Abstract
While it is mandated that reproductive and child health services be provided for free at public facilities in India, qualitative evidence suggests it is common for facilities to request bribes and other informal payments for medicines, medical tests or equipment. This article examines the prevalence of bribe requests, total out-of-pocket expenditures (OOPEs) and associations between bribe requests and total OOPEs on the experience of quality of care and maternal complications during childbirth. Women who delivered in public facilities in Uttar Pradesh, India were administered a survey on sociodemographic characteristics, bribe requests, total OOPEs, types of health checks received and experience of maternal complications. Data were analysed using descriptive, bivariate and multivariate statistics. Among the 2018 women who completed the survey, 43% were asked to pay a bribe and 73% incurred OOPEs. Bribe requests were associated with lower odds of receiving all health checks upon arrival to the facility (aOR = 0.49; 95% CI: 0.24–0.98) and during labour and delivery (aOR = 0.44; 95% CI: 0.25–0.76), lower odds of receiving most or all health checks after delivery (aOR = 0.44; 95% CI: 0.31–0.62) and higher odds of experiencing maternal complications (aOR = 1.45; 95% CI: 1.13–1.87). Although it is mandated that maternity care be provided for free in public facilities in India, these findings suggest that OOPEs are high, and bribes/tips contribute significantly. Interventions centred on improving person-centred care (particularly guidelines around bribes), health system conditions and women’s expectations of care are needed.
Keywords: Bribes, quality of care, out-of-pocket expenditures, maternal health, India
Key Messages
Although mandated that maternity care be provided for free, women commonly reported being asked to pay a bribe or make other informal payments by staff during childbirth at public facilities in Uttar Pradesh.
Women who were asked to pay bribes received fewer health checks at every stage of labour and delivery and were more likely to experience complications during labour and delivery compared with women who were not asked to pay a bribe.
Providers and staff at health facilities should be trained on the provision of person-centred care, particularly guidelines around the request of bribes and other informal payments.
Interventions which improve health system conditions (e.g. overcrowding, stocking of essential supplies, workforce stress) and women’s expectations of care and awareness of no user fees applying to maternal care are also needed.
Introduction
The proportion of institutional deliveries, or births occurring in medical institutions, has increased dramatically in recent years, particularly in Africa and Asia (Diamond-Smith and Sudhinaraset, 2015). In India, improvements in institutional deliveries have been largely credited to national health campaigns like Janani Suraksha Yojana (JSY) (Lim et al., 2010). Launched in 2005 as one of the major components of India’s National Rural Health Mission for providing accessible, affordable and quality health care to rural or otherwise vulnerable populations, JSY is a conditional cash transfer programme that provides increased financial incentive to women who give birth in medical institutions vs at home. This difference in the financial package offered is theorized to promote changes in health-seeking behaviour and is the programme’s strategy for improving maternal mortality by increasing women’s access to skilled birth attendants and emergency obstetric care (National Health Systems Resource Center, 2011). According to JSY’s guidelines, eligible women who deliver in a public or accredited private health facility receive the equivalent of about $10 United States Dollars (USD) (Ministry of Health and Family Welfare, Government of India, 2018). In 10 ‘high-focus’ states—Uttar Pradesh (UP), Uttarakhand, Bihar, Jharkhand, Madhya Pradesh, Chhattisgarh, Himachal Pradesh, Rajasthan, Orissa and Jammu and Kashmir—where rates of institutional delivery are lowest and maternal mortality is highest, all pregnant women are eligible to participate in the JSY programme, and benefits for institutional delivery range from about $14 USD in urban areas to $20 USD in rural areas (Ministry of Health and Family Welfare, Government of India, 2018).
Within 5 years of JSY’s introduction, the proportion of institutional deliveries in high-focus states increased from 20% to 49% (Randive et al., 2013). This proportion is even higher in UP, one of the 10 ‘high-focus’ states of JSY and site of the present study, where currently 60% of deliveries take place in institutional facilities (Office of the Registrar and Census Commissioner, 2016). Still, these improvements have yet to result in the expected decreases in national and state-level maternal mortality ratios (MMR). In UP, recent data estimate the MMR to be 201 deaths per 100 000 live births (Sample Registration System, 2018a), a ratio significantly higher than that of the national average of 130 deaths per 100 000 live births as reported by the Government of India’s National Institution for Transforming India (Sample Registration System, 2018b). Furthermore, while the MMR in UP has decreased by >50% in 10 years, it remains one of the highest of any state in the country (Sample Registration System, 2018a). These sluggish reductions in MMR provide the impetus for a shift from focusing solely on increases in institutional delivery to the provision of quality maternal health care as a key mechanism for improving maternal health outcomes. Specifically, the World Health Organization (WHO) recognizes women’s experiences of care, and person-centred care in particular, as important aspects of quality of care for childbirth (Tunçalp et al., 2015).
The provision of person-centred maternity care (PCMC) is defined as the provision of care during pregnancy and childbirth that is respectful of and responsive to each woman’s individual needs, values and preferences (Institute of Medicine, 2001; Afulani et al., 2017). PCMC emphasizes a more comprehensive approach to maternity care that moves beyond the provision of essential services alone, and instead, includes dimensions such as communication, respect and dignity, and emotional support (Institute of Medicine, 2001). These dimensions of PCMC have been shown to determine patients’ perceptions of and satisfaction with the quality of care received and can also affect clinical outcomes (Sixma et al., 1998; Sun et al., 2000; Groene, 2011; Larson et al., 2014; Srivastava et al., 2015). In India, there is increasing evidence of the mistreatment of women during childbirth occurring in both private and public facilities, including experiences of abuse, stigma and discrimination, the provision of treatment without consent of the mother, and abandonment (Hulton et al., 2007; Sudhinaraset et al., 2016b; Raj et al., 2017). Another aspect of poor PCMC that is particularly salient in India is the request for bribes and informal payments. While it is mandated that reproductive and child health services be provided for free at public facilities in India, qualitative evidence suggests it is common for facilities to request bribes and other informal payments for medicines, medical tests or equipment (Bruce et al., 2015; Sudhinaraset et al., 2016a, 2016a; Vellakkal et al., 2017). Indeed, one study conducted among women living in slum communities in UP found that nearly 25% of women who had delivered within the previous 5 years were asked to pay a bribe or informal payment during childbirth (Sudhinaraset et al., 2016b).
