Abstract
Trunk exoskeletons are wearable devices that support humans during physically demanding tasks by reducing biomechanical loads on the back. While most trunk exoskeletons are rigid devices, more lightweight soft exoskeletons (exosuits) have recently been developed. One such exosuit is the HeroWear Apex, which achieved promising results in the developers’ own work but has not been independently evaluated. This paper thus presents an evaluation of the Apex with 20 adult participants during multiple brief tasks: standing up from a stool with a symmetric or asymmetric load, lifting a unilateral or bilateral load from the floor to waist level, lifting the same bilateral load with a 90-degree turn to the right, lowering a bilateral load from waist level to floor, and walking while carrying a bilateral load. The tasks were performed in an ABA-style protocol: first with exosuit assistance disengaged, then with it engaged, then disengaged again. Four measurement types were taken: electromyography (of the erector spinae, rectus abdominis, and middle trapezius), trunk kinematics, self-report ratings, and heart rate. The exosuit decreased the erector spinae electromyogram by about 15% during object lifting and lowering tasks; furthermore, participants found the exosuit mildly to moderately helpful. No adverse effects on other muscles or during non-lifting tasks were noted, and a decrease in middle trapezius electromyogram was observed for one task. This confirms that the HeroWear Apex could reduce muscle demand and fatigue. The results may transfer to other exoskeletons with similar design principles, and may inform researchers working with other wearable devices.
Keywords: Trunk exoskeletons, exosuits, HeroWear Apex, lifting, low-back pain
1. Introduction
Low back pain is a major cause of disability (James et al., 2018), and is associated with repetitive heavy lifting or long-term tiring postures (Swain et al., 2020). To reduce incidence of such pain, researchers have developed trunk exoskeletons (also called back-assist exoskeletons): wearable devices that physically support the trunk, reducing biomechanical loads. Most such exoskeletons are intended for occupational uses (e.g., construction, logistics) (Baltrusch et al., 2020; Huysamen et al., 2018), though they have also been proposed for people with chronic injuries (Goršič et al., 2020a; Kozinc et al., 2021).
Trunk exoskeletons differ from better-known limb and full-body exoskeletons in that they reduce load on the back without supporting the limbs (Kermavnar et al. , 2021). They are divided into active (powered) devices and passive (unpowered) devices that can store energy using elements like springs. As discussed by a recent review (Kermavnar et al., 2021), most trunk exoskeletons are passive (Baltrusch et al., 2020; Goršič et al., 2020a; Koopman et al., 2020; Lamers et al., 2018); however, active exoskeletons can provide additional assistance (Huysamen et al., 2018; Koopman et al., 2019). While existing evidence is mainly laboratory-based, it indicates that both passive and active exoskeletons can reduce back muscle load and spinal compression (Kermavnar et al., 2021).
While most trunk exoskeletons are ‘rigid’, there has recently been a push toward ‘soft’ exoskeletons (i.e., exosuits), which are lighter and could result in less interference to the wearer’s natural motion. Such exosuits are common for upper (Correia et al., 2020) and lower limbs (Schmidt et al., 2017), and back-assist exosuits have now begun to appear (Alemi et al., 2019; Lamers et al., 2018; Tsuneyasu et al., 2018). One commercial example is the HeroWear Apex (HeroWear, Nashville, USA), first described as a prototype in 2018 (Lamers et al., 2018). The prototype reduced erector spinae (ES) muscle activity by 23–43% in leaning tasks and 14–16% in lifting tasks (Lamers et al., 2018), and a follow-up study found fatigue reductions during leaning (Lamers et al., 2020). However, both evaluations were done by the original developers and only studied lifting in a limited fashion - lifting a box in the sagittal plane with both arms. A follow-up study in real-world environments was recently presented by the developers, but was very brief and only discussed positives (Yandell et al., 2020). This paper thus presents an independent evaluation of the Apex during multiple brief tasks, with the goal of providing objective and detailed evidence about the device’s short-term benefits and drawbacks. This information could be useful both for consumers and for experts working with other devices, who could use it to improve their own designs.
2. Materials and methods
2.1. HeroWear Apex
A participant wearing the Apex passive back-assist exosuit is shown in Figure 1. The device weighs 1.5 kg and comprises an upper-body section (like a backpack with shoulder and chest straps), thigh sleeves, and two elastic bands along the back that connect the upper-body section to the thigh sleeves. A switch allows the assistive mechanism to be engaged or disengaged. If engaged, the elastic bands stretch whenever the wearer leans forward or crouches, generating assistive torques about the lumbar spine (Lamers et al., 2018). If disengaged, the device is slack and applies no force.
Figure 1.

A participant wearing the Apex (HeroWear, Nashville, USA), front and back views. The exosuit consists of an upper-body part similar to a backpack, two thigh sleeves, and two elastic bands on the back that connect the upper-body part to the thigh sleeves. The participant is also wearing the sensors used in the study (e.g., wireless electromyography sensors under shirt, optical tracking markers on shoulders, heart rate bracelet).
The exosuit package includes multiple sizes of each component, with components for a specific wearer chosen based on body dimensions following the manufacturer’s instructions. It also includes elastic bands in ‘strong’ and ‘very strong’ versions (with different stiffnesses); the manufacturer recommends leaving the band strength to the wearer’s preference.
2.2. Participants
Twenty individuals (5 women, 15 men) with no history of chronic back pain or back injury took part in the study. They were 25.5 ± 4.7 (mean ± standard deviation) years old (range 21–39), with heights of 178.5 ± 8.9 cm (range 167–192) and weights of 79.7 ± 20.5 kg (range 51–144). All were right-handed.
2.3. Study protocol
The study was approved by the University of Wyoming Institutional Review Board (IRB), protocol #20200129DN02643. Data collection took place in late 2020. Due to the COVID-19 pandemic, participants and researchers wore face masks, and social distancing was maintained whenever possible.
Each participant took part in one ~1.5-hour session. The Apex was first demonstrated, the study was explained, and the participant gave informed consent. Exosuit component sizes were selected following manufacturer instructions. Participants then donned the exosuit, engaged the assistance, and walked around and lifted/carried objects in an unstructured manner for a few minutes with first ‘strong’ and then ‘very strong’ elastic bands. They then chose between the ‘strong’ and ‘very strong’ bands according to what they considered most helpful; if unable to decide, they could try both bands again. Thirteen participants chose ‘very strong’ while 7 chose ‘strong’ bands. They then performed the same unstructured tasks with the engaged exosuit until they felt reasonably familiar with it (self-determined, usually ~5 minutes). During this time, any reported comfort issues were addressed. Sensors were then applied (section 2.4), and data collection began.
