Abstract
Background
The lockdowns during the COVID-19 pandemic created major obstacles for individuals with disabilities to obtain support in their daily living.
Objectives
This study was to examine the psychological and behavioral responses of US individuals with mobility and/or self-care disabilities during the pandemic.
Methods
From a nationally representative longitudinal survey (n = 6403) administered during the pandemic, individuals were classified at baseline as having no mobility/self-care disability (ADL = 0, n = 4975), mobility or self-care disability (ADL = 1, n = 1061), and both mobility and self-care disabilities (ADL = 2, n = 367). Weighted mean of baseline mental distress scores (PHQ4), psychological risk factors (loneliness, stress, perceived COVID risk), resilience, and coping were compared among these groups. Random effects models were employed to assess the effects of disability and disability-moderated effects of risk factors on mental distress.
Results
At baseline, mental distress increased with greater ADL disabilities (Mean[95%CI] = 1.88[1.77, 1.98], 2.54[2.29, 2.79], and 3.55[3.01, 4.08] for ADL = 0, 1, and 2, respectively, p < .0001). Loneliness, stress, and perceived risk increased with ADL disabilities, but resilience and social coping decreased with it (p's < 0.0001). In the random-effects models, greater ADL disabilities, higher psychological risks, and use of cannabis and other recreational drugs were associated with greater mental distress. Greater ADL disabilities augmented the detrimental effects of risk factors on mental health, but resilience protected mental health both independently and through a buffering effect on its risk factors across all groups.
Conclusion
Individuals with mobility and/or self-care disability tend to have poorer mental health and are differentially more affected by its risk factors. Mental health professionals should address these modifiable factors in interventions.
Keywords: Disability, ADL, Mobility, Self-care, Mental health, Resilience, Adversity, COVID-19 pandemic
More than one billion people are living with disabilities worldwide.1 In the US, one in every four noninstitutionalized adults reported some kind of disability.2 These individuals may be disproportionately affected by the COVID-19 pandemic due to their elevated risks of morbidity and mortality, access barriers to health care, greater unmet health needs, and discriminatory laws and stigma.1 They tend to have multiple comorbidities and live in congregate settings, both of which may increase their risk of infection.3, 4, 5 In addition, the lockdowns, social distancing, and self-isolation may have created major obstacles for these individuals to receive routine health care and instrumental support critical for their daily living. For instance, self-isolation is not practical for individuals who rely on caregivers in daily life. Interruptions and discontinuation of physical therapies for people in need of rehabilitation are likely to cause functional declines in these individuals.6 People with physical disabilities reported cessation of home-based physiotherapy, lack of access to hospital care and medications, and change in usual care, in addition to restrictions to acquisition of goods and services and transportation for daily activities during the pandemic.7 Those infected with COVID may experience disabling post-COVID effects, such as their newly acquired disabilities due to inadequate health care, organ damage, or mental disorder induced by COVID infection.6
The COVID-19 pandemic has led to elevated psychological distress worldwide.8 , 9 The mental health is exacerbated by necessary containment measures such as physical distancing, self-isolation, and social and economic factors, especially for those with limited access to economic and social resources.10 Individuals with disability were at an increased risk of social isolation and loneliness, and this was magnified during the pandemic when social restrictions were implemented and social support was diminished as a result.10 , 11 This may cause long-term detrimental health effects. For example, changes have been observed in emotional responses, behavioral disturbances, mood swings, and sleep problems among those with physical disabilities during the pandemic.7 In addition, people with disability may be advised to implement stricter social distancing guidelines since they often have other chronic health conditions and are at greater risk for infections and complications. Those who rely on a caregiver for assistance with daily living activities are more likely to become a victim of abuse due to less availability of backup caregivers as a consequence of social distancing and quarantine rules and lack of a reliable (in-person) private channel to report these cases during the pandemic.12 Interpersonal violence is also linked to an array of mental illnesses including depression and posttraumatic symptoms.13 , 14
Individuals with high resilience tend to use adaptive coping skills and thus fare better on mental health in the pandemic. Resilience refers to positive adaption in the face of significant adversity.15 Resilience level in a US sample declined significantly during the pandemic compared to data reported before the pandemic.16 Those with lower resilience reported most significant increase in mental distress.17 Nearly half of individuals living with disability had depression symptoms and generalized anxiety disorder symptoms in Ethiopia in face of the pandemic, and a similar proportion (47%) were low resilient copers to their psychopathology.18 Similar research is needed in other regions of the world. In addition to the direct mental health benefit, resilience also buffered the adverse effect of stress on depression.19 A study of family members of individuals with special educational needs and disability reported that those with higher levels of resilience and meaning in life experienced less anxiety during the COVID-19 pandemic.20 These family members may have activated resilient coping strategies to maintain their mental health.
In terms of coping, it has been shown that adaptive coping style, characterized by behavioral responses that minimize the physical, psychological or social harm of a situation,21 was also shown to be protective against psychotic symptomatology in a Chinese sample during the pandemic.22 Passive coping (i.e., helplessness, avoidance, or blaming), in contrast, was associated with psychopathology. Individuals with disabilities reported using substance and alcohol to cope with distress and anxiety before the pandemic, and such tendency may be exacerbated during the pandemic when routine health care needs, especially for mental health, were less likely to be met.
Although multiple vulnerabilities, such as racial and ethnic minorities and older adults, have been revealed to be associated with COVID infection risk, little has been reported on the pandemic impacts on people living with disabilities.3 Thus disability, as a critical demographic identifier, should be incorporated into data collection to monitor the COVID-19 outbreak.3
People with impairment in activities of daily living (ADL) functions such as walking, bathing and dressing oneself, are more likely to experience the negative impacts of the pandemic due to their greater needs for ADL support and/or specialized health care, whereas such support and care can be dramatically diminished due to the lockdown and social distancing rules. These obstacles are likely to cause enormous damage on their daily living, preventive care, and mental and physical health. Greater ADL impairment was found to be associated with increased risk for mortality,23 hospitalization,24 use of long-term care facilities,25 chronic conditions,26 underuse of recommended care,27 and poorer mental health.28 With regards to coping, individuals with mobility impairment were also less likely to use problem-focused coping.29
The mental health state, associated risk factors, resilience and coping strategies among individuals with disabilities during the COVID-19 pandemic have not been adequately studied, yet such research is urgently needed. In this study, we aimed to examine the effects of perceived adversities, resilience, and coping behaviors on the mental health of those living with either or both types of ADL disabilities, mobility impairment and self-care disability (i.e., difficulty in bathing and dressing), as compared to those without such ADL limitations. Subsequently, we would assess the buffering effect of resilience on mental health as modified by ADL status. This work will address the following research questions: 1) To what extent the disparities in perceived adversities, resilience, and coping exist among individuals with mobility and/or self-care disabilities as compared to those without these ADL disabilities? 2) Does ADL status modify the buffering effect of resilience on mental health?
Methods
Data source
Data were drawn from the Understanding America Study (UAS) on the COVID-19 pandemic.30 It is an online panel survey administered to a nationally representative sample. The UAS consists of American households with respondents aged 18 and above. The survey was launched in March 2020 and had been on-going up to January 2021 when data were collected. Respondents were assessed every two weeks, and thus including 18 waves of data collection. The core COVID-19 survey includes a wide range of questions, such as personal experiences with COVID-19, risk perception, preventive behavior endorsement, attitudes toward COVID-19 vaccines, coping behaviors, and mental health.