Especially among India’s poorest women, the anticipation of bribes and other informal payments during childbirth may deter women from choosing an institutional delivery and instead encourage home deliveries (Mohanty and Srivastava, 2013; Bohren et al., 2014; Bruce et al., 2015; Vellakkal et al., 2017). In other words, requests for informal payments may be counterproductive to JSY’s core mission and underlying theoretical framework if women expect these requests to outweigh the potential financial benefit of JSY. Qualitative studies have also demonstrated a belief among women that the payment of a bribe will translate to the receipt of better, more timely care (Bohren et al., 2015; Sudhinaraset et al., 2016a). As a result, women may feel obligated to provide the payment to ensure the health of their baby.
Unfortunately, despite the qualitative evidence, there remain little quantitative data on just how common it is for women to be asked to make informal payments during childbirth, nor is there quantitative data which provide insight into the demographic characteristics of women who are most likely to be targeted for informal payments. Moreover, there are no published studies which examine the association between requests for informal payments and associated out-of-pocket expenditures (OOPEs) and maternal care quality indicators. Increasing our understanding of when and among whom bribes and other informal payments occur, as well as how these payments relate to quality of care, will have important programme and policy implications. To that end, this study fills a critical gap in the literature by investigating: (1) the prevalence of requests for bribes; (2) whether women who are asked to pay bribes differ in their sociodemographic characteristics; and (3) if women who are asked to pay bribes experience better or worse care and outcomes during labour and delivery. This article also summarizes total OOPEs on informal payments and examines differences in mean OOPEs by sociodemographic characteristics and labour- and delivery-related quality of care indicators and outcomes.
Materials and methods
The facility sample used in this study was drawn from 727 government hospitals and clinics across UP. About 10 facilities were selected from each of UPs 75 districts to include all high-volume health facilities (performing 200 or more deliveries per month during the previous quarter). We focused on high-volume facilities because they represent hospitals and clinics where the overwhelming majority of women are delivering and therefore most representative of women’s delivery experiences in UP. These facilities included district hospitals (DH), community health centres and primary health clinics. These high-volume facilities were classified into quartiles based on clinical quality score criteria and then ranked by geographic zone and level of care. Following this stratification, 40 geographically representative facilities from the top and bottom quartiles were selected for study inclusion.
A survey was administered to ∼50 patients at each study site from August to October 2017. Information was collected on patient sociodemographic characteristics, bribe requests, types of health checks received, experiences of complications and costs incurred during labour and delivery. Women were eligible to participate if they were 18 years or older and delivered within the last 48 h. Patient recruitment and informed consent processes occurred in the post-natal ward, and informed consent was obtained from all patients in the study. Patients were able to continue with the interview at their bed or in another private space within the facility. All interviews were conducted in Hindi by trained enumerators (with 5% of all surveys back checked). Study procedures and materials were approved by the ethics review boards of the authors’ home institutions.
Being asked to pay a bribe or tip and total OOPEs incurred during childbirth were the primary variables of interest. Bribe requests were assessed by asking, ‘Did the doctors, nurses, or other staff at the facility ask you or your family for money other than the official cost?’ Tip requests were assessed by asking, ‘Were you asked to give a tip by any health worker after delivery?’ Both questions included ‘Yes’ or ‘No’ response options. A binary variable was created where a response of ‘Yes’ to either question was considered to indicate that a woman had been asked to pay a bribe or tip during or after labour and delivery. Total OOPEs were calculated by summing the reported amount paid by patients for transportation to the health facility for delivery, labour and delivery care, medicines, medical tests and tips. Missing values for any of these costs were set to 0, and the total expenditures, reported in Indian National Rupees (INR), were converted to USD using the 2017 conversion rate of 1 USD to INR 65.1 (Reserve Bank of India, 2018).
Other variables of interest included various individual-level sociodemographic characteristics (e.g. age, education, occupation, caste) and labour- and delivery-related quality of care indicators and outcomes. Women were asked if they had received benefits of the JSY programme (‘Yes’ or ‘No’; responses of ‘Do not know’ were categorized as ‘No’). Facilities were categorized into one of four levels of care: primary health clinic (PHC), community health clinic (CHC), first referral unit community health centre (FRU-CHC) and DH. Quality of care received upon arrival to the facility and during labour and delivery was assessed by asking women if a health provider checked their blood pressure, checked their pulse, timed contractions, listened to the baby’s heartbeat and performed a vaginal examination. To assess the quality of care received after delivery, women were asked if a health provider checked their blood pressure, checked their pulse, examined their abdomen, examined their perineum, checked for bleeding, examined the baby, checked to ensure breastfeeding was going well and asked if urine and stool were being easily passed. Responses were used to create ordinal variables assessing the number of health checks performed at each stage of labour and delivery (‘None’, ‘Few’, ‘Most’ or ‘All’). Experience of complications was assessed by asking women, ‘At any time just during the delivery did you suffer from any problems?’ and ‘At any time during labour and after delivery did you suffer from any problems?’ Each question had response options of ‘Yes’ or ‘No’, and those who responded ‘Yes’ were then asked to indicate the type of problem(s) experienced. A binary variable was created where a response of ‘Yes’ to either question was considered to indicate that a woman had experienced complications during or after labour and delivery.
