Abstract
Background
In Europe, survival-rates after out-of-hospital cardiac arrest (OHCA) vary widely between regions. Whether a system dispatching First Responders (FRs; main FR-types: firefighters, police officers, citizen-responders) is present or not may be associated with survival-rates. This study aimed to assess the association between having a dispatched FR-system and rates of return of spontaneous circulation (ROSC) and survival across Europe.
Methods
Results of an inventory of dispatched FR-systems for OHCA in Europe were combined with aggregate ROSC and survival data from the EuReCa-TWO study and additionally collected data. Regression analysis (weighted on number of patients included per region) was performed to study the association between having a dispatched FR-system and ROSC and survival-rates to hospital discharge in the total population and in patients with shockable initial rhythm, witnessed OHCA and bystander cardiopulmonary resuscitation (CPR; Utstein comparator group). For regions without a dispatched FR-system, the theoretical survival-rate if a dispatched FR-system would have existed was estimated.
Findings
We included 27 European regions. There were 15,859 OHCAs in the total group and 2,326 OHCAs in the Utstein comparator group. Aggregate ROSC and survival-rates were significantly higher in regions with an FR-system compared to regions without (ROSC: 36% [95%CI 35%-37%] vs. 24% [95%CI 23%–25%]; P<0.001; survival in total population [N=15.859]: 13% [95%CI 12%–15%] vs. 5% [95%CI 4%–6%]; P<0.001; survival in Utstein comparator group [N=2326]: 33% [95%CI 30%–36%] vs. 18% [95%CI 16%–20%]; P<0.001), and in regions with more than one FR-type compared to regions with only one FR-type. All main FR-types were associated with higher survival-rates (all P<0.050).
Interpretation
European regions with dispatched FRs showed higher ROSC and survival-rates than regions without.
Funding
This project/work has received funding from the European Union's Horizon 2020 research and innovation programme under acronym ESCAPE-NET, registered under grant agreement No 733381 (IO, HLT and MTB) and the European Union's COST programme under acronym PARQ, registered under grant agreement No CA19137 (IO, DC, HLT, MTB). HLT and MTB were supported by a grant from the Netherlands CardioVascular Research Initiative, Dutch Heart Foundation, Dutch Federation of University Medical Centres, Netherlands Organization for Health Research and Development, Royal Netherlands Academy of Sciences - CVON2017-15 RESCUED (HLT), and CVON2018-30 Predict2 (HLT and MTB).
Research in context.
Evidence before this study
When treating out-of-hospital cardiac arrest (OHCA), early cardiopulmonary resuscitation (CPR) and defibrillation by an Automated External Defibrillator (AED) is essential. To increase the likelihood of immediate provision of CPR and use of AEDs, several systems that dispatch First Responders (FRs; main types: firefighters, police officers, citizen responder) have been developed across Europe. At present, over 50% of European countries have a dispatched FR-system.
Whether a dispatched FR-system is present or not may contribute to the variation of OHCA survival in Europe. A few prior studies, based on local regions only, found higher OHCA survival-rate when FRs were dispatched. However, research into the association between FR-systems and OHCA survival-rates is scarce.
Added value of this study
Our study is based on 27 different European regions. We found that regions dispatching FRs show significantly higher rates in OHCA survival when compared to European regions that do not have a dispatched FR-system. Presence of any of the main dispatched FR-types was associated with higher survival-rates. Moreover, our estimations suggest that, if an FR-system would be implemented in European regions without an FR-system, this might result in a higher OHCA survival-rate in each region.
Implications of the available evidence
Although further research is needed, these findings could help inform future public health initiatives towards the implementation of FR-systems and improvement of OHCA survival.
