Abstract
Study Design:
Review of the best-validated measures of cervical spine alignment in the sagittal axis.
Objective:
Describe the C2-C7 Cobb Angle, C2-C7 sagittal vertical axis, chin-brow to vertical angle, T1 slope minus C2-C7 lordosis, C2 slope, and different types of cervical kyphosis.
Methods:
Search PubMed for recent technical literature on radiograph-based measurements of the cervical spine.
Results:
Despite the continuing use of measures developed many years ago such as the C2-C7 Cobb angle, there are new radiographic parameters being published and utilized in recent years, including the C2 slope. Further research is needed to compare older and newer measures for cross-validation. Utilizing these measures to determine the degree of correction intraoperatively and postoperatively will enable surgeons to optimize patient-level outcomes.
Conclusion:
Cervical spinal deformity can be a debilitating condition characterized by cervical spinal misalignment that affects the elderly more commonly than young populations. Many of these validated measures of cervical spinal alignment are useful in clinical settings due to their ease of implementation and correlations with various postoperative and health-related quality of life outcomes.
Keywords: cervical spinal deformity, cobb angle, sagittal vertical axis, horizontal gaze, T1 slope, C2 slope, lordosis, kyphosis
Introduction
Cervical spinal deformity (CSD) is a debilitating condition characterized by cervical spinal misalignment that mainly affects adults. Despite its severity, cervical spinal deformities (Figure 1) are less well-characterized than thoracolumbar spinal deformity. However, there are a number of well-validated radiographic measures that correlate with outcomes. In this section, we describe some of the most common, best-validated measures of cervical spinal alignment in the sagittal axis, including C2-C7 Cobb Angle, C2-C7 sagittal vertical axis, chin-brow to vertical angle, T1 slope minus C2-C7 lordosis, C2 slope, and different types of cervical kyphosis.
Figure 1.

Lateral cervical radiograph demonstrating satisfactory lordotic alignment with mild-moderate degenerative disc disease, most notable at C5-6.
C2-C7 Cobb Angle
Sagittal alignment is determined by calculating the Cobb angle between C2 and C7 (Figure 2).1 The Cobb angle is obtained by drawing parallel lines extending from the lower endplate of the most superior vertebral level and the lower endplate of the most inferior vertebral level being considered. From there, perpendicular lines are drawn from the previous lines, and the angle of their intersection is equal to the Cobb angle. Though other measures of cervical angular alignment do exist, including the Harrison posterior tangent and the Jackson physiological stress line, the C2-C7 Cobb angle remains one of the most frequently used for determining lordosis and kyphosis in the cervical spine.
Figure 2.
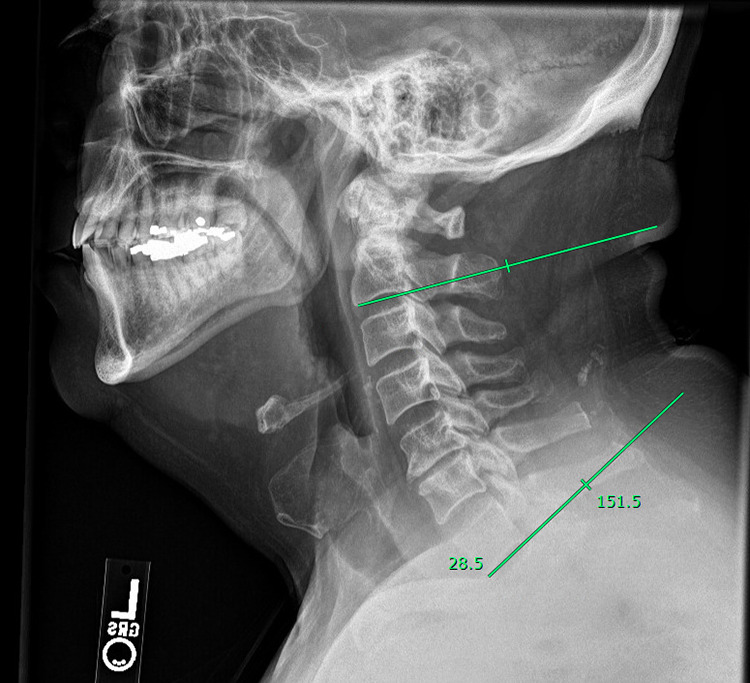
C2-7 Cobb Angle. Lateral cervical radiograph demonstrating the measurement of C2-7 Cobb Angle. The Cobb angle is obtained by drawing parallel lines extending from the lower endplate of the most superior vertebral level (C2) and the lower endplate of the most inferior vertebral level (C7). Perpendicular lines are then drawn from the parallel lines, and the angle of their intersection is equal to the Cobb angle.
