Abstract
Rheumatoid arthritis (RA) is a chronic, progressive and systemic autoimmune disease mainly characterized by symmetric multijoint synovitis. Quercetin has anti-inflammatory, anti-oxidation and immune regulation activities, and therefore shows high medicinal value. The present study aimed to observe the effect of quercetin on fibroblast-like synoviocytes (FLSs) in RA. Rheumatoid arthritis fibroblast-like synoviocytes (RAFLSs) were pretreated with 50 nmol/l quercetin for 2 h and were then stimulated using TNF-α for 24 h for subsequent experiments. RAFLSs were transfected with short interfering (si)-X-inactive specific transcript (XIST), microRNA (miR)-485 mimic, miR-485 inhibitor or si-PSMB8 or combination. ELISA, PCR and western blotting was used to evaluate the effect of quercetin on RAFLSs treated with TNF-α. It was revealed that quercetin inhibited the production of inflammatory cytokines and the expression of XIST in RAFLSs induced by TNF-α. Bioinformatics analysis indicated that XIST acted as a sponge for miR-485 and that proteasome subunit β type-8 (PSMB8) was a direct target of miR-485. Moreover, PSMB8 functioned as a suppressor in inflammatory cytokine production of RAFLSs induced by TNF-α. Overall, quercetin was observed to inhibit the production of inflammatory cytokines and the expression of XIST in RAFLSs induced by TNF-α. Moreover, XIST-silencing could suppress the inflammatory reaction by sponging miR-485 in cells treated with TNF-α. Altogether, quercetin could suppress the development of RA in vitro.
Keywords: rheumatoid arthritis, quercetin, X-inactive specific transcript, microRNA-485, proteasome subunit β type-8
Introduction
Rheumatoid arthritis (RA) is a common inflammatory disease characterized by inflammatory cell infiltration that leads to degeneration of the synovium, articular cartilage and bone (1). The occurrence and development of RA involves the release of a large number of inflammatory cytokines and mediators, which causes irreversible destruction of cartilage and bone in the joint (2). With the increase of an ageing population in human society, the incidence of RA has shown an increased trend in developed countries from 1995 to 2001 (3,4). Currently, RA treatment relies on non-steroidal anti-inflammatory drugs, glucocorticoids, methotrexate and other symptomatic methods of controlling the disease. These drugs can improve the symptoms of RA, but long-term use has strong toxic side effects, such as inhibiting the immune function of the body (5). Therefore, finding safe and effective drugs for the treatment of RA is of great importance.
Quercetin is the most important bioflavonoid in the human diet, and is widely found in the flowers, leaves and fruits of plants (6,7). Quercetin has anti-inflammatory, anti-oxidation and immune regulation activities (8,9), and therefore shows high medicinal value. Clinical studies have shown that quercetin has a good effect on relieving knee osteoarthritis, as well as rheumatoid joint and body pain after exercise (10-12). Fibroblast-like synoviocytes (FLSs) are the main effector cells and can release a variety of inflammatory cytokines, aggravating the progression of RA (13,14). In addition, TNF-α can promote the activation and bone resorption of osteoclasts, and can induce the expression of other inflammatory factors, adhesion molecules and proteases associated with bone and cartilage; thus, causing the thickening of the synovial lining layer and further exacerbating the inflammatory response of the joints (15). The present study therefore aimed to observe the effect of quercetin on FLSs in RA and explore the possible mechanism of quercetin in the treatment of RA.
Materials and methods
Cell culture
The primary cells RAFLSs were attained from The Cell Bank of the Type Culture Collection of The Chinese Academy of Sciences (cat. no. 408-05a). All cells were maintained in DMEM (Invitrogen; Thermo Fisher Scientific, Inc.) containing 10% FBS (HyClone; Cytiva) 100 U/ml penicillin and 100 µg/ml streptomycin in an incubator at 37˚C. After culturing for 24 h, RAFLSs were pretreated with 50 nmol/l quercetin (MilliporeSigma) for 2 h at 37˚C and then were stimulated using 50 ng/ml TNF-α for 24 h at 37˚C for the following experiments.
