Abstract
Background:
After serious postoperative complications, patients and families may experience conflict about goals of care.
Methods:
We performed a multisite randomized clinical trial to test the effect of a question prompt list on postoperative conflict. We interviewed family members and patients age ≥ 60 who experienced serious complications. We used qualitative content analysis to analyze conflict and characterize patient experiences with complications.
Results:
Fifty-six of 446 patients suffered a serious complication. Participants generally did not report conflict relating to postoperative treatments and expressed support for the care they received. We did not appreciate a difference in conflict between intervention and usual care. Respondents reported feeling unprepared for complications, witnessing heated interactions among team members, and a failure to develop trust for their surgeon preoperatively.
Conclusion:
Postoperative conflict following serious complications is well described but its incidence may be low. Nonetheless, patient and family observations reveal opportunities for improvement.
Keywords: Postoperative conflict, surgical complications, high-risk surgery, older adults, goals of care
Introduction
Older adults considering major surgery have an increased risk for serious postoperative complications, intensive care, prolonged hospitalization and death. [1, 2] While surgery may improve symptoms, restore function, or even prolong life, it may also lead to unwanted outcomes, decreased quality of life or care that is inconsistent with personal preferences and goals. Preoperative conversations infrequently address what to do in the setting of unwanted outcomes when the original goals of surgery are no longer achievable. [3] As such, it is often unclear how to care for older patients who may not tolerate certain health states or burdensome treatments. Family members and patients who find their expectations for surgery unrealized may then face unwanted procedures or unacceptable changes in cognition or physical function.
Within the framework of informed consent, surgeons routinely disclose the risks of surgery and their expectations for patient recovery, but patients may find it difficult to translate a list of risks into a range of possible outcomes. This can lead to a disconnect between surgeon and patient; because the patient has agreed to proceed with surgery the surgeon believes the patient has also committed to any additional postoperative treatments required for survival, regardless of the burdens of these treatments or the functional outcome. This phenomenon known as “surgical buy-in” [4] can lead to conflict in the setting of serious postoperative complications as patients or their families may wish to withhold or withdraw therapies to which surgeon believes they previously agreed. [5–7]
Conflict about treatment limitations and end-of-life care is well described, with over 70% of ICU clinicians reporting frequent experiences of conflict with other clinicians or patients and family members. [8–10] A national survey of surgeons found 43% of respondents reported experiencing conflict related to life-supporting treatments and disagreement about their patient’s goals of care postoperatively. [11] While most conflict is between family members and clinicians or among members of the healthcare team, intrapersonal conflict also exists wherein family members, and sometimes patients, struggle to navigate patient care and question their own decisions. [12] ICU conflict negatively impacts patient safety and quality of care [10, 13] with consequences that include prolonged ICU stay, decreased quality of life for surrogate decision makers [14], negative health effects on survivors [15, 16] e.g., depression, post-traumatic stress disorder, and clinician burnout. [10]
To address this problem, we worked with surgeons, patients and family stakeholders to develop a question prompt list (QPL) intervention [17] that specifically targets, among other things, the occurrence of serious postoperative complications and how to care for the patient in the event that the patient can no longer care or make decisions for themselves. This tri-fold brochure (Supplement A) is sent to patients prior to their outpatient consultation with a surgeon and includes questions such as “Can you describe serious complications and explain what those might mean for me?” We theorized that patients who used the QPL during their preoperative visit might experience less postoperative conflict related to additional life-supporting treatments and goals of care than patients who did not receive the QPL. Because the incidence of serious postoperative complications is low, even for high-risk patients, we planned a comparative qualitative study to characterize patient experiences. The objective of this study was to test the effectiveness of the QPL on conflict about treatments and goals of care following serious postoperative complications. When we found there was limited evidence of postoperative conflict, we aimed to characterize the postoperative experiences of patients who had serious complications.
Methods
Design
We conducted a pragmatic multisite randomized clinical trial testing the effectiveness of a QPL intervention on preoperative communication, psychological well-being and postoperative conflict. The QPL includes 11 questions about treatment options, expectations for recovery, and complication management. We used a stepped-wedged design to allow for sequential QPL implementation. With this study design patients were randomly assigned to receive the QPL brochure prior to their outpatient surgical consultation or usual care based on the timing of their visit with the study surgeon who at that time was assigned usual care or had crossed over to the intervention group. We previously reported the modest effect of the QPL intervention on outcomes related to patient and family engagement and well-being. [18] Participating study sites included Oregon Health & Science University, University of California San Francisco, University of Wisconsin Hospital and Clinics, Rutgers University Hospital and Brigham and Women’s Hospital. The Institutional Review Board at each site approved this study, all participants provided written informed consent and the study was registered at ClinicalTrails.gov (NCT02623335).
