Abstract
Background:
Excess deaths during the COVID-19 pandemic compared with those expected from historical trends have been unequally distributed, both geographically and socioeconomically. Not all excess deaths have been directly related to COVID-19 infection. We investigated geographical and socioeconomic patterns in excess deaths for major groups of underlying causes during the pandemic.
Methods:
Weekly mortality data from 27/12/2014 to 2/10/2020 for England and Wales were obtained from the Office of National Statistics. Negative binomial regressions were used to model death counts based on pre-pandemic trends for deaths caused directly by COVID-19 (and other respiratory causes) and those caused indirectly by it (cardiovascular disease or diabetes, cancers, and all other indirect causes) over the first 30 weeks of the pandemic (7/3/2020–2/10/2020).
Findings:
There were 62,321 (95% CI: 58,849 to 65,793) excess deaths in England and Wales in the first 30 weeks of the pandemic. Of these, 46,221 (95% CI: 45,439 to 47,003) were attributable to respiratory causes, including COVID-19, and 16,100 (95% CI: 13,410 to 18,790) to other causes. Rates of all-cause excess mortality ranged from 78 per 100,000 in the South West of England and in Wales to 130 per 100,000 in the West Midlands; and from 93 per 100,000 in the most affluent fifth of areas to 124 per 100,000 in the most deprived. The most deprived areas had the highest rates of death attributable to COVID-19 and other indirect deaths, but there was no socioeconomic gradient for excess deaths from cardiovascular disease/diabetes and cancer.
Interpretation:
During the first 30 weeks of the COVID-19 pandemic there was significant geographic and socioeconomic variation in excess deaths for respiratory causes, but not for cardiovascular disease, diabetes and cancer. Pandemic recovery plans, including vaccination programmes, should take account of individual characteristics including health, socioeconomic status and place of residence.
Funding:
None.
Keywords: Mortality, COVID-19, Deprivation, Causes of death
Research in context.
Evidence before this study
Deaths during the COVID-19 pandemic have been unevenly distributed both geographically and socioeconomically. In our previous study on the COVID-19 pandemic in England and Wales, a fifth of excess deaths during the first wave of the pandemic (7 March to 8 May 2020) were attributable to causes other than COVID-19.
Delayed responses to acute health conditions and exacerbations of pre-existing health conditions led to substantial increases in mortality for a number of diseases, including cardiovascular diseases and diabetes. Mortality rates for some health conditions, including other infectious respiratory diseases, fell, whilst for unnatural causes, including accidents, poisonings and suicides, temporal trends are difficult to discern because several months elapse before coronial inquests are issued.
Added value of this study
By the 30th week of the pandemic in England and Wales, a quarter of all excess deaths were not directly attributable to COVID-19 infection. There were wide variations in all-cause excess deaths across regions, largely driven by deaths due to COVID-19. The highest mortality rates were in the West Midlands and the lowest were in the South West of England and in Wales. Geographic and socioeconomic patterns in excess deaths differed by underlying cause. Whilst there was a strong socioeconomic gradient for respiratory and ‘other’ indirect causes, with the highest rates in the most deprived areas, there was no clear gradient for excess deaths from cardiovascular disease & diabetes, nor cancer.
Implications of all the available evidence
Future plans to manage the pandemic, including decisions about current and future phases of vaccination roll-out, should include understanding of regional and socioeconomic variation and how this has exacerbated long-standing health inequalities. Current strategies recognise this, but this response needs to be sustained to address the underlying health inequalities that placed certain groups at greater risk during the pandemic, using both public health measures and wider socioeconomic interventions. Immediate and longer-term recovery planning for communities and their health and social services should reflect historical disparities as well as the COVID-19 related patterns described in this study.
Alt-text: Unlabelled box
1. Introduction
Excess deaths (the number of deaths above the expected average for a given period in a population) is a valuable measure of the impact of pandemics because cause of death may not be accurately reported, particularly in the early stages when awareness and diagnostic tools are limited, or where there is asymptomatic disease. Pandemics may also lead to increases in deaths for causes other than the infectious disease; of the estimated 47,243 excess deaths in England and Wales during the first ten weeks of the COVID-19 pandemic, 9948 (21%) were reported as being caused indirectly by COVID-19 [1]. Although some of these deaths will have been undiagnosed COVID-19 cases, public and institutional responses to the pandemic also affected mortality risks for a range of other conditions. Pressure on health services and social care sectors reduced the supply of non-urgent diagnostic and treatment services [2,3] and, to avoid the risk of COVID-19 infection, people were less likely to use healthcare services [4,5]. Delayed responses to acute health conditions and exacerbations of pre-existing health conditions led to substantial increases in mortality for a number of diseases, including cardiovascular diseases [6,7] and diabetes [8,9]. Conversely, mortality rates for some health conditions, including other infectious respiratory diseases, fell [10], whilst for unnatural causes, including accidents, poisonings and suicides, temporal trends are difficult to discern because several months elapse before coronial inquests are issued [11,12]. For some other health conditions, such as cancer, the full impact of the pandemic on delayed diagnoses and mortality is not yet known [13].
The risk of being infected with COVID-19 has followed sociodemographic and geographical patterns. Higher infection rates are recorded both for socioeconomically deprived and minority ethnic groups in the population, in part because these groups continued to work outside the home as keyworkers and often in non-COVID-secure environments. Furthermore, these groups are typically more likely to have pre-existing medical conditions such as heart disease or diabetes. Complex geographical patterns have also emerged: in the first wave, London, then the West Midlands and northern regions had the highest rates of COVID-19 deaths. However, evidence on non-COVID deaths during the pandemic is less clear; and it is unknown whether they follow similar geographic and social patterns, or whether they vary by cause of death. It is also unclear whether socioeconomic and regional/geographic patterns in deaths changed after the first wave. Therefore, we extended our previous analysis of geographical and socioeconomic patterns in excess deaths [1], up until the first 30 weeks of the pandemic, for the major underlying causes of death. The patterns that emerge are important because they could influence later phases of vaccination roll-out and COVID-19 recovery planning for local communities.
2. Methods
2.1. Data
Deaths registered in England and Wales from 27/12/2014 until 01/03/2021 were accessed using the secure Amazon Workspaces environment setup by NHS Digital. To minimise the effect of delayed death registration, the observation period was from the 1st week of 2015 (ending 2nd Jan) to the 40th week of 2020 (ending 2nd Oct). For each death, the underlying cause (defined as the disease or injury that initiated the series of events leading directly to death, or the circumstances of the accident or violence that produced the fatal injury [14]) and up to 15 contributory causes are recorded on the death certificate. Additional information in the database included: unique NHS identifier, age, sex, registered date of death, residence postcode and place of death category.
Using residential postcodes, the database was linked to Lower Super Output Areas (LSOAs), which are small geographical areas containing a median of around 1500 residents. Additional information was linked through LSOAs, including region, population sizes by age and sex strata, and socioeconomic deprivation information. Deprivation was measured using the Indices of Multiple Deprivation (IMD), a composite score across seven domains: income, employment, health, education & skills, housing, crime and environment. Deprivation rankings and scores change very little over time [15], and so we used the latest available IMDs reported as scores (for 2019 in England and 2014 in Wales). Population estimates at the LSOA level were available from the ONS up to 2019 [16], and were extrapolated to 2020 using linear regression. Regional information pertained to the 10 former Strategic Health Authorities in England plus Wales.