Cell transfection
Small interfering (si)-RNAs targeting XIST (si-XIST; final concentration, 20 nM) and its scrambled negative control (NC) siRNA (final concentration, 20 nM), miR-485 inhibitor (final concentration, 30 nM) and scrambled inhibitor control (miR-NC; final concentration, 30 nM) and miR-485 mimics (final concentration, 15 nM) and scrambled mimic control (miR-NC mimics; final concentration, 15 nM) were obtained from Shanghai GenePharma Co., Ltd. A total of 1x106 RAFLSs were plated into six-well plates for 12 h, then the constructs were transfected into RAFLSs by mixing with Lipofectamine® 2000 reagent (Invitrogen; Thermo Fisher Scientific, Inc.) at 37˚C for 15 min following the manufacturer's instructions. A total of 24-72 h after transfection, the transfected cells were collected for subsequent experiments. The sequences of the transfected molecules were as follows: si-XIST, 5'-GCAAAUGAAAGCUACCAAU-3'; si-NC, 5'-AAUUCUCCGAACGUGUCACGU-3'; miR-485 inhibitor, 5'-UCACGCGAGCCGAACGAACAAA-3'; anti-miR-NC, 5'-CAGUACUUUUGUGUAGUACAAA-3'; miR-485 mimic, 5'-GUCAUACACGGCUCUCCUCUCU-3'; miR-NC, 5'-UUCUCCGAACGUGUCACGUTT-3'.
Enzyme-linked immunosorbent assay (ELISA)
The concentration of inflammatory cytokines in transfected and non-transfected RAFLSs (IL-1β, IL-6 and IL-8) was determined using ELISA kits (cat. nos. KE00021, KE00139 and KE00006; Proteintech Group, Inc.) following the manufacturer's protocol. A microplate reader was used to read the absorbance at 450 nm.
Reverse transcription-quantitative (RT-q)PCR analysis
Total cellular RNAs were extracted from transfected and non-transfected RAFLSs using the TRIzol® reagent (Invitrogen; Thermo Fisher Scientific, Inc.). cDNA synthesis was performed using Maxima Probe qPCR Master mix (Fermentas; Thermo Fisher Scientific, Inc.) according to the manufacturer's instructions. Quantitative analysis of XIST and PSMB8 expression was performed using SYBR® Premix Ex Taq™ reagent (Takara Bio, Inc.) and GAPDH was used as the endogenous control. Thermocycling conditions were as follows: 94˚C for 3 min; 40 cycles of 94˚C for 30 sec, 55˚C for 30 sec and 72˚C for 1 min; and 72˚C for 10 min. The expression level of miR-485 was analyzed using SYBR® PrimeScript™ miRNA RT-PCR kit (Takara Biotechnology Co., Ltd.) and U6 small nuclear RNA was used as the internal reference. Thermocycling conditions were as follows: Denaturation at 95˚C for 10 sec; 40 cycles of 95˚C for 5 sec and 60˚C for 20 sec; followed by dissociation curve analysis at 95˚C for 60 sec, 55˚C for 30 sec and 95˚C for 30 sec. Primers were purchased from Sangon Biotech Co., Ltd., and primer sequences were as follows: GAPDH Forward, 5'-CTTTGGTATCGTGGAAGGACTC-3' and reverse, 5'-GTAGAGGCAGGGATGATGTTCT-3'; U6 forward, 5'-GCTTCGGCAGCACATATACTAAAAT-3' and reverse, 5'-CGCTTCACGAATTTGCGTGTCAT-3'; lncRNA XIST forward, 5'-AATGGAACGGGCTGAGTTTTAC-3' and reverse, 5'-TCATCCGCTTGCGTTCATAG-3'; miR-485 forward, 5'-CAGAGGCTGGCCGTGAT-3' and reverse, 5'-GTCGTATCCAGTGCAGGGTCCGAGGTATTCGCACTGGATACGACGAATTC-3'; PSMB8 forward, 5'-GCTGCCTTCAACATAACATCA-3' and reverse, 5'-CTGCCACCACCACCATTA-3'. The relative expression was analysis using 2-ΔΔCq (16).
Western blotting
Total protein was isolated from RAFLSs using pre-cold RIPA lysis buffer (Beyotime Institute of Biotechnology) including protease inhibitor. Total protein was quantified using a BCA protein assay kit (Pierce; Thermo Fisher Scientific, Inc.). A total of 30 µg protein sample per lane were separated by 10% SDS-PAGE, and subsequently transferred onto a nitrocellulose membrane (MilliporeSigma). The membranes were blocked with 5% non-fat milk at room temperature for 1 h. Subsequently, the membranes were incubated overnight at 4˚C with primary antibodies targeted against: PSMB8 (1:1,000; cat. no. ab180606) and GAPDH (1:1,000; cat. no. ab181602) (all from Abcam). The membranes were incubated with a horseradish peroxidase-labeled anti-rabbit IgG secondary antibody (1:1,000; sc-2027; Santa Cruz Biotechnology, Inc.) at room temperature for 1 h. Protein bands were visualized using an ECL detection kit (Pierce; Thermo Fisher Scientific, Inc.) and analyzed with Quantity One v4.6.2 software (Bio-Rad Laboratories, Inc.). GAPDH was used as the loading control.
