Abstract
Dental anxiety is a crucial problem for dentistry because it may represent a significant risk to oral health. Different factors, whether non‐cognitive (e.g., traumatic dental events) or cognitive (e.g., the patient's subjective perceptions), may cause dental anxiety. However, previous studies have assessed these factors as independent predictors of dental anxiety, without providing any exploration of potential mediational pathways. The current study assessed the role of certain cognitive dimensions (i.e., the dentist's perceived professionalism and communicational attitudes, and the patient's perceived lack of control) as mediators between traumatic dental events and dental anxiety. The sample comprised 253 patients who had accessed a public university hospital dental surgery. The mediation analysis used a structural equation modeling. Traumatic dental events were positively associated with dental anxiety but, among the cognitive factors, only lack of control was. Furthermore, lack of control mediated the relationship between traumatic dental events and dental anxiety, although this mediation was only partial. This study sheds light on the mechanisms through which non‐cognitive and cognitive factors may affect dental anxiety. The clinical implications for dental practice, in terms of improving the psychological well‐being of patients, are discussed.
Keywords: cognition, control, dental anxiety, mediation, trauma
INTRODUCTION
Dental anxiety is a psychophysiological state which can be defined as an emotional state of worry or apprehension in anticipation of dental treatment [1]. Excessive levels of dental anxiety may induce a low compliance with dental treatment or psychological distress, representing a serious risk for oral health or, in extreme cases, a significant barrier to the access to dental care [2, 3]. Epidemiological research in Western contexts has reported that a percentage ranging from 10% to 20% of adults suffer from high levels of dental anxiety [4, 5]. Thus, addressing dental anxiety in the patient population should be considered a fundamental priority for dentistry and public health.
According to Beaton et al. [6], factors causing dental anxiety may be exogenous (e.g., previous and direct distressing or traumatic dental experiences), endogenous (e.g., personality traits, such as neuroticism) or vicarious (e.g., negative dental experiences recounted by significant others or in the media). In this regard, while some studies have attributed to past traumatic episodes experienced within a dental setting (i.e., the non‐cognitive factors) a central pathogenetic factor in terms of the development of dental anxiety [7, 8], others have highlighted the role of subjective factors in the processing of dental‐related stimuli (i.e., the cognitive factors), such as the patient's personal perceptions of the dentist and dental treatment [1, 9, 10].
Concerning non‐cognitive factors, previous studies have found associations between traumatic dental events and high levels of dental anxiety. In this regard, the model by Rachman [11] assumes that negative dental experiences – as well as vicarious conditioning or reports of the harmfulness of dental procedures – are crucial factors in the development of dental anxiety, because such experiences lead patients to associate dental treatments and stimuli with discomfort and pain. Some examples of traumatic dental events include invasive dental treatment (e.g., root canal treatments or injections) [12], pain [13, 14] or distress caused by the dentist's behavior [12]. In this regard, de Jongh et al. [7] found that patients with higher levels of dental anxiety were more likely to report traumatic dental events than those with lower levels (73% versus 21%) and that horrific experiences within the dental setting were the most common traumatic events recounted. Similarly, Oosterink et al. [15] found that invasive dental procedures (e.g., extractions or injections) are among the distressing dental events most frequently associated with high levels of dental anxiety, while Scandurra et al. [8] found that, in a clinical sample of Italian dental patients, the likelihood of having high dental anxiety was greater with more exposure to traumatic dental events.
However, another line of research has stressed the impact that non‐cognitive factors may have on dental anxiety, debunking the general assumption that traumatic dental experiences have the greatest value in terms of predicting dental anxiety. In this regard, the Cognitive Vulnerability Model (CVM) [16] proposes that the central dimension associated with dental anxiety is represented by the vulnerability schema, which is activated when the fearful patient is exposed to dental stimuli. The contents of this schema involve four interconnected perceptions of the dental event, designated uncontrollable, unpredictable, potentially dangerous or harmful, and disgusting. Once this schema is activated, two processes occur simultaneously; namely, an immediate and automatic affective response (i.e., fear) and a cognitive assessment of the event. Armfield [1] found that vulnerability‐related perceptions accounted for more than 45% of the variance in dental anxiety, in contrast to dental negative experiences which accounted for <1%. Similarly, Carrillo‐Diaz et al. [9] found that cognitive factors were the best predictors of dental anxiety and that, once included in a unique regression model comprising both non‐cognitive and cognitive factors, non‐cognitive factors were no longer predictors. Further, de Jongh et al. [10] demonstrated that patients reporting having been exposed to a traumatic event perceived as associated with the cause of dental anxiety did not differ in dental anxiety severity from those not having reported any such experience. Nevertheless, the CVM does not preclude previous traumatic experiences or individual factors (e.g., personality traits) playing a role in dental fear responses, since subjective perceptions seem to originate from a combination of individual traits and personal experiences. Indeed, Armfield [16] asserted that the vulnerability schema may be activated even through experiential factors, such as the pathways highlighted by Rachman [11].
