Abstract
Background
Transthoracic defibrillation is a potentially life‐saving treatment for people with ventricular fibrillation (VF) and haemodynamically unstable ventricular tachycardia (VT). In recent years, biphasic waveforms have become more commonly used for defibrillation than monophasic waveforms. Clinical trials of internal defibrillation and transthoracic defibrillation of short‐duration arrhythmias of up to 30 seconds have demonstrated the superiority of biphasic waveforms over monophasic waveforms. However, out‐of‐hospital cardiac arrest (OHCA) involves a duration of VF/VT of several minutes before defibrillation is attempted.
Objectives
To determine the efficacy and safety of biphasic defibrillation waveforms, compared to monophasic, for resuscitation of people experiencing out‐of‐hospital cardiac arrest.
Search methods
We searched the following electronic databases for potentially relevant studies up to 10 September 2014: the Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE and EMBASE. Also we checked the bibliographies of relevant studies and review articles, contacted authors of published reviews and reviewed webpages (including those of device manufacturers) relevant to the review topic. We handsearched the abstracts of conference proceedings for the American Heart Association, American College of Cardiology, European Society of Cardiology, European Resuscitation Council, Society of Critical Care Medicine and European Society of Intensive Care Medicine. Regarding language restrictions, we did not apply any.
Selection criteria
We included randomised controlled trials (RCTs) that compared biphasic and monophasic waveform defibrillation in adults with OHCA. Two review authors independently screened the literature search results.
Data collection and analysis
Two review authors independently extracted data from the included trials and performed 'Risk of bias' assessments. We resolved any disagreements by discussion and consensus. The primary outcome was the risk of failure to achieve return of spontaneous circulation (ROSC). Secondary outcomes included risk of failure to revert VF to an organised rhythm following the first shock or up to three shocks, survival to hospital admission and survival to discharge.
Main results
We included four trials (552 participants) that compared biphasic and monophasic waveform defibrillation in people with OHCA. Based on the assessment of five quality domains, we identified two trials that were at high risk of bias, one trial at unclear risk of bias and one trial at low risk of bias. The risk ratio (RR) for failure to achieve ROSC after biphasic compared to monophasic waveform defibrillation was 0.86 (95% CI 0.62 to 1.20; four trials, 552 participants). The RR for failure to defibrillate on the first shock following biphasic defibrillation compared to monophasic was 0.84 (95% CI 0.70 to 1.01; three trials, 450 participants); and 0.81 (95% CI 0.61 to 1.09; two trials, 317 participants) for one to three stacked shocks. The RR for failure to achieve ROSC after the first shock was 0.92 (95% CI 0.81 to 1.04; two trials, 285 participants). Biphasic waveforms did not reduce the risk of death before hospital admission (RR 1.05, 95% CI 0.90 to 1.23; three trials, 383 participants) or before hospital discharge (RR 1.05, 95% CI 0.78 to 1.42; four trials, 550 participants). There was no statistically significant heterogeneity in any of the pooled analyses. None of the included trials reported adverse events.
Authors' conclusions
It is uncertain whether biphasic defibrillators have an important effect on defibrillation success in people with OHCA. Further large studies are needed to provide adequate statistical power.
Plain language summary
Type of electrical shock to restart the heart in a non‐hospitalised person whose heart stops beating
Background
When a person's heart stops beating it may be necessary to deliver an electrical shock (called 'defibrillation') to the person's chest to restart their heart. Two electrodes are placed on the person's chest to allow the defibrillator to deliver the electrical shock. Historically, the electrical current applied to the chest has travelled in one direction between the electrodes. More recently, defibrillators have been designed to send the electrical pulse in one direction and then in the reverse direction. This is known as a 'biphasic' waveform.
Objective
Cochrane researchers conducted this review to determine whether the newer biphasic waveform defibrillators are better at restarting a person's heart than the 'monophasic' waveform defibrillators previously used.
Study characteristics
We searched the literature up to 10 September 2014 and tried to find all available research (published and unpublished) that compared these two types of defibrillators. We only included trials with a high‐quality study design to avoid the possibility of inaccurate results.
Key results
Four trials (552 participants) met the inclusion criteria of our review. Several included trials were potentially at risk of misleading results due to features of their study design. When we combined these trial results, we found that using the newer biphasic waveform defibrillators may be associated with lower failure rates of restarting a person's heart, but these results were imprecise. There was no difference in the number of people who were alive on arrival at the hospital or who were discharged from the hospital alive. No included trials reported on side effects or operator safety.
Conclusion
We are uncertain as to whether biphasic defibrillators have an important effect on being able to restart a person's heart because the results were imprecise.
Background
Description of the condition
Ischaemic heart disease is the leading cause of death worldwide (WHO 2014). About 25% of people with ischaemic heart disease present with sudden cardiac arrest (Keuper 2007). In Europe alone there are an estimated 275,000 out‐of‐hospital cardiac arrests (OHCAs) per year due to coronary artery disease where resuscitation is attempted (Atwood 2005).
The incidence of ventricular fibrillation (VF) or ventricular tachycardia (VT) as the first recorded rhythm in people with OHCA is difficult to determine, with rates as low as 16.8% (Nishiuchi 2003) and as high as 63.3% reported (Waalewijn 1998). With the deployment of automated external defibrillators (AEDs), first responders can access people with OHCA before emergency medical services arrive. The incidence of VF/VT as the first recorded rhythm may be as high as 85% (Holmberg 2000). VF/VT is the most salvageable rhythm in cardiac arrest and electrical countershock or "defibrillation", the definitive treatment, can be given out of hospital.
Description of the intervention
Transthoracic defibrillation is a potentially life‐saving treatment for people with VF and haemodynamically unstable VT. VF is characterised by chaotic electrical activity in the person's heart. The resulting absence of coordinated myocardial contraction leads to cessation of forward blood flow from the heart. The lack of cardiac output quickly leads to cerebral, myocardial and end organ death.
In recent years biphasic waveforms have become more commonly used for defibrillation than monophasic waveforms. Biphasic waveforms are characterised by an initial positive current flow followed by a reversal to negative current flow. Extensive research with implantable defibrillators and transthoracic defibrillation of short‐duration VF/VT has shown that these waveforms are able to defibrillate with less energy than monophasic, requiring lower voltage and, hence, smaller and lighter battery and capacitor banks (Bardy 1996). However, more expensive, biphasic waveform technology may be preferred if the results in short duration VF/VT can be replicated in people with OHCA.
How the intervention might work
Clinical trials of internal defibrillation and transthoracic defibrillation of short‐duration arrhythmias of up to 30 seconds have demonstrated the superiority of biphasic waveforms over monophasic ones (Bardy 1996; Echt 1993; Greene 1995; Herre 1998; Mittal 1999; Szili‐Torok 2002). Biphasic waveforms can reduce the risk of persistent VF by up to 81% compared to monophasic waveforms of the same energy (Faddy 2003). However, OHCA involves a duration of VF/VT of several minutes before defibrillation is attempted. Success of defibrillation falls by as much as 7% for each minute the VF/VT goes untreated (Holmberg 2000; Larsen 1993). Biphasic waveforms are increasingly being used for transthoracic defibrillation of people with long‐duration OHCA.