Study Participants
We used purposeful sampling to ensure variation in surgical specialty and then randomly selected 40 surgeons across participating study sites (1–2 surgeons per specialty) who routinely perform high-risk surgery in older adults. High-risk surgery for older adults includes operations with a 30-day in-hospital mortality rate of 1% or greater. [19] We excluded surgeons who perform mostly low-risk procedures as serious postoperative complications were unlikely. We enrolled patients age ≥60 with one or more chronic conditions who met with a study-enrolled surgeon to discuss surgery for a major oncological or vascular problem. We identified a subgroup of patients who experienced serious complications [20] including prolonged hospitalization (>8 days) and/or prolonged intensive care (>3 days) and their family members and invited them for an interview and a $25 incentive (per respondent). We excluded patients and family members who were not proficient in English or Spanish and study-enrolled patients who did not go on to have surgery.
Data Collection
Trained study personnel conducted in person or by telephone interviews, which were audio-recorded and transcribed verbatim. The interview script included questions related to the following four domains: patient’s values and goals, treatment decision making, relationships between clinicians and patient or family and conflict (Supplement B). Additionally, interviewers were briefed about the phenomenon of surgical buy-in and how this could lead to conflict in the setting of serious postoperative complications. We also examined data collected for other study outcomes including audio-recorded preoperative decision-making conversations with the surgeon and patient and family members and chart abstraction from the date of enrollment until 6 weeks postoperatively.
Analysis
We used content analysis to analyze interviews with patients and/or family members. Three investigators (MLS, AB, AK) independently reviewed the interview transcripts, generating codes to describe and catalogue key concepts in the text. Transcripts were then conjointly reviewed by at least two investigators who discussed each code, considering how coding discordance exposed different perspectives on the data. We used NVivo 10 (QSR International), qualitative research software, to store coded transcripts. We then created context charts to facilitate higher level analysis [21] and compare similarities and differences between usual care and intervention group interviews. To further our understanding of postoperative conflict and the experience of postoperative complications we triangulated data by linking the postoperative interview transcript with chart abstraction and the transcript of the initial outpatient surgical consultation.
Results
Sample Characteristics