Luciferase reporter assay
The XIST fragments and PSMB8 3'-untranslated regions containing wild-type (WT) or mutant (MUT) miR-485 binding sites were attained from Shanghai GenePharma Co., Ltd. They were cloned into the firefly luciferase gene reporter vector pmiRGLO (Promega Corporation). The plasmid was synthesized by Invitrogen; Thermo Fisher Scientific, Inc. Then 48 h after transfection using Lipofectamine® 2000 reagent (Invitrogen; Thermo Fisher Scientific, Inc.) at 37˚C with 5% CO2, the luciferase assay was performed using the dual-luciferase reporter assay system kit (Promega Corporation) according to the manufacturer's instructions. The luciferase activity was analyzed using a Modulus single-tube multimode reader (Promega Corporation) in comparison with Renilla luciferase activity. The following sequences were used: XIST-WT Forward, 5'-CGCCAGCTTCGACAATTCGAC-3', and reverse, 5'-ACTTGAAGCGGCCATACGTTGACAA-3'; XIST-MUT forward, 5'-TCAAAACCCAACTAGAGGACGATTTGTGA-3', and reverse, 5'-AACCCAGAAAACCGTACGGCAATCGT-3'; PSMB8-WT forward, 5'-CCGCTAAGTCCGAGTAGTCA-3', and reverse, 5'-ATAAGAATGCGGCCGAATTCATGGGAA-3'; and PSMB8-MUT forward, 5'-TTAGGACACGCATCGGATTACGCTATTAT-3', and reverse, 5'-GACACCTGTTTACGGCTACCCGCAAATATGCCAA-3'.
Bioinformatics analysis
The binding sites between miR-485 and XIST, as well as miR-485 and PSMB8 were predicted by StarBase v2.0 (http://www.microrna.gr/lncBase) or TargetScan software v7.1 (http://www.targetscan.org/vert_71/), respectively.
Statistical analysis
All measured data are expressed as the mean ± standard deviation. Differences were calculated with paired Student's t-test for comparisons between two groups or one-way ANOVA followed by Dunnett's or Tukey's post hoc test for multiple comparisons. All statistical analyses were performed using GraphPad Prism 5.0 (GraphPad Software, Inc.) and SPSS 14.0 (SPSS, Inc.). P<0.05 was considered to indicate a statistically significant difference. Experiments were repeated three times.
Results
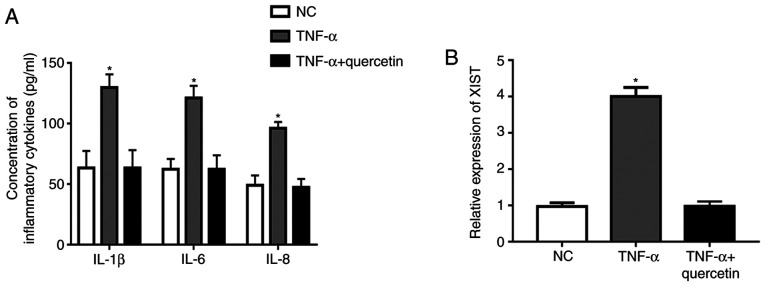
Quercetin inhibits the production of inflammatory cytokines and the expression of XIST in RAFLSs induced by TNF-α
Under TNF-α stimulation, the concentration of inflammatory cytokines (IL-1β, IL-6 and IL-8) and the expression level of XIST were significantly upregulated in RAFLSs compared with those in the NC (Fig. 1A and B). However, treatment with quercetin could markedly suppress the promotion of TNF-α in the production of inflammatory cytokines, and the expression level of XIST was markedly decreased in the FLSs (Fig. 1A and B). These results indicated that quercetin could suppress the inflammation reaction in RAFLSs induced by TNF-α.
Figure 1.
