Abstract
Purpose
To compare the clinical features, histopathology features, treatment, and prognosis of patients with and without pagetoid tumour spread secondary to periocular sebaceous gland carcinoma (SGC).
Methods
Retrospective study of 130 patients with SGC who underwent conjunctival map biopsy.
Results
Of the 130 patients with SGC, 30 (23%) patients had histopathology proven pagetoid tumour spread. On multivariate analysis, increasing tumour basal diameter (p < 0.001) was predictive of pagetoid tumour spread. The odds ratio for tumour basal diameter in prediction of map biopsy positivity for pagetoid tumour spread was 1.13 (95% CI, 1.07–1.19). The sensitivity and specificity of clinicopathological correlation of pagetoid tumour spread was 57 and 90%. Overall, globe salvage was better in those without pagetoid tumour spread compared to those with pagetoid tumour spread (95% vs 33%; p < 0.0001). Comparing those with pagetoid tumour spread vs those without, the 5-year Kaplan–Meier estimate of systemic metastasis was 21% vs 4% (p = 0.15) and death was 28% vs 4% (p = 0.21), respectively.
Conclusion
Increasing tumour basal diameter can predict the risk of pagetoid tumour spread. Every mm increase in tumour basal diameter increases the risk of pagetoid tumour spread by 13%. Map biopsy is recommended for all patients with periocular SGC’s. Though the globe salvage rates are poor in those with pagetoid tumour spread, the occurrence of systemic metastasis and death are not significantly higher compared to those without pagetoid tumour spread.
Subject terms: Eye cancer, Eye cancer
Introduction
Sebaceous gland carcinoma (SGC) of the eyelid and periocular region is a common eyelid malignancy, particularly in Asian population compared to the West [1–7]. It is the most common eyelid malignancy in the Asian Indian population [2–5]. It primarily affects the elderly age group and has a slight female preponderance [1–3]. Periocular SGC has a tendency for diffuse intraepithelial (pagetoid) spread beyond the site of the main tumour mass [8]. The occurrence of pagetoid tumour spread in SGC is noted to be between 16 and 80% [2, 4]. SGC is often misdiagnosed as recurrent chalazion in 8–20% [3, 9] and as chronic blepharoconjunctivitis in 28% cases [9]. SGC with diffuse pagetoid tumour spread is often misdiagnosed as chronic blepharoconjunctivitis leading to a delayed diagnosis.
Conjunctival map biopsies for periocular SGC’s were first used by Putterman in 1986 to accurately determine the extent of the tumour spread [10]. Putterman performed 16 site map biopsy including 4 from bulbar conjunctiva, 3 each from upper and lower forniceal conjunctiva, and 3 each from upper and lower tarsal conjunctiva in 12 cases of periocular SGC, which revealed pagetoid tumour spread in 4 (33%) cases necessitating orbital exenteration [10]. The technique was subsequently modified to include fewer biopsy sites (10 to 14) based on clinical suspicion [8]. Other variations include a technique of 17 site map biopsy including an additional sample from the caruncle [2, 3].
Though map biopsy is not universally performed in every case of periocular SGC, it is indicated in cases with clinical suspicion of pagetoid tumour spread. Herein, we retrospectively analysed the cases of periocular SGC who underwent 17-site conjunctival map biopsy to determine the indications of map biopsy, sensitivity and specificity of clinical diagnosis of pagetoid tumour spread, and the role of map biopsy in predicting the prognosis of periocular SGC.
Methods
This is a retrospective study conducted by the Operation Eyesight Universal Institute for Eye Cancer, L V Prasad Eye Institute, Hyderabad, India. Institutional Ethics Committee approval was obtained. The study adhered to the tenets of the declaration of Helsinki. Informed consent for use of data for research purpose was obtained from the patients. Written consent was obtained from patients for use of their image(s) in published media. A database search was conducted and all histologically proven cases of periocular sebaceous gland carcinoma from June 1995 to September 2016 were reviewed. Of these 241 patients with periocular SGC, 130 patients had undergone 17-site conjunctival map biopsy before or at the time of therapeutic intervention and were included for further analysis. Those patients who had not undergone the 17-site map biopsy were excluded from the study.