Alt-text: Unlabelled box
1. Introduction
When treating out-of-hospital cardiac arrest (OHCA), a swift pre-hospital response is essential. If the delay in response is too long, an initial shockable rhythm may dissolve into a non-shockable rhythm, thereby decreasing survival chances.[1] The use of automated external defibrillators (AEDs) before Emergency Medical Service (EMS) arrival reduces the time from call to defibrillation of OHCA-patients with a shockable initial rhythm, thereby increasing their chances on survival.[2] To increase the likelihood of immediate provision of cardiopulmonary resuscitation (CPR) and rapid defibrillation with an AED, systems that dispatch First Responders (FRs) have been developed all over Europe.[3,4] Because the implementation of such systems may be influenced by local circumstances and policies, there is a wide variety of dispatched FR-systems, both between and within European countries.[5] At present, over 50% of European countries have a dispatched FR-system to respond to a suspected OHCA in place.[5]
Survival-rates after OHCA vary widely between European regions.[6] Whether a dispatched FR-system is present or not may contribute to this variation. The number and type(s) of dispatched FR may also play a role (FR-system may dispatch one or more of the following types of FR: 1) firefighters, 2) police officers, 3) citizen-responders). For instance, it was estimated that, in a region in the Netherlands where firefighters and police officers are dispatched as FRs, 7% of OHCA-patients would not have received a first shock within six minutes if citizen-responders would not also have been dispatched.[7] On the other hand, an additional gain in OHCA survival-rate upon dispatch of a second or third FR-type may level-off as the number of dispatched FR-types increases, because of the competing contribution of each FR-type.[8]
This study aimed to assess if having a dispatched FR-system is associated with higher rates of return of spontaneous circulation (ROSC) and survival to hospital discharge across Europe. Second, we aimed to assess if European regions with more than one dispatched FR-type have higher rates of ROSC and survival than European regions with one dispatched FR-type. Finally, for European regions without a dispatched FR-system, we aimed to estimate the theoretical survival-rate that would be achieved if a dispatched FR-system would have existed.
2. Methods
2.1. Design and data collection
This research was conducted as part of the ESCAPE-NET project that aims to discover the causes of and best treatments for OHCA.[9] Results of a previous study (FR-ONE), which inventoried all current dispatched FR-systems for OHCA across 29 European regions (countries [if one FR-system applied to the total country] or parts thereof [if individual regions within one country used a specific FR-system])[5], were combined with published aggregate ROSC and survival results from the EuReCa-TWO study[6] and additionally collected survival-rates. EuReCa-TWO was a prospective study, for which data were collected from 28 European regions in the period October 1, 2017 - December 31, 2017. Because FR-ONE was not performed during the same study period as EuReCa-TWO, the information on FR-systems that was collected during the FR-ONE study was updated by re-consulting the OHCA professionals that contributed to FR-ONE.[5]
OHCA-patients per study region and their corresponding aggregate rates of survival to hospital discharge came from two sources: 1) the EuReCa-TWO published survival-rates, and 2) by contacting the coordinator of the OHCA registry when different FR-systems existed within one EuReCa region or when survival data were not published in the EuReCa-TWO study. This applied to the following regions: Province of Pavia (Italy), Region of Emilia Romagna (Italy), Region of Stockholm (Sweden), Region of Marburg-Biedenkopf (Germany), and the Region of Hradec Kralove (Czech Republic). To obtain survival-rates from these regions, the coordinators of the OHCA-registry were contacted through the ESCAPE-NET FR-ONE and EuReCa network. All data collected complied with the Utstein definitions.[10]
2.2. Definitions
A dispatched FR-system was defined as a system in which a dispatch centre directs persons not on medical duty to attend OHCA events and initiate early CPR and possibly early defibrillation. Dispatched FR-types studied in the present study were: firefighters, police officers, and citizen-responders. An extensive description of FRs and EMS per region is provided in Supplementary materials: definitions.
Regions were categorized into one of three categories of comparable size: (1) region without FRs; (2) region with one FR-type, and (3) region with >one FR-type.
ROSC was defined as a period of at least 30 seconds of pre-hospital ROSC. The Utstein comparator group was defined as the group of patients with a shockable initial rhythm (defined as pulseless ventricular-tachycardia or ventricular-fibrillation) and a bystander witnessed-OHCA.[11]
2.3. Outcomes
The primary outcome was defined as pre-hospital ROSC-rate and survival to hospital discharge rate in the total study population (survivaltotal), and the secondary outcome was survival-rate to hospital discharge of the Utstein comparator group (survivalcomparator).
2.4. Data analysis as performed per protocol
Rates of ROSC and survival were reported as mean (95% Confidence Interval [CI]). Weighted regression analysis (based on number of patients included per region) was used to study the association between having a dispatched FR-system and rates of (1) ROSC, (2) survivaltotal, and (3) survivalcomparator.
