Key words: Cardiometabolic, Cardiovascular disease, Fasting triglycerides, Non-fasting triglycerides, Postprandial triglycerides, Risk screening, Triglyceride-rich lipoproteins
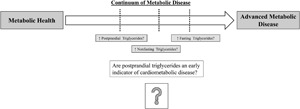
Fasting triacylglycerols have long been associated with cardiovascular disease (CVD) and other cardiometabolic conditions. Evidence suggests that non-fasting triglycerides (i.e. measured within 8 h of eating) better predict CVD than fasting triglycerides, which has led several organisations to recommend non-fasting lipid panels as the new clinical standard. However, unstandardised assessment protocols associated with non-fasting triglyceride measurement may lead to misclassification, with at-risk individuals being overlooked. A third type of triglyceride assessment, postprandial testing, is more controlled, yet historically has been difficult to implement due to the time and effort required to execute it. Here, we review differences in assessment, the underlying physiology and the pathophysiological relevance of elevated fasting, non-fasting and postprandial triglycerides. We also present data suggesting that there may be a distinct advantage of postprandial triglycerides, even over non-fasting triglycerides, for early detection of CVD risk and offer suggestions to make postprandial protocols more clinically feasible.
Introduction
High fasting triglycerides have been associated with cardiovascular disease (CVD) since the 1950s, and nearly one-third of Americans display elevated triglycerides (>1⋅70 mmol/l or 150 mg/dl)(1,2). Triglycerides >1⋅70 mmol/l (150 mg/dl) are also one criterion for diagnosis of the metabolic syndrome and are frequently observed in those with type 2 diabetes(3–6). Chronically elevated fasting triglycerides in the absence of a genetic lipid disorder are associated with some degree of metabolic derangement, which can include long-term positive energy balance and adipose tissue expansion, hepatic steatosis and subsequent very-low-density lipoprotein (VLDL) oversecretion and/or insulin resistance(1,7–16). In addition to their relationship with these metabolic changes, fasting triglycerides strongly correlate with other adverse, and more complex, lipid profile changes that are less easily measured (e.g. increased small, dense low-density lipoprotein (LDL), increased LDL triglycerides)(17,18). Given that 84 % of those with fasting triglycerides marginally above the recommended cut-off (i.e. >2⋅0 mmol/l or 177 mg/dl) with increased waist circumference also display elevated insulin, apolipoprotein (apo)B and small LDL-particles , fasting triglycerides are likely most useful in screening for more moderate stages of declining metabolic health(19).
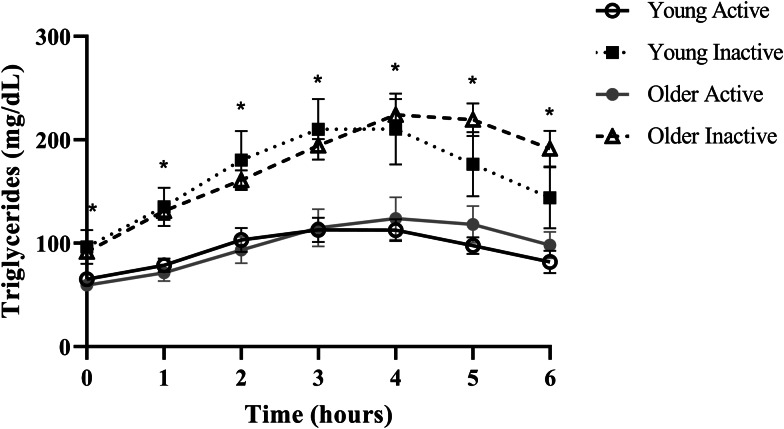
Despite triglycerides historically being measured in the fasted state, the rise in triglycerides following a meal, or postprandial lipaemia, has become increasingly examined due to epidemiological evidence that non-fasting triglycerides (i.e. triglycerides measured within 8 h of an unstandardised meal) are a strong predictor of CVD, and in some cases, more closely related to risk than fasting triglycerides(20–22). A recent report from our group in generally healthy younger (18–35 years) and older (≥60 years) individuals defined as either active (i.e. ≥150 min moderate to vigorous physical activity/week) or sedentary (i.e. <150 min moderate to vigorous physical activity/week and <30 min planned exercise/week) also illustrates this point using a postprandial triglyceride assessment (serial measurement of triglycerides after a standardised test meal). Inactive participants presented with normal fasting triglycerides (1⋅10 mmol/l or 97⋅4 mg/dl), glucose and high-density lipoprotein cholesterol (HDL-C), but following a high-fat meal challenge (Marie Callendar's chocolate pie; 12 kcal/kg; 63 % fat (47 % saturated fat)) experienced a 236 % increase in peak triglycerides (2⋅60 mmol or 230⋅3 mg/dl) and a large triglyceride area under the curve relative to active counterparts (Fig. 1)(23). Importantly, this increase in postprandial triglycerides is above the current recommended threshold for what is considered adverse (i.e. ≥2⋅48 mmol/l or 220 mg/dl), and in this population, was one of the only apparent signs of declining metabolic health(22,24). Therefore, a large postprandial lipemic response may serve as a sensitive risk detection tool in apparently healthy individuals. This exaggerated triglyceride response could be due to many factors including intestinal and hepatic triglyceride-rich lipoprotein (TRL) oversecretion, reduced LPL activity and LPL saturation(1,25–34). TRL remnants (i.e. VLDL and chylomicrons with partially hydrolysed triglyceride cargo) appear to account for the increased CVD risk in those with high post-meal triglycerides because they are selectively retained in the subintimal space, readily engulfed by macrophages in their unmodified form, and contain 5–20× the cholesterol content of LDL, making them highly atherogenic(18,35–38). Overall, a growing body of epidemiological and clinical evidence suggests that the rise in triglycerides after a meal may be a more sensitive screening tool than fasting triglycerides for detecting disease risk and may be abnormal when other traditional risk factors (i.e. fasting triglycerides, HDL-C, glucose) are in the normal range.
Fig. 1.
Postprandial triglycerides in active and inactive individuals with healthy fasting triglycerides. Despite normal fasting triglycerides, glucose, and HDL, disease-free, inactive individuals experienced an adverse postprandial triglyceride response. Young adults were 18–35 years old and older adults were ≥60 years. Physically active was defined as ≥150 min moderate to vigorous physical activity per week and physically inactive was <150 min moderate to vigorous physical activity per week and <30 min planned exercise per week. Significant differences (denoted by *; P < 0⋅05) were observed at every time point when comparing pooled inactive v. active individuals using Bonferroni corrected independent t-tests. Data reproduced with permission.
Given the usefulness of post-meal triglyceride measurement for predicting CVD, it is important to further delineate between non-fasting and postprandial triglyceride assessment, which are often described interchangeably. Measurement of non-fasting triglycerides is one such method and describes a triglyceride measurement taken anytime within 8 h of eating a free-living, unstandardised meal(22). Given this wide assessment window, non-fasting triglycerides are conveniently measured and often used in large epidemiological studies, but usually cannot control for a variety of factors that modify triglycerides (e.g. meal composition and timing, recent physical activity) and there is a possibility that peak post-meal triglycerides are not captured. The other form of triglyceride assessment after a meal is known as postprandial testing. In contrast to non-fasting triglycerides, postprandial triglyceride evaluation refers to hourly triglyceride measurement following a predetermined high-fat meal in a laboratory setting. Generally, individuals are asked to report to a research laboratory after an overnight fast, a fasting blood draw is collected and then a standardised high-fat meal (i.e. either a set bolus of fat or a high-fat meal scaled to body weight) is consumed followed by hourly triglyceride measurement for 6–8 h. Other relevant modifiers of triglycerides such as physical activity and length of the overnight fast are also controlled. Although postprandial testing is ideal for determining an individuals’ peak triglycerides after a meal challenge and captures the total triglyceride area under the curve, postprandial protocols in their current form are time-intensive and not amenable to large-scale studies or clinical practice. Nonetheless, post-meal triglycerides, in particular postprandial triglycerides, appear to be a valuable marker for detecting early disease risk, warranting more efforts to make postprandial testing more clinically feasible.
In this review, we discuss commonalities and draw clear distinctions between the underlying physiological and metabolic changes that lead to elevated fasting, non-fasting and postprandial triglycerides and the implications of these changes for different triglyceride assessment methods. We also attempt to estimate the daily triglyceride burden experienced by the average individual consuming a Western-style diet, and review key pathophysiological mechanisms by which elevated fasting and non-fasting/postprandial triglycerides likely contribute to CVD risk. Lastly, we argue that in a subset of the population, postprandial triglycerides may be the preferred form of testing, even over non-fasting triglycerides, and offer suggestions to make postprandial protocols more practical.
General overview of triglyceride metabolism
Triglycerides provide approximately 95 % of kilocalories derived from dietary fat and act as a stored energy reserve in adipose tissue. Due to their hydrophobic nature, triglycerides are transported within lipoproteins in the bloodstream along with cholesteryl ester, phospholipid and other fat-soluble molecules. In the fasted state, triglycerides are predominantly transported within apoB100 containing VLDL secreted by the liver(1). Some triglyceride is also present in intermediate-density lipoproteins and LDL, which form as VLDL triglycerides are progressively cleaved by lipoprotein lipase (LPL), releasing free fatty acids to be utilised as energy or stored. Following a meal, it is normal to observe a moderate peak in triglycerides 3–5 h after eating, 80 % of which are packaged into apoB48 containing chylomicrons produced by enterocytes(39). Chylomicrons initially enter the lymphatic system and ultimately reach the bloodstream where their triglyceride is also hydrolysed by LPL(39). However, despite dietary triglyceride being mostly carried in chylomicrons, the increase in apoB containing particles after a meal is largely explained by a rise in VLDL, as postprandial VLDL secretion is only partially suppressed by insulin (approximately 50 %), and chylomicrons are preferentially hydrolysed by LPL(34,40,41). Collectively, VLDL and chylomicrons are referred to as TRLs, and following LPL hydrolysis are termed TRL remnants. The dynamic process of TRL hydrolysis is influenced by many apolipoproteins that either activate LPL (e.g. apoC-II) or inhibit LPL such as apoC-I, apoC-III, angiopoietin-like protein-3, -4 and -8(1,42–44). After the majority of TRL-triglyceride has been hydrolysed (approximately 6–8 h after a meal), TRL remnants and LDL are cleared by hepatic receptors (i.e. LDL receptor, LDL receptor-related protein-1), which is facilitated by apoE(45–47).