Data collection was done in three blocks: first, multiple tasks were done with exosuit assistance disengaged; then, the same tasks were done with assistance engaged; then, with it disengaged again. The tasks were:
stand up from stool with 17.5-lb (7.9-kg) dumbbell in dominant hand,
stand up from stool with 17.5-lb dumbbell in each hand,
lift 17.5-lb dumbbell from floor beneath participant’s dominant hand to standing position,
lift plastic box with handles and 15-lb (6.8-kg) weight from floor in front of participant to waist level in sagittal plane using both arms,
lower same box and weight from waist level to floor in sagittal plane,
lift same box with 30-lb (13.6-kg) weight from floor to waist level in sagittal plane,
lower same box and weight from waist level to floor in sagittal plane,
lift same box with 15-lb weight from floor onto elbow-height table located 90 degrees to participant’s right, approximately elbow-to-wrist length away horizontally,
walk across room while carrying same box with 15-lb weight.
No strategy was prescribed for the tasks. The task order within each block was varied randomly between participants but was the same for all three blocks of a participant. Within each block, each task was performed once and measured signals were monitored; if signal quality was poor (due to noticeable electrode movement or occluded optical markers), that trial was discarded and repeated until a good measurement was obtained. If necessary, exosuit adjustments were made prior to repetition to address issues such as elastic bands shifting and ‘bumping’ against sensors. Photos of a participant performing two tasks are shown in Figure 2.
Figure 2.

A participant performing two tasks while wearing the exosuit and sensors: lifting a box from the floor (left) and standing up from a stool while holding dumbbells (right). Optical tracking markers are visible on the body and lifted objects, and the heart rate bracelet is visible on the left wrist. Electromyography sensors are not visible from this angle.
Since the exosuit was designed for lifting and leaning tasks (Lamers et al., 2018 and 2020), these were also the focus of our study. While HeroWear developers had investigated loads up to 24 kg (Lamers et al., 2018), we limited ourselves to lighter loads following IRB recommendations regarding physically intensive research during the COVID-19 pandemic.
After block 3, participants removed the exosuit and completed maximum voluntary contraction (MVC) tests for all evaluated muscles.
2.4. Measurements
Four measurement types were taken: kinematics, electromyography (EMG), self-report ratings, and heart rate (HR). Participants’ body kinematics were measured using eight Vicon Bonita optical cameras (Vicon Motion Systems, UK) and retroreflective markers at 160 Hz. Markers were placed at left and right acromioclavicular joints, greater trochanters, lateral knees, lateral malleoli, toes, and heels. They were attached to a form-fitting shirt rather than skin to reduce marker detachment due to sweat and reduce direct skin contact during the COVID-19 pandemic. Markers were also placed on each side of the box and each end of both dumbbells.
EMG was measured from the left and right ES, rectus abdominis (RA), and middle trapezius (MT) using the Trigno Avanti wireless system (Delsys Inc, Boston, MA) at 1926 Hz. The skin was shaved and cleaned, and bipolar electrodes were placed following SENIAM recommendations (Hermens et al., 1999): for ES, at L3 height, ~4 cm left and right from the midline of the spine; for RA, 3 cm from the midline of the abdomen and 2 cm above the umbilicus; for MT, at 50% between the medial border of the scapula and spine, at T3 height, in the direction of the line between T5 and the acromion. A sensor close-up is shown in Figure 3. Sensors were taped to the skin to reduce noise. While MT sensors are covered by the exosuit, this was not problematic since the tight exosuit holds sensors in place. To reduce ES noise, the exosuit’s elastic bands were centered between sensors and periodically readjusted.
Figure 3.
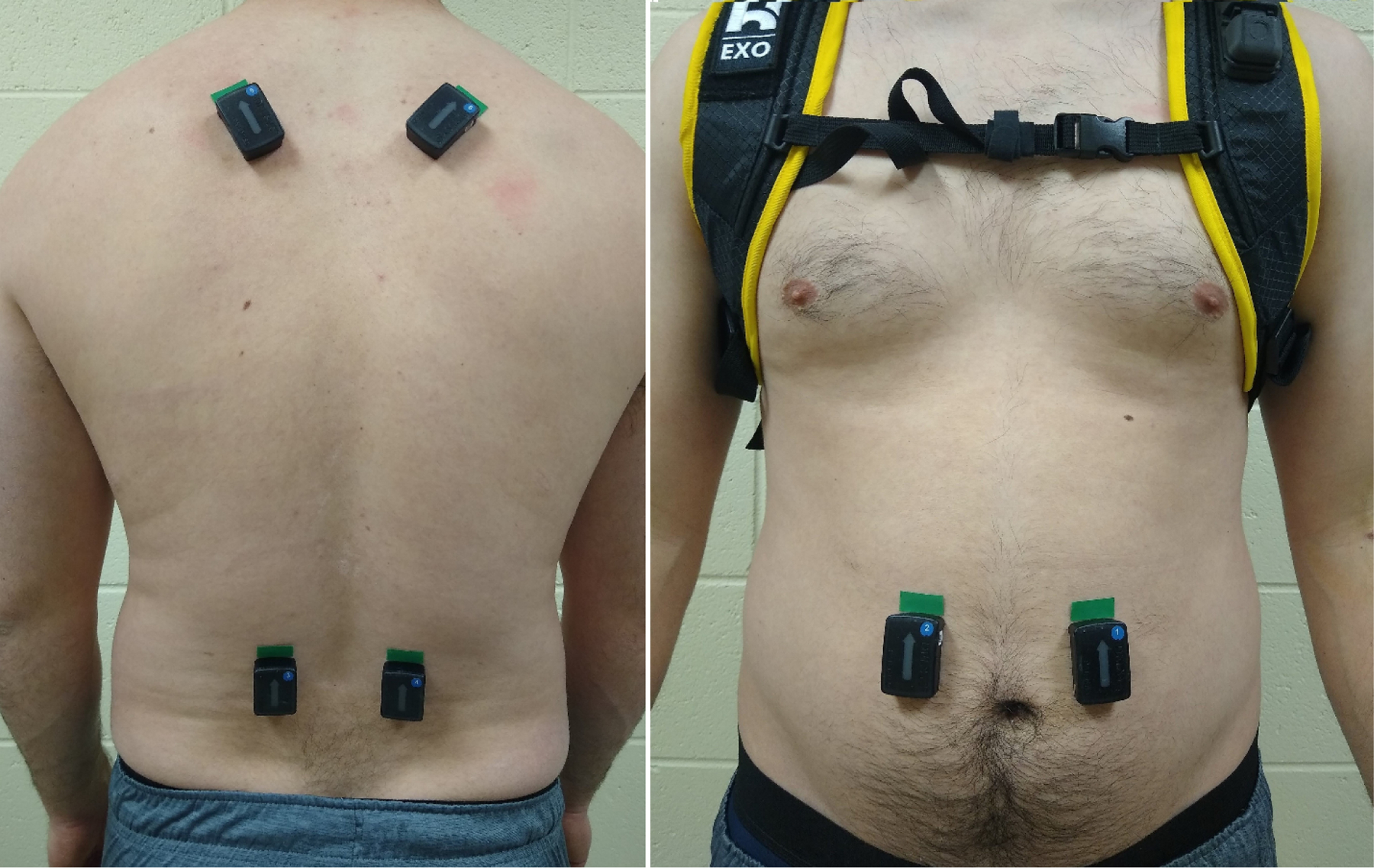
Close-up of the electromyography sensors on the back (bottom: erector spinae; top: middle trapezius) and front (rectus abdominis). Prior to beginning the study protocol, additional tape was placed over the sensors for better fixation, and a shirt and the full exosuit were donned.
