Abstract
Background
Coronavirus disease 2019 (COVID-19) is now globally considered a serious economic, social and health threat. A wide range of health related factors including Body Mass Index (BMI) is reported to be associated with the disease. In the present study, we analyzed global databases to assess the correlation of BMI and cholesterol with the risk of COVID-19.
Methods
In this ecological study, we used age-standardized BMI and cholesterol levels as well as the incidence and mortality ratio of COVID-19 at the national-levels obtained from the publicly available databases such as the World Health Organization (WHO) and NCD Risk Factor Collaboration (NCD-RisC). Bivariate correlation analysis was applied to assess the correlations between the study variables. Mean differences (standard deviation: SD) of BMI and cholesterol levels of different groups were tested using independent sample t-test or Mann–Whitney rank test as appropriate. Multivariable linear regression analysis was performed to identify variables affecting the incidence and mortality ratio of COVID-19.
Results
Incidence and mortality ratio of COVID-19 were significantly higher in developed (29,639.85 ± 20,210.79 for cases and 503.24 ± 414.65 for deaths) rather than developing (8153.76 ± 11,626.36 for cases and 169.95 ± 265.78 for deaths) countries (P < 0.01). Results indicated that the correlations of BMI and cholesterol level with COVID-19 are stronger in countries with younger population. In general, the BMI and cholesterol level were positively correlated with COVID-19 incidence ratio (β = 2396.81 and β = 30,932.80, p < 0.01, respectively) and mortality ratio (β = 38.18 and β = 417.52, p < 0.05, respectively) after adjusting for socioeconomic and demographic factors.
Conclusion
Countries with higher BMI or cholesterol at aggregate levels had a higher ratios of COVID-19 incidence and mortality. The aggregated level of cholesterol and BMI are important risk factors for COVID-19 major outcomes, especially in developing countries with younger populations. We recommend monitoring and promotion of health indicices to better prevent morbidity and mortality of COVID-19.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12889-021-11715-7.
Keywords: COVID-19; mortality, BMI, Obesity, Cholesterol, Risk factors
Background
Coronavirus disease 2019 (COVID-19), is a life-threatening condition that is caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) emerged first in Wuhan, China, at the end of 2019. This disease is now considered a globally severe economic, social and health issue [1]. Up to now, COVID-19 has infected approximately 180 million people worldwide, and the deaths due to the infection surpassed 3.9 million cases by June 27, 2021 [2].
World Health Organization (WHO) has declared COVID-19 a global pandemic associated with multiple affecting factors [3, 4] such as air pollution, sociodemographic indixes and genetic factors [5–10]. Previous studies suggested that Body Mass Index (BMI) and obesity are positively correlated with infection, mortality, and hospitalization due to COVID-19 [11–14]. The association of obesity with hospitalization, duration of the use of mechanical ventilation and death has been reported for other respiratory viruses, such as influenza [15, 16]. Based on the previous studies, being in a younger age is associated with a remarkably lower risk of severe COVID-19 infection [17, 18]. Furthermore, evidence indicates that young and obese individuals hospitalized with COVID- 19 diagnosis are at a higher risk for adverse outcomes [13].
On the other hand, several studies reported a lower cholesterol level in severe or end-stage COVID-19 patients than those in moderate-condition [19–23]. Currently, it is well established that BMI and serum cholesterol level have a direct correlation with the severity of COVID-19 infection [24]. However, the possible interaction between obesity, cholesterol level and age has not been fully addressed yet. Understanding COVID-19 risk factors would help both health care providers and policy makers to focus on targeted preventive and therapeutic strategies [25, 26]. In this regard, we hypothesized that a population with a higher cholesterol level and a higher rate of obesity might experience higher COVID-19 incidence and mortality (COVID-19 variables), especially in countries with a low median age (< 20 years old). To address this hypothesis, using an ecological approach, we investigated the correlation between BMI, serum cholesterol level, and COVID-19 incidence and mortality in 159 countries.
Methods
Study area and COVID-19 data collection
In this study, we followed the “Strengthening the Reporting of Observational Studies in Epidemiology” (STROBE) guidelines [27, 28]. We included 159 countries (each with at least 10 deaths). COVID-19 data were obtained from the free-access and publicly available World Health Organization website (WHO Coronavirus Disease Dashboard, https://covid19.who.int/). The data includes the total number of confirmed cases of COVID-19 and the death toll, along with the incidence and mortality ratios per million population by December 21, 2020. The mentioned data is updated on a daily base. The organization (WHO) also provides additional data on demographic variables such as median age (low< 20, average = 20–40 and > 40 years old), age > 65, age > 70, Gross National Product (GDP) per capita and population density (persons per km2) for every country. According to the United Nations, countries with high Human Development Index (HDI) scores (≥0.788) are regarded as developed, and otherwise as developing countries [29]. All methods were performed in accordance with the relevant guidelines and regulations.
BMI and cholesterol assessment
The retrospective data on BMI and cholesterol level were collected from several publically available dataset such as WHO, Global Burden Of Diseases (GBD) and Non-Communicable Diseases Risk Factor Collaboration (NCD-RisC) [30–32]. The mean values of BMI (kg/m2) for every country is reported as the prevalence of underweight (BMI ≤18.5), overweight (BMI ≥25) and obese (BMI ≥30) among adults in 2016. Also, we extracted the mean total serum cholesterol level (mmole/L), prevalence of increased total cholesterol (≥5 mmol/L) and (≥6.2 mmol/L) for 2009. We obtained the mean values of the serum levels of total cholesterol, HDL and non-HDL cholesterol (mmol/L) for 2018 from NCD-RisC website [30]. Data is age-adjusted for males, females and both genders. Also, several risk factors such as air pollution, prevalence of insufficient physical activity, alcohol use, tobacco and unsafe water, sanitation, and handwashing were assessed in male, females and both genders according to GBD and WHO databases. We used data on the burden of tuberculosis and other respiratory infections (based on disability-adjusted life year (DALY) as confounder’s variables.
Statistical analysis
Descriptive analyses (frequency distribution of qualitative variables, mean and standard deviation (SD) and median and interquartile range (IQR) for quantitative variables) were done for all variables. Spearman and Pearson’s correlation were used to estimate the associations between the COVID-19 related indexes (absolute number and cases and death per capita) with BMI, serum cholesterol level and other selected variables. The normality of data was checked by Kolmogorov–Smirnov test. Parametric approaches were applied for normally distributed data (e.g. Pearson’s’ correlation test) and non-parametric methods were used when data was not normally distributed (Spearman test). Also, to determine the adjusted contributions of independent variables, multivariable regression models were applied to reveal the association between COVID-19 incidence and mortality ratios per million and BMI and serum cholesterol level. To compare mean of quantitative variables in two or more groups, student T-test (or Mann–Whitney U if appropriate) and one-way ANOVA (or Kruskal-Wallis if appropriate) tests were used. A Scatter plot is provided to indicate the correlation of the mean values of the study variables. Statistical analyses were done using IBM SPSS Statistics 20 software and the graphical presentations are prepared by GraphPad Prism (version 6). Figures indicating the distribution of COVID-19 and independent variables are provided by GIS (Arc map 10.3).
Role of the funding source
The funders of the study had no role in the study design, data collection, data analysis, data interpretation, or the writing of the report. The correspondig authors had full access to the data and had final responsibility for the decision to submit for publication.
Results
Description analysis
A total number of 77,364,641 confirmed cases and 1,702,596 deaths have been reported from 190 countries and territories by December 21, 2020. As aforementioned, our study evaluated 159 countries which included 77,102,624 COVID-19 cases and 1,697,759 deaths. USA, India, Brazil, Russia, France, UK and Turkey were the top seven countries with more than 2 million cases of COVID-19. Moreover, the USA, Brazil, India, Mexico, Italy, the UK and France reported the highest death toll.
In terms of incidence ratio (per million), Andorra, Luxembourg, Montenegro, San Marino, Czechia, USA and Belgium had the greatest values. However, San Marino, Belgium, Italy, Slovenia, Bosnia and Herzegovina, Peru and Spain had the highest mortality ratios. Ethiopia and Kuwait were the countries with lowest and highest BMI, respectively, and Vietnam and Kuwait had the lowest and highest prevalence of obesity respectively. Niger and Iceland had the lowest and highest cholesterol level (mmol/L) in 2009, respectively and Rwanda and Lithuania had the lowest and highest values in 2018 of cholesterol level. The descriptive statistics for the study variables and confounding variables are shown in Table 1 and Table S1 and S2. Until December 21, 2020, the worldwide geographic distributions of the incidence and mortality ratios due to COVID-19 are shown in Fig. 1.
Table 1.
