Abstract
Herpes simplex (HSV) esophagitis is usually identified in patients with significant immunosuppressive conditions such as AIDS. Short course of immunosuppressive therapy is an uncommon risk factor for this condition. We present a case of acute gastrointestinal bleeding secondary to HSV type 1-induced esophageal ulcers. A 63-year-old woman developed acute hypoxic hypercapnic respiratory failure. Past medical history was significant for COPD for which the patient was taking short-acting bronchodilator inhalers. The patient was intubated and started on mechanical ventilation. Intravenous Solu-Medrol 40 mg Q6 was started. Hospital course was complicated by sepsis of unknown source. Empiric broad-spectrum antibiotic therapy was started. On the 11th hospital day, the patient experienced multiple episodes of coffee ground emesis. There was abdominal tenderness on physical examination. Significant laboratory results were lipase 1,911 U/L and lymphopenia (ALC = 300/mm3). Endoscopy revealed severe erosive esophagitis and multiple punched-out ulcerations of the esophagus. Empiric treatment with valacyclovir 500 mg OD was started. The patient required PEG tube insertion for dysphagia. Complete resolution of esophagitis was noted then. Immunohistochemical staining for HSV was strongly positive in the cells with inclusions. Short course of intravenous corticosteroids is an uncommon cause of HSV-1 esophagitis. Corticosteroid-induced lymphopenia impedes underlying cellular immunity, which might explain the reactivation of latent herpes and esophageal ulcer formation. Given the rarity of the disease, evidence of treatment is available from case reports only. We found complete resolution of esophageal ulcers after the patient received valacyclovir therapy for 10 days.
Keywords: Herpes simplex esophagitis, Immunocompetent host, Corticosteroid, COPD, Abdominal pain, Antiviral treatment response, Dysphagia, Endoscopy, Esophagus, Hematemesis, Upper gastrointestinal bleeding
Introduction
Herpes simplex virus (HSV) is a globally widespread opportunistic virus transmitted via the oral and genital routes (HSV type 1 or HSV-1) or is sexually transmitted (HSV type 2 or HSV-2). Most commonly involved sites for HSV are either oral or genital; the esophagus is rarely involved. This infection – being opportunistic – is mostly seen in an immunocompromised host, such as in patients with AIDS, with underlying malignancy, or who received an organ transplant. It is rare to see HSV, specifically HSV esophagitis, in an immunocompetent host [1, 2]. However, a short course of immunosuppressive therapy, such as steroids, is an infrequent risk factor for primary herpes or reactivation of latent herpes in an immunocompetent host. Complications, such as bleeding or perforation, are less frequent in immunocompetent than in the immunocompromised host. We present a case of acute gastrointestinal bleeding (GIB) secondary to HSV-2-induced esophageal ulcers, which itself is rare, in an immunocompetent host as most of the reported cases are from HSV-1.
Case Presentation
A 63-year-old immunocompetent woman with a significant medical history of COPD on 3 L of home oxygen presented to the emergency department (ED) with an acute hypoxic hypercapnic respiratory failure. Home medications consisted of short-acting bronchodilator inhalers, metformin, hydrochlorothiazide, and aspirin. In the ED, her vitals revealed a blood pressure of 220/134, HR 133/min, RR 36/min, SpO2 of 98% on nonrebreather. CXR exposed bilateral hyperinflated lungs with a flattened diaphragm. Initial laboratory tests were pertinent for a high-sensitivity troponin of 8 ng/L, BNP 19 pg/mL, and WBC 8.5 K/CUMM with absolute lymphocyte count of 1,200/mm3, and flu swabs were negative. She was becoming dyspneic and hypoxic. ABGs revealed a pH of 7.29 with a pCO2 of 58 and HCO3 of 27. Noninvasive mechanical ventilation, including BiPAP, was initiated, with IPAP 10, EPAP 5, rate 8, and oxygen 40%. The patient did not improve on BiPAP. MICU consultation recommended intubating her and placing her on a ventilator. Initially, in the ED, the patient was given albuterol-ipratropium, methylprednisolone, magnesium for her COPD exacerbation, and IV nitroglycerin for hypertensive urgency. She was started on intravenous methylprednisolone 40 mg q6h. The hospital course got complicated by sepsis of unknown cause. Her in-patient COPD management protocol included methylprednisolone 40 mg IV q6h, albuterol-ipratropium nebulization q4h, and budesonide inhaler twice daily. She also received empiric broad-spectrum antibiotics for her sepsis.