Estimated daily triglyceride kinetics in Westernised countries
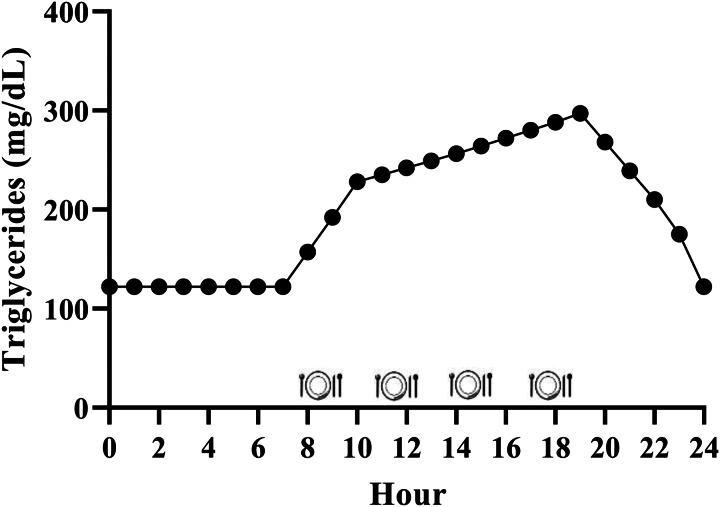
While it is generally accepted that triglycerides remain elevated for the majority of the day due to the additive effective of multiple meals, the exact magnitude is relatively unclear in the context of the typical Western dietary pattern. We have performed calculations to estimate this, and it appears that consuming the Western dietary pattern may lead to a substantial triglyceride peak, with triglycerides remaining above fasting 75 % of the day (Fig. 2). Consider the average American male whose fasting triglycerides are 1⋅37 mmol/l (122 mg/dl)(1) and who consumes approximately 2400 kcal/d(48), 35 % of which are from fat(49) over 4–5 meals and snacks. These averages equate to consumption of approximately 93 g of fat each day, or approximately 23 g per meal if divided across four meals. Taguchi and colleagues(50) determined that a similar quantity of fat (20 g) increased postprandial triglycerides by approximately 1⋅20 mmol/l (approximately 106 mg/dl) in subjects with normal fasting triglycerides <1⋅70 mmol/l (<150 mg/dl). Emerson et al. (26) demonstrated that consuming one moderate fat meal (sausage, egg, cheese, whole-grain crust; 8⋅5 kcal/kg; 30 % fat (13 % saturated fat)) containing similar total fat (22 g fat; 660 kcal), followed by the same meal 3 h later, sustained the initial triglyceride peak and caused approximately 3 % change per hour increase in serum triglycerides over the next 3 h before triglycerides began to decline. If four meals spaced 3 h apart are assumed, and postprandial triglyceride kinetics are similar following the third and fourth meals, we estimate that the average man may experience a triglyceride peak near 3⋅39 mmol/l (300 mg/dl) approximately 7 PM and will not return to baseline until approximately 1 AM (Fig. 2). Although this is a relatively crude estimate, specific meal patterns are assumed, and one would expect some differences in females due to the influence of sex hormones on triglycerides and having less visceral fat than men (presumably reducing hepatic VLDL-triglyceride secretion), it still likely provides insight into the daily triglyceride kinetics of many adults following a Western dietary pattern.
Fig. 2.
Estimated triglyceride kinetics of a typical U.S. male following a western dietary pattern. Since dietary triglycerides following a meal peak over 3–5 h, there is an additive effect of meals resulting in postprandial lipaemia during most of the day. Hour 0 represents midnight.
Statistical considerations and epidemiology of fasting, non-fasting and postprandial triglycerides
Statistical adjustments for fasting triglycerides
Although fasting triglycerides are the traditional method of triglyceride assessment, there has been extensive debate as to whether they are an independent risk factor for CVD. This controversy is largely based on whether other risk factors should be accounted for when evaluating the relationship between triglycerides and disease risk, implying that triglycerides are a correlate with metabolic disease rather than a causal factor. In most early studies where statistical adjustments were minimal, nearly all studies found that triglycerides were an independent CVD risk factor(51). However, when adjustments for other factors, such as total cholesterol, HDL-C and BMI, were made, the association between fasting triglycerides and CVD was lost in some cases(51). While this approach is logical, it should be considered that lipid concentrations often correlate with one another, an important example being the inverse relationship between triglycerides and HDL-C(52). Presently, adjusting for these risk factors and others (e.g. blood pressure, smoking status) in large epidemiological cohorts is performed when examining the relationship between triglycerides and CVD in an attempt to tease apart the most relevant risk factors in multivariate analysis.
Epidemiology of fasting triglycerides and CVD
In 1996, Hokanson and Austin(53) performed a meta-analysis of seventeen prospective studies evaluating the relationship between fasting triglycerides and fatal and non-fatal cardiac events. Univariate analysis of >46 000 men revealed that a 1⋅00 mmol (89 mg/dl) increase in fasting triglycerides was associated with a 32 % increased relative risk of incident cardiac events. Similarly, women displayed a 76 % increased relative risk for cardiovascular events in a sample of nearly 11 000 women with a 1⋅00 mmol (89 mg/dl) increase in fasting triglycerides. After adjustment for age, total cholesterol, HDL-C and LDL-C, smoking, BMI and blood pressure, these relationships were still significant, but reduced to 14 and 37 % increased risk for men and women, respectively. Therefore, this large meta-analysis observed that fasting triglycerides were independently associated with cardiac events in men and women, although this relationship was weakened, but not completely negated, when considering other risk factors.
Statistical adjustments for non-fasting triglycerides
Statistical adjustments made in studies evaluating non-fasting triglycerides and CVD risk largely include the same metabolic parameters as fasting triglycerides (e.g. other lipids, smoking, BMI). It is ideal to additionally adjust for meal timing and composition and physical activity, given that these factors have a large influence on non-fasting triglycerides and that non-fasting triglycerides can be measured within a large time frame and thus dramatically different results can be obtained depending on when the measurement is taken(54). However, this data is frequently not available in large epidemiological cohorts, and this lack of control is the primary limitation of non-fasting triglyceride assessment.
Epidemiology of non-fasting triglycerides and CVD
Several epidemiological studies have investigated the association between non-fasting triglycerides and CVD. In the Women's Health Study cohort (26 000 initially healthy women, mean follow-up of 11⋅4 years), those that fell within the top two tertiles of non-fasting triglycerides (i.e. 1⋅19–1⋅21 mmol/l (105–107 mg/dl) and ≥1⋅93 mmol/l (171 mg/dl)) were at 44 and 98 % increased risk for incident CVD in the fully adjusted model, which accounted for total and HDL-C, C-reactive protein and BMI, among other covariates(22). In contrast, the association between fasting triglycerides and CVD was lost in the fully adjusted model, suggesting that non-fasting triglycerides may have more utility than fasting triglycerides for predicting future CVD events. When reanalysing the data as quintiles, only the highest quintile of non-fasting triglycerides (≥ 2⋅43 mmol/l or 215 mg/dl) was associated with increased risk for CVD events (99 % increased relative risk) after adjustments for covariates, and again, there was no association with fasting triglycerides.
Similarly, the Copenhagen City Heart Study (approximately 14 000 men and women; mean follow-up >26 years) found that incidence of myocardial infarction, ischaemic heart disease and total mortality significantly increased within all five quintiles of non-fasting triglycerides, beginning as low as 1⋅00–1⋅99 mmol/l (89–176 mg/dl), compared with the reference group (<1⋅00 mmol or 89 mg/dl) in both men and women(21). Additionally, fully adjusted hazard ratios revealed that for every 1⋅00 mmol/l (89 mg/dl) increase in non-fasting triglycerides, women were 20 and 18 % more likely to experience myocardial infarction and death, respectively. However, in men, no relationship was observed between cardiac events or mortality and non-fasting triglycerides in the full model, despite 6–10 % increased risk for myocardial infarction, ischaemic heart disease and mortality in models adjusting only for age and HDL-C.
In the Norwegian Counties Study (86 000 men and women; mean follow-up 27 years), non-fasting triglycerides were associated with increased all-cause mortality and death from CVD in women within the main study population following adjustment for typical covariates (but not HDL-C), which included time since last meal(20). Women were at 17 % increased risk of all-cause mortality beginning at 1⋅02 mmol/l (90⋅3 mg/dl) of non-fasting triglycerides with the highest quintile (>1⋅71 mmol/l; >151⋅5 mg/dl) exhibiting 42 % increased risk. Furthermore, women in the second, third and fourth quintiles were 28–37 % more likely to die of CVD relative to the lowest quintile, and the highest quintile was associated with 77 % increased risk of CVD death. In men, these relationships were generally not observed, although a 20–21 % increased risk of death from ischaemic heart disease was seen in the two highest quintiles of non-fasting triglycerides. Interestingly, in a subset where HDL-C data was available and included in the model, for every 1 mmol/l (89 mg/dl) increase in non-fasting triglycerides, a 6 % increase risk of all-cause mortality was observed in both sexes, as well as a 6 % increased risk of death from CVD in men. Taken together, epidemiological evidence suggests that non-fasting triglycerides are associated with CVD events and death, even after adjustment for relevant confounding variables, and are arguably a better predictor of CVD than fasting triglycerides in some populations.
Statistical adjustments for postprandial triglycerides
While many of the same general and metabolic variables (e.g. age, sex, BMI, cholesterol metrics) are also often adjusted for in small postprandial studies when sample size permits, the limitations and ideal statistical adjustments relevant to non-fasting triglycerides are directly accounted for in the postprandial study design. Specifically, participants are typically asked to refrain from exercise before and during the postprandial fat tolerance test and the time since their last meal is either controlled for or recorded by study personnel by virtue of study design, removing the need for statistical adjustment. However, this level of control compromises the size of the study population, limiting the number statistical adjustments that can be made.
Epidemiology of postprandial triglycerides and CVD
To our knowledge, only one cohort study has evaluated the relationship between postprandial triglycerides determined by a controlled fat tolerance test and CVD outcomes(55). The Atherosclerosis Risk in Communities (ARIC) study administered a fat tolerance test to 559 participants and then assessed the relationship between postprandial lipaemia and CVD events over a 20-year follow-up. The liquid test meal utilised was a set bolus and composed of heavy whipping cream, ice cream, safflower oil, chocolate syrup and protein powder (1265 kcal; 105 g fat (50 % saturated fat)). Among several indicators of postprandial lipaemia (i.e. triglycerides, TRL-triglycerides, retinyl palmitate and the apoB48/apoB100 ratio), there was no relationship between postprandial lipaemia and CVD events when the population was divided into tertiles. Although this was an important first attempt to study postprandial triglycerides and CVD outcomes in an epidemiological context, the investigators acknowledged that this study was underpowered and larger-scale studies similar in study design are needed.
Genetic evidence for involvement of triglycerides in CVD
While epidemiological evidence is somewhat conflicting, genetic evidence provides another perspective on the role of triglycerides in CVD risk. That is, genetic studies consistently support some involvement of triglycerides and/or their clearance in the atherosclerotic process. For example, both rare loss-of-function mutations and more common variants in the LPL gene lead to elevated triglycerides and are associated with increased CVD risk(56,57). Similarly, variants in the APOA5 gene, another apolipoprotein involved in LPL activation, selectively increase triglycerides and the likelihood of developing CVD(58,59). Conversely, loss-of-function mutations in genes encoding LPL inhibitors (i.e. APOC3, ANGPTL4) are associated with reduced triglycerides and lower risk of CVD(60,61). Using genetic risk scores, Ference and colleagues(62) compared the risk reduction associated with lowering triglycerides and LDL-C. Interestingly, the effect of lowering triglycerides and LDL-C normalised to apoB particles were both associated with an approximately 33 % reduced risk for CVD, suggesting that there may be a benefit to lowering triglycerides specifically beyond what fibrates can generally accomplish. This genetic benefit from lowering triglycerides was attributed to a reduction in VLDL particles, which are arguably more atherogenic than LDL, albeit fewer in number(62,63). Overall, these studies demonstrate that genetic mutations leading to reduced triglycerides (regardless of fasting or non-fasting context) reduce the risk for CVD and imply that there may be a cardiovascular benefit to lowering fasting and non-fasting/postprandial triglycerides.
