Abstract
Purpose of Review:
In recent decades, the incidence of myocardial infarction (MI) has declined among the general population. However, MI rates in the young have not decreased as much as has been observed among older individuals. This review will focus on recent trends of MI in young patients, factors that may account for these trends, and implications for future prevention.
Recent Findings:
MI rates in young patients, particularly in women, have not decreased in the same fashion as they have for their older counterparts, with some studies reporting an increase. The reasons for these findings include under-estimation of cardiovascular risk, and accordingly treatment, in the young, as well as an increasing prevalence of risk factors such as obesity and diabetes.
Summary:
Better recognition and treatment of cardiovascular risk factors among young adults may improve outcomes. There is a need for improved methods to assess and treat cardiovascular risk in young individuals.
Keywords: myocardial infarction, prevention, young, risk factor
Introduction
Significant progress in the prevention of acute myocardial infarction (MI) and the use of effective medical therapy has led to a declining mortality rate and incidence of MI.(1–3) However, MI rates among young individuals, particularly in women, have not decreased in the same fashion as they have for older individuals.(4) This trend highlights the importance of improving primary and secondary prevention measures among young individuals, especially since their risk factor profiles and prognosis may be different from that of their older counterparts.(4–7) Furthermore, consequences of MI in the young can be especially devastating as they may have a larger economic and societal impact given the higher number of productive years of life at-risk. Therefore, we sought to report on recent trends of MI in young patients, factors that may account for these trends, and implications for future prevention.
Definition of “Young”
In past literature, there has not been a universal definition of “young” in regards to MI patients, with “young” being defined as anywhere from <30 years of age to <55 years of age.(4–9) As such, this paper will focus on the broader concept of “young” which includes various age cut-off defined by the authors of each study being reviewed.
Trends in Myocardial Infarction in the Young
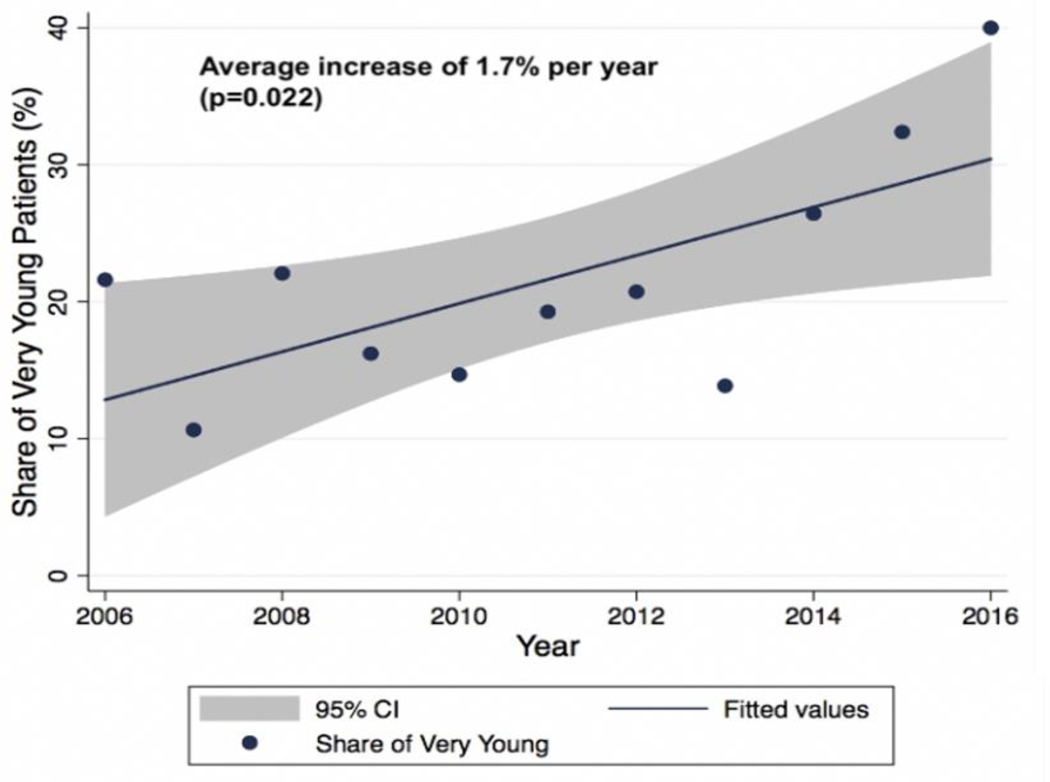
Although rates of MI have decreased among the general population, young patients have benefited less from these favorable trends.(4) The Atherosclerosis Risk in Communities (ARIC) surveillance study found that despite the decreasing percentage of young (35–54 years of age) ARIC community residents over time relative to the entire ARIC community residents (35–75 years of age), the annual proportion of acute MI admissions attributable to young patients increased significantly from 27% between 1995–1999 to 32% between 2010–2014 (p<0.0001).(4) The Partners YOUNG-MI registry – a study that focuses on patients who experienced an MI at less than or equal to 50 years of age – reported an increase of 1.7% per year in the proportion of very young (<40 years of age) individuals presenting with MI from 2007 to 2016 (p=0.022) (Figure 1).(9)
Figure 1.