Although sagittal alignment can vary in the normal cervical spine, a lordotic curvature somewhere between 20-35 degrees is typically maintained. One study by Yukawa et al used the C2-C7 Cobb angle to determine the degree of C2-C7 cervical lordosis in a population of 1,200 asymptomatic patients in Japan,2 and found that the average lordosis in the C2-C7 region was 13.9 ± 12.3 degrees. Gore et al. took a similar approach to determining the normal C2-C7 lordosis by using the Jackson physiological stress line method in a population of asymptomatic patients without any local kyphotic regions.1 This study found an average lordosis of 23 degrees. A study by Harrison et al. compared some of the various measures of cervical angular alignment, including the C1-C7 and C2-C7 Cobb angles and the Harrison posterior tangent method, and found that all measures had high inter- and intraclass correlations.3 Interestingly, this study also found that the C2-C7 Cobb angle may lead to an underestimation of lordosis in the cervical spine due to the orientation of the inferior endplate of C2. This finding appears to mirror the differences in normal cervical lordosis that were observed in the studies by Yukawa and Gore.
While the average degree of cervical lordosis does not appear to differ between males and females, there does appear to be a significant trend toward increased lordosis with age. A retrospective analysis of 151 patients with lateral cervical radiographs by Tang et al. found that the C2-C7 Cobb angle showed a significant positive correlation with age and that patients aged 65 years and older had significantly higher C2-C7 Cobb angles than patients in younger subgroups.4
C2-C7 Sagittal Vertical Axis
In general, measuring the cervical sagittal balance of a patient involves measuring the horizontal offset from a vertical reference line to a fixed location on some more inferior structure. The C2-C7 Sagittal Vertical Axis (SVA) is one of the most commonly implemented measures of cervical sagittal balance and is calculated by taking the horizontal distance between the posterosuperior corner of the C7 vertebral body and a plumb line drawn from the centroid of C2 (Figure 3).5 In contrast to the large variations described previously for normal angles of cervical lordosis, cervical sagittal balance as measured by C2-C7 SVA has classically been described as having a much narrower range. For example, Hardacker et al. determined that the C2-C7 SVA in standing asymptomatic volunteers was around 16.8 ± 11.2 mm.6
Figure 3.

C2-7 Sagittal Vertical Axis (SVA) is calculated by measuring the horizontal distance between the posterosuperior corner of the C7 vertebral body and a plumb line drawn from the centroid of C2. In general, C2-7 SVA < 4 centimeters is considered to be normal.
Importantly, several studies have found direct correlations with C2-C7 SVA measurements and patient scores on health-related quality of life measures. For example, one study found that C2-C7 SVA was significantly correlated with modified Japanese Orthopedic Association (mJOA) scores in patients with clinically diagnosed cervical spondylotic myelopathy.7 Another study found that C2-C7 SVA positively correlated with neck disability index (NDI) scores and negatively correlated with SF-36 physical component scores in patients following multilevel posterior cervical fusions.8 This same study also suggested that a C2-C7 SVA measurement of 40 mm or more could represent an upper limit, above which would be a cause for clinical concern given the strong correlation between cervical sagittal malalignment and quality of life outcomes.
