Abstract
Line‐field confocal optical coherence tomography (LC‐OCT) is a new noninvasive technique for a real‐time, vertical, and horizontal imaging of the skin at cellular resolution. A 47‐year‐old female presented with a 6‐month history of an asymptomatic yellowish papule. LC‐OCT evaluation was able to show the diagnostic microscopic features of xanthogranuloma and showed an excellent correlation with vertical and horizontal histopathological sections by revealing enlarged dermal papillae containing multiple, bright roundish giant cells, corresponding to foamy histiocytes, and giant cells characterized by a dark center surrounded by a highly hyper‐refractile peripheral ring, corresponding to Touton cells. LC‐OCT may represent a valid, noninvasive alternative to histopathological examination in clinically atypical cases of xanthogranuloma.
Keywords: foamy histiocytes, histopathology, line‐field confocal optical coherence tomography, Touton cells, xanthogranuloma
1. INTRODUCTION
Xanthogranuloma (XG) is a benign non‐Langerhans‐cell histiocytosis occurring in 40% to 70% of cases during the first year of life and rarely in adulthood [1, 2]. It appears as single or multiple, asymptomatic, yellow, orange, or reddish papules or nodules. Spontaneous regression often occurs, although XG in adults may persist [3]. Differential diagnosis mainly includes Spitz nevus, balloon cell nevus, and molluscum contagiosum [2]. Histopathologically, XG is characterized by a dense, granulomatous, dermal infiltrate consisting of foamy cells and multinucleated giant histiocytes with wreath‐shaped nuclei and foamy cytoplasm, called “Touton giant cells” [1].
Line‐field confocal optical coherence tomography (LC‐OCT) is a new noninvasive technique for a real‐time, vertical (or en‐coupe), horizontal (or en‐face) and three‐dimensional imaging of the skin at cellular resolution [4, 5]. It is based on a two‐beam interference microscope with line illumination and line detection using a broadband spatially coherent light source and a line‐scan camera [4, 5]. The device consists of a handheld probe connected to a central unit and a monitor where the images are displayed in a gray scale based on the light backscattering from the sample microstructures [4, 5]. Moreover, an integrated dermoscopic camera allows a precise, timely positioning over the examined lesion.
A case of XG evaluated by LC‐OCT is presented along with the correlation of the obtained images with vertical and horizontal histopathology.
2. CASE REPORT
A 47‐year‐old female presented with a 6‐month history of an asymptomatic papule. Skin examination revealed on the pubis a well‐demarcated, yellowish papule of about 0.7 cm (Figure 1A). Polarized dermoscopy at X10 (Illuco IDS‐1100, Tre T Medical, Camposano, Italy) showed yellow clods on an orange‐yellowish background (Figure 1B). Medical history, clinical, and dermoscopic data were consistent with XG.
FIGURE 1.
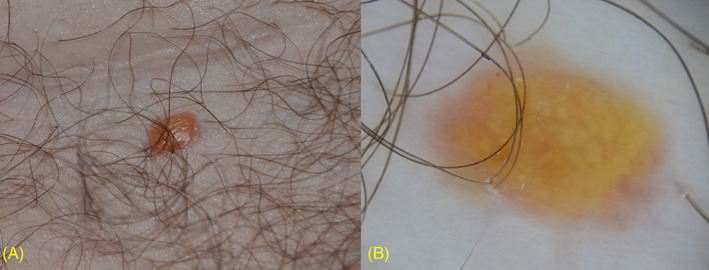
Xanthogranuloma. A, Clinical presentation. B, Polarized dermoscopy (×10) showing yellowish clods on an orange‐yellowish background
LC‐OCT (DeepLive DAMAE Medical, Paris, France; axial resolution 1.1 μm, lateral resolution 1.3 μm, field of view of 1.2 mm × 0.5 mm × 0.5 mm) evaluation revealed a normal epidermis and enlarged dermal papillae, appearing as dark spaces in the vertical sections, and as roundish areas separated by thin septa in the horizontal sections (Figure 2). In both sections, the dermal papillae contained multiple, bright roundish giant cells (diameter up to 70 μm), and giant cells characterized by a dark center surrounded by a highly hyper‐refractile peripheral ring (diameter up to 80 μm).
FIGURE 2.
