research are needed to elucidate these effects in individuals with underlying cardiorespiratory disease.
Our study had several limitations. First, we collected data on healthy healthcare workers. Then, the extrapolation of the results to patients is questionable. Indeed, the dyspnoea at rest was negligible in our cohort of young healthy adults. Moreover, our subjects had a high level of physical activity as illustrated by the results of GPAQ and were more used to wearing a mask due to their job as healthcare workers. Second, the masks were tightly attached around the face of the participants and may have collapsed during the effort, potentially increasing dyspnoea. Third, although a learning effect with the 1STST was anticipated and took into account, we could not exclude a potential residual improvement of performance over more training tests. To the best of our knowledge, the learning effect of repetitive 1STST is unknown in healthy participants. However, the similar number of 1STST repetitions with or without masks, regardless the order of the randomization, is reassuring. Finally, we only tested one type of CM and the results may vary depending on the material used and its breathability.
To conclude, cloth and surgical facemasks had minimal to no impact on dyspnoea, cardiorespiratory parameters, and exercise performance during a short submaximal exercise test in healthy adults.
Funding
No funding for the study. Gregory Reychler and William Poncin received a grant from the Institut de Recherche Expérimentale et Clinique (Université catholique de Louvain – Brussels – Belgium).
CRediT authorship contribution statement
Gregory Reychler: Conceptualization, Methodology, Formal analysis, Writing – original draft, Writing – review & editing, Visualization, Supervision. Charlie vander Straeten: Conceptualization, Formal analysis, Writing – original draft, Writing – review & editing. Adrien Schalkwijk: Conceptualization, Formal analysis, Writing – original draft, Writing – review & editing. William Poncin: Conceptualization, Methodology, Formal analysis, Writing – original draft, Writing – review & editing, Visualization, Supervision.
Declaration of competing interest
None.
Acknowledgements
The authors thank Christel Vanvuchelen for the conception and the donation of the cloth masks. The authors also thank Nomics for making the Somnolter available for this study. Finally, we thank all the participants for participating in this study.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.rmed.2021.106530.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Abboah-Offei M., Salifu Y., Adewale B., Bayuo J., Ofosu-Poku R., Opare-Lokko E.B.A. A rapid review of the use of face mask in preventing the spread of COVID-19. Int J Nurs Stud Adv. 2021;3:100013. doi: 10.1016/j.ijnsa.2020.100013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Worby C.J., Chang H.H. Face mask use in the general population and optimal resource allocation during the COVID-19 pandemic. Nat. Commun. 2020;11(1):4049. doi: 10.1038/s41467-020-17922-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Matuschek C., Moll F., Fangerau H., Fischer J.C., Zänker K., van Griensven M., Schneider M., Kindgen-Milles D., Knoefel W.T., Lichtenberg A., Tamaskovics B., Djiepmo-Njanang F.J., Budach W., Corradini S., Häussinger D., Feldt T., Jensen B., Pelka R., Orth K., Peiper M., Grebe O., Maas K., Gerber P.A., Pedoto A., Bölke E., Haussmann J. Face masks: benefits and risks during the COVID-19 crisis. Eur. J. Med. Res. 2020;25(1):32. doi: 10.1186/s40001-020-00430-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wang Y., Xu G., Huang Y.W. Modeling the load of SARS-CoV-2 virus in human expelled particles during coughing and speaking. PloS One. 2020;15(10) doi: 10.1371/journal.pone.0241539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Scheuch G. Breathing is enough: for the spread of influenza virus and SARS-CoV-2 by breathing only. J. Aerosol Med. Pulm. Drug Deliv. 2020;33(4):230–234. doi: 10.1089/jamp.2020.1616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Anfinrud P., Stadnytskyi V., Bax C.E., Bax A. Visualizing speech-generated oral fluid droplets with laser light scattering. N. Engl. J. Med. 2020;382(21):2061–2063. doi: 10.1056/NEJMc2007800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stadnytskyi V., Bax C.E., Bax A., Anfinrud P. The airborne lifetime of small speech droplets and their potential importance in SARS-CoV-2 transmission. Proc. Natl. Acad. Sci. U. S. A. 2020;117(22):11875–11877. doi: 10.1073/pnas.2006874117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Esposito S., Principi N., Leung C.C., Migliori G.B. Universal use of face masks for success against COVID-19: evidence and implications for prevention