Quercetin inhibits the expression level of XIST and the production of inflammatory cytokines in FLSs induced by TNF-α. (A) Under TNF-α stimulation, the concentrations of inflammatory cytokines (IL-1β, IL-6 and IL-8) were increased in RAFLSs, which was suppressed by quercetin. (B) Under TNF-α stimulation, the expression level of XIST was significantly upregulated in RAFLSs, which was suppressed by quercetin. *P<0.05 vs. NC group. XIST, X-inactive specific transcript; RAFLSs, rheumatoid arthritis fibroblast-like synoviocytes; NC, negative control.
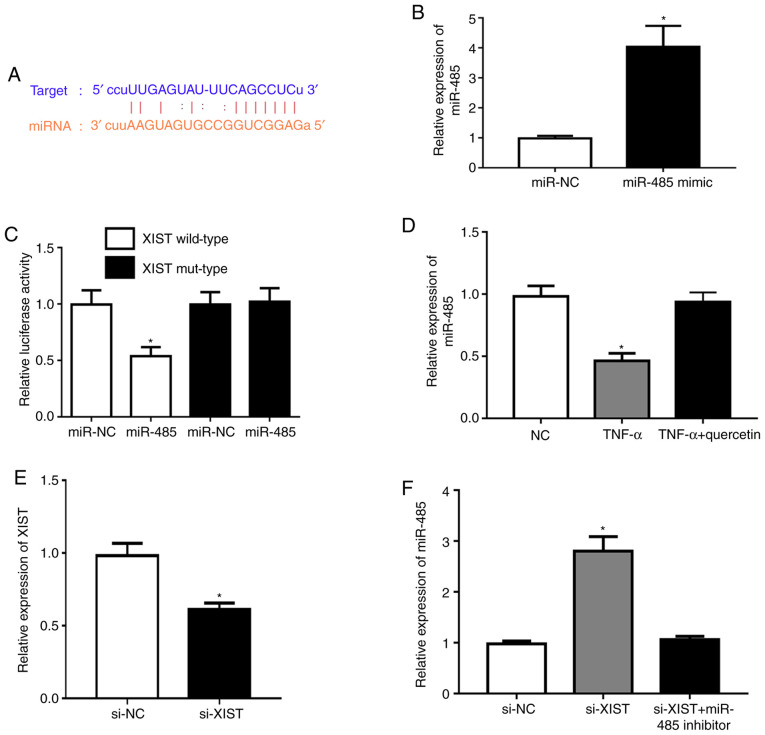
XIST acts as a sponge for miR-485
Subsequently, the potential molecular mechanisms were explored and the possible targets of XIST were predicted using the StarBase database v2.0. The bioinformatics analysis indicated that miR-485 had a potential binding site with the XIST sequence (Fig. 2A). Transfection with the miR-485 mimic was demonstrated to upregulate the expression of miR-485 in RAFLSs (Fig. 2B). Meanwhile, the miR-485 mimic markedly repressed luciferase activity in the XIST wild-type compared with that in the NC (Fig. 2C). TNF-α could significantly downregulate the expression level of miR-485 in RAFLSs, which was rescued by quercetin (Fig. 2D). XIST was significantly underexpressed in RAFLSs after transfection with si-XIST (Fig. 2E). In addition, XIST-silencing significantly promoted the expression of miR-485, which was reversed by the miR-485 inhibitor in RAFLSs treated with TNF-α (Fig. 2F). These results indicated that XIST interacted with miR-485.
Figure 2.
XIST acts as a sponge for miR-485. (A) Potential binding site of miR-485 with the XIST sequence. (B) miR-485 mimic upregulated the expression of miR-485 in RAFLSs. (C) Luciferase activity reporter assays demonstrated that the miR-485 mimic inhibited luciferase activity in the XIST wild-type. (D) TNF-α could downregulate the level of miR-485 expression in RAFLSs, which was rescued by quercetin. (E) The expression of XIST was significantly downregulated in RAFLSs transfected with si-XIST. (F) XIST-silencing effectively promoted the expression of miR-485, which was abolished by miR-485 inhibitor in RAFLSs treated with TNF-α. *P<0.05 vs. NC group. XIST, X-inactive specific transcript; miR/miRNA, microRNA; NC, negative control; si-, short interfering; mut; mutant; RAFLSs, RA fibroblast-like synoviocytes.