First, the association between FR-type and OHCA survival was evaluated using weighted regression analysis. For the categorical variable: “FR-type”, two dummy variables were created. Next, main FR-types were analysed as a binary variable (FR-type dispatched [either alone or complementary to other FR-types in one FR-system] vs. FR-type not dispatched) using weighted regression analysis. As a post-hoc exploratory analysis, we performed a weighted regression analysis to explore a possible association between having a dispatched FR-system and rates of bystander-CPR.
Finally, for regions without a dispatched FR-system and without missing data (Spain, Croatia, Hungary, Italy [Province of Pavia], France and Serbia), we estimated the theoretical change between observed and expected survivaltotal rate to estimate the survival-rate in these regions if a dispatched FR-system would have existed. The observed rate was the mean survival-rate as reported in the EuReCa-TWO study and/or additionally collected data through the ESCAPE-NET FR-ONE study network. The expected rate was calculated by multiplying the observed rate of a region without an FR-system by the relative increase in mean survival-rate between regions with and without an FR-system. The relative increase was calculated as (mean rate in regions with dispatched FR-system - mean rate in regions without dispatched FR-system)/mean rate in regions without dispatched FR-system. This is described in more detail in Supplementary materials methods: theoretical increase. To calculate these estimations, we assumed that the following changes take place after implementation of an FR-system: (1) the proportion of OHCA-patients in the Utstein comparator group would increase, because the proportion of patients with a shockable initial rhythm would increase (due to a shorter response time) and (2) survival increase would be more substantial for patients in the Utstein comparator group than for patients outside of it (non-comparator group) as patients with a non-shockable initial rhythm and unwitnessed OHCA are less likely to benefit from early defibrillation and CPR.
Statistical tests were two-tailed, with P<0.050 considered statistically significant, and performed in SPSS (version 24.0 for Mac). To account for multiple comparisons, the significance level was set at P≤0.010 for the linear regression analyses.
3. Results
3.1. First responder systems in Europe
In total, 27 European regions were included (Table 1). Of 22 from the 29 FR-ONE regions, data could be combined with the aggregate data of EuReCa-TWO; of 5 from the 29 FR-ONE regions additional aggregate data was collected by contacting the coordinator of the OHCA registry. Of 2 from the 29 FR-ONE regions data could not be retrieved (Supplementary materials: data collection per region).
Table 1.
Overview per study region.
| Country (N=Population served) | First Responder types (N) | OHCA confirmed (N) | Total population of cardiac OHCAs included for analyses – CPR started (N) | CPR started (%) | ROSC rate of total population | Survival rate of total population | Utstein comparator group (N) | Survival rate of Utstein comparator group |
|---|---|---|---|---|---|---|---|---|
| First Responders dispatched | N=10,038 | N=7,948 | N=1,116 | |||||
| Austria N=3.444.711 | Police officers (1) | 457 | 348 | 76% | 35% | 8% | 73 | 19% |