Since physical functional status were assessed only at wave 4 (April 2020), this wave was used as the baseline. The end of the follow up was cut off at wave 21 (January 2021). The number of unique individuals included at baseline was n = 6403.
Outcome variable
Mental distress was assessed by the 4-item Patient Health Questionnaire (PHQ4)31: Over the past fourteen days, how often have you been bothered by any of the following problems? 1) Feeling nervous, anxious, or on edge; 2) Not being able to stop or control worrying; 3) Feeling down, depressed, or hopeless; 4) Little interest or pleasure in doing things. Each response was a 4-point Likert scale (0–3): not at all, several days, more than half the days, nearly every day. The Cronbach alpha for this construct was 0.91. Mental distress was measured by the sum (0-12) of these items. PHQ4 reliability was previously reported as 0.8531 and .90.32
Main independent variable
Physical functions were assessed with the EQ-5D-5L instrument,33 only for April 2020 (wave 4). Mobility disability was dichotomized into “No” (I have no problems walking) vs. “Yes” (I have slight/moderate/severe problems walking or I am not able to walk). Self-care disability was dichotomized as “No” (I have no problems washing or dressing myself) vs. “Yes” (I have slight/moderate/severe problems washing or dressing myself or I am not able to wash or dress myself). Disability status was initially categorized at baseline as no mobility or self-care disability (None), n = 4975; having mobility disability only (M), n = 1023; having self-care disability only (SC), n = 38; mobility and self-care disabilities (Both), n = 367. Because of the very small number of individuals with self-care disability only, categories M and SC were combined into either mobility or self-care disability, but not both, with n = 1061. Another way to express the categorization was by the count of ADL disabilities: ADL = 0 (None), ADL = 1 (M or SC), and ADL = 2 (M and SC). Both expressions were used interchangeably in this study.
Covariates – perceived adversities
Perceived stress was measured by Perceived Stress Scale (PSS4).34 Respondents were asked in the past 14 days, how often they felt 1) unable to control the important things in your life; 2) confident about your ability to handle your personal problems; 3) that things were going their way; and 4) difficulties were piling up so high that they could not overcome them. Responses were 5-point Likert scale: never, almost never, sometimes, fairly often, very often. Responses were reverse coded when appropriate so that higher score indicated greater stress. The Cronbach alpha for this construct was 0.65. Perceived stress was measured by the sum (range 4–20) of these four items. The reliability alpha of this scale was previously reported as 0.6035 and 0.75.36
Loneliness was measured by a single item: In the past 7 days, how often have you felt lonely? The responses were: not at all or less than 1 day, 1–2 days, 3–4 days, 5–7 days. This variable was treated as continuous (range 1–4).
Perceived COVID risk was assessed by perceived risk of death from COVID-19, hospitalization from COVID-19, contracting COVID-19, and risk of running out of money in the next 3 months. The respondents rated each risk on a 0%–100% scale. An exploratory factor analysis was done on the four items and yielded a single factor, with Cronbach alpha at 0.72. The total risk was calculated as the average of these risks multiplied by 0.1, to keep its scale comparable to other independent variables.
Covariates – moderators
Resilience was assessed with the Brief Resilience Scale (BRS)37 of six questions: 1) I tend to bounce back quickly after hard times; 2) I have a hard time making it through stressful events; 3) It does not take me long to recover from a stressful event; 4) It is hard for me to snap back when something bad happens; 5) I usually come through difficult times with little trouble; 6) I tend to take a long time to get over set-backs in my life. The responses were each a 5-point Likert scale: strongly disagree, disagree, neutral, agree, strongly agree. The Cronbach alpha of this scale was 0.86. Resilience was taken as the sum of the six items (range 6–30). The reliability of resilience scale was previously reported as 0.80–0.91.37 , 38
Coping behaviors were derived from an original 13 behaviors. For each behavior, respondents were asked, “Out of the past 7 days, what is your best estimate of the number of days that you did each of the following activities?” These behaviors include drank alcohol, used cannabis products such as marijuana, used recreational drugs other than alcohol or cannabis products, used an e-cigarette or vaping device to vape e-liquids with nicotine, smoked all or part of a cigarette, meditated, got extra exercise, made time to relax, connected socially with friends or family (either online or in person), spent time posting or browsing on Facebook, Twitter, Instagram, or Snapchat, had a phone call or video call with a family member or a friend, messaged or emailed with a family member or friend, spent time interacting with a family member or friend in person. Responses ranged from 0 to 7. A principal component analysis with Promax rotation yielded 4 components: social coping, alcohol coping, substance (non-alcohol) use, and relaxation. Cronbach alpha for social coping was 0.7 but was <0.5 for substance use and relaxation. Given the low reliability of substance use and relaxation, we chose three single items for modeling: 1) made time to relax, 2) used cannabis products, and 3) used recreational drugs other than alcohol or cannabis products. The construct social coping took the mean of related items (range 0–7). The three single items took the original measure (range 0–7). With additional assessment of alcohol intake in the survey, alcohol coping was modified as the product of number of days of alcohol consumption in the past 7 days and average amount of consumption each day (range 0–210).
Demographic covariates/confounders
Demographic covariates were assessed at baseline, including age, gender, education (range 1–16), household income (range 1–16), race/ethnicity (Non-Hispanic Whites, Non-Hispanic blacks, Hispanics, Native Americans, Asians and Pacific Islanders, Non-Hispanic mixed race), chronic health condition including asthma, autoimmune disorder, COPD, diabetes, non-skin cancer, heart disease, high blood pressure, kidney disease, mental health condition, and obesity.
Statistical analysis
The weighted mean and standard error of the mental distress outcome, three adversity variables, resilience, and four coping strategies were assessed at baseline and plotted over time for each disability group. The correlations between adversity variables and coping variables were assessed at baseline. Hierarchical random-effects model (random intercept) was employed to assess the theoretical effects of disability and covariates on mental health. The sandwich estimator was implemented to generate robust standard errors and protect against error covariance misspecification and subsequent inaccurate inferences about the fixed effects due to an inflation of type-I error.39 We specified an unstructured error variance-covariance matrix and Gauss-Hermite quadrature algorithm. Model 0 included only sociodemographics, clinical characteristics, and survey waves. Model 1 added disability status upon model 0. Model 2 further added perceived stress, loneliness, perceived risk, resilience and coping variables (alcohol, cannabis, other recreational drugs, social coping, relaxation) as independent variables. Model 3 further added the interaction effects of ADL status with each adversity and coping variable as two-way interactions. Two sets of three-way interactions were added 1) ADL status, resilience, and each adversity variable; 2) ADL status, resilience and each coping variable. To keep the model parsimonious, only significant interaction effects were included in the final model (Model 3). The attrition of the sample over the observation period (18 waves) was around 13% (down from n = 6403 in wave 4 to n = 5303 in wave 21). The analyses were based on complete cases on all variables in any wave. The average number of waves per person by ADL status included in the analyses was similar, 15.6, 16.1 and 16.2 waves per person for ADL as 0, 1, and 2, respectively. All analyses incorporated survey weights and accounted for within-person correlations across survey waves when appropriate. All analyses were done in SAS 9.4.