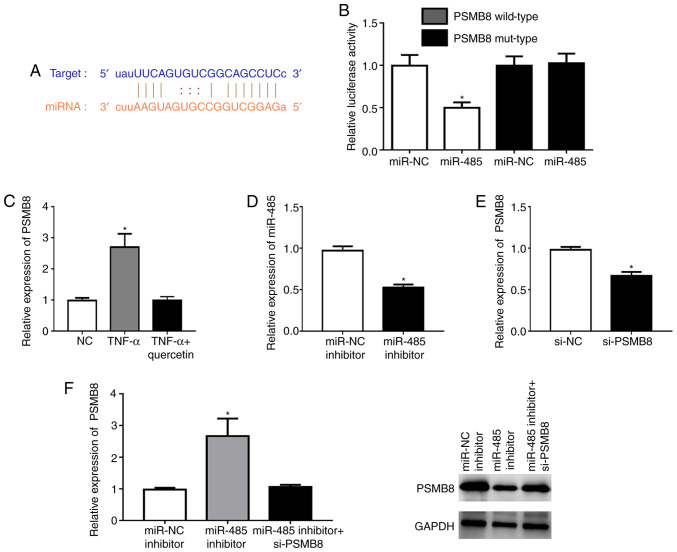
PSMB8 is a direct target of miR-485
According to TargetScan analysis, a highly conserved putative binding site with miR-485 was identified at the PSMB8 3'-untranslated region (Fig. 3A). The miR-485 mimic significantly repressed the fluorescence in the PSMB8 wild-type compared with that in the NC (Fig. 3B). TNF-α could significantly upregulate the expression level of PSMB8 in RAFLSs, which was reversed by quercetin (Fig. 3C). The miR-485 inhibitor could significantly downregulate the expression level of miR-485 in RAFLSs (Fig. 3D). In addition, the expression of PSMB8 was significantly decreased in RAFLSs after transfection with si-PSMB8 (Fig. 3E). miR-485 inhibitor could significantly enhance the expression of PSMB8 at the mRNA and protein levels, which was abolished by si-PSMB8 in RAFLSs treated with TNF-α (Fig. 3F). These results indicated that miR-485 directly targeted PSMB8.
Figure 3.
PSMB8 is a direct target of miR-485. (A) A highly conserved putative binding site with miR-485 was identified at the PSMB8 3'-untranslated region. (B) miR-485 mimic could repress the fluorescence in the PSMB8 wild-type. (C) TNF-α could significantly upregulate the level of PSMB8 expression in RAFLSs, which was reversed by quercetin. (D) miR-485 inhibitor could downregulate the expression of miR-485 in RAFLSs. (E) Expression of PSMB8 was significantly decreased in RAFLSs after transfection with si-PSMB8. (F) miR-485 inhibitor could significantly increase PSMB8 expression at the mRNA and protein levels, which was abolished by si-PSMB8 in RAFLSs treated with TNF-α. *P<0.05 vs. NC group. PSMB8, proteasome subunit β type-8; miR/miRNA, microRNA; si-, short interfering; NC, negative control; RAFLSs, rheumatoid arthritis fibroblast-like synoviocytes.
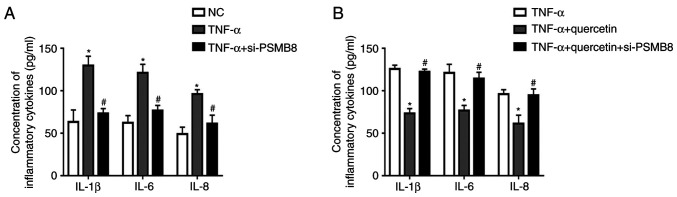
PSMB8 functions as a suppressor in the production of inflammatory cytokines in RAFLSs induced by TNF-α
After transfection with si-PSMB8, the concentrations of inflammatory cytokines (IL-1β, IL-6 and IL-8) were significantly decreased in transfected RAFLSs treated with TNF-α compared with the untransfected cells treated with TNF-α (Fig. 4A). Furthermore, quercetin suppressed the inflammatory reaction in RAFLSs under TNF-α stimulation, which was rescued by transfection with si-PSMB8 (Fig. 4B). These results indicated that PSMB8 could suppress the inflammation reaction in RAFLSs induced by TNF-α.
Figure 4.