Self-report ratings were collected during block 2 (when assistance was engaged) and after blocks 2 and 3. During block 2, after each task, participants rated how much effort it took to perform that task with the exosuit engaged relative to the exosuit disengaged. Answers were given on a scale from +5 (much easier engaged) to −5 (much easier disengaged), with 0 representing no difference and ±1 and ±3 representing mildly and moderately easier. After block 2, participants answered the same question over all tasks; after block 3, they answered it again.
HR was measured using the E4 wristband (Empatica, Boston, USA). This was a secondary measurement recommended by our IRB to avoid excessive strain during the COVID-19 pandemic. Mean HR was calculated over each block, as E4 event logging is done manually by the participant and was considered too time-consuming for each task.
2.5. Signal processing for EMG and kinematics
EMG and kinematic signals were first segmented into individual tasks. The start and end times for each task were determined as follows:
Walking while carrying box: one gait cycle midway across room.
Lifting box with 90-degree turn: from minimal height of greater trochanters to farthest load placement.
All other lifting and sit-to-stand tasks: from minimal to maximal height of greater trochanters.
Object lowering tasks: from maximal to minimal height of greater trochanters.
For kinematic analysis, the three-dimensional trunk reference frame was defined by the two acromioclavicular joints and the center of the two greater trochanters. Cardan angles with a rotation order of flexion-extension, left-right bending, and left-right rotation were calculated between the trunk and global reference frames to determine three-dimensional trunk angles. The two-dimensional thigh vector was defined by the greater trochanter and lateral knee. Two-dimensional thigh flexion-extension angles were calculated as the angle between the thigh vector and the vertical axis in the sagittal plane (Goršič et al., 2020b). Trunk ranges of motion (ROM) in flexion-extension, left-right bending, and left-right rotation as well as thigh ROM in flexion-extension were used as outcome variables. The thigh ROM was calculated as the mean of the left and right thigh ranges.
Segmented EMG signals were visually inspected for artifacts, and segments with excessively high EMG amplitudes were discarded. Signals were first filtered using a fourth-order Butterworth bandpass filter (20–450 Hz), then rectified and filtered using a fourth-order Butterworth lowpass filter (10 Hz) to obtain linear envelopes. Envelopes were normalized by maximum values obtained during corresponding MVC tests. Finally, peak and mean envelope values were used as outcome variables.
2.6. Statistical analysis
For kinematics and EMG, one-way repeated-measures analyses of variance (RMANOVA) followed by Holm-Sidak tests were conducted for each outcome variable and task, with the within-subjects variable being the block (1–3). When normality requirements were violated, one-way RMANOVA on ranks followed by Tukey tests were conducted instead. The significance threshold was p = .05.
For mean HR, similar RMANOVA and post-hoc tests were conducted; however, as mean HR was calculated over an entire block, RMANOVA was only done once rather than for each task.
For self-report ratings, one-sample t-tests were used to compare ratings to a mean of zero. This was done for each task within block 2 and for the two overall ratings. When normality requirements were violated, one-sample Wilcoxon signed-rank tests were used instead.
3. Results
All participants completed the protocol. Two participants’ EMG data were discarded due to poor quality, resulting in valid EMG from 18 participants. All other data are reported for 20 participants. Numerical results are presented as median (interquartile range) and p-values.
RMANOVA found no difference between blocks for mean HR (p = .29). Mean HR for the three blocks were 91.1 (84.9 – 96.8), 89.5 (83.5 – 95.6), and 91.4 (88.8 – 96.2) beats/min.
3.1. Electromyography
Table 1 shows p-values for RMANOVA for different EMG outcome variables and tasks. While many RMANOVA were significant, the exosuit-engaged (second) block was significantly different from both other blocks primarily for the ES. Specifically, the engaged exosuit decreased both left and right ES mean EMG for all four lifting tasks and both box-lowering tasks.
Table 1.
P-values for repeated-measures analyses of variance on different electromyography outcome variables in different tasks.
| Rectus abdominis | Erector spinae | Middle trapezius | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Task | Left mean | Left peak | Right mean | Right peak | Left mean | Left peak | Right mean | Right peak | Left mean | Left peak | Right mean | Right peak |
| Stand up with 1 dumbbell | .02 | .07 | .005 | .49 | .009 | .16 | .015 | .13 | .68 | .22 | .22 | .08 |
| Stand up with 2 dumbbells | .11 | .29 | .11 | .19 | .09 | .65 | .12 | .007 | .49 | .67 | .001 | .02 |
| Lift 1 dumbbell from floor | .42 | .16 | .07 | .06 | .006 | .06 | .024 | .18 | .02 | .004 | .13 | .20 |
| Lift 15-lb box, no turn | .29 | .59 | .09 | .06 | <.001 | .01 | .003 | .32 | .18 | .07 | .28 | .25 |
| Lift 30-lb box, no turn | .01 | .66 | .03 | .12 | <.001 | .02 | .002 | .009 | .84 | .24 | .85 | .21 |
| Lift 15-lb box, 90-degree turn | .35 | .68 | .07 | .21 | <.001 | .35 | .005 | .08 | .29 | .64 | .44 | .59 |
| Lower 15-lb box, no turn | .33 | .47 | .06 | .02 | .047 | .046 | .01 | .004 | .19 | .08 | .49 | .31 |
| Lower 30-lb box, no turn | .22 | .49 | .11 | .10 | .03 | .047 | <.001 | .004 | .89 | .92 | .69 | .99 |
| Walk with 15-lb box | .03 | .16 | .003 | .16 | .11 | .29 | .66 | .94 | .23 | .39 | .96 | .53 |
Values under .05 are bolded. If post-hoc tests found the second (exosuit-engaged) block to be significantly different from both other blocks, the value is also underlined.
Additionally, it decreased both ES peak EMG during both box-lowering tasks. Finally, only one difference was observed in other muscles: the engaged exosuit decreased right MT mean EMG when standing up with two dumbbells.
For left and right ES mean EMG, results are shown in Figures 4 (left ES) and 5 (right ES). For both left and right ES peak EMG, results are shown in Figure 6. For right MT mean EMG when standing up with two dumbbells, percentages of MVC value in the three blocks were 15.1 (10.3 – 18.4), 12.2 (10.2 – 17.6), and 13.4 (10.4 – 18.4). In this case, post-hoc tests found p-values below 0.001 between blocks 1 and 3 and 0.005 between blocks 2 and 3. For outcome variables and tasks where RMANOVA were significant but post-hoc tests did not find significant differences between block 2 and both other blocks, results are given in the Appendix.
Figure 4.