Trend in the proportion of very young myocardial infarction patients in the Young-MI Registry (2006–2016) – there is a significant average increase of 1.7% per year in proportion of young (40 years of age) individuals presenting with a type 1 myocardial infarction from 2007 to 2016.
The ARIC study found that the increasing rates of MI in young patients was especially pronounced in young women.(4) Specifically, the study reported a significant increase in the annual proportion of acute MI admissions attributable to young women (21% in 1995–1999 to 31% in 2010–2014, p<0.0001), representing an increase of 10% as compared with 5% in young men.(4) Similar findings were found in a study from the Polish PL-ACS registry from 2009–2013.(10) In addition to a larger increase in annual proportion of acute MI attributable to young women as compared with young men, the annual incidence of acute MI hospitalizations in the ARIC study increased in young women, but decreased in young men.(4) This trend may be explained by the higher burden of comorbidities and risk factors in young females compared with their male counterparts.(4) Despite these trends, and the higher burden of co-morbidities among women in the study, there was no difference in 1-year mortality between the sexes,(4) although other studies have reported mixed findings regarding mortality between sexes.(8, 11, 12)
Interestingly, while the proportion of patients who experience an MI at a young age is increasing, a recent study found that the percentage of admissions for ST-elevation MI has decreased (71.7% vs. 63.9%, p=0.002) among young patients (age <40 years) from 2009 to 2013.(10) This is hypothesized to be related to advancements in prevention and wide use of high-sensitivity troponin.(10)
Risk Factors
The concerning trends regarding the proportionally higher rate of MI in young individuals are likely multifactorial. First, there is an under-recognition and paucity of data regarding cardiovascular (CV) risk factors in the young.(7, 13) Importantly, this can lead to underestimation of risk, and accordingly utilization of primary prevention strategies.(13, 14) Second, there is an increasing prevalence of several important modifiable risk factors in those who have an MI at a young age.(4, 5, 7, 8, 15–17)
Under-recognition of Risk Factors
Although patients of all ages who experience an MI share many traditional CV risk factors – with studies suggesting that over 80– 90% of young MI patients had at least 1 traditional CV risk factor prior to MI (7, 14) – there are some notable differences between younger and older cohorts. In particular, the prevalence of both modifiable and unmodifiable risk factors and their association with future CV events may be different in the younger age subset (Figure 2).(4–9, 15)
Figure 2.
Leading causes of myocardial infarction among young individuals – substance use, tobacco use, type 2 diabetes, obesity, elevated lipids, and positive family history are major risk factors for myocardial infarction among young adults.
Tobacco
Smoking still remains one of the strongest and most prevalent risk factors among young patients presenting with MI.(7, 10, 18) A recent study found that young (18–49 years of age) men and women who smoked had an approximately 9-fold and 13-fold increased risk of MI, respectively, compared to their non-smoking counterparts (IRR: 8.60, 95% CI: 7.70–9.59 in men vs. IRR: 13.22, 95% CI: 10.33–16.66 in women).(18) In addition, young smokers had the highest increased risk of MI compared with smokers from other age groups of the study,(18) suggesting that smoking may be a particularly strong predictor of future MI in the young. Yandrapalli et al found that among the 280,736 MI patients classified as young (age 18–44), smoking (56.8%), dyslipidemia (51.7%), and hypertension (49.8%) were ranked as the most prevalent risk factors respectively.(7) The same study also showed that the prevalence of smoking, which has been trending downward in the general population, increased from 54.3% to 60.3% from 2005 to 2015 among young MI patients (p<0.001),(7) although other studies have reported a slight decrease.(4) Furthermore, a study from the Young-MI registry found that patients who quit smoking post-MI had a substantial reduction in long-term CV death compared with those who continued to smoke.