The demographic details and tumour laterality were noted. The duration of symptoms and referral clinical diagnosis were noted. The tumour features including tumour location, size, extent and morphology were recorded. Clinical evidence of pagetoid tumour spread (location and extent) if any was noted. Histological features including growth pattern, degree of differentiation and presence of perivascular or perineural invasion, if any, were recorded. Primary treatment details (Miotomycin-C, excisional biopsy, orbital exenteration, chemotherapy or radiotherapy) were recorded. Outcome measures including tumour recurrence, locoregional lymph node metastasis, systemic metastases, and metastases-related death were recorded.
Statistical analysis
Statistical analysis was performed using the software STATA v11.0 (StataCorp, College Station, TX, USA). Continuous data were checked for the normality of distribution using Shapiro-Wilk test. Equality of variance was assessed by Levene test. Between cases with and without pagetoid tumour spread, continuous data were compared by Mann–Whitney test due to either non-normal distribution or heteroscedasticity and categorical data by Chi-square test or Fisher Exact test. To assess the predictors of pagetoid tumour spread, logistic regression analysis was performed and, if the variables were significant, odds ratio was estimated. For clinicopathological correlation of pagetoid tumour spread by map biopsy, sensitivity, specificity, positive and negative predictive values were assessed. Kaplan–Meier analysis was performed to evaluate the estimates of locoregional metastasis, systemic metastasis and death. The equality of survival functions between cases with and without pagetoid tumour spread was assessed by log rank test. A p value of <0.05 was considered statistically significant.
Results
Of the 130 patients with SGC who underwent 17-site conjunctival map biopsy, 30 (23%) patients had histopathology proven pagetoid tumour spread (Fig. 1). Comparison of those with pagetoid vs those without pagetoid tumour spread revealed no difference in mean age at presentation (median age, 59 years vs 56 years; p = 0.48), gender (male:female ratio (1:1 vs 0.5:1; p = 0.11)), duration of symptoms (median, 13 months vs 13 months; p = 0.68), tumour epicenter (upper eyelid:lower eyelid, 5:1 vs 2.5:1; p = 0.27), tumour origin (Meibomian vs Zeiss glands, 14:1 vs 9:1; p = 0.73) and orbital (3% vs 2%; p = 1.00), paranasal sinus (3% vs 0%; p = 0.23), or lacrimal system (3% vs 2%; p = 1.00) tumour extension (Table 1). Statistically significant differences were noted between those with pagetoid vs those without pagetoid tumour spread in referral diagnosis as blepharoconjunctivitis (7% vs 0%; p = 0.05), tumour morphology (diffuse tumour configuration, 37% vs 17%; 0.04), and tumour basal dimension (median, 19 mm vs 12 mm; p = 0.0001). On univariate logistic regression, both tumour morphology (p = 0.03) and tumour basal diameter (p < 0.001) were significant predictors of pagetoid tumour spread. However, on multivariate logistic regression, only increasing tumour basal diameter (p < 0.001) was predictive of pagetoid tumour spread. The odds ratio for tumour basal diameter (p < 0.001) in prediction of map biopsy positivity for pagetoid tumour spread was 1.13 (95% CI, 1.07–1.19), indicating that every mm increase in tumour basal diameter increased the odds of pagetoid tumour spread by 13% (Fig. 2).
Fig. 1. Pagetoid tumour spread in periocular sebaceous gland carcinoma.
A A 30-year-old female with an upper eyelid nodule. B Localized infiltration of upper tarsal conjunctiva was noted on eyelid eversion suggestive of localized pagetoid tumour spread. C A 70-year-old male with a localized eyelid thickening which was being treated as blepharitis by the local ophthalmologist. D There was diffuse upper tarsal and forniceal conjunctival congestion on eyelid eversion suggestive of pagetoid tumour spread tumour. E A 55-year-old male with ill-defined eyelid lesion. F Eyelid eversion revealed diffuse upper tarsal and forniceal conjunctival congestion suggestive of pagetoid tumour spread tumour. G An 87-year-old male with diffuse conjunctival congestion and lower eyelid lesion with ill-defined margins. H A 60-year-old female with diffuse upper and lower eyelid margin and overlying skin along with diffuse conjunctival congestion suggestive of diffuse pagetoid tumour spread. This patient was receiving treatment for chronic blepharoconjunctivitis locally for more than 5 years.
Table 1.