Results
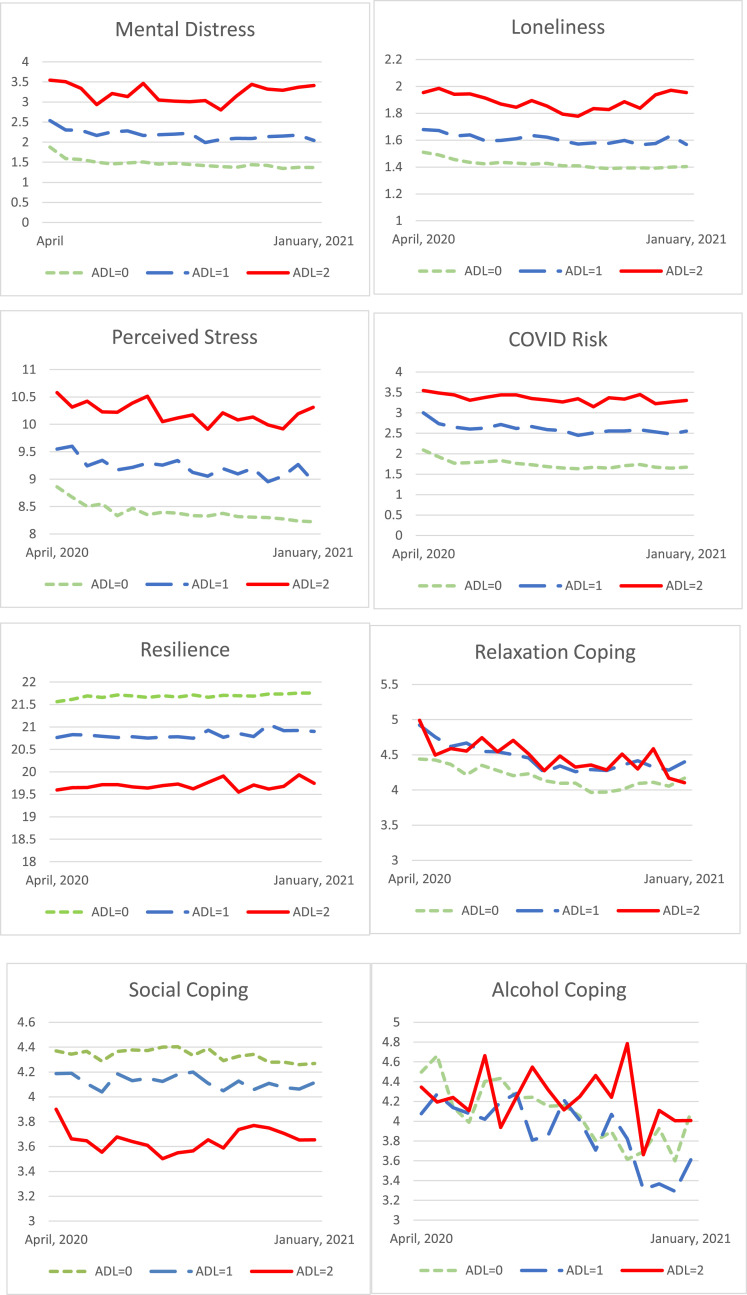
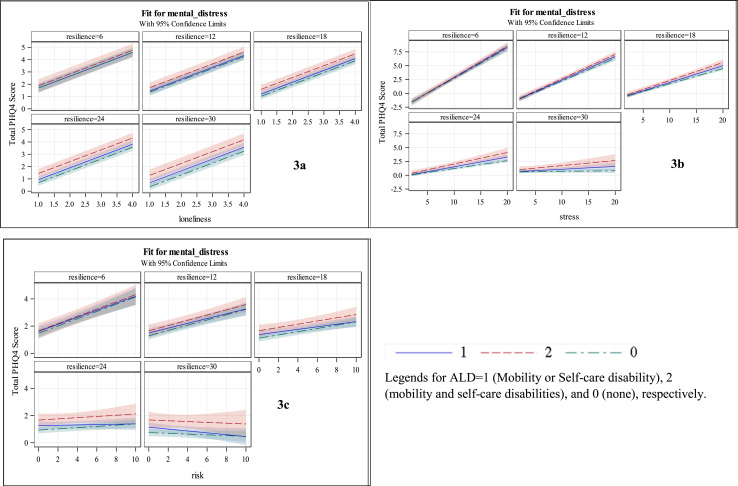
At baseline, as shown in Table 1 , mental distress increased with greater ADL disability. The mental distress (mean and 95% CI) was 1.88 (1.77, 1.98), 2.54 (2.29, 2.79), and 3.55 (3.01, 4.08), p < .0001 for no mobility or self-care disability (ADL = 0), mobility or self-care disability only (ADL = 1), and both mobility and self-care disabilities (ADL = 2), respectively. Similarly, each adversity, including perceived stress, loneliness, and perceived COVID risk, also increased with greater ADL impairment (all p's < 0.0001). For instance, the mean (95% CI) of perceived stress was 8.86 (8.74, 8.98), 9.55 (9.30, 9.79), 10.58 (10.14, 11.02) for 0, 1, and 2 ADL disabilities, respectively. Resilience decreased with greater ADL limitation (p < .0001), with the mean (95% CI) as 21.56 (21.39, 21.74), 20.77 (20.39, 21.14), 19.59 (18.96, 20.23) for 0, 1, and 2 ADL disabilities. Social coping decreased with greater ADL limitation, but use of cannabis increased with ADL impairment. These patterns persisted over time during the pandemic, as shown in Fig. 1 .
Table 1.
Mental distress, adversities, resilience, and coping by disability status at baseline.
| Variables | Total N = 6363 Mean (95%CI) |
ADL = 0 N = 4973 Mean (95% CI) |
ADL = 1 N = 1061 Mean (95% CI) |
ADL = 2 N = 329 Mean (95% CI) |
P value |
|---|---|---|---|---|---|
| Mental distress (PHQ4) | 2.07 (1.97, 2.17) | 1.88 (1.77, 1.98) | 2.54 (2.29, 2.79) | 3.55 (3.01, 4.08) | <.0001 |
| Perceived stress (PSS4) | 9.06 (8.96, 9.17) | 8.86 (8.74, 8.98) | 9.55 (9.30, 9.79) | 10.58 (10.14, 11.02) | <.0001 |
| Loneliness | 1.56 (1.53, 1.59) | 1.51 (1.48, 1.54) | 1.68 (1.60, 1.76) | 1.95 (1.79, 2.12) | <.0001 |
| Perceived Risk | 2.32 (2.25, 2.38) | 2.09 (2.02, 2.16) | 3.00 (2.84, 3.16) | 3.55 (3.22, 3.87) | <.0001 |
| Resilience | 21.33 (21.17, 21.48) | 21.56 (21.39, 21.74) | 20.77 (20.39, 21.14) | 19.59 (18.96, 20.23) | <.0001 |
| Relaxation Coping | 4.55 (4.46, 4.63) | 4.44 (4.34, 4.54) | 4.92 (4.72, 5.12) | 4.99 (4.65, 5.33) | <.0001 |
| Social Coping | 4.32 (4.25, 4.38) | 4.37 (4.30, 4.44) | 4.19 (4.05, 4.33) | 3.90 (3.61, 4.19) | <.0001 |
| Alcohol Coping | 4.42 (4.04, 4.80) | 4.50 (4.06, 4.94) | 4.08 (3.20, 4.95) | 4.34 (2.81, 5.88) | <.5157 |
| Cannabis Use | 0.60 (0.54, 0.66) | 0.53 (0.46, 0.6) | 0.79 (0.61, 0.97) | 1.10 (0.75, 1.46) | <.0001 |
| Other Recreational Drug Use | 0.18 (0.15, 0.21) | 0.17 (0.13, 0.21) | 0.19 (0.12, 0.27) | 0.25 (0.1, 0.4) | 0.3091 |
Note. ADL = 0 no mobility or selfcare disability; ADL = 1 mobility or selfcare disability; ADL = 2 both mobility and selfcare disabilities.