Previous studies have assessed cognitive and non‐cognitive factors as independent predictors of dental anxiety, without providing any exploration of the potential mediational pathways which may shed light on the mechanisms through which such factors might operate. Indeed, an approach to understand the effective role of cognitive factors in accounting for dental anxiety could be an examination of whether such factors partially or fully mediate the relationship between non‐cognitive factors and dental anxiety. Accordingly, the aim of the current study was to explore such a mediational model, assessing cognitive factors using the Milgrom et al. model [17], which is a well‐established theoretical model of the patient's perception of the dentist and dental treatment which is widely used in research on dental anxiety [18, 19, 20, 21]. Milgrom et al. [17] identified three main dimensions of the patient's perceptions of the dentist and dental treatment: (a) Professionalism, referring to the perceived technical competence and integrity of the dentist; (b) Communication, referring to the patient's perceptions of the dentist's attitudes in relation to communication and how comfortable the patient feels in talking to the dentist; and (c) Lack of control, which is the perception of not being in control of the situation and not having the possibility of taking a break during treatment. All of these dimensions have been shown to be associated with dental anxiety, with the more negative the impression of the dentist and the treatment situation the higher the levels of dental anxiety [22, 23].
Thus, based on previous studies highlighting the associations between traumatic dental events and dental anxiety [7, 8, 12], we hypothesized that traumatic dental events would be a non‐cognitive factor associated with dental anxiety (Hypothesis 1). Furthermore, based on the CVM [1, 16], we hypothesized that cognitive factors would also be associated with dental anxiety (Hypothesis 2). Finally, since cognitive factors may be influenced by experiential factors [1] and are also predictors of dental anxiety [1, 16], we also hypothesized that cognitive factors would mediate the relationship between traumatic dental events and dental anxiety (Hypothesis 3). The hypothesized mediation model is depicted in Figure 1.
FIGURE 1.
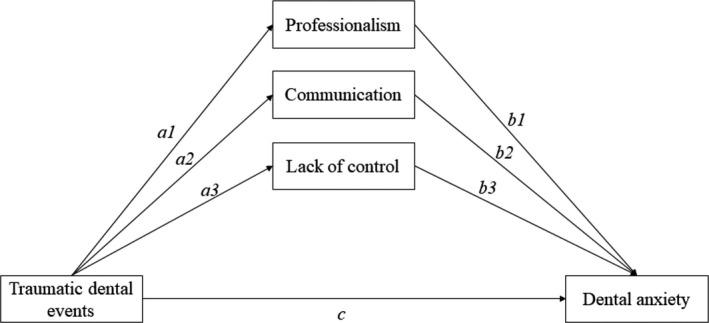
The hypothesized mediation model
MATERIAL AND METHODS
Procedures and participants
The data analyzed in this cross‐sectional study are part of a larger project launched in September 2018 assessing the psychological dimensions (e.g., attachment, personality traits, and defences) related to dental anxiety. Between September 2018 and October 2019, patients who accessed the Dental Surgery Unit of the University of Naples Federico II for the day hospital, ordinary hospitalization, or pre‐recovery were invited to participate in this study during their first appointment.
Patients could participate in the study if they were aged between 18 and 80 years, able to understand the informed consent and complete the questionnaires independently, and had accessed the Dental Surgery Unit to undergo dental surgery in the day hospital, ordinary hospitalization, or pre‐recovery. All of these eligibility criteria were evaluated by the dentists during the completion of the initial medical record. The patients were carefully informed about the study and completed the questionnaires independently and anonymously only after signing the informed consent form on a separate sheet.
A total of 253 patients (124 men and 129 women) took part in the survey. The patients ranged in age from 18 to 80 (mean = 49.1; SD = 16.4). Furthermore, 219 (86.6%) patients had an educational level ≤ high school, while 34 (13.4%) an educational level ≥ university or college. Most of the patients (n = 239; 94.5%) had accessed the clinic for the day hospital, with only 4 (1.6%) for an ordinary recovery and 10 (4%) for a pre‐recovery.
The current study was approved by the Ethical Committee of the University of Naples Federico II (protocol number: 1043/18), conducted in accordance with the EU General Data Protection Regulation, and designed in respect of the principles of the Declaration of Helsinki.