Why it is important to do this review
With the proliferation of biphasic waveform defibrillators, research that compares these waveforms to the traditional monophasic waveforms has emerged. Despite clinical trial findings that suggest biphasic defibrillation waveforms are more effective in reversing lethal arrhythmias and improving survival from OHCA, a recent retrospective case review following introduction of biphasic waveform defibrillators showed no improvement in survival rates with biphasic waveforms (Freeman 2008).
Objectives
To determine the efficacy and safety of biphasic defibrillation waveforms, compared to monophasic, for resuscitation of people experiencing out‐of‐hospital cardiac arrest.
Methods
Criteria for considering studies for this review
Types of studies
We included randomised controlled trials (RCTs), either published or unpublished, that compared biphasic and monophasic waveforms in the treatment of people with out‐of‐hospital cardiac arrest (OHCA). We included RCTs that performed randomisation of individual patients, cluster randomisation of geographic locations or daily randomisation of ambulance defibrillators.
Types of participants
Adults experiencing OHCA of presumed cardiac origin with ventricular fibrillation (VF)/ventricular tachycardia (VT) as the presenting rhythm.
Types of interventions
We included trials that compared any type of biphasic waveform defibrillation pulse with any monophasic pulse. As cardiac arrest is treated according to standard protocols (de Latorre 2001), there was little chance that concomitant medications or therapies were used selectively in either trial group.
Types of outcome measures
Primary outcomes
Overall rate of return of spontaneous circulation (ROSC).
Secondary outcomes
First shock efficacy.
Efficacy of up to three shocks.
Survival to hospital discharge.
Delivered current.
Adverse outcomes, such as ST segment deviation, elevation of cardiac markers and assessment of left ventricular function.
Search methods for identification of studies
Electronic searches
We searched the following databases up to 10 September 2014:
the Cochrane Central Register of Controlled Trials (CENTRAL, Issue 8 of 12, 2014) in the Cochrane Library.
MEDLINE (OVID, 1946 to August Week 4 2014).
EMBASE (OVID, 1980 to 2014 Week 36).
We applied the RCT filter for MEDLINE, which is the Cochrane sensitivity‐maximising RCT filter, and for EMBASE, terms as recommended in the Cochrane Handbook for Systematic Reviews of Interventions (Lefebvre 2011).
Biphasic transthoracic defibrillators were developed from the early‐ to mid‐1990s. Therefore, we performed electronic searches for the period 1990 to 10 September 2014. We did not apply any language restrictions.
The search strategies are listed in Appendix 1.
Searching other resources
We reviewed bibliographies of relevant studies and review articles, contacted authors of published reviews and reviewed webpages (including those of device manufacturers) relevant to the review topic.
We handsearched the abstracts of conference proceedings for the American Heart Association, American College of Cardiology, European Society of Cardiology, European Resuscitation Council, Society of Critical Care Medicine and European Society of Intensive Care Medicine. We conducted the searches for the years 2000 to 2007.
Data collection and analysis
Selection of studies
The two review authors, SCF and PAJ, independently selected trials for inclusion in this Cochrane review. We have presented the search strategy results as a flowchart based on the Quality of Reporting of Meta‐analyses (QUOROM) statement (Moher 1999). We independently assessed the titles and abstracts identified by the search strategy. We obtained the full‐text articles of potentially relevant studies to determine whether or not they satisfied the inclusion criteria. In cases of disagreement, we resolved these by consensus.
Where more than one publication of a trial existed, we only included the publication with the most complete data unless the various publications contained mutually exclusive data. Where publications did not report important data or reported data that were inconsistent with our pre‐defined outcomes, we attempted to contact the original study authors to obtain the necessary information.
Data extraction and management
We independently extracted the following data using a standardised data collection form. We resolved any disagreements by discussion and consensus.
General Information: author, title and journal.
Interventions: type and dose of biphasic and monophasic waveforms.
Study quality: particularly the criteria we defined in the 'Assessment of risk of bias in included studies' section.
Participants: baseline characteristics of study groups, and inclusion and exclusion criteria.
Covariates: pre‐defined variables that may affect the pooled analysis, including duration of cardiac arrest and proportion receiving bystander cardiopulmonary resuscitation (CPR).
Outcomes: we collected dichotomous data on the number of outcomes and total number of subjects. We collected continuous data on the mean and standard deviation values and the number of subjects.
Assessment of risk of bias in included studies
We independently assessed each included trial for risk of bias. In the case of disagreement, we resolved any issues by consensus. We assessed the risk of bias with particular attention to the four main sources of systematic bias in trials: selection bias, performance bias, attrition bias and detection bias.
Selection bias
Randomisation: we considered the randomisation procedures adequate if the resulting sequences were unpredictable (e.g. computer‐generated, random number tables).
Allocation concealment: we considered allocation concealment adequate if the participants could not foresee the assignment (e.g. central randomisation centre, sequentially numbered, sealed, opaque containers).
Performance bias
Blinding
As the trials required different machines to deliver the trial intervention and control waveforms, adequate blinding of the personnel that treated the participants was difficult to achieve. However, paramedics work within strict protocols and prior knowledge of the waveform in use is unlikely to lead to preferential treatment of one group or the other.
We paid particular attention to all other aspects of care being the same in the trial groups.
Equality of treatment
We considered equality of treatment adequate if all aspects of participant care were the same for the trial groups. We rated this criterion as high risk of bias if any other factor was altered or performed differently depending on the waveform being used.
Attrition bias
Completeness of follow‐up
We considered the handling of drop‐outs adequate if an included trial gave a description of all participants that failed to participate until the end of the trial, the drop‐out rate was less than 15% and the difference in drop‐out rate between the trial groups was less than 10%.
Detection bias
Blinding of outcome assessment
Blinding of outcome assessment was adequate if all trial operators were unaware of the study waveform.
Blinding of analysis
If a cardiologist performed the subsequent analysis of electrocardiograms (ECGs), he/she should have done it without the knowledge of the study waveform or the outcome of the resuscitation.
During the 'Risk of bias' assessments, we subdivided these criteria into the three categories listed below.
Low risk of bias.
High risk of bias.
Unclear risk of bias.
Although we used specific criteria to judge the risk of bias in the included trials (Higgins 2011), we recognise and accept that there is some subjectivity involved in these judgements.
Measures of treatment effect
We analysed dichotomous data (ROSC, first shock efficacy, survival to hospital discharge and adverse events) and used the risk ratio (RR) with 95% confidence intervals (CIs). We assessed the differences in delivered current using the weighted mean difference values.
Unit of analysis issues
All of the included trials randomised individual participants.
Dealing with missing data
Regarding trials with missing outcome data, we considered these trials eligible for inclusion if the trial authors had performed a full intention‐to‐treat (ITT) analysis or an available‐case analysis. We considered trials that accounted for all randomised participants or analysed those participants with outcome data in the groups to which they were randomised, regardless of the intervention that the participants received, as eligible for inclusion in the review. We graded the ITT analysis as either yes, no or not stated.