Two hundred and thirteen of the 446 patients enrolled in the primary study went on to have a high-risk oncological or vascular operation. Five patients died postoperatively during the data collection period, but only 2 of these patients died within 30 days of their index operation. Fifty-six patients experienced at least one serious postoperative complication, prolonged hospitalization (>8 days) and/or prolonged ICU stay (>3 days). Of the 56 eligible patients, we approached 34 patients and/or family members for an open-ended interview. We were unable to approach 22 patients for an interview because (1) the patient was functionally or cognitively impaired and their family was not enrolled in the study, (2) research staff appreciated or anticipated distress about study participation and (3) qualifying participants were not identified as eligible in time to perform an interview. Six patients or family members declined to participate, and 7 patients or family members could not be reached despite repeated attempts. We conducted 21 open-ended interviews and had one missing audio file (Figure 1).
Figure 1.
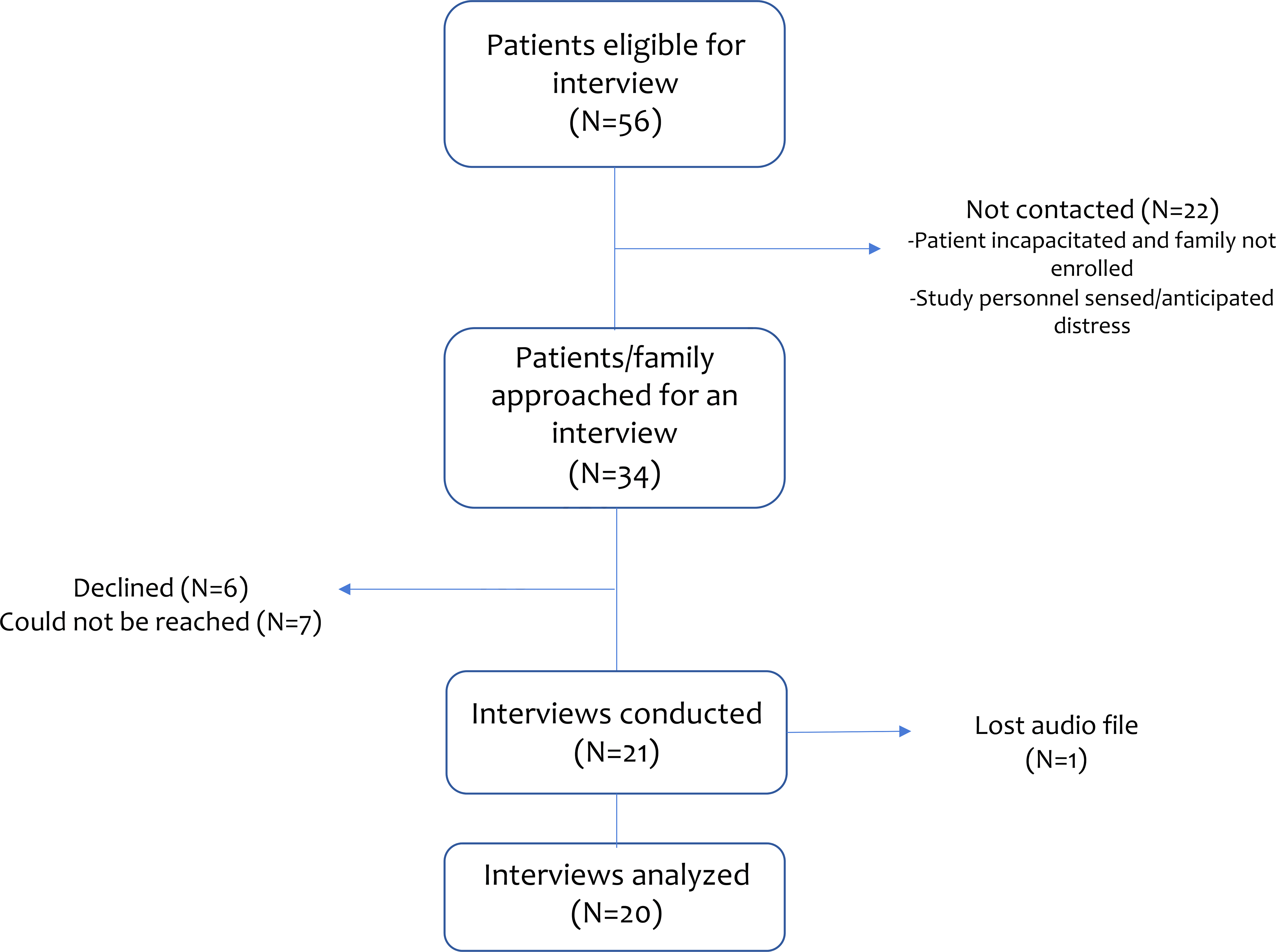
CONSORT Diagram for Patient Interviews
Interviews included patients together with their family members (N=10), patients alone (N=8) and family members alone (N=2). There were 8 patients in the control group and 12 patients in the QPL intervention group. The mean age was 71 and participants were mainly white (90%) and male (65%). All patients suffered one or more serious postoperative complication and 2 patients died within 30 days of surgery (Table 1). Serious postoperative complications included cardiac arrest, hemorrhage requiring reoperation, initiation of dialysis and prolonged mechanical ventilation.
Table 1.
Qualifying characteristics of patients who participated or whose family members participated in interviews
| Characteristic | Total (%) N=20 |
|---|---|
|
| |
| Study Arm | |
| Control | 8 (40) |
| Intervention | 12 (60) |
|
| |
| Age: mean (range) | 71(60–86) |
|
| |
| Gender | |
| Male | 13 (65) |
|
| |
| Race | |
| White or Caucasian | 18 (90) |
| Black or African American | 1 (5) |
| Asian | 1 (5) |
| Other | 0 |
|
| |
| Surgical Indication | |
| Cardiac | 2 (10) |
| Colorectal | 3 (15) |
| Hepatobiliary | 6 (30) |
| Neurosurgical | 1 (5) |
| Thoracic | 7 (35) |
| Otolaryngology | 1 (5) |
|
| |
| Charlson Comorbidity Score: mean (sd) | 5.5 (2.2) |
|
| |
| Complications a | |
| Cardiovascular | 10 |
| Pulmonary | 14 |
| Infectious | 4 |
| Hemorrhage | 5 |
| Renal | 6 |
| Death | 2 |
|
| |
| Prolonged length of Stay b | |
| Hospitalization | 12 |
| ICU care | 5 |
sd: standard deviation
Cardiovascular: Myocardial infarction, deep venous thrombosis, heart failure, arrythmia, pericardial effusion requiring intervention
Pulmonary: Pulmonary embolism, pneumonia, unplanned intubation, respiratory failure, prolonged mechanical ventilation, pleural effusion requiring intervention
Infectious: septic shock, surgical site infection
Hemorrhage: Postoperative bleeding requiring intervention
Renal: Acute renal failure requiring dialysis, renal insufficiency, urinary tract infection
Prolonged hospitalization defined as LOS > 8 days postoperatively. Prolonged ICU care defined as LOS in intensive care > 3 days postoperatively.