| Czech Republic (Hradrec Kralove) N=92.921 | Firefighters, citizen-responders, police officers (3) | 91 | 83 | 91% | 55% | 13% | 18 | 39% |
| Germany (Marburg- Biedenkopf) N=245.013 | Citizen-responders (1) | 38 | 38 | (100%) | 45% | 18% | 7 | 43% |
| Denmark (Copenhagen) N=1.821.577 | Citizen-responders (1) | 391 | 331 | 85% | 42% | 12% | 56 | 55% |
| Finland N=4.138.648 | Firefighters (1) | 1133 | 565 | 51% | 41% | 15% | 113 | 41% |
| Ireland N=4.757.97 | Firefighters, citizen-responders, police officers, off duty EMS (4) | 870 | 592 | 68% | 25% | 7% | 83 | 32% |
| Italy (Emilia Romagna) N=4.449.000 | Firefighters, citizen-responders, police officers, taxi drivers (4) | 52 | 52 | (100%) | 52% | 27% | 17 | 59% |
| Luxembourg N=549.680 | Firefighters (1) | 138 | 64 | 46% | 29% | Missing | 12 | Missing |
| The Netherlands N=3.869.347 | Firefighters, police officers, citizen-responders (3) | 574 | 440 | 77% | 43% | 19% | 123 | 45% |
| Norway N=5.267.128 | Firefighters (3) | 711 | 711 | (100%) | 28% | 12% | 121 | 39% |
| Poland N=3.385.000 | Firefighters (1) | 739 | 382 | 52% | 32% | 8% | 57 | 25% |
| Portugal N=514.531 | Firefighters (1) | 99 | 52 | 53% | 35% | Missing | Missing | Missing |
| Romania N=4.086.753 | Firefighters, citizen-responders (2) | 642 | 463 | 72% | 16% | Missing | 42 | 0% |
| Sweden (Stockholm) N=1.553.000 | Firefighters, citizen responder, police officers (3) | 202 | 202 | (100%) | Missing | 10% | 29 | 28% |
| Switzerland N=2.415.000 | ⁎⁎ | 432 | 264 | 61% | 31% | Missing | 47 | 10% |
| Slovenia N=1.209.479 | Firefighters (1) | 284 | 176 | 68% | 38% | 13% | 41 | 32% |
| United Kingdom N=20.245.023 | ⁎⁎ | 3185 | 3185 | (100%) | 41% | 9% | 277 | 27% |
| First Responders not dispatched | N=13,393 | N=7,911 | N=1,210 | |||||
|---|---|---|---|---|---|---|---|---|
| Bosnia & Herzegovina N=110.979 | None | 46 | 22 | 79% | Missing | 0% | Missing | Missing |
| Cyprus N=650.000 | None | 103 | 46 | 28% | 20% | 0% | Missing | Missing |
| France* N=9.993.658 | None | 2433 | 2276 | 94% | 19% | 5% | 341 | 20% |
| Greece N=8.146.660 | None | 1129 | 742 | 36% | 7% | Missing | 52 | 11% |
| Hungary N=9.797.561 | None | 3430 | 1993 | 58% | 23% | 4% | 299 | 12% |
| Croatia N=1.895.000 | None | 429 | 284 | 66% | 22% | 9% | 54 | 24% |
| Iceland N=237.538 | None | 40 | Missing | 75% | 43% | Missing | Missing | Missing |
| Italy (Pavia) N=547.251 | None | 204 | 204 | (100%) | 24% | 6% | 15 | 20% |
| Serbia N=1.227.069 | None | 405 | 197 | 49% | 20% | 7% | 41 | 10% |
| Spain N=31.751.584 | None | 5174 | 2147 | 41% | 37% | 11% | 408 | 32% |
Abbreviations: EMS, emergency medical system; NA, Not Applicable; OHCA, out-of-hospital cardiac arrest; ROSC, return of spontaneous circulation
Firefighters are considered EMS
Region was only taken into account in the main analysis (First Responders available versus First Responder not available). Region was left out in the sub-analyses with number and type of First Responders, as this could not be determined accurately.
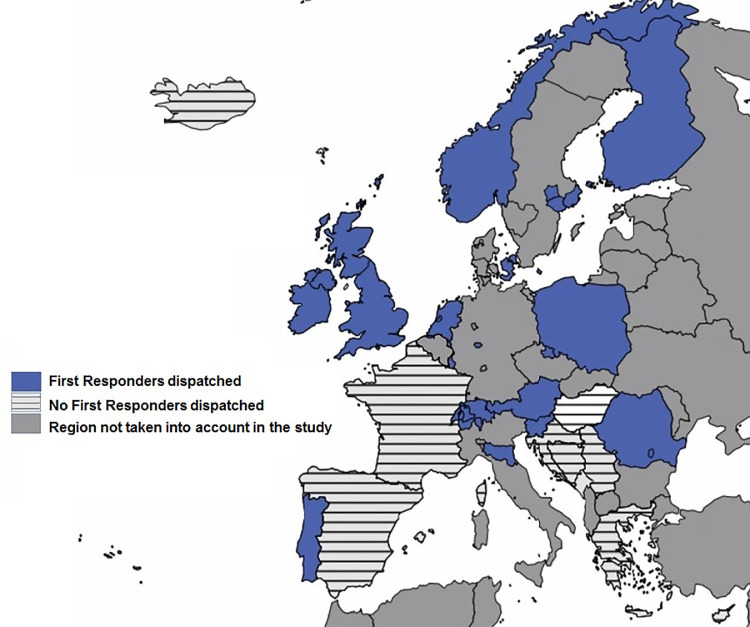
The updated results from the FR-systems inventory showed that more than half (17 of 27) of the regions had an FR-system in place (Fig. 1), including 10 regions with one FR-type and 7 regions with >one FR-type (Table 1). Geographical clustering of dispatched FR-types in Europe was not observed.