Measures
To assess the degree of distress of traumatic dental experiences we used the Level of Exposure‐Dental Experiences Questionnaire (LOE‐DEQ) [24], a 23‐item scale evaluating distressing events related to dental procedures or to dentists, as well as general traumatic life events. Since we were interested in assessing only the traumatic events experienced within the dental setting, we used only the 16‐item subscale ‘Traumatic dental experiences’. The LOE‐DEQ requires the respondents to indicate whether or not (yes versus no) they had experienced any specific distressing events. The Cronbach alpha coefficient for the current sample was 0.78, while Guttman's Lambda was 0.80, suggesting good internal consistency reliability.
The patients’ perceptions of the dentist and dental treatment were assessed using the revised version of the Dental Beliefs Survey (DBS‐R) [17], a 28‐item scale comprising three subscales (Professionalism, Communication, and Lack of Control). The responses were scored from 1 (never) to 5 (nearly always), with higher scores on each subscale indicating more negative beliefs and perceptions. The respective alpha coefficients were 0.86, 0.92, and 0.91 for the subscales.
Finally, dental anxiety was evaluated through the Modified Dental Anxiety Scale (MDAS) [25], a 5‐item scale measuring dental anxiety on a five‐point Likert scale and generating a total score ranging from 5 (not anxious) to 25 (extremely anxious). A cut‐off of 19 is considered to indicate a high level of dental anxiety. The Cronbach alpha coefficient for the current sample was 0.92.
Data analysis
Preliminary analyses concerned the handling of missing data. Only a few data were missing (1.4% of the total) and these were considered as missing at random because they were not related to the total scale scores. A missing value imputation was performed using the k nearest neighbors (KNN) algorithm [26], with the Euclidean distance as a distance metric in the multi‐dimensional space.
We calculated descriptive statistics (distribution of frequencies, means, and standard deviations) and bivariate correlations between variables, and assessed the differences between participants with low and high levels of dental anxiety in relation to traumatic dental events and the patient's perceptions of the dentist by using the Student t‐test.
The mediation analysis was performed with the “lavaan” R package [27], which estimates the model parameters using the structural equation modeling approach. Kline [28] suggested that a sample size of at least 200 participants is necessary to estimate the model parameters. As an estimator method, the maximum likelihood with robust standard errors and a mean and variance adjusted test statistic (the Satterthwaite approach) was used. Thus, as shown in Figure 1, we tested the main effect of traumatic dental events on dental anxiety (path c; Hypothesis 1), the main effect of the three cognitive factors (i.e., Professionalism, Communication, and Lack of Control) on dental anxiety (path a; Hypothesis 2), and the mediating role of each cognitive factor in the relationship between traumatic dental events and dental anxiety (paths a*b; Hypothesis 3). Because sociodemographic characteristics are also associated with dental anxiety, we adjusted for gender, age, and educational level in the models. Indeed, previous studies have demonstrated that female [29, 30, 31], younger [25, 32], and less educated [25, 32, 33] people experience higher levels of dental anxiety.
RESULTS
Almost a third of the sample (28.9%) proved to be above the MDAS cut‐off (>19), the threshold to detect people with high levels of dental anxiety.
Summary statistics and bivariate correlations among the study variables are reported in Table 1. Specifically, traumatic dental events were positively correlated with both the cognitive factors (i.e., professionalism, communication, and lack of control) and dental anxiety, indicating that higher rates of distressing dental events were associated with higher levels of negative perceptions of the dentist as well as with higher levels of dental anxiety. Similarly, all of the cognitive factors were positively correlated with dental anxiety, indicating that higher levels of negative perceptions about the dentist and the dental treatment were associated with a greater dental anxiety.
TABLE 1.
Bivariate correlations between scores for traumatic dental events, patient's subjective cognitions, and dental anxiety
| 1 | 2 | 3 | 4 | 5 | Mean | SD | |
|---|---|---|---|---|---|---|---|
| 1. Traumatic dental events | 1 | 2.3 | 2.7 | ||||
| 2. Professionalism | 0.41 | 1 | 22.8 | 9.3 | |||
| 3. Communication | 0.38 | 0.79 | 1 | 16.5 | 7.9 | ||
| 4. Lack of control | 0.43 | 0.74 | 0.84 | 1 | 15.5 | 7.5 | |
| 5. Dental anxiety | 0.32 | 0.30 | 0.33 | 0.40 | 1 | 14.4 | 5.7 |
Abbreviation: SD, standard deviation.
Mean scores for traumatic dental events and patients’ subjective cognitions by dental anxiety level are reported in Table 2. Patients with high dental anxiety had higher scores on both non‐cognitive and cognitive factors.
TABLE 2.