Substance Use
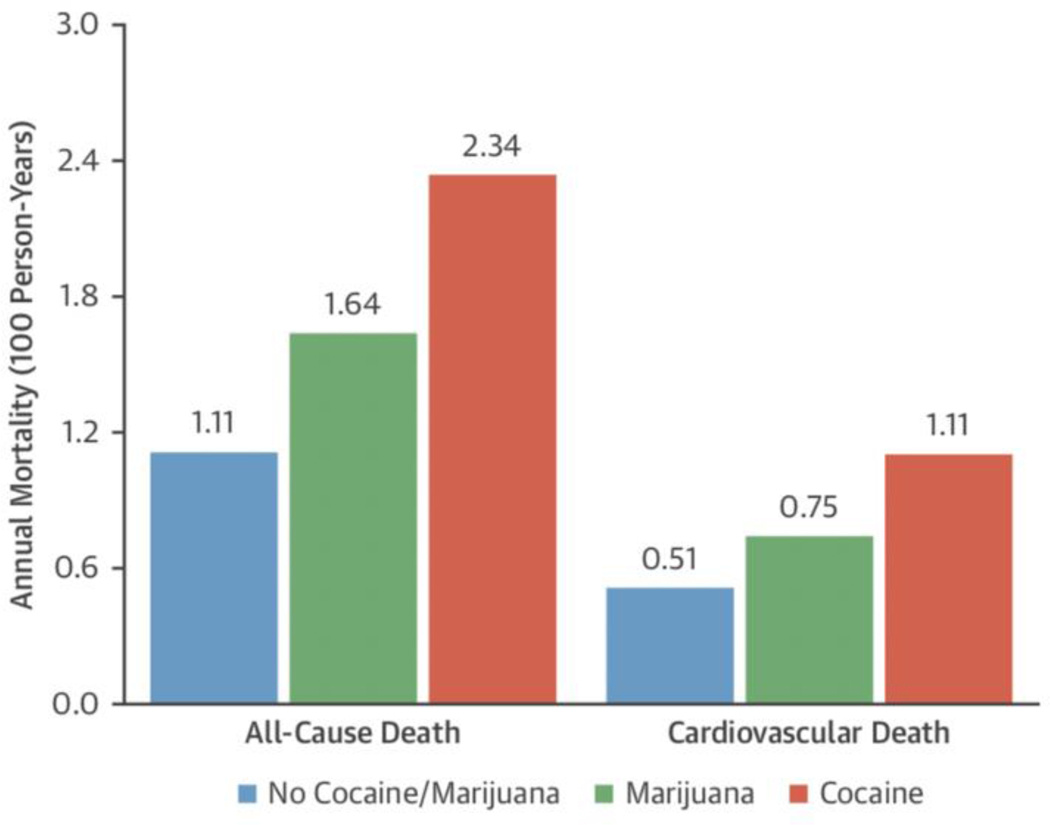
Substance use, especially cocaine and marijuana, is particularly prevalent in young patients who experience myocardial infarction.(5, 19) A study from the Partners YOUNG-MI registry found that cocaine or marijuana use was present in over 10% of young (<50 years of age) MI patients over the study period (2000–2016) and was associated with an increase in all-cause (HR 1.99, p=0.001) and CV mortality (HR 2.22, p=0.005) over a median follow-up period of 11.2 years (Figure 3).(5) Cocaine use was found in 4.7% of patients while marijuana use was found in 6.0% of patients.(5) Older studies have reported rates of cocaine use among young MI patients to be as high as 25%.(19) Another study from the Partner’s YOUNG-MI registry determined that very young MI patients (age<40 years) had an even higher prevalence of marijuana and/or cocaine abuse than patients aged 40–50 (17.9% vs 9.3%, p<0.001).(9) These rates are especially concerning given that most young individuals may not perceive marijuana use as a risk factor for MI.(20) Furthermore, the past decade has seen a significant increase in marijuana use across all age groups, including young individuals,(5) a fact that is almost certainly due to the recent legalization of marijuana in many US states.(4, 5, 7, 8, 15) This is especially important given that several studies have found that marijuana use is associated with an increased risk of MI.(20–22)
Figure 3.
Annual incidence rates for all-cause death and cardiovascular death – observed annual death and cardiovascular death rates are shown by drug of abuse in 100 person-years.