policies. Eur. Respir. J. 2020;55(6) doi: 10.1183/13993003.01260-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Soriano J.B., Anzueto A., Bosnic Anticevich S., Kaplan A., Miravitlles M., Usmani O., Papadopoulos N.G., Puggioni F., Canonica G.W., Roche N. Face masks, respiratory patients and COVID-19. Eur. Respir. J. 2020;56(5):2003325. doi: 10.1183/13993003.03325-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jefferson T., Del Mar C.B., Dooley L., Ferroni E., Al-Ansary L.A., Bawazeer G.A., van Driel M.L., Jones M.A., Thorning S., Beller E.M., Clark J., Hoffmann T.C., Glasziou P.P., Conly J.M. Physical interventions to interrupt or reduce the spread of respiratory viruses. Cochrane Database Syst. Rev. 2020;11 doi: 10.1002/14651858.CD006207.pub5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Canini L., Andréoletti L., Ferrari P., D'Angelo R., Blanchon T., Lemaitre M., Filleul L., Ferry J.-P., Desmaizieres M., Smadja S., Valleron A.-J., Carrat F. Surgical mask to prevent influenza transmission in households: a cluster randomized trial. PloS One. 2010;5(11) doi: 10.1371/journal.pone.0013998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mask Use in the Context of COVID-19: Interim Guidance. World Health Organization; 2020. https://apps.who.int/iris/handle/10665/337199 1 December. [Internet] [Google Scholar]
- 13.Chandrasekaran B., Fernandes S. Exercise with facemask; Are we handling a devil's sword?" - a physiological hypothesis. Med. Hypotheses. 2020;144:110002. doi: 10.1016/j.mehy.2020.110002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Roberge R.J., Kim J.H., Benson S.M. Absence of consequential changes in physiological, thermal and subjective responses from wearing a surgical mask. Respir. Physiol. Neurobiol. 2012;181(1):29–35. doi: 10.1016/j.resp.2012.01.010. [DOI] [PubMed] [Google Scholar]
- 15.Roberge R.J., Coca A., Williams W.J., Powell J.B., Palmiero A.J. Physiological impact of the N95 filtering facepiece respirator on healthcare workers. Respir. Care. 2010;55(5):569–577. [PubMed] [Google Scholar]
- 16.Bohannon R.W., Crouch R. 1-Minute Sit-to-Stand Test: systematic review of procedures, performance, and clinimetric properties. J Cardiopulm Rehabil Prev. 2019;39(1):2–8. doi: 10.1097/HCR.0000000000000336. [DOI] [PubMed] [Google Scholar]
- 17.Miller M.R., Hankinson J., Brusasco V., Burgos F., Casaburi R., Coates A., Crapo R., Enright P., van der Grinten C.P., Gustafsson P., Jensen R., Johnson D.C., MacIntyre N., McKay R., Navajas D., Pedersen O.F., Pellegrino R., Viegi G., Wanger J. Standardisation of spirometry. Eur. Respir. J. 2005;26(2):319–338. doi: 10.1183/09031936.05.00034805. [DOI] [PubMed] [Google Scholar]
- 18.Graham B.L., Steenbruggen I., Miller M.R., Barjaktarevic I.Z., Cooper B.G., Hall G.L., Hallstrand T.S., Kaminsky D.A., McCarthy K., McCormack M.C., Oropez C.E., Rosenfeld M., Stanojevic S., Swanney M.P., Thompson B.R. Standardization of spirometry 2019 update. An official American thoracic society and European respiratory society technical statement. Am. J. Respir. Crit. Care Med. 2019;200(8):e70–e88. doi: 10.1164/rccm.201908-1590ST. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Quanjer P.H., Stanojevic S., Cole T.J., Baur X., Hall G.L., Culver B.H., Enright P.L., Hankinson J.L., Ip M.S., Zheng J., Stocks J. Multi-ethnic reference values for spirometry for the 3-95-yr age range: the global lung function 2012 equations. Eur. Respir. J. 2012;40(6):1324–1343. doi: 10.1183/09031936.00080312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wanner M., Hartmann C., Pestoni G., Martin B.W., Siegrist M., Martin-Diener E. Validation of the global physical activity questionnaire for self-administration in a European context. BMJ Open Sport Exerc Med. 2017;3(1) doi: 10.1136/bmjsem-2016-000206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.World Health Organization Global Physical activity questionnaire (GPAQ) analysis guide. http://www.who.int/ncds/surveillance/steps/resources/GPAQ_Analysis_Guide.pdf Accessed on 23 February 2021. Available online:
- 22.Smets E.M., Garssen B., Bonke B., De Haes J.C. The Multidimensional Fatigue Inventory (MFI) psychometric qualities of an instrument to assess fatigue. J. Psychosom. Res. 1995;39(3):315–325. doi: 10.1016/0022-3999(94)00125-o. [DOI] [PubMed] [Google Scholar]
- 23.Engberg I., Segerstedt J., Waller G., Wennberg P., Eliasson M. Fatigue in the general population- associations to age, sex, socioeconomic status, physical activity, sitting time and self-rated health: the northern Sweden MONICA study 2014. BMC Publ. Health. 2017;17(1) doi: 10.1186/s12889-017-4623-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.van Dixhoorn J., Folgering H. The Nijmegen Questionnaire and dysfunctional breathing. ERJ Open Res. 2015;1(1) doi: 10.1183/23120541.00001-2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Borg E., Borg G., Larsson K., Letzter M., Sundblad B.M. An index for breathlessness and leg fatigue. Scand. J. Med. Sci. Sports. 2010;20(4):644–650. doi: 10.1111/j.1600-0838.2009.00985.x. [DOI] [PubMed] [Google Scholar]