Data were analysed using descriptive, bivariate and multivariate statistics using StataSE 15.1 (StataCorp, 2017). Pearson’s chi-square, t-tests and one-way analysis of variance (ANOVA) were used to examine differentials in being asked to pay a bribe or tip and mean OOPEs by sociodemographic characteristics, facility level of care, and labour and delivery quality of care indicators and outcomes. Multinomial logistic regression was used to further examine the associations between requests for bribes or tips and OOPEs and each of the three quality of care indicators (i.e. number of health checks performed). Multiple logistic regression was used to examine the associations between requests for bribes or tips and OOPEs on the experience of complications during labour and delivery. All logistic regression analyses controlled for facility level of care and key sociodemographic characteristics. For the logistic regression analyses examining the association between bribes and OOPEs on the number of health checks performed after delivery, the ‘Most’ and ‘All’ categories were collapsed as the number of women who received all health checks after delivery was too small to conduct meaningful analyses.
Results
Among the 2018 women who completed the survey, >40% of were asked to pay a bribe or tip during childbirth. Sociodemographic characteristics stratified by bribe or tip request, as well as results of chi-square tests, are presented in Table 1. Monthly income was found to be associated with a request for bribe or tip; a higher proportion of women who were asked to pay a bribe had a monthly household income of $150 or more (26.0% vs 21.5%, P < 0.001). Being asked to pay a bribe or tip was not found to be associated with any other sociodemographic characteristics.
Table 1.
Demographic characteristics of women delivering across level of care in Uttar Pradesh, India, stratified by request for bribe or tip, N (%)
| Characteristic | Total (N = 2018) | Asked to pay bribe or tip |
P-valuea | |
|---|---|---|---|---|
| No (N = 1155) | Yes (N = 863) | |||
| Age (years) | 0.59 | |||
| 18–24 | 990 (49.1) | 572 (49.5) | 418 (48.4) | |
| 25–30 | 860 (42.6) | 493 (42.7) | 367 (42.5) | |
| 31-46 | 168 (8.3) | 90 (7.8) | 78 (9.0) | |
| Education | 0.97 | |||
| None | 564 (28.0) | 316 (27.4) | 248 (28.7) | |
| Some primary or primary | 377 (18.7) | 217 (18.8) | 160 (18.5) | |
| Eight | 387 (19.2) | 223 (19.3) | 164 (19.0) | |
| Secondary or vocational | 441 (21.9) | 256 (22.2) | 185 (21.4) | |
| College or higher | 249 (12.3) | 143 (12.4) | 106 (12.3) | |
| Occupation | 1.00 | |||
| Unemployed or homemaker | 1905 (94.4) | 1091 (94.5) | 814 (94.3) | |
| Agricultural labour | 40 (2.0) | 23 (2.0) | 17 (2.0) | |
| Casual labour | 38 (1.9) | 22 (1.9) | 16 (1.9) | |
| Salaried worker | 18 (0.9) | 10 (0.9) | 8 (0.9) | |
| Self-employed in petty trade | 17 (0.8) | 9 (0.8) | 8 (0.9) | |
| Place of residence | 0.14 | |||
| Rural | 1725 (85.5) | 999 (86.5) | 726 (84.1) | |
| Urban | 293 (14.5) | 156 (13.5) | 137 (15.9) | |
| Religionb | 0.65 | |||
| Hindu | 1675 (83.1) | 955 (82.8) | 720 (83.5) | |
| Muslim | 341 (16.9) | 199 (17.2) | 142 (16.5) | |
| Caste | 0.45 | |||
| Other backward class | 1112 (55.1) | 632 (54.7) | 480 (55.6) | |
| Scheduled caste/tribes | 574 (28.4) | 340 (29.4) | 234 (27.1) | |
| General | 332 (16.5) | 183 (15.8) | 119 (17.3) | |
| Monthly Income (US dollars) | <0.001 | |||
| Less than $50 | 447 (22.2) | 294 (25.5) | 153 (17.7) | |
| $50–$99 | 709 (35.1) | 398 (34.5) | 311 (36.0) | |
| $100–$149 | 390 (19.3) | 215 (18.6) | 175 (20.3) | |
| $150 or more | 472 (23.4) | 248 (21.5) | 224 (26.0) | |
| Wealth Quintile | 0.32 | |||
| Poorest | 404 (20.0) | 236 (20.4) | 168 (19.5) | |
| Poorer | 404 (20.0) | 220 (19.1) | 184 (21.3) | |
| Middle | 403 (20.0) | 226 (19.6) | 177 (20.5) | |
| Richer | 404 (20.0) | 226 (19.6) | 178 (20.6) | |
| Richest | 403 (20.0) | 247 (21.4) | 156 (18.1) | |
| Parity (including this delivery) | 0.54 | |||
| 1 | 706 (35.0) | 407 (35.2) | 299 (34.7) | |
| 2 | 609 (30.2) | 351 (30.4) | 258 (29.9) | |
| 3 | 393 (19.5) | 213 (18.4) | 180 (20.9) | |
| 4+ | 310 (15.4) | 184 (15.9) | 126 (14.6) | |
Percentages may not add to 100 due to rounding.
P-values are for Pearson’s chi-square tests.
Missing: n = 2.
Labour- and delivery-related characteristics stratified by bribe or tip request, as well as results of chi-square and t-tests, are provided in Table 2. Three-quarters of women reported to have received benefits from JSY, and no differences were detected between women who were asked to pay a bribe or tip and those who were not. More than one-third of all women delivered in a DH. Women who were asked to pay a bribe or tip were significantly more likely than those who were not to have delivered in a CHC (31.5% vs 20.1%; P < 0.0001). Mean OOPEs incurred during labour and delivery were significantly higher among women who were asked to pay a bribe or tip compared with those who were not ($8.18 vs $3.82; P < 0.0001). In general, women who were asked to pay a bribe or tip received fewer health checks during all stages of labour and delivery (all with a P < 0.0001) and were also more likely to experience complications (20.5% vs 15.2%; P < 0.01) compared with women not asked to pay a bribe or tip. Among all women, postpartum haemorrhage, difficulty breathing, dizziness, excessive vomiting, abdominal pain and fever were the most commonly reported complications experienced (data not shown).
