Naima Thavory Joseph, MD, MPH.
Torri D. Metz, MD, MS.

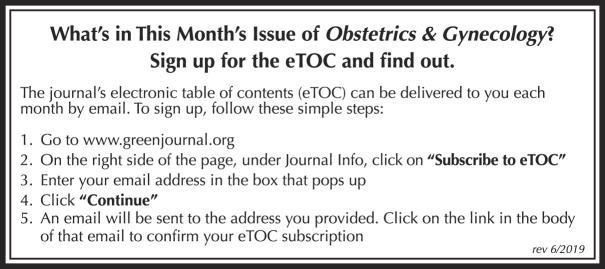
Early in the coronavirus disease 2019 (COVID-19) pandemic, information regarding severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection and pregnancy was limited to case reports. As the number of pregnancies affected by SARS-CoV-2 increased, national and international cohorts were assembled and allowed more valid assessments of the maternal and perinatal risks of SARS-CoV-2 infection. However, initial data were flawed in that they were not derived from nationally representative samples, were subject to bias, and lacked appropriate comparison groups.
In this month's issue of Obstetrics & Gynecology (see page 542), Son et al1 report on more than 800,000 pregnancies from an electronic medical record database comparing pregnancy outcomes before and during the pandemic and outcomes of pregnancies in individuals with and without SARS-CoV-2 infection. By using an electronic medical record database, the authors avert biases in reporting and are able to examine a large, geographically diverse U.S. population. Given the limitation of existing vital statistics, this may be the most representative sample available. The authors found no difference in adverse pregnancy outcomes before and during the pandemic, nor between individuals with and without infection.
With numerous available publications on SARS-CoV-2 infection and pregnancy, we ask how this study contributes to our understanding of pregnancy outcomes during the COVID-19 pandemic and what remains unknown.
International data related to common adverse pregnancy outcomes for the general population are mixed, with the most controversy related to preterm birth. Some studies demonstrate an association between preterm birth and lockdown,2,3 whereas U.S. data have not shown any change.4,5 In the Son et al study, pregnancy during the pandemic was not associated with preterm birth, cesarean delivery, or hypertensive disorders of pregnancy when compared with prepandemic pregnancies. These data are reassuring, especially in light of drastic changes to the structure of prenatal care, including reduced in-office visits, reduced antenatal surveillance, and rapid incorporation of telemedicine.
It is well-established that SARS-CoV-2 infection in pregnancy is associated with adverse perinatal outcomes, although the risks are likely modulated by disease severity and underlying comorbidities. Although Son et al argue that there are no increased perinatal risks with SARS-CoV-2 infection in pregnancy, they were unable to ascertain disease severity. In other large national and international cohort studies, severe infection has been associated with cesarean delivery, hypertensive disorders of pregnancy, and preterm birth.6 Nonetheless, based on the totality of available data, we can be reassured that testing positive for SARS-CoV-2 infection alone is unlikely to have significant pregnancy ramifications and that complications are instead driven by severity of illness. What remains somewhat unclear is how much SARS-CoV-2 infection itself drives adverse outcomes as opposed to clinicians' response to the symptoms and signs of the infection; for example, iatrogenic preterm delivery for deteriorating maternal status. In addition, we do not know whether SARS-CoV-2 infection results in inflammation and placental damage that causes preeclampsia or whether the diagnostic criteria for preeclampsia simply overlap with the signs and symptoms of severe COVID-19.
We need more data examining the association between SARS-CoV-2 infection and stillbirth and pregnancy loss. There are still not enough data to inform risk to pregnancy when SARS-CoV-2 infection is acquired in the first and second trimesters. Some studies have shown increased risk of early pregnancy loss, whereas others have not. In a Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal Fetal-Medicine Units Network study, fetal loss occurred in 4.3% of the severe–critical group compared with 1.9% in the asymptomatic group; however, the sample was predominantly individuals with third-trimester infection and was underpowered to detect a difference.7 Similarly, the INTERCOVID-19 study compared 706 women with COVID-19 with 1,424 women without COVID-19 and found increased risks for low birth weight and severe perinatal morbidity in the COVID-19 group, but differences in perinatal mortality were not reported.8 So, although there is biologic plausibility for heightened risk of stillbirth attendant to COVD-19, the data are not conclusive enough to inform clinical management.
Similarly, more data are needed to ascertain maternal risks. Standardized reporting from the Centers for Disease Control and Prevention National Notifiable Disease Surveillance System demonstrate that pregnancy appears to be independently associated with higher risk for severe disease as defined by hospitalization, intensive care unit admission, mechanical ventilation, extracorporeal membrane oxygenation, and death.9 However, the association between infrequent or rare outcomes, such as venous thromboembolism, is unknown, and it is also unclear how gestational age at viral acquisition mediates maternal disease severity. Pregnant individuals, however, do not experience increased rates of adverse events after SARS-CoV-2 vaccination, with a number of studies demonstrating safety and now efficacy of SARS-CoV-2 vaccination in pregnancy.10 There is also robust evidence of antibody transfer across the placenta for protection of the neonate, with improved efficiency of transfer after vaccination compared with natural infection.11
Finally, the COVID-19 pandemic has unfortunately reiterated the contribution of structural racism, social vulnerability, and social determinants of health to health inequities. Son et al demonstrate that living in the most socioeconomically deprived ZIP codes was associated with significantly higher risks of testing positive for SARS-CoV-2 infection. Other researchers have shown that a disproportionate number of COVID-19 hospitalizations and deaths occur in Black and Hispanic individuals and people with lower socioeconomic status.12 In light of already disparate rates of maternal morbidity and mortality, it will be important to review not only birth outcomes directly attributed to SARS-CoV-2 infection, but also those that may be indirectly related to the COVID-19 pandemic, such as those influenced by changes in care practices or delays in seeking care during the pandemic.