Fig. 1.
Overview of First Responders in Europe
Figure shows European regions that do dispatch First Responders in the event of an out-of-hospital cardiac arrest and regions that do not.
3.2. ROSC and survival-rates of regions with first responder system vs. no first responder system
The number of OHCAs included for ROSC and survival analyses was 15,859 in the total group (N=7,948 in regions with an FR-system, N=7,911 in regions without an FR-system) and 2,326 in the Utstein comparator group (N=1,210 in regions with an FR-system, N=1,116 in regions without an FR-system). Rates of ROSC and survival per study region are shown in Table 1.
Mean ROSC-rates were significantly higher in regions with an FR-system than in regions without an FR-system (36% [95%CI 35%-37%] vs. 24% [95%CI 23%–25%], P=0.001). Also, mean survival-rates were significantly higher in regions with an FR-system than in regions without an FR-system in both the total population and the Utstein comparator group (mean survivaltotal 13% [95%CI 12%-14%] vs. 5% [95%CI 4%–6%], P=0.001; mean survivalcomparator 33% [95%CI 30%-36%] vs. 18% [95%CI 16%–20%], P=0.001).
The post-hoc exploratory analysis showed that regions with an FR-system showed higher bystander-CPR rates than regions without an FR-system (mean 59% [95%CI 58%-60%] vs. 46% [95%CI 45%–47%] P=0.003).
3.3. Association between number and type of FR-systems, and survival-rates
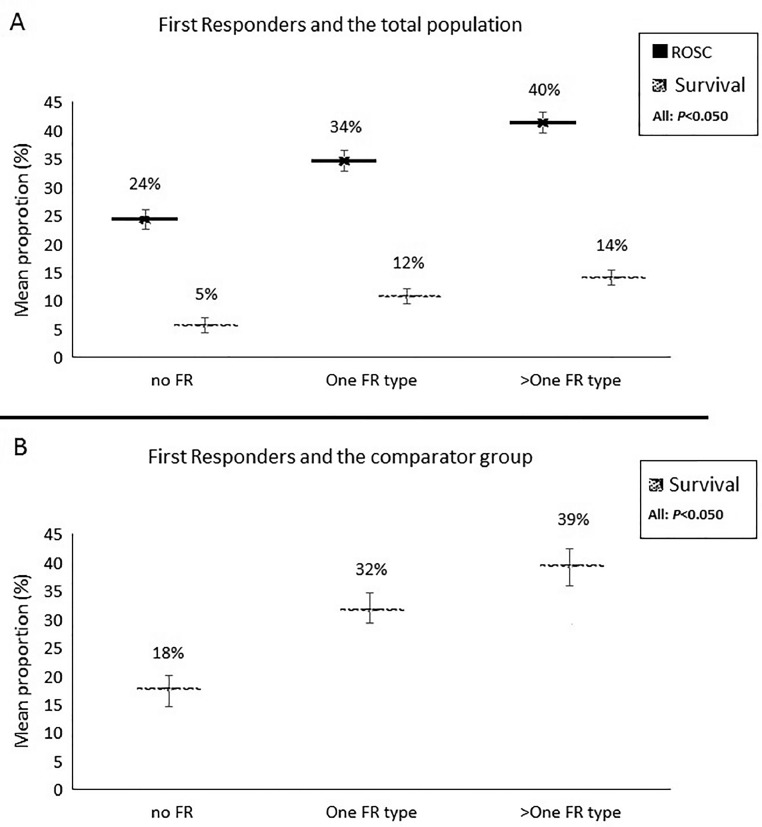
Regions dispatching one FR-type and regions dispatching one FR-type had significantly higher mean ROSC-rates than regions that do not dispatch FRs: 34% [95%CI 32%–36%] vs. 24% [95%CI 23%–25%] P=0.001 and 40% [95%CI 39%–41%] vs. 24% [95%CI 23%–25%] P=0.001, respectively (Fig. 2A). Moreover, regions dispatching >one FR-type had significantly higher mean ROSC-rates than regions dispatching only one FR-type: mean 40% [95%CI 39%–41%] vs. 34% [95%CI 32%–46%], P=0.001 (Fig. 2A).