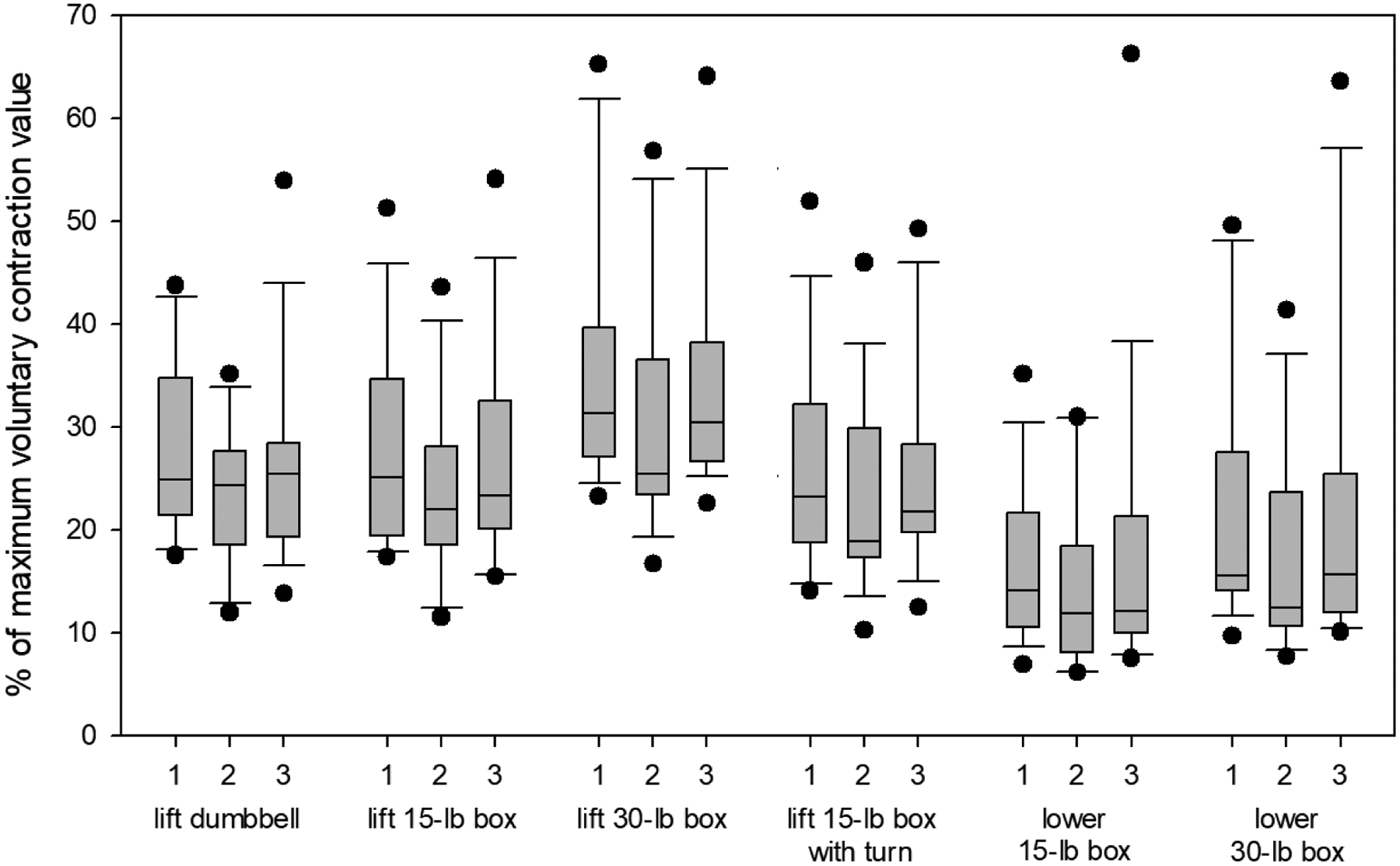
Box plot of left erector spinae mean electromyogram envelope value for the six tasks where the exosuit-engaged block (2) was significantly different from the two exosuit-disengaged blocks (1 and 3). Whiskers represent 10th and 90th percentiles while dots are individual outliers.
Figure 5.
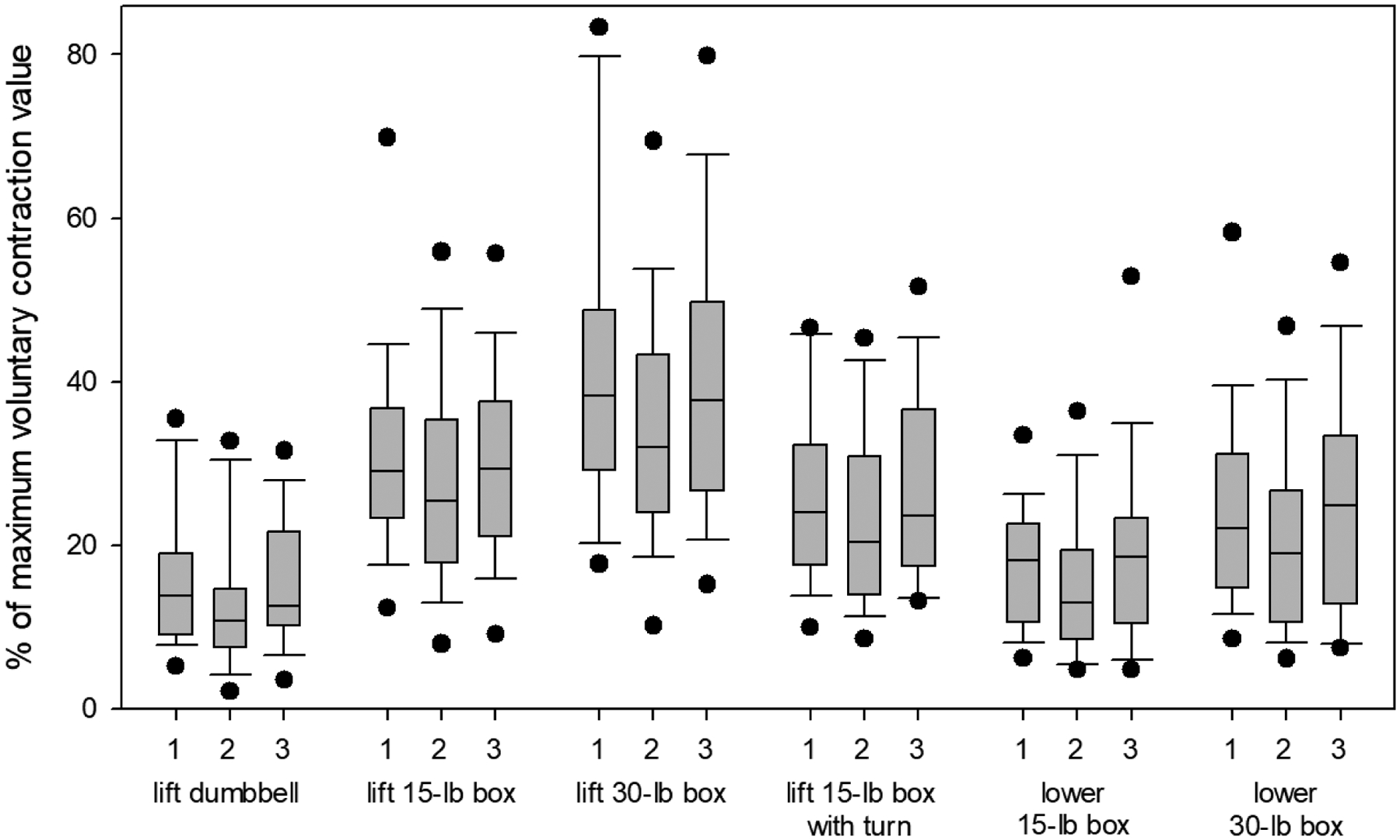
Box plot of right erector spinae mean electromyogram envelope value for the six tasks where the exosuit-engaged block (2) was significantly different from the two exosuit-disengaged blocks (1 and 3). Whiskers represent 10th and 90th percentiles while dots are individual outliers.