Mechanisms and pathophysiological relevance of high fasting triglycerides
Mechanisms leading to high fasting triglycerides
Given that there is reason to believe that triglycerides and/or post-meal triglycerides are involved in the atherosclerotic process, it is important to understand the underlying causes and potential pathophysiological relevance of elevated fasting, non-fasting and postprandial triglycerides. High fasting triglycerides are generally the result of increased VLDL-triglyceride secretion (commonly related to hepatic steatosis) and/or impaired triglyceride clearance by LPL(64) (Fig. 3(a)). These metabolic changes leading to elevated fasting triglycerides have been attributed to many factors including insulin resistance, diet and lifestyle behaviours that promote obesity and ectopic fat accumulation(7–12,65,70,71,84,85) (Table 1). Perhaps the most accepted mechanism for increasing fasting triglycerides is adipose tissue insulin resistance, leading to uninhibited lipolysis, increased free fatty acid flux to the liver and ultimately increased VLDL-triglyceride secretion(7–9,129). Indeed, the homeostatic model of insulin resistance (HOMA-IR) strongly correlates with triglyceride-rich VLDL1 secretion and VLDL1 apoB pool size(12). While visceral adipose tissue is more insulin resistant than subcutaneous fat, and consequently is often cited as a contributor to elevated triglycerides, it should be noted that the majority of free fatty acids reaching the liver are derived from peripheral depots(130,131). Lastly, enhanced hepatic de novo lipogenesis in the fasted state appears to contribute to liver fat accumulation and subsequent VLDL secretion in obese, hyperinsulinemic individuals(65).
Fig. 3.
Mechanisms leading to raised fasting v. non-fasting/postprandial triglycerides. (a) Mechanisms leading to high fasting triglycerides. Primary drivers of high fasting triglycerides appear to be hepatic steatosis (driven in part by adipose insulin resistance and lifestyle factors) and subsequent increased VLDL-triglyceride secretion. Impaired triglyceride clearance due to reduced LPL activity and enrichment of TRLs with apoC-III are also implicated in high fasting triglycerides. (b) Mechanisms leading to high non-fasting/postprandial triglycerides. In addition to mechanisms that also increase fasting triglycerides, failure of insulin to suppress postprandial VLDL secretion, competition between VLDL-triglycerides and chylomicron-triglycerides for LPL hydrolysis, and oversecretion of intestinal chylomicrons are unique drivers of high non-fasting/postprandial triglycerides. Abbreviations: apo, apolipoprotein; CHO, carbohydrate; CM, chylomicron; DNL, de novo lipogenesis; FFA, free fatty acid; LPL, lipoprotein lipase; TG, triglyceride; TRL, triglyceride-rich lipoprotein; VLDL, very-low-density lipoprotein.
Table 1.
Non-genetic factors contributing to elevated fasting and non-fasting/postprandial triglycerides
| Physiological disturbance | Pathophysiological mechanism leading to hypertriglyceridemia | Reference |
|---|---|---|
| Insulin resistance-related | ||
| Adipose insulin resistance | ↑ lipolysis and FFA flux to liver → ↑ VLDL secretion | (7–9) |
| Hepatic insulin resistance | ↑ VLDL secretion | (10–12) |
| ↑ DNL | (14,65,66) | |
| ↓ suppression of postprandial VLDL | (67,68) | |
| Reduced LPL activity | Delayed VLDL clearance in fasted state | (31–33) |
| Delayed CM and VLDL clearance postprandially | (31–33) | |
| ↑ apoC-III → LPL inhibition, impaired TRL clearance | (69) | |
| Intestinal CM over secretion | ↑ apoB48 stability, intestinal DNL and MTP stability | (28–30) |
| Diet-related | ||
| High-carbohydrate diets (>60 %) | ↑ DNL | (65,70,71) |
| High fructose intake (chronic) | ↑ visceral adipose, hepatic insulin resistance, DNL → ↑ VLDL | (72–78) |
| High fructose intake (acute) | ↑ DNL | (72,79,80) |
| Chronic positive energy balance | ↑ total, visceral and hepatic fat → ↑ VLDL production, insulin resistance | (81–83) |
| High alcohol consumption (chronic) | ↑ in VLDL secretion, inhibition of LPL, ↑ adipose lipolysis and VAT | (84–87) |
| High alcohol consumption (acute) | ↑ in VLDL secretion, inhibition of LPL | (88–90) |
| High-fat meal rich in TGs (acute) | ↑ CM secretion | (1) |
| LPL saturation | Competition between high postprandial CM and VLDL | (1) |
| Disease-related | ||
| Hypothyroidism | ↓ LPL activity | (91–93) |
| ↓ LDL uptake (contain some TG) | (93–95) | |
| Uncontrolled T1D | ↑ VLDL production | (96–98) |
| ↓ adipose LPL activity | (31,99,100) | |
| T2D | ↑ VLDL production | (4–6) |
| ↓ CM clearance | (101) | |
| ↓ activity/quantity of LPL | (31–33) | |
| ↑ apoC-III: apoC-II ratio → favours LPL inhibition, impaired TRL clearance | (102) | |
| Obesity | ↓ adipose LPL and LRP1 gene expression | (103) |
| ↑ FFA influx to liver → ↑ VLDL secretion | (1,15,16) | |
| ↑ CETP activation → ↑ transfer of TGs to HDL and LDL | (104) | |
| Hepatic steatosis/NAFLD | ↑ DNL and TG storage → ↑ VLDL secretion | (13,14) |
| Chronic kidney disease | ↓ LPL activity | (105,106) |
| ↓ apoC-II → ↓ LPL activation | (107) | |
| ↑ apoC-III → LPL inhibition, impaired TRL clearance | (106,107) | |
| Lifestyle-related | ||
| Increased visceral adipose | ↑ FFA influx to liver → ↑ VLDL secretion | (1,15,16) |
| Low muscle mass | ↓ quantity of muscle LPL | (108) |
| Physical inactivity | Lack of physical activity induced muscle LPL quantity/activity | (109–111) |
| Smoking | Potentially inflammation and insulin resistance | (112–114) |
| Other | ||
| Low blood plasma volume | ↑ circulating concentration of TGs | (115–117) |
| Age | Likely multifactorial including ↑ visceral adipose, physical inactivity, etc. | (118) |
| Sex | Women display greater apoC-III/C-II ratio than men → favours LPL inhibition, impaired TRL clearance | (119) |
| Oral contraceptive use | ↓ LPL activity, increased VLDL secretion | (120–122) |
| Pregnancy | ↑ adipose lipolysis → ↑ VLDL secretion, reduced adipose LPL activity | (123–125) |
| Menopause status | ↑ visceral fat → ↑ risk for insulin resistance | (126–128) |
Notes: Potential factors other than genetic lipid disorders leading to elevated fasting and non-fasting/postprandial triglycerides. All factors described can contribute to hypertriglyceridemia, but many cluster together and are likely interrelated. Plain text indicates factors that contribute to high fasting triglycerides and by extension also partially contribute to non-fasting/postprandial triglycerides. Highlighted and bolded rows denote factors uniquely leading to elevated non-fasting/postprandial triglycerides.
Abbreviations: apo, apolipoprotein; CETP, cholesterol ester transfer protein; CM, chylomicrons; DNL, de novo lipogenesis; FFA, free fatty acid; HDL, high-density lipoprotein; LDL, low-density lipoprotein; LPL, lipoprotein lipase; LRP1, LDL receptor-related protein-1; MTP, microsomal triglyceride transfer protein; T1D, type 1 diabetes; T2D, type 2 diabetes; TG, triglycerides; TRL, triglyceride-rich lipoprotein; VAT, visceral adipose tissue; VLDL, very-low-density lipoprotein.
From a triglyceride clearance standpoint, insulin resistance and type 2 diabetes are associated with reduced adipose LPL expression and LPL activity, interfering with hydrolysis of VLDL-triglyceride and likely prolonging VLDL particle residence time(31–33,132). Insulin resistance is also characterised by higher serum apoC-III, which contributes to high triglycerides by inhibiting apoE mediated uptake of apoB particles and reducing triglyceride hydrolysis by LPL(69).
Pathophysiological relevance of high fasting triglycerides
Despite the controversy over whether triglycerides are an independent risk factor for CVD, mechanistic work provides indirect explanations by which chronically elevated fasting triglycerides are a cardiometabolic liability. In the context of insulin resistance, triglyceride-enriched VLDL are oversecreted(10–12) and cleared more slowly than in insulin-sensitive individuals(31–33). Due to longer residence time and insulin's activation of cholesterol ester transfer protein (CETP), triglyceride in VLDL is transferred to HDL and LDL particles to a greater degree(1). After triglyceride is further hydrolysed from these HDL and LDL by hepatic lipase, they adopt a small, dense phenotype. Consequences of these small, dense LDL and HDL include impaired LDL uptake by the LDL receptor, higher likelihood LDL are retained in the subintimal space, and increased HDL degradation leading to decreased circulating HDL. Together, these adverse lipid changes are associated with increased CVD risk and can be traced back to a high hepatic triglyceride burden and VLDL secretion(1).
Another potential indirect role of disturbed triglyceride metabolism in the fasted state is a higher burden of VLDL remnants, which are rich in cholesterol and have similar properties to pro-atherogenic LDL. That is, remnants <70 nm in diameter can enter the subintimal space, are selectively retained, and may be phagocytosed by macrophages forming foam cells in their unoxidised form, thereby contributing to atherosclerotic plaque(36,133,134).
In vitro work has demonstrated TRL remnants and TRL lipolysis products have pro-inflammatory properties that may promote CVD. Specifically, TRL remnants increase monocyte adhesion to endothelial cells by upregulating protein expression of adhesion molecules (i.e. vascular cell adhesion molecule (VCAM)-1, intracellular adhesion molecule (ICAM)-1, E-selectin), increase endothelial production of tumour necrosis factor (TNF)-α and interleukin (IL)-1β, and promote platelet activation(135–137). These effects of remnants may be related to TRL enrichment of apoC-III, which is common in dyslipidemic individuals and similarly activates NF-κB and increases monocyte adhesion(138–140) and/or production of triglyceride lipolysis products by LPL which may promote inflammation and endothelial cell apoptosis(141–144).
Remnant TRLs and their high cholesterol content, rather than the triglycerides they carry, seem to be primarily responsible for the adverse effects associated with high triglycerides. However, it cannot be ignored that VLDL-triglyceride export is generally viewed as driven by increased substrate (i.e. triglyceride, fatty acids) reaching the liver(130). Therefore, regardless of the source of hepatic triglyceride (i.e. hepatic uptake of free fatty acids, de novo lipogenesis or previously accumulated hepatic triglyceride), the more VLDL that will be secreted and the more remnants that will be in circulation. Overall, high fasting triglycerides appear to indirectly promote LDL and VLDL remnant retention in the subintimal space, reduce HDL, and potentially increase inflammation and endothelial cell dysfunction.