Map biopsy in sebaceous gland carcinoma: demographics and clinical fea- tures.
| Feature | Patients with pagetoid tumour spreada n = 30 n (%) |
Patients without pagetoid tumour spreada n = 100 n (%) |
p value |
|---|---|---|---|
|
Age (years) mean (median; range) |
59 (59; 21–100) | 56 (56; 30–83) | 0.48 |
| Gender | |||
| Male | 15 (50) | 32 (32) | 0.11 |
| Female | 15 (50) | 68 (68) | |
| Laterality | |||
| Unilateral | 30 (100) | 100 (100) | 1.00 |
| Bilateral | 0 (0) | 0 (0) | |
| Referral diagnosis | |||
| Sebaceous gland carcinoma | 6 (20) | 32 (32) | 0.30 |
| Squamous cell carcinoma | 6 (20) | 9 (9) | 0.11 |
| Basal cell carcinoma | 3 (10) | 4 (4) | 0.35 |
| Stye | 0 (0) | 1 (1) | 1.00 |
| Chalazion | 1 (3) | 6 (6) | 0.69 |
| Blepharoconjunctivitis | 2 (7) | 0 (0) | 0.05 |
| Eyelid mass | 2 (7) | 2 (2) | 0.23 |
| Duration of symptoms (months) mean (median; range) | 24 (13; 2 to 130) | 18 (13; 1 to 130) | 0.68 |
| Tumour epicentre | |||
| Upper eyelid | 25 (83) | 71 (71) | 0.27 |
| Lower eyelid | 5 (17) | 29 (29) | |
| Tumour morphology | |||
| Solitary nodule | 19 (63) | 83 (83) | 0.04 |
| Diffuse lesion | 11 (37) | 17 (17) | |
| Tumour Basal Dimension (mm) mean, (median; range) | 19 (18; 3 to 35) | 12 (10; 1 to 30) | 0.0001 |
| Gland of origin based on tumour location | |||
| Meibomian glands | 28 (93) | 90 (90) | 0.73 |
| Glands of Zeiss | 2 (7) | 10 (10) | |
| Extent of tumour involvement | |||
| Orbit | 1 (3) | 2 (2) | 1.00 |
| Paranasal sinus | 1 (3) | 0 (0) | 0.23 |
| Lacrimal system | 1 (3) | 2 (2) | 1.00 |
aHistopathology proven.
Fig. 2.
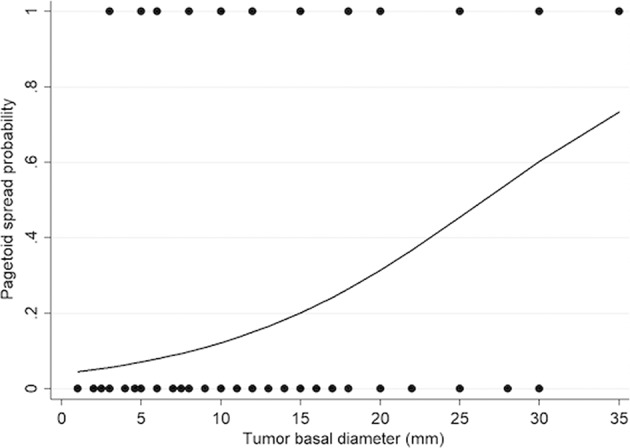
Probability of pagetoid tumour spread compared to the range of tumour basal diameter at presentation.
Histopathology features of tumour differentiation, growth pattern, mitotic activity, perivascular and perineural invasion were comparable in both the groups (Table 2). Conjunctival congestion leading to clinical suspicion of pagetoid tumour spread was noted in 37 cases, of which pagetoid tumour spread was confirmed on histopathology in 21 cases. In 9 other cases who had pagetoid tumour spread on histopathology, there was no clinical suspicion of the same. The sensitivity, specificity, positive predictive value, and negative predictive value of clinicopathological correlation of pagetoid tumour spread was 57%, 90%, 70%, and 84% respectively (Table 2).
Table 2.