Furthermore, given the important role that sagittal balance in the cervical spine plays in both the maintenance of head position and in the development of chronic neck pain, it is not surprising that some studies have examined the correlations between cervical sagittal imbalance and outcomes after cervical spine surgery. For example, one study found that patients with preoperative cervical sagittal translation had increased axial neck pain after surgery,9 while another study found that preoperative cervical sagittal imbalance was associated with significantly worse functional outcomes after cervical fusion.10
Horizontal Gaze
The chin-brow to vertical angle (CBVA) is one of the most frequently used measures of horizontal gaze (Figure 4). The CBVA is determined by drawing a line from the patient’s chin to their brow and taking the angle between this line and a vertical line drawn perpendicular to the ground. As such, tilting the head down so that the gaze is toward the floor produces a positive CBVA, while tilted the head up produces a negative CBVA. When the head is in a neutral position with the chin-brown line perpendicular to the floor, the CBVA is zero degrees. The CBVA may be measured using either standing radiographic methods or simply with a clinical photograph of the patient standing with the head in a neutral position and the knees and hips fully extended. These characteristics make the CBVA a relatively simple measurement to acquire. While there is no formal definition for a normal CBVA, one study reported an average CBVA or -1.7 degrees in 120 asymptomatic adults,11 while another study reported that a CBVA between -4.7 and +17.7 degrees was associated with the lowest scores on the Oswestry Disability Index in a cohort of 303 patients.12
Figure 4.
Chin-Brow Vertical Angle (CBVA) is determined by measuring a line drawn from the patient’s chin to their brow and taking the angle between this line and a vertical line drawn perpendicular to the ground. As such, tilting the head down so that the gaze is toward the floor produces a positive CBVA, while tilted the head up produces a negative CBVA. When the head is in a neutral position with the chin-brown line perpendicular to the floor, the CBVA is zero degrees.
Horizontal gaze is a fundamentally important aspect of a person’s quality of life and daily functioning. Accordingly, surgeries for spinal deformities that have incorporated the CBVA as a parameter of consideration have been shown to be significantly correlated with good outcomes postoperatively, including ambulation, gaze, and daily living activities.13-19 Although no studies in the literature have formally defined or rigorously validated a measurement of what an ideal target range CBVA is, one study suggested that a CBVA of approximately ±10 degrees may be desirable.18 Another study of patients who underwent surgery for ankylosing spondylitis recommended targeting a postoperative CBVA between 10-20 degrees to allow for optimal horizontal gaze, as patients with this postoperative CBVA range demonstrated the best results in terms of being able to carry out their daily activities.20 Of note, just as a large CBVA can interfere with many activities of daily living by preventing adequate horizontal gaze, overcorrection of the CBVA can pose similar detrimental effects, particularly during activities requiring a downward gaze such as walking down stairs. One previous study noted that a patient cohort whose CBVAs were overcorrected to < -10 degrees also reported experiencing difficulty with certain daily activities due to their significantly reduced scores for horizontal gaze.19
T1 Slope Minus C2-C7 Lordosis