Mean scores for traumatic dental events and patients' subjective cognitions by dental anxiety level
| Dental anxiety |
Difference High − Low |
||
|---|---|---|---|
|
Low (cut‐off <19) N = 180 Mean (SD) |
High (cut‐off >19) N = 73 Mean (SD) |
||
| Mean (95% CI) | |||
| Traumatic dental events | 1.9 (2.2) | 3.3 (3.4) | 1.4 (0.7, 2.1)*** |
| Professionalism | 21.6 (8.1) | 25.8 (9.6) | 4.2 (1.9, 6.5)*** |
| Communication | 15.3 (7.0) | 19.3 (9.1) | 4.0 (1.9, 6.1)*** |
| Lack of control | 14.1 (6.7) | 19.0 (8.1) | 4.9 (3.0, 6.8)*** |
Abbreviation: SD, standard deviation.
p < 0.001.
Because the mediators were strongly correlated with each other, we first checked for their multicollinearity through an assessment of Variance Inflation Factors (VIF). However, no multicollinearity was identified, since the largest VIF was equal to 4 (a VIF greater than 10 suggests the presence of multicollinearity). Nevertheless, because the correlations between the mediators were strong and we were interested in assessing the direct comparison between the effects through standardized coefficients, we used standardized variables.
As shown in Figure 2 and with respect to Hypothesis 1, traumatic dental events were positively associated with dental anxiety [c = 0.186; 95% CI (0.020, 0.351); p = 0.028], confirming our hypothesis.
FIGURE 2.
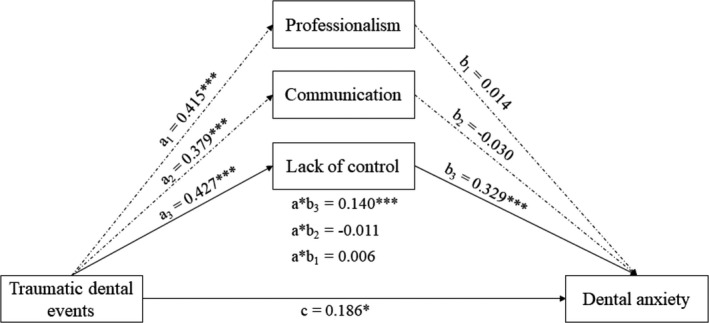
Results from the Structural Equation Modeling of the hypothesized mediation model. Standardized path coefficients are reported. Dashed lines represent non‐significant paths. For simplicity, associations with control variables are omitted. *p < 0.05; ***p < 0.001
Instead, with regard to Hypothesis 2, we found that, among the cognitive factors, only lack of control was positively associated with dental anxiety [b3 = 0.329; 95% CI (0.204, 0.453); p < 0.001], partially confirming our hypothesis. On the contrary, neither professionalism [b1 = 0.014; 95% CI (−0.108, 0.136); p = 0.828] nor communication [b2 = −0.030; 95% CI (−0.152, 0.092); p = 0.633] were associated with dental anxiety. The R 2 of the multiple regression model was 0.262.
Finally, with respect to Hypothesis 3, experiences of traumatic dental events were associated with higher levels of all cognitive factors [a1 = 0.415; 95% CI (0.299, 0.532); p < 0.001]; [a2 = 0.379; 95% CI (0.247, 0.511); p < 0.001]; and [a3 = 0.427; 95% CI (0.307, 0.548); p < 0.001], but only lack of control mediated the relationship between traumatic dental events and dental anxiety [a*b3 = 0.140; 95% CI (0.075, 0.206); p < 0.001], thus partially confirming our hypothesis. Specifically, the strength of the association between traumatic dental events and dental anxiety was greater with lower control. This mediation was partial, since traumatic dental events continued to be a significant predictor of dental anxiety.
DISCUSSION
The aim of this study was to assess the mediating role of cognitive factors (such as professionalism, communication, and lack of control) in the relationship between traumatic dental events and dental anxiety. Generally, the findings have confirmed this main hypothesis. However, they have indicated that, among the cognitive factors, only lack of control mediates the direct path between non‐cognitive factors and dental anxiety and that this mediation is partial. To the best of our knowledge, this is the first study testing this mediational model, highlighting potentially significant pathways through which traumatic dental events might affect dental anxiety.
With regard to the descriptive analyses, we found that cognitive and non‐cognitive factors correlated with each other, as well as with dental anxiety. Furthermore, we found that patients with high levels of dental anxiety had experienced a greater number of traumatic dental events and had experienced more negative perceptions of the dentist and dental treatments than those with a low dental anxiety. These findings are consistent with previous studies highlighting that both cognitive and non‐cognitive factors are important determinants of high dental anxiety [1, 7, 31].