Effect of the QPL on postoperative conflict
We did not appreciate a difference between respondents in the intervention or usual care groups. Participants described how unprepared they felt for unwanted outcomes, but only a few participants experienced conflict between themselves and the care team relating to management of postoperative complications. Some also reported episodes of conflict among members of their treatment team that they described as filled with animosity or hostility. Most respondents experienced little conflict related to their care and ultimately survived a difficult postoperative course; they expressed overwhelming support and appreciation for the care they received.
Anticipating Complications
Respondents reflected on complications with either acceptance or disbelief. Some were seemingly dispassionate and reported they did not feel letdown when complications occurred. This detachment from their experience stemmed from a perception of a protective or covenantal relationship with their surgeon. “They [surgeon] are the professional who knows what they’re doing and we [patient] are along for the ride.” Some respondents assumed an even more positive view about their care in the face of serious complications. They viewed unwanted outcomes as a tradeoff for the hope of life-prolonging surgery. Because they had full faith in the treating team, and at times noted they intentionally neglected to learn about unwanted outcomes preoperatively, they trusted medical professionals to make decisions on their behalf, assuming they would know what was best.
In contrast, some participants felt uninformed and unprepared for surgical complications (Table 2). While the risks of surgery and expectations for recovery were discussed during their preoperative visit, they struggled to convert a list of risks into imaginable outcomes—for example, that the risk of bleeding may require a second operation, or that the risk of infection may mean life-threatening sepsis. They were frustrated because they had been apprised about the occurrence or even management of surgical risks and complications but felt unaware of what the experience might entail for the patient in both the short and long term. Thus, when complications occurred, they felt lost and ill-equipped. At times, patients or family transferred these negative emotions to the surgeon who they blamed for the surprise of a bad outcome.
Table 2.
Participant Reflections on Postoperative Experiences Illustrative Quotes
| Illustrative Quotes | |
|---|---|
| Postoperative complications were difficult to anticipate based on their preoperative discussion | Family Member: He had drains in his neck he had drains in his arm this was all built up he had, bandages on his legs where they did the skin grafts and, you know the holes and the tubes and the, it was, freaking scary! I was not prepared... None whatsoever! ...None whatsoever. |
| Family Member: They never told us how long the surgery would be...But, at NO time was I prepared for...what was involved at all. At ALL!. And like I said I walked in there [after the patient had surgery] and I walked out crying’, the nurse looked at me and I go, “I, I can’t handle this! ...I cannot handle this.” You know? | |
| Family Member: We just didn’t, you had to think about it because the doctor did say that recovery would be long, but we didn’t realize that it would take so long to get her back on her feet. She had nurses come and, and be with her every day for a while and physical therapy. | |
| Patient: [Reflecting on risks of surgery] And uh, I was prepared for those in my, in my brain. The reality sometimes is harsher... | |
| Patient: No, I guess I, you know the way the surgeon talked I would be cancer free and uh, get my strength back and go on about my business and that’s, that’s all I wanted I just wanted to uh, get it done and over with and uh, uh, be cancer free uh, be pain free, not have any problems. You know it’s been, 117 days since I took any food or drink in my mouth. | |
|
Interviewer: Okay. Can you tell me a little bit more about, you say return to health, kind of what that means to you? What kind of things were you hoping to be able to return to? Patient: Being able to be independent, to thrive, to do things with friends, play with my grandchildren. None of which I can do now. Interviewer: Were you aware that that could potentially be an outcome? Like the- in the conversations that you had with your surgeon prior to the surgery? Patient: No. |
Decisions about Life-supporting Treatments
The few family members and patients who experienced postoperative complications requiring prolonged mechanical ventilation or artificial nutrition, reported that that they were “on the same page as the healthcare team.” They believed their goals of care were obtainable and found themselves aligned with the care team in their efforts to achieve the patient’s survival. Even participants who felt blindsided by the event of a serious complication, did not report antagonism between themselves and the surgical team when making decisions about additional interventions. One family member of a patient who required life-support following postoperative cardiac arrest, reported feeling confused and devastated by this outcome—the surgeon had discussed the risks of surgery including death, but the family member never imagined that the worst case scenario could happen. Despite this sadness, the family member and surgical team found themselves in agreement to withdraw life-sustaining treatment. The family member had discussed preferences for end-of-life care with the patient prior to surgery, and felt confident about the patient’s preferences, while the surgical team recognized the patient’s unlikely chance for recovery.