Fig. 2.
First Responder system and survival-rates
Abbreviations: FR, First Responder
Figure shows (A) ROSC and the survival-rate in the total population and (B) the survival-rate in the Utstein comparator group; per dispatched First Responder category (No First Responders, One First Responder type, >One First responder type). P values indicate the differences between FR categories (groups compared: 1. One First responder type vs. No First Responder type, 2. >One First responder type vs. No First Responder type and 3. >One First responder type vs. One First Responder type). The line within a First Responder category corresponds to the 95% Confidence Interval.
Similar results were observed when survival-rates were studied. For survivaltotal this was as follows: (1) one FR-type vs. no FR-type: mean 12% [95%CI 11%–13%] vs. 5% [95%CI 4%–6%]; P=0.006; (2) >one FR-type vs. no FR-type: mean 14% [95%CI 13%–15%] vs. 5% [95%CI 4%–6%]; P<0.005 and (3) >one FR-type vs. one FR-type: mean 14% [95%CI 13%–15%] vs. 12% [95%CI 4%–6%]; P=0.015 (Fig. 2A). For survivalcomparator: (1) one FR-type vs. no FR-type: mean 32% [95%CI 28%–35%] vs. 18% [95%CI 16%–20%]; P=0.003; (2) >one FR-type vs. no FR-type: mean 39% [95%CI 36%–43%] vs. 18% [95%CI 16%–20%]; P=0.002 and (3) >one FR-type vs. one FR-type: mean 39% [95%CI 36%–43%] vs. 32% [95%CI 28%–35%]; P=0.022 (Fig. 2B).
Presence of any of the FR-types was statistically significantly associated with higher survival-rates (Supplementary materials: results).
3.4. Calculated theoretical survival-rates
The mean proportion of OHCA-patients in the Utstein comparator group was 1.36 times higher in regions with an FR-system than in regions without (19% vs. 14%, respectively, Table 2). The mean survival-rate in the Utstein comparator group was 1.83 times higher in regions with an FR-system than in regions without (33% vs. 18%). The mean survival-rate in the non-comparator group was 1.67 times higher in regions with an FR-system than in regions without (5% vs. 3%). With these calculated relative increases, we estimated survivaltotal rates for Spain, Croatia, Hungary, Italy (Province of Pavia), France and Serbia, if an FR-system would have existed (Table 2): Spain, from observed 11% to estimated 23%; Croatia, from 9% to 17%; Hungary, from 4% to 7%; Italy (Province of Pavia), from 6% to 8%; France, from 5% to 10% and Serbia from 7% to 8% (Table 2). Also, the following survivalcomparator rates were estimated: Spain, from observed 32% to estimated 59%; Croatia, from 24% to 44%; Hungary, from 12% to 22%; Italy (Province of Pavia), from 20% to 37%; France from 20% to 37% and Serbia from 10% to 18%.
Table 2.