Table 2.
Labour and delivery characteristics of women delivering across levels of care in Uttar Pradesh, India, N (%)
| Characteristic | Total (N = 2018) | Asked to pay bribe or tip |
P-valuea | |
|---|---|---|---|---|
| No (N = 1155) | Yes (N = 863) | |||
| Received JSY programme benefits | 1528 (75.7) | 879 (76.1) | 649 (75.2) | 0.64 |
| Level of facility | <0.0001 | |||
| Primary health clinic | 202 (10.0) | 153 (13.3) | 49 (5.7) | |
| Community health centre | 504 (25.0) | 232 (20.1) | 272 (31.5) | |
| First referral unit community health centre | 609 (30.2) | 356 (30.8) | 253 (29.3) | |
| District hospital | 703 (34.8) | 414 (35.8) | 289 (33.5) | |
| Total out-of-pocket medical expenditures (in US dollars); mean (SD) | 18.35 (12.6) | 3.82 (6.27) | 8.18 (7.24) | <0.0001 |
| Total number of health checks performed upon facility arrival; mean (SD) | 2.27 (1.34) | 2.47 (1.39) | 2.02 (1.34) | <0.0001 |
| Number of health checks performed upon facility arrival | <0.0001 | |||
| None | 57 (2.8) | 32 (2.8) | 25 (2.9) | |
| Few (1–2) | 1171 (58.0) | 599 (51.9) | 572 (66.3) | |
| Most (3–4) | 613 (30.4) | 395 (34.2) | 218 (25.3) | |
| All | 177 (8.8) | 129 (11.2) | 48 (5.6) | |
| Total number of health checks performed during labour and delivery; mean (SD) | 1.82 (1.30) | 2.01 (1.38) | 1.57 (1.15) | <0.0001 |
| Number of health checks performed during labour and delivery | <0.0001 | |||
| None | 184 (9.1) | 95 (8.2) | 89 (10.3) | |
| Few (1–2) | 1313 (65.1) | 692 (59.9) | 621 (72.0) | |
| Most (3–4) | 392 (19.4) | 270 (23.4) | 122 (14.1) | |
| All | 129 (6.4) | 98 (8.5) | 31 (3.6) | |
| Total number of health checks performed after delivery; mean (SD) | 1.56 (1.75) | 1.83 (1.88) | 1.19 (1.48) | <0.0001 |
| Number of health checks performed after delivery | <0.0001 | |||
| None | 774 (38.4) | 373 (32.3) | 401 (46.5) | |
| Few (1–3) | 982 (48.7) | 591 (51.2) | 391 (45.3) | |
| Most (4–7) | 246 (12.2) | 177 (15.3) | 69 (8.0) | |
| All | 16 (0.8) | 14 (1.2) | 2 (0.2) | |
| Experienced complications during or after labour and delivery | 353 (17.5) | 176 (15.2) | 177 (20.5) | <0.01 |
Percentages may not add to 100 due to rounding.
P-values are for Pearson’s chi-square tests (categorical variables) and t-test (means).
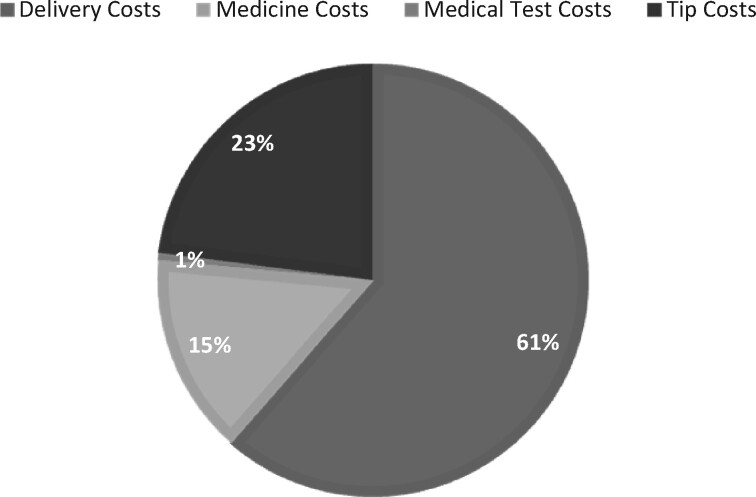
Approximately 73% of women incurred OOPEs during labour and delivery. A total of 930 (46.1%) women reported paying for delivery care, 549 (27.2%) for transportation costs, 438 (21.7%) for medications/medicines and 449 (21.2%) for tips to health workers; paying for medical tests was rare, reported by only 17 (0.8%) of women (data not shown). A breakdown of where women spent the most money during childbirth is shown in Figure 1. The largest burden arose from delivery and tip costs (accounting for 61% and 23% of total expenditures, respectively). Among the 1467 women who reported incurring some cost during labour and delivery, the mean (SD, range) amount paid (in USD) in OOPEs was $7.82 ($7.18, $0.15–$111.00; data not shown).
Figure 1.
Where are women spending the most money during childbirth? Delivery-related costs as a percentage of total OOPEs.
An examination of differentials in mean OOPEs by sociodemographic and delivery-related characteristics and outcomes are presented in Table 3. Mean OOPEs were highest among those in the youngest age group and increased as level of education increased (both with a P < 0.01). A similar trend was found by wealth quintile, whereby mean expenditures increased as wealth increased (P < 0.0001). Women residing in urban regions of UP had higher expenditures than those in rural regions (P < 0.01). No differences in mean OOPEs were found by occupation, religion or caste.
Table 3.