Assessment of heterogeneity
We assessed the heterogeneity of pooled results using a multi‐step process that involved the following steps.
Sensitivity and subgroup analyses, as described below.
Assessment for clinical heterogeneity in the primary trials (participants, study setting, intervention, age of defibrillator etc.).
We considered a Chi² test for heterogeneity with a P value of less than 0.1 to be indicative of significant heterogeneity.
We calculated the I² statistic to describe the proportion of variability due to heterogeneity and, therefore, the consistency of the evidence.
Assessment of reporting biases
We assessed publication bias from visual inspection of the funnel plot generated from the fixed‐effect analysis for the primary outcome. This method is at its most limited when the meta‐analysis comprises only a few small studies. The more formal statistical methods of Begg 1994 and Egger 1997 are also limited in their power to detect publication bias when the meta‐analysis consists of a small number of included studies.
Data synthesis
Studies of defibrillation vary widely with respect to their definition of defibrillation success. For the purpose of this Cochrane review, we defined successful defibrillation as termination of the ventricular arrhythmia with ROSC. This definition complies with the Utstein Guidelines for uniform reporting of data from people with OHCA (Cummins 1991). We contacted any trial authors who reported outcomes outside this definition, such as electrical defibrillation (termination of the arrhythmia to any rhythm including asystole), and asked them to provide their data for re‐analysis.
Defibrillation efficacy is defined as the number of participants successfully defibrillated divided by the total number of participants in which defibrillation was attempted. The Cochrane Handbook for Systematic Reviews of Interventions states that when a trial aims to reduce the incidence of an adverse outcome there is empirical evidence that RRs of the adverse outcome are more consistent than RRs of the non‐event (Deeks 2005). For this reason, we expressed the secondary outcomes of "first shock efficacy" and "efficacy of up to three shocks" as the "failure to terminate the arrhythmia with resulting return of spontaneous circulation".
In the absence of substantial clinical or statistical heterogeneity, we used a fixed‐effect model with RRs and 95% CIs. In the presence of statistical heterogeneity or substantial variability in primary trial populations or interventions, we considered whether to pool the trial results using a random‐effects model with appropriate caution in interpretation, or not to combine trial results. We planned to perform further analyses to explore possible the sources of significant heterogeneity.
We used Review Manager (RevMan) software (RevMan 2014) for the analyses.
Subgroup analysis and investigation of heterogeneity
In the presence of significant heterogeneity and a sufficient number of trials reporting the outcome, we planned to conduct exploratory analyses to investigate the potential sources of heterogeneity.
We planned to use subgroup analysis to explore the possible sources of heterogeneity (e.g. participants, treatments and trial quality). Heterogeneity among participants could be related to age, gender or co‐morbid pathology. Heterogeneity in treatments could be related to duration of cardiac arrest, bystander CPR, rhythm (VF/VT or other non‐shockable rhythm initially), drugs used and cycles of CPR.
Sensitivity analysis
We were unable to perform the planned sensitivity analyses due to the small number of included trials.
Results
Description of studies
Our literature search identified 265 unique references of interest. We have presented the results of the study selection process in Figure 1. Four trials (six articles) met the inclusion criteria of this Cochrane review. We identified two references that referred to the same trial, and the latter reference compared the experimental waveform with two monophasic (control) waveforms separately. A follow‐up paper, which compared the efficacy of the intervention using different definitions of shock success, presented the results of another included trial. Thus, we included four trials with a total of 552 participants in our meta‐analysis (ORCA 2000; ORBIT 2005TIMBER 2006; van Alem 2003).
1.
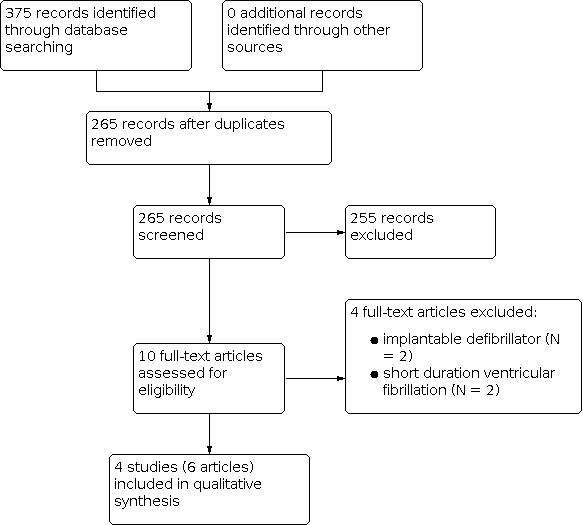
Study flow diagram.
Designs
All included trials were RCTs that randomised the order of biphasic and monophasic defibrillation at either the ambulance station or EMT/first‐responder unit level with periods varying from one day to four months. Only one trial was double blinded (van Alem 2003). One trial blinded the emergency medical technicians (EMTs) but not the trial investigator that interpreted the post‐shock ECG (TIMBER 2006). Another included trial blinded the trial investigator but not the EMTs (ORBIT 2005).
Populations
All of the included trials enrolled adult participants experiencing out‐of‐hospital cardiac arrest (OHCA). One trial compared biphasic and monophasic shocks from automated external defibrillators (AEDs) delivered by non‐medical responders prior to the arrival of EMTs (van Alem 2003). Typically, trials excluded participants whose cardiac arrest was witnessed by EMTs but one trial included participants who received a shock at any time during advanced life support treatment, which may have included EMT‐witnessed arrests (ORBIT 2005).
Interventions
All trials included participants in the pre‐hospital setting with advanced life support protocols following the ILCOR 2000 guidelines. Three trials investigated the efficacy of an escalating energy biphasic waveform. In two of these trials the first two shocks were delivered at 200 J with subsequent shocks at 360 J. In the third included trial, the energy of delivered shocks was 120 J for the first shock, 150 J for the second shock and 200 J for each shock thereafter. The fourth trial delivered fixed energy biphasic waveform at 150 J. All of the included trials employed escalating‐energy 200‐200‐360 J monophasic waveforms in their control groups.
Two trials used impedence‐compensating biphasic truncated exponential (BTE) waveforms, one used a standard BTE waveform and the fourth trial employed a rectilinear biphasic waveform. All trials used monophasic damped sine (MDS) waveforms as controls, and one trial also used a monophasic truncated exponential (MTE) control waveform.
Outcomes
The included trials reported a variety of outcome measures. Table 1 shows the definition of successful defibrillation that each included trial used. This Cochrane review focused on conversion of VF/VT to an organised rhythm and, where possible, we retrieved this information from the included trials.
1. Definitions of successful defibrillation.
| Trial | Definition |
| ORBIT 2005 | Organised rhythm at 5 seconds post‐shock |
| ORCA 2000 | Termination of VF for at least 5 seconds without regard to haemodynamic factors |
| TIMBER 2006 | Displacement to an organised rhythm |
| van Alem 2003 | Termination of VF into an organised rhythm within 1 minute |
Abbreviations: VF: ventricular fibrillation.