Mechanisms and pathophysiological relevance of high non-fasting/postprandial triglycerides
Mechanisms leading to high non-fasting/postprandial triglycerides
Since the difference between non-fasting and postprandial triglycerides is related to assessment method and not the underlying physiology, we will not distinguish between these terms in this section. Several mechanisms exist that uniquely contribute to high triglycerides in the fed state, many of which are tied to insulin resistance (Fig. 3(b)). Perhaps the most intuitive pathway is the competition of newly secreted chylomicron-triglyceride and already present VLDL-triglyceride for LPL hydrolysis(1,31–33). This phenomenon occurs in both healthy and insulin-resistant individuals; however, in the context of insulin resistance, VLDL secretion is poorly suppressed and LPL activity is reduced, promoting an even greater and sustained postprandial response(31–33,67,68,101). Further exacerbating competition for LPL hydrolysis is that intestinal chylomicrons are oversecreted in insulin-resistant individuals, which appears to be due to increased stability of proteins needed for chylomicron formation (i.e. apoB48, microsomal transfer protein) and enhanced de novo lipogenesis within enterocytes(28–30). Importantly, increased chylomicron secretion and subsequent uptake of chylomicron remnants by the liver could be another mechanism contributing to hepatic steatosis, potentially exacerbating postprandial dyslipidemia in the future(130). Postprandial hepatic de novo lipogenesis was reported to be approximately 14 and 18 % greater relative to the fasted state after consumption of two consecutive high-carbohydrate mixed meals (54 % CHO, 32 % fat, 14 % pro), contributing to the postprandial triglyceride pool(145). Although fasting triglycerides are a strong predictor of peak postprandial triglycerides, these mechanisms may explain why some have a disproportionately high triglyceride response following a meal. Furthermore, one or more of these processes are likely occurring in those who have elevated non-fasting/postprandial triglycerides(23,146).
Pathophysiological relevance of high non-fasting/postprandial triglycerides
Although mechanisms involving CETP-mediated lipid exchange are relevant in the postprandial state, much attention has been paid to TRL remnants as a major pathophysiological mechanism linking postprandial lipaemia to increased CVD risk. TRL remnants are far more numerous in the fed state due to the addition of intestinal TRLs and the temporary delayed VLDL hydrolysis due to chylomicron competition and LPL saturation. Given that high-fat meals lead to increased chylomicron secretion(147), increasing dietary triglyceride will increase the number of chylomicron remnants with pro-atherogenic potential and will delay hydrolysis of existing VLDL/VLDL remnants by LPL. In the context of very pronounced postprandial lipaemia, whether diet- and/or metabolic disease-induced, remnants will have even longer residence time, increasing their likelihood of entering the subendothelial space.
High-fat meals are associated with several other pro-atherogenic changes within the postprandial period. From an inflammatory standpoint, IL-6, IL-8, TNF-α and adhesion molecules (i.e. sICAM-1, sVCAM-1) are increased in the serum following a high-fat meal(148–150). In the case of Nappo et al.(150), several of these inflammatory markers (i.e. TNF-α, IL-6 and VCAM-1) correlated with postprandial triglycerides. Similar to studies discussed with fasting triglycerides, mechanistic evidence suggests that increased postprandial inflammation may be linked to TRLs and their triglyceride lipolysis products. In an endothelial cell line treated with TRLs from hypertriglyceridemic subjects, both fasting and postprandial TRLs upregulated genes encoding adhesion molecules such as VCAM-1, E-selectin and platelet endothelial cell adhesion molecule 1 (PECAM-1), among others(151). Importantly, for many of these genes, the response was even greater when postprandial TRLs were used relative to fasting TRLs. A similar study suggested postprandial, but not fasting, TRLs increased adhesion molecule expression and low-dose TNF-α must be present(152). Fasting and postprandial TRLs similarly increased NF-κB DNA binding activity more than 2-fold in vitro, which in theory could lead to increased transcription of a host of inflammatory mediators. Taken together, fasting and postprandial TRLs may increase inflammation through similar mechanisms, but there is reason to believe that this effect is more pronounced with postprandial TRLs.
Inflammation resulting from high-fat meals, and potentially TRLs, appears to be largely explained by innate immune system activation. For example, after a fat bolus, circulating neutrophils increased by 59 % from baseline and peaked alongside postprandial triglycerides(153). Furthermore, increased serum lipopolysaccharide (LPS) and indicators of the LPS-induced innate immune response (i.e. LPS binding protein and peripheral blood mononuclear cell of toll-like receptor (TLR)-4 protein abundance) are observed postprandially(154,155). Traditionally, the increase in LPS from the gut and subsequent TLR-4 signalling has been considered a primary driver of postprandial inflammation. However, a recent report suggested that high-fat meal induced postprandial inflammation may be more related to hydrolysis of TRL-triglyceride by LPL than LPS(156). This finding is consistent with work showing that the natural lipolysis of TRL-derived saturated free fatty acids (i.e. lauric acid) promotes a TLR-4 and TLR-2-mediated immune response in monocyte/macrophage cell lines(141–143). Complement component 3 (C3) rises following a fat bolus in both healthy controls and individuals with coronary artery disease(157). In vitro evidence suggests that this phenomenon may be due to the interaction between chylomicrons and adipocytes, which prompts adipocytes to release C3(158). However, protein expression of the classical complement pathway inhibitor C4b-binding protein is increased in the postprandial period, partially bringing into question the relevance of increased postprandial C3(159).
In addition to inflammation, several other adverse effects have been associated with postprandial lipaemia. It is well-established that vascular function (as measured by flow-mediated dilation) predicts future CVD and is impaired following a high-fat meal(160,161). The negative effect of high-fat meals on vascular function may be due to increased reactive oxygen species, which both decrease nitric oxide production and reduce nitric oxide bioavailability(160,162). Indeed, many reports indicate that postprandial triglycerides, flow-mediated dilation, and/or markers of oxidative stress correlate with one another. However, these relationships are not observed universally and can be seen after a glucose bolus and mixed meals as well(153). Regardless of the instigating meal, postprandial oxidative stress likely accounts for elevated postprandial oxidised LDL(163,164), which could enhance foam cell formation. Lastly, the angiogenic factors vascular endothelial growth factor (VEGF)-A and VEGF-C increased in response to a high-fat meal, but implications of this are unclear as VEGF promotes both blood vessel growth and is implicated in plaque expansion and potentially haemorrhage(149,165,166).
Clinical implementation
While there is no clear consensus, the evidence discussed thus far suggests at minimum an indirect role of triglycerides in the atherosclerotic process, making it important to identify the best method for triglyceride assessment. In many countries, triglycerides are still largely measured and interpreted in the fasted state to avoid the influence of diet and other confounders that accompany waking hours (e.g. physical activity, meal timing). As a result, fasting triglycerides have been extensively studied and have a well-established reference range of <1⋅70 mmol/l (150 mg/dl). Another major advantage with fasting triglycerides is that only one measurement is required and results can be generated in minutes. Despite the advantages of fasting triglycerides as a screening tool, they are less predictive of disease, and appear to be less sensitive than non-fasting and postprandial triglycerides for detecting CVD risk.
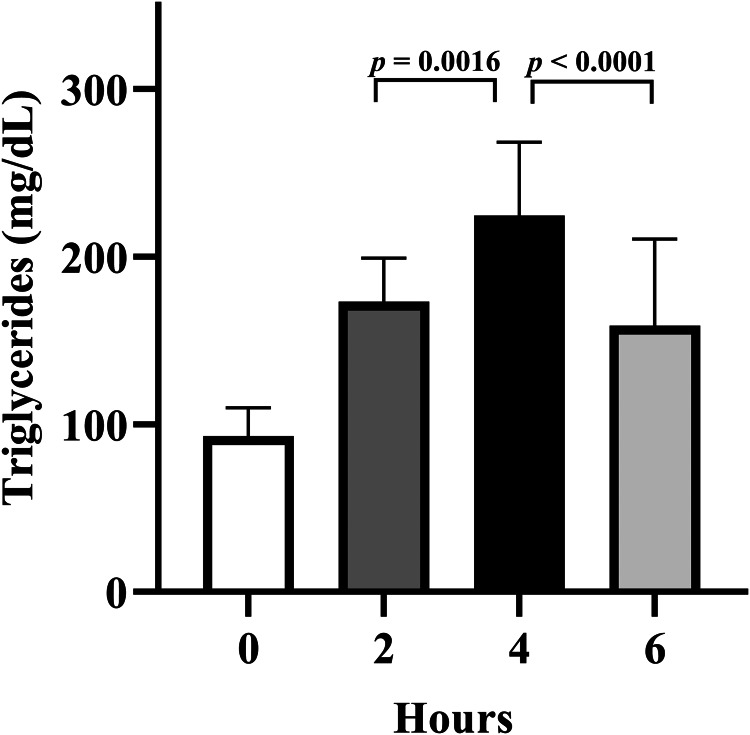
Non-fasting triglycerides include triglyceride measurements taken within 8 h of eating and are also easily measured with one blood draw. Non-fasting triglyceride measurement has not traditionally been the first choice of measurement in most countries, but several bodies including the American Heart Association, European Atherosclerosis Society, Danish Society for Clinical Chemistry, among others, now recommend non-fasting lipid panels be performed(1,24,167). Although an updated 2019 expert panel report recommends postprandial testing when non-fasting triglycerides are 1⋅30–2⋅26 mmol/l (115–200 mg/dl), European bodies and the American Heart association cut points are not as aggressive, defining ideal non-fasting triglycerides as <1⋅98 mmol/l (175 mg/dl) and <2⋅26 mmol/l (200 mg/dl), respectively(1,24). However, data from our lab suggests that individuals who have an adverse postprandial response following a fat tolerance test may be overlooked using these non-fasting reference ranges. In individuals with normal fasting triglycerides (<1⋅70 mmol/l or 150 mg/dl) subjected to a fat tolerance test who go on to have an adverse postprandial triglyceride response (≥2⋅26 mmol/l or 220 mg/dl), their mean 2-h and 6-h triglycerides are below the non-fasting recommendations of 1⋅98 and 2⋅26 mmol/l (175 and 200 mg/dl), and significantly lower than peak 4-h triglycerides (Fig. 4). Since 2 and 6 h post-meal is well within the 8-h non-fasting assessment window, and the amount of fat consumed prior to a non-fasting blood draw would often be less than in these postprandial lipid challenges, these at-risk individuals may be overlooked based on non-fasting triglycerides, but their CVD risk would be realised if subjected to a standardised fat tolerance test.
Fig. 4.
Adverse postprandial triglyceride response may not be detected with non-fasting triglyceride measurement. Individuals who presented with normal fasting triglycerides (<1⋅70 mmol/l or 150 mg/dl), yet experienced an adverse postprandial response (i.e. ≥2⋅26 mmol/l or 220 mg/dl) after being challenged with a high-fat meal (10–13 kcal/kg body mass; 61–64 % kcal from fat) were pooled from several studies (n 17). Paired t-tests were utilised to evaluate the difference between 2 v. 4 h and 4 v. 6 h. Despite this group having an adverse postprandial response, on average, they would not meet criteria for an adverse non-fasting triglyceride response at both 2 and 6 h, which are both acceptable times for non-fasting triglyceride measurement.
Postprandial triglycerides are almost exclusively measured in a research laboratory setting over periods of 6–8 h post-meal consumption with serial blood draws (often hourly). With this design, virtually all limitations of non-fasting triglycerides are addressed. Specifically, all postprandial studies control for meal composition, quantity and timing, and for exercise prior to and during the test. All of these factors make postprandial triglyceride assessment a more robust and insightful clinical measurement than non-fasting triglycerides, while still maintaining sensitivity. Unfortunately, the rigour associated with postprandial testing is expensive and time-consuming for both researchers and participants, hindering widespread adoption. In order to address these issues, ideally one, simplified fat tolerance test would be adopted by all. Our group has devoted work to this issue with some success. We recently determined that an abbreviated and simplified fat tolerance test was both valid and reliable(168,169). With this protocol, blood draws only occur at baseline and 4 h, and participants are allowed to leave the laboratory and engage in normal daily activities as long as they do not eat or perform planned exercise. This abbreviated postprandial protocol, or something similar, could be utilised in research and clinical settings for determination of postprandial lipaemia in a widespread manner.