Differentials in mean (standard deviation) OOPEs (in US dollars) during delivery by selected sociodemographic and delivery-related characteristics
| Characteristic | Total (N = 2018) | P-valuea |
|---|---|---|
| Age (years) | <0.01 | |
| 18–24 | 6.23 (7.26) | |
| 25–30 | 5.19 (6.99) | |
| 31–46 | 5.01 (5.68) | |
| Education | <0.01 | |
| None | 5.03 (6.17) | |
| Some primary or primary | 5.07 (6.21) | |
| Eight | 5.76 (6.14) | |
| Secondary or vocational | 6.46 (8.64) | |
| College or higher | 6.63 (7.99) | |
| Occupation | 0.14 | |
| Unemployed or homemaker | 5.71 (7.07) | |
| Agricultural labour | 5.07 (5.80) | |
| Casual labour | 4.75 (4.87) | |
| Salaried worker | 3.63 (4.05) | |
| Self-employed in petty trade | 9.27 (11.33) | |
| Place of residence | <0.01 | |
| Rural | 5.50 (7.02) | |
| Urban | 6.81 (7.08) | |
| Religionb | 0.45 | |
| Hindu | 5.64 (7.06) | |
| Muslim | 5.95 (6.98) | |
| Caste | 0.06 | |
| Other backward class | 5.80 (7.55) | |
| Scheduled caste/tribes | 5.15 (6.04) | |
| General | 6.22 (6.83) | |
| Monthly Income (US dollars) | <0.05 | |
| Less than $50 | 5.02 (5.96) | |
| $50–$99 | 5.50 (6.98) | |
| $100–$149 | 6.05 (8.20) | |
| $150 or more | 6.30 (6.99) | |
| Wealth quintile | <0.0001 | |
| Poorest | 4.23 (4.69) | |
| Poorer | 5.86 (8.33) | |
| Middle | 5.62 (7.03) | |
| Richer | 6.48 (7.16) | |
| Richest | 6.24 (7.11) | |
| Parity (including this delivery) | <0.0001 | |
| 1 | 6.67 (7.86) | |
| 2 | 5.44 (7.36) | |
| 3 | 5.25 (5.81) | |
| 4+ | 4.49 (5.41) | |
| Level of facility | <0.0001 | |
| Primary health clinic | 2.51 (3.71) | |
| Community health centre | 4.50 (5.01) | |
| First referral unit community health centre | 6.02 (6.87) | |
| District hospital | 7.16 (8.57) | |
| Received JSY programme benefits | 0.10 | |
| Yes | 5.54 (6.63) | |
| No | 6.15 (8.18) | |
| Number of health checks performed upon facility arrival | <0.0001 | |
| None | 4.25 (5.70) | |
| Few (1–2) | 5.96 (7.02) | |
| Most (3–4) | 5.96 (7.57) | |
| All | 3.39 (4.92) | |
| Number of health checks performed during labour and delivery | <0.0001 | |
| None | 6.43 (10.78) | |
| Few (1–2) | 6.12 (6.64) | |
| Most (3–4) | 4.60 (5.89) | |
| All | 3.51 (6.78) | |
| Number of health checks performed after delivery | <0.0001 | |
| None | 6.27 (6.65) | |
| Few (1–3) | 5.70 (7.24) | |
| Most (4–7) | 4.10 (7.31) | |
| All | 0.97 (2.17) | |
| Experienced complications during or after labour and delivery | <0.05 | |
| Yes | 6.50 (7.02) | |
| No | 5.51 (7.04) |
Percentages may not add to 100 due to rounding.
P-values are for t-test (binary) and ANOVA (>2 categories).
Missing: n = 2.
Significant differences in mean OOPEs were found between level of facility; expenditures were highest among women who delivered in DHs and lowest among women who delivered in PHCs ($7.16 vs $2.51, respectively; P < 0.0001). Significant differences in mean OOPEs were also detected by the number of health checks performed upon arrival to the facility, during labour and delivery, and after delivery. In general, expenditures decreased as the number of health checks performed increased (all with a P < 0.0001). For example, women who received all health checks during labour and delivery paid an average of $3.51 in OOPEs vs women who received no health checks who paid an average of $6.43. Mean OOPEs were also significantly higher among women who experienced complications compared with those who did not ($6.50 vs $5.51, P < 0.05).
Table 4 provides results of the multinomial logistic regression analyses examining associations between requests for bribes or tips and OOPEs on labour- and delivery-related quality of care indicators, as well the results of the multiple logistic regression analysis examining the association between requests for bribes or tips and OOPEs on maternal complications. After controlling for facility level of care, women’s sociodemographic characteristics, and OOPEs, women who were asked to pay a bribe or tip had significantly lower odds of receiving all health checks upon arrival to the facility (aOR = 0.49; 95% CI: 0.24–0.98), lower odds of receiving all health checks during labour and delivery (aOR = 0.44; 95% CI: 0.25–0.76), and lower odds of receiving most or all health checks after delivery (aOR = 0.44; 95% CI: 0.31–0.62). Compared with women who were not, women who were asked to pay a bribe or tip had higher odds of experiencing complications during or after delivery (aOR = 1.45; 95% CI: 1.13–1.87). Total OOPEs were no longer associated with any labour- and delivery-related quality of care indicator nor the experience of complications after controlling for other factors.
Table 4.
Logistic regression adjusted odds ratios (95% confident intervals) of labour and delivery quality of care indicators and maternal complications by requests for bribes and total OOPEs among women delivering across levels of care in Uttar Pradesh, India
| Predictor variables | All health checks performed upon facility arrivala | All health checks performed during labour and deliverya | Most or all health checks performed after deliverya | Experienced complications during or after deliveryb |
|---|---|---|---|---|
| Asked to pay bribe or tip | 0.49 (0.24–0.98)* | 0.44 (0.25–0.76)** | 0.44 (0.31–0.62)*** | 1.45 (1.13–1.87)** |
| Total OOPEs | 1.00 (0.93–1.07) | 0.96 (0.91–1.00) | 0.97 (0.94–1.00) | 1.01 (0.99–1.03) |
All models control for level of care and women’s age, education, wealth quintile, resident status, parity and religion. aOR (95% CI).
