Abstract
Study Design:
Retrospective cohort study.
Objective:
Analysis of postoperative sagittal alignment of the unfused spine is lacking in patients with adult spinal deformity (ASD). The present study aims to evaluate the efficacy of the whole spine full-flexion lateral radiograph to predict the reciprocal change of the unfused spine after correction surgery. We hypothesized that the novel parameter (T1-UIV angle: angle between the upper vertebral endplate of the T1 and the upper vertebral endplate of the upper instrumented vertebra) of the preoperative whole spine full-flexion lateral radiograph is similar to that of the postoperative lateral radiograph if the patient has the ideal sagittal alignment.
Methods:
Twenty-six ASD patients who underwent correction surgery with a minimum 2-year follow-up were enrolled and separated into the Ideal and Non-Ideal groups according to the Scoliosis Research Society (SRS)-Schwab classification of the final follow-up radiograph. Radiographic parameters, including T1-UIV of the preoperative whole spine full-flexion lateral radiograph, were obtained.
Results:
Thirteen patients were included in the Ideal group and 13 were in Non-Ideal group. Preoperative T1-UIV of the whole spine full-flexion lateral radiograph exhibited significant correlations with the T1-UIV angles of the postoperative and final follow-up radiographs (r = 0.64, P < .01, y = 0.800x + 8.012, and r = 0.69, P < .01, y = 0.857x + 2.960, respectively). Interestingly, this correlation was stronger for the Ideal group (r = 0.77, P < .01, y = 1.207x − 1.517, and r = 0.89, P < .01, y = 0.986x + 0.694, respectively).
Conclusion:
A novel radiographic strategy (T1-UIV of preoperative the whole spine full-flexion lateral radiograph) could estimate the postoperative alignment of the unfused spine correctly.
Keywords: adult spinal deformity, compensatory mechanism, sagittal alignment, unfused spinal alignment, spinal surgery, correction surgery, thoracic spine, radiography, full-flexion, T1-UIV
Introduction
Adult spinal deformity (ASD) is a prevalent disorder associated with pain and disability.1-3 Surgical restoration of physiologic sagittal spinopelvic alignment has been demonstrated to improve health-related quality of life (QOL) outcomes.3-5 The ideal sagittal spinopelvic alignment is commonly estimated using the Scoliosis Research Society (SRS)-Schwab classification for ASD.6-8 Moreover, several formulae have been developed to predict the optimal alignment for correction.9-11 Although these approaches are efficient to estimate standing sagittal alignment for selected patients, they do not address the impact of the unfused thoracic spine that changes after correction surgery. Indeed, one of the factors of inadequate postoperative sagittal alignment is a change of the unfused thoracic spine after ASD surgery. Lafage et al reported that nearly half of the patients (18/34, 52.9%) had undergone negative reciprocal change leading to sagittal imbalance.12 Therefore, the reliable prediction of postoperative alignment, including unfused thoracic reciprocal change, is necessary for optimal surgical planning of spinal deformity. However, a method for predicting the behavior of the unfused spinal segments after correction surgery currently remains unknown.
From 2014, to predict the reciprocal change of the unfused thoracic spine, we have used a novel radiographic strategy based on the fact that the alignment of the unfused thoracic spine was improved to kyphosis postsurgery.12-16 We hypothesize that T1-UIV (the angle between the upper vertebral endplate of the T1 and the upper vertebral endplate of the UIV) of the preoperative whole spine full-flexion lateral radiograph is similar to that of postoperative sagittal alignment if the patient has the ideal sagittal alignment. Thus, we aimed to evaluate the efficacy of T1-UIV of the whole spine full-flexion lateral radiograph to predict the reciprocal change of the unfused spine after correction surgery.
Materials and Methods