Map biopsy in sebaceous gland carcinoma: histopathology features, clinicopathological correlation, treatment, and outcomes.
| Feature | Patients with pagetoid tumour spreada n = 30 n (%) |
Patients without pagetoid tumour spreada n = 100 n (%) |
p value |
|---|---|---|---|
| Tumour differentiation (n = 121) | |||
| Well differentiated | 6 (22) | 15 (16) | 0.08 |
| Moderately differentiated | 15 (56) | 71 (75) | |
| Poorly differentiated | 6 (22) | 8 (9) | |
| Growth pattern (n = 128) | |||
| Lobular | 14 (47) | 58 (59) | 0.33 |
| Comedo | 3 (10) | 8 (8) | |
| Papillary | 1 (3) | 8 (8) | |
| Mixed | 12 (40) | 24 (25) | |
| Mitotic activity (n = 125) | |||
| High | 15 (54) | 58 (60) | 0.78 |
| Moderate | 10 (36) | 32 (33) | |
| Low | 2 (7) | 6 (6) | |
| Atypical | 1 (3) | 1 (1) | |
| Perivascular invasion | 3 (10) | 8 (8) | 1.00 |
| Perineural invasion | 0 (0) | 4 (4) | 0.57 |
| Clinicopathological correlation of pagetoid tumour spreadb |
Positive map biopsy n = 30 n (%) |
Negative map biopsy n = 100 n (%) |
|
| Clinical suspicion of pagetoid tumour spread (n = 37) |
True Positive 21 (57) |
False Positive 16 (43) | |
| No clinical suspicion of pagetoid tumour spread (n = 93) |
False Negative 9 (10) |
True negative 84 (90) | |
| Primary treatment | |||
| Topical Mitomycin-C | 2 (7) | 0 (0) | 0.052 |
| Wide excision biopsy | 14 (47) | 95 (95) | <0.0001 |
| Orbital Exenteration | 11 (37) | 3 (3) | <0.0001 |
| Neoadjuvant Systemic Chemotherapy | 0 (0) | 2 (2) | 1.00 |
| External Beam Radiotherapy | 1 (3) | 0 (0) | 0.23 |
| Globe salvage | 10 (33) | 95 (95) | <0.0001 |
| Final outcome at last follow-up | |||
| Tumour recurrence | 6 (20) | 18 (18) | 0.79 |
| Regional lymph node metastasis | 4 (13) | 13 (13) | 1.00 |
| Systemic metastasis | 4 (13) | 4 (4) | 0.08 |
| Death due to metastasis | 4 (13) | 4 (4) | 0.08 |
Specificity: 90% (95% confidence interval, 82–95%).
Positive Predictive Value: 70% (95% confidence interval, 50–85%).
Negative Predictive Value: 84% (95% confidence interval, 75–90%).
aHistopathology proven.
bSensitivity: 57% (95% confidence interval, 40–73%).
Wide excisional biopsy (95% vs 47%; p < 0.0001) of the tumour was more common in those without pagetoid tumour spread while orbital exenteration (37% vs 3%; p < 0.0001) wa more common in those with pagetoid tumour spread (Table 2). Overall, globe salvage was higher in those without pagetoid tumour spread compared to those with pagetoid tumour spread (95% vs 33%; p < 0.0001).
Five and 10-year Kaplan–Meier estimates of systemic metastasis and death in those with pagetoid tumour spread vs those without was 21 and 21% vs 4 and 11% (p = 0.15) and 28 and 28% vs 4 and 4% (p = 0.20) respectively (Table 3). There was no statistically significant difference in the outcomes of those with pagetoid versus those without pagetoid tumour spread.
Table 3.
Kaplan–Meier analysis of the outcomes.