Analysed using multinomial logistic regression; Outcome is in relation to women who received no health checks at each stage of labour and delivery.
Analysed using multiple logistic regression.
P < 0.05;
P < 0.01;
P < 0.001.
Discussion
We found that >40% and 70% of women were asked to pay a bribe or tip and incurred some form of OOPE during childbirth, respectively. This corroborates results from previous qualitative studies conducted in India which had alluded to the pervasiveness of these practices (Bruce et al., 2015; Sudhinaraset et al., 2016a,b; Vellakkal et al., 2017). Asking for bribes and other informal payments may be a reflection of broader health system concerns. Although not focused on bribe requests alone, one systematic review by Bohren and colleagues (2015) sheds light on the potential drivers of the mistreatment of women during childbirth globally, including important health system conditions and constraints related to understaffing, high patient volume, long hours coupled with low wages and lack of infrastructure. Indeed, an evaluation of the JSY programme in high-focus states conducted on behalf of the Government of India in 2010 touched upon some of these exact health system constraints that occurred after the rapid increase in institutional delivery following the programme’s roll-out. For example, at the time of the evaluation, only 10% of public health facilities were providing 90% of delivery services, resulting in severe overcrowding, provider shortages and frequent supply stock-outs (National Health Systems Resource Center, 2011). Health systems constraints, therefore, may contribute to the need for facility staff to ask for bribes or tips and for women to incur OOPEs on supplies that should be available in public health facilities.
Results from mostly qualitative studies conducted globally have suggested that requests for bribes typically occur among poorer, less-educated women or women of lower social status (Rahmani and Brekke, 2013; Bohren et al., 2015; Sudhinaraset et al., 2016b; Warren et al., 2017). However, in this study, we found bribe requests to be significantly more prevalent among women with the highest monthly household income and found no other differences in bribe requests by, e.g. age, education, wealth or caste. This may partly explain why we find higher levels of bribe or tip requests (40%) compared with previous estimates of 25% among slum populations specifically (Sudhinaraset et al., 2016b) . It is possible that women of higher socio-economic status would be targeted for bribe requests more frequently because of health workers’ assumptions around their ability to fulfil these requests. This is supported by our finding that women with higher education and wealth paid significantly more in OOPEs. A study by Mohanty and Srivastava (2013) using nationally representative data from 2004 to 2008 also found that delivery-related OOPEs increased with increasing educational attainment and wealth index in both public and private facilities in India. Nevertheless, paying a bribe or making informal payments may be particularly economically catastrophic for India’s most socially disadvantaged women; this may in part explain why past studies have paid specific attention to poorer women, contributing to the perception that bribe and OOPEs occur mostly among this population. Certainly, informal payments can result in families being unable to anticipate the true costs associated with pregnancy and delivery, becoming a source of financial and emotional stress and placing greater burden on families who may have to borrow money from relatives or sell household goods to pay for childbirth (Modugu et al., 2012; Sudhinaraset et al., 2016a). Thus, delivering in a health facility may be a source of and perpetuate cycles of health and social inequities for women in India.
Another important and surprising finding was that those who are asked to pay bribes or tips received poorer care. We found that higher proportions of women who were asked to pay a bribe or tip received fewer health checks at every stage of labour and delivery and were more likely to experience maternal complications, even after controlling for level of care, women’s sociodemographic characteristics and total OOPEs. Again, this is contrary to other studies which found that women believe the payment of a bribe will translate to health workers providing improved, more timely care (Bohren et al., 2015; Sudhinaraset et al., 2016a), although a number of potential explanations exist. First, it is possible that being asked to pay a bribe is indicative of the quality of the facility where labour and delivery took place. Facilities where these practices are common may be more likely to provide poorer clinical care in general or be ill-equipped to provide quality clinical care due to, e.g. staff or equipment shortages. Second, it is plausible that the number of check-ups received is more an indicator of health problems than one of quality care. That is, providers may be more likely to request bribes from women who require extra attention and more check-ups than women who need fewer check-ups. Relatedly, women’s experience of complications may prompt health workers to make bribe and tip requests as a means of recovering the additional costs associated with providing necessary care. Indeed, we found OOPEs to be statistically significantly higher among women who received more health checks and experienced complications than those who did not. Third, it is possible that the significant associations found between requests for bribes or tips and the receipt of fewer health checks and increased odds of complications are suggestive of a woman’s refusal or inability to provide a bribe. In the systematic review by Bohren and colleagues (2015), the authors found that health workers were perceived to ignore women until a bribe was paid, at which point, the health workers would then become attentive to the woman’s needs. Another study among recent mothers living in slum communities in UP found that women reported being denied labour and delivery care altogether if bribes or informal payments were not paid (Sudhinaraset et al., 2016a). Taken together, these studies suggest that the refusal or inability to pay a bribe or tip may be met with poorer quality of care in the form of fewer health checks being performed, which would then lead to increased risk of complications. Additional studies employing mixed-method designs are warranted to help further disentangle the various mechanisms for explaining this surprising result, paying particular attention to potential differences across facility level.