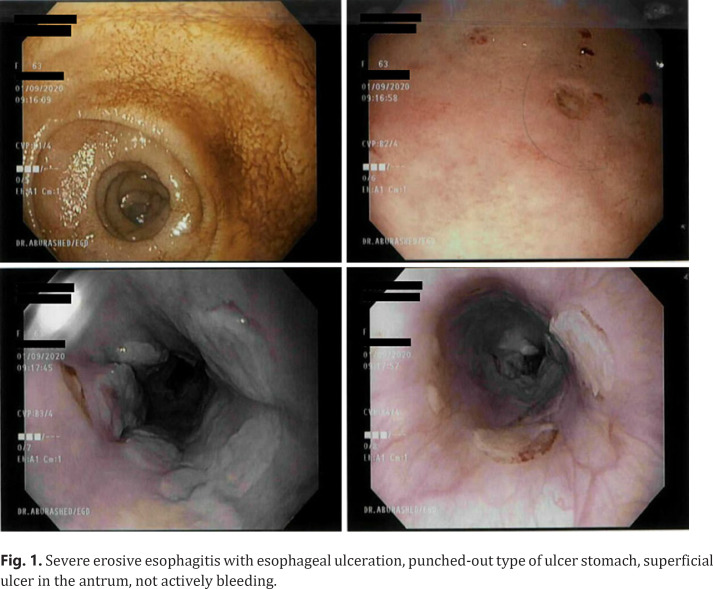
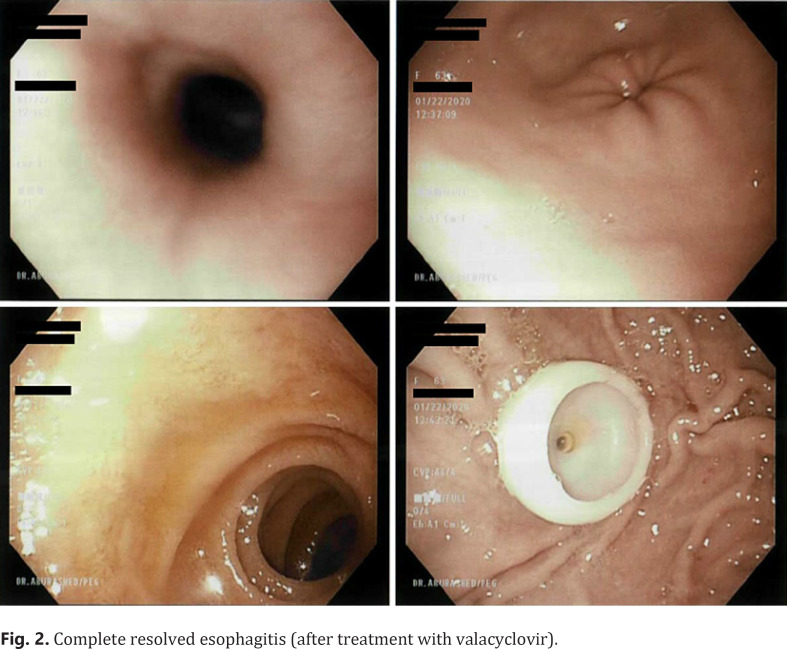
On the eleventh day of her admission and the 10th day of her steroid therapy, she started developing abdominal distention symptoms, and physical examination revealed generalized abdominal tenderness. Moreover, she had multiple episodes of coffee ground emesis. Laboratory investigation revealed lipase 1,911 U/L and WBCs of 24 K/CUMM with an absolute lymphocyte count of 300/mm3 (lymphopenia). Further, endoscopy showed severe erosive esophagitis and numerous punched-out ulceration of the esophagus (Fig. 1). Consequently, the patient was started on valacyclovir 500 mg, 2 caps t.i.d. Esophageal biopsy revealed immunohistochemical staining for HSV and strongly positive in cells with inclusions, further consolidating our diagnosis of herpes esophagitis (HSV-2). During the hospital stay, the patient required PEG tube insertion for dysphagia secondary to mechanical damage at intubation. Interestingly, on the 10th day after valacyclovir initiation, complete resolution of esophagitis was observed (Fig. 2).
Fig. 1.
Severe erosive esophagitis with esophageal ulceration, punched-out type of ulcer stomach, superficial ulcer in the antrum, not actively bleeding.
Fig. 2.
Complete resolved esophagitis (after treatment with valacyclovir).
Discussion
Herpes esophagitis is one of the most common causes of infectious esophagitis. It occurs mostly in immunosuppressed patients, like in patients with AIDS or patients undergoing organ transplants or receiving long-term immunosuppressive therapies, such as in anticancer therapies. It is rare to see HSV esophagitis even with a short course of steroids, which could cause a transient immunosuppressed phase. Oral and genital mucosa are the most commonly involved sites; it is rare for HSV to invade the esophagus and cause esophagitis, especially in immunocompetent patients. The most typical presentation includes acute onset of odynophagia, dysphagia [3], retrosternal chest pain (e.g., GERD symptoms), and fever. Less frequent symptoms include prodromal syndrome, weight loss, and upper respiratory symptoms such as cough. The literature [4] demonstrates multiple complications, including GIB, exhibited in our patient. A consolidated diagnosis is usually made based on endoscopy and biopsy. Early endoscopic findings reveal ulcer formations or vesicles, and mucosa necrosis appears in the late stages [5, 6]. The biopsy regularly displays cellular inclusions surrounded by inflammatory infiltrates.