All trials reported efficacy of the first defibrillation shock and two trials reported the efficacy of two and three consecutive shocks (ORBIT 2005; van Alem 2003). We recorded data on return of spontaneous circulation (ROSC), survival to hospital admission and survival to hospital discharge from all included trials.
No trials reported on aspects of operator safety or markers of myocardial damage. As such, we could not report these endpoints.
Risk of bias in included studies
The 'Risk of bias' graph in Figure 2 shows that two of the four included trials had allocation concealment that was poorly performed or reported. However, all trials yielded a low risk of bias for randomisation, completeness of outcome reporting and equality of treatments. The 'Risk of bias' summary in Figure 3 shows that van Alem 2003 was the only included trial to yield a low risk of bias across all five categories we assessed.
2.

'Risk of bias' graph: review authors' judgements about each 'Risk of bias' item presented as percentages across all included trials.
3.

'Risk of bias' summary: review authors' judgements about each 'Risk of bias' item for each included trial.
We reported that one of the four trials was at high risk of bias regarding allocation concealment (see the 'Characteristics of included studies' section). This finding is unlikely to have affected the trial results. Even if paramedics were aware of the treatment assignment, trials enrolled consecutive participants and paramedics were unable to selectively choose to enrol or exclude a participant from the trial. Similarly, paramedics work within strict protocols and prior knowledge of the waveform in use is unlikely to lead to preferential treatment of one group or the other.
We consider that high risk of bias for allocation concealment does not result in high risk of bias for the included trials. Therefore, two trials were at low risk of bias (ORBIT 2005; van Alem 2003), one study was at unclear risk of bias (ORCA 2000) and one trial was at high risk of bias (TIMBER 2006).
In general, blinding was adequate. Two of the four included trials, van Alem 2003 and TIMBER 2006, blinded the defibrillator operator. In two trials, ORCA 2000 and ORBIT 2005, the defibrillator operator was aware of the waveform assignment. However, as stated above, strict protocols are followed in the treatment of people with cardiac arrest and we do not believe that the lack of blinding led to significant performance bias. Three included trials used multiple outcome assessors who were blinded to the treatment allocation (ORBIT 2005; ORCA 2000; van Alem 2003). No trial demonstrated any aspect of care that differed between the trial groups.
The included trials poorly described the ITT analyses. However, there was only one defibrillator accessible at any time in three of the four included trials. Therefore, only the defibrillator that was meant to be in use was available to the crew, and minimised the possibility of crossover of treatment. In the fourth trial, ORCA 2000, the "carrying case of the selected AED type was tagged, clearly indicating which AED had to be used for the entire day". There was minimal loss to follow‐up and all included trials reported greater than 97.5% follow‐up of enrolled participants. Overall, we considered the ITT analysis acceptable in all included trials.
Effects of interventions
Return of spontaneous circulation
The RR for failure to achieve ROSC after biphasic compared to monophasic waveform defibrillation was 0.86 (95% CI 0.62 to 1.20; four trials, 552 participants; Analysis 1.1). There was a moderate, though non‐significant, degree of heterogeneity (P = 0.13, I² statistic = 47%). This heterogeneity was entirely due to the inclusion of ORCA 2000. The trial authors of ORCA 2000 did not provide a definition of ROSC, but notably their definition of defibrillation differed from all other included trials. When we removed this trial from the analysis, there was no difference in the risk of failure to achieve ROSC (RR 1.01, 95% CI 0.79 to 1.26) and no heterogeneity (P = 0.65, I² statistic = 0%).
1.1. Analysis.

Comparison 1: Return of spontaneous circulation, Outcome 1: Failure to achieve return of spontaneous circulation (ROSC)
ORCA 2000 was the only trial that included a MTE waveform in the control arm. Martens 2001 performed a later re‐analysis of this trial and compared the biphasic waveform with each of the two monophasic waveforms used for controls. This re‐analysis demonstrated identical rates of ROSC for each of the monophasic waveforms, but noted that the primary trial was powered for comparison of biphasic waveforms against all monophasic waveforms. Sensitivity analysis of the biphasic waveform against only the MDS waveform showed no changed in the study's RR, attenuation of the pooled RR and a reduction in the amount of heterogeneity in the pooled analysis. However, we did not include these results as there may be substantial differences between the control patients included and those excluded.
Failure to defibrillate
One included trial, ORCA 2000, used a different definition of defibrillation to our protocol (Faddy 2007). Despite our repeated requests to the trial authors, we were unable to obtain outcome data using the definitions we had established. Inclusion of this trial in the pooled analysis generated significant statistical heterogeneity. Consequently, we presented the summary estimate of effect without data from this trial. However, although the other three trials defined defibrillation as "termination of VF to an organised rhythm", all three trials used different definitions of "organised rhythm".
The RR value for failure to defibrillate on the first shock following biphasic defibrillation compared to monophasic was 0.84 (95% CI 0.70 to 1.01; three trials, 450 participants; Analysis 2.1). There was moderate heterogeneity (P = 0.14, I² statistic = 49%). This heterogeneity was entirely due to the inclusion of the van Alem 2003 trial.
2.1. Analysis.

Comparison 2: Failure to defibrillate, Outcome 1: Failure to defibrillate on first shock
Regarding failure to defibrillate with up to three shocks, the RR was 0.81 (95% CI 0.61 to 1.09; two trials, 317 participants; Analysis 2.2). This trial showed no significant reduction in the risk of failure to defibrillate. There was a moderate degree of heterogeneity in this pooled analysis (P = 0.19, I² statistic = 41%).
2.2. Analysis.

Comparison 2: Failure to defibrillate, Outcome 2: Failure to defibrillate with up to 3 shocks
Two trials (285 participants) compared the rate of ROSC after the first delivered defibrillation shock (Analysis 2.3). The RR for failure to achieve ROSC after the first shock was 0.92 (95% CI 0.81 to 1.04). There was no significant heterogeneity in the pooled analysis (P = 0.63, I² statistic = 0%).
2.3. Analysis.

Comparison 2: Failure to defibrillate, Outcome 3: Failure to achieve ROSC after first shock
Survival
The RR of death before hospital admission for participants treated with biphasic compared to monophasic waveforms was 1.05 (95% CI 0.90 to 1.23; three trials, 383 participants; Analysis 3.1). The RR of death before hospital discharge was 1.05 (95% CI 0.78 to 1.42; four trials, 550 participants; Analysis 3.2). There was no significant heterogeneity for either estimate (P = 0.36, I² statistic = 2% and P = 0.64, I² statistic = 0%; respectively).
3.1. Analysis.

Comparison 3: Survival, Outcome 1: Survival to hospital admission
3.2. Analysis.

Comparison 3: Survival, Outcome 2: Survival to hospital discharge
Publication bias
We have shown a funnel plot derived from the fixed‐effect model of the primary outcome in Figure 4. The figure shows an absence of small studies favouring either of biphasic or monophasic waveform defibrillators but no evidence of publication bias. Funnel plots for all other outcomes showed an overall lack of small studies, but even distribution of studies.