The present study has a number of limitations. While the study identifies whether women were requested to pay a bribe or tip, we did not collect data on the timing of when requests occurred or if and when these requests were fulfilled. Information on these factors would have been useful for investigating the potential mechanisms for which bribe requests are associated with fewer health checks and increased odds of complications. Another limitation of the study is the generalizability of the results. Our results are representative of public health facilities in UP, but may not be generalizable to private facilities, which make up 18% of deliveries in the state (Office of the Registrar and Census Commissioner, 2016), or to other states in India. The study also focused on high-volume facilities, so the results may not be generalizable to lower-volume facilities; however, different types of high-volume facilities were represented including DHs, community health centres and PHCs. One study conducted in UP found that women who delivered in lower-level facilities, such as PHCs, were more likely to report receiving better PCMC compared with women who attended higher-level facilities (Montagu et al., 2019); therefore, we would hypothesize that lower-volume facilities would potentially also report improved PCMC. Future studies should focus on investigating differences in bribes and OOPEs across different facility levels and the drivers that may predict such outcomes. Also, inaccurate recall of requests for bribes and tips, payments for various delivery-related costs, health checks received and complications experienced may have introduced error in our measurements. Although given that interviews were conducted within 48 h of delivery, we expect the impact of recall bias to be limited. Moreover, it is unclear whether women can accurately recognize bribe and tip requests, are aware of what would constitute payments beyond the official costs in order to accurately report such payments or recognize symptoms which would constitute ‘problems’ or complications associated with labour and delivery. This may have also contributed error in the measurement of these constructs. Furthermore, questions on requests for bribes and tips are centred on health workers and did not specifically ask about requests for bribes or tips from other facility personnel, such as guards and receptionists, who have been previously documented as demanding payments from women and/or their families during delivery (Bohren et al., 2014). Importantly, the definition of bribes and tips may differ between women and be context-specific, and women may not have felt comfortable reporting a bribe or tip request while still at the facility where interviews were conducted. Therefore, these results may underestimate the prevalence of bribe and tip requests.
Despite these limitations, this study offers several important programmatic, policy and future research implications. First, providers and staff at health facilities should be trained on the provision of person-centred care, particularly guidelines around bribe and tip requests. The qualitative arm of this study conducted with health workers has shown that there is a very fine line between what is considered a tip and what is considered a bribe. As an expression of their joy and contentment, family members willingly pay some amount to health workers and providers, which may be considered a cultural norm. While it may be common in India for women to give a tip out of genuine gratitude, providers should be trained to not ask women for tips as it may be misconstrued as a bribe request. Second, facilities may need quality improvement interventions focused on improving transparency among providers and staff. This may include facility managers working with staff to develop a culture of transparency—actions that should specifically include not accepting bribes and signage that reminds women and staff alike that tips are not necessary. Alternatively, it can also include transparent feedback mechanisms from women to the health facilities. Accountability for bribes should be enforced with clear punishments for facilities with high bribe and OOPE requests and clear rewards for those without. Third, the government should ensure that there are sufficient funds available for facilities to be adequately stocked with those supplies and equipment essential for care before, during and after delivery. A well-stocked facility and adequate supply chain, coupled with improvements in workforce availability and distribution, will minimize the need for women to incur OOPEs. Fourth, community programmes should focus on improving women’s expectations of care, including knowing their rights as patients in a health facility and empowering women to demand better care. Relatedly, programmes must ensure that knowledge around user fees not applying to pregnancy and delivery care in public facilities must be widespread. Importantly, women should also be educated that informal payments do not necessarily result in improved quality of care. As we also found that the average amount of OOPEs paid during labour and delivery account for a significant proportion of the JSY conditional cash transfer benefit, it is essential that OOPEs associated with pregnancy and delivery be eliminated to continue increasing institutional deliveries in India. Lastly, while this study was conducted in public health facilities in India, the issue of bribes is a significant concern in the region and globally (McMahon et al., 2014; Abuya et al., 2015; Balde et al., 2017; Bohren et al., 2019), with a cultural or gendered component to who pays bribes and for what purposes. Future studies should examine the role of bribes in maternity care across global settings to better understand the contexts, causes and consequences in which bribes are requested.
Acknowledgements
This work was supported by the Bill and Melinda Gates Foundation (BMGF) [OPP1127467]. The authors wish to acknowledge Dominic Montagu, Katie Giessler and Nadia Diamond-Smith for providing feedback on results from the manuscript, as well as the Community Empowerment Lab research team who rigorously conducted the data collection. We also give special thanks to the survey respondents and the facility staff and leadership at each health centre in Uttar Pradesh.
Conflict of interest statement. None declared.
Ethical approval. All study procedures and materials were approved by the Institutional Review Boards of the University of California San Francisco (study #: 15-18008) in San Francisco, CA, USA and Community Empowerment Lab in Lucknow, Uttar Pradesh, India. All subjects provided informed consent prior to the initiation of any study procedures.