Between January 2014 and June 2016, 97 ASD patients underwent surgery performed by 2 senior surgeons at a single institute. After obtaining institutional review board approval, the data of all patients with a minimum follow-up of 2 years was collected from the database. Patients aged >55 years at surgery and with ASD treated with osteotomy and long instrumented spinal fusion (≥5 levels) from the thoracolumbar spine (T8-L2) to the pelvis (iliac fixation), leaving sufficient unfused vertebrae for the adaptive decompensation mechanism of the thoracic spine, were included in the study. Patients were excluded from the study if they had the following factors after the primary surgery: (1) revision surgery to change spinal alignment (fusion extension) and (2) type-2 (bone failure) proximal junctional kyphosis (PJK) according to the previous report.17
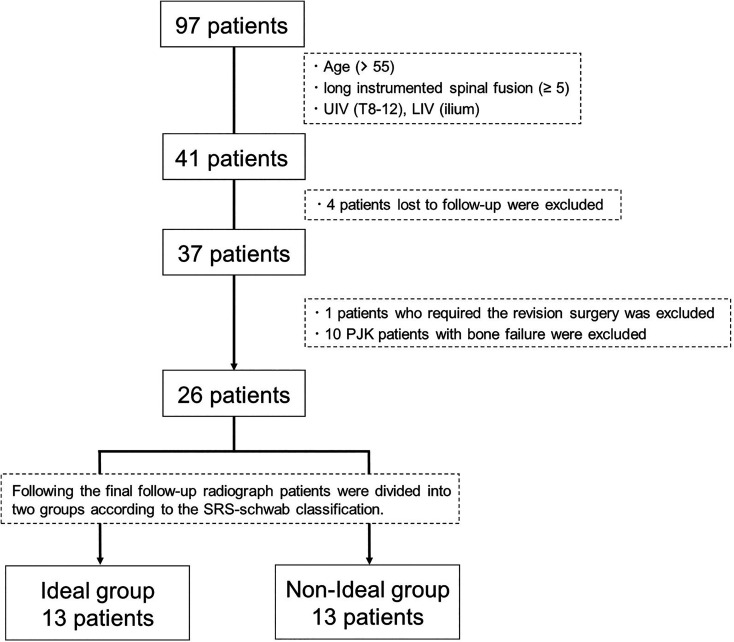
Of the initial 97-patient cohort, 41 who were instrumented from the thoracolumbar spine (T8-L2) to the pelvis (iliac fixation) were included. Four patients were excluded because they were either lost to follow-up or had incomplete radiographs (retrieval rate: 90.2%). One and 10 patients who had fusion extension surgery and type-2 PJK, respectively, were excluded. Therefore, 26 patients were eligible for the current study. After obtaining final follow-up radiographs, we divided the patients into 2 groups according to the SRS-Schwab classification,6 because if the patients had insufficient sagittal alignment postoperatively, a compensation mechanism was predicted that included kyphosis reduction of the unfused thoracic spine. Patients were categorized to the Non-Ideal group (n = 13) if they had one of the following sagittal deformity factors at the final follow-up: (1) pelvic incidence (PI)-lumbar lordosis (LL) ≥10°, (2) sagittal vertical axis (SVA) ≥40 mm, or (3) pelvic tilt (PT) ≥20.6 The remaining patients (n = 13) who achieved the ideal sagittal balance were categorized into the Ideal group. Figure 1 shows the flow diagram of patient selection. Informed consent was provided by the patients before participation.
Figure 1.
Flow diagram of study patient selection. Abbreviations: UIV, upper instrumented vertebra; LIV, lower instrumented vertebra; PJK, proximal junctional kyphosis; SRS-Schwab classification, Scoliosis Research Society-Schwab classification.
Surgical Decision Making and Operative Procedure
Surgery was performed in patients who complained of intractable pain in the lower back with deformity. All included patients presented with at least one of the following spinopelvic alignments: (1) SVA >50 mm and (2) PT >25. ASD patients with flexible sagittal imbalance were treated with multilevel posterior column osteotomy (PCO), whereas the patients with fixed sagittal imbalance were managed with pedicle subtraction osteotomy (PSO) and vertebral column resection (VCR). Postoperatively, the patients were required to wear a thoraco-lumbar-sacral orthosis brace for a minimum of 6 months and allowed to perform activities of daily living.
Data Collection and Radiographic Assessment
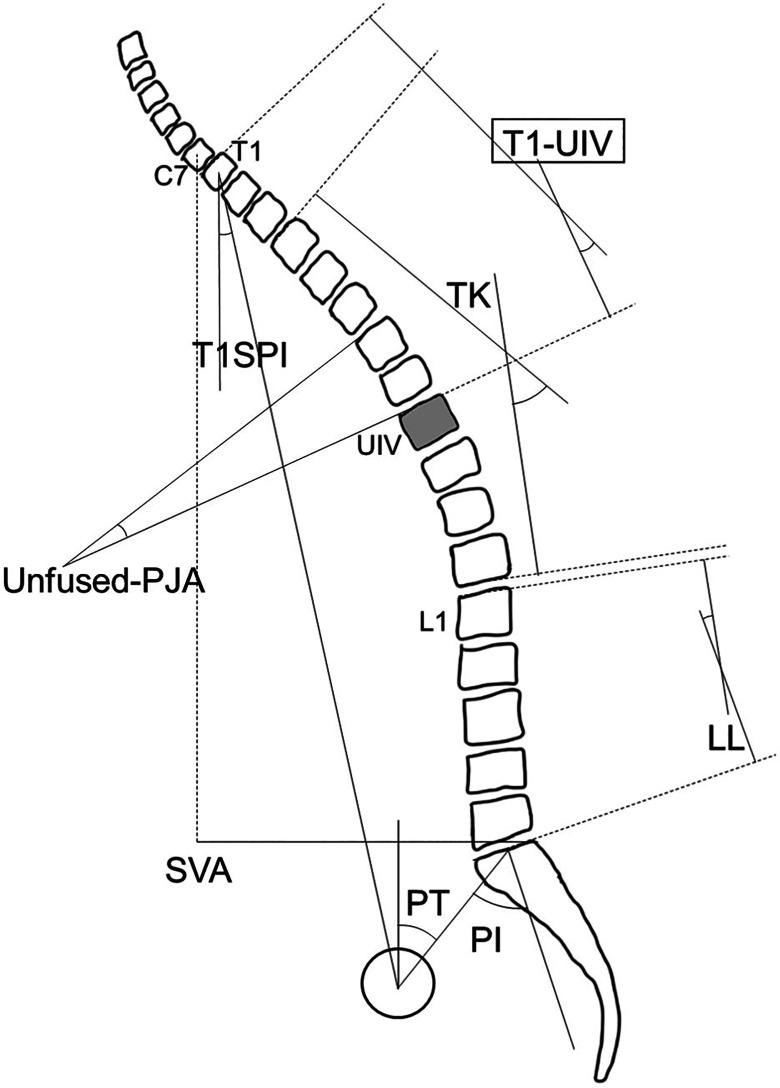
Patients’ data, including demographic and radiographic parameters, was collected. At baseline, immediate postoperative, and final follow-up, anteroposterior and lateral whole spine radiographs were obtained. Additionally, the patients’ spinal flexibility was examined preoperatively using the whole spine full-flexion lateral radiograph on lateral position. (Supplemental Material). Radiographic parameters of interest included PI, PT, LL, PI − LL, T4-T12 thoracic kyphosis (TK), SVA, and T1 spinopelvic inclination (T1SPI). T1-UIV, defined as the angle between the upper vertebral endplate of the T1 and the upper vertebral endplate of the UIV, was also measured to assess the unfused spinal alignment. Moreover, to clarify the magnitude of adjacent segment alignment change of the unfused spine, we measured the proximal junctional angle of the unfused spine (unfused-PJA) defined as the angle between the upper vertebral endplate of the UIV and the upper vertebral endplate of 2 proximal vertebrae. Radiographic parameters, including T1-UIV and the unfused-PJA, are shown in Figure 2.