The T1 slope is defined as the angle between a line drawn across the upper endplate of the T1 vertebra and the horizontal axis. The T1 slope is thus analogous to the sacral slope. Similar to how a greater pelvic incidence requires a greater lumbar lordosis to compensate, individuals with a greater T1 slope will also require more cervical lordosis to balance the head over the thoracic inlet.21 Although values for a normal range of cervical lordosis have not been fully established, it is well-documented in the literature that abnormal cervical lordosis in patients has been associated with worse postoperative outcomes following spine surgery. For example, one study found that abnormal cervical lordosis resulted in diminished improvements in neurological outcomes postoperatively following surgery for cervical myelopathy.22
Similar to the adverse effects of a mismatch in the compensation of lumbar lordosis to an increased pelvic incidence, a mismatch in the degree of cervical lordosis in response to an increased T1 slope can also be detrimental to patients. Accordingly, one relatively new metric that has been proposed in the literature to account for how much of a mismatch might exist is the T1 slope minus the degree of C2-C7 lordosis (TS-CL).5,8 To obtain the TS-CL measurement, the C2-C7 lordosis is first determined by drawing a line parallel to the C2 inferior endplate extending to the posterior aspect of the spinous process and another line parallel to the C7 inferior endplate. Perpendicular lines are then drawn from these previous lines, and the angle subtended by their intersection indicates the degree of cervical lordosis. Next, the T1 slope is calculated as previously described. The TS-CL angle is obtained by subtracting the previously determined C2-C7 lordosis angle from the T1 slope. Only recently have radiographic studies started to examine TS-CL both as a marker for cervical deformity and for defining the degree of surgical correction. One recent study used radiographic imaging of 103 spinal deformity cases along with linear regression analysis to more precisely understand the relationship between T1 slope and cervical lordosis.23 This study found a strong correlation between T1 slope and C2-C7 lordosis (r = 0.815), but no correlation between T1 slope and TS-CL. In addition, their linear regression analysis suggested that the TS-CL measure assumed a constant value of 16.5 ± 2 degrees, meaning that the degree of cervical lordosis could be estimated by using the equation: CL = T1 slope − 16.5 ± 2 degrees. Furthermore, the authors concluded that this formula could facilitate surgical decision making by helping provide a goal for correction.23 Recent studies have also sought to compare TS-CL with other measures of cervical misalignment as potential markers for preoperative measures of deformity severity and postoperative outcomes. For example, one study reported that pre- and post-operative NDI was significantly positively correlated with TS-CL, and suggested that TS-CL may be a more important estimate of cervical alignment than C2-C7 SVA.24
C2 Slope
The C2 slope (Figure 5A, B) has recently been proposed as a single, simplified measure of cervical deformity that approximates the TS-CL measure.25 It has been suggested that C2 slope can adequately describe cervical deformity due to its intimate connections with both the occipitocervical and cervico-thoracic spine. Mathematically, the following is reasoned: TS-CL = T1 slope − (C7 slope − C2 slope). In many patients, T1 slope and C7 slope are approximately equal, meaning that they cancel out in the equation, leaving C2 slope as the sole variable for measuring the deformity. In these instances in which T1 slope and C7 slope are approximately equal, the C2 slope can be obtained by drawing a line parallel to the C2 lower endplate and taking the angle between this line and the horizontal plane.
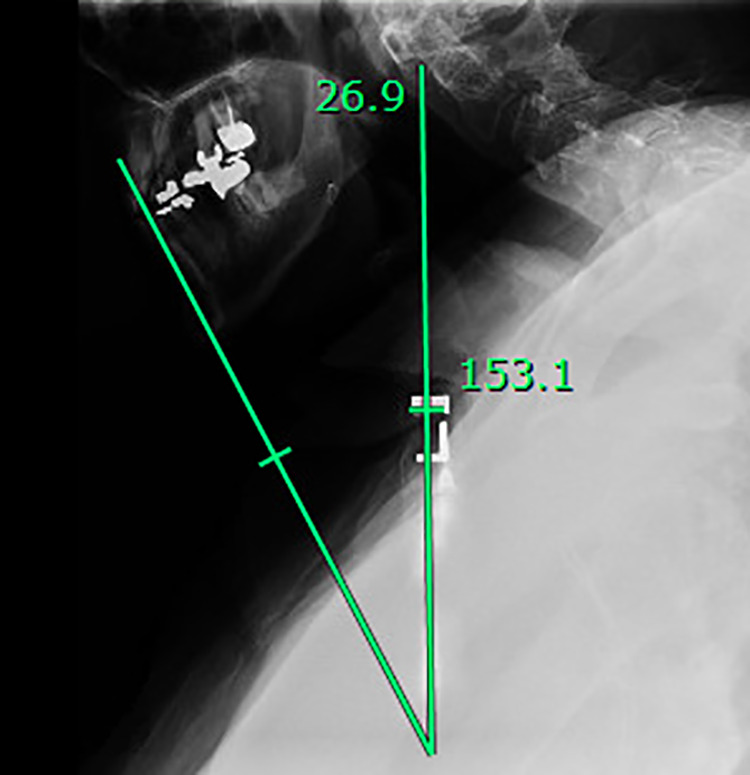
Figure 5.