Fig. 1.
Mental Distress, Perceived adversities, Resilience and Coping Over Time (April 2020 to January 2021) by ADL Disability Status at Baseline.
In terms of sociodemographics, as shown in Table 2 , compared to no ADL disability, those with only one or both disabilities were older (mean age (95% CI) = 45.9 (45.3, 46.6), 57.7 (56.4, 59.0), 58.1 (55.6, 60.6), p < .0001), had lower education and income, were more likely to have a chronic condition (all p's < 0.0001; including diabetes, non-skin cancer, heart disease, high blood pressure, asthma COPD, kidney disease, autoimmune disorder, mental health condition, and obesity).
Table 2.
Sociodemographics and clinical characteristics by disability status at baseline.
| Variable | Class | Total | Disability Type |
P-value | ||
|---|---|---|---|---|---|---|
| ADL = 0 n = 4975 | ADL = 1 n = 1061 | ADL = 2 n = 329 | ||||
| Gender | Female | 3718 (51.8) | 2883 (51.4) | 640 (53.7) | 195 (51.4) | 0.5518 |
| Male | 2647 (48.2) | 2092 (48.6) | 421 (46.3) | 134 (48.6) | ||
| Race/ethnicity | White | 4244 (62.9) | 3213 (60.5) | 792 (73.3) | 239 (66.4) | <.0001 |
| Black | 480 (11.9) | 369 (11.9) | 81 (11.1) | 30 (15.0) | ||
| Hispanic | 983 (16.5) | 845 (18.2) | 103 (10.3) | 35 (11.4) | ||
| Native | 53 (0.4) | 34 (0.3) | 14 (0.5) | 5 (1.2) | ||
| Asian/AAPI | 341 (5.3) | 304 (5.9) | 30 (2.6) | 7 (4.1) | ||
| Mixed | 255 (3.0) | 202 (3.2) | 41 (2.2) | 12 (1.9) | ||
| Age | Mean 95%CI | 48.5 (47.9, 49.0) | 45.9 (45.3, 46.6) | 57.7 (56.4, 59.0) | 58.1 (55.6, 60.6) | <.0001 |
| Education | Mean 95%CI | 10.8 (10.7, 10.9) | 11.0 (10.9, 11.1) | 10.10 (9.9, 10.3) | 9.6 (9.2, 9.9) | <.0001 |
| Income | Mean 95%CI | 10.9 (10.8, 11.1) | 11.4 (11.2, 11.6) | 9.5 (9.1, 9.8) | 8.7 (8.1, 9.3) | <.0001 |
| Asthma | yes | 731 (11.7) | 496 (10.2) | 169 (16.0) | 66 (19.8) | <.0001 |
| Autoimmune disorder | yes | 387 (5.5) | 202 (3.7) | 120 (10.9) | 65 (15.7) | <.0001 |
| Cancer (other than skin) | yes | 448 (5.9) | 275 (4.4) | 129 (11.5) | 44 (11.0) | <.0001 |
| COPD | yes | 256 (4.3) | 82 (1.7) | 111 (12.1) | 63 (18.8) | <.0001 |
| Diabetes | yes | 771 (12.3) | 417 (8.5) | 256 (24.2) | 98 (32.4) | <.0001 |
| Heart disease | yes | 416 (6.5) | 195 (3.9) | 154 (14.3) | 67 (20.3) | <.0001 |
| High blood pressure | yes | 2024 (31.6) | 1261 (24.7) | 567 (54.5) | 196 (62.3) | <.0001 |
| Kidney disease | yes | 169 (2.7) | 75 (1.6) | 65 (5.8) | 29 (8.6) | <.0001 |
| Mental health condition | yes | 707 (10.9) | 463 (8.9) | 164 (15.9) | 80 (24.6) | <.0001 |
| Obesity | yes | 1139 (16.6) | 675 (12.7) | 342 (30.2) | 122 (32.9) | <.0001 |
Note. ADL = 0 no mobility or selfcare disability; ADL = 1 mobility or selfcare disability; ADL = 2 both mobility and selfcare disabilities. For categorical variables, table cell values are raw counts and weighted % in the parentheses, and p values are derived from the Pearson chi-square test; for comparison of continuous variables, table cell values are weighted mean and 95% confidence interval, and p values are derived from the ANOVA test.
Table 3 shows the correlations between adversities, resilience, and coping variables. Most correlations were significantly different from 0. Three adversities were weakly to moderately correlated with each other in the positive direction. Resilience inversely and moderately correlated with loneliness (r = −0.40, p < .0001) and perceived stress (r = −0.56, p < .0001). Coping and three adversities were all weakly correlated, with few exceptions. Resilience negatively correlated with cannabis use (r = -0.08, p < .0001) and use of other recreational drugs (r = -0.07, p < .0001), but positively correlated with alcohol (r = 0.05, p < .0001), social (r = 0.09, p < .0001) and relaxation coping (r = 0.15, p < .0001). Social and relaxation coping were positively correlated with each other (r = 0.27, p < .0001).
Table 3.
Correlations and p values of adversities and coping covariates at baseline.
| Mental distress | Loneliness | Stress | Risk | Resilience | Relaxation | Social coping | Alcohol coping | Cannabis use | Use other recreational drugs | |
|---|---|---|---|---|---|---|---|---|---|---|
| Mental distress | 1 | |||||||||
| Loneliness |
0.56 <.0001 |
1 | ||||||||
| Stress |
0.59 <.0001 |
0.46 <.0001 |
1 | |||||||
| Risk |
0.22 <.0001 |
0.17 <.0001 |
0.24 <.0001 |
1 | ||||||
| Resilience |
−0.48 <.0001 |
−0.40 <.0001 |
−0.56 <.0001 |
−0.20 <.0001 |
1 | |||||
| Relaxation |
−0.12 <.0001 |
−0.07 <.0001 |
−0.21 <.0001 |
−0.01 (n.s.) |
0.15 <.0001 |
1 | ||||
| Social coping | 0.02 (n.s.) | 0.01 (n.s.) |
−0.07 <.0001 |
−0.06 <.0001 |
0.09 <.0001 |
0.27 <.0001 |
1 | |||
| Alcohol coping | 0.02 (n.s.) | 0.004 (n.s.) | −0.02 (n.s.) |
−0.03 0.006 |
0.05 <.0001 |
0.07 <.0001 |
0.03 0.017 |
1 | ||
| Cannabis use |
0.13 <.0001 |
0.09 <.0001 |
0.09 <.0001 |
0.10 <.0001 |
−0.08 <.0001 |
0.05 <.0001 |
0.06 <.0001 |
0.11 <.0001 |
1 | |
| Use other recreational Drugs |
0.11 <.0001 |
0.10 <.0001 |
0.08 <.0001 |
0.07 <.0001 |
−0.07 <.0001 |
0.01 (n.s.) | 0.02 (n.s.) |
0.15 <.0001 |
0.34 <.0001 |
1 |
Note. ADL = 0 no mobility or selfcare disability; ADL = 1 mobility or selfcare disability; ADL = 2 both mobility and selfcare disabilities. In each cell, the Pearson correlation coefficient is listed in the top row, with its p value listed in the second row. n.s. refers to not significant p > .05.