- 26.Strassmann A., Steurer-Stey C., Lana K.D., Zoller M., Turk A.J., Suter P., Puhan M.A. Population-based reference values for the 1-min sit-to-stand test. Int. J. Publ. Health. 2013;58(6):949–953. doi: 10.1007/s00038-013-0504-z. [DOI] [PubMed] [Google Scholar]
- 27.Li Y., Tokura H., Guo Y.P., Wong A.S., Wong T., Chung J., Newton E. Effects of wearing N95 and surgical facemasks on heart rate, thermal stress and subjective sensations. Int. Arch. Occup. Environ. Health. 2005;78(6):501–509. doi: 10.1007/s00420-004-0584-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Person E., Lemercier C., Royer A., Reychler G. [Effect of a surgical mask on six minute walking distance] Rev. Mal. Respir. 2018;35(3):264–268. doi: 10.1016/j.rmr.2017.01.010. [DOI] [PubMed] [Google Scholar]
- 29.Kim J.H., Benson S.M., Roberge R.J. Pulmonary and heart rate responses to wearing N95 filtering facepiece respirators. Am. J. Infect. Contr. 2013;41(1):24–27. doi: 10.1016/j.ajic.2012.02.037. [DOI] [PubMed] [Google Scholar]
- 30.Kyung S.Y., Kim Y., Hwang H., Park J.W., Jeong S.H. Risks of N95 face mask use in subjects with COPD. Respir. Care. 2020;65(5):658–664. doi: 10.4187/respcare.06713. [DOI] [PubMed] [Google Scholar]
- 31.Wong A.Y., Ling S.K., Louie L.H., Law G.Y., So R.C., Lee D.C., Yau F.C., Yung P.S. Impact of the COVID-19 pandemic on sports and exercise. Asia Pac J Sports Med Arthrosc Rehabil Technol. 2020;22:39–44. doi: 10.1016/j.asmart.2020.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lässing J., Falz R., Pökel C., Fikenzer S., Laufs U., Schulze A., Hölldobler N., Rüdrich P., Busse M. Effects of surgical face masks on cardiopulmonary parameters during steady state exercise. Sci. Rep. 2020;10(1):22363. doi: 10.1038/s41598-020-78643-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mapelli M., Salvioni E., De Martino F., Mattavelli I., Gugliandolo P., Vignati C., Farina S., Palermo P., Campodonico J., Maragna R., Lo Russo G., Bonomi A., Sciomer S., Agostoni P. “You can leave your mask on”: effects on cardiopulmonary parameters of different airway protection masks at rest and during maximal exercise. Eur. Respir. J. 2021:2004473. doi: 10.1183/13993003.04473-2020. [DOI] [PubMed] [Google Scholar]
- 34.Fikenzer S., Uhe T., Lavall D., Rudolph U., Falz R., Busse M., Hepp P., Laufs U. Effects of surgical and FFP2/N95 face masks on cardiopulmonary exercise capacity. Clin. Res. Cardiol. 2020;109(12):1522–1530. doi: 10.1007/s00392-020-01704-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Reychler G., Boucard E., Peran L., Pichon R., Le Ber-Moy C., Ouksel H., Liistro G., Chambellan A., Beaumont M. One minute sit-to-stand test is an alternative to 6MWT to measure functional exercise performance in COPD patients. Clin. Res. J. 2018;12(3):1247–1256. doi: 10.1111/crj.12658. [DOI] [PubMed] [Google Scholar]
- 36.Ozalevli S., Ozden A., Itil O., Akkoclu A. Comparison of the Sit-to-Stand Test with 6 min walk test in patients with chronic obstructive pulmonary disease. Respir. Med. 2007;101(2):286–293. doi: 10.1016/j.rmed.2006.05.007. [DOI] [PubMed] [Google Scholar]
- 37.Parshall M.B., Schwartzstein R.M., Adams L., Banzett R.B., Manning H.L., Bourbeau J., Calverley P.M., Gift A.G., Harver A., Lareau S.C., Mahler D.A., Meek P.M., O'Donnell D.E. An official American Thoracic Society statement: update on the mechanisms, assessment, and management of dyspnea. Am. J. Respir. Crit. Care Med. 2012;185(4):435–452. doi: 10.1164/rccm.201111-2042ST. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hopkins S.R., Dominelli P.B., Davis C.K., Guenette J.A., Luks A.M., Molgat-Seon Y., Sá R.C., Sheel A.W., Swenson E.R., Stickland M.K. Face masks and the cardiorespiratory response to physical activity in health and disease. Ann Am Thorac Soc. 2021;18(3):399–407. doi: 10.1513/AnnalsATS.202008-990CME. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kim J.H., Wu T., Powell J.B., Roberge R.J. Physiologic and fit factor profiles of N95 and P100 filtering facepiece respirators for use in hot, humid environments. Am. J. Infect. Contr. 2016;44(2):194–198. doi: 10.1016/j.ajic.2015.08.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Roberge R.J., Kim J.H., Powell J.B., Shaffer R.E., Ylitalo C.M., Sebastian J.M. Impact of low filter resistances on subjective and physiological responses to filtering facepiece respirators. PloS One. 2013;8(12) doi: 10.1371/journal.pone.0084901. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.