Obesity and Diabetes
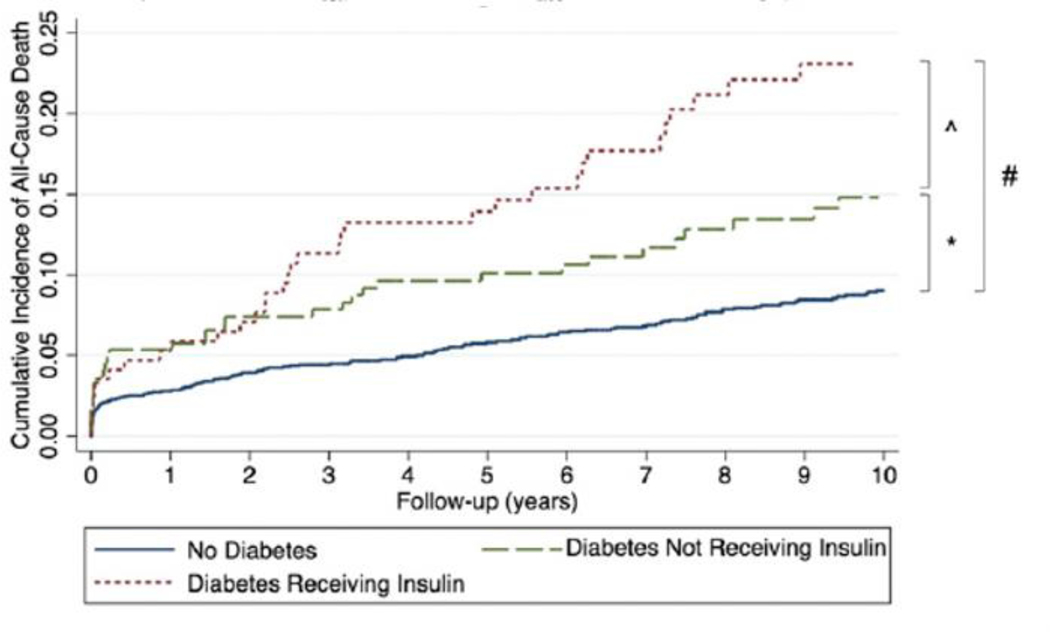
The prevalence of obesity has increased in the young.(7) Yandrapalli et al found that the risk factor with the largest increase in prevalence among young individuals was obesity, reporting a 98% increase from 2005 to 2015.(7) Similarly, the prevalence of metabolic syndrome in young individuals has increased,(16) with some studies showing that nearly half of young MI patients had metabolic syndrome.(23) This is especially concerning as the same study found that reinfarction rates were the highest in young MI patients with metabolic syndrome as compared with young patients without metabolic syndrome (4.8% vs. 1.4%, p=0.035), and older patients with or without metabolic syndrome (2.1% vs 1.5%, p=0.035).(23) Diabetes is another risk factor that may be highly prevalent in young individuals. A Partners YOUNG-MI study found that 1 in 5 young MI patients had diabetes at the time of their index hospitalization, and the presence of diabetes in these patients was associated with a higher long-term all-cause (HR 1.65, p=0.008) (Figure 4) and CV mortality (HR 2.10, p=0.004).(6)
Figure 4.
All-cause mortality in young adults following type 1 myocardial infarction stratified by diagnosis of diabetes – Kaplan–Meier curves of all-cause mortality in patients without diabetes, diabetes not receiving insulin, and diabetes receiving insulin. Unadjusted hazard ratio 1.61, 95% confidence interval 1.13–2.32, P ¼ 0.009; adjusted hazard ratio 1.48, 95% confidence interval 0.88–2.45, P ¼ 0.133. ^ Unadjusted hazard ratio 2.08, 95% confidence interval 1.35–3.20, P ¼ 0.001; adjusted hazard ratio 1.40, 95% confidence interval 0.85–2.30, P ¼ 0.182. # Unadjusted hazard ratio 3.34, 95% confidence interval 2.42–4.59, P < 0.001; adjusted hazard ratio 2.00, 95% confidence interval 1.28–3.13, P ¼ 0.002.
Unmodifiable Risk Factors
In addition to modifiable risk factors, there may be several unmodifiable risk factors that play a significant role in the development of MI in young patients. These include genetic risk factors such as elevated lipoprotein(a) [Lp(a)], familial hypercholesterolemia (FH), and polygenic risk that may be more prevalent in patients who experience a first MI at a young age.(24–28) These non-conventional CV risk factors may be especially important in predicting a future MI in the young as younger patients tend to have fewer traditional risk factors than their older counterparts. (5, 9, 28)
Elevated Lp(a) levels are prevalent in young patients who have experienced an MI, with at least one report estimating that nearly 30% of such patients had Lp(a) levels greater than the 80th percentile.(24) Many studies and meta-analyses have shown that an elevated Lp(a) level is independently associated with an increased risk of coronary artery disease (CAD) and MI.(29, 30) A recent study from Iceland found odds ratios of 1.16 and 1.18 for CAD and MI, respectively, for every 50nM increase in Lp(a) (p<0.0001).(31) In addition to elevated Lp(a) levels being a risk factor for MI, Lp(a) may also be a useful prognostic tool to predict risk of future adverse events in patients who have already experienced an MI.(32) For instance, Jin et al found that in MI patients who had pre-diabetes or diabetes, Lp(a) levels greater than 50 mg/dL were significantly associated with higher risk of future CV events (HR: 2.7, p<0.05 for pre-diabetes and HR: 3.5, p<0.05 for diabetes).(32) Neither of these studies focused specifically on young patients. However, given that Lp(a) levels are almost entirely genetically mediated and levels stay relatively stable over time,(33) these finds should be generalizable to younger patients.
FH is also a strong and prevalent genetic risk factor for the development of MI in young patients.(28, 34) Analysis from the Partner’s YOUNG-MI registry found that almost 10% of young (<50 years of age) MI patients had clinically defined FH.(28) Among patients with FH, nearly ½ were not on high intensity statin therapy prior to MI and ~1/3 were not discharged on high-intensity statin therapy post-MI, perhaps due to under-recognition of risk factors or underestimation of future CV risk.(28) These findings are important given that recent data comparing CV outcomes between FH children and their affected parents found that children with FH who initiate statin therapy in childhood have a lower incidence of future CV disease and CV death by age 40 versus their affected parents (1% vs 26% who have CV disease and 0% vs 7% who have CV death by age 40).(34) This finding illustrates the need for more aggressive lipid lowering therapy in patients with FH for primary prevention of MI.