Table 4 shows the results of three hierarchical random-intercept models (Models 1, 2, and 3). Results of model 0 with only sociodemographic and clinical variables and survey waves as predictors are shown in the appendix Table 1. The random effects (variances) of the intercept and individual residual for each of these four models were significant (all p's < 0.0001). As shown in Model 0, younger age, female, lower income, and having chronic conditions such as high blood pressure, autoimmune diseases, mental disorder, and obesity, all increased mental distress during the pandemic. In Model 1, after adjusting for survey waves, socidemographics, and clinical conditions, ADL disability had a monotonic effect on mental distress, with the increase in β (standard error, SE) in mental distress as 0.70 (0.12) for mobility or self-care disability only (ADL = 1), and 1.64 (0.23) for both mobility and self-care disabilities (ADL = 2), as compared to those without such limitations (p's < 0.0001). In Model 2, adversities and coping variables were added and the ADL disability effect remained to be significant (p's < 0.0001), with the increase in mental distress as 0.30 (0.08) for those with one ADL disability, and 0.79 (0.15) for those with both. Resilience [β (SE) = −0.10 (0.01), p < .0001)] and relaxation (β (SE): -0.02 (0.01), p = .0017) both predicted lower mental distress; whereas loneliness, stress and perceived risk all predicted higher mental distress [β (SE) = 0.98 (0.03), 0.20 (0.01), and 0.08 (0.01) respectively, p's < 0.0001]. Social coping and cannabis use and use of other recreational drugs were all related to higher mental distress [β (SE) = 0.04 (0.01), p < .0001; .05 (0.01), p = .0001; 0.06 (0.02), p = .0002, respectively). Model 3 added interaction effects and revealed three significant three-way interactions: 1) ADL, resilience, and stress; 2) ADL, resilience, and risk; 3) ADL, resilience, and social coping. Model fit index Bayesian information criterion (BIC) became smaller as the model became more complex. For the final Model 3, the BIC was the smallest at 342399.3, indicating best model fit.
Table 4.
Associations of covariates with mental distress derived from hierarchical random-effects models.
| Variable | Class | Model 1 |
Model 2 |
Model 3 |
|||
|---|---|---|---|---|---|---|---|
| Fixed Effects B (SE) | P | Fixed Effects B (SE) | P | Fixed Effects B (SE) | P | ||
| Intercept | 3.42 (0.25) | <.0001 | 0.17 (0.24) | 0.4837 | −7.01 (0.42) | <.0001 | |
| ADL | ADL = 0 | 0 | 0 | 0 | |||
| ADL = 1 | 0.70 (0.12) | <.0001 | 0.30 (0.08) | <.0001 | 0.10 (0.17) | 0.5587 | |
| ADL = 2 | 1.64 (0.23) | <.0001 | 0.79 (0.15) | <.0001 | 0.03 (0.32) | 0.9299 | |
| Loneliness | 0.98 (0.03) | <.0001 | 0.95 (0.03) | <.0001 | |||
| Stress | 0.20 (0.01) | <.0001 | 0.66 (0.03) | <.0001 | |||
| Risk | 0.08 (0.01) | <.0001 | 0.31 (0.05) | <.0001 | |||
| Resilience | −0.10 (0.01) | <.0001 | 0.19 (0.02) | <.0001 | |||
| Relaxation Coping | −0.02 (0.01) | 0.0017 | −0.02 (0.01) | 0.0023 | |||
| Social Coping | 0.04 (0.01) | <.0001 | 0.24 (0.05) | <.0001 | |||
| Alcohol Coping | 0.002 (0.001) | 0.0625 | 0.002 (0.001) | 0.0943 | |||
| Cannabis Coping | 0.05 (0.01) | 0.0001 | 0.05 (0.01) | <.0001 | |||
| Other Drugs Coping | 0.06 (0.02) | 0.0002 | 0.06 (0.02) | 0.0003 | |||
| Stress∗ADL∗resilience | ADL = 0 | −0.02 (0.001) | <.0001 | ||||
| ADL = 1 | −0.02 (0.002) | <.0001 | |||||
| ADL = 2 | −0.02 (0.002) | <.0001 | |||||
| Risk∗ADL∗resilience | ADL = 0 | −0.01 (0.002) | <.0001 | ||||
| ADL = 1 | −0.01 (0.002) | <.0001 | |||||
| ADL = 2 | −0.01 (0.003) | .0003 | |||||
| Social Coping ∗ADL∗resilience |
ADL = 0 | −0.01 (0.002) | <.0001 | ||||
| ADL = 1 | −0.01 (0.002) | <.0001 | |||||
| ADL = 2 |
−0.01 (0.003) |
0.0118 |
|||||
| Random Effects Variance (SE) |
Random Effects Var (SE) |
Random Effects Var (SE) |
|||||
| Intercept | 2.12 (0.04) | 1.33 (0.03) | 1.27 (0.03) | ||||
| Residual | 2.11 (0.07) | 1.77 (0.06) | 1.75 (0.06) | ||||
| Model Fit | AIC | 365582.4 | 343323.3 | 342001.2 | |||
| BIC | 365859.1 | 343660.6 | 342399.3 | ||||
Note. SE stands for standard error. AIC = Akaike Information Criterion; BIC=Bayesian Information Criteria. Models incorporated survey weights and sandwich estimator for standard errors. All p values for intercept variances were <0.0001. All models were adjusted for survey waves, age, gender, education, income, race/ethnicity, chronic conditions including diabetes, cancer, High blood pressure, heart conditions, asthma, COPD, kidney disease, autoimmune diseases, mental disorder, and obesity.