In support of our first hypothesis, we found that traumatic dental events were associated with higher levels of dental anxiety. These findings are consistent with previous research highlighting the predictive role for dental anxiety of traumatic and distressing events experienced within a dental setting [7, 8, 15]. In addition, gender was the only sociodemographic characteristic showing statistical significance, indicating that females are more likely to report higher levels of dental anxiety, consistent with previous findings [29, 30, 31]. A possible explanation for this gender difference is that women tend to pay more attention to physical symptoms and experience higher emotional distress relating to health problems than men, or, alternatively, that women tend to overestimate the probability of danger, with this cognitive appraisal then activating a greater anxiety response [34].
For the second and third hypotheses, our findings instead reflected two main points. First, lack of control is the only cognitive dimension within the Milgrom et al. model [17] which predicts dental anxiety. Second, the mediating action of lack of control is crucial for explaining the variance in dental anxiety, although, in addition to this cognitive factor, traumatic dental events continue to be a predictor of dental anxiety.
In respect of the first point, the perception of not being in control of the situation and, above all, of experiencing adverse emotional events has been widely recognized as a psychological vulnerability factor in the development of anxiety disorders, representing a mediator of the relationship between previous negative experiences and anxiety [35]. Indeed, deficits in perceived emotional control have proven to be associated with several anxiety disorders, such as panic disorder [36], post‐traumatic stress disorder [37], and generalized anxiety disorder [38]. However, such a vulnerability factor may over time become a crystallized trait which may moderate the relationship between environmental stressors and anxiety [35]. Specifically, considering the focus of this study, the relationship between lack of control and dental anxiety has been widely recognized, with lack of control identified as a central cognitive dimension in the development of dental anxiety [12, 20, 39]. In this regard, Milgrom et al. [17] themselves reported that the degree to which patients feel they have no control during dental treatment seems to represent the most important predictor of dental anxiety. This finding is consistent with the CVM [16, 40], which highlighted the central role of perceptions of having a lack of control. Thus, we can assert that this finding provides further confirmation of the CVM and that, therefore, cognitive dimensions play a crucial role in the expression and development of dental anxiety.
In respect of the second point, our findings partially confirm the CVM assumptions [16, 40], but not those studies reporting that real traumatic dental experiences can no longer be considered to be predictors of dental anxiety once cognitive factors are taken into account [9]. This finding may be attributed to the diverse nature of the samples. Indeed, in contrast to previous studies, which enrolled undergraduates [9] or the general population [1], we recruited a clinical sample of patients using a public dental clinic. This might mean that our sample, being clinical, may have experienced more dental needs and subsequent dental treatment than undergraduates or the general population and this, in turn, might have increased their likelihood of experiencing a greater number of real negative experiences. However, this is only speculation, since we cannot make any comparisons between such samples. Future studies should consider comparing clinical and non‐clinical samples, replicating our study by examining potential differences in rates and types of negative dental experiences, as well as in mediational pathways. Another possible explanation concerns the theoretical model used in the current study [17]. The CVM postulates that the vulnerability schema involves four kinds of perception relating to dentists and dental treatments, namely uncontrollability, unpredictability, dangerousness, and disgustingness, while the Milgrom et al. model [17] assesses the dentist's perceived professionalism and communication attitudes, along with the patient's perceived lack of control [41] Thus, in addition to the control‐related dimension, all of the other cognitive factors measure different constructs. Future research should replicate our study in assessing the specific CVM dimensions.
The findings of the current study should be understood in the light of its important limitations. First, its cross‐sectional nature does not allow the drawing of any conclusive inferences about the temporality and causality of the relationships among the variables explored. Indeed, based on the CVM, cognitions may have bidirectional relationships with events, and the interpretation of the event may be influenced retrospectively by the level of anxiety. Thus, future studies should use a longitudinal research design to discern the cause–effect relationships between cognitive/non‐cognitive factors and dental anxiety. Secondly, the sample is not representative and was recruited at a single hospital, thus precluding generalizability. Furthermore, participants in the current study reported higher rates of dental anxiety than the reference group (28.9% versus 10%–12%) [5, 25] and this may have influenced the findings. It is plausible that high levels of dental anxiety may lead people to overestimate the impact of certain dental procedures, as well as increasing their negative perceptions of the dentist and the dental treatment. Thus, it is possible that a population study would include a greater degree of variability in all measures and, therefore, strengthen associations which were not apparent in the current study or, on the contrary, weaken those which are currently observed. At the same time, future studies should recruit larger and more diversified samples to analyze the mediating role of cognitive factors in the relationships of single dental traumatic events and dental anxiety. Third, we assessed cognitive factors using only the Milgrom et al. model [17], and it is possible that different findings would have been obtained if we had used other measures specifically suggested by the CVM, such as unpredictability, dangerousness, and disgustingness. Fourth, we assessed the mediating role of cognitive factors, but it is also plausible to hypothesize that cognitive factors would act as moderators of the relationship between non‐cognitive factors and dental anxiety, because certain patterns of thinking may lead to interpretation of specific events in a way that could produce anxiety. Thus, future studies should consider assessing the potential interactive effects of cognitive factors increasing or decreasing the effects of dental traumatic events on dental anxiety. Finally, learning theories suggest that repeated critical events are crucial in the onset of anxiety and phobia [42], but we did not assess the role of repetitiveness of these events. Future studies should evaluate this dimension by examining how much variance in dental anxiety it explains.