Deaths were organised in two main categories: direct or indirect. Direct included deaths where the underlying cause of death was attributed to COVID-19 (ICD-10 code U071 virus identified, or U072 virus not identified), plus respiratory deaths (J00–J99). This aggregation was used because coding of COVID-19 varied over the study's observation period, with an unknown number of COVID-19 deaths being attributed to other respiratory diseases, especially in the early stages of the pandemic and in care homes. For comparison, we also present and model non-COVID-19 respiratory deaths separately. We examined three subcategories of indirect death: cardiovascular and diabetes (ICD-10 codes: I00–I99 and E10-E14, except for I426 alcoholic cardiomyopathy), since these are closely related disorders; cancer (ICD-10 codes: C00–D48); and other indirect deaths (including drug-related and alcohol-related deaths, suicides, accidents and all other causes). The latter category included those deaths where the cause was still under investigation by the coroner, which are most likely to be external causes of death [17]. Subcategories of indirect deaths were selected because they are common, are likely to have been affected by limited elective access because of the pandemic, and are robust to time-lags in coronial verdicts. Each subcategory was modelled separately. Categories were mutually exclusive; for example, cardiovascular deaths did not include alcoholic cardiomyopathy, which was included in the ‘other indirect’ category. ‘Other’ deaths include a very small number of cases (<2000 each year) where there was no underlying cause of death, or where the cause is being further investigated.
The study was conducted using aggregated national mortality data; ethical approval was, therefore, not needed. No specific funding was obtained for this study, the academic institutions funding the time of the authors (and Abbot and BMS for CG) had no role in the design and conduct of the study.
2.2. Analyses
Data were imported, cleaned and formatted as a time series in Stata v16. Death counts for each category were aggregated initially without stratification and then across the following strata: by deprivation quintile, by place of death, by place of death interacted with deprivation quintile, by region, and by region interacted with deprivation quintile. Aggregated datasets were extracted from the secure environment and analysed locally. We used a similar model for each outcome examined across the stratified data aggregations. To model excess mortality, data from week 9 in 2020 (22–28 February), two weeks before the first officially confirmed COVID-19 related deaths (7–13 March), were set to missing. Negative binomial regression models were fitted to weekly death counts in the pre-pandemic period, with covariates of week (categorical – to account for seasonality), and time in weeks (continuous – to account for a potential slope). To account for lags in reporting, the models also included: number of bank holidays in the week, whether the Friday of the previous week was a bank holiday, and whether the Friday of the current week was a bank holiday (weeks run from Saturday to Friday). Separate models were fitted to examine excess mortality by subgroup: sex, age group, region (as defined by former Strategic Health Authority), deprivation quintile, and place of death (care home, home, hospice, hospital or other/unknown). These models included additional respective categorical predictors, and their interaction terms with time, to allow for varying time-trends by stratum, respectively.
To account for differences in population totals, within subgroup and over time, for each model, the natural logarithm of the annual population estimate for each respective stratum was applied as the offset. We selected negative binomial regression models over Poisson models because of high variation in the outcome variable that is likely to cause over-dispersion. For weeks 11 (7 to 13 March) to 40 (29 Aug to 2 Oct 2020), from each model the exponentiated linear prediction (and its 95% confidence intervals), which provides an estimate of the expected death count, was subtracted from the respective observed event count to give an estimate of excess deaths. Excess death count and rate estimates, for each stratum and overall, were aggregated across all weeks in the COVID-19 observation period, with a pooled estimate for the standard error used to obtain the 95% confidence intervals. Additional figures by each categorisation of interest are provided in the supplementary file.
3. Results
3.1. Respiratory deaths
Between 7 Mar 2020 and 2 Oct 2020, there were an estimated 46,221 (95% CI: 45,439 to 47,003) excess deaths in England and Wales attributed to COVID-19 or another underlying respiratory cause (direct deaths, Table 1). Of these, 26,336 were deaths in males and 19,885 deaths in females. There was a steep upward gradient in the death count with increasing age: estimated excess direct deaths ranged from −11 for ages 0–14 to 18,800 for ages 85 years and over. There was also a clear deprivation gradient, ranging from 7883 excess deaths in the most affluent quintile to 10,750 in the most deprived. Most direct deaths occurred in hospitals (26,206), followed by care homes (15,261) and private homes (3739). Excluding COVID-19 deaths, there were an estimated −2710 excess respiratory deaths in England and Wales, i.e. there were fewer than expected deaths from respiratory diseases other than COVID-19. This applied to all age groups, except for ages 45–65.