Figure 6.
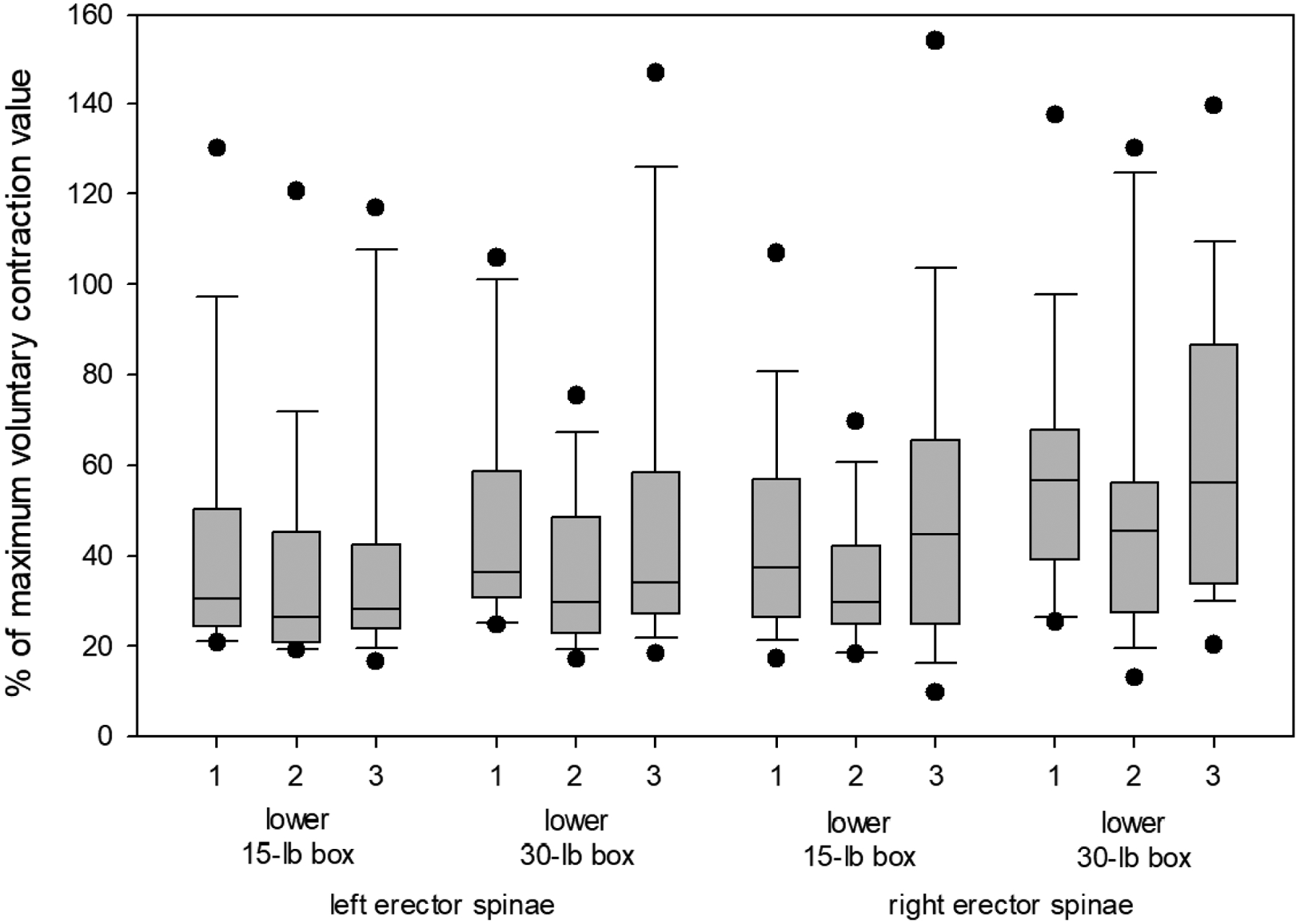
Box plot of left and right erector spinae peak electromyogram values for the two tasks where the exosuit-engaged block (2) was significantly different from the two exosuit-disengaged blocks (1 and 3). Whiskers represent 10th and 90th percentiles while dots are individual outliers.
3.2. Kinematics
Table 2 shows p-values for RMANOVA for different kinematic outcome variables and tasks. While many RMANOVA were significant, the exosuit-engaged (second) block was significantly different from both other blocks in only one case: when lifting a dumbbell from the floor, the engaged exosuit resulted in lower trunk flexion/extension ROM. In this case, ROM for the three blocks were 60.4 (56.4 – 67.5), 58.2 (52.3 – 64.3), and 64.4 (55.5 – 76.1) degrees. Post-hoc tests found p-values of .008 between blocks 1 and 2, .026 between blocks 1 and 3, and below .001 between blocks 2 and 3. For outcome variables and tasks where RMANOVA were significant but post-hoc tests did not find significant differences between block 2 and both other blocks, results are given in the Appendix.
Table 2.
P-values for repeated-measures analyses of variance on different kinematics outcome variables in different tasks.
| Task | Tr-FE | Tr-LRB | Tr-LRR | Th-FE |
|---|---|---|---|---|
| Stand up with 1 dumbbell | .005 | .46 | .09 | .01 |
| Stand up with 2 dumbbells | .07 | .57 | .15 | .23 |
| Lift 1 dumbbell from floor | <.001 | .26 | .27 | .13 |
| Lift 15-lb box, no turn | <.001 | .75 | .86 | .02 |
| Lift 30-lb box, no turn | <.001 | .48 | .29 | .005 |
| Lift 15-lb box, 90-degree turn | <.001 | .58 | .66 | .34 |
| Lower 15-lb box, no turn | <.001 | .39 | .22 | .003 |
| Lower 30-lb box, no turn | <.001 | .20 | .12 | <.001 |
| Walk with 15-lb box | .88 | .62 | .20 | .005 |
Tr = trunk, Th = thigh. FE, LRB, and LRR represent ranges of motion in flexion/extension, left/right bending, and left/right rotation. Values under .05 are bolded. If post-hoc tests found the second (exosuit-engaged) block to be significantly different from both other blocks, the value is also underlined.