Despite these limitations, the present study might have some useful clinical implications for dental practice. First, dentists should always assess their patient's level dental anxiety, through both semi‐structured interviews and appropriate scales (see Appukuttan [43] for a review of these methods). Indeed, a careful assessment of dental anxiety may enhance the general dental management, assisting the dentist in deciding an appropriate treatment plan. Second, dentists should not underestimate the potential relationship between previous traumatic dental experiences and dental anxiety. For example, the dentist should take time to inquire about the patients’ previous dental experiences and listen to their opinions about the dental care they have received, exploring the potential effects of such events on perceptions about the dentist and dental treatments, encouraging patients to ask questions about the treatment, and reassuring them if they show some degree of anxiety. Third, because a perception of not being in control of the situation increases the likelihood of experiencing dental anxiety (especially during the treatment procedure) dentists should do their best to allow their patients to feel that they have control over the situation. For example, the dentist may tell their patients that it is possible to interrupt the procedure in the case of excessive pain or for any other reason through a signal agreed before the procedure (e.g., a raised hand). Moreover, control can also be provided through behavioral methods [43]. A very useful behavioral technique able to reduce uncertainty and increase predictability in the clinical setting, both for adults and children, is ‘tell‐show‐do’ [44]. This technique consists, first, in verbally explaining which procedures will be performed, adapting the language to the appropriate developmental level of the patient (‘tell’); second, in demonstrating to the patient the visual, olfactory, auditory, and tactile aspects of the procedures in an unthreatening setting (‘show’); and third, in completing the treatment in a way which is coherent with the explanation and demonstration (‘do’).
CONFLICTS OF INTEREST
The authors declare that they have no conflict of interest.
AUTHOR CONTRIBUTIONS
Conceptualization: Cristiano Scandurra, Roberta Gasparro, Gilberto Sammartino, Nelson Mauro Maldonato; Methodology: Cristiano Scandurra, Roberta Gasparro, Gilberto Sammartino, Gaetano Marenzi, Nelson Mauro Maldonato; Formal analysis: Pasquale Dolce; Investigation: Cristiano Scandurra, Vincenzo Bochicchio, Benedetta Muzii, Gaetano Marenzi; Resources: Vincenzo Bochicchio, Benedetta Muzii, Gaetano Marenzi; Data curation: Cristiano Scandurra, Roberta Gasparro, Vincenzo Bochicchio, Benedetta Muzii; Writing – original draft: Cristiano Scandurra Roberta Gasparro; Writing – review & editing: Vincenzo Bochicchio, Benedetta Muzii, Gaetano Marenzi; Supervision: Gilberto Sammartino, Nelson Mauro Maldonato; Project administration: Gilberto Sammartino, Nelson Mauro Maldonato. All authors approved the final version of this article.
Scandurra C, Gasparro R, Dolce P, Bochicchio V, Muzii B, Sammartino G, et al. The role of cognitive and non‐cognitive factors in dental anxiety: A mediation model. Eur J Oral Sci. 2021; 129:e12793. 10.1111/eos.12793.