Descriptive statistics of study
| Variables | Mean | SD | Median | IQR (25, 75%) | |
|---|---|---|---|---|---|
| Total cases per million | 16,396.85 | 18,653.61 | 9987.79 | 1106.63 | 27,700.01 |
| Total deaths per million | 297.82 | 367.55 | 109.60 | 20.32 | 419.96 |
| Mean BMI (kg/m2) | 25.55 | 2.00 | 26.10 | 23.80 | 26.90 |
| Prevalence of underweight among adults | 5.44 | 5.04 | 2.95 | 1.43 | 9.18 |
| Prevalence of overweight among adults | 47.92 | 15.69 | 55.45 | 30.90 | 60.28 |
| Prevalence of obesity among adults | 18.58 | 8.88 | 20.35 | 9.53 | 25.23 |
| Mean total serum cholesterol-2009 | 4.72 | .43 | 4.75 | 4.35 | 5.10 |
| Prevalence of high cholesterol (≥ 5) -2009 | 39.90 | 14.36 | 39.40 | 27.30 | 52.95 |
| Prevalence of high cholesterol (≥ 6.2) -2009 | 10.60 | 6.00 | 9.40 | 5.30 | 15.40 |
| Mean total cholesterol (mmol/L)-2018 | 4.52 | .38 | 4.62 | 4.15 | 4.81 |
| Mean non-HDL cholesterol (mmol/L) -2018 | 3.28 | .36 | 3.32 | 2.95 | 3.55 |
| Mean HDL cholesterol (mmol/L) -2018 | 1.22 | .16 | 1.19 | 1.11 | 1.38 |
IQR Interquartile Range, BMI Body Mass Index, SD Standard Deviation
Fig. 1.
GIS distribution map of various variables; a cases ratio of COVID-19, b death ratio of COVID-19, c mean age-standardized BMI, d % prevalence of overweight (age-standardized), e % prevalence of obesity (age-standardized), f mean cholesterol level (age-standardized), g % prevalence of raised total cholesterol up 5 mmol/L (age-standardized) and h) % prevalence of raised total cholesterol up 6.2 mmol/L (age-standardized)
Correlation between the study variables and COVID-19 measures
Table 2 shows the Spearman and Pearson’s correlation between independent variables (BMI and cholesterol), sociodemographic factors (population density, and median age and GDP) for the selected countries with the dependent variables (COVID-19 variables).
Table 2.
Spearman and Pearson’s correlation (r) between COVID-19 parameters and the studied variables (sex-age-standardized)
| Variables | Total cases | Total deaths | Incidence ratio a | Mortality ratio a |
|---|---|---|---|---|
| Mean total serum cholesterol (2009) | .495** | .391** | .692** | .611** |
| Prevalence of high cholesterol (≥ 5) | .498** | .397** | .695** | .617** |
| Prevalence of high cholesterol (≥ 6.2) | .485** | .383** | .701** | .621** |
| Mean total cholesterol (mmol/L) | .450** | .409** | .609** | .602** |
| Mean non-HDL cholesterol (mmol/L) | .419** | .411** | .488** | .539** |
| Mean HDL cholesterol (mmol/L) | .199* | .139 | .476** | .390** |
| Mean BMI (kg/m2) | .364** | .356** | .586** | .617** |
| Prevalence of overweight among adults | .438** | .410** | .641** | .643** |
| Prevalence of obesity among adults | .388** | .374** | .588** | .604** |
| Prevalence of underweight among adults | −.457** | −.436** | −.704** | −.715** |
| GDP per capita | .475** | .356** | .679** | .564** |
| Median age | .523** | .447** | .679** | .621** |
| Aged > 65 older | .484** | .459** | .582** | .605** |
| Aged > 70 older | .480** | .454** | .594** | .615** |
| Population density | .149 | .066 | .141 | .033 |
GDP Gross Domestic Product per capita, ** P < .01, * P < .05, a = per million
The analysis revealed a significant and positive correlation between BMI and cholesterol with COVID-19 incidence and mortality ratios (r > 0.60 and P < 0.001). Althouogh, the result was not significant for the population density (P > .05), the association between COVID-19 indixes with BMI and serum cholesterol in males is robust (Supplementary Tables S3).
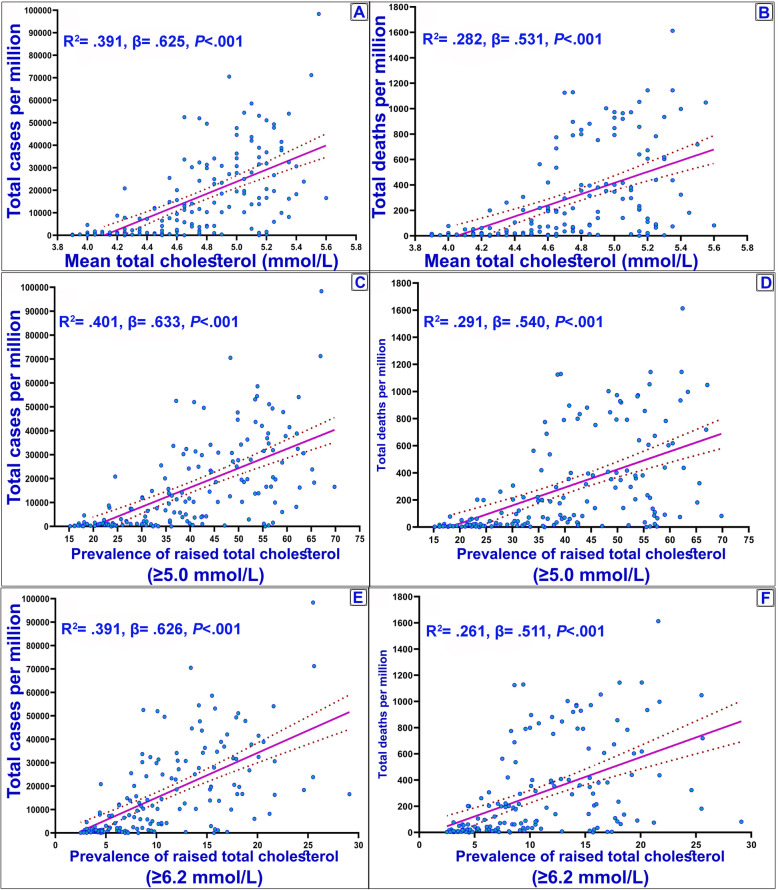
In addition, the analysis was also conducted to reveal the association between COVID-19 variables and the study variables in developed and developing countries (Supplementary Tables S4). According to the results, in developing countries, all variables have a significant and positive association with COVID-19 indixes. However, in developed countries, only the prevalence of underweight, age > 65, age > 70 and population density were significantly associated with the indixes. The associations of the independent study variables are shown in Supplementary Table S5. Accordingly, BMI had a significant positive correlation with cholesterol (r = 0.45 and r = 0.81 for BMI and Cholesterol, respectively, P < 0.001). The results of linear regression model also identified a positive association between the mean of total cholesterol, prevalence of raised cholesterol (≥5 mmol/L and ≥ 6.2 mmol/L) with the incidence and mortality ratios of COVID-19 (Fig. 2). These results are also observed for BMI (Fig. 3), HDL, and non-HDL cholesterol parameters (Supplementary Fig. S1).
Fig. 2.
Cases and deaths ratio of COVID-19 and cholesterol variables. a & b: Mean total serum cholesterol (mmol/L) (age-standardized estimate) reported in 2009 for evaluated countries; c & d: Prevalence of raised total cholesterol (≥ 5 mmol/L or ≥ 190 mg/dl); e & f: Prevalence of raised total cholesterol (≥ 6.2 mmol/L or ≥ 240 mg/dl). Best-fit lines (solid purple line) and the 95% confidence intervals of the best-fit line (dashed) by linear regression are indicated
Fig. 3.