One barrier to clinical implementation of postprandial triglyceride measurement is the absence of a standardised test meal. Across the postprandial literature, substantial variability exists in the composition of high-fat meals used to test postprandial lipaemia. In our abbreviated fat tolerance test mentioned earlier, the test meal is composed of coconut cream, chocolate syrup and protein powder (9 kcal/kg; 73 % fat (86 % saturated fat)), which allows for individuals with food allergies and/or following a vegan diet to consume it. This generally aligns well with a recommendation for oral fat tolerance testing from an expert panel(24), which recommended a set bolus of 75 g fat, 25 g carbohydrate and 10 g protein composed of whipped cream or cream cheese with added sugar. Overall, an agreed-upon standardised fat challenge is necessary before widespread implementation of postprandial triglyceride testing can be realised.
Conclusion/future directions
While much attention has been paid to reducing triglycerides as a strategy for reducing residual risk of CVD after lowering LDL-C, there is growing support of a role for post-meal triglycerides, and perhaps postprandial measurements in particular, as a tool for screening cardiometabolic risk. Nonetheless, several questions have yet to be addressed. First, in light of the opposing epidemiological evidence between non-fasting triglycerides and postprandial triglycerides, a larger prospective study focused on postprandial triglycerides specifically is needed. Based on the results of this future study and others, universally accepted reference ranges for non-fasting and postprandial triglycerides are needed that correspond with CVD risk.
In sum, our understanding of triglycerides and CVD risk has evolved dramatically since the 1950s, including the realisation that non-fasting and postprandial triglycerides appear to be useful CVD risk factors. Although there are many other useful CVD risk factors (e.g. LDL-C, HDL-C, body composition, etc.), our data and others suggest that triglycerides, in particular postprandial triglycerides, are an independent, sensitive and useful screening tool for cardiometabolic health. Future work should attempt to identify those whose CVD risk is ambiguous and would most benefit from postprandial triglyceride testing.
Acknowledgements
The authors thank Aubrey Keirns for assistance with figures and graphics.
The authors have no sources of funding to disclose.
Conceptualisation: S. R. E. and B. H. K.; Data collection: N. A. K. and C. M. S.; Data analysis: N. A. K.; Writing—original draft preparation: B. H. K.; Writing—reviewing and editing: B. H. K., S. R. E., C. M. S. and N. A. K.
The authors have no conflict of interest to disclose.
References
- 1.Miller M, Stone NJ, Ballantyne C, et al. (2011) Triglycerides and cardiovascular disease: a scientific statement from the American Heart Association. Circulation 123, 2292–2333. [DOI] [PubMed] [Google Scholar]
- 2.Gofman J, Strisower B, DeLalla O, et al. (1953) Index of coronary artery atherogenesis. Mod Med 21, 119–140. [Google Scholar]
- 3.Alberti SG, Zimmet P, Shaw J, et al. (2020) The IDF consensus wordwide definition of the metabolic syndrome. https://www.idf.org/e-library/consensus-statements/60-idfconsensus-worldwide-definitionof-the-metabolic-syndrome.
- 4.Dunn FL, Raskin P, Bilheimer DW, et al. (1984) The effect of diabetic control on very low-density lipoprotein-triglyceride metabolism in patients with type II diabetes mellitus and marked hypertriglyceridemia. Metab Clin Exp 33, 117–123. [DOI] [PubMed] [Google Scholar]
- 5.Kissebah AH, Alfarsi S, Evans DJ, et al. (1982) Integrated regulation of very low density lipoprotein triglyceride and apolipoprotein-B kinetics in non-insulin-dependent diabetes mellitus. Diabetes 31, 217–225. [DOI] [PubMed] [Google Scholar]
- 6.Malmström R, Packard C, Caslake M, et al. (1997) Defective regulation of triglyceride metabolism by insulin in the liver in NIDDM. Diabetologia 40, 454–462. [DOI] [PubMed] [Google Scholar]
- 7.Coppack S, Evans R, Fisher R, et al. (1992) Adipose tissue metabolism in obesity: lipase action in vivo before and after a mixed meal. Metab Clin Exp 41, 264–272. [DOI] [PubMed] [Google Scholar]
- 8.Baynes C, Henderson A, Hughes C, et al. (1991) Determinants of mild fasting hypertriglyceridaemia in non-insulin-dependent diabetes. J Intern Med 229, 267–273. [DOI] [PubMed] [Google Scholar]
- 9.Skowronski R, Hollenbeck C, Varasteh B, et al. (1991) Regulation of non-esterified fatty acid and glycerol concentration by insulin in normal individuals and patients with type 2 diabetes. Diabetic Med 8, 330–333. [DOI] [PubMed] [Google Scholar]
- 10.Björnsson O, Duerden J, Bartlett SM, et al. (1992) The role of pancreatic hormones in the regulation of lipid storage, oxidation and secretion in primary cultures of rat hepatocytes. Short-and long-term effects. Biochem J 281, 381–386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Olefsky JM, Farquhar JW & Reaven GM (1974) Reappraisal of the role of insulin in hypertriglyceridemia. Am J Med 57, 551–560. [DOI] [PubMed] [Google Scholar]
- 12.Gill JM, Brown JC, Bedford D, et al. (2004) Hepatic production of VLDL1 but not VLDL2 is related to insulin resistance in normoglycaemic middle-aged subjects. Atherosclerosis 176, 49–56. [DOI] [PubMed] [Google Scholar]
- 13.Adiels M, Taskinen M-R, Packard C, et al. (2006) Overproduction of large VLDL particles is driven by increased liver fat content in man. Diabetologia 49, 755–765. [DOI] [PubMed] [Google Scholar]
- 14.Diraison F, Moulin P & Beylot M (2003) Contribution of hepatic de novo lipogenesis and reesterification of plasma non esterified fatty acids to plasma triglyceride synthesis during non-alcoholic fatty liver disease. Diabetes Metab 29, 478–485. [DOI] [PubMed] [Google Scholar]
- 15.Rytka JM, Wueest S, Schoenle EJ, et al. (2011) The portal theory supported by venous drainage-selective fat transplantation. Diabetes 60, 56–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Foster MT, Shi H, Seeley RJ, et al. (2011) Removal of intra-abdominal visceral adipose tissue improves glucose tolerance in rats: role of hepatic triglyceride storage. Physiol Behav 104, 845–854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Griffin BA, Caslake MJ, Yip B, et al. (1990) Rapid isolation of low density lipoprotein (LDL) subfractions from plasma by density gradient ultracentrifugation. Atherosclerosis 83, 59–67. [DOI] [PubMed] [Google Scholar]
- 18.Saeed A, Feofanova EV, Yu B, et al. (2018) Remnant-like particle cholesterol, low-density lipoprotein triglycerides, and incident cardiovascular disease. J Am Coll Cardiol 72, 156–169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Blaton V (2007) How is the metabolic syndrome related to the dyslipidemia? EJIFCC 18, 15. [PMC free article] [PubMed] [Google Scholar]
- 20.Lindman AS, Veierød M, Tverdal A, et al. (2010) Nonfasting triglycerides and risk of cardiovascular death in men and women from the Norwegian Counties Study. Eur J Epidemiol 25, 789–798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nordestgaard BG, Benn M, Schnohr P, et al. (2007) Nonfasting triglycerides and risk of myocardial infarction, ischemic heart disease, and death in men and women. JAMA 298, 299–308. [DOI] [PubMed] [Google Scholar]
- 22.Bansal S, Buring JE, Rifai N, et al. (2007) Fasting compared with nonfasting triglycerides and risk of cardiovascular events in women. JAMA 298, 309–316. [DOI] [PubMed] [Google Scholar]
- 23.Koemel NA, Sciarrillo CM, Bode KB, et al. (2020) Postprandial metabolism and vascular function: impact of aging and physical activity level. Int J Sport Nutr Exerc Metab 30, 412–419. [DOI] [PubMed] [Google Scholar]
- 24.Kolovou GD, Watts GF, Mikhailidis DP, et al. (2019) Postprandial hypertriglyceridaemia revisited in the era of non-fasting lipid profile testing: a 2019 expert panel statement, main text. Curr Vasc Pharmacol 17, 498–514. [DOI] [PubMed] [Google Scholar]
- 25.Weiss EP, Fields DA, Mittendorfer B, et al. (2008) Reproducibility of postprandial lipemia tests and validity of an abbreviated 4-hour test. Metabolism 57, 1479–1485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Emerson SR, Kurti SP, Teeman CS, et al. (2017) Realistic test-meal protocols lead to blunted postprandial lipemia but similar inflammatory responses compared with a standard high-fat meal. Curr Dev Nutr 1, e000232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kolovou GD, Anagnostopoulou KK, Pavlidis AN, et al. (2005) Postprandial lipemia in men with metabolic syndrome, hypertensives and healthy subjects. Lipids Health Dis 4, 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ohnishi H, Saitoh S, Takagi S, et al. (2002) Relationship between insulin-resistance and remnant-like particle cholesterol. Atherosclerosis 164, 167–170. [DOI] [PubMed] [Google Scholar]
- 29.Haidari M, Leung N, Mahbub F, et al. (2002) Fasting and postprandial overproduction of intestinally derived lipoproteins in an animal model of insulin resistance evidence that chronic fructose feeding in the hamster is accompanied by enhanced intestinal de novo lipogenesis and apob48-containing lipoprotein overproduction. J Biol Chem 277, 31646–31655. [DOI] [PubMed] [Google Scholar]
- 30.Lewis GF, Uffelman K, Naples M, et al. (2005) Intestinal lipoprotein overproduction, a newly recognized component of insulin resistance, is ameliorated by the insulin sensitizer rosiglitazone: studies in the fructose-fed Syrian golden hamster. Endocrinology 146, 247–255. [DOI] [PubMed] [Google Scholar]
- 31.Nikkilä EA, Huttunen JK & Ehnholm C (1977) Postheparin plasma lipoprotein lipase and hepatic lipase in diabetes mellitus: relationship to plasma triglyceride metabolism. Diabetes 26, 11–21. [DOI] [PubMed] [Google Scholar]
- 32.Taskinen M-R, Nikkilä E, Kuusi T, et al. (1982) Lipoprotein lipase activity and serum lipoproteins in untreated type 2 (insulin-independent) diabetes associated with obesity. Diabetologia 22, 46–50. [DOI] [PubMed] [Google Scholar]
- 33.Brunzell JD, Porte D & Bierman EL (1975) Reversible abnormalities in postheparin lipolytic activity during the late phase of release in diabetes mellitus (postheparin lipolytic activity in diabetes). Metab Clin Exp 24, 1123–1137. [DOI] [PubMed] [Google Scholar]
- 34.Lewis GF & Steiner G (1996) Acute effects of insulin in the control of VLDL production in humans: implications for the insulin-resistant state. Diabetes Care 19, 390–393. [DOI] [PubMed] [Google Scholar]
- 35.Guerin M, Egger P, Soudant C, et al. (2002) Cholesteryl ester flux from HDL to VLDL-1 is preferentially enhanced in type IIB hyperlipidemia in the postprandial state. J Lipid Res 43, 1652–1660. [DOI] [PubMed] [Google Scholar]
- 36.Gianturco SH, Bradley WA, Gotto AM, et al. (1982) Hypertriglyceridemic very low density lipoproteins induce triglyceride synthesis and accumulation in mouse peritoneal macrophages. J Clin Invest 70, 168–178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Nordestgaard B, Tybjaerg-Hansen A & Lewis B (1992) Influx in vivo of low density, intermediate density, and very low density lipoproteins into aortic intimas of genetically hyperlipidemic rabbits. Roles of plasma concentrations, extent of aortic lesion, and lipoprotein particle size as determinants. Arterioscler Thromb Vasc Biol 12, 6–18. [DOI] [PubMed] [Google Scholar]
- 38.Varbo A & Nordestgaard BG (2016) Remnant cholesterol and triglyceride-rich lipoproteins in atherosclerosis progression and cardiovascular disease. Arteriosclerosis, Thrombosis, and Vascular Biology 36, 2133–2135. [DOI] [PubMed] [Google Scholar]
- 39.Cohn JS, Johnson EJ, Millar JS, et al. (1993) Contribution of apoB-48 and apoB-100 triglyceride-rich lipoproteins (TRL) to postprandial increases in the plasma concentration of TRL triglycerides and retinyl esters. J Lipid Res 34, 2033–2040. [PubMed] [Google Scholar]
- 40.Karpe F, Bell M, Björkegren J, et al. (1995) Quantification of postprandial triglyceride-rich lipoproteins in healthy men by retinyl ester labeling and simultaneous measurement of apolipoproteins B-48 and B-100. Arterioscler Thromb Vasc Biol 15, 199–207. [DOI] [PubMed] [Google Scholar]
- 41.Bjorkegren J, Packard C, Hamsten A, et al. (1996) Accumulation of large very low density lipoprotein in plasma during intravenous infusion of a chylomicron-like triglyceride emulsion reflects competition for a common lipolytic pathway. J Lipid Res 37, 76–86. [PubMed] [Google Scholar]
- 42.Sacks FM (2015) The crucial roles of apolipoproteins E and C-III in apoB lipoprotein metabolism in normolipidemia and hypertriglyceridemia. Curr Opin Lipidol 26, 56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ginsberg H, Le N-A, Goldberg I, et al. (1986) Apolipoprotein B metabolism in subjects with deficiency of apolipoproteins CIII and AI. Evidence that apolipoprotein CIII inhibits catabolism of triglyceride-rich lipoproteins by lipoprotein lipase in vivo. J Clin Invest 78, 1287–1295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wu SA, Kersten S & Qi L (2020) Lipoprotein lipase and its regulators: an unfolding story. Trends Endocrinol Metab 1, 48–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kowal RC, Herz J, Goldstein JL, et al. (1989) Low density lipoprotein receptor-related protein mediates uptake of cholesteryl esters derived from apoprotein E-enriched lipoproteins. Proc Natl Acad Sci USA 86, 5810–5814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Cooper AD (1997) Hepatic uptake of chylomicron remnants. J Lipid Res 38, 2173–2192. [PubMed] [Google Scholar]
- 47.Goldstein JL, Brown MS, Anderson RG, et al. (1985) Receptor-mediated endocytosis: concepts emerging from the LDL receptor system. Annu Rev Cell Biol 1, 1–39. [DOI] [PubMed] [Google Scholar]
- 48.US Department of Health and Human Services. Intake of Calories and Selected Nutrients for the United States Population, 1999–2000. https://www.cdc.gov/nchs/data/nhanes/databriefs/calories.pdf (2020).
