Abstract
Aim
To compare the efficacy and safety of dinoprostone vaginal insert (DVI) alone versus DVI with adjunctive sweeping of membranes (ASM) for induction of labor (IOL).
Methods
Single‐center, prospective, randomized controlled trial; women with singleton term pregnancies, cervical dilation ≥1 and <3 cm, intact membranes allocated to either DVI or DVI with ASM. The primary outcome was vaginal delivery within 24 h of insertion. Secondary outcomes included mean time from insertion to delivery, tachysystole, operative delivery for non‐reassuring fetal status (NRFS), tocolytics, fetal outcomes, pain information, and subject satisfaction.
Results
One hundred and four received DVI (Group 1) alone and 104 DVI with ASM (Group 2). The rate of vaginal delivery within 24 h was 53% versus 56%, cesarean rate 8.7% versus 10.6% in Groups 1 and 2 respectively. Although the duration of labor was similar in both groups, about 6% of women required additional ripening with dinoprostone vaginal tablets in Group 2 compared to 11.5% in Group 1 (p‐value = 0.2). The frequency of hyperstimulation syndrome, failed induction, analgesic requirements, and fetal outcomes were comparable. The majority (83%–86%) in either cohort were satisfied with their labor experience. Multivariate logistic regression demonstrated a slightly better chance for vaginal delivery within 24 h (odds ratio [OR] 1.22 [95% confidence interval, CI 0.65–2.29]; p‐value 0.53] for DVI with ASM, although statistically insignificant. Younger maternal age and multiparity (OR 10.36 [95% CI 4.88–23.67]; p‐value <0.0001) contributed to successful IOL.
Conclusion
DVI with ASM is at least as efficacious as DVI for cervical ripening with no increase in morbidity. Although DVI with ASM group less often needed additional dinoprostone tablets to complete the process of IOL (p‐value = 0.2), adjunctive sweeping has not been shown to have a significant impact on the duration of labor or mode of delivery.
Keywords: cervical ripening, dinoprostone vaginal insert, hyperstimulation, labor induction, patient comfort, vaginal delivery
Introduction
Induction of labor (IOL) is a common obstetric intervention used globally in 20% to 30% of pregnancies.1, 2, 3 Artificial initiation of labor is offered to pregnant women when the benefits of expeditious delivery in terms of maternal and perinatal outcomes outweigh the risks of continuing the pregnancy. Common indications include prolonged pregnancy, prelabor rupture of the membranes, fetal growth restriction, oligohydramnios, pre‐eclampsia, maternal medical conditions, and so on. Besides, the ARRIVE trial has shown the benefits of IOL at 39 weeks in low‐risk nulliparous women compared with expectant management.4
The physiological processes involved in the initiation of labor are complex and the success of induction is largely determined by the cervical status. Prostaglandins, naturally occurring hormone‐like compounds, facilitate cervical softening, thinning, and dilation resulting in its ripening.5, 6 They stimulate cervical remodeling, as well as other processes such as uterine contractions through different mechanisms. Hence, when cervical ripening has not occurred naturally before labor induction, prostaglandins have been successfully used for ripening. Mechanical methods used (e.g., membrane sweeping, or Foley or double‐balloon catheters or osmotic dilators) function in part by promoting the local release of endogenous prostaglandins.1, 5, 7
Dinoprostone is a synthetic preparation that is chemically identical to naturally occurring prostaglandin E2 (PGE2) while misoprostol, is an another synthetic prostaglandin E1 analogue.6 Dinoprostone is approved in many countries as an endocervical gel, vaginal tablet, and vaginal insert formulations. Dinoprostone vaginal insert (DVI) is FDA approved and provides a low‐dose, controlled‐release at 0.3 mg/h over 12–24 h. Its efficacy and safety have been evaluated in numerous randomized trials. It has been proven to be superior to placebo8, 9, 10 and generally comparable to other dinoprostone formulations or misoprostol.11, 12, 13, 14 The optimal method for ripening the cervix is still uncertain.