Cases and deaths ratio of COVID-19 and BMI variables. a & b: BMI in kg/m2 reported in 2016 for evaluated countries (age-standardized both sex); c & d: Prevalence of obesity among adults BMI ≥ 30 (age-standardized both sex); e & f: Prevalence of overweight among adults, BMI ≥ 25 (age-standardized both sex). Best-fit lines (solid purple line) and the 95% confidence intervals of the best-fit line (dashed) by linear regression are indicated
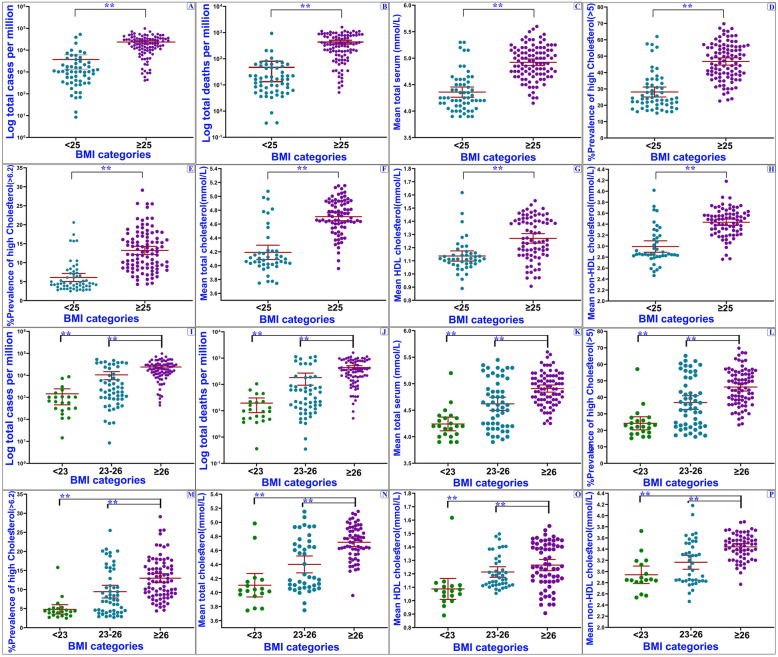
Additional analyses were performed for developed and developing countries to investigate the impact of independent variables on COVID-19 indixes. In this respect, we found significant differences between COVID-19 variables (P < 0.01) (Fig. 4). Among developing countries, the average mean cholesterol (2009) and BMI were 4.45 (95% Confidence Interval (95% CI): 4.39–4.51) and 24.90 (95% CI: 24.47–25.33), which was elevated with an increase in the incidence and mortality ratios of COVID-19 (P < 0.01). These variables were 5.14 (95% CI: 5.09–5.19) and 26.59 (95% CI: 26.26–26.91) in developed countries. There were significant differences between the countries in BMI categories (p < 0.001) (Fig. 5). Among countries with low (< 25 Kg/m2) and high (≥25 Kg/m2) BMI, the average incidence ratio (per million) was 3714.67 (95% CI: 1348.18–6081.14) and 23,551.94 (95% CI: 19858.26–27,245.63), and the mortality ratio was 46.93 (95% CI: 13.32–80.53) and 434.53 (95% CI: 361.60–507.46), respectively. The regions with larger BMI showed significantly higher cholesterol level and higher incidence of COVID-19 compared to the countries with low BMI (Fig. 5).
Fig. 4.

COVID-19 and independent variables in countries with different development levels. ** P < 0.01, Student’s t-test or Mann-Whitney U test was conducted in the comparison
Fig. 5.
Differences of COVID-19 and independent variables in two and three BMI levels. COVID-19 cases and deaths ratio in “high BMI countries” are significantly greater than that of the “low BMI countries”. ***P < .001. Horizontal lines represent group means. One-way ANOVA analysis or Kruskal–Wallis test was conducted in the comparison
Regression analysis
Table 3 demonstrates the results of regression analysis (adjusted and non-adjusted) on the association of the incidence and mortality ratios of COVID-19 with mean BMI and cholesterol variables.
Table 3.
Regression coefficientsa for mutually adjusted associations between COVID-19 indixes and independent variables, age-sex-adjusted
| Model | Unstandardized Coefficients | Standardized Coefficients | t | Sig. | |
|---|---|---|---|---|---|
| B | Std. Error | Beta (β) | |||
| Incidence ratio per million (no adjusted) | |||||
| Mean BMI (kg/m2) | 4432.45 | 647.12 | .48 | 6.85 | .000 |
| Mean total cholesterol | 26,843.19 | 2693.20 | .62 | 9.97 | .000 |
| Incidence ratio per million (Full Adjusted) | |||||
| Mean BMI (kg/m2) | 2396.81 | 881.54 | .26 | 2.72 | .007 |
| Mean total cholesterol | 30,932.80 | 8371.40 | .72 | 3.70 | .000 |
| Mortality ratio per million (no adjusted) | |||||
| Mean BMI (kg/m2) | 80.38 | 12.69 | .46 | 6.33 | .000 |
| Mean total cholesterol | 439.12 | 56.33 | .53 | 7.80 | .000 |
| Mortality ratio per million (Full Adjusted) | |||||
| Mean BMI (kg/m2) | 38.18 | 18.36 | .22 | 2.08 | .040 |
| Mean total cholesterol | 417.52 | 174.40 | .50 | 2.39 | .018 |
BMI Body Mass Index, HDI Human Development Index
aadjusted for HDI, air pollution, alcohol use, tobacco, unsafe water and sanitation, handwashing facility of respiratory infections, tuberculosis diseases and prevalence of insufficient physical activity
Results revealed a positive association between the incidence ratio (per million) and mean BMI (β = 2396.81, p = 0.007) and serum cholesterol level (β = 30,932.80, p < 0.001). Also, there were positive correlations between mortality ratio (per million) with mean BMI (β = 38.18, p < 0.001) and serum cholesterol level (β = 417.52, p < 0.001). Also, regression analysis between age groups showed a robust association between COVID-19 incidence and mortality ratios with BMI and cholesterol level in countries with a median age under 20 years compared to countries with the median age between 20 and 40 and > 40 years.
Discussion
In the present national-based study, we examined the association between BMI, cholesterol level and COVID-19 incidence and mortality ratios using an ecological approach. In contrast to the previous studies suggesting an inverse correlation between obesity and mortality in patients with pneumonia and acute respiratory distress syndrome ARDS [33–35], we reported a strong positive correlation between BMI, cholesterol level and incidence and mortality due to COVID-19, even after adjusting for potential confounding factors such as air pollution, socioeconomic status and lifestyle (Table 3). With regard to BMI, our findings were consistent with the previous studies indicating the role of obesity in the severity and mortality of COVID-19 disease and its associated complications [11, 12, 36–39]. Furthermore, in line with the previous population-level studies [11–13, 40, 41], we observed a correlation between larger BMI and higher incidence and mortality of COVID-19 (Figs. 1 and 5). For example, in a study by Hendren et al. (2020), it was demonstrated that obesity is more common in the population of patients hospitalized for COVID-19 compared to ambulatory cases, especially, among those who are under the age of 50 years [11].
It should be noted that the applied BMI cut-offs might be different among countries and throughout the years, which in turn may affected the results. However, WHO has categorized countries based on the same defined cut-off points. Various studies have also shown that the BMI categorisations used by WHO and NCD-RisC has undergone negligible changes over decades for children and adults [42, 43]. Considering the role of age, we conducted a subgroup analysis for the age categories (Table 4). Results indicated that in countries with a lower median age, there is a stronger associations between COVID-19 indixes with BMI and cholesterol level (Table 4). Similarly, a cross-sectional study has reported a higher risk of in-hospital death or the need for mechanical ventilation in obese patients who were under 35 years of age [44]. In another study, Tartof et al., reported stronger associations between BMI and COVID-19 mortality in patients under the age of 60 (compared to younger population) regardless of being either outpatient or inpatient [13]. Obesity is also associated with intubation or death among patients younger than 65 years [12].
Table 4.
Association between COVID-19 indixes and independent variables by median age categories
| Independent variables | Median age < 20 years | Median age20–40 years | Median age > 40 years | |||
|---|---|---|---|---|---|---|
| R2 | β | R2 | β | R2 | β | |
| Incidence ratio per million | ||||||
| Mean BMI (kg/m2) | .663 | .814** | .141 | .376** | .156 | .395* |
| Prevalence of overweight | .768 | .877** | .198 | .445** | .244 | .494** |
| Prevalence of obesity | .764 | .874** | .160 | .400** | .162 | .403* |
| Mean total cholesterol mmol/L (2009) | .307 | .554** | .212 | .460** | .139 | .373* |
| Prevalence of cholesterol ≥5 mmol/L(2009) | .394 | .628** | .220 | .469** | .133 | .365* |
| Prevalence of cholesterol ≥6.2 mmol/L (2009) | .456 | .675** | .194 | .440** | .152 | .389* |
| Mean total cholesterol (2018) | .670 | .819** | .092 | .303* | .045 | .211 |
| Mean non-HDL cholesterol (mmol/L) (2018) | .631 | .794** | .016 | .126 | .031 | .176 |
| Mean HDL cholesterol (mmol/L) (2018) | .163 | .403 | .037 | .192 | .004 | .063 |
| Mortality ratio per million | ||||||
| Mean BMI (kg/m2) | .675 | .822** | .140 | .375** | .145 | .380* |
| Prevalence of overweight | .762 | .873** | .163 | .403** | .246 | .496** |
| Prevalence of obesity | .761 | .872** | .105 | .324** | .147 | .383* |
| Mean total cholesterol mmol/L (2009) | .327 | .572** | .081 | .284** | .047 | .217 |
| Prevalence of cholesterol ≥5 mmol/L(2009) | .423 | .650** | .085 | .292** | .052 | .228 |
| Prevalence of cholesterol ≥6.2 mmol/L (2009) | .488 | .699** | .054 | .232* | .050 | .223 |
| Mean total cholesterol (2018) | .675 | .822** | .095 | .308** | .001 | .024 |
| Mean non-HDL cholesterol (mmol/L) (2018) | .653 | .808** | .060 | .245* | .000 | .003 |
| Mean HDL cholesterol (mmol/L) (2018) | .155 | .393 | .004 | −.063 | .000 | −.005 |
BMI Body Mass Index, β standardized coefficients for regression; **P < .001, *P < .05
The possible reason for the observed association between obesity with incidence, mortality and the need for respiratory support among younger individuals is not still clear. However, one possibility is that the weaker associations of high BMI with mortality in older individuals may reflect the fact that in older patients, there is more competing life-threatening risks such as co-morbid diseases. Thus, in younger individuals, obesity and high cholesterol levels affect COVID-19 incidence rate more significantly than older individuals.