Figure 2.
T1-UIV angle and unfused-PJA. T1-UIV is measured from the superior endplate of the upper instrumented vertebra to the superior endplate of T1 vertebra. Unfused-PJA is measured from the superior endplate of the upper instrumented vertebra to the superior endplate of the second vertebrae above. Abbreviations: C, cervical; T, thoracic; L, lumbar; T1SPI, T1 spino-pelvic inclination; TK, thoracic kyphosis; LL, lumbar lordosis; PT, pelvic tilt; PI, pelvic incidence; SVA, sagittal vertical axis; UIV, upper instrumented vertebra; T1-UIV, angle between T1 and UIV; Unfused-PJA, proximal junctional angle of unfused spine.
Data and Statistical Analysis
Chi-square test and Mann-Whitney U test were used to compare differences between the 2 groups. Friedman’s test was used for statistical comparison of differences among the 3 groups. The mean difference of continuous measures across the groups was compared using a one-way analysis of variance followed by Dunnett’s test. The correlations between each parameter of spinal alignment were determined using Spearman’s rank coefficients. Statistical analyses were performed using Stat Flex Ver. 6 (Artech, Tokyo).
Results
Demographic Data Comparison Between Groups
Demographics parameters are shown in Table 1. Twenty-six patients (23 women; 3 men) with a minimum follow-up of 2 years (34.9 ± 6.1 [24-44] months; mean ± SD [range]) were recruited. The average age at surgery was 72.5 ± 6.4 (57-83) years. Staged surgery was performed in 14 patients (53.8%). The average number of fused segments was 8.7 ± 1.6 (5-11) segments. Eight, 14, and 4 patients underwent multilevel PCO, PSO, and VCR, respectively. The most common upper instrumented vertebra and site of vertebral osteotomy was T10 and L3, respectively. There were no significant differences between the Ideal and Non-Ideal groups, except for the age and diagnosis ratio of degenerative kyphosis.
Table 1.
Baseline Demographic Parameters for All Patients and the Ideal and Non-Ideal Groups.
| All patients | Ideal group | Non-ideal group | P | |
|---|---|---|---|---|
| Follow-up (months) | 34.9 ± 6.1 | 34.7 ± 5.9 | 35.0 ± 6.6 | .79 |
| Sex (male: female) | 3:23 | 1:12 | 2:11 | .54 |
| Age at operation (years) | 72.5 ± 6.4 | 69.4 ± 7.4 | 75.6 ± 3.2 | <.05* |
| BMI (kg/m2) | 21.9 ± 3.4 | 21.6 ± 2.8 | 22.2 ± 4.0 | .82 |
| History of past operation, n (%) | 7 (26.9) | 2 (15.4) | 5 (38.5) | .18 |
| Diagnosis | ||||
| Degenerative kyphosis, n (%) | 15 (57.7) | 10 (76.9) | 5 (38.5) | <.05* |
| Posttraumatic kyphosis, n, (%) | 4 (15.4) | 1 (7.7) | 3 (23.1) | .28 |
| Iatrogenic flatback, n, (%) | 7 (26.9) | 2 (15.4) | 5 (38.5) | .18 |
| Type of operation | ||||
| Staged surgery, n, (%) | 14 (53.8) | 6 (46.2) | 8 (61.5) | .43 |
| UIVa | 10.4 ± 1.6 | 10.2 ± 1.8 | 10.5 ± 1.3 | .69 |
| Number of fused segments | 8.7 ± 1.6 | 8.8 ± 1.8 | 8.5 ± 1.3 | .49 |
| Method of osteotomy, n (PCO: PSO: VCR) | 8: 14: 4 | 5: 7: 1 | 3: 7: 3 | .47 |
| Site of osteotomya,b | 15.0 ± 1.5 | 15.1 ± 1.4 | 14.9 ± 1.7 | .82 |
Abbreviations: BMI, body mass index; UIV, upper instrumented vertebra; PCO, posterior column osteotomy; PSO, pedicle subtraction osteotomy; VCR, vertebral column resection.
a A numerical value has been attributed to each vertebral level, with 1 = T1, 2 = T2, 3 = T3,…, 12 = T12, 13 = L1,…, 17 = L5, 18 = Pelvis.
b Site of osteotomy was calculated only in patients with PSO or VCR.
* Statistically significant difference between the Ideal and Non-Ideal groups. P < .05 (statistical significance).