- 49.Prevention CfDCa (2017) Diet/Nutrition. Disability and Risk Factors. https://www.cdc.gov/nchs/fastats/diet.htm (2020).
- 50.Taguchi H, Watanabe H, Onizawa K, et al. (2000) Double-blind controlled study on the effects of dietary diacylglycerol on postprandial serum and chylomicron triacylglycerol responses in healthy humans. J Am Coll Nutr 19, 789–796. [DOI] [PubMed] [Google Scholar]
- 51.Hulley SB, Rosenman RH, Bawol RD, et al. (1980) Epidemiology as a guide to clinical decisions: the association between triglyceride and coronary heart disease. N Engl J Med 302, 1383–1389. [DOI] [PubMed] [Google Scholar]
- 52.Miller M, Langenberg P & Havas S (2007) Impact of lowering triglycerides on raising HDL-C in hypertriglyceridemic and non-hypertriglyceridemic subjects. Int J Cardiol 119, 192–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hokanson JE & Austin MA (1996) Plasma triglyceride level is a risk factor for cardiovascular disease independent of high-density lipoprotein cholesterol level: a metaanalysis of population-based prospective studies. J Cardiovasc Risk 3, 213–219. [PubMed] [Google Scholar]
- 54.Hurren NM, Eves FF & Blannin AK (2011) Is the effect of prior exercise on postprandial lipaemia the same for a moderate-fat meal as it is for a high-fat meal? Br J Nutr 105, 506–516. [DOI] [PubMed] [Google Scholar]
- 55.Kats D, Sharrett AR, Ginsberg HN, et al. (2017) Postprandial lipemia and the risk of coronary heart disease and stroke: the Atherosclerosis Risk in Communities (ARIC) study. BMJ Open Diabetes Res Care 5, e000335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Nordestgaard BG, Abildgaard S, Wittrup HH, et al. (1997) Heterozygous lipoprotein lipase deficiency: frequency in the general population, effect on plasma lipid levels, and risk of ischemic heart disease. Circulation 96, 1737–1744. [DOI] [PubMed] [Google Scholar]
- 57.Khera AV, Won H-H, Peloso GM, et al. (2017) Association of rare and common variation in the lipoprotein lipase gene with coronary artery disease. Jama 317, 937–946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Consortium TCDG & Collaboration ERF (2010) Triglyceride-mediated pathways and coronary disease: collaborative analysis of 101 studies. Lancet 375, 1634–1639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Merkel M, Loeffler B, Kluger M, et al. (2005) Apolipoprotein AV accelerates plasma hydrolysis of triglyceride-rich lipoproteins by interaction with proteoglycan-bound lipoprotein lipase. J Biol Chem 280, 21553–21560. [DOI] [PubMed] [Google Scholar]
- 60.Jørgensen AB, Frikke-Schmidt R, Nordestgaard BG, et al. (2014) Loss-of-function mutations in APOC3 and risk of ischemic vascular disease. N Engl J Med 371, 32–41. [DOI] [PubMed] [Google Scholar]
- 61.Dewey FE, Gusarova V, O'Dushlaine C, et al. (2016) Inactivating variants in ANGPTL4 and risk of coronary artery disease. N Engl J Med 374, 1123–1133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ference BA, Kastelein JJ, Ray KK, et al. (2019) Association of triglyceride-lowering LPL variants and LDL-C-lowering LDLR variants with risk of coronary heart disease. JAMA 321, 364–373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Sniderman AD, Thanassoulis G, Glavinovic T, et al. (2019) Apolipoprotein B particles and cardiovascular disease: a narrative review. JAMA Cardiol 4, 1287–1295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Choi SH & Ginsberg HN (2011) Increased very low density lipoprotein (VLDL) secretion, hepatic steatosis, and insulin resistance. Trends Endocrinol Metab 22, 353–363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Schwarz J-M, Linfoot P, Dare D, et al. (2003) Hepatic de novo lipogenesis in normoinsulinemic and hyperinsulinemic subjects consuming high-fat, low-carbohydrate and low-fat, high-carbohydrate isoenergetic diets. Am J Clin Nutr 77, 43–50. [DOI] [PubMed] [Google Scholar]
- 66.Koopmans SJ, Kushwaha RS & DeFronzo RA (1999) Chronic physiologic hyperinsulinemia impairs suppression of plasma free fatty acids and increases de novo lipogenesis but does not cause dyslipidemia in conscious normal rats. Metabolism 48, 330–337. [DOI] [PubMed] [Google Scholar]
- 67.Annuzzi G, De Natale C, Iovine C, et al. (2004) Insulin resistance is independently associated with postprandial alterations of triglyceride-rich lipoproteins in type 2 diabetes mellitus. Arterioscler Thromb Vasc Biol 24, 2397–2402. [DOI] [PubMed] [Google Scholar]
- 68.Søndergaard E, Sørensen LP, Rahbek I, et al. (2012) Postprandial VLDL-triacylglycerol secretion is not suppressed in obese type 2 diabetic men. Diabetologia 55, 2733–2740. [DOI] [PubMed] [Google Scholar]
- 69.Cohn JS, Patterson BW, Uffelman KD, et al. (2004) Rate of production of plasma and very-low-density lipoprotein (VLDL) apolipoprotein C-III is strongly related to the concentration and level of production of VLDL triglyceride in male subjects with different body weights and levels of insulin sensitivity. J Clin Endocrinol Metab 89, 3949–3955. [DOI] [PubMed] [Google Scholar]
- 70.Food, Nutrition Board I (2005) Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids (Macronutrients). Washington (DC): National Academy Press. [Google Scholar]
- 71.Mensink RP, Zock PL, Kester AD, et al. (2003) Effects of dietary fatty acids and carbohydrates on the ratio of serum total to HDL cholesterol and on serum lipids and apolipoproteins: a meta-analysis of 60 controlled trials. Am J Clin Nutr 77, 1146–1155. [DOI] [PubMed] [Google Scholar]
- 72.Livesey G & Taylor R (2008) Fructose consumption and consequences for glycation, plasma triacylglycerol, and body weight: meta-analyses and meta-regression models of intervention studies. Am J Clin Nutr 88, 1419–1437. [DOI] [PubMed] [Google Scholar]
- 73.Swarbrick MM, Stanhope KL, Elliott SS, et al. (2008) Consumption of fructose-sweetened beverages for 10 weeks increases postprandial triacylglycerol and apolipoprotein-B concentrations in overweight and obese women. Br J Nutr 100, 947–952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Stanhope KL, Schwarz JM, Keim NL, et al. (2009) Consuming fructose-sweetened, not glucose-sweetened, beverages increases visceral adiposity and lipids and decreases insulin sensitivity in overweight/obese humans. J Clin Invest 119, 1322–1334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Taskinen MR, Söderlund S, Bogl L, et al. (2017) Adverse effects of fructose on cardiometabolic risk factors and hepatic lipid metabolism in subjects with abdominal obesity. J Intern Med 282, 187–201. [DOI] [PubMed] [Google Scholar]
- 76.Lanaspa MA, Cicerchi C, Garcia G, et al. (2012) Counteracting roles of AMP deaminase and AMP kinase in the development of fatty liver. PLoS ONE 7, e48801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Stanhope KL & Havel PJ (2008) Fructose consumption: potential mechanisms for its effects to increase visceral adiposity and induce dyslipidemia and insulin resistance. Curr Opin Lipidol 19, 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Sobrecases H, Lê K-A, Bortolotti M, et al. (2010) Effects of short-term overfeeding with fructose, fat and fructose plus fat on plasma and hepatic lipids in healthy men. Diabetes Metab 36, 244–246. [DOI] [PubMed] [Google Scholar]
- 79.Teff KL, Elliott SS, Tschöp M, et al. (2004) Dietary fructose reduces circulating insulin and leptin, attenuates postprandial suppression of ghrelin, and increases triglycerides in women. J Clin Endocrinol Metab 89, 2963–2972. [DOI] [PubMed] [Google Scholar]
- 80.Teff KL, Kleim NL, Townsend RR, et al. (2005) Fructose-sweetened beverages decrease circulating leptin levels and increase postprandial triglycerides in obese men and women. Diabetes 54, A385. [Google Scholar]
- 81.Ford ES, Li C, Zhao G, et al. (2009) Hypertriglyceridemia and its pharmacologic treatment among US adults. Arch Intern Med 169, 572–578. [DOI] [PubMed] [Google Scholar]
- 82.May A, Kuklina E & Yoon P (2010) Prevalence of abnormal lipid levels among youths-United States, 1999-2006. Morb Mortal Wkly Rep 59, 29–33. [PubMed] [Google Scholar]
- 83.Fox CS, Massaro JM, Hoffmann U, et al. (2007) Abdominal visceral and subcutaneous adipose tissue compartments: association with metabolic risk factors in the Framingham Heart Study. Circulation 116, 39–48. [DOI] [PubMed] [Google Scholar]
- 84.Kang L, Chen X, Sebastian BM, et al. (2007) Chronic ethanol and triglyceride turnover in white adipose tissue in rats inhibition of the anti-lipolytic action of insulin after chronic ethanol contributes to increased triglyceride degradation. J Biol Chem 282, 28465–28473. [DOI] [PubMed] [Google Scholar]
- 85.Dorn JM, Hovey K, Muti P, et al. (2003) Alcohol drinking patterns differentially affect central adiposity as measured by abdominal height in women and men. J Nutr 133, 2655–2662. [DOI] [PubMed] [Google Scholar]
- 86.Chrysohoou C, Panagiotakos DB, Pitsavos C, et al. (2003) Effects of chronic alcohol consumption on lipid levels, inflammatory and haemostatic factors in the general population: the ‘ATTICA'study. Eur J Cardiovasc Prev Rehabil 10, 355–361. [DOI] [PubMed] [Google Scholar]
- 87.Foerster M, Marques-Vidal P, Gmel G, et al. (2009) Alcohol drinking and cardiovascular risk in a population with high mean alcohol consumption. Am J Cardiol 103, 361–368. [DOI] [PubMed] [Google Scholar]