REFERENCES
- 1.Armfield JM. Towards a better understanding of dental anxiety and fear: cognitions vs. experiences. Eur J Oral Sci. 2010;118:259–64. [DOI] [PubMed] [Google Scholar]
- 2.Halvari AEM, Halvari H, Deci EL. Dental anxiety, oral health‐related quality of life, and general well‐being: a self‐determination theory perspective. J Appl Soc Psychol. 2019;49:295–306. [Google Scholar]
- 3.Hill KB, Chadwick B, Freeman R, O’Sullivan I, Murray JJ. Adult Dental Health Survey 2009: relationships between dental attendance patterns, oral health behaviour and the current barriers to dental care. Br Dent J. 2013;214:25–32. [DOI] [PubMed] [Google Scholar]
- 4.Buunk‐Werkhoven YAB, Dijkstra A, van der Schans CP. Oral health‐quality of life predictors depend on population. Appl Res Qual Life. 2009;4:283. [Google Scholar]
- 5.Humphris G, Crawford JR, Hill K, Gilbert A, Freeman R. UK population norms for the modified dental anxiety scale with percentile calculator: adult dental health survey 2009 results. BMC Oral Health. 2013;13:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Beaton L, Freeman R, Humphris G. Why are people afraid of the dentist? Observations and explanations. Med Princ Pract. 2014;23:295–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.de Jongh A, Fransen J, Oosterink‐Wubbe F, Aartman I. Psychological trauma exposure and trauma symptoms among individuals with high and low levels of dental anxiety. Eur J Oral Sci. 2006;114:286–92. [DOI] [PubMed] [Google Scholar]
- 8.Scandurra C, Gasparro R, Dolce P, Bochicchio V, Muzii B, Spagnuolo G, et al. The Italian validation of the level of exposure‐dental experiences questionnaire. Appl Sci. 2020;10:1143. [Google Scholar]
- 9.Carrillo‐Diaz M, Crego A, Armfield JM, Romero‐Maroto M. Assessing the relative efficacy of cognitive and non‐cognitive factors as predictors of dental anxiety. Eur J Oral Sci. 2012;120:82–8. [DOI] [PubMed] [Google Scholar]
- 10.De Jongh A, van Eeden A, van Houtem CMHH, van Wijk AJ. Do traumatic events have more impact on the development of dental anxiety than negative, non‐traumatic events? Eur J Oral Sci. 2017;125:202–7. [DOI] [PubMed] [Google Scholar]
- 11.Rachman S. The conditioning theory of fear‐acquisition: a critical examination. Behav Res Ther. 1977;15:375–87. [DOI] [PubMed] [Google Scholar]
- 12.Abrahamsson KH, Berggren U, Hallberg L, Carlsson SG. Dental phobic patients’ view of dental anxiety and experiences in dental care: a qualitative study. Scand J Caring Sci. 2002;16:188–96. [DOI] [PubMed] [Google Scholar]
- 13.De Jongh A, van der Burg J, van Overmeir M, Aartman I, van Zuuren FJ. Trauma‐related sequelae in individuals with a high level of dental anxiety. Does this interfere with treatment outcome? Behav Res Ther. 2002;40:1017–29. [DOI] [PubMed] [Google Scholar]
- 14.Versloot J, Veerkamp JS, Hoogstraten J. Children’s self‐reported pain at the dentist. Pain. 2008;137:389–94. [DOI] [PubMed] [Google Scholar]
- 15.Oosterink FM, de Jongh A, Aartman IH. Negative events and their potential risk of precipitating pathological forms of dental anxiety. J Anxiety Disord. 2009;23:451–7. [DOI] [PubMed] [Google Scholar]
- 16.Armfield JM. Cognitive vulnerability: a model of the etiology of fear. Clin Psychol Rev. 2006;26:746–68. [DOI] [PubMed] [Google Scholar]
- 17.Milgrom P, Weinstein P, Getz T. Treating fearful dental patients: a patient management handbook. Seattle, WA: Continuing Dental Education; 1995. [Google Scholar]
- 18.Coolidge T, Hillstead MB, Farjo N, Weinstein P, Coldwell SE. Additional psychometric data for the Spanish Modified Dental Anxiety Scale, and psychometric data for a Spanish version of the Revised Dental Beliefs Survey. BMC Oral Health. 2010;10:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hathiwala S, Acharya S, Patil S. Personality and psychological factors: effects on dental beliefs. J Indian Soc Pedod Prev Dent. 2015;33:88–92. [DOI] [PubMed] [Google Scholar]
- 20.Maggirias J, Locker D. Five‐year incidence of dental anxiety in an adult population. Community Dent Health. 2002;19:173–9. [PubMed] [Google Scholar]
- 21.Moore R, Brødsgaard I, Abrahamsen RA. 3‐year comparison of dental anxiety treatment outcomes: hypnosis, group therapy and individual desensitization vs. no specialist treatment. Eur J Oral Sci. 2002;110:287–95. [DOI] [PubMed] [Google Scholar]