Stripping or sweeping the amniotic membranes is commonly practiced to induce labor. Phospholipase A2 activity and prostaglandin F2α (PGF2α) levels increase significantly following membrane stripping.15 There is evidence that it increases the likelihood of spontaneous labor within 48 h and reduces the incidence of induction. A recent 2020 Cochrane review update16, 17 including 44 studies, reported supporting data for 6940 women and their infants comparing membrane sweeping to expectant management or misoprostol or oxytocin. Guidelines generally recommend women should be offered a vaginal examination for membrane sweeping before formal IOL.18, 19, 20
Previous research was mainly focused on the comparison of prostaglandin E2 inserts with other mechanical methods such as Foley catheter, showing differences in efficacy outcomes.21, 22, 23 Little is known about the synergistic effects of prostaglandins and mechanical methods such as slow‐release vaginal prostaglandin E2 inserts and membrane sweeping. We believe that the adjunctive sweeping of membranes (ASM) before DVI insertion will increase the success rate of IOL and shorten the labor process. Thus, it may improve the clinical performance of DVI and patient satisfaction. We have conducted a prospective, randomized controlled trial comparing the efficacy and safety of DVI alone versus a combination of DVI with adjunctive sweeping for term IOL.
Material and Methods
This prospective cohort study was conducted at a single tertiary care medical center, KK Women's & Children's Hospital, Singapore. Women over 21 years of age with a term singleton pregnancy, requiring IOL at 37–42 weeks with an unfavorable cervix (Bishop's score <7, cervical dilatation of ≥1 cm and <3 cm) were eligible for the study. Prior cesarean delivery, history of uterine surgery, sensitivity to dinoprostone, grand multiparity (≥5 previous deliveries), nonvertex presentation of the fetus, ruptured membranes, abnormal cardiotocography (CTG) or suspected fetal compromise, abnormal uterine bleed during pregnancy, contraindications to vaginal delivery (e.g., active herpes, placenta previa), multiple gestations, who require urgent delivery (may benefit from surgical delivery) were exclusion criteria. Clinicians were instructed to omit sweeping in outpatient clinics before scheduling for IOL.
Planned IOL was performed at the Obstetric Monitoring Unit or delivery suite depending on the indication as per institutional protocol. An initial vaginal examination was done to determine the modified Bishop's score. Patients with an unfavorable cervix who consented to participate in the study were randomized to one of two arms: (1) DVI or (2) DVI and ASM. Block randomization of cases was done.
Women in Group 1 were treated with a slow‐release DVI (CERVIDIL® 10 mg Vaginal Delivery System; Ferring, UK), which was placed in the posterior vaginal fornix. Group 2 women had an adjunctive cervical sweep prior to insertion which entailed passage of the examining finger through the cervix so that it can be rotated against the wall of the uterus beyond the internal cervical os, thereby stripping the amnion away from the decidua. Electronic fetal monitoring was done for an hour after the insertion of DVI and repeated 4–6 h later. The insert was left in place for 24 h, or until active labor started or else there was hyperstimulation or spontaneous rupture of membranes. In both the groups, if the cervix was found to be ≥3 cm dilated on follow‐up examination, amniotomy was performed and oxytocin augmentation was started when contractions or progress were deemed inadequate. Continuous fetal monitoring by CTG was started after amniotomy. Cases where amniotomy was not possible after 24 h of DVI insertion were considered failed IOL and were managed with an additional trial of cervical ripening either with dinoprostone vaginal tablet or mechanical ripening using a balloon catheter.
Data were collected on women's characteristics, admission examination, continuous monitoring of uterine contractions, as well as subsequent labor management (e.g., oxytocin regimen and labor progression) and birth outcomes. After delivery, a member of the study team interviewed the patients. Information collected included patients' views on pain felt during the induction process, overall satisfaction, comments, and whether they would recommend their mode of induction to other women. A visual analog scale (Wong‐Baker Faces Pain Rating Scale) and satisfaction chart were shown to the subjects during the verbal survey to aid in the process.
Primary outcome: Successful IOL was defined as vaginal delivery within 24 h of initiation by the induction agent.
Secondary outcomes: Comparison between two study cohorts with respect to mean time from insertion to delivery, tachysystole, need for oxytocin for augmentation of labor, need for instrumental delivery or cesarean section, need for analgesia, and patient satisfaction.