Estimations of survival rates in regions without First Responder systems if a First Responder system would have been in place
|
Calculations used to determine the theoretical survival rate (from observed to expected) | ||||||
|---|---|---|---|---|---|---|
| No FR-systemMean % | FR-system dispatchedMean % | Relative increase*: FR- system dispatched vs. no FR-system | ||||
|
14% (95%CI 13%-15%) | 19% (95%CI 18%-20%) | 36% (*1.36) | |||
|
18% (95%CI z17%-19%) | 33% (95%CI 32%-34%) | 83% (*1.83) | |||
|
3% (95%CI 3%-3%) | 5% (95%CI 5%-5%) | 67% (*1.67) | |||
|
OHCA-patients |
OHCA survivors |
|||||
|---|---|---|---|---|---|---|
| Country |
Total group N |
Comparator group %⁎⁎ |
Non-comparator group %⁎⁎ | Survivaltotal %⁎⁎ | Comparator group %⁎⁎ | Non-comparator group %⁎⁎ |
| Observed rates | ||||||
| Spain | 2147 | 19% (95%CI 17%-21%) | 81% (95%CI 79%-83%) | 11% (95%CI 10%-12%) | 32% (95%CI 27%-37%) | 6% (95%CI 5%-7%) |
| Croatia | 284 | 19% (95%CI 14%-24%) | 81% (95%CI 76%-86%) | 9% (95%CI 6%-12%) | 24% (95%CI 13%-35%) | 4% (95%CI 1%-7%) |
| Hungary | 1993 | 15% (95%CI 13%-17%) | 85% (95%CI 83%-87%) | 4% (95%CI 3%-5%) | 12% (95%CI 8%-16%) | 2% (95%CI 0%-4%) |
| Italy (Pavia) | 204 | 7% (95%CI 3%-11%) | 93% (95%CI 89%-97%) | 6% (95%CI 3%-9%) | 20% (95%CI 0%-41%) | 3% (95%CI 0%-5%) |
| France÷ | 2276 | 15% (95%CI 14%-16%) | 85% (95%CI 84%-86%) | 5% (95%CI 4%-6%) | 20% (95%CI 16%-24%) | 2% (95%CI 1%-3%) |
| Serbia | 197 | 14% (95%CI 9%-19%) | 86% (95%CI 81%-91%) | 7% (95%CI 3%-11%) | 10% (95%CI 0%-21%) | 3% (95%CI 0%-6%) |
|
Total group N |
Comparator group N (%) |
Non-comparator group N (%) | Survivaltotal N (%) | Comparator group N (%) | Non-comparator group N (%) | |
|---|---|---|---|---|---|---|
| Expected rates | ||||||
| Spain | 2147 | 558 (26%; 95%CI 24%-28%)⁎⁎⁎ | 1589⁎⁎⁎⁎(74%; 95%CI 72%-76%) | 488 (23%; 95%CI 21%-25%)± | 329 (59%; 95%CI 55%-63%)‡ | 159†† (10%; 95%CI 9%-11%)‡‡ |
| Croatia | 284 | 74 (26%; 95%CI 21%-31%)⁎⁎⁎ | 210⁎⁎⁎⁎(74% 95%CI 69%-79%) | 48 (17%; 95%CI 13%-21%)± | 33 (44%; 95%CI 33%-55%)‡ | 15†† (7%; 95%CI 4%-10%)‡‡ |
| Hungary | 1993 | 399 (20%; 95%CI 18%-22%)⁎⁎⁎ | 1594⁎⁎⁎⁎(80%; 95%CI 78%-82%) | 136 (7%; 95%CI 6%-8%)± | 88 (22%; 95%CI 18%-26%)‡ | 48†† (3%; 95%CI 2%-4%)‡‡ |
| Italy (Pavia) | 204 | 20 (10%; 95%CI 6%-14%)⁎⁎⁎ | 184⁎⁎⁎⁎(90%; 95%CI 86%-94%) | 16 (8%; 95%CI 4%-12%)± | 7 (37%; 95%CI 16%-58%)‡ | 9†† (5%; 95%CI 2%-8%)‡‡ |
| France÷ | 2276 | 455 (20%; 95%CI 18%-22%) | 1821⁎⁎⁎⁎(80%; 95%CI 78%-82%) | 223 (10%; 95%CI 9%-11%)± | 168 (37%; 95%CI 33%-41%)‡ | 55 (3%; 95%CI 2%-4%)‡‡ |
| Serbia | 197 | 37 (19%; 95%CI 14%-24%) | 160⁎⁎⁎⁎(81%; 95%CI 69%-86%) | 15 (8%; 95%CI 12%-12%)± | 7 (18%; 95%CI 6%-30%)‡ | 8 (5%; 95%CI 2%-8%)‡‡ |
Abbreviations: FR, first responder; OHCA, out-of-hospital cardiac arrest
Relative increase was calculated as (mean (FR-system dispatched) – mean (No FR-system)) / (mean (No FR-system))
N is not reported for observed rates, only percentages could be collected accurately based on published data
Proportion in comparator group (expected): proportion comparator group (observed) *1.36 [=relative increase proportion patients in comparator group]
Non-comparator, N (expected) = N total – N comparator (expected)
Proportion survival in comparator group (expected): proportion survival in comparator group (observed) * 1.83 [=relative increase survival comparator group]
Proportion survival in non-comparator group (expected): proportion survival in non-comparator group (observed) * 1.67 [=relative increase survival non-comparator group]
Proportion survivaltotal(expected): N patients survived comparator (expected) + N patients survived non-comparator (expected) / N Total
Firefighters are part of the EMS in France. Therefore, the calculated expected survival rate only applies to the situation in which either citizen-responders or police officers will be added to an EMS system with firefighters being part of the EMS
4. Discussion
4.1. Main findings
In the present study, we included 27 different European regions. More than half (17 of 27) of the regions had an FR-system in place.