- 88.Veenstra J, Ockhuizen T, van de Pol H, et al. (1990) Effects of a moderate dose of alcohol on blood lipids and lipoproteins postprandially and in the fasting state. Alcohol Alcohol 25, 371–377. [PubMed] [Google Scholar]
- 89.Schneider J, Liesenfeld A, Mordasini R, et al. (1985) Lipoprotein fractions, lipoprotein lipase and hepatic triglyceride lipase during short-term and long-term uptake of ethanol in healthy subjects. Atherosclerosis 57, 281–291. [DOI] [PubMed] [Google Scholar]
- 90.Pownall HJ (1994) Dietary ethanol is associated with reduced lipolysis of intestinally derived lipoproteins. J Lipid Res 35, 2105–2113. [PubMed] [Google Scholar]
- 91.Pykälistö O, Goldberg AP & Brunzell JD (1976) Reversal of decreased human adipose tissue lipoprotein lipase and hypertriglyceridemia after treatment of hypothyroidism. J Clin Endocrinol Metab 43, 591–600. [DOI] [PubMed] [Google Scholar]
- 92.Valdemarsson S, Hedner P & Nilsson-Ehle P (1982) Reversal of decreased hepatic lipase and lipoprotein lipase activities after treatment of hypothyroidism. Eur J Clin Invest 12, 423–428. [DOI] [PubMed] [Google Scholar]
- 93.Lithell H, Boberg J, Hellsing K, et al. (1981) Serum lipoprotein and apolipoprotein concentrations and tissue lipoprotein-lipase activity in overt and subclinical hypothyroidism: the effect of substitution therapy. Eur J Clin Invest 11, 3–10. [DOI] [PubMed] [Google Scholar]
- 94.Abrams JJ & Grundy SM (1981) Cholesterol metabolism in hypothyroidism and hyperthyroidism in man. J Lipid Res 22, 323–338. [PubMed] [Google Scholar]
- 95.Ballantyne FC, Epenetos A, Caslake M, et al. (1979) The composition of low-density lipoprotein and very-low-density lipoprotein subfractions in primary hypothyroidism and the effect of hormone-replacement therapy. Clin Sci 57, 83–88. [DOI] [PubMed] [Google Scholar]
- 96.Nikkilä EA & Kekki M (1973) Plasma triglyceride transport kinetics in diabetes mellitus. Metab Clin Exp 22, 1–22. [DOI] [PubMed] [Google Scholar]
- 97.Ginsberg H & Grundy S (1982) Effect of caloric restriction on very low density lipoprotein triglyceride metabolism in subjects with diabetes mellitus. Diabetologia 23, 421–425. [DOI] [PubMed] [Google Scholar]
- 98.Ginsberg HN (1991) Lipoprotein physiology in nondiabetic and diabetic states: relationship to atherogenesis. Diabetes Care 14, 839–855. [DOI] [PubMed] [Google Scholar]
- 99.Taskinen M-R & Nikkilä EA (1979) Lipoprotein lipase activity of adipose tissue and skeletal muscle in insulin-deficient human diabetes. Diabetologia 17, 351–356. [DOI] [PubMed] [Google Scholar]
- 100.Taskinen M-R, Nikkilä EA, Nousiainen R, et al. (1981) Lipoprotein lipase activity in adipose tissue and skeletal muscle of human diabetics during insulin deprivation and restoration. Scand J Clin Lab Invest 41, 263–268. [DOI] [PubMed] [Google Scholar]
- 101.Cooper M, Tan K, Hales C, et al. (1996) Postprandial lipid metabolism and β-cell function in non-insulin-dependent (type 2) diabetes mellitus after a mixed meal with a high fat content. Diabetic Med 13, 816–827. [DOI] [PubMed] [Google Scholar]
- 102.Gabor J, Spain M & Kalant N (1980) Composition of serum very-low-density and high-density lipoproteins in diabetes. Clin Chem 26, 1261–1265. [PubMed] [Google Scholar]
- 103.Clemente-Postigo M, Queipo-Ortuno MI, Fernandez-Garcia D, et al. (2011) Adipose tissue gene expression of factors related to lipid processing in obesity. PLoS ONE 6, e24783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.MacLean PS, Tanner CJ, Houmard JA, et al. (2001) Plasma cholesteryl ester transfer protein activity is not linked to insulin sensitivity. Metab Clin Exp 50, 783–788. [DOI] [PubMed] [Google Scholar]
- 105.Chan MK, Persaud J, Varghese Z, et al. (1984) Pathogenic roles of post-heparin lipases in lipid abnormalities in hemodialysis patients. Kidney Int 25, 812–818. [DOI] [PubMed] [Google Scholar]
- 106.Sakurai T, Oka T, Hasegawa H, et al. (1992) Comparison of lipids, apoproteins and associated enzyme activities between diabetic and nondiabetic end-stage renal disease. Nephron 61, 409–414. [DOI] [PubMed] [Google Scholar]
- 107.Atger V, Beyne P, Frommherz K, et al. (1989) Presence of Apo B48, and relative Apo CII deficiency and Apo CIII enrichment in uremic very-low density lipoproteins. Ann Biol Clin 47, 497–501. [PubMed] [Google Scholar]
- 108.Matsumoto R, Tsunekawa K, Shoho Y, et al. (2019) Association between skeletal muscle mass and serum concentrations of lipoprotein lipase, GPIHBP1, and hepatic triglyceride lipase in young Japanese men. Lipids Health Dis 18, 84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Seip RL, Angelopoulos TJ & Semenkovich CF (1995) Exercise induces human lipoprotein lipase gene expression in skeletal muscle but not adipose tissue. Am J Physiol Endocrinol Metab 268, E229–E236. [DOI] [PubMed] [Google Scholar]
- 110.Bey L & Hamilton MT (2003) Suppression of skeletal muscle lipoprotein lipase activity during physical inactivity: a molecular reason to maintain daily low-intensity activity. J Physiol 551, 673–682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Svedenhag J, Lithell H, Juhlin-Dannfelt A, et al. (1983) Increase in skeletal muscle lipoprotein lipase following endurance training in man. Atherosclerosis 49, 203–207. [DOI] [PubMed] [Google Scholar]
- 112.Kabagambe EK, Ordovas JM, Tsai MY, et al. (2009) Smoking, inflammatory patterns and postprandial hypertriglyceridemia. Atherosclerosis 203, 633–639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Facchini FS, Hollenbeck CB, Jeppesen J, et al. (1992) Insulin resistance and cigarette smoking. Lancet 339, 1128–1130. [DOI] [PubMed] [Google Scholar]
- 114.Willett W, Hennekens CH, Castelli W, et al. (1983) Effects of cigarette smoking on fasting triglyceride, total cholesterol, and HDL-cholesterol in women. Am Heart J 105, 417–421. [DOI] [PubMed] [Google Scholar]
- 115.Hagan RD, Upton SJ, Avakian EV, et al. (1986) Increases in serum lipid and lipoprotein levels with movement from the supine to standing position in adult men and women. Prev Med 15, 18–27. [DOI] [PubMed] [Google Scholar]
- 116.Dixon M & Paterson CR (1978) Posture and the composition of plasma. Clin Chem 24, 824–826. [PubMed] [Google Scholar]
- 117.Miller M, Bachorik P & Cloey T (1992) Normal variation of plasma lipoproteins: postural effects on plasma concentrations of lipids, lipoproteins, and apolipoproteins. Clin Chem 38, 569–574. [PubMed] [Google Scholar]
- 118.Castelli WP (1986) The triglyceride issue: a view from Framingham. Am Heart J 112, 432–437. [DOI] [PubMed] [Google Scholar]
- 119.Sakurabayashi I, Saito Y, Kita T, et al. (2001) Reference intervals for serum apolipoproteins AI, A-II, B, C-II, C-III, and E in healthy Japanese determined with a commercial immunoturbidimetric assay and effects of sex, age, smoking, drinking, and Lp (a) level. Clin Chim Acta 312, 87–95. [DOI] [PubMed] [Google Scholar]
- 120.Godsland IF, Crook D, Simpson R, et al. (1990) The effects of different formulations of oral contraceptive agents on lipid and carbohydrate metabolism. N Engl J Med 323, 1375–1381. [DOI] [PubMed] [Google Scholar]
- 121.Hazzard WR, Spiger MJ, Bagdade JD, et al. (1969) Studies on the mechanism of increased plasma triglyceride levels induced by oral contraceptives. N Engl J Med 280, 471–474. [DOI] [PubMed] [Google Scholar]
- 122.Walsh BW & Sacks FM (1993) Effects of low dose oral contraceptives on very low density and low density lipoprotein metabolism. J Clin Invest 91, 2126–2132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Alvarez J, Montelongo A, Iglesias A, et al. (1996) Longitudinal study on lipoprotein profile, high density lipoprotein subclass, and postheparin lipases during gestation in women. J Lipid Res 37, 299–308. [PubMed] [Google Scholar]
- 124.Elliott JA (1975) The effect of pregnancy on the control of lipolysis in fat cells isolated from human adipose tissue. Eur J Clin Invest 5, 159–163. [DOI] [PubMed] [Google Scholar]
- 125.Martin-Hidalgo A, Holm C, Belfrage P, et al. (1994) Lipoprotein lipase and hormone-sensitive lipase activity and mRNA in rat adipose tissue during pregnancy. Am J Physiol Endocrinol Metab 266, E930–E935. [DOI] [PubMed] [Google Scholar]
- 126.Tchernof A, Desmeules A, Richard C, et al. (2004) Ovarian hormone status and abdominal visceral adipose tissue metabolism. J Clin Endocrinol Metab 89, 3425–3430. [DOI] [PubMed] [Google Scholar]
- 127.Jensen J, Nilas L & Christiansen C (1990) Influence of menopause on serum lipids and lipoproteins. Maturitas 12, 321–331. [DOI] [PubMed] [Google Scholar]
- 128.Matthews KA, Meilahn E, Kuller LH, et al. (1989) Menopause and risk factors for coronary heart disease. N Engl J Med 321, 641–646. [DOI] [PubMed] [Google Scholar]
- 129.Nielsen S, Guo Z, Johnson CM, et al. (2004) Splanchnic lipolysis in human obesity. J Clin Invest 113, 1582–1588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Nielsen S & Karpe F (2012) Determinants of VLDL-triglycerides production. Curr Opin Lipidol 23, 321–326. [DOI] [PubMed] [Google Scholar]
- 131.Meek SE, Nair KS & Jensen MD (1999) Insulin regulation of regional free fatty acid metabolism. Diabetes 48, 10–14. [DOI] [PubMed] [Google Scholar]