Table 1.
Estimated counts of direct, indirect and total excess deaths, weeks 11 to 40 (7 Mar 2020 to 2 Oct 2020).
| Direct | Indirect | |||||
|---|---|---|---|---|---|---|
| COVID or other respiratory | Other respiratory only | Cardiovascular and diabetes | Cancer | Other indirect deaths | Any cause | |
| England and Wales | 46,221 (45,439,47,003) | −2710 (−3492,−1928) | 6887 (5999,7774) | 1668 (289,3047) | 7056 (5693,8418) | 62,321 (58,849,65,793) |
| Sex | ||||||
| Males | 26,336 (26,041,26,631) | −768 (−1063,−473) | 3486 (3125,3847) | 857 (531,1183) | 1649 (1180,2118) | 32,825 (31,529,34,121) |
| Females | 19,885 (19,591,20,179) | −1942 (−2236,−1648) | 3388 (3075,3702) | 812 (527,1097) | 5307 (4736,5877) | 29,437 (28,150,30,724) |
| Age groups | ||||||
| 0–14 | −11 (−13,−9) | −14 (−16,−12) | 4 (1,6) | −5 (−9,−1) | −37 (−56,−19) | −57 (−75,−39) |
| 15–44 | 512 (506,518) | −11 (−17,−5) | 237 (224,249) | 20 (6,34) | −214 (−271,−157) | 534 (464,605) |
| 45–65 | 4671 (4635,4708) | 17 (−19,54) | 1379 (1314,1444) | 417 (329,505) | 397 (306,488) | 6925 (6686,7165) |
| 65–74 | 6776 (6697,6855) | −397 (−476,−318) | 1050 (965,1136) | 486 (358,615) | 292 (206,377) | 8596 (8270,8921) |
| 75–84 | 14,768 (14,619,14,918) | −1051 (−1200,−902) | 1359 (1199,1520) | 681 (517,845) | 1279 (1070,1489) | 17,789 (17,214,18,364) |
| 85+ | 18,800 (18,589,19,012) | −1959 (−2170,−1747) | 1907 (1673,2142) | −500 (−621,−378) | 2808 (2348,3267) | 22,146 (21,264,23,028) |
| Regions | ||||||
| North East | 2531 (2508,2553) | −208 (−231,−186) | 316 (291,341) | 67 (39,94) | 390 (351,428) | 3303 (3220,3386) |
| North West | 6990 (6933,7047) | −559 (−616,−502) | 488 (427,549) | 168 (107,228) | 1165 (1079,1251) | 8782 (8579,8985) |
| Yorkshire & Humber | 4349 (4311,4387) | −260 (−298,−222) | 469 (423,516) | 128 (79,176) | 314 (248,381) | 5295 (5145,5446) |
| East Midlands | 3478 (3447,3509) | −245 (−276,−214) | 733 (692,773) | 203 (160,247) | 310 (251,369) | 4750 (4621,4879) |
| West Midlands | 5255 (5215,5296) | −223 (−263,−182) | 1106 (1055,1156) | 293 (242,344) | 1044 (973,1114) | 7730 (7564,7896) |
| East of England | 4616 (4577,4655) | −174 (−213,−135) | 463 (408,518) | −39 (−92,14) | 879 (803,956) | 5995 (5821,6169) |
| London | 8134 (8103,8166) | 15 (−16,47) | 855 (809,902) | 116 (71,162) | 1154 (1092,1217) | 10,311 (10,166,10,456) |
| South East Coast | 3516 (3483,3548) | −201 (−234,−169) | 774 (734,815) | 359 (316,402) | 829 (767,892) | 5532 (5395,5669) |
| South Central | 2924 (2900,2948) | −145 (−169,−121) | 648 (616,680) | 147 (110,183) | 294 (246,342) | 4043 (3938,4147) |
| South West | 2465 (2429,2502) | −263 (−299,−226) | 846 (794,898) | 327 (274,380) | 703 (629,776) | 4410 (4243,4577) |
| Wales | 2057 (2030,2084) | −285 (−312,−258) | 367 (333,400) | −30 (−62,2) | 139 (97,181) | 2546 (2448,2644) |
| Deprivation quintiles | ||||||
| 1 (least deprived) | 7883 (7812,7955) | −617 (−688,−545) | 1227 (1131,1323) | 453 (357,549) | 1034 (890,1178) | 10,770 (10,427,11,113) |
| 2 | 8715 (8633,8796) | −587 (−669,−506) | 1137 (1034,1241) | 71 (−31,172) | 1358 (1205,1511) | 11,414 (11,046,11,782) |
| 3 | 9085 (9000,9169) | −456 (−541,−372) | 1746 (1640,1851) | 228 (128,328) | 1489 (1334,1644) | 12,649 (12,279,13,018) |
| 4 | 9838 (9749,9926) | −581 (−670,−493) | 1301 (1197,1405) | 446 (353,538) | 1440 (1296,1584) | 13,053 (12,698,13,408) |
| 5 (most deprived) | 10,750 (10,653,10,848) | −351 (−448,−253) | 1668 (1566,1770) | 542 (448,635) | 1878 (1729,2027) | 14,789 (14,424,15,154) |
| Place of death | ||||||
| Care home | 15,261 (15,188,15,335) | 879 (806,953) | 2736 (2635,2836) | −917 (−1000,−835) | 6377 (6005,6748) | 23,280 (22,778,23,781) |
| Home | 3739 (3642,3835) | 1598 (1501,1694) | 6667 (6481,6852) | 10,665 (10,498,10,833) | 4952 (4782,5121) | 26,141 (25,633,26,650) |
| Hospice | 361 (351,370) | −86 (−96,−77) | −3 (−14,8) | −2186 (−2278,−2094) | −125 (−143,−107) | −1603 (−1734,−1473) |
| Hospital | 26,206 (25,886,26,526) | −5256 (−5576,−4936) | −3082 (−3379,−2786) | −6655 (−6854,−6456) | −5143 (−5546,−4740) | 10,034 (9060,11,008) |
| Other/ Unknown | 647 (639,654) | 148 (140,155) | 249 (225,272) | 749 (735,762) | −53 (−97,−8) | 1565 (1499,1632) |
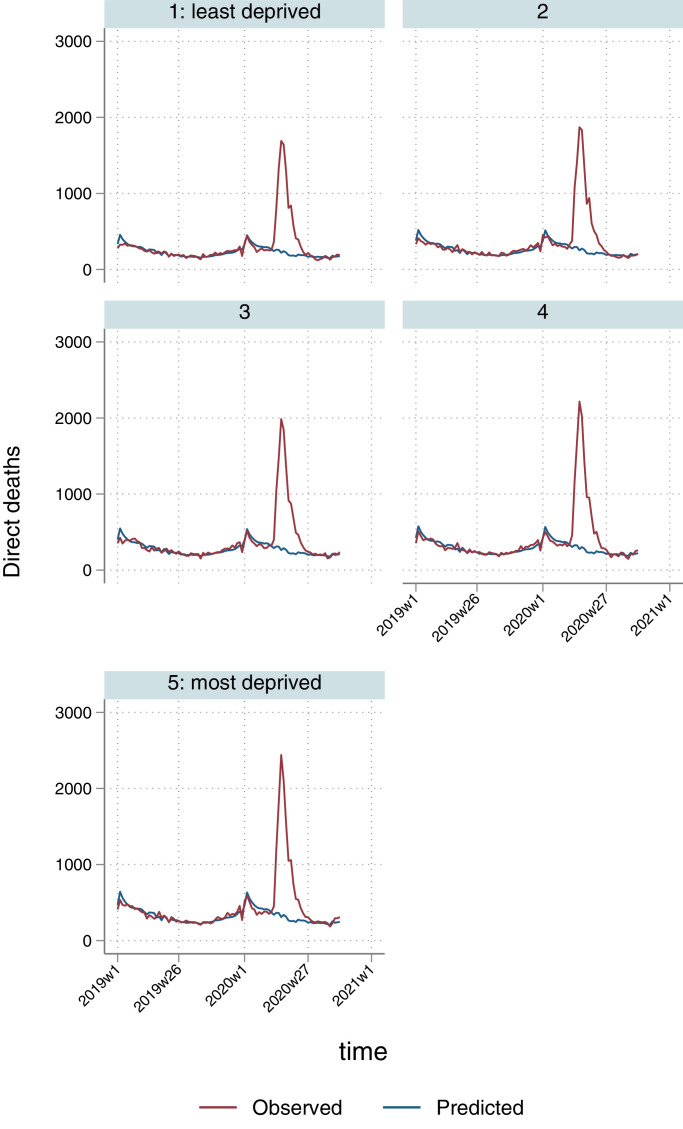
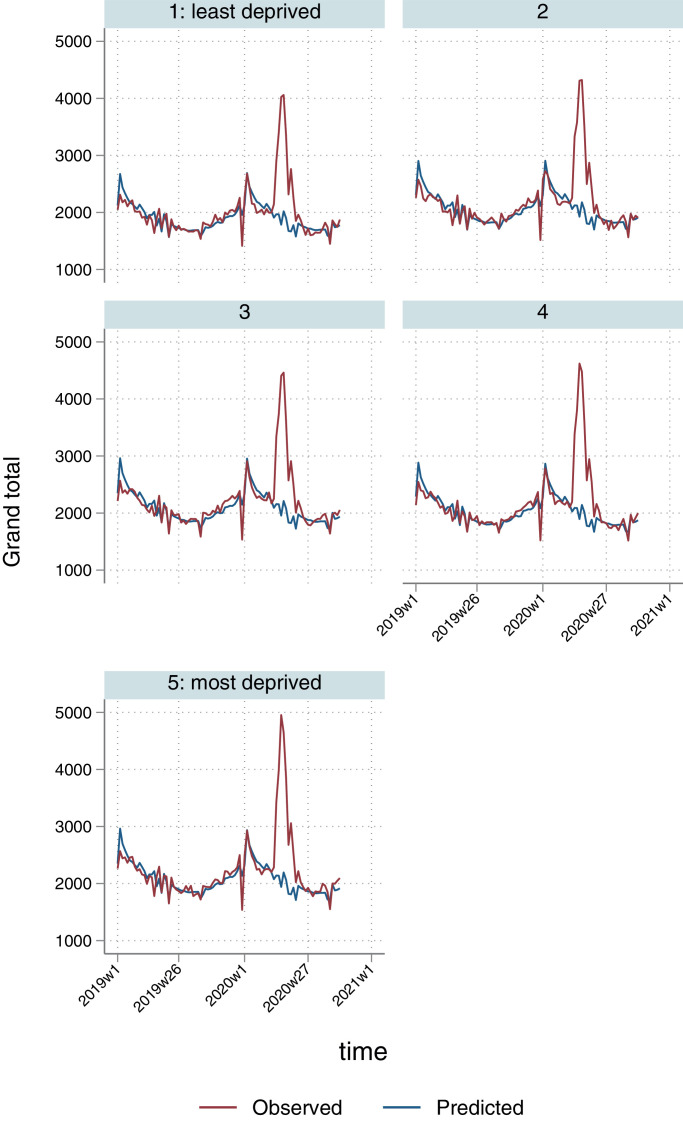
The overall excess mortality rate for England and Wales directly attributed to COVID-19 infection or respiratory causes was 77 per 100,000 population (Table 2), but there was substantial regional variation: rates ranged from 44 per 100,000 in the South West to 95 per 100,000 in the North West. By age group, direct deaths ranged from 0 per 100,000 for ages 0–14 to 1241 per 100,000 for ages 85 or over. In terms of area-level deprivation, rates ranged from 68 per 100,000 for the most affluent quintile to 90 per 100,000 for the most deprived, reflecting higher spikes in more deprived regions and localities during the first phase of the pandemic (April to July 2020; Fig. 1).