PSMB8 functions as a suppressor in inflammatory cytokine production of RAFLSs induced by TNF-α. (A) After transfection with si-PSMB8, the concentration of inflammatory cytokines (IL-1β, IL-6 and IL-8) was decreased in RAFLSs treated with TNF-α. (B) Quercetin did not suppress the inflammation reaction in RAFLSs treated with si-PSMB8 under TNF-α stimulation. *P<0.05 vs. NC group; #P<0.05 vs. TNF-α group. PSMB8, proteasome subunit β type-8; RAFLSs, RA fibroblast-like synoviocytes; si-, short interfering; NC, negative control
Discussion
As a natural active product from plants, quercetin is a secondary metabolite isolated and extracted from fagaceae plants by natural medicinal chemistry (17). In previous years, quercetin has been verified to inhibit the inflammatory response in a number of diseases, including malignant tumors (18), diabetic mellitus (19) and atherosclerosis (20). The present study assessed the role of quercetin on the development of RA. It is hypothesized that once fibroblasts are activated in the pathogenesis of RA, a series of inflammatory factors and extracellular matrix degrading enzymes will be produced to mediate the inflammatory response, causing the progressive destruction of bone and cartilage, and influencing the quality of life severely (21,22). The present study observed that quercetin suppressed the inflammatory cytokine production of FLSs induced by TNF-α.
As a class of non-coding transcripts, lncRNAs are >200 nucleotides in length and regulate gene expression at the epigenetic, transcriptional and post-transcriptional levels (23,24). lncRNA XIST was originally identified in the regulation of X inactivation in the female mammal somatic cell (25). Previous research suggests that deregulated expression of XIST is involved in the inflammatory reaction of some diseases including inflammatory neuralgia and acute pneumonia (26,27). Consistent with previous research, the present study found that the expression level of XIST was upregulated in FLSs induced by TNF-α, which was abolished by quercetin. lncRNAs can regulate gene expression by sponging miRNAs (28). Bioinformatics analysis indicated that miR-485 had a potential binding site with the XIST sequence. In addition, the level of miR-485 expression was downregulated in FLSs treated with TNF-α. Additionally, XIST-silencing effectively promoted miR-485 expression in cells after transfection.
miRNAs can target the 3'-untranslated region of mRNAs to control gene expression (29). The present study revealed that PSMB8 is a direct target of miR-485. PSMB8 can function as a subunit of the immunoproteasome to induce an inflammatory response as follows. Yamagishi (30) reported that specific inhibition of PSMB8 can decrease the secretion of inflammatory factors, thus delaying the inflammation response of diabetes mellitus. Koerner et al (31) revealed that the involvement of PSMB8 in the inflammatory response is closely associated with the development of colorectal cancer. The present study revealed that TNF-α could significantly upregulate the expression level of PSMB8 in RAFLSs. Furthermore, si-PSMB8 could inhibit the concentration of inflammatory cytokines in RAFLSs treated with TNF-α. In addition, quercetin could not suppress the inflammatory reaction in RAFLSs treated with si-PSMB8 under TNF-α stimulation. These data suggested that PSMB8 functions as a suppressor in the production of inflammatory cytokines in RAFLSs induced by TNF-α.
The present study observed that the suppression of inflammatory cytokine production by quercetin in FLSs induced by TNF-α is promising in vitro. However, the effect in vivo and the effect of pharmacokinetics and penetration of the synovial membrane on quercetin have yet to be investigated. Thus, further studies are planned to attempt to study the effect of quercetin on RA in vivo.
In conclusion, the present study observed quercetin-inhibited production of inflammatory cytokines and XIST expression in RAFLSs induced by TNF-α. Moreover, XIST-silencing could suppress the inflammatory reaction by sponging miR-485 in cells treated with TNF-α. Altogether, quercetin could suppress the development of RA in vitro.
Acknowledgements
Not applicable.
Funding Statement
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present study are available from the corresponding author on reasonable request.
Authors' contributions
HTS and JPL designed experiments. WQQ and MFY performed experiments. HY analyzed the data. GCH performed the preliminary experiments and wrote the manuscript, JPL and GCH revised the manuscript. HS and GCH confirm the authenticity of all the raw data. All authors have read and approved the final manuscript.