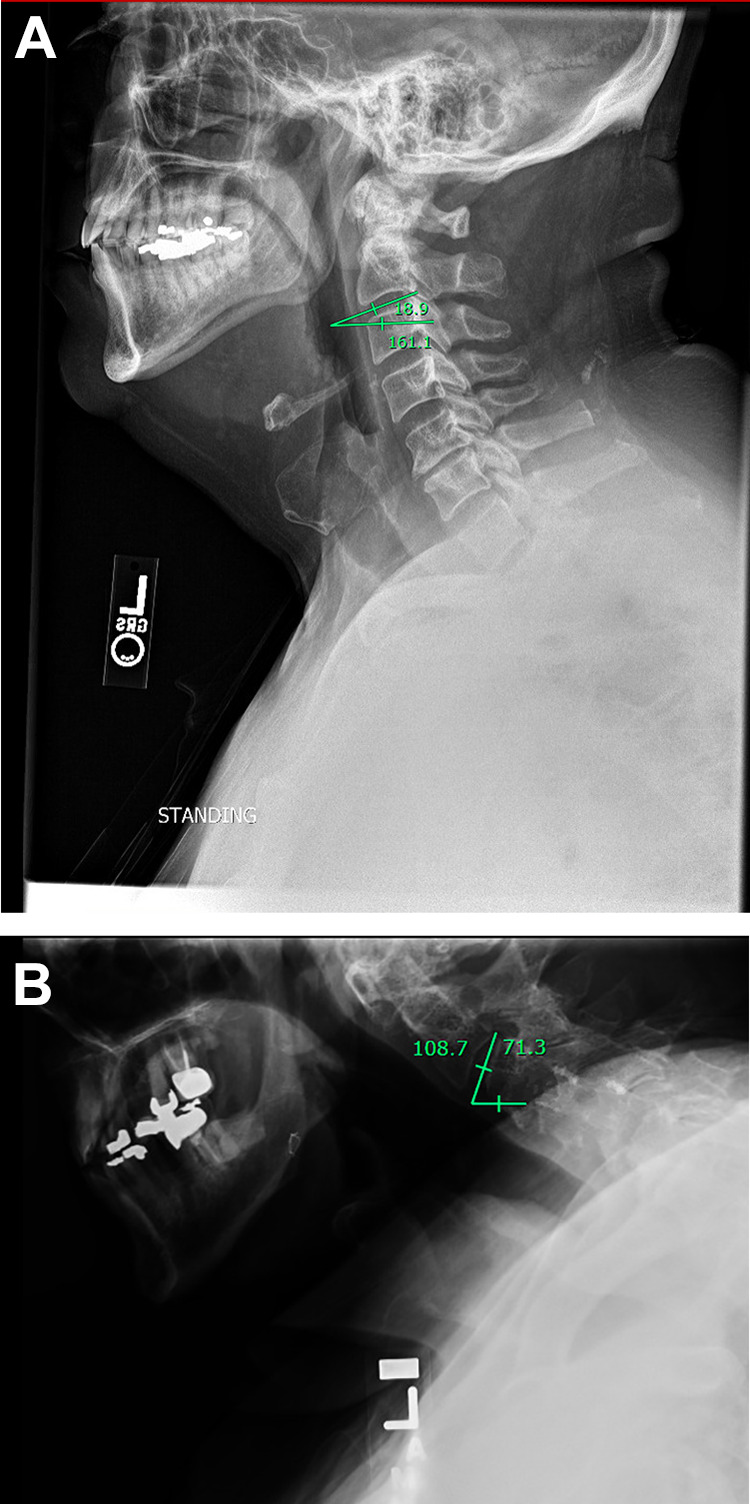
(A) C2 slope is measured on lateral radiograph by drawing a line parallel to the C2 lower endplate and taking the angle between this line and the horizontal plane. (B) In comparison to the patient in Figure 5(A), this patient, with C2-7 SVA > 4 centimeters and abnormal CBVA, the C2 slope is markedly elevated.