With regard to the mechanisms underlying the association between obesity and higher risk of COVID-19 infection, first, it is currently well established that obesity is associated with increased prevalence of cardiometabolic conditions such as diabetes and hypertension, that adversely complicate the therapeutic outcomes in COVID-19 patients [13, 45, 46]. Second, the virus responsible for COVID-19 disease (SARS-CoV-2), exhibits a high affinity for angiotensin-converting enzyme 2 (ACE2) in host cells which is essential for cellular resistance to infections [47]. ACE2 is widely expressed in adipose tissue; therefore, the excessive presence of fat (as we expect in obese patients) may aggravate the severity of infections [48, 49]. Third, obesity reduces the respiratory output parameters such as compliance, expiratory reserve volume and functional capacity [50]. These may worsen the severity of COVID-19 disease. Besides, there is evidence indicating that the capability of immune system to respond effectively against an infection is adversely altered in obese individuals [51–57].
Another aspect of our study addressed the correlation between cholesterol level and COVID-19 incidence and mortality ratios. Up to now, limited studies have assessed this issue in the context of COVID-19 and most of them reported that patients with more severe viral infection display lower cholesterol levels [20, 21, 23]. As for the lipoproteins, the literature is controversial. In a retrospective study conducted in Wuhan, China, it was shown that HDL and total cholesterol levels are inversely correlated with infection severity; however, serum LDL levels were found to be higher in more severe cases [58]. Another study from Wuhan has reported significantly lower total cholesterol, HDL and LDL among infected patients [59]. In addition there are findings obtained regarding other infectious diseases in this respect. For example, in a study conducted on 3961 sepsis cases, it was found that increased LDL level is associated with a higher risk of sepsis and the need for a stay in intensive care unit [60]. Lipid metabolism is critical for the virus lifecycle processes (such as endocytosis, exocytosis, replication and membrane homeostasis) [61].
Current clinical experiences from COVID-19 infection have revealed alteration in lipid metabolism after recovery of the patients, suggesting a potential biological relevance [62]. Pharmacological reduction of cholesterol has been found to suppress a type of coronavirus responsible for infectious bronchitis by disrupting lipid rafts that normally enable the virus to enter the cells [63].
Strengths and limitations
This is the first ecological study to evaluate the association of BMI and cholesterol level in the context of COVID-19 distribution. We believe our findings would help the researchers reach a broader and better understanding of the factors affecting COVID-19 incidene and mortality. Ecological studies are characterized with several appealing features such as reliance on anonymous (mostly public domain) data covering extensive geographical areas at both regional and national levels. This particularly matters when there is no available data at individual-level. In addition, the use of ecological data provides great advantage in terms of time and cost. Another benefit for this type of study is prevention of measurement error of individual-level such as air pollution exposure, age-gender-adjusted BMI, and alcoholic bevareage consumption [64, 65]. Moreover, ecological studies have also been conducted to assess the mortality patterns in different countries [66].
However, this work also faced certain limitations as follow: Considering the ecological nature of this study (ecological fallacy), data collection was large scale; therefore, individual values of BMI and cholesterol may not be thoroughly representative actual values. Moreover, COVID-19 variables, lifestyle and sociodemographic trends are described at the national level. As a result, discrepancies may exist among the population subgroups in each country. On the other hand, although obesity cut-off points were the same for all countries, this may not be precise for some regions, due to ethnic variations in reporting BMI [67]. It should be noted that BMI cut-offs for children and adolescents are different from adults, and due to the limited number and low incidence rate of COVID-19 in children and also the lack of categorization of COVID-19 data by age, the potential effects are not considered in this study. Ecological studies are generally regarded as the preliminary step of epidemiologic studies, focusing on disease prevalence amongst various populations [68]. Therefore, ecological correlation addressing the risk factors certainly requires further confirmation provided by longitudinal studies and randomized trials [65, 69, 70].
Conclusion
The incidence and mortality ratios of COVID-19 showed that in some developing and developed countries, there are significant differences with regard to age, BMI and cholesterol level. This may indicate the existance of underlying factors worldwide. However, future studies are needed to verify these possibilities more precisely. The regional variability of incidence and mortality ratios observed among different countries can be partly explained by the higher prevalence of obesity and higher cholesterol level in these areas. Collectively, our results suggest the promotion of specific health indicices (including BMI and cholesterol level) is effective to reduce the risk of COVID-19 disease. This is particularly important for developing countries with low median age.
Supplementary Information
Supplementary appendix.
Acknowledgements
The authors would like to thank the Torbat Heydariyeh University of Medical Sciences for their financial support (grant number: 99000191) and Milad Nazarzadeh in Oxford University for his insightful comments.
Abbreviations
- COVID-19
Coronavirus disease 2019
- BMI
Body Mass Index
- NCD-RisC
NCD-Risk Factor Collaboration
- WHO
World Health Organization
- GDP
Gross National Product
- GBD
Global Burden of Diseases
- HDI
Human Developlent Index
- HDL
High-Density Lipoprotein
- LDL
Low-Density Lipoprotein
- DALY
Disability-Adjusted Life Year
- ANOVA
Analysis of Variance
- UK
United Kingdom
- USA
United States of America
- IQR
Interquartile Range
- SD
Standard Deviation
- GIS
Geographic Information System
- CI
Confidence Interval
- ACE2
Angiotensin-Converting Enzyme 2
- SARS-CoV-2
Severe Acute Respiratory Syndrome Coronavirus 2
Authors’ contributions
MS: Conceptualization, Methodology, Formal analysis, Investigation, Resources, Data curation, Writing - original draft, Writing - review & editing, Supervision. S.MS: Conceptualization, Investigation, Writing - original draft, Writing - review & editing. MF: Formal analysis, Writing - original draft, Writing - review & editing. MD: Methodology, Formal analysis, Writing - original draft, Writing - review & editing. All authors read and approved the final manuscript.
Funding
This study support by the Torbat Heydariyeh University of Medical Sciences (grant number: 99000191).
Availability of data and materials
All data generated or analysed during this study are included in this published article and publicy avalable dataset. Risk factors data analyzed in this study are available in the GBD data tool: http://ghdx.healthdata.org/gbd-results-tool. The main source of BMI and cholestero data in the world was the WHO website: https://www.euro.who.int/en/health-topics/disease-prevention/nutrition/a-healthy-lifestyle/body-mass-index-bmi. Data related to the COVID-19 variables available in https://covid19.who.int/ website.
Declarations
Ethics approval and consent to participate
Ethics code (IR.THUMS.REC.1399.017) was obtained from the Ethics Committee of Torbat Heydariyeh University of Medical Sciences.
All methods were performed in accordance with the relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Mohammad Sarmadi and S. Mohammad Ahmadi-Soleimani contributed equally to this work.
Contributor Information
Mohammad Sarmadi, Email: msarmadi2@gmail.com.