Eighteen months from the start of the pandemic, our understanding of implications of SARS-CoV-2 infection in pregnancy has evolved remarkably. We know that SARS-CoV-2 infection in pregnancy is associated with worse birth outcomes, specifically a higher risk for preterm birth and cesarean delivery, in those with severe disease, and that health system changes to prenatal care delivery are not associated with common adverse pregnancy outcomes. Race and social determinants of health are associated with an increased risk of viral acquisition. Vaccination to prevent SARS-CoV-2 infection is safe and effective in pregnancy, with robust transplacental antibody transfer. What remains lacking is an understanding of whether infection in the first or second trimester affects birth outcomes, how outcomes differ with new SARS-CoV-2 variants, whether the rates of stillbirth and other rare outcomes are increased, and how SARS-CoV-2 infection in pregnancy affects long-term maternal and offspring outcomes.
Footnotes
Financial Disclosure Dr. Joseph disclosed receiving a royalty payment from UpToDate. Dr. Metz disclosed receiving royalties from UpToDate for two topics on trial of labor after cesarean. Money was paid to Dr. Metz's institution from Gestavision (site PI for preeclampsia point-of-care test; money was paid to her institution to conduct the study, which ended August 2020) and Pfizer (site PI for Phase III respiratory syncytial virus [RSV] vaccine trial; money was paid to her institution to conduct the study). Dr. Metz is a member of the Medical Advisory Board of Pfizer (1/15/2021) and site PI for a COVID-19 vaccination trial in pregnancy. She is the Chair of the subcommittee for the NICHD MFMU GRAVID study.
Figure.
No available caption
REFERENCES
- 1.Son M, Gallagher K, Lo JY, Lindgren E, Breden A, Handley SC, et al. Coronavirus disease 2019 (COVID-19) pandemic on pregnancy outcomes in a U.S. population. Obstet Gynecol 2021;138:542–51. doi: 10.1097/AOG.0000000000004547 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Philip RK, Purtill H, Reidy E, Daly M, Imcha M, McGrath D, et al. Unprecedented reduction in births of very low birthweight (VLBW) and extremely low birthweight (ELBW) infants during the COVID-19 lockdown in Ireland: a ‘natural experiment’ allowing analysis of data from the prior two decades. BMJ Glob Heal 2020;5:e003075. doi: 10.1136/bmjgh-2020-003075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Been JV, Ochoa LB, Bertens LC, Schoenmakers S, Steegers EA, Reiss IK. Impact of COVID-19 mitigation measures on the incidence of preterm birth: a national quasi-experimental study. Lancet Public Health 2020;5:e604–11. doi: 10.1016/S2468-2667(20)30223-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Handley SC, Mullin AM, Elovitz MA, Gerson KD, Montoya-Williams D, Lorch SA, et al. Changes in preterm birth phenotypes and stillbirth at 2 Philadelphia hospitals during the SARS-CoV-2 pandemic, March-June 2020. JAMA 2021;325:87–9. doi: 10.1001/jama.2020.20991 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wood R, Sinnott C, Goldfarb I, Clapp M, McElrath T, Little S. Preterm birth during the coronavirus disease 2019 (COVID-19) pandemic in a large hospital system in the United States. Obstet Gynecol 2021;137:403–4. doi: 10.1097/AOG.0000000000004237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Allotey J, Stallings E, Bonet M, Yap M, Chatterjee S, Kew T, et al. Clinical manifestations, risk factors, and maternal and perinatal outcomes of coronavirus disease 2019 in pregnancy: living systematic review and meta-analysis. BMJ 2020;370:m3320. doi: 10.1136/bmj.m3320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Metz TD, Clifton RG, Hughes BL, Sandoval G, Saade GR, Grobman WA, et al. Disease severity and perinatal outcomes of pregnant patients with coronavirus disease 2019 (COVID-19). Obstet Gynecol 2021;137:571–80. doi: 10.1097/AOG.0000000000004339 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Villar J, Ariff S, Gunier RB, Thiruvengadam R, Rauch S, Kholin A, et al. Maternal and neonatal morbidity and mortality among pregnant women with and without COVID-19 Infection: the INTERCOVID Multinational Cohort Study. JAMA Pediatr 2021:e211050. doi: 10.1001/jamapediatrics.2021.1050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zambrano LD, Ellington S, Strid P, Galang RR, Oduyebo T, Tong VT, et al. Update: characteristics of symptomatic women of reproductive age with laboratory-confirmed SARS-CoV-2 infection by pregnancy status—United States, January 22–October 3, 2020. MMWR Morb Mortal Wkly Rep 2020;69:1641–7. doi: 10.15585/mmwr.mm6944e3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shimabukuro TT, Kim SY, Myers TR, Moro PL, Oduyebo T, Panagiotakopoulos L, et al. Preliminary findings of mRNA Covid-19 vaccine safety in pregnant persons. N Engl J Med 2021;384:2273–82. doi: 10.1056/NEJMoa2104983 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Collier AY, McMahan K, Yu J, Tostanoski LH, Aguayo R, Ansel J, et al. Immunogenicity of COVID-19 mRNA vaccines in pregnant and lactating women. JAMA 2021;325:2370–80. doi: 10.1001/jama.2021.7563 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Joseph NT, Stanhope KK, Badell ML, Horton JP, Boulet SL, Jamieson DJ. Sociodemographic predictors of SARS-CoV-2 infection in obstetric patients, Georgia, USA. Emerg Infect Dis2020;26:2787–9. doi: 10.3201/eid2611.203091 [DOI] [PMC free article] [PubMed] [Google Scholar]