Importantly, there is evidence in the literature to suggest that C2 slope correlates with the TS-CL measurement, as well as health-related quality of life outcomes and measures of pain. A retrospective analysis of 104 patients with cervical deformity found that higher C2 slope postoperatively was associated with worse scores on the EuroQol 5 Dimension questionnaire (EQ5D), worse NDI scores, worse mJOA, and worse numeric rating scale for neck pain (cite Protopsaltis). Linear regression analysis revealed that a C2 slope of 20 degrees corresponded to moderate disability determined by the EQ5D. While the correlation to quality of life outcomes and the simplicity of obtaining this measurement are compelling reasons to consider using the C2 slope for assessing cervical deformity, this measurement is relatively new and further studies to validate its use and correlation to outcomes are warranted.
Cervical Kyphosis
When degenerative changes occur in the cervical spine, the natural lordotic curvature of this spinal region is lost. As the cervical spine becomes increasingly kyphotic, this can lead to greater spinal cord compression and adverse effects on cervical motion. There are several acknowledged subtypes of kyphotic cervical deformities. First, cervical kyphosis is classified as being either global (C-type) or focal. Focal kyphosis can be further subclassified as either a Sigmoid curve (S-type) or a Reverse sigmoid curve (R-type). The classification of these deformity subtypes can be determined by radiographic measurements as follows: for C-type deformities, all centroids of the cervical vertebrae must lie posterior to the C2-C7 centroid line (defined as a line connecting the C2 centroid with the C7 centroid), with at least 1 centroid sitting 2 mm or more away from the centroid line. For S-type deformities, at least one of the C2-C4 centroids must be anterior to the C2-C7 centroid line, while at least one of the C5-7 centroids must be posterior to this line and 1 centroid in the cervical spine must be at least 2 mm from the C2-C7 centroid line. For R-type deformities, at least one of the C2-C4 centroids must be posterior to the C2-C7 centroid line, while at least one of the C5-7 centroids must be anterior to this line and 1 centroid in the cervical spine must be at least 2 mm from the C2-C7 centroid line.26
Importantly, the effects of cervical kyphosis on spinal cord compression and cervical segmental motion depend upon the specific kyphotic subtype. These effects are detailed in a study by Ruangchainikom et al., which performed cervical kinematic magnetic resonance imaging (MRI) on symptomatic patients.26 This study found that R-type deformities produced more translational motion at the C3-C4 and C5-C6 levels compared to other deformity subtypes. In addition, patients with C- and R-type deformities were found to have increased angular motion of the C2-C4 levels upon extension compared to S-type deformity patients. Conversely, patients with S-type deformities were found to have increased angular motion of the C2-C4 levels upon flexion compared to C- and R-type deformity patients due to the fact that the S-type deformity have a lordosis in the C2-C4 region while C- and R-type deformity patients have a kyphosis. In terms of spinal cord compression, cervical extension produced more dynamic cord compression than flexion regardless of deformity subtype. Interestingly, however, R-type deformities were found to result in a higher degree of static cord compression at the C3-C4 level than the other deformity subtypes.
Given the demonstrated importance of the kyphotic deformity subtype in determining specific downstream effects such as spinal cord compression and cervical segmental motion, future work on cervical kyphotic deformities should be sure to characterize the specific deformity subtypes present in the patient population and, at the very least, control for these factors in subsequent analyses.