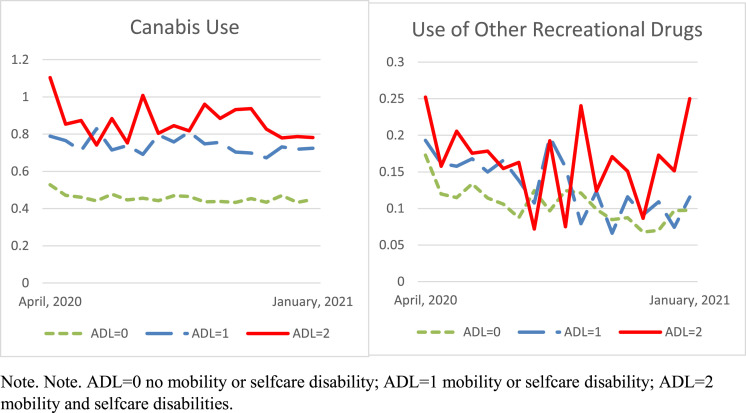
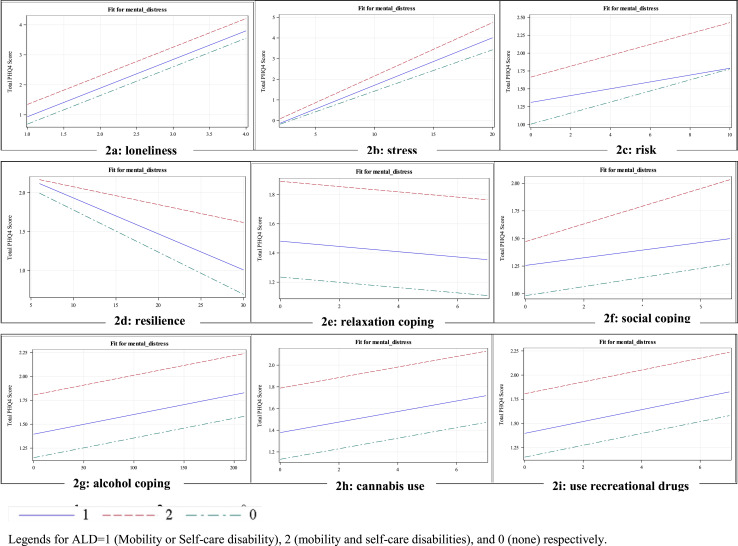
Fig. 2 series display the fixed effect of each adversity on mental distress, as moderated by ADL disability status if there was a significant interaction effect. For significant interactions, the estimated slopes for Fig. 2 series are listed in Appendix Table 2. The slopes without interaction effects can be found in Model 3 from Table 3. First of all, the two groups with ADL disabilities showed larger fixed intercepts in all graphs, suggesting greater average mental distress for the two groups with ADL disability when coping or adversity is at the lowest point. Resilience and ADL disability moderated the effect of stress, risk, and social coping on mental distress, respectively. In terms of the slope, ADL disabilities elevated the effect of perceived stress on mental distress (steeper slopes, Fig. 2b), with estimated slope B(SE) as 0.20 (0.01), 0.23 (0.02), 0.26 (0.03), for ADL = 0, 1, and 2, respectively, all p's < 0.0001. A flatter downward slope of resilience on mental distress was observed for the greatest ADL impairment with estimated B(SE) as −0.07 (0.01) p < .0001, −0.07 (0.01) p < .0001, −0.04 (0.02) p = .0102, for ADL = 0, 1, and 2 respectively; thus we could interpret that resilience had a stronger protective effect for those with none or only 1 ADL disability compared to those with greatest ADL impairment, as shown in Fig. 2d. The effects of social coping were not significant for the two groups with ADL impairment, but for those without ADL impairment, there was a positive effect of social coping on mental distress B(SE) = 0.04 (0.01), p < .0001. Relaxation coping, alcohol consumption, cannabis use, and use of other recreational drugs showed the same slope estimates on mental distress across ADL status (no interaction effects). Fig. 3 series display the effect of three adversity variables, loneliness, stress, and risk, on mental distress, as moderated by ADL disability status and resilience level. Both graphs of stress and risk convincingly show that resilience mitigated the negative effects of stress and perceived risk on mental distress for all ADL status, as indicated by gradually flattened slopes and/or decreased average (fixed) intercepts. interestingly, although resilience and ADL status did not change the slope of loneliness on mental distress (B(SE) = 0.95(0.03), p < .0001 for all ADL groups), with increasing resilience, the fixed intercept went down thus bring down the overall mental distress. The estimated slopes for stress and risk are listed in Appendix Table 3.
Fig. 2.
Series. Fixed effects of adversities, resilience and coping on mental distress.
Fig. 3.
Series. Buffering Effect of Resilience on the Association of Adversities (loneliness – 3a, perceived stress –3b, perceived COVID risk –3c) and mental distress.
Discussion
In this study we identified that individuals with greater ADL disabilities reported greater mental distress and greater perceived adversities (e.g., loneliness, perceived stress and COVID risk). However, they reported lower resilience, and adopted less social coping but greater substance use. These patterns persisted longitudinally. Even after adjusting for sociodemographics, clinical characteristics, survey waves, adversities, and coping, ADL disability still demonstrated independent effect on mental distress, suggesting ADL disability is a critical mental health risk factor. Resilience was found to be moderately and negatively correlated with perceived stress and loneliness, and it had a buffering effect of perceived adversities on mental distress. Those with greater ADL disability benefited less due to their reduced resilience.
During the unprecedented COVID-19 pandemic, a significant proportion of individuals living with disabilities experienced psychopathologies, such as depression, anxiety, insomnia, post-traumatic syndromes.18 , 40 , 41 The psychological outcomes revealed in our study were consistent with previously reported findings: individuals with ADL disabilities reported heightened mental distress in a persistent manner and showed a monotonic increase in mental distress with greater ADL disabilities.
Our study further quantified the resilience of individuals with ADL disabilities in a national sample and compared the resilience level among multiple groups with different degrees of ADL disabilities over time. Protective factors of resilience during the pandemic were identified as outdoor activities, exercise, social support, better sleep quality, and prayer.16 Our study found that the perceived adversities were negatively correlated with resilience, suggesting that highly resilient individuals may perceive lower levels of adversities, which in turn protected them form experiencing mental distress. The significant three-way interactions between resilience, adversities (stress and risk), and ADL status confirmed that resilience was shown not only as a protective factor but also a buffer between adversities and mental distress, even though the degree of protection varied by disability status.
Although our study found that self-reported resilience was lower among individuals with higher ADL disabilities and the protective effect of resilience on those with greatest ADL impairment (ADL = 2) was lower than others, resilience may be expressed differently in individuals with disabilities. Indeed, how and whether individuals are able to express resilience is determined by the resources available to them, including access to material resources, relationships, identity, power and control, cultural adherence, social justice and cohesion.42 Thus an exploration of resilience in individuals with disabilities should also include what resources are available and who is accessing those resources.43 Building resilience in the lives of people living with disabilities goes beyond building individual capacity or family support; it must also be a case of challenging social, attitudinal and structural barriers which increase adversity in the lives of people with disabilities.44 Future research may explore these contextual factors and how they affect the people living with disability.
Adaptive coping strategies are associated with subjective well-being, self-esteem and acceptance of disability.45 Adaptive coping during the COVID 19 pandemic may be more challenging for people with disabilities.38 Stress related to COVID19 was associated with passive coping, such as denial and substance use among individuals with disabilities and chronic conditions, and active coping was associated with subjective well-being38 Individuals with disabilities may be prone to the passive coping strategies.
A study reported that COVID-19 adversities were associated with less socially supported coping strategies,46 which corresponds to our finding that social coping increased mental stress during the pandemic among those without ADL disability, potentially due to the nature of the virus that requires social isolation to curb its spread. Avoidance coping, characterized by avoiding the stressor and reducing reaction to the stressors, has been considered maladaptive considering its link to depression symptoms and high-stress level and maladaptive behavior patterns.47 , 48 As an avoidance coping strategy, substance use temporarily “lifts up” oneself from the stressful reality, but one inevitably finds oneself falling back into it. Our study shows those with ADL disabilities tended to use cannabis more frequently than those without. Although there was no significant interaction between ADL disability and use of substances (alcohol, cannabis, and other recreational drugs), use of these substances increased level of psychological distress in all groups. Relaxation showed protective effect against mental distress, although such effect did not differ among ADL disability groups. Taken together, our results suggested that those with ADL disabilities were more likely to engage in maladaptive coping, which also rendered larger detrimental effect on their mental health.