4.

Funnel plot of comparison: 1. Return of spontaneous circulation (ROSC), outcome: 1.1 Failure to achieve ROSC.
Adverse events
None of the included trials reported adverse events associated with monophasic or biphasic waveform defibrillation. We did not identify any trials that specifically examined adverse events. Consequently, we were unable to report on adverse events associated with these waveforms.
Cost‐benefit analysis
None of the included trials reported on the costs associated with monophasic or biphasic waveform defibrillation. We did not identify any studies that specifically examined cost versus benefit. Consequently, we were unable to report on the cost effectiveness of biphasic or monophasic waveforms.
Discussion
In this Cochrane review we investigated whether biphasic or monophasic defibrillation waveforms are superior for transthoracic defibrillation in out‐of‐hospital cardiac arrest (OHCA). The pooled results failed to demonstrate a statistically significant beneficial effect of biphasic waveforms over monophasic waveforms. In terms of failure to achieve return of spontaneous circulation (ROSC), we cannot exclude a decrease in risk of 38% or an increase in risk of 20%.
Furthermore, there were no statistically significant differences in failure to defibrillate on the first shock and with up to three shocks, or survival to hospital admission or hospital discharge.
Although not statistically significant (P value of less than 0.1), there was a moderate degree of heterogeneity in several of our pooled analyses. This is likely due to different participant populations, slight differences in waveform characteristics and slightly different definitions of successful defibrillation between trials. We used a random‐effects model for pooled analyses to account for these differences.
There was no evidence of publication bias other than a paucity of studies.
This systematic review contradicts conventional beliefs on the superiority of biphasic waveforms for transthoracic defibrillation. All of the included trials showed significant superiority of biphasic waveforms in terms of achieving ROSC. However, when expressed in terms of failure to achieve ROSC, no trial showed significant superiority. In addition, the pooled results of these trials did not have sufficient precision to demonstrate a significant benefit of biphasic waveform defibrillation.
This finding is supported by a more recent retrospective case review in an unselected adult OHCA population before and after the introduction of biphasic waveform defibrillators in an urban population in the USA (Freeman 2008). Failure to achieve ROSC was the same in the biphasic and monophasic groups (70.0% vs 69.4%, P = 0.92) and there was a slightly lower (although not statistically significant) rate of hospital discharge in the biphasic group (10.3% vs 12.3%, P = 0.57).
Similarly, a population‐based propensity‐matched cohort study performed in Japan found no significant difference between patients defibrillated with biphasic compared to monophasic waveform defibrillators in terms of ROSC before hospital arrival (RR 1.05, 95% CI 0.94 to 1.17; P = 0.42), one month survival (RR 1.06, 95% CI 0.94 to 1.18; P = 0.39) or one month neurologically intact survival (RR 1.07, 95% CI 0.92 to 1.25; P = 0.36) (Tanabe 2012).
Although there are trends towards superiority of biphasic waveforms for first shock efficacy and efficacy of up to three (stacked) shocks, there was insufficient precision in the pooled analysis to demonstrate a reduction in the risk of failure to achieve ROSC at any time during the resuscitation effort.
None of the included trials investigated the potential risks to the trial participants or the rescuer associated with biphasic waveform defibrillation. We did not identify any other studies that specifically investigated adverse events. Therefore we are unable to report on the potential for adverse events from biphasic or monophasic waveform defibrillation.
An a priori definition of this systematic review was that lack of blinding of the defibrillator operator would not result in significant performance bias. The defibrillator operators in two of the included trials were aware of the treatment allocation. Although this should trigger a "high risk of bias" adjudication for these trials, we downgraded the risk for performance bias to "low risk" in line with our stated approach. We acknowledge that this is a value judgement which may not be shared by all readers of this Cochrane review.
This systematic review was subject to a number of limitations. First, we were limited to a small number of relatively small randomised controlled trials (RCTs). Second, for one included trial we were unable to obtain data in a format consistent with our study definitions for the outcome 'failure to defibrillate'. We did not include data from this trial in the pooled analyses for failure to defibrillate with the first shock and failure to defibrillate with up to three stacked shocks. Third, the small number and relatively small size of the primary studies precluded our pre‐defined subgroup analyses. Last, all of the trials we included in the analysis were performed using pre‐2005 resuscitation guidelines.
In addition, analysis of the primary outcome lacked statistical power to detect the observed level of effect. The pooled relative risk was 0.86 (95% CI 0.68 to 1.20). Power calculations show that this sample size has only 14% power to detect the observed level of effect. Hence, larger RCTs are needed to adequately explore the efficacy of biphasic compared to monophasic waveform defibrillation.
Funnel plots generated from the fixed‐effect model of the primary outcome suggest the potential for publication bias. Although there are only a small number of included trials in our analysis, there appears to be an absence of small studies that demonstrate no effect of biphasic waveform defibrillation.
Authors' conclusions
Implications for practice.
Although now considered standard of care, there was insufficient precision in this Cochrane review to demonstrate a statistically significant difference between monophasic waveforms for defibrillation of people with OHCA. Although this finding is unlikely to have an effect on clinical practice, it may preclude the need for more expensive technology in public access automated external defibrillators (AEDs) by negating the need for capacitors and solid‐state circuitry capable of creating biphasic defibrillation pulses.
Implications for research.
The lack of clarity around the superiority of biphasic waveforms demonstrated in this systematic review and a recent retrospective review needs to be the focus of further research. If biphasic waveforms are to remain the clinical standard, further research to improve the efficacy is required. Research is underway investigating phase duration, waveform tilt and a number of cardiopulmonary resuscitation (CPR) factors. The relative efficacy of biphasic and monophasic waveforms should be retested under the current international resuscitation guidelines.
None of the studies published to date have examined quality of life or cost‐benefit outcomes of biphasic or monophasic waveform defibrillators. Given the uncertainty around the superiority of biphasic waveform defibrillators, cost‐effectiveness analysis is warranted to justify the added cost of biphasic waveform defibrillators.
Several of the outcomes in this Cochrane review were subject to moderate levels of heterogeneity. Clear guidelines should be established to define outcomes in resuscitation research so that all trials report on the same outcomes.
We were unable to assess the potential for adverse effects as none of the included trials provided adequate information on adverse events. Future studies should include assessment of adverse effects.
What's new
| Date | Event | Description |
|---|---|---|
| 21 September 2021 | Review declared as stable | The research area is no longer active. The authors are not aware of new studies since 2006. |
History
Protocol first published: Issue 4, 2007 Review first published: Issue 2, 2016
| Date | Event | Description |
|---|---|---|
| 19 August 2008 | Amended | We converted the review to a new review format. |
Acknowledgements
We thank Mr Ron Cunningham for his assistance in the initial stages of this Cochrane review and Dr Ayan Sen for his help to prepare the Cochrane protocol (Faddy 2007).