Conclusion
In this review, we sought to describe several of the most-commonly-used, best validated cervical spine radiographic measures. Despite the continuing usage of measures developed many years ago, such as the C2-C7 Cobb angle, there are new measurements being published and utilized in recent years, including the C2 slope, that are promising due to their clinical ease of implementation and connection with outcomes health-related quality of life. Indeed, however, a number of gaps exist in the knowledge base about quantifying cervical spinal deformity radiographically, and further research will be needed to compare these measures to each other for cross-validation and to explore new ways of measuring these deformities. Finally, in line with an emphasis on deformity correction, utilizing such measures to determine the degree of correction intraoperatively and postoperatively will hopefully allow surgeons to best optimize patient-level outcomes.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Michael L. Martini, PhD  https://orcid.org/0000-0001-8169-7679
https://orcid.org/0000-0001-8169-7679
Sean N. Neifert, BS  https://orcid.org/0000-0001-9298-8295
https://orcid.org/0000-0001-9298-8295
Jonathan J. Rasouli, MD  https://orcid.org/0000-0002-5085-8422
https://orcid.org/0000-0002-5085-8422
References
- 1.Gore DR, Sepic SB, Gardner GM. Roentgenographic findings of the cervical spine in asymptomatic people. Spine (Phila Pa 1976). 1986;11(6):521–524. [DOI] [PubMed] [Google Scholar]
- 2.Yukawa Y, Kato F, Suda K, Yamagata M, Ueta T.Age-related changes in osseous anatomy, alignment, and range of motion of the cervical spine. Part I: radiographic data from over 1,200 asymptomatic subjects. Eur Spine J. 2012;21(8):1492–1498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Harrison DE, Harrison DD, Cailliet R, Troyanovich SJ, Janik TJ, Holland B. Cobb method or Harrison posterior tangent method: which to choose for lateral cervical radiographic analysis. Spine (Phila Pa 1976). 2000;25(16):2072–2078. [DOI] [PubMed] [Google Scholar]
- 4.Tang R, Ye IB, Cheung ZB, Kim JS, Cho SK. Age-related changes in cervical sagittal alignment: a radiographic analysis. Spine (Phila Pa 1976). 2019;44(19):E1144–E1150. [DOI] [PubMed] [Google Scholar]
- 5.Ames CP, Smith JS, Eastlack R, et al. Reliability assessment of a novel cervical spine deformity classification system. J Neurosurg Spine. 2015;23(6):673–683. [DOI] [PubMed] [Google Scholar]
- 6.Hardacker JW, Shuford RF, Capicotto PN, Pryor PW. Radiographic standing cervical segmental alignment in adult volunteers without neck symptoms. Spine (Phila Pa 1976). 1997;22(13):1472–1480; discussion 80. [DOI] [PubMed] [Google Scholar]
- 7.Smith JS, Lafage V, Ryan DJ, et al. Association of myelopathy scores with cervical sagittal balance and normalized spinal cord volume: analysis of 56 preoperative cases from the AOSpine North America Myelopathy study. Spine (Phila Pa 1976). 2013;38(22S):S161–170. [DOI] [PubMed] [Google Scholar]
- 8.Tang JA, Scheer JK, Smith JS, et al. The impact of standing regional cervical sagittal alignment on outcomes in posterior cervical fusion surgery. Neurosurgery. 2012;71(3):662–669; discussion 9. [DOI] [PubMed] [Google Scholar]
- 9.Kato M, Namikawa T, Matsumura A, Konishi S, Nakamura H. Effect of cervical sagittal balance on laminoplasty in patients with cervical myelopathy. Global Spine J. 2017;7(2):154–161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Roguski M, Benzel EC, Curran JN, et al. Postoperative cervical sagittal imbalance negatively affects outcomes after surgery for cervical spondylotic myelopathy. Spine (Phila Pa 1976). 2014;39(25):2070–2077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Iyer S, Lenke LG, Nemani VM, et al. Variations in occipitocervical and cervicothoracic alignment parameters based on age: a prospective study of asymptomatic volunteers using full-body radiographs. Spine (Phila Pa 1976). 2016;41(23):1837–1844. [DOI] [PubMed] [Google Scholar]