Onset of labor was defined as regular painful contractions (3 in 10 min) resulting in progressive effacement and dilatation of the cervix.
Uterine hyperstimulation was diagnosed if contraction frequency exceeded 5 in 10 min or contractions exceeded 2 min.24
Late decelerations, moderate and severe variable decelerations, and bradycardia were considered abnormalities on the fetal heart rate tracing. Factors affecting successful labor induction were analyzed separately.
All statistical analyses were conducted with “R” software. The sample size was calculated to be approximately 100 women in each group to achieve a statistically 80% power (α 0.05) to show a 20% reduction in the meantime from insertion to delivery from 25.2 h in DVI alone group to 20.2 h in the DVI with membrane sweeping group. The effect size of 20% reduction is a hypothetical estimate that is expected to be clinically meaningful to differentiate the two methods. Chi‐square test was used for categorical variables. Student's t‐test and Mann–Whitney U test were used for continuous variables comparing mean and median, respectively. Categorical variables were expressed as percentages and continuous variables as mean ± standard deviation or median with interquartile range (IQR). Multivariate logistic regressions were performed to assess the correlation between normal vaginal delivery within 24 h and risk factors. p < 0.05 was considered to indicate statistical significance.
The study was approved by the SingHealth Centralised Institutional Review Board and registered with the ID number 2018/2338.
Results
During the study period, 1613 women presenting for term IOL were contacted. A total of 208 women met the inclusion criteria and were included in the study, of them 104 underwent cervical ripening with a DVI while the rest of 104 had adjunctive cervical sweeping prior to insertion of DVI (Figure 1). The demographic and obstetric characteristics of both cohorts are shown in Table 1. Both groups were comparable with respect to maternal age, race, pregestational BMI, parity, and GA at induction. There were no differences in the indications for IOL between them as well.
FIGURE 1.
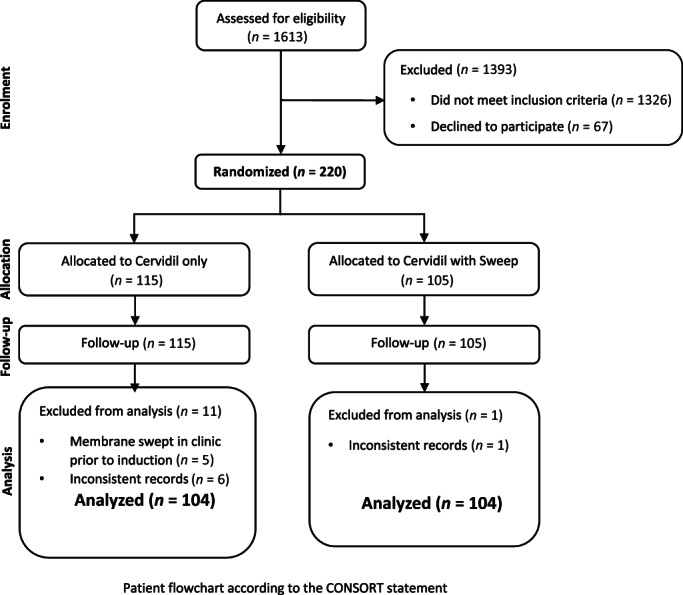
Patient flowchart according to the CONSORT statement
TABLE 1.