People living with ADL disabilities, such as mobility impairment, were reported to have poorer mental health,28 adopt less problem-focused coping,29 be less likely to use recommended care services,27 all of which may contribute to greater deterioration of mental and physical health during the pandemic when routine medical resources and personal support often became unavailable due to the lockdown measures and social distancing rules. Furthermore, individuals living with disabilities may be at greater risk of mortality and morbidity once contracting the virus.6 Due to their need of daily care, it is impossible for a person with ADL disabilities to self-isolate. Furthermore, those on rehabilitation services to prevent functional decline also face a dilemma due to the service interruptions during the pandemic.6 Despite of the enormous obstacles imposed on individuals with disabilities, research on the response to the pandemic in the disability community is scarce3 and surveillance of COVID-19 outbreak integrating disability as an identifier in its data collection has yet to become the standard practice.3 Thus it is critical to explore the psychological and mental experiences and coping of individuals with disabilities when such data are available to researchers. Our results will help policy makers and health care practitioners target intervention strategies and reduce ableism and related stereotypes and discrimination for the disability communities.
Our study used timely reported data on mental health needs among people with ADL disabilities during the pandemic from a nationally representative sample. The longitudinal data described the individual subjective experiences over time and showed persistent patterns of disparities in mental health, perceived adversities, resilience, and coping skills among those with living ADL disabilities.
This study has several limitations. Missing data were not included in our analyses. Mortality data were not available, thus those with severe ADL disabilities and worst mental health might not be able to survive the pandemic. Due to limited survey information, other dimensions of ADL disabilities (e.g., difficulty in eating and toileting; transferring from chair/bed) were not included. Additional disabilities such as sensory disability (blindness and deafness) or intellectual disabilities were not assessed. Future research may consider using established standardized instruments for cannabis use, use of other recreational drugs, and relaxation. These concepts were each measured with a single item in the study and can benefit from validated multiple-item measures. Our results were derived from a nationally representative online sample. The sample can be improved by including individuals who were not regularly online and thus less likely to be represented in this sample. Due to the scope of this paper, some important aspects of disparity known to affect morbidity and mortality of individuals with disabilities were not discussed. Future research may explore dimensions including, but not limited to, health care access, treatment needs, and interruption of routine care in the disability community during the pandemic.
Nevertheless, it should be noted that coping strategy could change over time. The results of the current study shed some light on the importance of stress-coping education and intervention to those vulnerable population is crucial and could greatly prevent and even reduce the mental health issues. Specifically, psychological interventions focusing on building resilience and developing positive coping skills can be viable means to ameliorate mental distress among the disability population, especially during a public health crisis such as the COVID-19 pandemic.
Presentation
A preliminary abstract of this work was accepted for presentation at the American Public Health Association Annual Meeting, October 2021.
Conflicts of interest
The authors declare no conflicts of interest. This work was not funded.
Footnotes
Supplementary material to this article can be found online at https://doi.org/10.1016/j.dhjo.2021.101216.
Supplementary material
The following is the Supplementary material to this article:
References
- 1.Armitage R., Nellums L.B. The COVID-19 response must be disability inclusive. The Lancet Public Health. 2020;5(5):e257. doi: 10.1016/S2468-2667(20)30076-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Okoro C.A., Hollis N.D., Cyrus A.C., Griffin-Blake S. Prevalence of disabilities and health care access by disability status and type Among adults — United States, 2016. Morb Mortal Wkly Rep. 2018;67:882–887. doi: 10.15585/mmwr.mm6732a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Boyle C.A., Fox M.H., Havercamp S.M., Zubler J. The public health response to the COVID-19 pandemic for people with disabilities. Disabil Health J. 2020;13(3):100943. doi: 10.1016/j.dhjo.2020.100943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Team C.C.-R., Chow N., Fleming-Dutra K., et al. Preliminary estimates of the prevalence of selected underlying health conditions among patients with coronavirus disease 2019—United States, February 12–March 28, 2020. MMWR (Morb Mortal Wkly Rep) 2020;69(13):382–386. doi: 10.15585/mmwr.mm6913e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kimball A., Hatfield K.M., Arons M., et al. Asymptomatic and presymptomatic SARS-CoV-2 infections in residents of a long-term care skilled nursing facility—King County, Washington, March 2020. MMWR (Morb Mortal Wkly Rep) 2020;69(13):377. doi: 10.15585/mmwr.mm6913e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kuper H., Banks L.M., Bright T., Davey C., Shakespeare T. Disability-inclusive COVID-19 response: what it is, why it is important and what we can learn from the United Kingdom's response. Wellcome Open Res. 2020;5 doi: 10.12688/wellcomeopenres.15833.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lebrasseur A., Fortin-Bédard N., Lettre J., et al. A rapid; 2020. Impact of COVID-19 on People with Physical Disabilities. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kowal M., Coll-Martín T., Ikizer G., et al. Who is the most stressed during the covid-19 pandemic? Data from 26 countries and areas. Appl Psychol: Health Well-Being. 2020;12(4):946–966. doi: 10.1111/aphw.12234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shah S.M.A., Mohammad D., Qureshi M.F.H., Abbas M.Z., Aleem S. Prevalence, Psychological Responses and associated correlates of depression, anxiety and stress in a global population, during the coronavirus disease (COVID-19) pandemic. Community Ment Health J. 2021;57(1):101–110. doi: 10.1007/s10597-020-00728-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lund E.M., Forber-Pratt A.J., Wilson C., Mona L.R. The COVID-19 pandemic, stress, and trauma in the disability community: a call to action. Rehabil Psychol. 2020;65(4):313. doi: 10.1037/rep0000368. [DOI] [PubMed] [Google Scholar]
- 11.Tough H., Siegrist J., Fekete C. Social relationships, mental health and wellbeing in physical disability: a systematic review. BMC Publ Health. 2017;17(1):1–18. doi: 10.1186/s12889-017-4308-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lund E.M. Interpersonal violence against people with disabilities: additional concerns and considerations in the COVID-19 pandemic. Rehabil Psychol. 2020;65(3):199. doi: 10.1037/rep0000347. [DOI] [PubMed] [Google Scholar]
- 13.Coston B.M. Disability, sexual orientation, and the mental health outcomes of intimate partner violence: a comparative study of women in the US. Disabil Health J. 2019;12(2):164–170. doi: 10.1016/j.dhjo.2018.11.002. [DOI] [PubMed] [Google Scholar]
- 14.Hughes R.B., Robinson-Whelen S., Raymaker D., et al. The relation of abuse to physical and psychological health in adults with developmental disabilities. Disabil Health J. 2019;12(2):227–234. doi: 10.1016/j.dhjo.2018.09.007. [DOI] [PubMed] [Google Scholar]