References
- Abuya T, Warren CE, Miller N et al. 2015. Exploring the prevalence of disrespect and abuse during childbirth in Kenya. PLoS One 10: e0123606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Afulani PA, Diamond-Smith N, Golub G, Sudhinaraset M. 2017. Development of a tool to measure person-centered maternity care in developing settings: validation in a rural and urban Kenyan population. Reproductive Health 14: 118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balde MD, Diallo BA, Bangoura A et al. 2017. Perceptions and experiences of the mistreatment of women during childbirth in health facilities in Guinea: a qualitative study with women and service providers. Reproductive Health 14: 3. doi:10.1186/s12978-016-0266-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bohren MA, Hunter EC, Munthe-Kaas HM et al. 2014. Facilitators and barriers to facility-based delivery in low- and middle-income countries: a qualitative evidence synthesis. Reproductive Health 11: 71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bohren MA, Mehrtash H, Fawole B et al. 2019. How women are treated during facility-based childbirth in four countries: a cross-sectional study with labour observations and community-based surveys. Lancet 394: 1750–63. doi:10.1016/S0140-6736(19)31992-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bohren MA, Vogel JP, Hunter EC et al. 2015. The mistreatment of women during childbirth in health facilities globally: a mixed-methods systematic review. PLoS Medicine 12: e1001847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruce SG, Blanchard AK, Gurav K et al. 2015. Preferences for infant delivery site among pregnant women and new mothers in Northern Karnataka, India. BMC Pregnancy and Childbirth 15: 49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diamond-Smith N, Sudhinaraset M. 2015. Drivers of facility deliveries in Africa and Asia: regional analyses using the demographic and health surveys. Reproductive Health 12: 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Groene O. 2011. Patient centredness and quality improvement efforts in hospitals: rationale, measurement, implementation. International Journal for Quality in Health Care 23: 531–7. [DOI] [PubMed] [Google Scholar]
- Hulton LA, Matthews Z, Stones RW. 2007. Applying a framework for assessing the quality of maternal health services in urban India. Social Science & Medicine 64: 2083–95. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. 2001. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academy Press. [PubMed] [Google Scholar]
- Larson E, Hermosilla S, Kimweri A, Mbaruku GM, Kruk ME. 2014. Determinants of perceived quality of obstetric care in rural Tanzania: a cross-sectional study. BMC Health Services Research 14: 483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lim SS, Dandona L, Hoisington JA et al. 2010. India’s Janani Suraksha Yojana, a conditional cash transfer programme to increase births in health facilities: an impact evaluation. The Lancet 375: 2009–23. [DOI] [PubMed] [Google Scholar]
- McMahon SA, George AS, Chebet JJ et al. 2014. Experiences of and responses to disrespectful maternity care and abuse during childbirth; a qualitative study with women and men in Morogoro Region, Tanzania. BMC Pregnancy and Childbirth 14: 268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ministry of Health and Family Welfare, Government of India. 2018. Janani Suraksha Yojana: Background [WWW Document]. National Health Mission. http://nhm.gov.in/nrhm-components/rmnch-a/maternal-health/janani-suraksha-yojana/background.html, accessed 31 October 2018. [Google Scholar]
- Modugu HR, Kumar M, Kumar A, Millett C. 2012. State and socio-demographic group variation in out-of-pocket expenditure, borrowings and Janani Suraksha Yojana (JSY) programme use for birth deliveries in India. BMC Public Health 12: 1048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohanty SK, Srivastava A. 2013. Out-of-pocket expenditure on institutional delivery in India. Health Policy and Planning 28: 247–62. [DOI] [PubMed] [Google Scholar]
- Montagu D, Landrian A, Kumar V et al. 2019. Patient-experience during delivery in public health facilities in Uttar Pradesh, India. Health Policy and Planning 34: 574–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Health Systems Resource Center. 2011. Programme Evaluation of the Janani Suraksha Yoyana. New Delhi, India: Ministry of Health and Family Welfare, Government of India. [Google Scholar]
- Office of the Registrar and Census Commissioner. 2016. Annual Health Survey Report—A Report on Core and Vital Health Indicators, Part 1. New Delhi: Ministry of Home Affairs, Government of India.
- Rahmani Z, Brekke M. 2013. Antenatal and obstetric care in Afghanistan—a qualitative study among health care receivers and health care providers. BMC Health Services Research 13: 166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raj A, Dey A, Boyce S et al. 2017. Associations between mistreatment by a provider during childbirth and maternal health complications in Uttar Pradesh, India. Maternal and Child Health Journal 21: 1821–33. [DOI] [PubMed] [Google Scholar]
- Randive B, Diwan V, Costa AD. 2013. India’s conditional cash transfer programme (the JSY) to promote institutional birth: is there an association between institutional birth proportion and maternal mortality? PLoS One 8: e67452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reserve Bank of India. 2018. Reference Rate Archive [WWW Document]. https://www.rbi.org.in/scripts/referenceratearchive.aspx, accessed 1 September 2018.
- Sample Registration System. 2018a. Maternal Mortality Ratio (MMR) (per 100000 live births) [WWW Document]. Office of Registrar General, India. http://niti.gov.in/content/maternal-mortality-ratio-mmr-100000-live-births, accessed 31 August 2018.
- Sample Registration System. 2018b. Special Bulletin on Maternal Mortality in India 2014-16. New Delhi, India: Office of Registrar General India.
- Sixma HJ, Kerssens JJ, Campen CV, Peters L. 1998. Quality of care from the patients’ perspective: from theoretical concept to a new measuring instrument. Health Expectations 1: 82–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Srivastava A, Avan BI, Rajbangshi P, Bhattacharyya S. 2015. Determinants of women’s satisfaction with maternal health care: a review of literature from developing countries. BMC Pregnancy and Childbirth 15: 97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- StataCorp. 2017. Stata Statistical Software: Release 15.1. College Station, TX: StataCorp LP. [Google Scholar]
- Sudhinaraset M, Beyeler N, Barge S, Diamond-Smith N. 2016a. Decision-making for delivery location and quality of care among slum-dwellers: a qualitative study in Uttar Pradesh, India. BMC Pregnancy and Childbirth 16: 148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sudhinaraset M, Treleaven E, Melo J, Singh K, Diamond-Smith N. 2016b. Women’s status and experiences of mistreatment during childbirth in Uttar Pradesh: a mixed methods study using cultural health capital theory. BMC Pregnancy and Childbirth 16: 332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun BC, Adams J, Orav EJ et al. 2000. Determinants of patient satisfaction and willingness to return with emergency care. Annals of Emergency Medicine 35: 426–34. [PubMed] [Google Scholar]
- Tunçalp Ö, Were W, MacLennan C et al. 2015. Quality of care for pregnant women and newborns—the WHO vision. BJOG 122: 1045–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vellakkal S, Reddy H, Gupta A et al. 2017. A qualitative study of factors impacting accessing of institutional delivery care in the context of India’s cash incentive program. Social Science & Medicine 178: 55–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warren CE, Njue R, Ndwiga C, Abuya T. 2017. Manifestations and drivers of mistreatment of women during childbirth in Kenya: implications for measurement and developing interventions. BMC Pregnancy and Childbirth 17: 102. [DOI] [PMC free article] [PubMed] [Google Scholar]