Conflict Between Clinicians
Respondents reported conflict among members of the teams involved in their care (Table 3). This conflict stemmed from ownership over decision making, dispute about how to best treat a specific problem or perceived pre-existing hostility. One patient witnessed animosity between specialty teams during an intense, life threatening complication. At this time, the surgeon expressed disapproval of the approach of the non-surgical clinicians and declared ownership of the patient’s care, noting that all further interventions would be dictated by the surgeon. Several respondents recalled similar episodes of conflict or hostility related to treatment recommendations from non-surgical teams and clinicians. Participants noted they were not the target of these episodes of conflict, but they felt directly affected by the disagreements among clinicians. Consequently, they were left with contradictory information that contributed to internal turmoil about whose opinion to support. They also described intra-team conflict among healthcare workers during uneventful day-to-day experiences of their hospitalization. One participant noted a “general hostility between radiology and other people,” while another noted a “disconnect between the nurses and physician.” While these situations didn’t always impact patient care, respondents felt that these interactions were noxious, adding stress to an already difficult time.
Table 3.
Patient and Family Reflections on Intra-team Dispute and Disagreement
| Illustrative Quotes | |
|---|---|
| Patients and family perceived negative intra-team interactions and exchanges affecting patient care | Family Member]: People were doing things without consulting him [surgeon] and he, laid down the law. He actually came in to see him [patient]. But on Thursday he looks at me and he said “there are a lot of good doctors here. But I want to be notified of anything, any change at all you will call my office first. I am in charge.” |
| Patient: There seemed to be a...general hostility between radiology and other people. I got the sense that other people had experienced it too and...all the eleven days I was in the hospital, I think I had x-rays six times. Only once did they actually come up to the room. Even though I know the doctors ordered [X-rays] it came to be a joke between me and the doctors. | |
| Patient: Uh, the doctors would come in and this and that, and um, it did seem to be a disconnect in other people’s care between doctors and nurses. And I, I can’t speak to what it is—But, I got the feeling from what I was hearing that there wasn’t a coordinated effort. | |
| Family Member: ...sometimes I get the feeling that the oncologist thinks, ‘Okay. [DOCTOR] did the surgery, he’s done, he’s out of things now. I don’t need to communicate back to [him], I’m in charge.’ And I still think it needs to be all of them working together. |
Concerns about preoperative communication
Although our interview focused on postoperative complications, several respondents raised issues they encountered preoperatively (Table 4). During the preoperative visit they felt that the surgeon was rushed or did not attend to their preferences or needs. Because of this, they struggled to generate trust for their surgeon which had a downstream impact on their relationship, as they felt cynical and wary about their surgeon’s subsequent recommendations for care. For an example, one family member noted that their surgical consultation felt “glossed over” and that their preoperative preparation was haphazard, calling it a “circus” This made them feel unsure about whether they were receiving the right care or if their surgeon had done an acceptable job. These feelings became exacerbated when complications and unwanted outcomes occurred, generating treatment-related regret and mistrust. Interaction
Table 4.
Patient and Family Descriptions of Troublesome Preoperative Interactions
| Illustrative Quotes | |
|---|---|
| Patients and family members described preoperative interactions that led to mistrust of the surgeon | Family Member: “And, we’re setting you up, we’ll have lab, and you’ll be doing your first chemo the end of this week”. It was just, and she was out of the room gone. My daughter looks at me and, so then when we went in for the actual chemo I said to the nurse, I said, “may I have a copy of the PET scan please?” And that’s when I found out all of the other places it [the cancer] is. So, a doctor has not even explained that to us. I was not real happy. |
| Patient: I felt, he was telling me, “forget about the tissue valve, it’s gonna be mechanical and to back up what I’m saying Dr. [XXX] is gonna come in and tell you the same thing. He was implying it would be foolish to not get the mechanical valve... He [clinician] was basically telling me I didn’t know what I was talking about because I wanted a tissue valve. I think he was trying to help us make a good decision, but it didn’t come across that way. | |
| Family Member: And, there, and again, there was NO preparation for what was gonna go through with this [post-op] chemo and radiation either. Don’t gloss over it. And again, you know hindsight, at the time I was furious, how can you just schedule this thing you don’t know, what’s the, what’s in him and that was my biggest thing why put somebody through it? If it was in his liver if it was in his lungs, let him have some quality of life not quantity. |
Experience of Complications
In interviews, respondents were more distressed by or focused on minor complications that were less serious than the qualifying complication they had suffered. Although they had survived life-threatening hemorrhage or septic shock, they felt their other problems were dismissed by the surgical team. The dismissiveness led to attempts to self-censor their concerns in response to the care team’s attitude. For example, one participant was emergently explored for postoperative bleeding. Although he had little to say about this near-death experience, he suffered a painful neuropraxia from positioning. He described experiencing agonizing pain while the surgical team had limited response: “this happens,” and “it’s probably from surgery, it will get better.” Although he expressed deep frustration about this problem during his interview, he and his family did not complain to the team about their care because they “did not want to be seen as complaining or negative...he [the surgeon] saved [my] life and I am going to tell him we are upset about this nerve pain? No.” Other respondents reported they experienced smaller and less concerning outcomes in addition to their serious complication, yet they wrestled with internalizing their experiences and concerns.