Radiographic Parameters at Baseline by Group
Radiographic parameters at baseline are described in Table 2. When comparing both groups, the Non-Ideal group had greater preoperative sagittal imbalance in terms of SVA (85.9 vs 175.0 mm, P < .01 [Ideal group vs Non-Ideal group]) and T1SPI (1.7° vs 12.7°, P < .01). When comparing the thoracic parameters, the Non-Ideal group had greater TK (17.2° vs 29.6°, P < .05) and T1-UIV (12.6° vs 22.0°, P < .05), indicating that the Ideal group had greater thoracic compensation than the Non-Ideal group.
Table 2.
Baseline Preoperative Radiographic Parameters for All Patients and the Ideal and Non-Ideal Groups.
| All patients | Ideal group | Non-Ideal group | P | |
|---|---|---|---|---|
| PI | 47.9 ± 9.1 | 46.1 ± 8.2 | 49.8 ± 10.0 | .26 |
| PT | 33.0 ± 11.8 | 32.5 ± 10.3 | 33.5 ± 13.6 | .72 |
| LL | 2.0 ± 17.4 | 4.1 ± 13.7 | −0.2 ± 20.9 | .70 |
| TK | 23.4 ± 14.5 | 17.2 ± 16.2 | 29.6 ± 9.6 | <.05* |
| PI − LL | 46.0 ± 19.4 | 42.0 ± 16.9 | 49.9 ± 21.5 | .32 |
| SVA | 130.5 ± 74.7 | 85.9 ± 43.6 | 175.0 ± 73.6 | <.01* |
| T1SPI | 7.2 ± 8.9 | 1.7 ± 4.7 | 12.7 ± 8.8 | <.01* |
| T1-UIV | 17.3 ± 15.1 | 12.6 ± 17.0 | 22.0 ± 11.7 | <.05* |
| Unfused-PJA | 1.2 ± 7.8 | −0.5 ± 9.5 | 2.9 ± 5.5 | .55 |
Abbreviations: PI, pelvic incidence; PT, pelvic tilt; LL, lumbar lordosis; TK, thoracic kyphosis; PI − LL, pelvic incidence minus lumbar lordosis; SVA, sagittal vertical axis; T1SPI, T1 spino-pelvic inclination; T1-UIV, angle between T1 and UIV; Unfused-PJA, proximal junctional angle of unfused spine.
* Statistically significant difference between the Ideal and Non-Ideal groups. P < .05 (statistical significance).
Radiographic Outcome by Group
The time courses of the radiographic parameters of spinal alignment after correction surgery are summarized in Table 3. In all the patients, all radiographic parameters, except for PI, showed significant differences from baseline to final follow-up. Concerning the unfused spine specifically, the average preoperative T1-UIV was 17.3°, which increased immediately to 29.5° after the operation and then to 33.5° at the final follow-up. The ratio of angles of the proximal junctional section (unfused-PJA) at the unfused thoracic spine gradually increased from postoperative to the final follow-up.
Table 3.
Radiographic Parameters of Preoperative, Postoperative, and Final Follow-up Radiographs for All Patients and the Ideal Group and Non-Ideal Groups.
| Preop | Postop | Final-follow | P (Friedman) | P (Dunnett’s) | ||
|---|---|---|---|---|---|---|
| P a | P b | |||||
| All patients | ||||||
| PI | 47.9 ± 9.1 | 46.2 ± 9.0 | 47.2 ± 10.2 | ns | ns | ns |
| PT | 33.0 ± 11.8 | 15.1 ± 8.2 | 19.5 ± 9.2 | <.001* | <.01* | <.01* |
| LL | 2.0 ± 17.4 | 42.0 ± 10.1 | 40.4 ± 10.3 | <.001* | <.01* | <.01* |
| TK | 23.4 ± 14.5 | 36.6 ± 11.9 | 42.4 ± 11.9 | <.001* | <.01* | <.01* |
| PI − LL | 46.0 ± 19.4 | 4.2 ± 11.3 | 6.8 ± 12.1 | <.001* | <.01* | <.01* |
| SVA | 130.5 ± 74.7 | 33.7 ± 49.7 | 41.7 ± 49.9 | <.001* | <.01* | <.01* |
| T1SPI | 7.2 ± 8.9 | −2.3 ± 6.5 | −1.8 ± 5.9 | <.001* | <.01* | <.01* |
| T1-UIV | 17.3 ± 15.1 | 29.5 ± 8.8 | 33.5 ± 9.5 | <.001* | <.01* | <.01* |
| Unfused-PJA | 1.2 ± 7.8 | 6.9 ± 6.4 | 10.8 ± 7.7 | <.001* | <.05* | <.01* |
| Ideal group | ||||||
| PI | 46.1 ± 8.2 | 45.1 ± 7.9 | 44.5 ± 7.1 | ns | ns | ns |
| PT | 32.5 ± 10.3 | 12.0 ± 4.1 | 15.9 ± 5.1 | <.001* | <.01* | <.01* |
| LL | 4.1 ± 13.7 | 45.8 ± 7.4 | 43.9 ± 8.5 | <.001* | <.01* | <.01* |
| TK | 17.2 ± 16.2 | 36.4 ± 10.5 | 41.5 ± 12.0 | <.001* | <.01* | <.01* |
| PI − LL | 42.0 ± 16.9 | −0.7 ± 7.3 | 0.7 ± 6.4 | <.001* | <.01* | <.01* |
| SVA | 85.9 ± 43.6 | 3.9 ± 24.4 | 5.3 ± 26.4 | <.001* | <.01* | <.01* |