3.3. Self-report ratings
Table 3 shows self-report ratings and results of one-sample t-tests or signed rank tests. Most medians are between 1 and 2, with 1 indicating “mildly easier”.
Table 3.
Self-reported ratings of how much effort it was to perform different tasks with the exosuit engaged compared to doing them with the exosuit engaged, presented as median (interquartile range).
| Task | Rating | P-value |
|---|---|---|
| Stand up with 1 dumbbell | 1 (0 – 1.25) | .003 |
| Stand up with 2 dumbbells | 1 (1 – 2) | .002 |
| Lift 1 dumbbell from floor | 1 (0.75 – 2.25) | < .001 |
| Lift 15-lb box, no turn | 2 (1 – 2) | < .001 |
| Lift 30-lb box, no turn | 1.8 (1 – 2) | < .001 |
| Lift 15-lb box, 90-degree turn | 1 (0.75 – 2) | < .001 |
| Lower 15-lb box, no turn | 1 (0 – 2) | .051 |
| Lower 30-lb box, no turn | 1 (0 – 1.625) | .013 |
| Walk with 15-lb box | 0 (−0.25 – 0) | .23 |
| Overall after second block | 1.5 (1 – 2) | < .001 |
| Overall after third block | 1.8 (1 – 2.625) | < .001 |
P-values indicate results of one-sample t-tests or one-sample signed rank tests comparing the ratings to zero.
4. Discussion
4.1. Electromyography
Engaging the exosuit reduced mean ES EMG during lifting and lowering tasks. Across these tasks, the mean EMG value with the engaged exosuit is approximately 85% of the value with the disengaged exosuit (and varies between specific tasks from about 70% to 95%). Decreases in peak ES EMG were similar in magnitude to those seen for mean EMG (see Appendix). This is similar to results shown by Apex developers in a smaller set of tasks (Lamers et al., 2018) as well as results obtained with rigid exoskeletons (Kermavnar et al., 2021). While most previous studies did not separately evaluate lifting and lowering (and instead combined them into a single task), we feel that reductions to both lifting and lowering are sensible – the ES are the primary muscles used to both raise the box and control the descent of the box. Since EMG reductions are associated with decreased fatigue (Kermavnar et al., 2021), this is a potentially beneficial effect of the Apex. The result would likely transfer to other similar exosuits – for example, the recently released LiftSuit (Auxivo AG, Switzerland) or the recently developed but not extensively evaluated expansion to the Apex (Lamers & Zelik, 2021).
A recent review (Kermavnar et al., 2021) only mentions one other scientifically evaluated passive soft trunk exoskeleton: the VT-Lowe’s exoskeleton (Alemi et al., 2019). An evaluation of that device found ES EMG decreases of ~29% (Alemi et al., 2019) – much more than the ~15% average observed in our study. However, two differences should be noted between their study and ours. First, their exoskeleton includes over 50 carbon fiber beams, which likely provide more support than the Apex’s elastic bands at the cost of greater bulk and weight. Second, participants in their study lifted loads of 20% of their body weight while our study used lighter loads. Similar explanations of the VT-Lowe’s results have been independently proposed by other researchers (Baltrusch et al., 2020).
No increases in EMG of any measured muscle were observed. We were originally concerned that any decreases in ES EMG during lifting tasks might be due to the load being redistributed onto other muscles, or that the exosuit might interfere with non-lifting tasks, as observed in our previous work (Goršič et al., 2020a) and suggested by others (Baltrusch et al., 2020).This did not appear to be the case: engaging the exosuit generally insignificantly reduced mean and peak EMG values (see Appendix). However, the study admittedly did not involve a block entirely without the exosuit, as discussed later.
Only one effect on muscles other than ES could be attributed to the engaged exosuit: it decreased right MT mean EMG when standing up with two dumbbells. This was not expected: the MT were primarily evaluated since we were concerned that the exosuit might redistribute load to them, thus increasing EMG. A recent review of trunk exoskeleton studies (Kermavnar et al., 2021) reports only one significant trapezius EMG result: an increase rather than a decrease (Amandels, het Eyndt, Daenen, & Hermans, 2018). However, our study does indicate insignificant decreases in MT EMG for other tasks too (Appendix); while we have no clear explanation for this, it may be a small effect of the exosuit redistributing load to other, unmeasured muscles, and may warrant further investigation.
4.2. Kinematics
Only one effect on kinematics could be attributed to the engaged exosuit: reduced trunk flexion/extension ROM during asymmetric dumbbell lifting. Our personal unverified explanation is as follows. While the external moments provided by the exosuit were generally helpful, they were likely somewhat inconvenient in this task since the dumbbell was relatively light and placed to the participant’s side. Thus, participants avoided trunk flexion and used motions unaffected by the exosuit (e.g., lateral bend). Such compensation was not possible during bilateral lifts, where participants had to lower their body with trunk flexion to handle a symmetric load placed in front of them. However, we have no evidence for this explanation - while higher lateral bend ROM was found during the asymmetric task, the difference was not significant. Additionally, in this task, the two exosuit-disengaged blocks (1 and 3) also differ from each other with regard to trunk flexion/extension ROM. This may be due to fatigue or experience, as discussed later.
4.3. Self-report ratings
Participants largely reported that the engaged exosuit was mildly to moderately helpful. In our opinion, this is adequate for a relatively lightweight and low-cost device; mild assistance during a single lift likely has a compounding effect over time in repetitive lifting. At worst, the exosuit was perceived as mildly annoying; only one score below −1 was seen across all tasks and participants. This confirms that the exosuit does not have obvious detrimental effects; the annoyance was generally due to discomfort and could likely be addressed with additional exosuit adjustments.
4.4. Effects of time and fatigue
As seen in the Appendix, there were several significant RMANOVA where block 2 was not significantly different from the other two blocks in post-hoc tests. Notably, there are several cases where block 1 is different from block 3. We believe that these differences are primarily due to fatigue (which may modify both EMG and posture) or other time-dependent effects such as sweating or increased familiarity with the exosuit over time (see next section).
Less clearly, there are several cases where block 2 is different from one of the other two blocks, but not both. These may also be due to time/fatigue, but may be genuine effects of the exosuit that are too small to be significant with our protocol and sample. For example, both ES peak EMG show decreases in block 2, but the block is not significantly different from both other blocks. This is almost certainly an effect of the engaged exosuit since mean EMG shows a similar significant pattern. Effects may simply be smaller and/or obscured by effects of fatigue - for example, when the exosuit is disengaged after block 2, we would expect higher EMG in block 3; however, fatigue may cause an EMG decrease in block 3, obscuring the exosuit’s effects.
4.5. Effect of familiarity with exosuit
Though this was not quantitatively evaluated, we subjectively noted that wearers had very different adjustment periods to the exosuit. While some immediately understood its assistive behavior, others had difficulty understanding it, needed longer familiarization, and had worse subjective impressions of the device. EMG and kinematics might also have been different in such participants, and we consider this a possible confounding factor worth reporting even without objective evidence.