| Kaplan–Meier analysis | All cases n = 130 | Pagetoid tumour spread n = 30 | No pagetoid tumour spread n = 100 | p value |
|---|---|---|---|---|
| Locoregional metastasis | ||||
| 1 year | 5.6% ± 2.5% | 0% | 7.4% ± 3.2% | 0.18 |
| 2 years | 5.6% ± 2.5% | 0% | 7.4% ± 3.2% | |
| 3 years | 10% ± 3.8% | 0% | 13.5% ± 5.1% | |
| 4 years | 10% ± 3.8% | 0% | 13.5% ± 5.1% | |
| 5 years | 14.1% ± 5.4% | 11.1% ± 10.5% | 13.5% ± 5.1% | |
| 10 years | 25.6% ± 9.1% | 11.1% ± 10.5% | 30.6% ± 11.8% | |
| 15 years | 25.6% ± 9.1% | na | 30.6% ± 11.8% | |
| Systemic metastasis | ||||
| 1 year | 3.9% ± 2.0% | 4.2% ± 4.1% | 3.9% ± 2.3% | 0.35 |
| 2 years | 3.9% ± 2.0% | 4.2% ± 4.1% | 3.9% ± 2.3% | |
| 3 years | 6.3% ± 3.0% | 11.5% ± 8.0% | 3.9% ± 2.3% | |
| 4 years | 6.3% ± 3.0% | 11.5% ± 8.0% | 3.9% ± 2.3% | |
| 5 years | 10.4% ± 4.9% | 21.4% ± 11.7% | 3.9% ± 2.3% | |
| 10 years | 15.1% ± 6.6% | 21.4% ± 11.7% | 11.3% ± 7.4% | |
| 15 years | 15.1% ± 6.6% | na | 11.3% ± 7.4% | |
| Metastasis related death | ||||
| 1 year | 3.1% ± 1.8% | 0% | 4.1% ± 2.4% | 0.20 |
| 2 years | 4.7% ± 2.3% | 5.9% ± 5.7% | 4.1% ± 2.4% | |
| 3 years | 9.2% ± 3.8% | 19.3% ± 10.1% | 4.1% ± 2.4% | |
| 4 years | 9.2% ± 3.8% | 19.3% ± 10.1% | 4.1% ± 2.4% | |
| 5 years | 13.0% ± 5.2% | 28.3% ± 12.3% | 4.1% ± 2.4% | |
| 10 years | 13.0% ± 5.2% | 28.3% ± 12.3% | 4.1% ± 2.4% | |
| 15 years | 27.5% ± 13.9% | na | 28.1% ± 20.8% | |
na not available.
Discussion
Of all eyelid malignancies, periocular SGC is commonly associated with pagetoid tumour spread. Conjunctival map biopsy allows definition of exact tumour extent in the event of skip lesions in the form of distant conjunctival intraepithelial spread. In a case series of 60 patients with SGC, Shields et al. noted conjunctival intraepithelial involvement in 28 (47%) cases [9]. In our previous study of 191 Asian Indian patients with periocular SGC, pagetoid tumour spread detected by 17-site map biopsy was noted in 21 (16%) patients [3]. There is no consensus whether conjunctival map biopsy should be performed in every case of periocular SGC. In a review of preferred practice patterns in the management of SGC in the Asia- Pacific region, Cheung et al noted that 30% respondents performed map biopsies only if clinical suspicion of pagetoid spread existed, 20% performed them in case of tumour recurrence, and 19% performed map biopsies if both eyelids were involved by the tumour [11]. Shields et al recommended that map biopsies be performed in all patients with ill-defined or diffuse tumour involvement [9]. Other studies have suggested that all patients with even a localised, well-defined eyelid nodule should undergo sampling of a few sites on the palpebral and bulbar conjunctiva to rule out conjunctival spread, even if not clinically evident [12, 13].
SGC has a high proportion of misdiagnosis that delays appropriate treatment [3, 9]. In those with pagetoid tumour spread, it is often misdiagnosed as an ocular surface inflammatory disease due to the congested appearance of ocular surface. In our series, the misdiagnosis as blepharoconjunctivitis was more common in patients with pagetoid tumour spread versus those without pagetoid tumour spread (7% vs 0%; p = 0.05). Any lesion resembling unilateral blepharoconjunctivitis should be diagnosed as SGC with pagetoid spread until proven otherwise.
In our study, the comparative analysis of the demographic and clinical features of those with pagetoid tumour spread versus those without pagetoid tumour spread revealed no statistically significant difference in the parameters except for tumour morphology and tumour basal diameter. In a study of 51 patients with SGC, conjunctival intraepithelial tumour was noted in 36 (71%) patients, of whom 23 (64%) presented with diffuse eyelid involvement, and 13 (36%) presented with a solitary nodule [13]. The overall incorrect clinical assessment (false-positives and false-negatives) in case of solitary nodular lesions was 44% [13]. In our study, conjunctival intraepithelial tumour was noted in 11 (37%) patients presenting with diffuse eyelid involvement, and 19 (63%) presenting with a solitary nodule. Diffuse eyelid involvement was more common in those with pagetoid tumour spread compared to those without (37% vs 17%; p = 0.04). The clinicopathological correlation of conjunctival intraepithelial tumour was not established in 25 (19%) cases. The sensitivity of clinical diagnosis of pagetoid tumour spread was moderate at 57% and the specificity was good at 90%. These findings suggest that all cases of conjunctival intraepithelial tumour cannot be diagnosed clinically but when the signs of conjunctival spread are suspected, it is confirmed by pathology in 90% cases. Thus, high degree of suspicion of pagetoid tumour spread is important. The clinical signs of conjunctival intraepithelial tumour are conjunctival congestion away from the primary tumour indicating distant skip lesions. Based on our results, we recommend conjunctival map biopsy in all cases since 10% of cases would otherwise be missed based on clinical diagnosis, and map biopsy does not cause any ocular morbidity.