| T1SPI | 1.7 ± 4.7 | −4.9 ± 4.8 | −5.2 ± 3.6 | <.001* | <.01* | <.01* |
| T1-UIV | 12.6 ± 17.0 | 29.6 ± 9.3 | 34.0 ± 12.1 | <.001* | <.01* | <.01* |
| Unfused-PJA | −0.5 ± 9.5 | 8.0 ± 6.4 | 12.2 ± 9.0 | <.001* | <.05* | <.01* |
| Non-Ideal group | ||||||
| PI | 49.8 ± 10.0 | 47.3 ± 10.2 | 49.8 ± 12.3 | ns | ns | ns |
| PT | 33.5 ± 13.6 | 18.2 ± 10.2 | 23.1 ± 11.1 | <.001* | <.01* | ns |
| LL | −0.2 ± 20.9 | 38.2 ± 11.8 | 36.9 ± 11.0 | <.001* | <.01* | <.01* |
| TK | 29.6 ± 9.6 | 36.8 ± 13.5 | 43.3 ± 12.2 | <.001* | ns | <.01* |
| PI − LL | 49.9 ± 21.5 | 9.1 ± 12.8 | 12.9 ± 13.6 | <.001* | <.01* | <.01* |
| SVA | 175.0 ± 73.6 | 63.5 ± 51.2 | 78.1 ± 40.4 | <.001* | <.01* | <.05* |
| T1SPI | 12.7 ± 8.8 | 0.4 ± 7.1 | 1.5 ± 5.9 | <.001* | <.01* | <.01* |
| T1-UIV | 22.0 ± 11.7 | 29.5 ± 8.7 | 33.0 ± 6.5 | <.001* | ns | <.01* |
| Unfused-PJA | 2.9 ± 5.5 | 5.7 ± 6.5 | 9.3 ± 6.2 | <.01* | ns | <.01* |
Abbreviations: Preop, preoperative radiograph; postop, postoperative radiograph; final-follow, final follow-up radiograph; PI, pelvic incidence; PT, pelvic tilt; LL, lumbar lordosis; TK, thoracic kyphosis; PI − LL, indicates pelvic incidence minus lumbar lordosis; SVA, sagittal vertical axis; T1SPI, T1 spino-pelvic inclination; T1-UIV, angle between T1 and UIV; Unfused-PJA, proximal junctional angle of unfused spine.
a Comparison of radiographic parameters between preoperative and postoperative X-rays.
b Comparison of radiographic parameters between preoperative and final follow-up X-rays.
*P < .05 (statistical significance).
Relationship of Reciprocal Change (T1-UIV Angle) Between Preoperative Whole Spine Full-Flexion Radiograph and Postoperative and Final Follow-up Radiographs by Group
Correlations of T1-UIV of the preoperative whole spine full-flexion radiograph and postoperative T1-UIV of the standing radiograph are presented in Table 4. In all patients, the T1-UIV of the whole spine full-flexion radiograph obtained preoperatively exhibited significant correlation with the T1-UIVs of the postoperative and final follow-up radiographs (r = 0.64, P < .01, y = 0.800x + 8.012, and r = 0.69, P < .01, y = 0.857x + 2.960). Interestingly, this correlation was stronger for the Ideal group (r = 0.77, P < .01, y = 1.207x - 1.517, and r = 0.89, P < .01, y = 0.986x + 0.694). However, there were no significant correlations found in the Non-Ideal group when the same analysis was performed.
Table 4.
Groupwise Correlations of T1-UIV Angle Measured Using Preoperative Whole Spine Full Flexion Lateral Radiograph, Postoperative Radiograph, and Final Follow-up Radiograph.
| Preop | Full flexion | Postop | Final-follow | Full flexion and postop | Full flexion and final-follow | |||
|---|---|---|---|---|---|---|---|---|
| r | P | r | P | |||||
| All patients | 17.3 ± 15.1 | 31.7 ± 10.9 | 29.5 ± 8.8 | 33.5 ± 9.5 | 0.64 | P < .01* | 0.69 | P < .01* |
| Ideal group | 12.6 ± 17.0 | 34.2 ± 13.2 | 29.6 ± 9.3 | 34.0 ± 12.1 | 0.77 | P < .01* | 0.89 | P < .01* |
| Non-Ideal group | 22.0 ± 11.7 | 29.1 ± 7.6 | 29.5 ± 8.7 | 33.0 ± 6.5 | 0.44 | ns | 0.35 | ns |
Abbreviations: preop, preoperative radiograph; full flexion, whole spine full flexion lateral radiograph; postop, postoperative radiograph; final-follow, final follow-up radiograph; T1-UIV, angle between T1 and UIV.
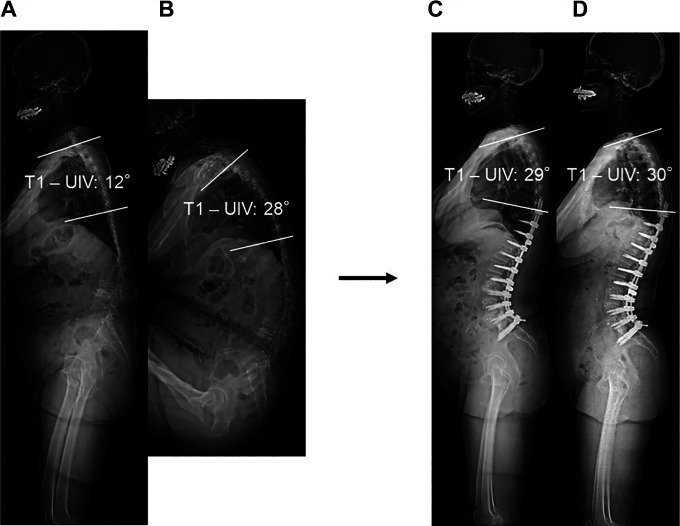
Case Presentation
Figure 3 shows that the Ideal group had hypokyphosis in the thoracic spine due to a compensatory mechanism preoperatively. The T1-UIV of the preoperative whole spine full-flexion lateral radiograph was similar to those postoperatively and at the final follow-up. ([a] T1-UIV preoperatively: 12°, [b] whole spine full-flexion radiograph: 28°, [c] postoperative: 29°, and [d] final follow-up: 30°).