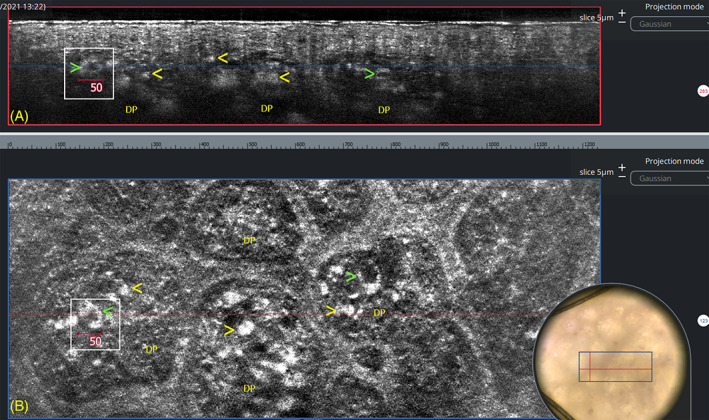
Line‐field confocal optical coherence tomography (LC‐OCT) examination of the central portion of the lesion. Vertical (A, field of view: 1200 × 250 μm) and horizontal (B, field of view: 1200 × 500 μm) sections showing enlarged dermal papillae (DP) containing roundish bright giant cells (yellow arrows) and giant cells showing a dark center surrounded by a highly hyper‐refractile peripheral ring (green arrows). The white squares indicate the same giant cell, measuring about 50 μm, located at the intersection of vertical and horizontal sections. The blue line in A corresponds to the level of the horizontal cut shown in B. The red line in B corresponds to the level of vertical cut shown in A. Insert: Dermoscopy of the examined lesion; the blue rectangle corresponds to the area shown in B (field of view: 1200 × 500 μm)
The lesion was excised for cosmetic reasons and processed to obtain vertical and horizontal histopathological sections that were stained with standard hematoxylin and eosin (H&E). The diagnosis of XG was confirmed, and both sections revealed the presence of enlarged dermal papillae filled with a dense inflammatory infiltrate mainly composed of foamy histiocytes and Touton giant cells, and surrounded by thinned rete ridges.
3. DISCUSSION
LC‐OCT is a novel optical technique that has shown to be useful for the evaluation of some cutaneous disorders such as skin tumors (basal cell carcinoma, malignant melanoma, actinic keratosis), scabies, herpes infection, and aquagenic keratoderma [6, 7, 8, 9, 10]. It allows a real‐time vertical and horizontal “navigation” within a skin volume of 1200 × 500 × 500 μm from the skin surface to the dermis, combining the advantages of reflectance confocal microscopy (RCM) and OCT in terms of resolution, penetration, and image orientation [4, 5, 6].
In our case, LC‐OCT showed an excellent correlation with vertical and horizontal histopathological sections (Figures 3 and 4), being able to show the diagnostic microscopic features of XG. More in detail, the enlarged dermal papillae at vertical and horizontal histopathology appear at LC‐OCT as dark spaces in vertical sections and as roundish areas separated by thin septa in horizontal sections; foamy histiocytes likely correspond at LC‐OCT to roundish, bright giant cells, and Touton cells to giant cells showing a dark center surrounded by a highly hyper‐refractile peripheral ring.
FIGURE 3.
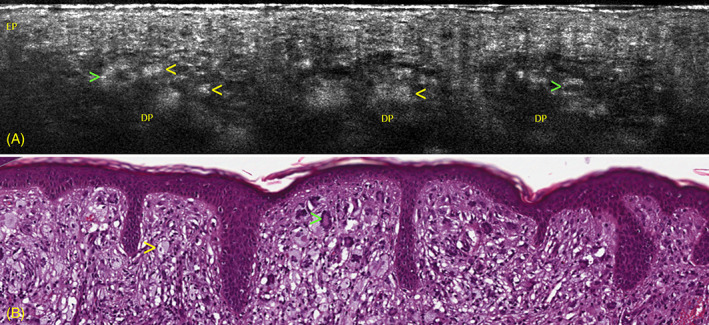
A, Line‐field confocal optical coherence tomography (LC‐OCT) vertical section showing a normal epidermis (EP), and enlarged dermal papillae (DP) appearing as darker areas containing roundish bright giant cells (yellow arrows) and giant cells showing a dark center surrounded by a highly hyper‐refractile peripheral ring (green arrows). B, Corresponding vertical histopathology section showing a dense inflammatory infiltrate of the superficial and mid dermis, mainly composed of foamy histiocytes (yellow arrow) with scattered Touton giant cells (green arrow) (H&E, original magnification ×200)
FIGURE 4.

A, Line‐field confocal optical coherence tomography (LC‐OCT) horizontal section showing enlarged dermal papillae (DP) appearing as roundish areas separated by thin septa and containing roundish bright giant cells (yellow arrows), and giant cells showing a dark center surrounded by a highly hyper‐refractile peripheral ring (green arrows). B, Corresponding horizontal histopathology section at the dermoepidermal junction level revealing the presence of enlarged dermal papillae filled with multiple foamy histiocytes (yellow arrow) and Touton giant cells (green arrow), and surrounded by thinned rete ridges (H&E, original magnification ×200)
Our finding from LC‐OCT in the horizontal mode was comparable to previous studies using RCM [11, 12, 13, 14]. Differently from RCM, LC‐OCT also enables the vertical mode, allowing the possibility to combine images and data from two different observation points.