Polygenic risk has recently gained interest as a risk factor in patients, especially young patients, who may be genetically pre-disposed to developing CAD.(35) Polygenic risk is directly determined from analyzing an individual’s genetic code, particularly CAD-risk associated single nucleotide polymorphisms, which remains unchanged since birth.(35) Since traditional risk calculators may provide an inaccurate assessment of cardiovascular risk in young patients,(14) polygenic risk scores (PRS) may have the potential to augment and refine risk stratification in these patients.
Consequences of Risk Factor Under-recognition
The 2019 American College of Cardiology/American Heart Association prevention guidelines recommend use of the Pooled Cohort Equations (PCE) to estimate 10-year ASCVD risk in patients aged 40–75 years who are being evaluated for cardiovascular disease prevention.(36) However, methods for risk calculation in patients younger than 40 years of age are less clear. According to data from the Partner’s YOUNG-MI registry, prior to their MI, only 31% of young MI patients (age <50 years) would have met criteria for statin eligibility per the 2013 American College of Cardiology/American Heart Association guidelines and only 18% would have met such criteria per the 2016 U.S. Preventative Services Task Force recommendations.(14) These numbers are even lower among women and among MI patients less than 40 years old.(9) The under underestimation of risk among young individuals may limit the utilization of primary prevention measures. Differences in risk factors profiles between younger and older MI patients likely also contribute to our inability to accurately assess the risk of CAD in the young as traditional risk assessment tools, such as PCE, focus on factors that are most relevant to older patient cohorts.(37) As such, there is a need for better methods to assess cardiovascular risk among younger individuals.
Implications on Prevention
Risk factors play a significant role in the development and progression of CAD, which may lead to myocardial infarction. The same risk factors that lead to MI also contribute to adverse long-term events following MI. Thus, preventative measures are critical in both primary and secondary prevention.
In the primary prevention setting, selective treatment of blood pressure and elevated cholesterol may be important to implement earlier in life. However, lifestyle interventions should be implemented in all individuals, including avoiding tobacco, exercising regularly, maintaining a healthy weight, and adhering to a diet which is low in processed foods and added sugars and which is mostly plant based.(36) A more plant-based diet may also help prevent or treat obesity as well as optimize blood sugar levels among those who are at risk for developing diabetes.(38, 39) A more aggressive intervention regarding substance use cessation is also needed.(5) Given the aforementioned limitation in the Pooled Cohort Equation calculators, it is important to recognize that lifestyle measures should be implemented regardless of the 10-year ASCVD score.
Improvements in risk factor calculation in young individuals can help optimize guidelines on the use of preventative medical therapy such as statins in younger age groups. For instance, the use of a PRS may have the potential to provide further risk stratification among young patients and provide more insight on the use of preventative therapies.(40, 41) A UK study found that the addition of PRS to the traditional Pooled Cohort Equations for ASCVD risk stratification was associated with a risk reclassification for 4.4% (95% CI: 3.5%−5.3%) of the patient cohort whose risk was calculated by PCE alone over a median follow-up of 8 years.(40) Natarajan et al determined that patients with a high PRS can derive an even greater relative risk reduction of CV events with statin therapy than patients with a normal or low PRS.(41) Furthermore, an analysis by Kathiresan et al showed that PRS can identify 8% of the population at >3-fold risk for CAD compared to the general population, a prevalence that is 20-fold higher than that detected from monogenic mutations conferring comparable CAD risk.(42) As such, PRS has shown potential as a tool for CV risk prediction, but further studies are needed to determine the incremental value of this information beyond other clinical risk factors, and whether this information can ultimately improve outcomes.
In addition, coronary artery calcium (CAC) scoring has proven to be a useful and cost-effective method to quantify calcified plaque in coronary arteries, which may provide insights into the presence and burden of CAD, and subsequently need for preventative therapy. The 2019 American College of Cardiology/American Heart Association guidelines suggest the measurement of a CAC score in patients aged 40–75 who are at intermediate 10-year ASCVD risk if the need for statin therapy is uncertain.(36) Although guidelines in very young patients (<40 years) are less established, current data suggest a possible role for selective use of CAC testing in this group.(43, 44) For instance, the Coronary Artery Risk Development in Young Adults study found that young individuals (32–46 years of age) with even minimal amount of calcification seen on coronary CT are at elevated risk for coronary heart disease events (HR: 5.0, 95% CI: 2.8–8.7) and CV death (HR: 3.0, 95% CI: 1.9–4.7) compared with those who have no calcifications.(43) Another recent study from the CAC Consortium study showed that 34% of young adults 30–49 years of age referred for CAC testing had evidence of any plaque (i.e. CAC>0). Those with a CAC score >100 (7% of the population studied) had an approximately 3-fold increased risk of CV death compared with those who had a CAC score of zero.(44) As such, selective use of CAC testing may be a useful at identifying young individuals who may benefit from more aggressive prevention measures.(45)
Conclusion
The prevalence of MI in the young has not decreased as it has for older individuals in recent years. In fact, the proportion of MI admissions attributable to young adults, particularly young women, is increasing. This suggests that current prevention strategies must be tailored to target risk factors that are implicated in cardiovascular disease among the young. In addition, improved methods for risk assessment among young individuals is needed, likely incorporating both traditional and novel risk factors, including in some cases genetic risk score and CAC testing. Importantly, treatment of modifiable risk factors should be implemented at a younger age.