Based on informal conversations, participants who had more difficulty tended to be those with lower physical fitness. Future studies should aim to reduce this confounding effect. One option would be to only include participants who are physically fit, but the target population may also include less fit participants, so this may not obtain a full picture of the device’s effects. Another option would be to give participants longer familiarization periods, then observe how their experience with the device develops and how it influences final results. Finally, participants could be divided into subgroups based on fitness, and their experiences could be compared – similarly to a recent study that compared exoskeleton experiences of people with and without chronic pain (Kozinc et al., 2021).
4.6. Study limitations
Some study limitations should be mentioned. First, while static leaning tasks are also relevant for exoskeletons (Koopman et al., 2020; Lamers et al., 2018), they were omitted to reduce session length. Leaning was extensively studied by the Apex developers (Lamers et al., 2018), and we thus focused on relatively unexplored lifting tasks.
Second, while tasks were performed with the exosuit both engaged and disengaged, they were never done without the exosuit. Thus, simply wearing the disengaged exosuit may have unobserved effects on the body – for example, increased sweating due to another layer of clothing. For better comparison, the study design would ideally include blocks without the exosuit; in the current study, this was not done due to the time required to don/doff the exosuit, which might have also moved the sensors.
Third, peak EMG sometimes exceeded MVC values (Figure 6). This may be due to fatigue since MVC tests were done at the end of the session, or may be due to suboptimal MVC test procedures. We will aim to reduce this issue in the future – potentially by doing MVC tests at the start.
Finally, while decreases in ES EMG are promising indicators of fatigue reduction (Kermavnar et al., 2021), they do not guarantee long-term benefits such as the ability to work longer, more safely, or more efficiently. Thus, longer-term studies are still needed and could, for example, be done as a more detailed version of the pilot study presented by the Apex developers (Yandell et al., 2020) that could also measure additional muscles (Kermavnar et al., 2021), compression forces (Koopman et al., 2020), and spinal moments (Faber et al., 2020).
4.7. Conclusion
Engaging the exosuit decreased ES EMG during lifting and lowering tasks by approximately 15% on average (with decreases ranging from 5% to 30% between tasks), which may in the long term reduce fatigue and allow wearers to work safely for longer periods of time. Furthermore, a decrease in MT EMG was noted in one task. No EMG increases were observed when the exosuit was engaged, suggesting no adverse effects on other measured muscles or tasks. Finally, participants rated the exosuit as mildly to moderately helpful. Results may transfer to similar exosuits, and may inform experts working with other wearable devices, who could use this information to improve their own designs.
Acknowledgments
This work was funded by the National Science Foundation under grant no. 1933409 as well as by the National Institute of General Medical Sciences of the National Institutes of Health under grant no. 2P20GM103432. The sponsors had no involvement in any aspect of the study.
Appendix
Table 4 shows outcome variables and tasks for which RMANOVA found a significant difference between blocks, but post-hoc tests did not find significant differences between the second (exosuit-engaged) block and both other blocks.
Table 4.
Outcome variables and tasks where repeated-measures analyses of variance (or repeated-measures analyses of variance on ranks) found a significant difference between blocks, but post-hoc tests did not find significant differences between the exosuit-engaged block (2) and both exosuit-disengaged blocks (1 and 3).
| Outcome variable | Task | Median (interquartile range) inthe three blocks | Significant difference? | ||||
|---|---|---|---|---|---|---|---|
| 1 | 3 | 1–2 | 2–3 | ||||
| Left RA mean EMG(% MVC) | Stand up with 1 dumbbell | 1.6 (0.9–2.7) |
1.3 (0.8–2.5) |
N | N | ||
| Lift 30-lb box, no turn | 1.2 (0.9–1.9) |
1.4 (1.0–3.0) |
Y | N | |||
| Right RA mean EMG (% MVC) | Stand up with 1 dumbbell | 1.9 (0.7–3.1) |
1.8 (0.7–3.2) |
N | N | ||
| Lift 30-lb box, no turn | 1.8 (0.9–2.9) |
1.7 (1.1–3.1) |
N | N | |||
| Walk with 15-lb box | 1.8 (0.8–2.6) |
1.5 (0.8–1.9) |
N | N | |||
| Right RA peak EMG (% MVC) | Lift 1 dumbbell from floor | 6.3 (2.6–10.4) |
2.9 (1.5–6.7) |
N | N | ||
| Lower 15-lb box, no turn | 3.9 (1.1–6.4) |
3.8 (1.3–9.1) |
Y | N | |||
| Left ES mean EMG(% MVC) | Stand up with 1 dumbbell | 18 (13–21) |
15 (12–17) |
Y | N | ||
| Left ES peak EMG(% MVC) | Lift 15-lb box, no turn | 48 (41–73) |
43 (36–64) |
Y | N | ||
| Lift 30-lb box, no turn | 60 (44–77) |
58 (50–83) |
Y | N | |||
| Right ES meanEMG (% MVC) | Stand up with 1 dumbbell | 8.9 (5.8–12.8) |
8.9 (5.5–11.0) |
Y | N | ||
| Right ES peak EMG | Stand up with 2 dumbbells | 49 (26–67) |
40 (32–53) |
Y | N | ||
| (% MVC) | Lift 30-lb box, no turn | 79 (65–92) |
72 (55–82) |
Y | N | ||
| Left MT mean EMG(% MVC) | Lift 1 dumbbell from floor | 6.1 (4.3–8.6) |
5.6 (4.3–8.5) |
Y | N | ||
| Left MT peak EMG(% MVC) | Lift 1 dumbbell from floor | 12.2 (9.4–17.5) |
11.5 (8.8–16.3) |
Y | N | ||
| Right MT peakEMG (% MVC) | Stand up with 2 dumbbells | 36 (25–43) |
26 (25–38) |
Y | N | ||
| Trunk flexion / extension ROM(degrees) | Stand up with 1 dumbbell | 36 (29–42) |
35 (33–46) |
N | Y | ||
| Lift 15-lb box, no turn | 63 (55–72) |
67 (61–78) |
N | Y | |||
| Lift 30-lb box, no turn | 63 (56–73) |
70 (61–77) |
N | Y | |||
| Lift 15-lb box, 90-deg. turn | 65 (52–75) |
67 (58–77) |
N | Y | |||
| Lower 15-lb box, no turn | 63 (58–71) |
75 (62–79) |
N | Y | |||
| Lower 30-lb box, no turn | 69 (55–73) |
75 (58–81) |
N | Y | |||
| Thigh flexion / extension ROM(degrees) | Stand up with 1 dumbbell | 72 (69–76) |
73 (70–77) |
N | Y | ||
| Lift 15-lb box, no turn | 65 (58–76) |
63 (55–67) |
N | N | |||
| Lift 30-lb box, no turn | 66 (61–74) |
66 (52–70) |
Y | N | |||
| Lower 15-lb box, no turn | 64 (61–72) |
60 (50–66) |
N | Y | |||
| Lower 30-lb box, no turn | 65 (57–75) |
62 (50–68) |
Y | N | |||
| Walk with 15-lb box | 36 (34–37) |
36 (35–41) |
N | Y | |||
EMG = electromyogram, RA = rectus abdominis, ES = erector spinae, MT = middle trapezius, MVC = maximum voluntary contraction, ROM = range of motion, LRR = left/right rotation. Y = yes, N = no.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of interest statement
The authors declare no conflicts of interest. HeroWear representatives provided standard consumer training on use of the exosuit prior to data collection, but did not otherwise influence the work.