S. Mohammad Ahmadi-Soleimani, Email: mostafaahmadi24@gmail.com.
References
- 1.Guan W-j, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.WHO . WHO Coronavirus Disease (COVID-19) Dashboard. 2021. [Google Scholar]
- 3.Arbel Y, Fialkoff C, Kerner A, Kerner M. Can reduction in infection and mortality rates from coronavirus be explained by an obesity survival paradox? An analysis at the US statewide level. Int J Obes (Lond) 2020;44(11):2339–2342. doi: 10.1038/s41366-020-00680-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sarmadi M, Rahimi S, Evensen D, Kazemi Moghaddam V. Interaction between meteorological parameters and COVID-19: an ecological study on 406 authorities of the UK. Environ Sci Pollut Res. 2021:16. 10.1007/s11356-021-15279-2. [DOI] [PMC free article] [PubMed]
- 5.Sarmadi, M., Moghanddam, V.K., Dickerson, A.S. et al. Association of COVID-19 distribution with air quality, sociodemographic factors, and comorbidities: an ecological study of US states. Air Qual, Atmos Health. 2020;14: 455–465. 10.1007/s11869-020-00949-w. [DOI] [PMC free article] [PubMed]
- 6.Sarmadi M, Marufi N, Moghaddam VK. Association of COVID-19 global distribution and environmental and demographic factors: an updated three-month study. Environ Res. 2020;188:109748. doi: 10.1016/j.envres.2020.109748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Li H, Xu XL, Dai DW, Huang ZY, Ma Z, Guan YJ. Air pollution and temperature are associated with increased COVID-19 incidence: a time series study. Int J Infect Dis. 2020;97:278–282. doi: 10.1016/j.ijid.2020.05.076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bolaño-Ortiz TR, Camargo-Caicedo Y, Puliafito SE, Ruggeri MF, Bolaño-Diaz S, Pascual-Flores R, Saturno J, Ibarra-Espinosa S, Mayol-Bracero OL, Torres-Delgado E, Cereceda-Balic F. Spread of SARS-CoV-2 through Latin America and the Caribbean region: a look from its economic conditions, climate and air pollution indicators. Environ Res. 2020;191:109938. doi: 10.1016/j.envres.2020.109938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Anastassopoulou C, Gkizarioti Z, Patrinos GP, Tsakris A. Human genetic factors associated with susceptibility to SARS-CoV-2 infection and COVID-19 disease severity. Hum Genomics. 2020;14(1):1–8. doi: 10.1186/s40246-020-00290-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shelton, J.F., Shastri, A.J., Ye, C. et al. Trans-ancestry analysis reveals genetic and nongenetic associations with COVID-19 susceptibility and severity. Nat Genet 53, 801–808 (2021). 10.1038/s41588-021-00854-7. [DOI] [PubMed]
- 11.Hendren NS, de Lemos JA, Ayers C, Das SR, Rao A, Carter S, Rosenblatt A, Walchok J, Omar W, Khera R, Hegde AA, Drazner MH, Neeland IJ, Grodin JL. Association of Body Mass Index and Age With Morbidity and Mortality in Patients Hospitalized With COVID-19: Results From the American Heart Association COVID-19 Cardiovascular Disease Registry. Circulation. 2021;143(2):135-144. 10.1161/CIRCULATIONAHA.120.051936. [DOI] [PubMed]
- 12.Anderson MR, Geleris J, Anderson DR, Zucker J, Nobel YR, Freedberg D, Small-Saunders J, Rajagopalan KN, Greendyk R, Chae SR, Natarajan K, Roh D, Edwin E, Gallagher D, Podolanczuk A, Barr RG, Ferrante AW, Baldwin MR. Body mass index and risk for intubation or death in SARS-CoV-2 infection: a retrospective cohort study. Ann Intern Med. 2020;173(10):782–790. doi: 10.7326/M20-3214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tartof SY, Qian L, Hong V, Wei R, Nadjafi RF, Fischer H, Li Z, Shaw SF, Caparosa SL, Nau CL, Saxena T, Rieg GK, Ackerson BK, Sharp AL, Skarbinski J, Naik TK, Murali SB. Obesity and mortality among patients diagnosed with COVID-19: results from an integrated health care organization. Ann Intern Med. 2020;173(10):773–781. doi: 10.7326/M20-3742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Aghili SMM, Ebrahimpur M, Arjmand B, Shadman Z, Pejman Sani M, Qorbani M, Larijani B, Payab M. Obesity in COVID-19 era, implications for mechanisms, comorbidities, and prognosis: a review and meta-analysis. Int J Obes (Lond) 2021;45(5):998–1016. doi: 10.1038/s41366-021-00776-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jain S, Chaves SS. Obesity and influenza. Clin Infect Dis. 2011;53(5):422–424. doi: 10.1093/cid/cir448. [DOI] [PubMed] [Google Scholar]
- 16.Kwong JC, Campitelli MA, Rosella LC. Obesity and respiratory hospitalizations during influenza seasons in Ontario, Canada: a cohort study. Clin Infect Dis. 2011;53(5):413–421. doi: 10.1093/cid/cir442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Centers for Disease Control Prevention. COVIDView: A weekly surveillance summary of US COVID-19 activity. Key updates for week 2020 [cited October 16, 2020]; Available from: https://www.cdc.gov/coronavirus/2019-ncov/covid-data/covidview/index.html.
- 18.Liu Y, Mao B, Liang S, Yang JW, Lu HW, Chai YH, et al. Association between age and clinical characteristics and outcomes of COVID-19. Eur Respir J. 2020;55(5). 10.1183/13993003.01112-2020. [DOI] [PMC free article] [PubMed]
- 19.Aung N, et al. Causal inference for genetic obesity, cardiometabolic profile and COVID-19 susceptibility: a Mendelian randomization study. Front Genet. 2020;11:1417. doi: 10.3389/fgene.2020.586308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Huang W, Li C, Wang Z, Wang H, Zhou N, Jiang J, Ni L, Zhang XA, Wang DW. Decreased serum albumin level indicates poor prognosis of COVID-19 patients: hepatic injury analysis from 2,623 hospitalized cases. Sci China Life Sci. 2020;63(11):1678–1687. doi: 10.1007/s11427-020-1733-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wang G, Zhang Q, Zhao X, Dong H, Wu C, Wu F, Yu B, Lv J, Zhang S, Wu G, Wu S, Wang X, Wu Y, Zhong Y. Low high-density lipoprotein level is correlated with the severity of COVID-19 patients: an observational study. Lipids Health Dis. 2020;19(1):1–7. doi: 10.1186/s12944-020-01382-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hu X, Chen D, Wu L, He G, Ye W. Declined serum high density lipoprotein cholesterol is associated with the severity of COVID-19 infection. Clin Chim Acta. 2020;510:105–110. doi: 10.1016/j.cca.2020.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wei X, Zeng W, Su J, Wan H, Yu X, Cao X, Tan W, Wang H. Hypolipidemia is associated with the severity of COVID-19. J Clin Lipidol. 2020;14(3):297–304. doi: 10.1016/j.jacl.2020.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Garrison RJ, Wilson PW, Castelli WP, Feinleib M, Kannel WB, McNamara PM. Obesity and lipoprotein cholesterol in the Framingham offspring study. Metabolism. 1980;29(11):1053–1060. doi: 10.1016/0026-0495(80)90216-4. [DOI] [PubMed] [Google Scholar]
- 25.Lipsitch M, Swerdlow DL, Finelli L. Defining the epidemiology of Covid-19—studies needed. N Engl J Med. 2020;382(13):1194–1196. doi: 10.1056/NEJMp2002125. [DOI] [PubMed] [Google Scholar]
- 26.Sarmadi M, Kakhki S, Foroughi M, Abadi TSH, Nayyeri S, Moghadam VK, Ramezani M. Hospitalization period of COVID-19 for future plans in hospital. Br J Surg. 2020;107(10):e427–e428. doi: 10.1002/bjs.11871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Vandenbroucke JP, von Elm E, Altman DG, Gøtzsche PC, Mulrow CD, Pocock SJ, Poole C, Schlesselman JJ, Egger M, STROBE Initiative Strengthening the reporting of observational studies in epidemiology (STROBE): explanation and elaboration. Int J Surg. 2014;12(12):1500–1524. doi: 10.1016/j.ijsu.2014.07.014. [DOI] [PubMed] [Google Scholar]