Demographic characteristics
| Characteristics | DVI only (n = 104) | DVI with sweep (n = 104) |
|---|---|---|
| Maternal age (years), mean ± SD | 30.4 ± 5.35 | 31.0 ± 5.12 |
| Advanced maternal age (≥35 years) | 22 (21.2) | 28 (26.9) |
| Chinese race | 55 (52.9) | 47 (45.2) |
| Malay | 24 (23.1) | 33 (31.7) |
| Indian | 13 (12.5) | 8 (7.69) |
| Others | 12 (11.5) | 16 (15.4) |
| Body mass index, mean ± SD | 25.2 ± 5.35 | 25.9 ± 6.31 |
| BMI ≥ 30 | 18 (17.3) | 27 (26.0) |
| BMI ≥ 40 | 1 (0.962) | 3 (2.88) |
| Nulliparous | 64 (61.5) | 62 (59.6) |
| Multiparous | 40 (38.5) | 42 (40.4) |
| GA at induction (weeks), median (IQR) | 39.2 (1.6) | 39.3 (1.7) |
| Bishop score, median (IQR) | 4 (2) | 4 (2) |
| Indications | ||
| Term | 25 (24.0) | 22 (21.2) |
| Gestational/pre‐existing diabetes | 23 (22.1) | 26 (25.0) |
| Post date | 19 (18.3) | 17 (16.3) |
| Macrosomia | 17 (16.3) | 12 (11.5) |
| Amniotic fluid index <6 | 9 (8.65) | 11 (10.6) |
| Maternal request | 5 (4.81) | 6 (5.77) |
| Reduced fetal movement | 3 (2.88) | 10 (9.6) |
| Pre‐eclampsia/hypertension | 3 (2.88) | 5 (4.81) |
| Intrauterine growth restriction | 1 (0.962) | 0 (0.0) |
| Advanced maternal age | 1 (0.962) | (0.0) |
Note: Data presented as n (%).
Abbreviations: BMI, body mass index; DVI, dinoprostone vaginal insert; GA, gestational age; SD, standard deviation.
The primary efficacy outcome variable was delivery within 24 h of insertion of the induction agent. Both induction methods were equally effective in terms of achieving vaginal delivery within 24 h of insertion. Also, the number of women undergoing cesarean section within 24 h of insertion was not significantly different between the two groups. The time interval from the insertion of DVI to the onset of regular uterine contractions and the insertion‐to‐delivery interval were not different between the groups (Table 2). There was no significant difference in the mode of delivery between the two groups.
TABLE 2.
Labor outcomes
| Outcomes | DVI only (n = 104) | DVI with sweep (n = 104) | p‐value |
|---|---|---|---|
| Primary labor outcomes | |||
| Vaginal delivery within 12 h | 20 (19.2) | 16 (15.4) | 0.58 |
| Vaginal delivery within 24 h | 55 (52.9) | 59 (56.7) | 0.67 |
| Cesarean section within 24 h | 9 (8.65) | 11 (10.6) | 0.81 |
| Delivery after 24 h | 40 (38.5) | 34 (32.7) | 0.46 |
| Secondary labor outcomes | |||
| Duration: insertion to onset of labor (h)a | 10.7 (10.9) | 10.6 (9.2) | 0.99 |
| Duration: insertion to full dilatation (h)a | 17.6 (13.6) | 18.8 (10.8) | 0.64 |
| Duration: insertion to delivery (h)a | 20.4 (16.2) | 21.3 (14.8) | 0.76 |
| Duration: onset of labor to delivery (h)a | 9.1 (8.1) | 8.9 (8.3) | 0.35 |
| Need for oxytocin | 50 (48.1) | 61 (58.7) | 0.16 |
| Need for dinoprostone vaginal tablet | 12 (11.5) | 6 (5.8) | 0.22 |
Note: Data presented as n (%).
Abbreviation: DVI, dinoprostone vaginal insert.
Data presented as median (IQR).
There were no differences between the two groups regarding the frequency of uterine hyperstimulation, the occurrence of abnormal fetal heart rate patterns during the first stage of labor, Apgar scores, or umbilical artery pH values. Likewise, oxytocin and analgesic requirements were similar in both groups. Twelve women required additional dinoprostone vaginal tablets in Group 1 compared to six in Group 2 (p‐value = 0.2).
A total of 12 women in Group 1 experienced uterine hyperstimulation (Table 3), of which, in 9 of these women, it resolved immediately on removal of the insert and/or administration of a tocolytic; a β2‐sympathomimetic drug (Terbutaline). Four women required immediate instrumental or cesarean birth within 1 h. Two newborns required observation in a special care nursery. In Group 2, 14 women experienced hyperstimulation syndrome. Five women required removal of insert, in three of these women, removal of the insert was sufficient to stop the uterine hyperstimulation, and no tocolytic therapy was required. In six cases, a tocolytic was necessary to end the hyperstimulation. Three mothers required immediate delivery for abnormal fetal heart rate patterns. One woman induced for gestational diabetes mellitus experienced uterine hyperstimulation associated with an abnormal fetal heart rate pattern and tachysystole abated after removal of insert and tocolytic. She had a cesarean section 8 h later for non‐reassuring fetal status, the baby was under observation in the nursery for 24 h without adverse outcome. Three women in each cohort did not require any interventions.