- 12.Lafage R, Challier V, Liabaud B, et al. Natural head posture in the setting of sagittal spinal deformity: validation of chin-brow vertical angle, slope of line of sight, and McGregor’s slope with health-related quality of life. Neurosurgery. 2016;79(1):108–115. [DOI] [PubMed] [Google Scholar]
- 13.Deviren V, Scheer JK, Ames CP. Technique of cervicothoracic junction pedicle subtraction osteotomy for cervical sagittal imbalance: report of 11 cases. J Neurosurg Spine. 2011;15(2):174–181. [DOI] [PubMed] [Google Scholar]
- 14.Etame AB, Than KD, Wang AC, La Marca F, Park P. Surgical management of symptomatic cervical or cervicothoracic kyphosis due to ankylosing spondylitis. Spine (Phila Pa 1976). 2008;33(16):E559–564. [DOI] [PubMed] [Google Scholar]
- 15.Kim KT, Lee SH, Son ES, et al. Surgical treatment of “chin-on-pubis” deformity in a patient with ankylosing spondylitis: a case report of consecutive cervical, thoracic, and lumbar corrective osteotomies. Spine (Phila Pa 1976). 2012;37(16):E1017–1021. [DOI] [PubMed] [Google Scholar]
- 16.Kim KT, Suk KS, Cho YJ, Hong GP, Park BJ. Clinical outcome results of pedicle subtraction osteotomy in ankylosing spondylitis with kyphotic deformity. Spine (Phila Pa 1976). 2002;27(6):612–618. [DOI] [PubMed] [Google Scholar]
- 17.Pigge RR, Scheerder FJ, Smit TH, Mullender MG, Van Royen BJ. Effectiveness of preoperative planning in the restoration of balance and view in ankylosing spondylitis. Neurosurg Focus. 2008;24(1):E7. [DOI] [PubMed] [Google Scholar]
- 18.Scheer JK, Tang JA, Smith JS, et al. Cervical spine alignment, sagittal deformity, and clinical implications: a review. J Neurosurg Spine. 2013;19(2):141–159. [DOI] [PubMed] [Google Scholar]
- 19.Suk KS, Kim KT, Lee SH, Kim JM. Significance of chin-brow vertical angle in correction of kyphotic deformity of ankylosing spondylitis patients. Spine (Phila Pa 1976). 2003;28(17):2001–2005. [DOI] [PubMed] [Google Scholar]
- 20.Song K, Su X, Zhang Y, et al. Optimal chin-brow vertical angle for sagittal visual fields in ankylosing spondylitis kyphosis. Eur Spine J. 2016;25(8):2596–2604. [DOI] [PubMed] [Google Scholar]
- 21.Lee SH, Kim KT, Seo EM, Suk KS, Kwack YH, Son ES. The influence of thoracic inlet alignment on the craniocervical sagittal balance in asymptomatic adults. J Spinal Disord Tech. 2012;25(2):E41–47. [DOI] [PubMed] [Google Scholar]
- 22.Naderi S, Ozgen S, Pamir MN, Özek MM, Erzen C. Cervical spondylotic myelopathy: surgical results and factors affecting prognosis. Neurosurgery. 1998;43(1):43–49; discussion 9-50. [DOI] [PubMed] [Google Scholar]
- 23.Staub BN, Lafage R, Kim HJ, et al. Cervical mismatch: the normative value of T1 slope minus cervical lordosis and its ability to predict ideal cervical lordosis. J Neurosurg Spine. 2018;30(1):31–37. [DOI] [PubMed] [Google Scholar]
- 24.Lan Z, Huang Y, Xu W. Relationship between T1 slope minus C2-7 lordosis and cervical alignment parameters after adjacent 2-level anterior cervical diskectomy and fusion of lower cervical spine. World Neurosurg. 2019;122:e1195–e1201. [DOI] [PubMed] [Google Scholar]
- 25.Protopsaltis TS, Ramchandran S, Tishelman JC, et al. The Importance of C2 slope, a singular marker of cervical deformity, correlates with patient-reported outcomes. Spine (Phila Pa 1976). 2020;45(3):184–192. [DOI] [PubMed] [Google Scholar]
- 26.Ruangchainikom M, Daubs MD, Suzuki A, et al. Effect of cervical kyphotic deformity type on the motion characteristics and dynamic spinal cord compression. Spine (Phila Pa 1976). 2014;39(12):932–938. [DOI] [PubMed] [Google Scholar]