Some respondents were more vocal about their care, noting they had concerns about the timing of medications or discharge plans. While members of the health care team acknowledged their concerns and preferences, their needs were occasionally not met. Participants noted that they didn’t expect all of their needs or requests to be accommodated, but when they didn’t receive an explanation about why their needs were unaddressed, they felt unimportant and dismissed.
Discussion
In this multisite randomized clinical trial, there was little participant reported postoperative conflict about the use of life-supporting treatments or goals of care. Instead, patients and family members reported a range of experiences related to the serious complications they had suffered. Many noted that their goals of care, focused on survival, were supported and protected by their surgeon. This was also endorsed by a family member whose loved one died as there seemed to be little uncertainty about the patient’s inability to survive. Nonetheless, patients and family observed hostility between clinicians, and expressed concerns related to preoperative communication that interfered with their care or their ability to anticipate and prepare for an unwanted outcome. While some patients did not seem emotionally impacted by serious complications, several noted distress, including concerns about more benign events when their care team seemed dismissive of these complaints. Although our study was likely compromised by our inability to access those with the most serious complications, these observations shed light on how patients and their family experience complications and suggest steps surgeons can take to support patients and families when such events occur.
Patient and family experiences of major surgery and complications are viewed through a lens of trust within the surgeon-patient relationship. When trust is difficult to generate preoperatively, failure of the relationship continues postoperatively with impact on patient care and outcomes. Participants who trusted their surgeon, expressed less distress about postoperative complications and continued to look to the surgical team to make decisions and manage their care. How this trusting relationship is generated preoperatively is less clear. Levinson and colleagues [22] have shown that surgeons who have a good, informative relationship with patients are less likely to face malpractice claims. Moreover, the covenantal relationship described by Cassell, “I will not abandon you” seems also to depend on prolonged and sustained interaction with the surgeon preoperatively. [6] It is difficult to assess from our data, including preoperative transcripts, what specifically generates a connection between surgeon, patient, and family. While patients in our study were informed of risks and about technical aspects of surgery, their articulated concerns seem related to a broader perspective of how well the surgeon understood their personal needs and their life beyond their surgical problem or attended to specific items they brought to the conversation. Our data suggests that trust and a shared understanding of the patient’s goals of care are interconnected and likely require exploration of patient concerns preoperatively, including the context of the patient’s health trajectory beyond surgical risks and benefits. In generating shared goals with the patient and their family, the surgeon reveals an understanding of the patient and their values, is candid about the limitations of surgery (by not simply disclosing complications but clarifying what surgery can realistically achieve) and acknowledges the treatment decision as a reasonable course of action.
It is difficult to discern whether participants whose expression of being “surprised” or “upset” is related to miscommunication or the emotional toll of an unwanted outcome. Translating a list of risks and complications into an imaginable experience is undoubtedly difficult for patients and family and may leave them feeling unprepared and ill-equipped when such events occur. Using narrative description or attempting to describe what serious complications might mean for the patient, e.g., loss of physical functioning, or a change in care needs, can go beyond simple risk disclosure to help patients anticipate and prepare if unwanted events occur. [23] By describing what life would look like in both the short and long term in the setting of serious complications, surgeons can in turn examine patients’ fears, reluctance and worries. Nonetheless, bad outcomes are upsetting regardless of preparation and complaints we heard from patients and families at times related to lack of acknowledgement of their distress. Clinicians who are working hard to prolong life or even mitigate discomfort often forsake the need to attend to emotion in a manner that would allow patients and families to feel heard and understood. [24, 25] Simple communication skills like naming emotion, e.g., “this is so frustrating,” or respect, e.g., “clearly you love your spouse, you are asking so many great questions,” have potential to reduce patient and family distress in the setting of unwanted outcomes. [26, 27]
We were surprised that participants reported hostile interactions among members of the healthcare team. Although we had asked whether everyone on the care team was on the same page, participants were troubled by and reported behaviors of interprofessional animosity. Although poor behavior is not novel in the medical literature, it is remarkable to hear patients and family describe it and report its impact on their care, even though it was not directed at them. Whether these observations reflect the surgeon’s emotional response to a patient’s poor outcome or a long-term bad habit, disruptive behaviors reduce team collaboration, cause adverse events [28] and lead to clinician burnout [29, 30] and attempts should be made to reduce them. Steps to mitigate conflict include professional awareness and education about conflict de-escalation strategies. Additionally, institutional barriers that raise conflict such as vexing workloads, toxic work culture and poor leadership should be addressed.