TABLE 3.
Perinatal outcomes and side effects profile
| Outcomes | DVI only (n = 104) | DVI with sweep (n = 104) | p‐value |
|---|---|---|---|
| Birth weight (g), ±SD | 3428.8 ± 378.3 | 3164.2 ± 380.6 | 0.11 |
| 5 min APGAR < 7 | 0 (0.0) | 1 (0.9) | 1 |
| Cesarean section for NRFS | 8 (7.7) | 7 (6.7) | 1 |
| Failed induction | 13 (12.5) | 13 (12.5) | 1 |
| • Required dinoprostone vaginal tablet | 9/13 (69.2) | 6/13 (46.2) | 0.5 |
| • Cesarean section | 9/13 (69.2) | 9/13 (69.2) | 1 |
| • Instrumental delivery | 4/13 (30.8) | 0/13 | 0.13 |
| • Normal vaginal delivery | 0/13 | 4/13 (30.8) | 0.13 |
| Post‐partum hemorrhage | 1 (0.9) | 0 (0.0) | 1 |
| Uterine rupture | 0 (0.0) | 0 (0.0) | NA |
| Fever | 25 (24.0) | 23 (22.1) | 0.87 |
| Vomiting | 7 (6.7) | 5 (4.8) | 0.77 |
| Hyperstimulation syndrome | 12 (11.5) | 14 (13.5) | 0.83 |
| • Required removal of DVI only | 2 (16.7) | 3 (21.4) | 1 |
| • Required tocolysis only | 2 (16.7) | 6 (42.8) | 0.31 |
| • Required removal of DVI and tocolysis | 5 (41.7) | 2 (14.3) | 0.51 |
| • No intervention | 3 (25) | 3 (21.4) | 1 |
| • Required immediate delivery | 4 (33.3) | 3 (21.4) | 0.81 |
| • Cord pH ≤7.1 | 2/8 (25) | 5/10 (50) | 0.55 |
| • Required SCN/NICU stay | 2 (16.7) | 3 (21.4) | 1 |
| Tachysystole | 26 (25.0) | 28 (26.9) | 0.87 |
| Required removal of DVI | 18/26 (69.2) | 18/28 (64.3) | |
| Required tocolysis | 1/26 (3.85) | ||
| Patient satisfaction | |||
| Pain scorea | 1 (4) | 2 (2) | 0.03 |
| Discomfort scorea | 5 (3.3) | 5 (4) | 0.65 |
| Recommend this method | 86 (82.7) | 83 (79.8) | 0.72 |
Note: Data presented as n (%).
Abbreviations: DVI, dinoprostone vaginal insert; NICU, neonatal intensive care unit; NRFS, non‐reassuring fetal status; SCN, special care nursery; SD, standard deviation.
Data presented as median (IQR).
Women from Group 2 who underwent membrane sweeping before DVI insertion did report additional discomfort or pain from the procedure compared to Group 1 (p‐value = 0.03) but still, they did not require additional analgesics and the majority (83%) of participants were satisfied with their labor experience and would choose or recommend this method of IOL (Table 3).
Factors that significantly increased the likelihood of achieving the primary outcome of vaginal delivery within 24 h were younger maternal age and multiparity. DVI with adjunctive membrane sweeping was associated with a slightly increased likelihood of vaginal delivery (OR 1.22 [0.65–2.29] p = 0.5), although not statistically significant (Table 4).
TABLE 4.
Multivariate logistic regression for vaginal delivery within 24 h
| Factors | ORs | 95% CI | p‐value |
|---|---|---|---|
| Allocation | 1.22 | 0.65–2.29 | 0.53 |
| Maternal age | 0.88 | 0.82–0.94 | 0.0003 |
| Parity | 10.36 | 4.88–23.67 | <0.0001 |
| Booking BMI | 0.96 | 0.90–1.01 | 0.14 |
| Birth weight | 0.9 | 0.99–1 | 0.01 |
| GA at delivery | 1.16 | 0.82–1.65 | 0.39 |
Abbreviations: BMI, body mass index; CI, confidence interval; ORS, odds ratios; GA, gestational age.