Key points:
Myocardial infarction rates in young patients have not decreased as they have for older individuals.
Risk score may underestimate the risk of cardiovascular disease among young individuals. In select cases CAC testing, or in the future polygenic risk scores, may be helpful at refining risk assessment.
Risk factors that may be particularly important among young individuals include tobacco use, substance abuse, obesity, and diabetes.
Footnotes
Conflicts of Interest: Dr. Blankstein receives research support from Astellas Inc and Amgen Inc. The remaining authors have nothing to disclose.
References
- 1.Reynolds K, Go AS, Leong TK, Boudreau DM, Cassidy-Bushrow AE, Fortmann SP, et al. Trends in Incidence of Hospitalized Acute Myocardial Infarction in the Cardiovascular Research Network (CVRN). Am J Med. 2017;130(3):317–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wilmot KA, O’Flaherty M, Capewell S, Ford ES, Vaccarino V. Coronary Heart Disease Mortality Declines in the United States From 1979 Through 2011: Evidence for Stagnation in Young Adults, Especially Women. Circulation. 2015;132(11):997–1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Krumholz HM, Normand S-LT, Wang Y. Twenty-Year Trends in Outcomes for Older Adults With Acute Myocardial Infarction in the United States. JAMA Netw Open. 2019;2(3):e191938-e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Arora S, Stouffer GA, Kucharska-Newton AM, Qamar A, Vaduganathan M, Pandey A, et al. Twenty Year Trends and Sex Differences in Young Adults Hospitalized With Acute Myocardial Infarction. Circulation. 2019;139(8):1047–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. DeFilippis EM, Singh A, Divakaran S, Gupta A, Collins BL, Biery D, et al. Cocaine and Marijuana Use Among Young Adults With Myocardial Infarction. J Am Coll Cardiol. 2018;71(22):2540–51. *This analysis found that young MI patients with substance use have worse long-term outcomes than those who do not, which highlights the importance of screening and treatment for substance use among young patients who experience an MI.
- 6.Divakaran S, Singh A, Biery D, Yang J, DeFilippis EM, Collins BL, et al. Diabetes Is Associated With Worse Long-term Outcomes in Young Adults After Myocardial Infarction: The Partners YOUNG-MI Registry. Diabetes Care. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yandrapalli S, Nabors C, Goyal A, Aronow WS, Frishman WH. Modifiable Risk Factors in Young Adults With First Myocardial Infarction. J Am Coll Cardiol. 2019;73(5):573–84. [DOI] [PubMed] [Google Scholar]
- 8.Guo X, Li Z, Vittinghoff E, Sun Y, Pletcher MJ. Trends in rate of acute myocardial infarction among patients aged <30 years. Nature Reviews Cardiology. 2018;15(2):119-. [DOI] [PubMed] [Google Scholar]
- 9.Yang J, Biery DW, Singh A, Divakaran S, DeFilippis EM, Wu WY, et al. Risk Factors and Outcomes of Very Young Adults Who Experience Myocardial Infarction: The Partners YOUNG-MI Registry. Am J Med. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Trzeciak P, Gierlotka M, Polonski L, Gasior M. Treatment and outcomes of patients under 40 years of age with acute myocardial infarction in Poland in 2009–2013: an analysis from the PLACS registry. Pol Arch Intern Med. 2017;127(10):666–73. [DOI] [PubMed] [Google Scholar]
- 11.Izadnegahdar M, Singer J, Lee MK, Gao M, Thompson CR, Kopec J, et al. Do younger women fare worse? Sex differences in acute myocardial infarction hospitalization and early mortality rates over ten years. J Womens Health (Larchmt). 2014;23(1):10–7. [DOI] [PubMed] [Google Scholar]
- 12.Sabbag A, Matetzky S, Porter A, Iakobishvili Z, Moriel M, Zwas D, et al. Sex Differences in the Management and 5-Year Outcome of Young Patients (<55 Years) with Acute Coronary Syndromes. Am J Med. 2017;130(11):1324.e15-.e22. [DOI] [PubMed] [Google Scholar]
- 13.Shah N, Kelly AM, Cox N, Wong C, Soon K. Myocardial Infarction in the “Young”: Risk Factors, Presentation, Management and Prognosis. Heart Lung Circ. 2016;25(10):955–60. [DOI] [PubMed] [Google Scholar]
- 14. Singh A, Collins BL, Gupta A, Fatima A, Qamar A, Biery D, et al. Cardiovascular Risk and Statin Eligibility of Young Adults After an MI: Partners YOUNG-MI Registry. J Am Coll Cardiol. 2018;71(3):292–302. **This analysis underscores the need for better CV risk prediction and classification in young individuals, as most individuals who experienced an MI at a young age would have been classified as low risk (prior to their event) by current guidelines.