Figure 3.
Time course of T1-UIV after correction surgery in a patient with Ideal group. (a) Baseline preoperative radiograph in standing position. (b) Whole spine full flexion lateral radiograph. (c) Postoperative radiograph. (d) Final follow-up radiograph. These X-ray images demonstrating reciprocal changes and whole spine full flexion lateral radiograph correctly estimate the postoperative alignment of unfused thoracic spine. Abbreviations: T1-UIV, angle between T1 and UI.V.
Discussion
ASD is a health care issue of increasing concern owing to the super-aging society. Surgical restoration of spinopelvic harmony following correction strategies is essential.6-11 Increasing attention has been given to the reciprocal change of the unfused spine, which may negatively affect global sagittal alignment after correction surgery.12-16 Formulae that do not consider this reciprocal change may underestimate the amount of correction required.12,16,18 A recent article evaluated the postoperative outcomes based on the thoracic compensatory mechanism and concluded that patients with less compensatory changes in the thoracic spine have poorer outcomes.19 Furthermore, another study that assessed the surgeon’s ability to accurately predict postoperative alignment demonstrated that predicting postoperative parameters represents a significant challenge, especially in TK, although all survey participants had experience with high levels of spine deformity.20 Therefore, to obtain the ideal sagittal alignment, we must focus more on the reciprocal mechanism of the unfused spine.
T1-UIV is a novel parameter defined to represent the alignment of the unfused spine, and there were no reports on a similar concept. In the present study, using a novel radiographic strategy (T1-UIV of preoperative whole spine full-flexion lateral radiograph), we could estimate the postoperative alignment of the unfused thoracic spine correctly. It was more useful if the surgery achieved adequate correction. The results of our study are relatively intuitive based on previous reports describing that the alignment of the unfused thoracic spine changes from hypokyphosis to “resume” kyphosis alignment.12-16 However, this has not been previously investigated.
Lafage et al showed that the majority of compensatory changes of the unfused thoracic spine after correction surgery led to a poorer overall sagittal alignment.12 Although the extension of fusion to the proximal thoracic levels would decrease the sagittal imbalance caused by reciprocal thoracic change,11,19 Miyakoshi et al showed that a decrease in the spinal range of motion (ROM) had adverse effects on QOL.21 Furthermore, Imagama et al identified that thoracic ROM is an important factor for good QOL.22 Therefore, the number of fused levels would be minimal. Notably, in these patients, preoperative assessments of the unfused spine using our strategy will help plan the surgery.
To clarify the reciprocal change of the unfused spine, we divided the patients into the Ideal and Non-Ideal groups according to the final follow-up radiograph because persistent imbalance postoperatively can affect the thoracic compensatory mechanism. To validate the classification of the Ideal group, we assessed the optimal PT of our subjects using another formula that was constructed using Japanese healthy elderly volunteers, and we concluded that the optimal PT of our Ideal group was almost equivalent.10
The patients in the Non-Ideal group were 6 years older, and the group had fewer cases of degenerative kyphosis than the Ideal group. In the present study, relatively older patients were investigated in both groups, which is consistent with literature indicating that patients with failed realignment surgery were older.23 Patients with degenerative kyphosis were more likely to achieve better correction when undergoing correction surgery than when undergoing revision surgery, which was also consistent with the findings of a previous study.24 We also evaluated the preoperative radiographic parameters between groups and observed that the Non-Ideal group has significantly greater sagittal imbalance. Interestingly, despite having greater preoperative imbalance, TK of the Non-Ideal group was greater, indicating that the Non-Ideal group had lesser thoracic compensation than the Ideal group, which might be the effect of the back muscle. Even though we could not evaluate the back muscle, a previous study showed that sagittal balance was maintained well in patients with strong back muscle strength.22
In the present study, the average TK was improved from 23.4° to 36.6° postoperatively and further increased at the final follow-up to 42.4°. These TK changes were consistent with the findings of previous studies.13,14,16 Notably, we found that the unfused-PJA/T1-UIV ratio gradually increased from 23.4% to 32.0% at the final follow-up, which might reflect degenerative disc changes that generally occur at the adjacent discs after spinal instrumentation, as there were no changes in vertebral body shape because we excluded patients with type-2 PJK (bone failure).17
Some previous articles demonstrated that the postoperative alignment of the thoracic spine was improved to kyphosis.12-16 These findings were interesting, but these results may be difficult to use in a clinical setting. Given that they measured TK from T4 or T5 to T12, some of those segments were fixed. Therefore, there was a possibility that the increase in kyphosis in these articles was affected by the fused segment. Yasuda et al have developed the equation for predicting postoperative TK.13 Although this formula represents important steps in improving postoperative alignment prediction, they measured TK, including the fused segment. Furthermore, the lack of information on the flexibility may be crucial because spine flexibility differs in each patient, as shown in the present study. Thus, the present study is more feasible, as we evaluated the true postoperative change of unfused spine.