- 22.Abrahamsson KH, Hakeberg M, Stenman J, Ohrn K. Dental beliefs: evaluation of the Swedish version of the revised Dental Beliefs Survey in different patient groups and in a non‐clinical student sample. Eur J Oral Sci. 2006;114:209–15. [DOI] [PubMed] [Google Scholar]
- 23.Coolidge T, Heima M, Coldwell SE, Weinstein P, Milgrom P. Psychometric properties of the revised dental beliefs survey. Community Dent Oral Epidemiol. 2005;33:289–97. [DOI] [PubMed] [Google Scholar]
- 24.Oosterink FM, de Jongh A, Hoogstraten J, Aartman IH. The Level of Exposure‐Dental Experiences Questionnaire (LOE‐DEQ): a measure of severity of exposure to distressing dental events. Eur J Oral Sci. 2008;116:353–61. [DOI] [PubMed] [Google Scholar]
- 25.Humphris GM, Dyer TA, Robinson PG. The modified dental anxiety scale: UK general public population norms in 2008 with further psychometrics and effects of age. BMC Oral Health. 2009;9:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Andridge RR, Little RJ. A review of hot deck imputation for survey non‐response. Int Stat Rev. 2010;78:40–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rosseel Y. Lavaan: an R package for structural equation modeling. J Stat Softw. 2012;48:1–36. [Google Scholar]
- 28.Kline RB. Principles and practice of structural equation modeling, 3rd edn. New York, NY: Guilford Press; 2011. [Google Scholar]
- 29.Arslan S, Ertaş E, Ülker M. The relationship between dental fear and sociodemographic variables. Erciyes Med J. 2011;33:295–300. [Google Scholar]
- 30.Erten H, Akarslan ZZ, Bodrumlu E. Dental fear and anxiety levels of patients attending a dental clinic. Quintessence Int. 2006;37:304–10. [PubMed] [Google Scholar]
- 31.Humphris G, King K. The prevalence of dental anxiety across previous distressing experiences. J Anxiety Disord. 2011;25:232–6. [DOI] [PubMed] [Google Scholar]
- 32.do Nascimento DL, da Silva Araújo AC, Gusmão ES, Cimões R. Anxiety and fear of dental treatment among users of public health services. Oral Health Prev Dent. 2011;9:329–37. [PubMed] [Google Scholar]
- 33.Doerr PA, Lang WP, Nyquist LV, Ronis DL. Factors associated with dental anxiety. J Am Dent Assoc. 1998;129:1111–9. [DOI] [PubMed] [Google Scholar]
- 34.Carrillo‐Diaz M, Crego A, Romero‐Maroto M. The influence of gender on the relationship between dental anxiety and oral health‐related emotional well‐being. Int J Paediatr Dent. 2013;23:180–7. [DOI] [PubMed] [Google Scholar]
- 35.Barlow DH. Anxiety and its disorders: the nature and treatment of anxiety and panic, 2nd edn. New York: Guilford Press; 2002. [Google Scholar]
- 36.Bentley KH, Gallagher MW, Boswell JF, Gorman JM, Shear MK, Woods SW, et al. The interactive contributions of perceived control and anxiety sensitivity in panic disorder: a triple vulnerabilities perspective. J Psychopathol Behav. 2013;35:57–64. [Google Scholar]
- 37.Vujanovic AA, Zvolensky MJ, Bernstein A. Incremental associations between facets of anxiety sensitivity and posttraumatic stress and panic symptoms among trauma‐exposed adults. Cogn Behav Ther. 2008;37:76–89. [DOI] [PubMed] [Google Scholar]
- 38.Stapinski LA, Abbott MJ, Rapee RM. Fear and perceived uncontrollability of emotion: evaluating the unique contribution of emotion appraisal variables to prediction of worry and generalised anxiety disorder. Behav Res Ther. 2010;48:1097–104. [DOI] [PubMed] [Google Scholar]
- 39.Levin RP. Helping your patients overcome dental phobia. Compend Contin Educ Dent. 2003;24:8–10. [PubMed] [Google Scholar]
- 40.Armfield JM, Slade GD, Spencer AJ. Cognitive vulnerability and dental fear. BMC Oral Health. 2008;8:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gasparro R, Scandurra C, Maldonato NM, Dolce P, Bochicchio V, Valletta A, et al. Perceived Job Insecurity and Depressive Symptoms among Italian Dentists: The Moderating Role of Fear of COVID‐19. Int J Environment Res Public Health. 2020;17:5338. 10.3390/ijerph17155338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mineka S, Zinbarg R. A contemporary learning theory perspective on the etiology of anxiety disorders: it’s not what you thought it was. Am Psychol. 2006;61:10–26. [DOI] [PubMed] [Google Scholar]
- 43.Appukuttan DP. Strategies to manage patients with dental anxiety and dental phobia: literature review. Clin Cosmet Investig Dent. 2016;8:35–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.McTigue DJ. Behavior management for the pediatric dental patient. Pediatr Dent. 2004;26:110. [PubMed] [Google Scholar]