Table 2.
Rates of direct, indirect and total excess deaths per 100,000 population, weeks 11 to 40 (7 Mar 2020 to 2 Oct 2020).
| Direct | Indirect | |||||
|---|---|---|---|---|---|---|
| COVID or other respiratory | Other respiratory only | Cardiovascular and diabetes | Cancer | Other indirect deaths | Any cause | |
| England and Wales | 77 (76,79) | −5 (−6,−3) | 12 (10,13) | 3 (0,5) | 12 (10,14) | 104 (98,110) |
| Sex | ||||||
| Males | 89 (88,90) | −3 (−4,−2) | 12 (11,13) | 3 (2,4) | 6 (4,7) | 111 (107,115) |
| Females | 66 (65,67) | −6 (−7,−5) | 11 (10,12) | 3 (2,4) | 18 (16,19) | 97 (93,102) |
| Age groups | ||||||
| 0–14 | 0 (0,0) | 0 (0,0) | 0 (0,0) | 0 (0,0) | 0 (−1,0) | −1 (−1,0) |
| 15–44 | 2 (2,2) | 0 (0,0) | 1 (1,1) | 0 (0,0) | −1 (−1,−1) | 2 (2,3) |
| 45–65 | 31 (30,31) | 0 (0,0) | 9 (9,9) | 3 (2,3) | 3 (2,3) | 45 (44,47) |
| 65–74 | 114 (112,115) | −7 (−8,−5) | 18 (16,19) | 8 (6,10) | 5 (3,6) | 144 (139,149) |
| 75–84 | 397 (393,401) | −28 (−32,−24) | 37 (32,41) | 18 (14,23) | 34 (29,40) | 479 (463,494) |
| 85+ | 1241 (1227,1254) | −129 (−143,−115) | 126 (110,141) | −33 (−41,−25) | 185 (155,216) | 1461 (1403,1519) |
| Regions | ||||||
| North East | 94 (94,95) | −8 (−9,−7) | 12 (11,13) | 2 (1,4) | 15 (13,16) | 123 (120,126) |
| North West | 95 (94,95) | −8 (−8,−7) | 7 (6,7) | 2 (1,3) | 16 (15,17) | 119 (116,122) |
| Yorkshire & Humber | 79 (78,79) | −5 (−5,−4) | 8 (8,9) | 2 (1,3) | 6 (4,7) | 96 (93,99) |
| East Midlands | 71 (71,72) | −5 (−6,−4) | 15 (14,16) | 4 (3,5) | 6 (5,8) | 98 (95,100) |
| West Midlands | 88 (87,89) | −4 (−4,−3) | 19 (18,19) | 5 (4,6) | 17 (16,19) | 130 (127,132) |
| East of England | 74 (73,74) | −3 (−3,−2) | 7 (7,8) | −1 (−1,0) | 14 (13,15) | 96 (93,98) |
| London | 90 (90,91) | 0 (0,1) | 9 (9,10) | 1 (1,2) | 13 (12,13) | 114 (113,116) |
| South East Coast | 73 (73,74) | −4 (−5,−4) | 16 (15,17) | 7 (7,8) | 17 (16,19) | 115 (112,118) |
| South Central | 66 (65,67) | −3 (−4,−3) | 15 (14,15) | 3 (2,4) | 7 (6,8) | 91 (89,94) |
| South West | 44 (43,44) | −5 (−5,−4) | 15 (14,16) | 6 (5,7) | 12 (11,14) | 78 (75,81) |
| Wales | 65 (64,66) | −9 (−10,−8) | 12 (11,13) | −1 (−2,0) | 4 (3,6) | 80 (77,83) |
| Deprivation quintiles | ||||||
| 1 (least deprived) | 68 (67,69) | −5 (−6,−5) | 11 (10,11) | 4 (3,5) | 9 (8,10) | 93 (90,96) |
| 2 | 74 (73,74) | −5 (−6,−4) | 10 (9,10) | 1 (0,1) | 11 (10,13) | 97 (93,100) |
| 3 | 75 (74,75) | −4 (−4,−3) | 14 (13,15) | 2 (1,3) | 12 (11,14) | 104 (101,107) |
| 4 | 80 (79,81) | −5 (−5,−4) | 11 (10,11) | 4 (3,4) | 12 (11,13) | 106 (104,109) |
| 5 (most deprived) | 90 (89,91) | −3 (−4,−2) | 14 (13,15) | 5 (4,5) | 16 (14,17) | 124 (121,127) |
| Place of death | ||||||
| Care home | 26 (25,26) | 1 (1,2) | 5 (4,5) | −2 (−2,−1) | 11 (10,11) | 39 (38,40) |
| Home | 6 (6,6) | 3 (3,3) | 11 (11,11) | 18 (18,18) | 8 (8,9) | 44 (43,45) |
| Hospice | 1 (1,1) | 0 (0,0) | 0 (0,0) | −4 (−4,−4) | 0 (0,0) | −3 (−3,−2) |
| Hospital | 44 (43,44) | −9 (−9,−8) | −5 (−6,−5) | −11 (−11,−11) | −9 (−9,−8) | 17 (15,18) |
| Other/ Unknown | 1 (1,1) | 0 (0,0) | 0 (0,0) | 1 (1,1) | 0 (0,0) | 3 (3,3) |
Fig. 1.
Temporal patterns in excess direct death rates per 100,000 population by deprivation quintile.
3.2. Cardiovascular and diabetes deaths
In addition to deaths directly attributed to COVID-19 and other respiratory causes, there was also an increase in cardiovascular and diabetes deaths, with an estimated 6887 (95% CI: 5999 to 7774) excess deaths nationally, with similar numbers for males and females. The highest number of excess deaths occurred in the 85 years and over age group (1907), followed by the 45–65 (1379) and 75–84 (1359) age groups. There was no socioeconomic gradient evident in these excess deaths. There were fewer than expected cardiovascular and diabetes deaths in hospitals (−3082) but more in private homes (6667) and care homes (2736).
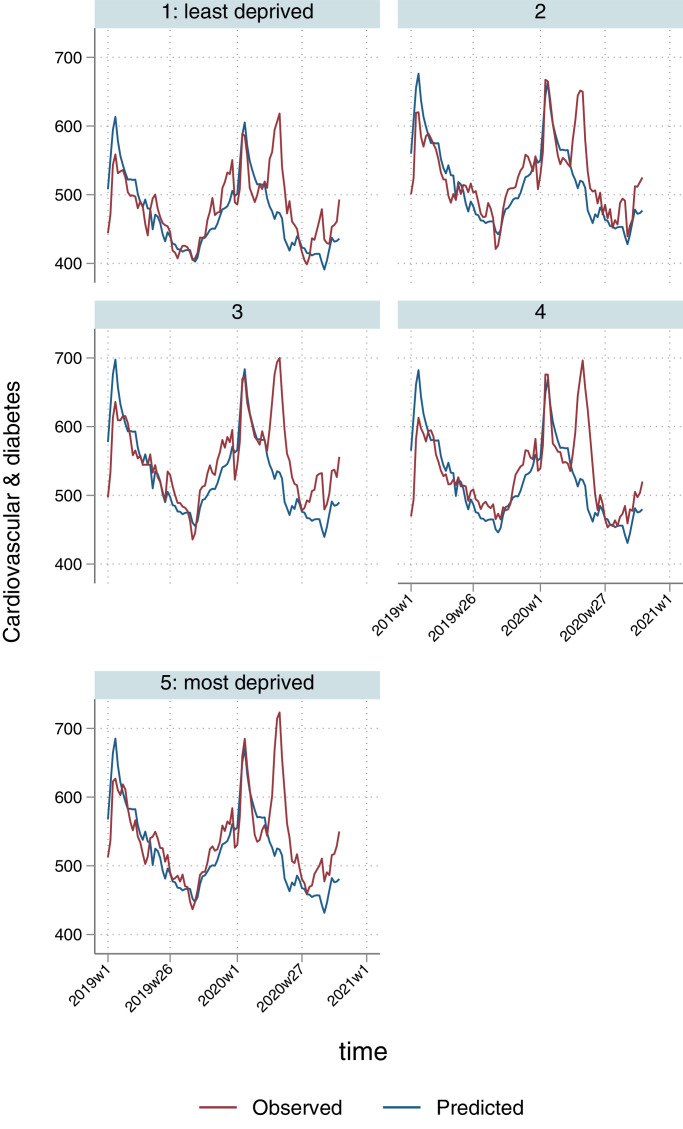
Nationally, most of excess deaths due to cardiovascular disease/diabetes occurred during the first half of the first wave of the pandemic (April to mid-May), with a second, smaller increase from mid-July to August (Fig. 2). There were 12 excess direct deaths per 100,000 of the population, ranging from 7 per 100,000 in the North West and East of England to 19 per 100,000 in the West Midlands. Rates ranged for deprivation quintiles from 11 per 100,000 for quintile 2 to 14 per 100,000 for quintiles 3 and 5.