- 15.Patel RS, Katta SR, Patel R, Ravat V, Gudipalli R, Patel V, et al. Cannabis Use Disorder in Young Adults with Acute Myocardial Infarction: Trend Inpatient Study from 2010 to 2014 in the United States. Cureus. 2018;10(8):e3241-e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zarich S, Luciano C, Hulford J, Abdullah A. Prevalence of metabolic syndrome in young patients with acute MI: does the Framingham Risk Score underestimate cardiovascular risk in this population? Diab Vasc Dis Res. 2006;3(2):103–7. [DOI] [PubMed] [Google Scholar]
- 17.Wu WY, Biery DW, Singh A, Divakaran S, Berman AN, Ayuba G, et al. Recovery of Left Ventricular Systolic Function and Clinical Outcomes in Young Adults With Myocardial Infarction. Journal of the American College of Cardiology. 2020;75(22):2804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Palmer J, Lloyd A, Steele L, Fotheringham J, Teare D, Iqbal J, et al. Differential Risk of ST-Segment Elevation Myocardial Infarction in Male and Female Smokers. J Am Coll Cardiol. 2019;73(25):3259–66. [DOI] [PubMed] [Google Scholar]
- 19.Qureshi AI, Suri MF, Guterman LR, Hopkins LN. Cocaine use and the likelihood of nonfatal myocardial infarction and stroke: data from the Third National Health and Nutrition Examination Survey. Circulation. 2001;103(4):502–6. [DOI] [PubMed] [Google Scholar]
- 20.DeFilippis EM, Bajaj NS, Singh A, Malloy R, Givertz MM, Blankstein R, et al. Marijuana Use in Patients With Cardiovascular Disease. Journal of the American College of Cardiology. 2020;75(3):320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nawrot TS, Perez L, Kunzli N, Munters E, Nemery B. Public health importance of triggers of myocardial infarction: a comparative risk assessment. Lancet. 2011;377(9767):732–40. [DOI] [PubMed] [Google Scholar]
- 22.Richards JR, Bing ML, Moulin AK, Elder JW, Rominski RT, Summers PJ, et al. Cannabis use and acute coronary syndrome. Clin Toxicol (Phila). 2019;57(10):831–41. [DOI] [PubMed] [Google Scholar]
- 23.Kim I, Kim MC, Sim DS, Hong YJ, Kim JH, Jeong MH, et al. Effect of the Metabolic Syndrome on Outcomes in Patients Aged <50 Years Versus >50 Years With Acute Myocardial Infarction. Am J Cardiol. 2018;122(2):192–8. [DOI] [PubMed] [Google Scholar]
- 24.Berman A, Biery D, Singh A, Wu W, Divakaran S, DeFilippis E, et al. PREVALENCE AND TESTING OF LIPOPROTEIN(A) AMONG YOUNG ADULTS WITH MYOCARDIAL INFARCTION: THE PARTNERS YOUNG-MI REGISTRY. Journal of the American College of Cardiology. 2020;75(11 Supplement 1):1867. [Google Scholar]
- 25.Enas EA, Varkey B, Dharmarajan TS, Pare G, Bahl VK. Lipoprotein(a): An underrecognized genetic risk factor for malignant coronary artery disease in young Indians. Indian Heart J. 2019;71(3):184–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kamstrup PR, Tybjærg-Hansen A, Steffensen R, Nordestgaard BG. Genetically Elevated Lipoprotein(a) and Increased Risk of Myocardial Infarction. JAMA. 2009;301(22):2331–9. [DOI] [PubMed] [Google Scholar]
- 27.Otaki Y, Gransar H, Berman DS, Cheng VY, Dey D, Lin FY, et al. Impact of family history of coronary artery disease in young individuals (from the CONFIRM registry). Am J Cardiol. 2013;111(8):1081–6. [DOI] [PubMed] [Google Scholar]
- 28.Singh A, Gupta A, Collins BL, Qamar A, Monda KL, Biery D, et al. Familial Hypercholesterolemia Among Young Adults With Myocardial Infarction. J Am Coll Cardiol. 2019;73(19):2439–50.*This paper investigated the prevalence of familial hypercholesterolemia in young adults who experience an MI, and also emphasized the need for more aggressive lipid lowering therapies among young individuals. [DOI] [PubMed] [Google Scholar]
- 29.Cai G, Huang Z, Zhang B, Yu L, Li L. Elevated lipoprotein (a) levels are associated with the acute myocardial infarction in patients with normal low-density lipoprotein cholesterol levels. Biosci Rep. 2019;39(4):BSR20182096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Danesh J, Collins R, Peto R. Lipoprotein(a) and coronary heart disease. Meta-analysis of prospective studies. Circulation. 2000;102(10):1082–5. [DOI] [PubMed] [Google Scholar]