In a study of 25 SGC patients by Chao et al, the mean tumour diameter was 14 mm in the positive group and 8 mm in the negative group, indicating a larger tumour in the group with pagetoid tumour spread [14]. In our study, the mean tumour diameter in those with pagetoid tumour spread was 19 mm versus 12 mm in those without pagetoid tumour spread (p = 0.0001). Every mm increase in tumour basal diameter increases the risk of pagetoid tumour spread by 13%. Larger the tumour higher is the risk of pagetoid tumour spread.
Histopathological features were comparable in both groups of those with and without pagetoid tumour spread. There was no correlation between poor tumour differentiation, perineural or perivascular invasion and pagetoid tumour spread. Current management of cases with pagetoid tumour spread focuses on local disease control with an attempt at globe salvage [8]. Lesions with tumour spread confined to the epithelium, may be treated with a combination of cryotherapy and topical chemotherapy with Mitomycin-C [2, 3, 9]. Lesions with stromal invasion on map biopsy may be treated with conservative excision of involved sites with reconstruction of the anterior and posterior lamellae through various techniques [1]. SGC with extensive tumour spread necessitates orbital exenteration. In our study, globe salvage rates were better in the group without pagetoid tumour spread compared to those with pagetoid tumour spread (95% vs 33%; p < 0.0001). The poor globe salvage rates indicate extensive disease in our series.
In a comparative analysis of 25 patients with and without pagetoid tumour spread by Chao et al., tumour recurrence (9% vs 14%) and metastasis (18% vs 14%) were comparable in both groups [14]. In another study of 34 patients with SGC by Takahashi et al., pagetoid tumour spread was associated with higher incidence of tumour recurrence and metastasis [12]. Rao et al. reported higher mortality of 50% in patients with pagetoid tumour spread compared to 11% in those without pagetoid tumour spread [15], while other studies reported a comparable outcome [14, 16]. In our study, there was no difference in the time-related risk of tumour recurrence, lymph node metastasis, systemic metastasis, and metastasis-related death in patients with and without conjunctival disease.
In conclusion, every mm increase in tumour basal diameter increases the risk of pagetoid tumour spread by 13%. The sensitivity and specificity of clinical diagnosis of pagetoid tumour spread are 57 and 90% respectively. Conjunctival map biopsy should be performed in all cases with periocular SGC. Globe salvage rates are poor with pagetoid tumour spread but the incidence of tumour recurrence, metastasis, and death are comparable to the patients without conjunctival intraepithelial tumour spread.
Summary
What was known before
Sebaceous gland carcinoma is associated with pagetoid tumour spread Pagetoid tumour spread can be detected by conjunctival map biopsy
What this study adds
Basal tumour diameter is an important risk factor that can predict the risk of pagetoid tumour spread in periocular sebaceous gland carcinoma Every mm increase in tumour diameter of periocular sebaceous gland carcinoma increases the risk of pagetoid tumour spread by 13%
Acknowledgments
Funding
Support provided by The Operation Eyesight Universal Institute for Eye Cancer (SK) and Hyderabad Eye Research Foundation (SK), Hyderabad, India. The funders had no role in the preparation, review or approval of the manuscript.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Shields JA, Demirci H, Marr BP, Eagle RC, Jr, Shields CL. Sebaceous carcinoma of the ocular region: a review. Surv Ophthalmol. 2005;50:103–22.. doi: 10.1016/j.survophthal.2004.12.008. [DOI] [PubMed] [Google Scholar]