Fig. 2.
Temporal patterns in excess cardiovascular and diabetes death rates per 100,000 population by deprivation quintile.*
* 3-week smoothed.
3.3. Cancer deaths
Nationally, there were 1668 (95% CI: 289 to 3047) excess cancer deaths over the study period, ranging from −500 in those aged 85 or over to 681 in ages 75–84. Numbers of excess deaths were similar in females and males. More deaths were recorded in the most deprived quintile, although there was no clear gradient. There were fewer than expected deaths in hospitals (−6655), hospices (−2186), and care homes (−917), but more in private homes (10,665).
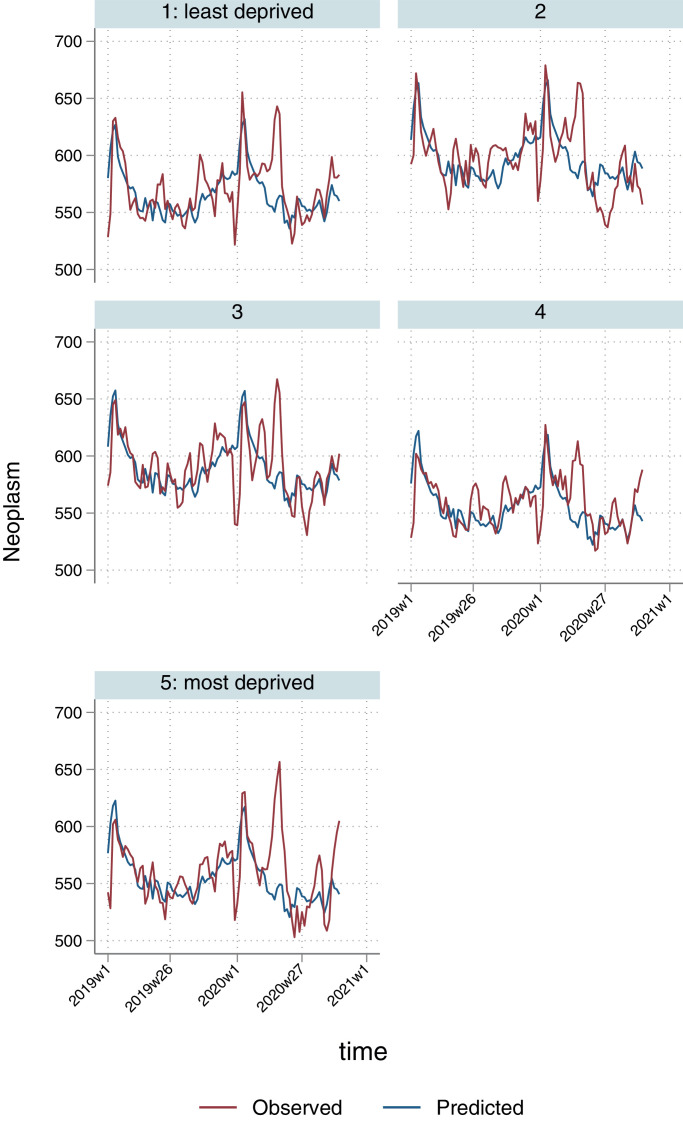
We estimated 3 excess cancer deaths per 100,000 population nationally, ranging from −1 per 100,000 in the East of England and in Wales to 7 per 100,000 in the South East Coast region. The highest rates were in the 65–75 and 75–84 age groups, with 8 and 18 excess deaths per 100,000, respectively. There was no clear linear socioeconomic gradient, but with the most excess deaths per 100,000 population observed in the most deprived quintile (5 per 100,000). For the quintiles with the most excess deaths, we observed the same pattern as for cardiovascular and diabetes deaths, with a primary spike during the first wave of the pandemic and a secondary increase from July onwards (Fig. 3). For other deprivation quintiles, there was also a sharp increase in excess deaths during the first wave followed by a period of fewer than expected deaths from July onwards.
Fig. 3.
Temporal patterns in excess cancer deaths per 100,000 population by deprivation quintile*
* 3-week smoothed.
3.4. Other indirect deaths (including drug-related and alcohol-related deaths, suicides, fatal accidents, and all other causes)
There were 7056 (95% CI: 5693 to 8418) excess deaths from other indirect causes over the study period (Table 1). A large difference was observed between female (5307) and male (1649) deaths. There were fewer than expected deaths for ages 0–14 (−37) and 15–44 (−214), increasing to 2808 for ages 85 or over. Excess deaths ranged from 1034 in the most affluent quintile to 1878 in the most deprived. Again, there was a shift from deaths in hospital (−5143) to deaths in care homes (6377) and private homes (4952).
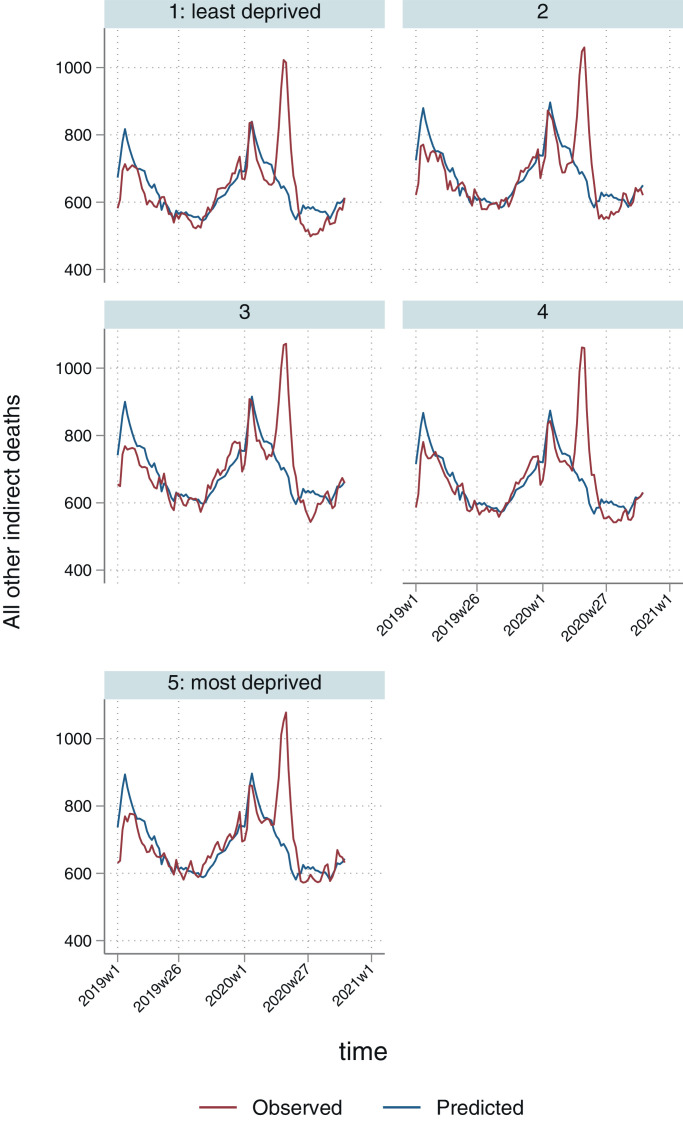
There were 12 excess other indirect deaths per 100,000 for England and Wales (Table 2), ranging from 4 per 100,000 in Wales to 17 per 100,000 in the West Midlands and South East Coast. The highest rates were for ages 85 or over (185 per 100,000) and lowest for ages 15–44 (−1 per 100,000). Rates ranged from 9 excess deaths per 100,000 in the most affluent quintile to 16 per 100,000 in the most deprived. For all quintiles, there was a sharp increase in other indirect excess deaths during the first part of the first wave of the pandemic, immediately followed by a period of fewer than expected deaths from June to August (Fig. 4).