References
- Alemi MM, Geissinger J, Simon AA, Chang SE, & Asbeck AT (2019). A passive exoskeleton reduces peak and mean EMG during symmetric and asymmetric lifting. Journal of Electromyography and Kinesiology, 47, 25–34. 10.1016/j.jelekin.2019.05.003 [DOI] [PubMed] [Google Scholar]
- Amandels S, het Eyndt HO, Daenen L, & Hermans V (2018). Introduction and testing of a passive exoskeleton in an industrial working environment. Proceedings of the 20th Congress of the International Ergonomics Association (IEA 2018; ), 387–392. [Google Scholar]
- Baltrusch SJ, van Dieën JH, Koopman AS, Näf MB, Rodriguez-Guerrero C, Babič J, & Houdijk H (2020). SPEXOR passive spinal exoskeleton decreases metabolic cost during symmetric repetitive lifting. European Journal of Applied Physiology, 120, 401–412. 10.1007/s00421-019-04284-6 [DOI] [PubMed] [Google Scholar]
- Correia C, Nuckols K, Wagner D, Zhou YM, Clarke M, Orzel D, … Walsh CJ (2020). Improving grasp function after spinal cord injury with a soft robotic glove. IEEE Transactions on Neural Systems and Rehabilitation Engineering, 28(6), 1407–1415. 10.1109/TNSRE.2020.2988260 [DOI] [PubMed] [Google Scholar]
- Faber GS, Kingma I, Chang CC, Dennerlein JT, & van Dieën JH (2020). Validation of a wearable system for 3D ambulatory L5/S1 moment assessment during manual lifting using instrumented shoes and an inertial sensor suit. Journal of Biomechanics, 102, 109671. [DOI] [PubMed] [Google Scholar]
- Goršič M, Regmi Y, Johnson AP, Dai B, & Novak D (2020). A pilot study of varying thoracic and abdominal compression in a reconfigurable trunk exoskeleton during different activities. IEEE Transactions on Biomedical Engineering, 67(6), 1585–1594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goršič M, Rochelle LAE, Layer JS, Smith DT, Novak D, & Dai B (2020). Biomechanical comparisons of back and front squats with a straight bar and four squats with a transformer bar. Sports Biomechanics, in press. 10.1080/14763141.2020.1832563 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hermens HJ, Frerisk B, Merletti R, Stegeman D, Blok J, Rau G, … Hägg G (1999). European Recommendations for Surface Electromyography: Results of the SENIAM project. Enschede, Netherlands: Roessingh Research and Development. [Google Scholar]
- Huysamen K, de Looze M, Bosch T, Ortiz J, Toxiri S, & O’Sullivan LW (2018). Assessment of an active industrial exoskeleton to aid dynamic lifting and lowering manual handling tasks. Applied Ergonomics, 68, 125–131. [DOI] [PubMed] [Google Scholar]
- James SL, Abate D, Abate KH, Abay SM, Abbafati C, Abbasi N, … Murray CJL (2018). Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. The Lancet, 392, 1789–1858. 10.1016/S0140-6736(18)32279-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kermavnar T, de Vries AW, de Looze MP, & O’Sullivan LW (2021). Effects of industrial back-support exoskeletons on body loading and user experience: an updated systematic review. Ergonomics, in press. [DOI] [PubMed] [Google Scholar]
- Koopman AS, Näf M, Baltrusch SJ, Kingma I, Rodriguez-Guerrero C, Babič J, … van Dieën JH (2020). Biomechanical evaluation of a new passive back support exoskeleton. Journal of Biomechanics, 105, 109795. 10.1016/j.jbiomech.2020.109795 [DOI] [PubMed] [Google Scholar]
- Koopman AS, Toxiri S, Power V, Kingma I, van Dieën JH, Ortiz J, & de Looze MP (2019). The effect of control strategies for an active back-support exoskeleton on spine loading and kinematics during lifting. Journal of Biomechanics, 91, 14–22. 10.1016/j.jbiomech.2019.04.044 [DOI] [PubMed] [Google Scholar]
- Kozinc Ž, Baltrusch S, Houdijk H, & Šarabon N (2021). Short-term effects of a passive spinal exoskeleton on functional performance, discomfort and user satisfaction in patients with low back pain. Journal of Occupational Rehabilitation, 31(1), 142–152. 10.1007/s10926-020-09899-7 [DOI] [PubMed] [Google Scholar]
- Lamers EP, Soltys JC, Scherpereel KL, Yang AJ, & Zelik KE (2020). Low-profile elastic exosuit reduces back muscle fatigue. Scientific Reports, 10, 15958. 10.1038/s41598-020-72531-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lamers EP, Yang AJ, & Zelik KE (2018). Feasibility of a biomechanically-assistive garment to reduce low back loading during leaning and lifting. IEEE Transactions on Biomedical Engineering, 65(8), 1674–1680. 10.1109/TBME.2017.2761455 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lamers EP, & Zelik KE (2021). Design, modeling, and demonstration of a new dual-mode back-assist exosuit with extension mechanism. Wearable Technologies, 2, e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmidt K, Duarte JE, Grimmer M, Sancho-Puchades A, Wei H, Easthope CS, & Riener R (2017). The Myosuit: Bi-articular anti-gravity exosuit that reduces hip extensor activity in sitting transfers. Frontiers in Neurorobotics, 11, 57. 10.3389/fnbot.2017.00057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swain CTV, Pan F, Owen PJ, Schmidt H, & Belavy DL (2020). No consensus on causality of spine postures or physical exposure and low back pain: A systematic review of systematic reviews. Journal of Biomechanics, 102, 109312. 10.1016/j.jbiomech.2019.08.006 [DOI] [PubMed] [Google Scholar]
- Tsuneyasu K, Ohno A, Fukuda S, Ogawa K, Tsuji T, & Kurita Y (2018). A soft exoskeleton suit to reduce muscle fatigue with pneumatic artificial muscles. AH ‘18: Proceedings of the 9th Augmented Human International Conference. 10.1145/3174910.3174933 [DOI] [Google Scholar]
- Yandell MB, Wolfe AE, Marino MC, Harris MP, & Zelik KE (2020). Effect of a back-assist exosuit on logistics worker perceptions, acceptance and muscle activity. International Symposium on Wearable Robotics (WeRob). [Google Scholar]