Ethics approval and consent to participate
All patients gave informed consent and this study was approved by The Ethics Committee of Nanjing University of Chinese Medicine.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
- 1.Smolen JS, Aletaha D, McInnes IB. Rheumatoid arthritis. Lancet. 2016;388:2023–2038. doi: 10.1016/S0140-6736(16)30173-8. [DOI] [PubMed] [Google Scholar]
- 2.Firestein GS. Evolving concepts of rheumatoid arthritis. Nature. 2003;423:356–361. doi: 10.1038/nature01661. [DOI] [PubMed] [Google Scholar]
- 3.Gabriel SE, Michaud K. Epidemiological studies in incidence, prevalence, mortality, and comorbidity of the rheumatic diseases. Arthritis Res Ther. 2009;11(229) doi: 10.1186/ar2669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Klareskog L, Catrina AI, Paget S. Rheumatoid arthritis. Lancet. 2009;373:659–672. doi: 10.1016/S0140-6736(09)60008-8. [DOI] [PubMed] [Google Scholar]
- 5.Tłustochowicz M, Śliwczyński AM, Brzozowska M, Teter Z, Marczak M. Sequentiality of treatment in the rheumatoid arthritis drug programme in the years 2009-2014. Arch Med Sci. 2018;14:569–571. doi: 10.5114/aoms.2016.58924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Garcia-Mateos R, Aguilar-Santelises L, Soto-Hernández M, Nieto-Angel R. Flavonoids and antioxidant activity of flowers of Mexican Crataegus spp. Nat Prod Res. 2013;27:834–836. doi: 10.1080/14786419.2012.704370. [DOI] [PubMed] [Google Scholar]
- 7.Harnly JM, Doherty RF, Beecher GR, Holden JM, Haytowitz DB, Bhagwat S, Gebhardt S. Flavonoid content of U.S. fruits, vegetables, and nuts. J Agric Food Chem. 2006;54:9966–9977. doi: 10.1021/jf061478a. [DOI] [PubMed] [Google Scholar]
- 8.Boots AW, Wilms LC, Swennen EL, Kleinjans JC, Bast A, Haenen GR. In vitro and ex vivo anti-inflammatory activity of quercetin in healthy volunteers. Nutrition. 2008;24:703–710. doi: 10.1016/j.nut.2008.03.023. [DOI] [PubMed] [Google Scholar]
- 9.McAnulty LS, Miller LE, Hosick PA, Utter AC, Quindry JC, McAnulty SR. Effect of resveratrol and quercetin supplementation on redox status and inflammation after exercise. Appl Physiol Nutr Metab. 2013;38:760–765. doi: 10.1139/apnm-2012-0455. [DOI] [PubMed] [Google Scholar]
- 10.Mamani-Matsuda M, Kauss T, Al-Kharrat A, Rambert J, Fawaz F, Thiolat D, Moynet D, Coves S, Malvy D, Mossalayi MD. Therapeutic and preventive properties of quercetin in experimental arthritis correlate with decreased macrophage inflammatory mediators. Biochem Pharmacol. 2006;72:1304–1310. doi: 10.1016/j.bcp.2006.08.001. [DOI] [PubMed] [Google Scholar]
- 11.Natarajan V, Krithica N, Madhan B, Sehgal PK. Formulation and evaluation of quercetin polycaprolactone microspheres for the treatment of rheumatoid arthritis. J Pharm Sci. 2011;100:195–205. doi: 10.1002/jps.22266. [DOI] [PubMed] [Google Scholar]
- 12.O'Fallon KS, Kaushik D, Michniak-Kohn B, Dunne CP, Zambraski EJ, Clarkson PM. Effects of quercetin supplementation on markers of muscle damage and inflammation after eccentric exercise. Int J Sport Nutr Exerc Metab. 2012;22:430–437. doi: 10.1123/ijsnem.22.6.430. [DOI] [PubMed] [Google Scholar]
- 13.Bustamante MF, Garcia-Carbonell R, Whisenant KD, Guma M. Fibroblast-like synoviocyte metabolism in the pathogenesis of rheumatoid arthritis. Arthritis Res Ther. 2017;19(110) doi: 10.1186/s13075-017-1303-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mor A, Abramson SB, Pillinger MH. The fibroblast-like synovial cell in rheumatoid arthritis: A key player in inflammation and joint destruction. Clin Immunol. 2005;115:118–128. doi: 10.1016/j.clim.2004.12.009. [DOI] [PubMed] [Google Scholar]
- 15.Davis JM III, Matteson EL. My treatment approach to rheumatoid arthritis. Mayo Clin Proc. 2012;87:659–673. doi: 10.1016/j.mayocp.2012.03.011. American College of Rheumatology; European League Against Rheumatism. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) method. Methods. 2001;25:402–408. doi: 10.1006/meth.2001.1262. [DOI] [PubMed] [Google Scholar]