- 28.Von Elm E, et al. Strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Br Med J. 2007;335(7624):806–808. doi: 10.1136/bmj.39335.541782.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Xu Z, Yu D, Yin X, Zheng F, Li H. Socioeconomic status is associated with global diabetes prevalence. Oncotarget. 2017;8(27):44434–44439. doi: 10.18632/oncotarget.17902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.NCD Risk Factor Collaboration (NCD-RisC) DATA DOWNLOADS, Download files containing country risk factor data. 2020. [Google Scholar]
- 31.WHO . Body mass index - BMI. 2020. [Google Scholar]
- 32.Global Burden of Disease Collaborative Network . Global Burden of Disease Study 2019 (GBD 2019) results. 2020. [Google Scholar]
- 33.Zhi G, et al. “Obesity paradox” in acute respiratory distress syndrome: asystematic review and meta-analysis. PLoS One. 2016;11(9):e0163677. doi: 10.1371/journal.pone.0163677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.King P, Mortensen EM, Bollinger M, Restrepo MI, Copeland LA, Pugh MJV, Nakashima B, Anzueto A, Hitchcock Noël P. Impact of obesity on outcomes for patients hospitalised with pneumonia. Eur Respir J. 2013;41(4):929–934. doi: 10.1183/09031936.00185211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nie W, Zhang Y, Jee SH, Jung KJ, Li B, Xiu Q. Obesity survival paradox in pneumonia: a meta-analysis. BMC Med. 2014;12(1):61. doi: 10.1186/1741-7015-12-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sattar N, Ho FK, Gill JMR, Ghouri N, Gray SR, Celis-Morales CA, Katikireddi SV, Berry C, Pell JP, McMurray JJV, Welsh P. BMI and future risk for COVID-19 infection and death across sex, age and ethnicity: preliminary findings from UK biobank. Diabetes Metab Syndr Clin Res Rev. 2020;14(5):1149–1151. doi: 10.1016/j.dsx.2020.06.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jung C-Y, Park H, Kim DW, Lim H, Chang JH, Choi YJ, et al. Association between body mass index and risk of coronavirus disease 2019 (COVID-19): a nationwide case-control study in South Korea. Clin Infect Dis. 2020. 10.1093/cid/ciaa1257. [DOI] [PMC free article] [PubMed]
- 38.Nakeshbandi M, Maini R, Daniel P, Rosengarten S, Parmar P, Wilson C, Kim JM, Oommen A, Mecklenburg M, Salvani J, Joseph MA, Breitman I. The impact of obesity on COVID-19 complications: a retrospective cohort study. Int J Obes (Lond) 2020;44(9):1832–1837. doi: 10.1038/s41366-020-0648-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yates T, Razieh C, Zaccardi F, Rowlands AV, Seidu S, Davies MJ, Khunti K. Obesity, walking pace and risk of severe COVID-19 and mortality: analysis of UK biobank. Int J Obes (Lond) 2021;45(5):1155–1159. doi: 10.1038/s41366-021-00771-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Peters SA, MacMahon S, Woodward M. Obesity as a risk factor for COVID-19 mortality in women and men in the UK biobank: comparisons with influenza/pneumonia and coronary heart disease. Diabetes Obes Metab. 2021;23(1):258–262. doi: 10.1111/dom.14199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kang Z, Luo S, Gui Y, Zhou H, Zhang Z, Tian C, Zhou Q, Wang Q, Hu Y, Fan H, Hu D. Obesity is a potential risk factor contributing to clinical manifestations of COVID-19. Int J Obes (Lond) 2020;44(12):2479–2485. doi: 10.1038/s41366-020-00677-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Onis Md, et al. Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organ. 2007;85(09):660–667. doi: 10.2471/BLT.07.043497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Abarca-Gómez L, Abdeen ZA, Hamid ZA, Abu-Rmeileh NM, Acosta-Cazares B, Acuin C, Adams RJ, Aekplakorn W, Afsana K, Aguilar-Salinas CA, Agyemang C, Ahmadvand A, Ahrens W, Ajlouni K, Akhtaeva N, al-Hazzaa HM, al-Othman AR, al-Raddadi R, al Buhairan F, al Dhukair S, Ali MM, Ali O, Alkerwi A', Alvarez-Pedrerol M, Aly E, Amarapurkar DN, Amouyel P, Amuzu A, Andersen LB, Anderssen SA, Andrade DS, Ängquist LH, Anjana RM, Aounallah-Skhiri H, Araújo J, Ariansen I, Aris T, Arlappa N, Arveiler D, Aryal KK, Aspelund T, Assah FK, Assunção MCF, Aung MS, Avdicová M, Azevedo A, Azizi F, Babu BV, Bahijri S, Baker JL, Balakrishna N, Bamoshmoosh M, Banach M, Bandosz P, Banegas JR, Barbagallo CM, Barceló A, Barkat A, Barros AJD, Barros MVG, Bata I, Batieha AM, Batista RL, Batyrbek A, Baur LA, Beaglehole R, Romdhane HB, Benedics J, Benet M, Bennett JE, Bernabe-Ortiz A, Bernotiene G, Bettiol H, Bhagyalaxmi A, Bharadwaj S, Bhargava SK, Bhatti Z, Bhutta ZA, Bi H, Bi Y, Biehl A, Bikbov M, Bista B, Bjelica DJ, Bjerregaard P, Bjertness E, Bjertness MB, Björkelund C, Blokstra A, Bo S, Bobak M, Boddy LM, Boehm BO, Boeing H, Boggia JG, Boissonnet CP, Bonaccio M, Bongard V, Bovet P, Braeckevelt L, Braeckman L, Bragt MCE, Brajkovich I, Branca F, Breckenkamp J, Breda J, Brenner H, Brewster LM, Brian GR, Brinduse L, Bruno G, Bueno-de-Mesquita HB(), Bugge A, Buoncristiano M, Burazeri G, Burns C, de León AC, Cacciottolo J, Cai H, Cama T, Cameron C, Camolas J, Can G, Cândido APC, Capanzana M, Capuano V, Cardoso VC, Carlsson AC, Carvalho MJ, Casanueva FF, Casas JP, Caserta CA, Chamukuttan S, Chan AW, Chan Q, Chaturvedi HK, Chaturvedi N, Chen CJ, Chen F, Chen H, Chen S, Chen Z, Cheng CY, Chetrit A, Chikova-Iscener E, Chiolero A, Chiou ST, Chirita-Emandi A, Chirlaque MD, Cho B, Cho Y, Christensen K, Christofaro DG, Chudek J, Cifkova R, Cinteza E, Claessens F, Clays E, Concin H, Confortin SC, Cooper C, Cooper R, Coppinger TC, Costanzo S, Cottel D, Cowell C, Craig CL, Crujeiras AB, Cucu A, D'Arrigo G, d'Orsi E, Dallongeville J, Damasceno A, Damsgaard CT, Danaei G, Dankner R, Dantoft TM, Dastgiri S, Dauchet L, Davletov K, de Backer G, de Bacquer D, de Curtis A, de Gaetano G, de Henauw S, de Oliveira PD, de Ridder K, de Smedt D, Deepa M, Deev AD, Dehghan A, Delisle H, Delpeuch F, Deschamps V, Dhana K, di Castelnuovo AF, Dias-da-Costa JS, Diaz A, Dika Z, Djalalinia S, Do HTP, Dobson AJ, Donati MB, Donfrancesco C, Donoso SP, Döring A, Dorobantu M, Dorosty AR, Doua K, Drygas W, Duan JL, Duante C, Duleva V, Dulskiene V, Dzerve V, Dziankowska-Zaborszczyk E, Egbagbe EE, Eggertsen R, Eiben G, Ekelund U, el Ati J, Elliott P, Engle-Stone R, Erasmus RT, Erem C, Eriksen L, Eriksson JG, la Peña JED, Evans A, Faeh D, Fall CH, Sant'Angelo VF, Farzadfar F, Felix-Redondo FJ, Ferguson TS, Fernandes RA, Fernández-Bergés D, Ferrante D, Ferrari M, Ferreccio C, Ferrieres J, Finn JD, Fischer K, Flores EM, Föger B, Foo LH, Forslund AS, Forsner M, Fouad HM, Francis DK, Franco MC, Franco OH, Frontera G, Fuchs FD, Fuchs SC, Fujita Y, Furusawa T, Gaciong Z, Gafencu M, Galeone D, Galvano F, Garcia-de-la-Hera M, Gareta D, Garnett SP, Gaspoz JM, Gasull M, Gates L, Geiger H, Geleijnse JM, Ghasemian A, Giampaoli S, Gianfagna F, Gill TK, Giovannelli J, Giwercman A, Godos J, Gogen S, Goldsmith RA, Goltzman D, Gonçalves H, González-Leon M, González-Rivas JP, Gonzalez-Gross M, Gottrand F, Graça AP, Graff-Iversen S, Grafnetter D, Grajda A, Grammatikopoulou MG, Gregor RD, Grodzicki T, Grøntved A, Grosso G, Gruden G, Grujic V, Gu D, Gualdi-Russo E, Guallar-Castillón P, Guan OP, Gudmundsson EF, Gudnason V, Guerrero R, Guessous I, Guimaraes AL, Gulliford MC, Gunnlaugsdottir J, Gunter M, Guo X, Guo Y, Gupta PC, Gupta R, Gureje O, Gurzkowska B, Gutierrez L, Gutzwiller F, Hadaegh F, Hadjigeorgiou CA, Si-Ramlee K, Halkjær J, Hambleton IR, Hardy R, Kumar RH, Hassapidou M, Hata J, Hayes AJ, He J, Heidinger-Felso R, Heinen M, Hendriks ME, Henriques A, Cadena LH, Herrala S, Herrera VM, Herter-Aeberli I, Heshmat R, Hihtaniemi IT, Ho SY, Ho SC, Hobbs M, Hofman A, Hopman WM, Horimoto ARVR, Hormiga CM, Horta BL, Houti L, Howitt C, Htay TT, Htet AS, Htike MMT, Hu Y, Huerta