Appendices
Appendix 1. Search strategies
CENTRAL
#1MeSH descriptor: [Heart Arrest] explode all trees #2heart next arrest* #3cardiac next arrest* #4heart next attack* #5heart next standstill #6asystol* #7circulat* next arrest* #8sudden next death* #9MeSH descriptor: [Ventricular Fibrillation] this term only #10MeSH descriptor: [Tachycardia, Ventricular] explode all trees #11ventricular next fibrillation* #12ventricular next tachycardia #13#1 or #2 or #3 or #4 or #5 or #6 or #7 or #8 or #9 or #10 or #11 or #12 #14MeSH descriptor: [Electric Countershock] this term only #15MeSH descriptor: [Defibrillators] this term only #16MeSH descriptor: [Advanced Cardiac Life Support] this term only #17defibrillat* #18#14 or #15 or #16 or #17 #19#13 and #18 #20biphasic #21waveform* #22gurvich #23edmark #24rectilinear #25multipulse near biowave #26#20 or #21 or #22 or #23 or #24 or #25 #27#19 and #26
MEDLINE
1. exp Heart Arrest/ 2. (heart adj2 (arrest* or attack* or standstill or asystol*)).tw. 3. ((cardiac or circulat*) adj2 arrest*).tw. 4. (sudden adj2 death*).tw. 5. Ventricular Fibrillation/ 6. exp Tachycardia, Ventricular/ 7. (ventric* adj2 (fibrillation* or tachycardia)).tw. 8. or/1‐7 9. Electric Countershock/ 10. Defibrillators/ 11. Advanced Cardiac Life Support/ 12. defibrillat*.tw. 13. or/9‐12 14. 8 and 13 15. biphasic.tw. 16. waveform*.tw. 17. gurvich.tw. 18. edmark.tw. 19. rectilinear.tw. 20. (multipulse adj2 biowave).tw. 21. or/15‐20 22. 14 and 21 23. randomized controlled trial.pt. 24. controlled clinical trial.pt. 25. randomized.ab. 26. placebo.ab. 27. drug therapy.fs. 28. randomly.ab. 29. trial.ab. 30. groups.ab. 31. 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 32. exp animals/ not humans.sh. 33. 31 not 32 34. 22 and 33
EMBASE
1. exp heart arrest/ 2. (heart adj2 (arrest* or attack* or standstill or asystol*)).tw. 3. ((cardiac or circulat*) adj2 arrest*).tw. 4. sudden death/ 5. (sudden adj2 death*).tw. 6. heart ventricle fibrillation/ 7. heart ventricle tachycardia/ 8. (ventric* adj2 (fibrillation* or tachycardia)).tw. 9. or/1‐7 10. cardioversion/ 11. defibrillation/ 12. resuscitation/ 13. defibrillat*.tw. 14. exp defibrillator/ 15. or/10‐14 16. 9 and 15 17. biphasic.tw. 18. waveform*.tw. 19. gurvich.tw. 20. edmark.tw. 21. rectilinear.tw. 22. (multipulse adj2 biowave).tw. 23. or/17‐22 24. 16 and 23 25. random$.tw. 26. factorial$.tw. 27. crossover$.tw. 28. cross over$.tw. 29. cross‐over$.tw. 30. placebo$.tw. 31. (doubl$ adj blind$).tw. 32. (singl$ adj blind$).tw. 33. assign$.tw. 34. allocat$.tw. 35. volunteer$.tw. 36. crossover procedure/ 37. double blind procedure/ 38. randomized controlled trial/ 39. single blind procedure/ 40. 25 or 26 or 27 or 28 or 29 or 30 or 31 or 32 or 33 or 34 or 35 or 36 or 37 or 38 or 39 41. exp animals/ or exp invertebrate/ or animal experiment/ or animal model/ or animal tissue/ or animal cell/ or nonhuman/ 42. human/ or normal human/ or human cell/ 43. 41 and 42 44. 41 not 43 45. 40 not 44 46. 24 and 45
Data and analyses
Comparison 1. Return of spontaneous circulation.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 Failure to achieve return of spontaneous circulation (ROSC) | 4 | 552 | Risk Ratio (M‐H, Random, 95% CI) | 0.86 [0.62, 1.20] |
Comparison 2. Failure to defibrillate.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 2.1 Failure to defibrillate on first shock | 3 | 450 | Risk Ratio (M‐H, Random, 95% CI) | 0.84 [0.70, 1.01] |
| 2.2 Failure to defibrillate with up to 3 shocks | 2 | 317 | Risk Ratio (M‐H, Random, 95% CI) | 0.81 [0.61, 1.09] |
| 2.3 Failure to achieve ROSC after first shock | 2 | 285 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.92 [0.81, 1.04] |
Comparison 3. Survival.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 3.1 Survival to hospital admission | 3 | 383 | Risk Ratio (M‐H, Random, 95% CI) | 1.05 [0.90, 1.23] |
| 3.2 Survival to hospital discharge | 4 | 550 | Risk Ratio (M‐H, Random, 95% CI) | 1.05 [0.78, 1.42] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
ORBIT 2005.
| Study characteristics | ||
| Methods | Block RCT | |
| Participants | 169 adult patients (86 intervention, 83 control) who experienced VF/ventricular tachycardia (VT) during advanced life support by paramedics and who received at least 1 defibrillator shock | |
| Interventions | Intervention: 120 J to 200 J escalating energy rectilinear biphasic defibrillation shock Control: 200 J to 360 J escalating energy MDS defibrillation shock |
|
| Outcomes |
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated block randomisation at station level |
| Allocation concealment (selection bias) | Low risk | Central randomisation |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Paramedics were aware of treatment allocation but were unable to deviate from treatment protocols |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | The outcome assessors, validation committee and DMSB were blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Most participants (167/169) had outcome data |
| Equality of treatment | Low risk | The trial authors followed ILCOR 2000 guidelines |
ORCA 2000.
| Study characteristics | ||
| Methods | Randomised controlled trial (RCT) | |
| Participants | 115 participants (54 intervention, 61 control), > 36 kg in weight, with known or suspected cardiac arrest attended by emergency medical services | |
| Interventions | Intervention: fixed energy 150 J impedence‐compensating biphasic truncated exponential defibrillation shock Control: 200 J to 360 J escalating energy monophasic damped sine (MDS) or monophasic truncated exponential (MTE) defibrillation shock |
|
| Outcomes |
|
|
| Notes | Martens 2001 is a subgroup analysis of this trial that separately compared the MDS and MTE control groups | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation of devices in daily blocks |
| Allocation concealment (selection bias) | High risk | Paramedics were aware of which defibrillator was to be used |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Paramedics were aware of treatment allocation but were unable to deviate from treatment protocols |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | The outcome adjudication committee was blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The trial authors included all participants in the analyses |
| Equality of treatment | Low risk | The trial authors followed ERC guidelines |
TIMBER 2006.