- 31.Gudbjartsson DF, Thorgeirsson G, Sulem P, Helgadottir A, Gylfason A, Saemundsdottir J, et al. Lipoprotein(a) Concentration and Risks of Cardiovascular Disease and Diabetes. Journal of the American College of Cardiology. 2019;74(24):2982. [DOI] [PubMed] [Google Scholar]
- 32.Jin J-L, Cao Y-X, Zhang H-W, Sun D, Hua Q, Li Y-F, et al. Lipoprotein(a) and Cardiovascular Outcomes in Patients With Coronary Artery Disease and Prediabetes or Diabetes. Diabetes Care. 2019;42(7):1312. [DOI] [PubMed] [Google Scholar]
- 33.Langsted A, Kamstrup PR, Nordestgaard BG. Lipoprotein(a): fasting and nonfasting levels, inflammation, and cardiovascular risk. Atherosclerosis. 2014;234(1):95–101. [DOI] [PubMed] [Google Scholar]
- 34.Luirink IK, Wiegman A, Kusters DM, Hof MH, Groothoff JW, de Groot E, et al. 20-Year Follow-up of Statins in Children with Familial Hypercholesterolemia. New England Journal of Medicine. 2019;381(16):1547–56. [DOI] [PubMed] [Google Scholar]
- 35.Natarajan P. Polygenic Risk Scoring for Coronary Heart Disease: The First Risk Factor. Journal of the American College of Cardiology. 2018;72(16):1894–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Arnett Donna K, Blumenthal Roger S, Albert Michelle A, Buroker Andrew B, Goldberger Zachary D, Hahn Ellen J, et al. 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;140(11):e596–e646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gooding HC, Ning H, Gillman MW, Shay C, Allen N, Goff DC, Jr., et al. Application of a Lifestyle-Based Tool to Estimate Premature Cardiovascular Disease Events in Young Adults: The Coronary Artery Risk Development in Young Adults (CARDIA) Study. JAMA Intern Med. 2017;177(9):1354–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hemler EC, Hu FB. Plant-Based Diets for Cardiovascular Disease Prevention: All Plant Foods Are Not Created Equal. Curr Atheroscler Rep. 2019;21(5):18. [DOI] [PubMed] [Google Scholar]
- 39.McMacken M, Shah S. A plant-based diet for the prevention and treatment of type 2 diabetes. J Geriatr Cardiol. 2017;14(5):342–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Elliott J, Bodinier B, Bond TA, Chadeau-Hyam M, Evangelou E, Moons KGM, et al. Predictive Accuracy of a Polygenic Risk Score-Enhanced Prediction Model vs a Clinical Risk Score for Coronary Artery Disease. Jama. 2020;323(7):636–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Natarajan P, Young R, Stitziel Nathan O, Padmanabhan S, Baber U, Mehran R, et al. Polygenic Risk Score Identifies Subgroup With Higher Burden of Atherosclerosis and Greater Relative Benefit From Statin Therapy in the Primary Prevention Setting. Circulation. 2017;135(22):2091–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Khera AV, Chaffin M, Aragam KG, Haas ME, Roselli C, Choi SH, et al. Genome-wide polygenic scores for common diseases identify individuals with risk equivalent to monogenic mutations. Nature Genetics. 2018;50(9):1219–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Carr JJ, Jacobs DR Jr., Terry JG, Shay CM, Sidney S, Liu, et al. Association of Coronary Artery Calcium in Adults Aged 32 to 46 Years With Incident Coronary Heart Disease and Death. JAMA Cardiol. 2017;2(4):391–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Miedema MD, Dardari ZA, Nasir K, Blankstein R, Knickelbine T, Oberembt S, et al. Association of Coronary Artery Calcium With Long-term, Cause-Specific Mortality Among Young Adults. JAMA Netw Open. 2019;2(7):e197440-e. *This large study provides data on the potential yield and prognostic implications of coronary artery calcium (CAC) testing among young individuals who were referred for CAC testing.
- 45.Miedema MD, Nauffal VD, Singh A, Blankstein R. Statin therapy for young adults: A long-term investment worth considering. Trends Cardiovasc Med. 2020;30(1):48–53. [DOI] [PubMed] [Google Scholar]