Fig. 4.
Temporal patterns in ‘other’ excess indirect deaths per 100,000 population by deprivation quintile.*
* 3-week smoothed.
3.5. All-cause excess deaths
For all causes of death combined, there were 62,321 (95% CI: 58,849 to 65,793) excess deaths in a total of 346,502 during the study period across England and Wales. The number of excess deaths was higher for males (32,825) compared to females (29,437). There was a clear age gradient with −57 excess deaths for ages 0–14, increasing to 22,146 for ages 85 or over. The highest number of excess deaths was in the most deprived quintile (14,789) and the lowest in the least deprived (10,770).
There were 104 excess deaths per 100,000 nationally, ranging from 78 per 100,000 in the South West to 130 per 100,000 in West Midlands; and from −1 per 100,000 in ages 0–14 to 1461 per 100,000 in ages 85 or over. Excess deaths per 100,000 population ranged from 93 in the most affluent quintile to 124 in the most deprived. Patterns were broadly similar to those for deaths caused directly by COVID-19 or other respiratory causes, which comprised the majority of excess deaths over the study period (Fig. 5).
Fig. 5.
Temporal patterns in overall excess deaths per 100,000 population by deprivation quintile.
Supplementary file Table 1 presents total observed deaths across each category, and percentages of excess deaths in relation to these totals.
4. Discussion
Compared with historical trends in the past 5 years, we estimate that there were 62,321 excess deaths (104 per 100,000 population) in England and Wales during the first 30 weeks of the COVID-19 pandemic. Of these, 46,221 (74.2%) were from respiratory causes, including COVID-19. and 16,100 (25.8%) were from other causes. There were marked regional variations in all cause excess deaths, ranging from 78 per 100,000 in the South West to 130 per 100,000 in the West Midlands, largely driven by deaths from COVID-19 infection. Regional and socioeconomic patterns in excess deaths differed by cause; the highest numbers of excess deaths occurred in the most deprived areas in England and Wales across all groups, but there was no clear linear gradient for cardiovascular and diabetes or cancer deaths.
4.1. Strengths and limitations
Our analysis provides a comprehensive picture of excess deaths during the first 30 weeks of pandemic, including major causes both related and unrelated to COVID-19 infection. This enabled us to estimate the total impact of the pandemic on mortality, including regional and socioeconomic patterns. There are some limitations to our study. For deaths not referred for investigation and adjudication by a coroner, data on cause of death rely on accurate reporting, diagnosis and recording by clinicians through the use of ICD-10 codes. During a pandemic, assessing the contribution of COVID-19 to some deaths can be challenging [11]. We defined COVID-19 deaths as those for which the underlying cause was attributed to COVID-19 on the death certificate, and, inevitably, there will have been misclassification, particularly in the early part of the pandemic when COVID-19 testing was not widespread and doctors’ awareness may have been more limited [18,19]. This is also a problem for estimating deaths caused indirectly by the pandemic, so in addition to excluding COVID-19 deaths from the total excess deaths, we also excluded other respiratory causes of death (the most likely source of ‘missed’ COVID-19 diagnoses). Furthermore, this approach enabled us to apply data from earlier years to create a reference ‘baseline’, in the absence of COVID-19 deaths occurring before 2020. Consequently, our estimates of excess deaths that occurred as an indirect effect of the pandemic are unlikely to include substantial numbers of deaths caused directly by COVID-19 infection, but they also do not include respiratory deaths not attributable to COVID-19. The aggregates of weekly estimates included negative estimates (i.e. not set to zero), to allow for more conservative estimates. Finally, time-lags for coronial verdicts will have been long for many cases, particularly for external causes such as accidents and suicides, and we are therefore unable to determine excess deaths within these categories. We categorised groups to minimise the impact of these time-lags, with the most affected causes contributing to a single group along with those whose causes remained undetermined (‘other indirect deaths’).
4.2. Clinical interpretation and implications of findings
There were an estimated 46,221 excess respiratory deaths in England and Wales during the first 30 weeks of the COVID-19 pandemic (77 deaths per 100,000 population). Pre-existing conditions like cardiovascular disease and diabetes are known to increase susceptibility to death from COVID-19 infection [20]. However, we found that mortality rates for both of these conditions also increased in the absence of a COVID-19 diagnosis, resulting in another 6887 excess deaths. We have previously reported that the volume of hospital admissions decreased, and overall mortality rates for acute coronary syndromes and heart failure increased during the first and second COVID-19 waves, and that decreased elective capacity for treatment of time-sensitive coronary artery disease interventions is also likely to have contributed to excess cardiovascular mortality risk [7,21,22]. The highest number of excess cardiovascular/diabetes deaths was observed in the 85 or over age group; in addition to delays in seeking care, misclassification of the underlying cause could explain this finding, especially in the early stages of the pandemic. COVID-19 is known to have prothrombotic effects with increases in both arterial and venous thromboembolic events [23] that can exacerbate existing cardiovascular problems and lead to cardiovascular deaths. Furthermore, co-infection with COVID-19 increases the mortality of acute cardiovascular conditions such as acute coronary syndromes and stroke [24,25]. Worryingly, the age group with the second highest number of excess cardiovascular/diabetes deaths (after those aged 85 or over) was those aged 45–65, a young population that would particularly benefit from early invasive treatment of conditions such as acute coronary syndromes and critical valvular heart disease [26]. NHS guidance already states that patients with sudden onset chest pain or severe symptoms suggestive of heart failure should seek emergency medical help; and therefore reinforcing these messages may help to prevent avoidable deaths. Similarly, the data on excess diabetes-related deaths is of great concern. At this stage of the pandemic, it is important that people living with diabetes attend hospital if they have symptoms suggesting life-threatening diabetes-related emergencies such as hyperosmolar hyperglycaemic state or ketoacidosis. As for cancer, the full impact of the lower screening rates, delays in chemo- and radiation therapy due to the pandemic, and deaths from thrombotic events related to COVID-19 in combination with cancer will not be known until years from now [13]. The large excess in care homes and private homes has previously been reported and it reflects discharge and admission policies that were affected by the pandemic, especially during the first wave [27].