- 15.Masten A.S., Reed M.-G.J. Resilience in development. Handb Posit Psychol. 2002;74:88. [Google Scholar]
- 16.Killgore W.D., Taylor E.C., Cloonan S.A., Dailey N.S. Psychological resilience during the COVID-19 lockdown. Psychiatr Res. 2020;291:113216. doi: 10.1016/j.psychres.2020.113216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Riehm K.E., Brenneke S.G., Adams L.B., et al. Association between psychological resilience and changes in mental distress during the COVID-19 pandemic. J Affect Disord. 2021;282:381–385. doi: 10.1016/j.jad.2020.12.071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Necho M., Birkie M., Gelaye H., Beyene A., Belete A., Tsehay M. Depression, anxiety symptoms, Insomnia, and coping during the COVID-19 pandemic period among individuals living with disabilities in Ethiopia, 2020. PloS One. 2020;15(12) doi: 10.1371/journal.pone.0244530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Havnen A., Anyan F., Hjemdal O., Solem S., Gurigard Riksfjord M., Hagen K. Resilience moderates negative outcome from stress during the COVID-19 pandemic: a moderated-mediation approach. Int J Environ Res Publ Health. 2020;17(18):6461. doi: 10.3390/ijerph17186461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tsibidaki A. Anxiety, meaning in life, self-efficacy and resilience in families with one or more members with special educational needs and disability during COVID-19 pandemic in Greece. Res Dev Disabil. 2021;109:103830. doi: 10.1016/j.ridd.2020.103830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Folkman S., Lazarus R.S. An analysis of coping in a middle-aged community sample. J Health Soc Behav. 1980:219–239. [PubMed] [Google Scholar]
- 22.Song S., Yang X., Yang H., et al. Psychological resilience as a protective factor for depression and anxiety among the public during the outbreak of COVID-19. Running Title: protective factor of the public during COVID-19. Front Psychol. 2020;11:4104. doi: 10.3389/fpsyg.2020.618509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hennessy S., Kurichi J.E., Pan Q., et al. Disability stage is an independent risk factor for mortality in medicare beneficiaries aged 65 Years and older. Pm r. Dec 2015;7(12):1215–1225. doi: 10.1016/j.pmrj.2015.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Na L., Pan Q., Xie D., et al. Activity limitation stages are associated with risk of hospitalization among medicare beneficiaries. Pm r. May 2017;9(5):433–443. doi: 10.1016/j.pmrj.2016.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kurichi J.E., Streim J.E., Xie D., et al. The association between activity limitation stages and admission to facilities providing long-term care among older medicare beneficiaries. Am J Phys Med Rehabil. Jul 2017;96(7):464–472. doi: 10.1097/phm.0000000000000653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Stineman M.G., Streim J.E., Pan Q., Kurichi J.E., Schussler-Fiorenza Rose S.M., Xie D. Activity limitation stages empirically derived for activities of daily living (ADL) and instrumental ADL in the U.S. Adult community-dwelling medicare population. Pm r. Nov. 2014;6(11):976–987. doi: 10.1016/j.pmrj.2014.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Na L., Hennessy S., Bogner H.R., et al. Disability stage and receipt of recommended care among elderly medicare beneficiaries. Disabil Health J. Jan. 2017;10(1):48–57. doi: 10.1016/j.dhjo.2016.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Na L., Streim J.E. Psychosocial well-being associated with activity of daily living stages among community-dwelling older adults. Gerontol Geriatr Med. Jan-Dec 2017;3 doi: 10.1177/2333721417700011. 2333721417700011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Na L., Singh S. Disparities in mental health, social support and coping among individuals with mobility impairment. Disabil Health J. 2021;14(2):101047. doi: 10.1016/j.dhjo.2020.101047. [DOI] [PubMed] [Google Scholar]
- 30.Understanding America Study. Understanding coronavirus in America. Accessed Feb 3, 2021. https://uasdata.usc.edu/index.php.
- 31.Kroenke K., Spitzer R.L., Williams J.B., Löwe B. An ultra-brief screening scale for anxiety and depression: the PHQ–4. Psychosomatics. 2009;50(6):613–621. doi: 10.1176/appi.psy.50.6.613. [DOI] [PubMed] [Google Scholar]
- 32.Umucu E., Grenawalt T.A., Reyes A., et al. Flourishing in student veterans with and without service-connected disability: psychometric validation of the flourishing scale and exploration of its relationships with personality and disability. Rehabil Counsel Bull. 2019;63(1):3–12. [Google Scholar]
- 33.EUROQOL. EQ-5D-5L. Accessed March 1, 2021. https://euroqol.org/eq-5d-instruments/eq-5d-5l-about/.
- 34.Cohen S., Kamarck T., Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983:385–396. [PubMed] [Google Scholar]
- 35.Cohen S. 1988. Perceived Stress in a Probability Sample of the United States. [Google Scholar]
- 36.Ingram I.V.P.B., Clarke E., Lichtenberg J.W. Confirmatory factor analysis of the perceived stress Scale-4 in a community sample. Stress Health. 2016;32(2):173–176. doi: 10.1002/smi.2592. [DOI] [PubMed] [Google Scholar]
- 37.Smith B.W., Dalen J., Wiggins K., Tooley E., Christopher P., Bernard J. The brief resilience scale: assessing the ability to bounce back. Int J Behav Med. 2008;15(3):194–200. doi: 10.1080/10705500802222972. [DOI] [PubMed] [Google Scholar]
- 38.Umucu E., Lee B. Examining the impact of COVID-19 on stress and coping strategies in individuals with disabilities and chronic conditions. Rehabil Psychol. 2020;65(3):193–198. doi: 10.1037/rep0000328. Epub 2020 May 14. PMID: 32406739. [DOI] [PubMed] [Google Scholar]
- 39.Gurka M.J., Edwards L.J., Muller K.E. Avoiding bias in mixed model inference for fixed effects. Stat Med. 2011;30(22):2696–2707. doi: 10.1002/sim.4293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ahmed M.Z., Ahmed O., Aibao Z., Hanbin S., Siyu L., Ahmad A. Epidemic of COVID-19 in China and associated psychological problems. Asian J Psychiatr. 2020;51:102092. doi: 10.1016/j.ajp.2020.102092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Cao W., Fang Z., Hou G., et al. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatr Res. 2020;287:112934. doi: 10.1016/j.psychres.2020.112934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ungar M. Putting a Human Face on Child Welfare: Voices from the Prairies. 2007. Contextual and cultural aspects of resilience in child welfare settings; pp. 1–23. [Google Scholar]
- 43.Runswick-Cole K., Goodley D. Resilience: a disability studies and community psychology approach. Soc Pers Psychol Compass. 2013;7(2):67–78. [Google Scholar]
- 44.Young A., Green L., Rogers K. Resilience and deaf children: a literature review. Deaf Educ Int. 2008;10(1):40–55. [Google Scholar]
- 45.Miller Smedema S., Catalano D., Ebener D.J. The relationship of coping, self-worth, and subjective well-being: a structural equation model. Rehabil Counsel Bull. 2010;53(3):131–142. [Google Scholar]
- 46.Fluharty M., Fancourt D. vol. 26. 2020. p. 580. (How Have People Been Coping during the COVID-19 Pandemic? Patterns and Predictors of Coping Strategies Amongst). UK adults. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Doron J., Trouillet R., Maneveau A., Neveu D., Ninot G. Coping profiles, perceived stress and health-related behaviors: a cluster analysis approach. Health Promot Int. 2014;30(1):88–100. doi: 10.1093/heapro/dau090. [DOI] [PubMed] [Google Scholar]
- 48.Holahan C.J., Moos R.H., Holahan C.K., Brennan P.L., Schutte K.K. Stress generation, avoidance coping, and depressive symptoms: a 10-year model. J Consult Clin Psychol. 2005;73(4):658. doi: 10.1037/0022-006X.73.4.658. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.