- 2.Cicinelli MV, Kaliki S. Ocular sebaceous gland carcinoma: an update of the literature. Int Ophthalmol. 2019;39:1187–97. doi: 10.1007/s10792-018-0925-z. [DOI] [PubMed] [Google Scholar]
- 3.Kaliki S, Ayyar A, Dave TV, Ali MJ, Mishra DK, Naik MN. Sebaceous gland carcinoma of the eyelid: clinicopathological features and outcome in Asian Indians. Eye. 2015;29:958–63.. doi: 10.1038/eye.2015.79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kaliki S, Gupta A, Ali MH, Ayyar A, Naik MN. Prognosis of eyelid sebaceous gland carcinoma based on the tumor (T) category of the American Joint Committee on Cancer (AJCC) classification. Int Ophthalmol. 2016;36:681–90. doi: 10.1007/s10792-016-0187-6. [DOI] [PubMed] [Google Scholar]
- 5.Kaliki S, Bothra N, Bejjanki KM, et al. Malignant eyelid tumors in India: a study of 536 Asian Indian patients. Ocul Oncol Pathol. 2019;5:210–9. doi: 10.1159/000491549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Watanabe A, Sun MT, Pirbhai A, et al. Sebaceous carcinoma in Japanese patients: clinical presentation, staging and outcomes. Br J Ophthalmol. 2013;97:1459–63.. doi: 10.1136/bjophthalmol-2013-303758. [DOI] [PubMed] [Google Scholar]
- 7.Lam SC, Li EYM, Yuen HKL. 14-year case series of eyelid sebaceous gland carcinoma in Chinese patients and review of management. Br J Ophthalmol. 2018;102:1723–7. doi: 10.1136/bjophthalmol-2017-311533. [DOI] [PubMed] [Google Scholar]
- 8.Shields JA, Demirci H, Marr BP, Eagle RC, Jr, Stefanyszyn M, Shields CL. Conjunctival epithelial involvement by eyelid sebaceous carcinoma The 2003 J. Howard Stokes Lecture. Ophthalmic Plast Reconstr Surg. 2005;21:92–6. doi: 10.1097/01.IOP.0000152494.47038.0E. [DOI] [PubMed] [Google Scholar]
- 9.Shields JA, Demirci H, Marr BP, Eagle RC, Jr, Shields CL. Sebaceous carcinoma of the eyelids: personal experience with 60 cases. Ophthalmology. 2004;111:2151–7. doi: 10.1016/j.ophtha.2004.07.031. [DOI] [PubMed] [Google Scholar]
- 10.Putterman AM. Conjunctival map biopsy to determine pagetoid spread. Am J Ophthalmol. 1986;102:87–90. doi: 10.1016/0002-9394(86)90214-X. [DOI] [PubMed] [Google Scholar]
- 11.Cheung JJC, Esmaeli B, Lam SC, Kwok T, Yuen HKL. The practice patterns in the management of sebaceous carcinoma of the eyelid in the Asia Pacific region. Eye. 2019;33:1433–42. doi: 10.1038/s41433-019-0432-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Takahashi Y, Takahashi E, Nakakura S, Kitaguchi Y, Mupas-Uy J, Kakizaki H. Risk factors for local recurrence or metastasis of eyelid sebaceous gland carcinoma after wide excision with paraffin section control. Am J Ophthalmol. 2016;171:67–74. doi: 10.1016/j.ajo.2016.08.028. [DOI] [PubMed] [Google Scholar]
- 13.McConnell LK, Syed NA, Zimmerman MB, Carter KD, Nerad JA, Allen RC, et al. An analysis of conjunctival map biopsies in sebaceous carcinoma. Ophthalmic Plast Reconstr Surg. 2017;33:17–21. doi: 10.1097/IOP.0000000000000616. [DOI] [PubMed] [Google Scholar]
- 14.Chao AN, Shields CL, Krema H, Shields JA. Outcome of patients with periocular sebaceous gland carcinoma with and without conjunctival intraepithelial invasion. Ophthalmology. 2001;108:1877–83.. doi: 10.1016/S0161-6420(01)00719-9. [DOI] [PubMed] [Google Scholar]
- 15.Rao NA, Hidayat AA, McLean IW, Zimmerman LE. Sebaceous carcinomas of the ocular adnexa: a clinicopathologic study of 104 cases, with five-year follow-up data. Hum Pathol. 1982;13:113–22. doi: 10.1016/S0046-8177(82)80115-9. [DOI] [PubMed] [Google Scholar]
- 16.Margo CE, Lessner A, Stern GA. Intraepithelial sebaceous carcinoma of the conjunctiva and skin of the eyelid. Ophthalmology. 1992;99:227–31. doi: 10.1016/S0161-6420(92)31988-8. [DOI] [PubMed] [Google Scholar]