There were a further 1668 excess cancer deaths (3 per 100,000 population) and 7056 excess deaths from all other causes (12 per 100,000 population). These excesses are largely the result of spikes occurring during the first wave of COVID-19, suggesting that COVID-19 infection may have been directly involved in many of these excess deaths. By definition the ‘other’ cause of death category is very broad and varies in composition by age. Overall, dementia is by far the largest contributor to ‘other’ causes of death, and was associated with a quarter of COVID-19 deaths during the first wave [28]. Whether diagnosed or not, COVID-19 will have hastened the death of many people approaching the end of life and who, under normal circumstances, may have died later of a pre-existing disease. This is likely to explain much of the negative ‘excess’ in cancer and other indirect causes of death observed over the summer months, when direct COVID-19 deaths were subsiding. Some of the reduction may also be explained by reduced risk of dying from road traffic accidents, other accidents and injuries as a result of lockdown restrictions. However, although lockdowns reduced the volume of road traffic and the frequency of minor collisions in most areas, rates of fatal road traffic accidents did not necessarily fall in all areas [29]. Early evidence indicated a marked deterioration in population mental health in the UK during the first COVID-19 wave [30], leading to predictions of an increase in suicide rates. Expedited analysis of ‘probable suicide’ cases indicates that suicide risk did not, in fact, rise between the Spring and Autumn of 2020 in the UK [31], and other high-income western countries, although rates did rise in Japan [32].
Geographic variations in death are expected during a pandemic. Over the first 30 weeks of the pandemic, the highest excess mortality rates in England and Wales were in the West Midlands, the North East, and the North West. Although these are not bordering regions, they are well-connected with the capital and include some of the most deprived areas in England. Geographic variation also reflects: population susceptibility, in terms of age and pre-existing disease; local factors such as housing density, transport infrastructure and air quality; concentration of ‘essential’ workplaces such as factories and warehouses (some without appropriate infection prevention practices and protective equipment); a population's occupational mix and ability and willingness to engage in public health measures such as social distancing; and the capacity and quality of local public health, social and healthcare services. Socioeconomic factors are a key driver of regional variation in mortality rates but, whilst there was a clear socioeconomic gradient in COVID-19 and ‘other’ indirect deaths, no such gradient was evident for cardiovascular disease, diabetes and cancer deaths. The absence of the usual association between socioeconomic status and excess mortality from these conditions may reflect higher mortality from COVID-19 among more vulnerable populations being concentrated in more deprived areas during the study period. It is important to note, however, that underlying the trends in excess deaths are baseline mortality rates that retain strong socioeconomic gradients, including those usually seen for cardiovascular and associated diseases as well as cancer.
5. Conclusion
Our models demonstrate that the COVID-19 pandemic has caused many more deaths than would have been expected during the same time-period for all causes examined. Our findings are in agreement with research conducted in the US, Italy, Brazil and Germany, with similar age patterns in excess deaths, increases in cardiovascular deaths, and greater volume excess deaths in more deprived populations [[33], [34], [35], [36]]. For England and Wales, these deaths were not evenly distributed across the population, with rates varying markedly by region, and between deprived and less deprived neighbourhoods. This suggests that future plans to manage the pandemic, including decisions about current and future phases of vaccination roll-out, should include understanding of regional and socioeconomic variation and how this has exacerbated long-standing health inequalities. This has been recognised in strategies developed by organisations including NHS England [37], and the British Medical Association [38], which emphasise the need to address both immediate public health imperatives (for example, ensuring equitable access to vaccines, improving health literacy and trust in disadvantaged groups [39]) and the longer-term consequences of the national pandemic response (for example, restoring routine services equitably and mitigating the social and economic impacts of social distancing restrictions). However, this response needs to be sustained and to address the underlying health inequalities that placed certain groups at greater risk during the pandemic, using both public health measures (for example, restoring local public health infrastructures) and wider socioeconomic interventions (for example, reducing income insecurity).
Geographic inequalities in health, driven by differences in social conditions and physical infrastructure, were already increasing in England & Wales prior to the pandemic [40,41]. Immediate and longer-term recovery planning for communities and their health and social services should reflect these historical disparities as well as the COVID-19 related patterns described in this study. Future studies could usefully extend our analyses to other causes of death and to COVID-19 related morbidity, providing further information to inform a targeted social and public health response.
Author contributions
EK, TD, MM and RW designed the study. EK extracted the data from the secure environment. EK and GM conducted the statistical analyses. EK and TD drafted the paper and all co-authors critically revised it.
Data availability statement
Currently, we do not have permission to share the data but the corresponding author is happy to request permission to share from NHS Digital, on a case by case basis.
Declaration of Interests
CG declares receiving support from Abbot and BMS towards this work, consulting fees from Amgen and AstraZeneca, honoraria from AstraZeneca, participation in Data Safety Monitoring Boards for several trials (TACTIC, DUAL-ACS, DANBLOCK, PROFID, RAPID NSTEMI, STEEER-AF), stock options with the European Heart Journal Quality of Care and Clinical Outcomes as Deputy Editor, and other financial interests with Wondr Medical. None of the other authors have anything relevant to declare.
Acknowledgements
This work would have not been possible without the support of NHS Digital, in making all mortality data in England and Wales available to us, through a secure data environment.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.lanepe.2021.100144.
Appendix. Supplementary materials
References
- 1.Kontopantelis E., Mamas M.A., Deanfield J., Asaria M., Doran T. Excess mortality in England and Wales during the first wave of the COVID-19 pandemic. J Epidemiol Commun Health. 2021;75:213–223. doi: 10.1136/jech-2020-214764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Williams R., Jenkins D.A., Ashcroft D.M., Brown B., Campbell S., Carr M.J. Diagnosis of physical and mental health conditions in primary care during the COVID-19 pandemic: a retrospective cohort study. Lancet Publ Health. 2020;5:e543–ee50. doi: 10.1016/S2468-2667(20)30201-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mohamed M.O., Banerjee A., Clarke S., de Belder M., Patwala A., Goodwin A.T. Impact of COVID-19 on cardiac procedure activity in England and associated 30-day mortality. Eur Heart J-Qual Care Clin Outcomes. 2020;7(3):247–256. doi: 10.1093/ehjqcco/qcaa079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Charlesworth A., Watt T., Thorlby R. The Health Foundation; 2020. Early insight into the impacts of COVID-19 on care for people with long-term conditions. [Google Scholar]
- 5.NHS England. A&E attendances and emergency admissions 2020–21. 2020. https://www.england.nhs.uk/statistics/statistical-work-areas/ae-waiting-times-and-activity/ae-attendances-and-emergency-admissions-2020-21/
- 6.Colivicchi F., Di Fusco S.A., Magnanti M., Cipriani M., Imperoli G. The impact of the COVID-19 pandemic and Italian lockdown measures on clinical presentation and management of acute heart failure. J Card Fail. 2020;26(6):464–465. doi: 10.1016/j.cardfail.2020.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wu J., Mamas M.A., Mohamed M.O., Kwok C.S., Roebuck C., Humberstone B. Place and causes of acute cardiovascular mortality during the COVID-19 pandemic. Heart. 2021;107:113–119. doi: 10.1136/heartjnl-2020-317912. [DOI] [PubMed] [Google Scholar]
- 8.Woolf S.H., Chapman D.A., Sabo R.T., Weinberger D.M., Hill L. Excess deaths from COVID-19 and other causes, March-April 2020. JAMA. 2020;324:510–513. doi: 10.1001/jama.2020.11787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Woolf S.H., Chapman D.A., Sabo R.T., Weinberger D.M., Hill L., Taylor D.D. Excess deaths from COVID-19 and other causes, March-July 2020. JAMA. 2020;324:1562–1564. doi: 10.1001/jama.2020.19545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Qi J., Zhang D., Zhang X., Yin P., Liu J., Pan Y., et al. Do lockdowns bring about additional mortality benefits or costs? Evidence based on death records from 300 million Chinese people. medRxiv. 2021:2020.08. 28.20183699.