| Study characteristics | ||
| Methods | Block RCT | |
| Participants | 148 adults (68 intervention, 80 control) who experienced non‐traumatic cardiac arrest with VF as the initial recorded rhythm | |
| Interventions | Intervention: 200 J to 360 J escalating energy biphasic truncated exponential defibrillation shock Control: 200 J to 360 J escalating energy MDS defibrillation shock |
|
| Outcomes |
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation at unit level in blocks of 3 months |
| Allocation concealment (selection bias) | Unclear risk | Unit "changed for its counterpart" on a quarterly basis |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Automated external defibrillator (AED) operators were blinded to waveform |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Waveform appeared on the ECG tracing |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Primary outcome: 20/168 (12%) participants received mixed shocks (biphasic and monophasic) and trial authors excluded them from the analyses (defined a priori) |
| Equality of treatment | Low risk | The trial authors followed Modified 2000 guidelines |
van Alem 2003.
| Study characteristics | ||
| Methods | Block RCT | |
| Participants | 120 participants (51 intervention, 69 control), with witnessed or unwitnessed cardiac arrest and VF as the initial recorded rhythm, in whom an automated defibrillator shock was delivered by a non‐medical responder | |
| Interventions | Intervention: escalating 200 J to 360 J impedence‐compensating biphasic truncated exponential defibrillation shock Control: 200 J to 360 J escalating energy MDS defibrillation shock |
|
| Outcomes |
|
|
| Notes | Koster 2006 presented re‐analysed data with different definitions of shock success | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The trial authors randomised devices in blocks of 4 months |
| Allocation concealment (selection bias) | Low risk | Units were identical in shape, size and design |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double blinding. Waveform details were removed from electrocardiogram (ECG) traces |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Two physicians performed blinded outcome assessments |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The trial authors included most (120/123) eligible participants. They presented the outcome data for all included participants |
| Equality of treatment | Low risk | Standard treatment protocols |
Abbreviations: AED: automated external defibrillators; ECG: electrocardiogram; J: joules; MDS: monophasic damped sine; MTE: monophasic truncated exponential; VF: ventricular fibrillation; VT: ventricular tachycardia; RCT: randomised controlled trial; ROSC: return of spontaneous circulation.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Bardy 1995 | Implantable defibrillator |
| Bardy 1996 | Short duration VF |
| Higgins 2000 | Short duration VF |
| Strickberger 1996 | Implantable defibrillator |
Abbreviations: VF: ventricular fibrillation.
Contributions of authors
Steven C Faddy (SCF) is the guarantor of this Cochrane review.
SCF drafted and critical appraised the protocol and approved the final protocol draft (Faddy 2007); conceived, designed and coordinated the review; performed the literature searches; selected and appraised studies; entered data into Review Manager (RevMan) (RevMan 2014); drafted and appraised the review; and approved the final review version.
Paul A Jennings (PAJ) drafted and critical appraised the protocol; approved the final version of the protocol (Faddy 2007); designed the review; performed the literature searches; selected and critically appraised studies; drafted and appraised the review; and approved the final review version.
Sources of support
Internal sources
St Vincent's Hospital, Sydney, Australia
Rural Ambulance Victoria, Australia
Department of Community Emergency Health and Paramedic Practice, Monash University, Melbourne, Australia
Ambulance Service of New South Wales, Sydney, Australia
External sources
No sources of support provided
Declarations of interest
SCF has no known conflicts of interest. PAJ has no known conflicts of interest.
Stable (no update expected for reasons given in 'What's new')
References
References to studies included in this review
ORBIT 2005 {published data only}
- Morrison LJ, Dorian P, Long J, Vermeulen M, Schwartz B, Sawadsky B, et al. Out-of-hospital cardiac arrest rectilinear biphasic to monophasic damped sine defibrillation waveforms with advanced life support intervention trial (ORBIT). Resuscitation 2005;66(2):149-57. [DOI] [PubMed] [Google Scholar]
ORCA 2000 {published data only}
- Martens PR, Russell JK, Wolcke B, Paschen H, Kuisma M, Gliner BE, et al. Optimal Response to Cardiac Arrest study: defibrillation waveform effects. Resuscitation 2001;49(3):233-43. [DOI] [PubMed] [Google Scholar]
- Schneider T, Martens PR, Paschen H, Kuisma M, Wolcke B, Gliner BE, et al. Multicenter, randomized, controlled trial of 150-J biphasic shocks compared with 200- to 360-J monophasic shocks in the resuscitation of out-of-hospital cardiac arrest victims. Optimized Response to Cardiac Arrest(ORCA) Investigators. Circulation 2000;102(15):1780-7. [DOI] [PubMed] [Google Scholar]
TIMBER 2006 {published data only}
- Kudenchuk PJ, Cobb LA, Copass MK, Olsufka M, Maynard C, Nichol G. Transthoracic incremental monophasic versus biphasic defibrillation by emergency responders (TIMBER): a randomized comparison of monophasic with biphasic waveform ascending energy defibrillation for the resuscitation of out-of-hospital cardiac arrest due to ventricular fibrillation. Circulation 2006;114(19):2010-8. [DOI] [PubMed] [Google Scholar]
van Alem 2003 {published data only}
- Koster RW, Walker RG, Alem AP. Definition of successful defibrillation. Critical Care Medicine 2006;34(12 Suppl):S423-6. [DOI] [PubMed] [Google Scholar]
- Alem AP, Chapman FW, Lank P, Hart AA, Koster RW. A prospective, randomised and blinded comparison of first shock success of monophasic and biphasic waveforms in out-of-hospital cardiac arrest. Resuscitation 2003;58(1):17-24. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Bardy 1995 {published data only}
- Bardy GH, Gliner BE, Kudenchuk PJ, Poole JE, Dolack GL, Jones GK, et al. Truncated biphasic pulses for transthoracic defibrillation. Circulation 1995;91(6):1768-74. [DOI] [PubMed] [Google Scholar]
Bardy 1996 {published data only}
- Bardy GH, Marchilinski FE, Sharma AD, Worley SJ, Luceri RM, Yee R, et al. Multicenter comparison of truncated biphasic shocks and standard damped sine wave monophasic shocks for transthoracic ventricular defibrillation. Circulation 1996;94(10):2507-14. [DOI] [PubMed] [Google Scholar]
Higgins 2000 {published data only}
- Higgins SL, Herre JM, Epstein AE, Greer GS, Friedman PL, Gleva ML, et al. A comparison of biphasic and monophasic shocks for external defibrillation. Prehospital Emergency Care 2000;4(4):305-13. [DOI] [PubMed] [Google Scholar]