Corticosteroid-induced lymphopenia impedes underlying cellular immunity, leading to the activation of latent herpes or the occurrence of primary herpes. Steroid-induced Th2 over Th1 immune response impairs Th1 pro-inflammatory activity [7]; the primary immune response to HSV gets inhibited afterward [8]. Our patient's laboratory values showed absolute lymphocytopenia on the 10th day of steroid use, causing a transient immunosuppressed phase. COPD exacerbation presents an additional risk factor in our patient. Consequently, it is possible that in COPD exacerbation, the immune disruption abnormally favored Th1 response [9], which could also trigger HSV occurrence or reactivation.
Herpes esophagitis usually self-resolves in immunocompetent patients [10]; few case reports show empiric treatment with valacyclovir. The use of antiviral is still controversial in this case. Our patient took 10 days of valacyclovir, and eventually, repeat endoscopy (Fig. 2) showed a total clearance of ulcerations in the esophagus. Therefore, it is very likely that antiviral treatment can hasten symptomatic relief and shorten the clinical course.
To conclude, the case findings suggested that clinicians must be aware and have a high index of HSV suspicion for patients with GIB or those presenting with dysphagia while using a short course of corticosteroids for any disease. The occurrence of herpes esophagitis can be dangerous as causing lifetime stricture with dysphagia or can occur as mild symptoms of odynophagia and mild upper GIB. Given the rarity of the disease, the evidence of treatment is available from case reports only. Repeated endoscopy within 10 days of antiviral treatment revealed a total resolution of ulcers.
Statement of Ethics
Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
Conflict of Interest Statement
The authors have no conflicts of interest to declare.
Funding Sources
The authors have no funding source to declare.
Author Contributions
Maryam Bilal Haider (first and corresponding author): made substantial contributions to the conception and design of the work, the acquisition and analysis of data for the work, and drafting the work. Brinda Basida and Anusha Bapatla: helped in revising it critically for important intellectual content. Rana Ismail and Wasif Hafeez: final approval of the version to be published. Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
References
- 1.Diezma-Martín AM, Gigante-Miravalles E, Castro Limo JD, Quimbayo Arcila CA, Puche Paniagua JJ. Herpetic esophagitis in immunocompentent host: cases report. BMC Infect Dis. 2020;20((1)):605. doi: 10.1186/s12879-020-05328-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ramanathan J, Rammouni M, Baran J, Jr, Khatib R. Herpes simplex virus esophagitis in the immunocompetent host: an overview. Am J Gastroenterol. 2000;95((9)):2171–6. doi: 10.1111/j.1572-0241.2000.02299.x. [DOI] [PubMed] [Google Scholar]
- 3.Jetté-Côté I, Ouellette D, Béliveau C, Mitchell A. Total dysphagia after short course of systemic corticotherapy: herpes simplex virus esophagitis. World J Gastroenterol. 2013;19((31)):5178–81. doi: 10.3748/wjg.v19.i31.5178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lida T, Nakase H. Herpes simplex virus esophagitis. QJM. 2019;113((1)):58. doi: 10.1093/qjmed/hcz114. [DOI] [PubMed] [Google Scholar]
- 5.Elliott SY, Kerns FT, Kitchen LW. Herpes esophagitis in immunocompetent adults: report of two cases and review of the literature. W V Med J. 1993;89((5)):188–90. [PubMed] [Google Scholar]
- 6.Mosimann F, Cuénoud PF, Steinhäuslin F, Wauters JP. Herpes simplex esophagitis after renal transplantation. Transpl Int. 1994;7((2)):79–82. doi: 10.1007/BF00336466. [DOI] [PubMed] [Google Scholar]
- 7.Kadayakkara DK, Candelaria A, Kwak YE, Loeser C. Herpes simplex virus-2 esophagitis in a young immunocompetent adult. Case Rep Gastrointest Med. 2016;2016:7603484. doi: 10.1155/2016/7603484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hemstreet MP, Reynolds DW, Meadows J., Jr Oesophagitis: a complication of inhaled steroid therapy. Clin Allergy. 1980;10((6)):733–8. doi: 10.1111/j.1365-2222.1980.tb02158.x. [DOI] [PubMed] [Google Scholar]
- 9.Knobloch J, Schild K, Jungck D, Urban K, Müller K, Schweda EKH, et al. The T-helper cell type 1 immune response to gram-negative bacterial infections is impaired in COPD. Am J Respir Crit Care Med. 2011;183((2)):204–14. doi: 10.1164/rccm.201002-0199OC. [DOI] [PubMed] [Google Scholar]
- 10.Smith LA, Gangopadhyay M, Gaya DR. Catastrophic gastrointestinal complication of systemic immunosuppression. World J Gastroenterol. 2015;21((8)):2542–5. doi: 10.3748/wjg.v21.i8.2542. [DOI] [PMC free article] [PubMed] [Google Scholar]