To calculate the minimum goal of LL, Rose et al developed the formula “LL ≤45 − TK − PI” (LL is expressed as a negative number).11 However, after predicting the LL goal, they only performed modest adjustment without a theoretical approach because TK increases after correction surgery. Other formulae did not also address the reciprocal change of the unfused spine.6,10 Thus, after calculating LL, surgeons should perform radiographic tracing/cutout procedures, including for the unfused thoracic spine, following our strategy. Through this procedure, the surgeon can predict the precise postoperative sagittal alignment, including unfused thoracic compensation. Consequently, we can prevent both overcorrection and undercorrection, which may be a risk factor of PJK development. Furthermore, in some cases where significant reciprocal change was expected, fixation should be extended to the upper thoracic levels, as a previous study found that preoperative and postoperative TK did not change in patients with fusion in the upper thoracic levels after correction surgery.11
This study has several limitations. First, the number of subjects was inadequate for drawing conclusions from, because the study was retrospective in nature. Hence, the participants may not be representative of the general population. Second, our minimum follow-up period of 2 years can also be interpreted as being relatively short, especially because unfused spinal alignment could develop at >2 years postoperatively in some patients. Third, we could not evaluate the clinical outcomes, and the impact of our strategy is still unknown. Further studies focusing on clinical outcomes are needed. Finally, we excluded patients with type-2 PJK (bone failure). A previous article interpreted that PJK was a compensatory mechanism rather than just an alignment failure.15 However, other articles revealed that postoperative alignment changes of the thoracic spine after correction surgery, including PJK, were not simply due to junctional failure.12 Therefore, to clarify the pure mechanism of unfused reciprocal change, we excluded these patients. Nevertheless, our study also has strengths. Our novel strategy is simple enough to be used in a clinical setting, since we only performed the whole spine full-flexion lateral radiograph preoperatively. Furthermore, this is the first study to analyze unfused spinal alignment using a new parameter known as T1-UIV.
Conclusion
The present investigation can offer insights into unfused thoracic reciprocal change after correction surgery and confirmed that the novel radiographic parameter (T1-UIV of whole spine full-flexion lateral radiograph) facilitates the prediction of postoperative unfused thoracic alignment. Accounting for these changes may prevent postoperative imbalance in some cases and permit greater confidence in selecting fused segments and the amount of correction.
Supplementary Materials
Supplemental Material, GSJ,_recipro,_Supplemental_Material for Thoracic Reciprocal Change Can Be Predicted Before Surgery in Adult Spinal Deformity by Koji Ishikawa, Yusuke Nakao, Fumihiko Oguchi, Tomoaki Toyone and Shigeo Sano in Global Spine Journal
Supplemental Material, Reciprocal_change_Supplemental_legend_200629 for Thoracic Reciprocal Change Can Be Predicted Before Surgery in Adult Spinal Deformity by Koji Ishikawa, Yusuke Nakao, Fumihiko Oguchi, Tomoaki Toyone and Shigeo Sano in Global Spine Journal
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Koji Ishikawa, MD, PhD  https://orcid.org/0000-0003-3689-5662
https://orcid.org/0000-0003-3689-5662
Yusuke Nakao, MD  https://orcid.org/0000-0002-3869-2941
https://orcid.org/0000-0002-3869-2941
Supplementary Materials: Supplemental material for this article is available online.
References
- 1.Schwab F, Dubey A, Gamez L, et al. Adult scoliosis: prevalence, SF-36, and nutritional parameters in an elderly volunteer population. Spine (Phila Pa 1976). 2005;30:1082–1085. [DOI] [PubMed] [Google Scholar]
- 2.Glassman SD, Bridwell K, Dimar JR, Horton W, Berven S, Schwab F. The impact of positive sagittal balance in adult spinal deformity. Spine (Phila Pa 1976). 2005;30:2024–2029. [DOI] [PubMed] [Google Scholar]
- 3.Lafage V, Schwab F, Patel A, Hawkinson N, Farcy JP. Pelvic tilt and truncal inclination: two key radiographic parameters in the setting of adults with spinal deformity. Spine (Phila Pa 1976). 2009;34:E599–E606. [DOI] [PubMed] [Google Scholar]
- 4.Kim YJ, Bridwell KH, Lenke LG, Rhim S, Cheh G. Sagittal thoracic decompensation following long adult lumbar spinal instrumentation and fusion to L5 or S1: causes, prevalence, and risk factor analysis. Spine (Phila Pa 1976). 2006;31:2359–2366. [DOI] [PubMed] [Google Scholar]
- 5.Lazennec JY, Ramaré S, Arafati N, et al. Sagittal alignment in lumbosacral fusion: relations between radiological parameters and pain. Eur Spine J. 2000;9:47–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schwab F, Ungar B, Blondel B, et al. Scoliosis Research Society-Schwab adult spinal deformity classification: a validation study. Spine (Phila Pa 1976). 2012;37:1077–1082. [DOI] [PubMed] [Google Scholar]