Discussion
“The spontaneous onset of labour is a robust and effective mechanism which is preceded by the maturation of several fetal systems and should be given every opportunity to operate on its own. We should only induce labour when we are sure that we can do better”—Alec Turnbull, 1976.25 The successful IOL and achieving vaginal delivery will reduce the percentage of cesarean births. Despite the availability of numerous mechanical and pharmacological methods, the best intervention still eludes us as outcomes may vary according to maternal and obstetric characteristics. The present study was undertaken to assess whether the combination of the routine obstetric practice of sweeping the membranes and prostaglandin E2 vaginal insert is superior to prostaglandin E2 without sweeping the membranes to achieve vaginal delivery within 24 h.
Sweeping of the amniotic membranes for inducing labor was first documented by James Hamilton, in England in 1810.26 Several studies have reported that membrane sweeping is associated with higher rates of spontaneous vaginal delivery, shorter induction‐to‐delivery interval, reduced likelihood of post‐term pregnancy, and a decreased need for IOL.15, 16, 27, 28, 29 A Cochrane review in 200516 demonstrated that membrane sweeping does not increase the risk of maternal and neonatal infection. The “STRIP‐G” study confirmed that stripping was a safe procedure in women who were even found to be carriers of Streptococcus agalactiae (Group B Streptococcus).30
DVI (Cervidil®; Propess®), a retrievable vaginal pessary—a controlled‐release drug delivery device, is approved in many countries worldwide for inducing cervical ripening in patients at term prior to labor induction. The effectiveness of DVI has been demonstrated in a vast range of randomized clinical trials in women at term.8, 9, 10, 11, 12, 13, 14 The insert is well tolerated, with generally favorable maternal, fetal, and neonatal outcomes. Sustained constant slow release of PGE2 from the vaginal insert with or without prior sweep was an important advantage of this induction method in terms of controlling the labor and in particular rapidly reversing uterine hyperstimulation through easy retrieval of the vaginal insert.
The present study demonstrated both DVI alone or DVI with ASM are effective and safe for cervical ripening with no increase in morbidity. Additional membrane sweeping was expected to improve the chances for vaginal delivery within 24 h by the release of additional local endogenous prostaglandins, however statistical significance and hence its clinical merits could not be proven. There were no additional maternal or fetal morbidities reported in either of the cohorts. There were no significant additional reports of uterine hyperstimulation or tachysystole with adjunctive membrane sweeping. No additional emergent instrumental or cesarean births were required in Group 2 women with hyperstimulation confirming the safety of the induction method.
The addition of sweeping did not compromise patient satisfaction although labor was perceived as more painful, there were no additional analgesic requirements in Group 2. Measuring patient satisfaction allowed patients to evaluate received services and treatments. It also helps to identify possible problems and suggests ways of improving the quality of care or interventions. There have been no randomized studies so far reporting efficacy and safety of this mechanical method, that is, membrane sweeping, with DVI for term IOL. To our knowledge, this is the first prospective randomized trial comparing DVI alone and DVI with prior sweeping.
The strength of this study lies in its prospective, randomized control design, enabling complete and thorough data collection. Another important strength of this study is being done at a single center where the structured, detailed protocol for labor induction with DVI was followed and all women were treated similarly. This attenuates any biases related to different management approaches.
Limitation of this study was that the patients and clinicians were not blinded to the allocation of the study groups because of the nature of the intervention. This study was likely underpowered to evaluate the benefits of the addition of sweeping to DVI for IOL, future studies with larger cohorts are needed to better assess these issues. Better results may be possible if ASM is performed and prostaglandin insert (PGI) inserted 12 h later but such hypotheses need to be tested in clinical trials.
Conclusion
Results of this randomized trial showed that both DVI with membrane sweeping and DVI alone were effective in the IOL. Adjunctive sweeping although safe does not benefit in terms of achieving successful vaginal delivery within 24 h earlier compared to DVI alone. Patient satisfaction scores were comparable in both groups.