JM, Petrescu CH, Huisman M, Husseini A, Huu CN, Huybrechts I, Hwalla N, Hyska J, Iacoviello L, Iannone AG, Ibarluzea JM, Ibrahim MM, Ikeda N, Ikram MA, Irazola VE, Islam M, Ismail AS, Ivkovic V, Iwasaki M, Jackson RT, Jacobs JM, Jaddou H, Jafar T, Jamil KM, Jamrozik K, Janszky I, Jarani J, Jasienska G, Jelakovic A, Jelakovic B, Jennings G, Jeong SL, Jiang CQ, Jiménez-Acosta SM, Joffres M, Johansson M, Jonas JB, Jørgensen T, Joshi P, Jovic DP, Józwiak J, Juolevi A, Jurak G, Jureša V, Kaaks R, Kafatos A, Kajantie EO, Kalter-Leibovici O, Kamaruddin NA, Kapantais E, Karki KB, Kasaeian A, Katz J, Kauhanen J, Kaur P, Kavousi M, Kazakbaeva G, Keil U, Boker LK, Keinänen-Kiukaanniemi S, Kelishadi R, Kelleher C, Kemper HCG, Kengne AP, Kerimkulova A, Kersting M, Key T, Khader YS, Khalili D, Khang YH, Khateeb M, Khaw KT, Khouw IMSL, Kiechl-Kohlendorfer U, Kiechl S, Killewo J, Kim J, Kim YY, Klimont J, Klumbiene J, Knoflach M, Koirala B, Kolle E, Kolsteren P, Korrovits P, Kos J, Koskinen S, Kouda K, Kovacs VA, Kowlessur S, Koziel S, Kratzer W, Kriemler S, Kristensen PL, Krokstad S, Kromhout D, Kruger HS, Kubinova R, Kuciene R, Kuh D, Kujala UM, Kulaga Z, Kumar RK, Kunešová M, Kurjata P, Kusuma YS, Kuulasmaa K, Kyobutungi C, la QN, Laamiri FZ, Laatikainen T, Lachat C, Laid Y, Lam TH, Landrove O, Lanska V, Lappas G, Larijani B, Laugsand LE, Lauria L, Laxmaiah A, Bao KLN, le TD, Lebanan MAO, Leclercq C, Lee J, Lee J, Lehtimäki T, León-Muñoz LM, Levitt NS, Li Y, Lilly CL, Lim WY, Lima-Costa MF, Lin HH, Lin X, Lind L, Linneberg A, Lissner L, Litwin M, Liu J, Loit HM, Lopes L, Lorbeer R, Lotufo PA, Lozano JE, Luksiene D, Lundqvist A, Lunet N, Lytsy P, Ma G, Ma J, Machado-Coelho GLL, Machado-Rodrigues AM, Machi S, Maggi S, Magliano DJ, Magriplis E, Mahaletchumy A, Maire B, Majer M, Makdisse M, Malekzadeh R, Malhotra R, Rao KM, Malyutina S, Manios Y, Mann JI, Manzato E, Margozzini P, Markaki A, Markey O, Marques LP, Marques-Vidal P, Marrugat J, Martin-Prevel Y, Martin R, Martorell R, Martos E, Marventano S, Masoodi SR, Mathiesen EB, Matijasevich A, Matsha TE, Mazur A, Mbanya JCN, McFarlane SR, McGarvey ST, McKee M, McLachlan S, McLean RM, McLean SB, McNulty BA, Yusof SM, Mediene-Benchekor S, Medzioniene J, Meirhaeghe A, Meisfjord J, Meisinger C, Menezes AMB, Menon GR, Mensink GBM, Meshram II, Metspalu A, Meyer HE, Mi J, Michaelsen KF, Michels N, Mikkel K, Miller JC, Minderico CS, Miquel JF, Miranda JJ, Mirkopoulou D, Mirrakhimov E, Mišigoj-Durakovic M, Mistretta A, Mocanu V, Modesti PA, Mohamed MK, Mohammad K, Mohammadifard N, Mohan V, Mohanna S, Yusoff MFM, Molbo D, Møllehave LT, Møller NC, Molnár D, Momenan A, Mondo CK, Monterrubio EA, Monyeki KDK, Moon JS, Moreira LB, Morejon A, Moreno LA, Morgan K, Mortensen EL, Moschonis G, Mossakowska M, Mostafa A, Mota J, Mota-Pinto A, Motlagh ME, Motta J, Mu TT, Muc M, Muiesan ML, Müller-Nurasyid M, Murphy N, Mursu J, Murtagh EM, Musil V, Nabipour I, Nagel G, Naidu BM, Nakamura H, Námešná J, Nang EEK, Nangia VB, Nankap M, Narake S, Nardone P, Navarrete-Muñoz EM, Neal WA, Nenko I, Neovius M, Nervi F, Nguyen CT, Nguyen ND, Nguyen QN, Nieto-Martínez RE, Ning G, Ninomiya T, Nishtar S, Noale M, Noboa OA, Norat T, Norie S, Noto D, Nsour MA, O'Reilly D, Obreja G, Oda E, Oehlers G, Oh K, Ohara K, Olafsson Ö, Olinto MTA, Oliveira IO, Oltarzewski M, Omar MA, Onat A, Ong SK, Ono LM, Ordunez P, Ornelas R, Ortiz AP, Osler M, Osmond C, Ostojic SM, Ostovar A, Otero JA, Overvad K, Owusu-Dabo E, Paccaud FM, Padez C, Pahomova E, Pajak A, Palli D, Palloni A, Palmieri L, Pan WH, Panda-Jonas S, Pandey A, Panza F, Papandreou D, Park SW, Parnell WR, Parsaeian M, Pascanu IM, Patel ND, Pecin I, Pednekar MS, Peer N, Peeters PH, Peixoto SV, Peltonen M, Pereira AC, Perez-Farinos N, Pérez CM, Peters A, Petkeviciene J, Petrauskiene A, Peykari N, Pham ST, Pierannunzio D, Pigeot I, Pikhart H, Pilav A, Pilotto L, Pistelli F, Pitakaka F, Piwonska A, Plans-Rubió P, Poh BK, Pohlabeln H, Pop RM, Popovic SR, Porta M, Portegies MLP, Posch G, Poulimeneas D, Pouraram H, Pourshams A, Poustchi H, Pradeepa R, Prashant M, Price JF, Puder JJ, Pudule I, Puiu M, Punab M, Qasrawi RF, Qorbani M, Bao TQ, Radic I, Radisauskas R, Rahman M, Rahman M, Raitakari O, Raj M, Rao SR, Ramachandran A, Ramke J, Ramos E, Ramos R, Rampal L, Rampal S, Rascon-Pacheco RA, Redon J, Reganit PFM, Ribas-Barba L, Ribeiro R, Riboli E, Rigo F, de Wit TFR, Rito A, Ritti-Dias RM, Rivera JA, Robinson SM, Robitaille C, Rodrigues D, Rodríguez-Artalejo F, del Cristo Rodriguez-Perez M, Rodríguez-Villamizar LA, Rojas-Martinez R, Rojroongwasinkul N, Romaguera D, Ronkainen K, Rosengren A, Rouse I, Roy JGR, Rubinstein A, Rühli FJ, Ruiz-Betancourt BS, Russo P, Rutkowski M, Sabanayagam C, Sachdev HS, Saidi O, Salanave B, Martinez ES, Salmerón D, Salomaa V, Salonen JT, Salvetti M, Sánchez-Abanto J, Sandjaja, Sans S, Marina LS, Santos DA, Santos IS, Santos O, dos Santos RN, Santos R, Saramies JL, Sardinha LB, Sarrafzadegan N, Saum KU, Savva S, Savy M, Scazufca M, Rosario AS, Schargrodsky H, Schienkiewitz A, Schipf S, Schmidt CO, Schmidt IM, Schultsz C, Schutte AE, Sein AA, Sen A, Senbanjo IO, Sepanlou SG, Serra-Majem L, Shalnova SA, Sharma SK, Shaw JE, Shibuya K, Shin DW, Shin Y, Shiri R, Siani A, Siantar R, Sibai AM, Silva AM, Silva DAS, Simon M, Simons J, Simons LA, Sjöberg A, Sjöström M, Skovbjerg S, Slowikowska-Hilczer J, Slusarczyk P, Smeeth L, Smith MC, Snijder MB, So HK, Sobngwi E, Söderberg S, Soekatri MYE, Solfrizzi V, Sonestedt E, Song Y, Sørensen TIA, Soric M, Jérome CS, Soumare A, Spinelli A, Spiroski I, Staessen JA, Stamm H, Starc G, Stathopoulou MG, Staub K, Stavreski B, Steene-Johannessen J, Stehle P, Stein AD, Stergiou GS, Stessman J, Stieber J, Stöckl D, Stocks T, Stokwiszewski J, Stratton G, Stronks K, Strufaldi MW, Suárez-Medina R, Sun CA, Sundström J, Sung YT, Sunyer J, Suriyawongpaisal P, Swinburn BA, Sy RG, Szponar L, Tai ES, Tammesoo ML, Tamosiunas A, Tan EJ, Tang X, Tanser F, Tao Y, Tarawneh MR, Tarp J, Tarqui-Mamani CB, Tautu OF, Braunerová RT, Taylor A, Tchibindat F, Theobald H, Theodoridis X, Thijs L, Thuesen BH, Tjonneland A, Tolonen HK, Tolstrup JS, Topbas M, Topór-Madry R, Tormo MJ, Tornaritis MJ, Torrent M, Toselli S, Traissac P, Trichopoulos D, Trichopoulou A, Trinh OTH, Trivedi A, Tshepo L, Tsigga M, Tsugane S, Tulloch-Reid MK, Tullu F, Tuomainen TP, Tuomilehto J, Turley ML, Tynelius P, Tzotzas T, Tzourio C, Ueda P, Ugel EE, Ukoli FAM, Ulmer H, Unal B, Uusitalo HMT, Valdivia G, Vale S, Valvi D, van der Schouw YT, van Herck K, van Minh H, van Rossem L, van Schoor NM, van Valkengoed IGM, Vanderschueren D, Vanuzzo D, Vatten L, Vega T, Veidebaum T, Velasquez-Melendez G, Velika B, Veronesi G, Verschuren WMM, Victora CG, Viegi G, Viet L, Viikari-Juntura E, Vineis P, Vioque J, Virtanen JK, Visvikis-Siest S, Viswanathan B, Vlasoff T, Vollenweider P, Völzke H, Voutilainen S, Vrijheid M, Wade AN, Wagner A, Waldhör T, Walton J, Bebakar WMW, Mohamud WNW, Wanderley RS, Jr, Wang MD, Wang Q, Wang YX, Wang YW, Wannamethee SG, Wareham N, Weber A, Wedderkopp N, Weerasekera D, Whincup PH, Widhalm K, Widyahening IS, Wiecek A, Wijga AH, Wilks RJ, Willeit J, Willeit P, Wilsgaard T, Wojtyniak B, Wong-McClure RA, Wong JYY, Wong JE, Wong TY, Woo J, Woodward M, Wu FC, Wu J, Wu S, Xu H, Xu L, Yamborisut U, Yan W, Yang X, Yardim N, Ye X, Yiallouros PK, Yngve A, Yoshihara A, You QS, Younger-Coleman NO, Yusoff F, Yusoff MFM, Zaccagni L, Zafiropulos V, Zainuddin AA, Zambon S, Zampelas A, Zamrazilová H, Zdrojewski T, Zeng Y, Zhao D, Zhao W, Zheng W, Zheng Y, Zholdin B, Zhou M, Zhu D, Zhussupov B, Zimmermann E, Cisneros JZ, Bentham J, di Cesare M, Bilano V, Bixby H, Zhou B, Stevens GA, Riley LM, Taddei C, Hajifathalian K, Lu Y, Savin S, Cowan MJ, Paciorek CJ, Chirita-Emandi A, Hayes AJ, Katz J, Kelishadi R, Kengne AP, Khang YH, Laxmaiah A, Li Y, Ma J, Miranda JJ, Mostafa A, Neovius M, Padez C, Rampal L, Zhu A, Bennett JE, Danaei G, Bhutta ZA, Ezzati M. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet. 2017;390(10113):2627–2642. doi: 10.1016/S0140-6736(17)32129-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cunningham JW, et al. Clinical outcomes in young US adults hospitalized with COVID-19. JAMA Intern Med. 2021181(3):379-381. 10.1001/jamainternmed.2020.5313. [DOI] [PMC free article] [PubMed]