- 7.Kim HJ, Lenke LG, Shaffrey CI, Van Alstyne EM, Skelly AC. Proximal junctional kyphosis as a distinct form of adjacent segment pathology after spinal deformity surgery: a systematic review. Spine (Phila Pa 1976). 2012;37(27 suppl):S144–S164. [DOI] [PubMed] [Google Scholar]
- 8.Schwab FJ, Blondel B, Bess S, et al. Radiographical spinopelvic parameters and disability in the setting of adult spinal deformity: a prospective multicenter analysis. Spine (Phila Pa 1976). 2013;38:E803–E812. [DOI] [PubMed] [Google Scholar]
- 9.Schwab F, Patel A, Ungar B, Farcy JP, Lafage V. Adult spinal deformity-postoperative standing imbalance: how much can you tolerate? An overview of key parameters in assessing alignment and planning corrective surgery. Spine (Phila Pa 1976). 2010;35:2224–2231. [DOI] [PubMed] [Google Scholar]
- 10.Yamato Y, Hasegawa T, Kobayashi S, et al. Calculation of the target lumbar lordosis angle for restoring an optimal pelvic tilt in elderly patients with adult spinal deformity. Spine (Phila Pa 1976). 2016;41:E211–E217. [DOI] [PubMed] [Google Scholar]
- 11.Rose PS, Bridwell KH, Lenke LG, et al. Role of pelvic incidence, thoracic kyphosis, and patient factors on sagittal plane correction following pedicle subtraction osteotomy. Spine (Phila Pa 1976). 2009;34:785–791. [DOI] [PubMed] [Google Scholar]
- 12.Lafage V, Ames C, Schwab F, et al. Changes in thoracic kyphosis negatively impact sagittal alignment after lumbar pedicle subtraction osteotomy: a comprehensive radiographic analysis. Spine (Phila Pa 1976). 2012;37:E180–E187. [DOI] [PubMed] [Google Scholar]
- 13.Yasuda T, Hasegawa T, Yamato Y, et al. Postoperative change of thoracic kyphosis after corrective surgery for adult spinal deformity. Spine Surg Relat Res. 2018;2:283–289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jang JS, Lee SH, Min JH, Maeng DH. Influence of lumbar lordosis restoration on thoracic curve and sagittal position in lumbar degenerative kyphosis patients. Spine (Phila Pa 1976). 2009;34:280–284. [DOI] [PubMed] [Google Scholar]
- 15.Lafage R, Bess S, Glassman S, et al. Virtual modeling of postoperative alignment after adult spinal deformity surgery helps predict associations between compensatory spinopelvic alignment changes, overcorrection, and proximal junctional kyphosis. Spine (Phila Pa 1976). 2017;42:E1119–E1125. [DOI] [PubMed] [Google Scholar]
- 16.Klineberg E, Schwab F, Ames C, et al. Acute reciprocal changes distant from the site of spinal osteotomies affect global postoperative alignment. Adv Orthop. 2011;2011:415946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yagi M, Akilah KB, Boachie-Adjei O. Incidence, risk factors and classification of proximal junctional kyphosis: surgical outcomes review of adult idiopathic scoliosis. Spine (Phila Pa 1976). 2011;36:E60–E68. [DOI] [PubMed] [Google Scholar]
- 18.Lafage V, Schwab F, Vira S, Patel A, Ungar B, Farcy JP. Spino-pelvic parameters after surgery can be predicted: a preliminary formula and validation of standing alignment. Spine (Phila Pa 1976). 2011;36:1037–1045. [DOI] [PubMed] [Google Scholar]
- 19.Oe S, Togawa D, Yamato Y, et al. Comparison of postoperative outcomes according to compensatory changes of the thoracic spine among patients with a T1 slope more than 40°. Spine (Phila Pa 1976). 2019;44:579–587. [DOI] [PubMed] [Google Scholar]
- 20.Ailon T, Scheer JK, Lafage V, et al. Adult spinal deformity surgeons are unable to accurately predict postoperative spinal alignment using clinical judgment alone. Spine Deform. 2016;4:323–329. [DOI] [PubMed] [Google Scholar]
- 21.Miyakoshi N, Itoi E, Kobayashi M, Kodama H. Impact of postural deformities and spinal mobility on quality of life in postmenopausal osteoporosis. Osteoporos Int. 2003;14:1007–1012. [DOI] [PubMed] [Google Scholar]
- 22.Imagama S, Matsuyama Y, Hasegawa Y, et al. Back muscle strength and spinal mobility are predictors of quality of life in middle-aged and elderly males. Eur Spine J. 2011;20:954–961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schwab FJ, Patel A, Shaffrey CI, et al. Sagittal realignment failures following pedicle subtraction osteotomy surgery: are we doing enough? Clinical article. J Neurosurg Spine. 2012;16:539–546. [DOI] [PubMed] [Google Scholar]
- 24.Gupta MC, Ferrero E, Mundis G, et al. Pedicle subtraction osteotomy in the revision versus primary adult spinal deformity patient: is there a difference in correction and complications? Spine (Phila Pa 1976). 2015;40:E1169–E1175. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, GSJ,_recipro,_Supplemental_Material for Thoracic Reciprocal Change Can Be Predicted Before Surgery in Adult Spinal Deformity by Koji Ishikawa, Yusuke Nakao, Fumihiko Oguchi, Tomoaki Toyone and Shigeo Sano in Global Spine Journal
Supplemental Material, Reciprocal_change_Supplemental_legend_200629 for Thoracic Reciprocal Change Can Be Predicted Before Surgery in Adult Spinal Deformity by Koji Ishikawa, Yusuke Nakao, Fumihiko Oguchi, Tomoaki Toyone and Shigeo Sano in Global Spine Journal