Conflict of Interest
This study was funded by a commercial manufacturer of the dinoprostone slow release pessary product used for this study (Cervidil, Ferring, UK).
Author contributions
Anju Bhatia and George SH Yeo contributed to the concept, design of trial, acquisition, analysis of data, as well as drafting and critical revision of this manuscript. Manisha Mathur and Shephali Tagore were involved in concept, design and provided administrative support. Beatrice and Joanne helped in the acquisition and analysis of data. Li Mingyue was involved in designing the concept of trial. Puay Ling provided administrative support and helped in the recruitment of patients. Tai Wai and George Yeo obtained funding. Sabaratnam Arulkumaran contributed to concept design and critically revised the manuscript.
Acknowledgments
We would like to thank all women and obstetricians who participated in this trial as well as and midwives of Obstetric Monitoring Unit and delivery suite for their excellent work. We would also like to acknowledge Du Rouchen for helping us with the data analysis for this study.
Data Availability Statement
Research data are not shared.
References
- 1.EURO‐PERISTAT Project, with SCPE EUROCAT EURONEOSTAT . European Perinatal Health Report; data from 2004; 2008.
- 2.Martin JA, Hamilton BE, Ventura SJ, Osterman MJK, Kirmeyer S, Mathews TJ, et al. Births: final data for 2009. Natl Vital Stat Rep. 2011;60:1–70. [PubMed] [Google Scholar]
- 3.The Health and Social Care Information Centre . NHS Maternity Statistics, England 2007–8; 2010. http://www.ic.nhs.uk/pubs/maternity0910
- 4.Grobman WA, Rice MM, Reddy UM, Tita ATN, Silver RM, Mallett G, et al. Labor induction versus expectant management in low‐risk nulliparous women. N Engl J Med. 2018;379:513–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tenore JL. Methods for cervical ripening and induction of labor. Am Fam Physician. 2003;67:2123–8. [PubMed] [Google Scholar]
- 6.Bakker R, Pierce S, Myers D. The role of prostaglandins E1 and E2, dinoprostone, and misoprostol in cervical ripening and the induction of labor: a mechanistic approach. Arch Gynecol Obstet. 2017;296:167–79. [DOI] [PubMed] [Google Scholar]
- 7.Leduc D, Biringer A, Lee L, Dy J. SOGC clinical practice guideline: induction of labour. J Obstet Gynaecol Can. 2013;35:840–57. [DOI] [PubMed] [Google Scholar]
- 8.Rayburn WF, Wapner RJ, Barss VA, Spitzberg E, Molina RD, Mandsager N, et al. An intravaginal controlled‐release prostaglandin E2 pessary for cervical ripening and initiation of labor at term. Obstet Gynecol. 1992;79:374–9. [DOI] [PubMed] [Google Scholar]
- 9.Witter FR, Mercer BM. Improved intravaginal controlled‐release prostaglandin E2 insert for cervical ripening at term. J Matern Fetal Med. 1996;5:64–9. [DOI] [PubMed] [Google Scholar]
- 10.Witter FR, Rocco LE, Johnson TRB. A randomized trial of prostaglandin E2 in a controlled‐release vaginal pessary for cervical ripening at term. Am J Obstet Gynecol. 1992;166:830–4. [DOI] [PubMed] [Google Scholar]
- 11.Wing DA, Brown R, Plante LA, Miller H, Rugarn O, Powers BL. Misoprostol vaginal insert and time to vaginal delivery: a randomized controlled trial. Obstet Gynecol. 2013;122(2 Pt 1):201–9. [DOI] [PubMed] [Google Scholar]
- 12.Thomas J, Fairclough A, Kavanagh J, Kelly AJ. Vaginal prostaglandin (PGE2 and PGF2a) for induction of labour at term. Cochrane Database Syst Rev. 2014;19:CD003101. [DOI] [PubMed] [Google Scholar]