- 132.Semenkovich C, Wims M, Noe L, et al. (1989) Insulin regulation of lipoprotein lipase activity in 3T3-L1 adipocytes is mediated at posttranscriptional and posttranslational levels. J Biol Chem 264, 9030–9038. [PubMed] [Google Scholar]
- 133.Gianturco SH, Ramprasad M, Song R, et al. (1998) Apolipoprotein B-48 or its apolipoprotein B-100 equivalent mediates the binding of triglyceride-rich lipoproteins to their unique human monocyte-macrophage receptor. Arterioscler Thromb Vasc Biol 18, 968–976. [DOI] [PubMed] [Google Scholar]
- 134.Rapp JH, Lespine A, Hamilton RL, et al. (1994) Triglyceride-rich lipoproteins isolated by selected-affinity anti-apolipoprotein B immunosorption from human atherosclerotic plaque. Arterioscler Thromb Vasc Biol 14, 1767–1774. [DOI] [PubMed] [Google Scholar]
- 135.Park SY, Lee JH, Kim YK, et al. (2005) Cilostazol prevents remnant lipoprotein particle-induced monocyte adhesion to endothelial cells by suppression of adhesion molecules and monocyte chemoattractant protein-1 expression via lectin-like receptor for oxidized low-density lipoprotein receptor activation. J Pharmacol Exp Ther 312, 1241–1248. [DOI] [PubMed] [Google Scholar]
- 136.Shin HK, Kim YK, Kim KY, et al. (2004) Remnant lipoprotein particles induce apoptosis in endothelial cells by NAD (P) H oxidase-mediated production of superoxide and cytokines via lectin-like oxidized low-density lipoprotein receptor-1 activation: prevention by cilostazol. Circulation 109, 1022–1028. [DOI] [PubMed] [Google Scholar]
- 137.Saniabadi AR, Umemura K, Shimoyama M, et al. (1997) Aggregation of human blood platelets by remnant like lipoprotein particles of plasma chylomicrons and very low density lipoproteins. Thromb Haemostasis 77, 0996–1001. [PubMed] [Google Scholar]
- 138.Marcoux C, Tremblay M, Fredenrich A, et al. (2001) Lipoprotein distribution of apolipoprotein C-III and its relationship to the presence in plasma of triglyceride-rich remnant lipoproteins. Metab Clin Exp 50, 112–119. [DOI] [PubMed] [Google Scholar]
- 139.Zheng C, Azcutia V, Aikawa E, et al. (2013) Statins suppress apolipoprotein CIII-induced vascular endothelial cell activation and monocyte adhesion. Eur Heart J 34, 615–624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Kawakami A, Aikawa M, Libby P, et al. (2006) Apolipoprotein CIII in apolipoprotein B lipoproteins enhances the adhesion of human monocytic cells to endothelial cells. Circulation 113, 691–700. [DOI] [PubMed] [Google Scholar]
- 141.Lee JY, Zhao L, Youn HS, et al. (2004) Saturated fatty acid activates but polyunsaturated fatty acid inhibits Toll-like receptor 2 dimerized with Toll-like receptor 6 or 1. J Biol Chem 279, 16971–16979. [DOI] [PubMed] [Google Scholar]
- 142.Lee JY, Ye J, Gao Z, et al. (2003) Reciprocal modulation of Toll-like receptor-4 signaling pathways involving MyD88 and phosphatidylinositol 3-kinase/AKT by saturated and polyunsaturated fatty acids. J Biol Chem 278, 37041–37051. [DOI] [PubMed] [Google Scholar]
- 143.Lee JY, Sohn KH, Rhee SH, et al. (2001) Saturated fatty acids, but not unsaturated fatty acids, induce the expression of cyclooxygenase-2 mediated through Toll-like receptor 4. J Biol Chem 276, 16683–16689. [DOI] [PubMed] [Google Scholar]
- 144.Higgins LJ & Rutledge JC (2009) Inflammation associated with the postprandial lipolysis of triglyceride-rich lipoproteins by lipoprotein lipase. Curr Atheroscler Rep 11, 199–205. [DOI] [PubMed] [Google Scholar]
- 145.Timlin MT & Parks EJ (2005) Temporal pattern of de novo lipogenesis in the postprandial state in healthy men. Am J Clin Nutr 81, 35–42. [DOI] [PubMed] [Google Scholar]
- 146.Tarigan TJ, Khumaedi AI, Wafa S, et al. (2019) Determinant of postprandial triglyceride levels in healthy young adults. Diabetes Metab Syndr: Clin Res Rev 13, 1917–1921. [DOI] [PubMed] [Google Scholar]
- 147.Dash S, Xiao C, Morgantini C, et al. (2015) New insights into the regulation of chylomicron production. Annu Rev Nutr 35, 265–294. [DOI] [PubMed] [Google Scholar]
- 148.Emerson SR, Kurti SP, Harms CA, et al. (2017) Magnitude and timing of the postprandial inflammatory response to a high-fat meal in healthy adults: a systematic review. Adv Nutr 8, 213–225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Emerson SR, Sciarrillo CM, Kurti SP, et al. (2019) High-fat meal-induced changes in markers of inflammation and angiogenesis in healthy adults who differ by age and physical activity level. Curr Dev Nutr 3, nzy098. [Google Scholar]
- 150.Nappo F, Esposito K, Cioffi M, et al. (2002) Postprandial endothelial activation in healthy subjects and in type 2 diabetic patients: role of fat and carbohydrate meals. J Am Coll Cardiol 39, 1145–1150. [DOI] [PubMed] [Google Scholar]
- 151.Norata GD, Grigore L, Raselli S, et al. (2007) Post-prandial endothelial dysfunction in hypertriglyceridemic subjects: molecular mechanisms and gene expression studies. Atherosclerosis 193, 321–327. [DOI] [PubMed] [Google Scholar]
- 152.Wang YI, Schulze J, Raymond N, et al. (2011) Endothelial inflammation correlates with subject triglycerides and waist size after a high-fat meal. Am J Physiol Heart Circ Physiol 300, H784–H791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Van Oostrom A, Sijmonsma T, Verseyden Cet al. (2003) Postprandial recruitment of neutrophils may contribute to endothelial dysfunction. J Lipid Res 44, 576–583. [DOI] [PubMed] [Google Scholar]
- 154.Ghanim H, Abuaysheh S, Sia CL, et al. (2009) Increase in plasma endotoxin concentrations and the expression of Toll-like receptors and suppressor of cytokine signaling-3 in mononuclear cells after a high-fat, high-carbohydrate meal: implications for insulin resistance. Diabetes Care 32, 2281–2287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Rohr MW, Narasimhulu CA, Rudeski-Rohr TA, et al. (2020) Negative effects of a high-fat diet on intestinal permeability: a review. Adv Nutr 11, 77–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Mo Z, Huang S, Burnett DJ, et al. (2020) Endotoxin may not be the major cause of postprandial inflammation in adults who consume a single high-fat or moderately high-fat meal. J Nutr 150, 1303–1312. [DOI] [PubMed] [Google Scholar]
- 157.Halkes C, Van Dijk H, De Jaegere PT, et al. (2001) Postprandial increase of complement component 3 in normolipidemic patients with coronary artery disease: effects of expanded-dose simvastatin. Arterioscler Thromb Vasc Biol 21, 1526–1530. [DOI] [PubMed] [Google Scholar]
- 158.Scantlebury T, Maslowska M & Cianflone K (1998) Chylomicron-specific enhancement of acylation stimulating protein and precursor protein C3 production in differentiated human adipocytes. J Biol Chem 273, 20903–20909. [DOI] [PubMed] [Google Scholar]
- 159.Xu N, Dahlbäck B, Öhlin A-K, et al. (1998) Association of vitamin K-dependent coagulation proteins and C4b binding protein with triglyceride-rich lipoproteins of human plasma. Arterioscler Thromb Vasc Biol 18, 33–39. [DOI] [PubMed] [Google Scholar]
- 160.Wallace J, Johnson B, Padilla J, et al. (2010) Postprandial lipaemia, oxidative stress and endothelial function: a review. Int J Clin Pract 64, 389–403. [DOI] [PubMed] [Google Scholar]
- 161.Ras RT, Streppel MT, Draijer R, et al. (2013) Flow-mediated dilation and cardiovascular risk prediction: a systematic review with meta-analysis. Int J Cardiol 168, 344–351. [DOI] [PubMed] [Google Scholar]
- 162.Sun J, Druhan LJ & Zweier JL (2010) Reactive oxygen and nitrogen species regulate inducible nitric oxide synthase function shifting the balance of nitric oxide and superoxide production. Arch Biochem Biophys 494, 130–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Burton-Freeman B, Talbot J, Park E, et al. (2012) Protective activity of processed tomato products on postprandial oxidation and inflammation: a clinical trial in healthy weight men and women. Mol Nutr Food Res 56, 622–631. [DOI] [PubMed] [Google Scholar]
- 164.Jenkins NT, Landers RQ, Thakkar SR, et al. (2011) Prior endurance exercise prevents postprandial lipaemia-induced increases in reactive oxygen species in circulating CD31+ cells. J Physiol 589, 5539–5553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Sluimer JC & Daemen MJ (2009) Novel concepts in atherogenesis: angiogenesis and hypoxia in atherosclerosis. J Pathol 218, 7–29. [DOI] [PubMed] [Google Scholar]
- 166.Mitsos S, Katsanos K, Koletsis E, et al. (2012) Therapeutic angiogenesis for myocardial ischemia revisited: basic biological concepts and focus on latest clinical trials. Angiogenesis 15, 1–22. [DOI] [PubMed] [Google Scholar]
- 167.Catapano AL, Graham I, De Backer G, et al. (2016) 2016 ESC/EAS guidelines for the management of dyslipidaemias. Eur Heart J 37, 2999–3058. [DOI] [PubMed] [Google Scholar]
- 168.Sciarrillo CM, Koemel NA, Kurti SP, et al. (2019) Validity of an abbreviated, clinically feasible test for postprandial lipemia in healthy adults: a randomized cross-over study. Nutrients 11, 180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Dixon MD, Koemel NA, Sciarrillo CM, et al. (2021) The reliability of an abbreviated fat tolerance test: a comparison to the oral glucose tolerance test. Clin Nutr ESPEN 43, 428–435. [DOI] [PubMed] [Google Scholar]