- 11.Luce T. Covid 19: death certification in England and Wales. BMJ. 2020;369:m1571. doi: 10.1136/bmj.m1571. [DOI] [PubMed] [Google Scholar]
- 12.Pell R., Fryer E., Manek S., Winter L., Roberts I.S.D. Coronial autopsies identify the indirect effects of COVID-19. Lancet Publ Health. 2020;5:e474. doi: 10.1016/S2468-2667(20)30180-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Maringe C., Spicer J., Morris M., Purushotham A., Nolte E., Sullivan R. The impact of the COVID-19 pandemic on cancer deaths due to delays in diagnosis in England, UK: a national, population-based, modelling study. Lancet Oncol. 2020;21:1023–1034. doi: 10.1016/S1470-2045(20)30388-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Office for National Statistics. User guide to mortality statistics. 2020.https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/methodologies/userguidetomortalitystatisticsjuly2017
- 15.Kontopantelis E., Mamas M.A., van Marwijk H., Ryan A.M., Buchan I.E., Ashcroft D.M. Geographical epidemiology of health and overall deprivation in England, its changes and persistence from 2004 to 2015: a longitudinal spatial population study. J Epidemiol Commun Health. 2018;72:140–147. doi: 10.1136/jech-2017-209999. [DOI] [PubMed] [Google Scholar]
- 16.Office for National Statistics. Lower layer super output area population estimates. 2020. https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationestimates/datasets/lowersuperoutputareamidyearpopulationestimates
- 17.Office for National Statistics. Impact of registration delays on mortality statistics in England and Wales: 2019. 2021. https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/articles/impactofregistrationdelaysonmortalitystatisticsinenglandandwales/2019
- 18.Surkova E., Nikolayevskyy V., Drobniewski F. False-positive COVID-19 results: hidden problems and costs. Lancet Respir Med. 2020;8:1167–1168. doi: 10.1016/S2213-2600(20)30453-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Arevalo-Rodriguez I., Buitrago-Garcia D., Simancas-Racines D., Zambrano-Achig P., Del Campo R., Ciapponi A. False-negative results of initial RT-PCR assays for COVID-19: a systematic review. PLoS One. 2020;15 doi: 10.1371/journal.pone.0242958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Madjid M., Safavi-Naeini P., Solomon S.D., Vardeny O. Potential effects of coronaviruses on the cardiovascular system: a review. JAMA Cardiol. 2020;5:831–840. doi: 10.1001/jamacardio.2020.1286. [DOI] [PubMed] [Google Scholar]
- 21.Mafham M.M., Spata E., Goldacre R., Gair D., Curnow P., Bray M. COVID-19 pandemic and admission rates for and management of acute coronary syndromes in England. Lancet. 2020;396:381–389. doi: 10.1016/S0140-6736(20)31356-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wu J., Mamas M.A., de Belder M.A., Deanfield J.E., Gale C.P. Second decline in admissions with heart failure and myocardial infarction during the COVID-19 pandemic. J Am Coll Cardiol. 2021;77:1141–1143. doi: 10.1016/j.jacc.2020.12.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Aktaa S., Wu J., Nadarajah R., Rashid M., de Belder M., Deanfield J. Incidence and mortality due to thromboembolic events during the COVID-19 pandemic: multi-sourced population-based health records cohort study. Thromb Res. 2021;202:17–23. doi: 10.1016/j.thromres.2021.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rashid M., Wu J., Timmis A., Curzen N., Clarke S., Zaman A. Outcomes of COVID-19 Positive acute coronary syndrome patients; a multisource electronic healthcare records study from England. J Intern Med. 2021 doi: 10.1111/joim.13246. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lee K.W., Khan A.H.K.Y., Ching S.M., Chia P.K., Loh W.C., Rashid AMiA. Stroke and novel coronavirus infection in humans: a systematic review and meta-analysis. Front Neurol. 2020;11 doi: 10.3389/fneur.2020.579070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wu J., Mafham M., Mamas M.A., Rashid M., Kontopantelis E., Deanfield J.E. Place and underlying cause of death during the COVID-19 pandemic: retrospective cohort study of 3.5 million deaths in England and Wales, 2014 to 2020. Mayo Clin Proc. 2021;96:952–963. doi: 10.1016/j.mayocp.2021.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Morciano M., Stokes J., Kontopantelis E., Hall I., Turner A.J. Excess mortality for care home residents during the first 23 weeks of the COVID-19 pandemic in England: a national cohort study. BMC Med. 2021;19:71. doi: 10.1186/s12916-021-01945-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Public Health England. Excess Mortality in England. 2021. https://fingertips.phe.org.uk/static-reports/mortality-surveillance/excess-mortality-in-england-week-ending-02-Oct-2020.html#deaths-by-underlying-cause
- 29.Qureshi A.I., Huang W., Khan S., Lobanova I., Siddiq F., Gomez C.R. Mandated societal lockdown and road traffic accidents. Accid Anal Prev. 2020;146 doi: 10.1016/j.aap.2020.105747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pierce M., Hope H., Ford T., Hatch S., Hotopf M., John A. Mental health before and during the COVID-19 pandemic: a longitudinal probability sample survey of the UK population. Lancet Psychiatry. 2020;7:883–892. doi: 10.1016/S2215-0366(20)30308-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Appleby L., Richards N., Ibrahim S., Turnbull P., Rodway C., Kapur N. Suicide in England in the COVID-19 pandemic: early observational data from real time surveillance. Lancet Region Health-Europe. 2021 doi: 10.1016/j.lanepe.2021.100110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pirkis J., John A., Shin S., DelPozo-Banos M., Arya V., Analuisa-Aguilar P. Suicide trends in the early months of the COVID-19 pandemic: an interrupted time-series analysis of preliminary data from 21 countries. Lancet Psychiatry. 2021 doi: 10.1016/S2215-0366(21)00091-2. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Woolf S.H., Chapman D.A., Sabo R.T., Zimmerman E.B. Excess deaths from COVID-19 and other causes in the US, March 1, 2020, to January 2, 2021. JAMA. 2021;325(17):1786–1789. doi: 10.1001/jama.2021.5199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Michelozzi P., de'Donato F., Scortichini M., Pezzotti P., Stafoggia M., De Sario M. Temporal dynamics in total excess mortality and COVID-19 deaths in Italian cities. BMC Publ Health. 2020;20:1238. doi: 10.1186/s12889-020-09335-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Brant L.C.C., Nascimento B.R., Teixeira R.A., Lopes M., Malta D.C., Oliveira G.M.M. Excess of cardiovascular deaths during the COVID-19 pandemic in Brazilian capital cities. Heart. 2020;106:1898–1905. doi: 10.1136/heartjnl-2020-317663. [DOI] [PubMed] [Google Scholar]
- 36.Stang A., Standl F., Kowall B., Brune B., Böttcher J., Brinkmann M. Excess mortality due to COVID-19 in Germany. J Infect. 2020;81:797–801. doi: 10.1016/j.jinf.2020.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.NHS England. Action required to tackle health inequalities in latest phase of COVID-19 response and recovery. 2021. https://www.england.nhs.uk/about/equality/equality-hub/action-required-to-tackle-health-inequalities-in-latest-phase-of-covid-19-response-and-recovery/
- 38.British Medical Association . BMA; 2021. Mitigating the impact of Covid-19 on health inequalities.https://www.fva.org/downloads/bma-mitigating-the-impact-of-covid-19-on-health-inequalities-report-march-2021.pdf [Google Scholar]
- 39.Paakkari L., Okan O. COVID-19: health literacy is an underestimated problem. Lancet Publ Health. 2020;5:e249–ee50. doi: 10.1016/S2468-2667(20)30086-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.The British Academy . The British Academy; 2021. Shaping the COVID decade: addressing the long-term societal impacts of COVID-19.https://www.thebritishacademy.ac.uk/documents/3239/Shaping-COVID-decade-addressing-long-term-societal-impacts-COVID-19.pdf [Google Scholar]
- 41.Kontopantelis E., Buchan I., Webb R.T., Ashcroft D.M., Mamas M.A., Doran T. Disparities in mortality among 25–44-year-olds in England: a longitudinal, population-based study. Lancet Publ Health. 2018;3:e567–ee75. doi: 10.1016/S2468-2667(18)30177-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Currently, we do not have permission to share the data but the corresponding author is happy to request permission to share from NHS Digital, on a case by case basis.