- 13.Zeng X, Zhang Y, Tian Q, Xue Y, Sun R, Zheng W, et al. Efficiency of dinoprostone insert for cervical ripening and induction of labor in women of full‐term pregnancy compared with dinoprostone gel: a meta‐analysis. Drug Discov Ther. 2015;9:165–72. [DOI] [PubMed] [Google Scholar]
- 14.Alfirevic Z, Keeney E, Dowswell T, Welton NJ, Dias S, Jones LV, et al. Labour induction with prostaglandins: a systematic review and network meta‐analysis. BMJ. 2015;350:h217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McColgin SW, Bennett WA, Roach H, Cowan BD, Martin JN Jr, Morrison JC. Parturitional factors associated with membrane stripping. Am J Obstet Gynecol. 1993;169:71–7. [DOI] [PubMed] [Google Scholar]
- 16.Boulvain M, Stan C, Irion O. Membrane sweeping for induction of labour. Cochrane Database Syst Rev. 2005;2005:CD000451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Finucane EM, Murphy DJ, Biesty LM, Gyte GML, Cotter AM, Ryan EM, et al. Membrane sweeping for induction of labour. Cochrane Database Syst Rev. 2020;2:CD000451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.ACOG Practice Bulletin No 107. Induction of labour. Obstet Gynecol. 2009;114:386–97. [DOI] [PubMed] [Google Scholar]
- 19.National Institute for Health and Care Excellence . Inducing Labour. CG70. NICE; 2008. https://www.nice.org.uk/guidance/cg70 [PubMed]
- 20.Leduc D, Biringer A, Lee L, Dy J, Corbett T, Duperron L, et al. Induction of labour. J Obstet Gynaecol Can. 2013;35:840–57. [DOI] [PubMed] [Google Scholar]
- 21.Cromi A, Ghezzi F, Agosti M, Serati M, Uccella S, Arlant V, et al. Is transcervical Foley catheter actually slower than prostaglandins in ripening the cervix? A randomized study. Am J Obstet Gynecol. 2011;204:338.e1–7. [DOI] [PubMed] [Google Scholar]
- 22.Edwards RK, Szychowski JM, Berger JL, Petersen M, Ingersoll M, Bodea‐Braescu AV, et al. Foley catheter compared with the controlled release dinoprostone insert: a randomized controlled trial. Obstet Gynecol. 2014;123:1280–7. [DOI] [PubMed] [Google Scholar]
- 23.Wang H, Hong S, Liu Y, Duan Y, Yin H. Controlled release dinoprostone insert versus Foley catheter for labor induction: a meta‐analysis. J Matern Fetal Neonatal Med. 2016;29:2382–8. [DOI] [PubMed] [Google Scholar]
- 24.Egarter C, Husslein P, Rayburn W. Uterine hyperstimulation after prostaglandin E2 therapy: tocolytic treatment in 181 cases. Am J Obstet Gynecol. 1990;163:794–9. [DOI] [PubMed] [Google Scholar]
- 25.Chodankar R, Sood A, Gupta J. An overview of the past, current and future trends for cervical ripening in induction of labour. Obstet Gynaecol. 2017;19:219–26. [Google Scholar]
- 26.Krammer J, O'Brien WF. Mechanical methods of cervical ripening. Clin Obstet Gynecol. 1995;38:280–6. [DOI] [PubMed] [Google Scholar]
- 27.De Miranda E, Van Der Bom JG, Bonsel GJ, Bleker OP, Rosendaal FR. Membrane sweeping and prevention of post‐term pregnancy in low risk pregnancies: a randomized controlled trial. BJOG. 2006;113:402–8. [DOI] [PubMed] [Google Scholar]
- 28.Tan PC, Jacob R, Omar SZ. Membrane sweeping at initiation of formal labor induction: a randomized controlled trial. Obstet Gynecol. 2006;107:569–77. [DOI] [PubMed] [Google Scholar]
- 29.Heilman E, Sushereba E. Amniotic membrane sweeping. Semin Perinatol. 2015;39:466–70. [DOI] [PubMed] [Google Scholar]
- 30.Kabiri D, Hants Y, Yarkoni TR, Shaulof E, Friedman SE, Paltiel O, et al. Antepartum membrane stripping in GBS carriers, is it safe? (The STRIP‐G study). PLoS One. 2015;10:e0145905. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Research data are not shared.