In conclusion, this article firstly describes the LC‐OCT features of XG. Although further studies on larger series are suggested, this technique may be a valid, noninvasive alternative to histopathological examination in clinically atypical cases. LC‐OCT confirms to represent a further advancement in the noninvasive diagnosis of different cutaneous disorders.
CONFLICT OF INTEREST
The authors declare no potential conflict of interest.
Lacarrubba F, Verzì AE, Puglisi DF, Broggi G, Caltabiano R, Micali G. Line‐field confocal optical coherence tomography of xanthogranuloma: Correlation with vertical and horizontal histopathology. J Cutan Pathol. 2021;48(9):1208–1211. 10.1111/cup.14067
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- 1.Janssen D, Harms D. Juvenile xanthogranuloma in childhood and adolescence: a clinicopathologic study of 129 patients from the Kiel pediatric tumor registry. Am J Surg Pathol. 2005;29(1):21‐28. [DOI] [PubMed] [Google Scholar]
- 2.Micali G, Verzì AE, Quattrocchi E, Ng CY, Lacarrubba F. Dermatoscopy of common lesions in pediatric dermatology. Dermatol Clin. 2018;36(4):463‐472. [DOI] [PubMed] [Google Scholar]
- 3.Ferreira BR, Cardoso JC, Reis JP, Tellechea Ó. Multiple adult‐onset xanthogranuloma, an uncommon diagnosis. An Bras Dermatol. 2017;92(2):294‐295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dubois A, Levecq O, Azimani H, et al. Line‐field confocal optical coherence tomography for high‐resolution noninvasive imaging of skin tumors. J Biomed Opt. 2018;23(10):1‐9. [DOI] [PubMed] [Google Scholar]
- 5.Ruini C, Schuh S, Pellacani G, French L, Welzel J, Sattler E. In vivo imaging of Sarcoptes scabiei infestation using line‐field confocal optical coherence tomography. J Eur Acad Dermatol Venereol. 2020;34(12):e808‐e809. [DOI] [PubMed] [Google Scholar]
- 6.Monnier J, Tognetti L, Miyamoto M, et al. In vivo characterization of healthy human skin with a novel, non‐invasive imaging technique: line‐field confocal optical coherence tomography. J Eur Acad Dermatol Venereol. 2020;34(12):2914‐2921. [DOI] [PubMed] [Google Scholar]
- 7.Ruini C, Schuh S, Sattler E, Welzel J. Line‐field confocal optical coherence tomography‐practical applications in dermatology and comparison with established imaging methods. Skin Res Technol. 2021;27(3):340‐352. 10.1111/srt.12949. [DOI] [PubMed] [Google Scholar]
- 8.Suppa M, Fontaine M, Dejonckheere G, et al. Line‐field confocal optical coherence tomography of basal cell carcinoma: a descriptive study. J Eur Acad Dermatol Venereol. 2021;35(5):1099‐1110. 10.1111/jdv.17078. [DOI] [PubMed] [Google Scholar]
- 9.Lacarrubba F, Verzì AE, Puglisi DF, Micali G. Line‐field confocal optical coherence tomography: a novel, non‐invasive imaging technique for a rapid, in‐vivo diagnosis of herpes infection of the skin. J Eur Acad Dermatol Venereol. 2021;35(6):e404‐e406. 10.1111/jdv.17182. [DOI] [PubMed] [Google Scholar]
- 10.Tognetti L, Fiorani D, Cinotti E, Rubegni P. Tridimensional skin imaging in aquagenic keratoderma: virtual histology by line‐field confocal optical coherence tomography. Int J Dermatol. 2021;60(2):e52‐e54. [DOI] [PubMed] [Google Scholar]
- 11.Haroon A, Shafi S, Rao B. Adult xanthogranuloma diagnosed on reflectance confocal microscopy. J Cutan Pathol. 2017;44(9):809‐810. [DOI] [PubMed] [Google Scholar]
- 12.Lacarrubba F, Ardigò M, Di Stefani A, Verzì AE, Micali G. Dermatoscopy and reflectance confocal microscopy correlations in nonmelanocytic disorders. Dermatol Clin. 2018;36(4):487‐501. [DOI] [PubMed] [Google Scholar]
- 13.Lacarrubba F, Verzì AE, Barresi S, Micali G. Multiple xanthogranulomas in an adult patient: clinical, dermoscopic, reflectance confocal microscopy and histopathological features. BMJ Case Rep. 2019;12(7):e229772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Reilly C, Chuchvara N, Rao B. Diagnosing juvenile xanthogranuloma with reflectance confocal microscopy. JAAD Case Rep. 2020;6(10):975‐976. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