Finally, although our study was designed to evaluate postoperative conflict about life supporting treatments, we found a relatively low rate of conflict about limitations for life-sustaining treatment or goals of care. Although postoperative conflict is often highlighted in the lay press [31] and ICU literature, it is difficult to capture these moments in a prospective study and as such, its incidence and etiology remain unclear. Given it is a problem that seems to have low incidence but high impact, alternative strategies to evaluate and fully understand this phenomenon are needed.
Study Limitations
This study has both strengths and limitations. There are few studies that have tried to systematically capture episodes of postoperative conflict. Although we had previous experience interviewing patients and family members who had suffered serious complications, we were surprised that it was so difficult in this study. Patients with the most serious complications were often too ill to participate or could not be reached as they were in a skilled nursing or long-term care facility. Unfortunately, many patients who couldn’t be reached did not have a family member who was enrolled in the study and could be contacted on their behalf. As research coordinators sensed distress and hesitancy in participants with a difficult postoperative course, the cohort we interviewed was more emotionally settled and amenable to study participation. For future studies, researchers who aim to examine postoperative conflict might consider approaching families and patients after more time has passed to mitigate the impact of emotional discomfort on study participation. Additionally, study personnel should be encouraged to develop rapport with patients and their families prior to surgery to promote comfort in approaching participants for ongoing data collection in the setting of serious complications.
Conclusion
Although postoperative conflict in the setting of serious complications is well described, its incidence may be too low to evaluate in a study of this size, particularly when patients and their family members who suffered the most serious complications could not participate. Nonetheless, patient and family observations about their care reveal opportunities for improvement including preoperative communication, acknowledgment of patient and family concerns, and intra-team interactions.
Supplementary Material
Highlights.
Most patients experienced little conflict related to life sustaining treatments or goals of care.
Patients and their families felt unprepared for complications and struggled to trust their surgeon following based on preoperative conversations.
Respondents often focused on minor issues, like atypical pain or dietary restrictions, even though they had experienced serious complications and life-threatening events.
Patients witnessed overt conflict among team members including heated interactions and authoritative personalities during difficulties related to their postoperative course.
Acknowledgments
FUNDING/SUPPORT and COI/DISCLOSURE:
Funding/Support: All authors reported receiving Patient-Centered Outcomes Research Institute (PCORI) grants. Dr. Schwarze reported receiving funding from the Patient-Centered Outcomes Research Institute (PCORI) (award CDR1502–27462) and the National Institutes of Health (NIH) (grant R21AG055876–01). Dr. Kalbfell reported being supported by a training award from the NIH. Dr. Kata reported receiving grants from the National Institute on Aging.
Footnotes
COI/Disclosure: Dr. Schwarze has no related conflicts of interest to declare. Dr. Kalbfell has no related conflicts of interest to declare. Dr. Kata has no related conflicts of interest to declare. Dr. Mosenthal has no related conflicts of interest to declare. Dr. Finlayson is a founding shareholder in Ooney Inc. Anne Buffington has no related conflicts of interest to declare. Dr. Brasel has no related conflicts of interest to declare. Dr. Cooper has no related conflicts of interest to declare.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Finlayson EV and Birkmeyer JD, Operative mortality with elective surgery in older adults. Eff Clin Pract, 2001. 4(4): p. 172–7. [PubMed] [Google Scholar]
- 2.Finlayson E, Fan Z, and Birkmeyer JD, Outcomes in octogenarians undergoing high-risk cancer operation: a national study. J Am Coll Surg, 2007. 205(6): p. 729–34. [DOI] [PubMed] [Google Scholar]
- 3.Kata A, et al. , Increasing Advance Care Planning Using a Surgical Optimization Program for Older Adults. Journal of the American Geriatrics Society, 2018. 66(10): p. 2017–2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schwarze ML, Bradley CT, and Brasel KJ, Surgical “buy-in”: the contractual relationship between surgeons and patients that influences decisions regarding life-supporting therapy. Crit Care Med, 2010. 38(3): p. 843–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schwarze ML, et al. , Surgeons expect patients to buy-in to postoperative life support preoperatively: results of a national survey. Crit Care Med, 2013. 41(1): p. 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cassell J, et al. , Surgeons, intensivists, and the covenant of care: administrative models and values affecting care at the end of life--Updated. Crit Care Med, 2003. 31(5): p. 1551–7. [PubMed] [Google Scholar]