Strickberger 1996 {published data only}
- Strickberger SA, Daoud E, Goyal R, Chan KK, Bogun F, Castellani M, et al. Prospective randomized comparison of anodal monophasic shocks versus biphasic cathodal shocks on defibrillation energy requirements. American Heart Journal 1996;131(5):961-5. [DOI] [PubMed] [Google Scholar]
Additional references
Atwood 2005
- Atwood C, Eisenberg MS, Herlitz J, Rea TD. Incidence of EMS-treated out-of-hospital cardiac arrest in Europe. Resuscitation 2005;67(1):75-80. [DOI] [PubMed] [Google Scholar]
Begg 1994
- Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics 1994;50(4):1088-101. [PubMed] [Google Scholar]
Cummins 1991
- Cummins RO, Chamberlain DA, Abramson NS, Allen M, Baskett PJ, Becker L, et al. Recommended guidelines for uniform reporting of data from out-of-hospital cardiac arrest: the Utstein style. A statement for health professionals from a task force of the American Heart Association, the European Resuscitation Council, the Heart and Stroke Foundation of Canada, and the Australian Resuscitation Council. Circulation 1991;84(2):960-75. [DOI] [PubMed] [Google Scholar]
Deeks 2005
- Deeks JJ, Higgins JPT, Altmad DG (editors). Analysing and presenting results. In: Higgins JPT, Green S, editors(s). Cochrane Handbook for Systematic Reviews of Interventions Version 4.2.5 [updated May 2005]. Chichester: John Wiley and Sons Ltd, 2005. [Google Scholar]
de Latorre 2001
- Latorre F, Nolan J, Robertson C, Chamberlain D, Baskett P, European Resuscitation Council. European Resuscitation Council Guidelines 2000 for Adult Advanced Life Support: A statement from the Advanced Life Support Working Group and approved by the Executive Committee of the European Resuscitation Council. Resuscitation 2001;48(3):211-21. [DOI] [PubMed] [Google Scholar]
Echt 1993
- Echt DS, Greene HL, Kudenchuk PJ, DiMarco JP, Tang ASL, Reiter MJ, et al. Biphasic waveform is more efficacious than monophasic waveform for transthoracic cardioversion. PACE 1993;16:914A. [DOI] [PubMed] [Google Scholar]
Egger 1997
- Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997;315(7109):629-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
Faddy 2003
- Faddy SC, Powell J, Craig JC. Biphasic and monophasic shocks for transthoracic defibrillation: a meta analysis of randomised controlled trials. Resuscitation 2003;58(1):9-16. [DOI] [PubMed] [Google Scholar]
Freeman 2008
- Freeman K, Hendey GW, Shalit M, Stroh M. Biphasic defibrillation does not improve outcomes compared to monophasic defibrillation in out-of-hospital cardiac arrest. Prehospital Emergency Care 2008;12(2):152-6. [DOI] [PubMed] [Google Scholar]
Greene 1995
- Green HL, DiMarco JP, Kudenchuk PJ, Scheinman MM, Tang ASL, Reiter MJ, et al. Comparison of monophasic and biphasic defibrillating pulse waveforms for transthoracic cardioversion. American Journal of Cardiology 1995;75(16):1135-9. [DOI] [PubMed] [Google Scholar]
Herre 1998
- Herre JM, Higgins SL, Epstein AE, Greer S, Friedman PL, Gleva MJ, et al. A comparison of biphasic and monophasic shocks for external defibrillation of humans. Circulation 1998;98:1-173. [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane-handbook.org.
Holmberg 2000
- Holmberg M, Holmberg S, Herlitz J. Incidence, duration and survival of ventricular fibrillation in out-of-hospital cardiac arrest patients in Sweden. Resuscitation 2000;44(1):7-17. [DOI] [PubMed] [Google Scholar]
Keuper 2007
- Keuper W, Dieker H-J, Brouwer MA, Verheugt FWA. Reperfusion therapy in out-of-hospital cardiac arrest: current insights. Resuscitation 2007;73(2):189-201. [DOI] [PubMed] [Google Scholar]
Larsen 1993
- Larsen MP, Eisenberg MS, Cummins RO, Hallstrom AP. Predicting survival from out-of-hospital cardiac arrest: a graphic model. Annals of Emergency Medicine 1993;22(11):1652-8. [DOI] [PubMed] [Google Scholar]
Lefebvre 2011
- Lefebvre C, Manheimer E, Glanville J. Chapter 6: Searching for studies. In: Higgins JPT, Green S (editors) Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane-handbook.org.
Martens 2001
- Martens PR, Russell JK, Wolcke B, Paschen H, Kuisma M, Gliner BE, et al. Optimal Response to Cardiac Arrest study: defibrillation waveform effects. Resuscitation 2001;49(3):233-43. [DOI] [PubMed] [Google Scholar]
Mittal 1999
- Mittal S, Ayati S, Stein KM, Knight BP, Morady F, Schwartzman D, et al. Comparison of a novel rectilinear biphasic waveform with a damped sine wave monophasic waveform for transthoracic ventricular defibrillation. Journal of the American College of Cardiology 1999;34(5):1595-601. [DOI] [PubMed] [Google Scholar]
Moher 1999
- Moher D, Cook DJ, Eastwood S, Olkin I, Rennie D, Stroup DF. Improving the quality of reports of meta-analyses of randomised controlled trials: the QUOROM statement. Quality of Reporting of Meta-analyses. Lancet 1999;354(9193):1896-900. [DOI] [PubMed] [Google Scholar]
Nishiuchi 2003
- Nishiuchi T, Hiraide A, Hayashi Y, Uejima T, Morita H, Yukioka H, et al. Incidence and survival rate of bystander-witnessed out-of-hospital cardiac arrests with cardiac etiology in Osaka, Japan: a population-based study according to the Utstein style. Resuscitation 2003;59(3):329-35. [DOI] [PubMed] [Google Scholar]
RevMan 2014 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration Review Manager (RevMan). Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Szili‐Torok 2002
- Szili-Torok T, Theuns D, Verblaauw T, Scholten M, Kimman GJ, Res J, et al. Transthoracic defibrillation of short-lasting ventricular fibrillation: a randomised trial for comparison of the efficacy of low-energy biphasic rectilinear and monophasic damped sine shocks. Acta Cardiologica 2002;57(5):329-34. [DOI] [PubMed] [Google Scholar]
Tanabe 2012
- Tanabe S, Yasunaga H, Ogawa T, Koike S, Akahane M, Horiguchi H, et al. Comparison of outcomes after use of biphasic or monophasic defibrillators among out-of-hospital cardiac arrest patients: a nationwide population-based observational study. Circulation. Cardiovascular Quality Outcomes 2012;5(5):689-96. [DOI] [PubMed] [Google Scholar]
Waalewijn 1998
- Waalewijn RA, Vos R, Koster RW. Out-of-hospital cardiac arrests in Amsterdam and its surrounding areas: results from the Amsterdam resuscitation study (ARREST) in Utstein style. Resuscitation 1998;38(3):157-67. [DOI] [PubMed] [Google Scholar]
WHO 2014
- World Health Organization. Global Health Estimates 2014 - summary tables. http://www.who.int/healthinfo/global_burden_disease/estimates/en/index1.html (accessed 5 February 2016).
References to other published versions of this review
Faddy 2007
- Faddy S, Jennings P, Cunningham R, Sen A. Biphasic versus monophasic waveforms for transthoracic defibrillation in out-of-hospital cardiac arrest. Cochrane Database of Systematic Reviews 2007, Issue 4. Art. No: CD006762. [DOI: 10.1002/14651858.CD006762] [DOI] [PMC free article] [PubMed] [Google Scholar]