- 17.Wang LL, Jiang MX, Xu SX, Sun QS, Zeng GY, Zhou YJ. Two acylated flavonoid glycosides from the leaves of Quercus dentata. Nat Prod Commun. 2010;5:1597–1599. [PubMed] [Google Scholar]
- 18.Lamson DW, Brignall MS. Antioxidants and cancer, part 3: Quercetin. Altern Med Rev. 2000;5:196–208. [PubMed] [Google Scholar]
- 19.Fu J, Huang J, Lin M, Xie T, You T. Quercetin promotes diabetic wound healing via switching macrophages from M1 to M2 polarization. J Surg Res. 2020;246:213–223. doi: 10.1016/j.jss.2019.09.011. [DOI] [PubMed] [Google Scholar]
- 20.Tribolo S, Lodi F, Connor C, Suri S, Wilson VG, Taylor MA, Needs PW, Kroon PA, Hughes DA. Comparative effects of quercetin and its predominant human metabolites on adhesion molecule expression in activated human vascular endothelial cells. Atherosclerosis. 2008;197:50–56. doi: 10.1016/j.atherosclerosis.2007.07.040. [DOI] [PubMed] [Google Scholar]
- 21.Firestein GS. Invasive fibroblast-like synoviocytes in rheumatoid arthritis. Passive responders or transformed aggressors? Arthritis Rheum. 1996;39:1781–1790. doi: 10.1002/art.1780391103. [DOI] [PubMed] [Google Scholar]
- 22.Zhang F, Zhang L, Zhang C. Long noncoding RNAs and tumorigenesis: Genetic associations, molecular mechanisms, and therapeutic strategies. Tumour Biol. 2016;37:163–175. doi: 10.1007/s13277-015-4445-4. [DOI] [PubMed] [Google Scholar]
- 23.Geisler S, Coller J. RNA in unexpected places: Long non-coding RNA functions in diverse cellular contexts. Nat Rev Mol Cell Biol. 2013;14:699–712. doi: 10.1038/nrm3679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mattick JS, Rinn JL. Discovery and annotation of long noncoding RNAs. Nat Struct Mol Biol. 2015;22:5–7. doi: 10.1038/nsmb.2942. [DOI] [PubMed] [Google Scholar]
- 25.Brown CJ, Ballabio A, Rupert JL, Lafreniere RG, Grompe M, Tonlorenzi R, Willard HF. A gene from the region of the human X inactivation centre is expressed exclusively from the inactive X chromosome. Nature. 1991;349:38–44. doi: 10.1038/349038a0. [DOI] [PubMed] [Google Scholar]
- 26.Sun W, Ma M, Yu H, Yu H. Inhibition of lncRNA X inactivate-specific transcript ameliorates inflammatory pain by suppressing satellite glial cell activation and inflammation by acting as a sponge of miR-146a to inhibit Nav 1.7. J Cell Biochem. 2018;119:9888–9898. doi: 10.1002/jcb.27310. [DOI] [PubMed] [Google Scholar]
- 27.Zhang Y, Zhu Y, Gao G, Zhou Z. Knockdown XIST alleviates LPS-induced WI-38 cell apoptosis and inflammation injury via targeting miR-370-3p/TLR4 in acute pneumonia. Cell Biochem Funct. 2019;37:348–358. doi: 10.1002/cbf.3392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zeisel MB, Druet VA, Wachsmann D, Sibilia J. MMP-3 expression and release by rheumatoid arthritis fibroblast-like synoviocytes induced with a bacterial ligand of integrin alpha5beta1. Arthritis Res Ther. 2005;7:R118–R126. doi: 10.1186/ar1462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.He L, Hannon GJ. MicroRNAs: Small RNAs with a big role in gene regulation. Nat Rev Genet. 2004;5:522–531. doi: 10.1038/nrg1379. [DOI] [PubMed] [Google Scholar]
- 30.Yamagishi S. Role of advanced glycation end products (AGEs) and receptor for AGEs (RAGE) in vascular damage in diabetes. Exp Gerontol. 2011;46:217–224. doi: 10.1016/j.exger.2010.11.007. [DOI] [PubMed] [Google Scholar]
- 31.Koerner J, Brunner T, Groettrup M. Inhibition and deficiency of the immunoproteasome subunit LMP7 suppress the development and progression of colorectal carcinoma in mice. Oncotarget. 2017;8:50873–50888. doi: 10.18632/oncotarget.15141. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the present study are available from the corresponding author on reasonable request.