- 7.Bosk CL, Introduction, in Forgive and Remember. 1979, The University of Chicago Press: Chicago. p. 2–34. [Google Scholar]
- 8.Studdert DM, et al. , Conflict in the care of patients with prolonged stay in the ICU: types, sources, and predictors. Intensive Care Med, 2003. 29(9): p. 1489–97. [DOI] [PubMed] [Google Scholar]
- 9.Breen CM, et al. , Conflict associated with decisions to limit life-sustaining treatment in intensive care units. J Gen Intern Med, 2001. 16(5): p. 283–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Azoulay E, et al. , Prevalence and factors of intensive care unit conflicts: the conflicus study. Am J Respir Crit Care Med, 2009. 180(9): p. 853–60. [DOI] [PubMed] [Google Scholar]
- 11.Paul Olson TJ, et al. , Surgeon-reported conflict with intensivists about postoperative goals of care. JAMA Surg, 2013. 148(1): p. 29–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nabozny MJ, Steffens NM, and Schwarze ML, When Do Not Resuscitate Is a Nonchoice Choice: A Teachable Moment. JAMA Intern Med, 2015. 175(9): p. 1444–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Embriaco N, et al. , Burnout syndrome among critical care healthcare workers. Curr Opin Crit Care, 2007. 13(5): p. 482–8. [DOI] [PubMed] [Google Scholar]
- 14.Lemiale V, et al. , Health-related quality of life in family members of intensive care unit patients. J Palliat Med, 2010. 13(9): p. 1131–7. [DOI] [PubMed] [Google Scholar]
- 15.Hurel D, et al. , Quality of life 6 months after intensive care: results of a prospective multicenter study using a generic health status scale and a satisfaction scale. Intensive Care Medicine, 1997. 23(3): p. 331–337. [DOI] [PubMed] [Google Scholar]
- 16.Kowalczyk M, et al. , Emotional sequelae among survivors of critical illness: a long-term retrospective study. Eur J Anaesthesiol, 2013. 30(3): p. 111–8. [DOI] [PubMed] [Google Scholar]
- 17.Steffens NM, et al. , Engaging Patients, Health Care Professionals, and Community Members to Improve Preoperative Decision Making for Older Adults Facing High-Risk Surgery. JAMA Surg, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schwarze ML, et al. , Effectiveness of a Question Prompt List Intervention for Older Patients Considering Major Surgery: A Multisite Randomized Clinical Trial. JAMA Surg, 2019. 155(1): p. 6–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schwarze ML, et al. , Development of a List of High-Risk Operations for Patients 65 Years and Older. JAMA Surg, 2015. 150(4): p. 325–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ghaferi AA, Birkmeyer JD, and Dimick JB, Variation in Hospital Mortality Associated with Inpatient Surgery. New England Journal of Medicine, 2009. 361(14): p. 1368–1375. [DOI] [PubMed] [Google Scholar]
- 21.Miles M and Huberman A, Within-Case Displays: Exploring and Describing, in Qualitative Data Analysis. 1994, SAGE Publications: Thousand Oaks, CA. p. 102–105. [Google Scholar]
- 22.Levinson W, et al. , Physician-patient communication. The relationship with malpractice claims among primary care physicians and surgeons. JAMA, 1997. 277(7): p. 553–9. [DOI] [PubMed] [Google Scholar]
- 23.Schwarze ML and Taylor LJ, Managing uncertainty—harnessing the power of scenario planning. New England Journal of Medicine, 2017. 377(3): p. 206–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Strull WM, Lo B, and Charles G, Do patients want to participate in medical decision making? Jama, 1984. 252(21): p. 2990–4. [PubMed] [Google Scholar]
- 25.Gramling R, et al. , Feeling Heard and Understood: A Patient-Reported Quality Measure for the Inpatient Palliative Care Setting. J Pain Symptom Manage, 2016. 51(2): p. 150–4. [DOI] [PubMed] [Google Scholar]
- 26.Suchman AL, et al. , A model of empathic communication in the medical interview. Jama, 1997. 277(8): p. 678–82. [PubMed] [Google Scholar]
- 27.Fortin AH, et al. , Smith’s Patient Centered Interviewing: An Evidence-Based Method, Third Edition. 2012: McGraw-Hill Education. [Google Scholar]
- 28.Rosenstein AH and O’Daniel M, A survey of the impact of disruptive behaviors and communication defects on patient safety. Jt Comm J Qual Patient Saf, 2008. 34(8): p. 464–71. [DOI] [PubMed] [Google Scholar]
- 29.Seys D, et al. , Health care professionals as second victims after adverse events: a systematic review. Eval Health Prof, 2013. 36(2): p. 135–62. [DOI] [PubMed] [Google Scholar]
- 30.Shanafelt TD, et al. , Burnout and medical errors among American surgeons. Ann Surg, 2010. 251(6): p. 995–1000. [DOI] [PubMed] [Google Scholar]
- 31.Chen C, The Family Wanted a Do Not Resuscitate Order. The Doctors Didn’t. ProPublica, 2019. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