- 45.Zhou F, Yu T, du R, Fan G, Liu Y, Liu Z, Xiang J, Wang Y, Song B, Gu X, Guan L, Wei Y, Li H, Wu X, Xu J, Tu S, Zhang Y, Chen H, Cao B. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Mokdad AH, Ford ES, Bowman BA, Dietz WH, Vinicor F, Bales VS, Marks JS. Prevalence of obesity, diabetes, and obesity-related health risk factors, 2001. Jama. 2003;289(1):76–79. doi: 10.1001/jama.289.1.76. [DOI] [PubMed] [Google Scholar]
- 47.Hendren NS, Drazner MH, Bozkurt B, Cooper LT., Jr Description and proposed management of the acute COVID-19 cardiovascular syndrome. Circulation. 2020;141(23):1903–1914. doi: 10.1161/CIRCULATIONAHA.120.047349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kassir R. Risk of COVID-19 for patients with obesity. Obes Rev. 2020;21(6):e13034. doi: 10.1111/obr.13034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Al-Benna S. Association of high level gene expression of ACE2 in adipose tissue with mortality of COVID-19 infection in obese patients. Obes Med. 2020;19:100283. doi: 10.1016/j.obmed.2020.100283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Gong MN, Bajwa EK, Thompson BT, Christiani DC. Body mass index is associated with the development of acute respiratory distress syndrome. Thorax. 2010;65(1):44–50. doi: 10.1136/thx.2009.117572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Huttunen R, Syrjänen J. Obesity and the risk and outcome of infection. Int J Obes (Lond) 2013;37(3):333–340. doi: 10.1038/ijo.2012.62. [DOI] [PubMed] [Google Scholar]
- 52.Peters MC, McGrath K, Hawkins GA, Hastie AT, Levy BD, Israel E, Phillips BR, Mauger DT, Comhair SA, Erzurum SC, Johansson MW, Jarjour NN, Coverstone AM, Castro M, Holguin F, Wenzel SE, Woodruff PG, Bleecker ER, Fahy JV, National Heart, Lung, and Blood Institute Severe Asthma Research Program Plasma interleukin-6 concentrations, metabolic dysfunction, and asthma severity: a cross-sectional analysis of two cohorts. Lancet Respir Med. 2016;4(7):574–584. doi: 10.1016/S2213-2600(16)30048-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Zhang X, et al. Allergy & Asthma Proceedings. 2018. Systemic inflammation mediates the detrimental effects of obesity on asthma control. [DOI] [PubMed] [Google Scholar]
- 54.Nieman DC, et al. Influence of obesity on immune function. J Am Diet Assoc. 1999;99(3):294–299. doi: 10.1016/S0002-8223(99)00077-2. [DOI] [PubMed] [Google Scholar]
- 55.Francisco V, Pino J, Campos-Cabaleiro V, Ruiz-Fernández C, Mera A, Gonzalez-Gay MA, Gómez R, Gualillo O. Obesity, fat mass and immune system: role for leptin. Front Physiol. 2018;9:640. doi: 10.3389/fphys.2018.00640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Sheridan PA, Paich HA, Handy J, Karlsson EA, Hudgens MG, Sammon AB, Holland LA, Weir S, Noah TL, Beck MA. Obesity is associated with impaired immune response to influenza vaccination in humans. Int J Obes (Lond) 2012;36(8):1072–1077. doi: 10.1038/ijo.2011.208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Solt CM, et al. Obesity-induced immune dysfunction and immunosuppression: TEM observation of visceral and subcutaneous lymph node microarchitecture and immune cell interactions. Horm Mol Biol Clin Invest. 2019;39(14). 10.1515/hmbci-2018-0083. [DOI] [PubMed]
- 58.Wei C, et al. Cholesterol metabolism--impact for SARS-CoV-2 infection prognosis, entry, and antiviral therapies. MedRxiv.2020. 25p. 10.1101/2020.04.16.20068528.
- 59.Hu X, et al. Low serum cholesterol level among patients with COVID-19 infection in Wenzhou, China. SSRN. 2020; 21. 10.2139/ssrn.3544826. [DOI]
- 60.Feng Q, Wei WQ, Chaugai S, Leon BGC, Mosley JD, Leon DAC, et al. Association between low-density lipoprotein cholesterol levels and risk for sepsis among patients admitted to the hospital with infection. JAMA Netw Open. 2019;2(1):–e187223. 10.1001/jamanetworkopen.2018.7223. [DOI] [PMC free article] [PubMed]
- 61.Abu-Farha M, Thanaraj TA, Qaddoumi MG, Hashem A, Abubaker J, al-Mulla F. The role of lipid metabolism in COVID-19 virus infection and as a drug target. Int J Mol Sci. 2020;21(10):3544. doi: 10.3390/ijms21103544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Wu Q, Zhou L, Sun X, Yan Z, Hu C, Wu J, Xu L, Li X, Liu H, Yin P, Li K, Zhao J, Li Y, Wang X, Li Y, Zhang Q, Xu G, Chen H. Altered lipid metabolism in recovered SARS patients twelve years after infection. Sci Rep. 2017;7(1):1–12. doi: 10.1038/s41598-017-09536-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Guo H, Huang M, Yuan Q, Wei Y, Gao Y, Mao L, Gu L, Tan YW, Zhong Y, Liu D, Sun S. The important role of lipid raft-mediated attachment in the infection of cultured cells by coronavirus infectious bronchitis virus beaudette strain. PLoS One. 2017;12(1):e0170123. doi: 10.1371/journal.pone.0170123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Susser M. The logic in ecological: I. The logic of analysis. Am J Public Health. 1994;84(5):825–829. doi: 10.2105/AJPH.84.5.825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Neumark Y. What can ecological studies tell us about death? Isr J Health Policy Res. 2017;6(1):52. doi: 10.1186/s13584-017-0176-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Ginsberg GM, Tulchinsky TH, Salahov E, Clayman M. Standardized mortality ratios by region of residence, Israel, 1987-1994: a tool for public health policy. Public Health Rev. 2003;31(2):111–131. [PubMed] [Google Scholar]
- 67.Oggioni C, Cena H, Wells JCK, Lara J, Celis-Morales C, Siervo M. Association between worldwide dietary and lifestyle patterns with total cholesterol concentrations and DALYs for infectious and cardiovascular diseases: an ecological analysis. J Epidemiol Glob Health. 2015;5(4):315–325. doi: 10.1016/j.jegh.2015.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Munnangi S, Boktor SW. Epidemiology of study design. 2017. [PubMed] [Google Scholar]
- 69.Pearce N. The ecological fallacy strikes back. J Epidemiol Community Health. 2000;54(5):326–327. doi: 10.1136/jech.54.5.326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Barratt H, Kirwan M. Public Health Textbook: Research methods appropriate to public health practice, including epidemiology, statistical methods and other methods of enquiry including qualitative research methods. 2009. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary appendix.
Data Availability Statement
All data generated or analysed during this study are included in this published article and publicy avalable dataset. Risk factors data analyzed in this study are available in the GBD data tool: http://ghdx.healthdata.org/gbd-results-tool. The main source of BMI and cholestero data in the world was the WHO website: https://www.euro.who.int/en/health-topics/disease-prevention/nutrition/a-healthy-lifestyle/body-mass-index-bmi. Data related to the COVID-19 variables available in https://covid19.who.int/ website.