European regions dispatching FRs (either one FR-type or more than one FR-type dispatched) have significantly higher rates of ROSC and survival after OHCA when compared to regions that do not have a dispatched FR-system. This is in line with prior research regarding FR-systems for ROSC[12] and for OHCA survival.[13] Moreover, modestly higher ROSC and OHCA survival-rates were observed in regions dispatching more than one FR-type when compared to regions dispatching one single FR-type.
Presence of any of the main dispatched FR-types (firefighters, police officers and citizen-responders) was statistically significant associated with higher survival-rates.
4.2. Number of FR-types per system dispatched
Our study showed that the differences in number of FR-types dispatched (within one FR-system) may contribute to differences in ROSC and OHCA survival-rates across Europe. When dispatching more than one FR-type, a modest but significant increase in both ROSC and OHCA survival-rate was observed when compared to dispatching one single FR-type. A second or third dispatched FR-type may provide an early defibrillation shock to OHCA-patients who may not have received an early shock if the FR-system was limited to one or two FR-type(s) as observed in a prior study from the Netherlands.[7] This could possibly increase ROSC and OHCA survival-rate. However, the increase in ROSC and OHCA survival-rate was only modest when more than one FR-type was dispatched compared to one single FR-type and (for survival) not statistically significant after we reduced the P value to ≤0.010. A study from 2005 showed that equipping police cars with AEDs in an urban area in the United States where firefighters are dispatched did not improve OHCA Survival-rate to hospital discharge.[8] It is possible that the increase in OHCA survival-rate may level-off with an increasing number of dispatched FR-types, because of their competing contribution to the OHCA chain of care. In our study, there were too few observations to analyse the association of FR-systems dispatching two or three different FR-types with survival, thus not allowing for comparisons between two or three dispatched FR-types.
It was already observed in 1996 that an increase in OHCA survival may be associated with the use of a two-tier EMS system (the additional dispatch of BLS-providers or firefighters) as opposed to a one-tier EMS system[14] and that changing from a one-tier to a two-tier EMS system might be an attractive cost-effective option.[15] However, recent studies into the relation between dispatching FR-types and its health-economic impact that could provide insight into the costs and benefits are scarce. A previous study from the Netherlands that dispatched AED use during resuscitation showed no association with lower in-hospital health care costs (nor with higher costs).[16] Another study from Ireland showed that an increased number of AEDs alone is unlikely to improve survival in a cost-effective manner, though the study does suggest that strategic deployment of AEDs by CPR-trained FRs may be an important link in OHCA survival.[17] Future research in the health economic field is needed.
4.3. Type of dispatched FR
The FR-ONE study showed that firefighters feature highly as FR-types in Europe[5]. Other prior research suggested that firefighters have a role in increasing OHCA survival-rate.[13,[18], [19], [20]] Also, FR-systems involving police officers and/or dispatched citizen-responders may be promising.[13,21,22] In line with prior research, the present study observed that all main FR-types individually may contribute to higher OHCA survival-rates. Based on these results and supported by results from a prior study[5], we could hypothesize that it is less important which specific FR-type is dispatched but that differences between characteristics of the main FR-types, such as whether the FR-type is trained in CPR or not, may play a larger role.[5] For instance, although frequent CPR-training is a feature of most dispatched FR-systems in Europe, some regions allow citizen-responders to register without validation of CPR-training.[5] Also, differences in response capabilities between FR-types and/or the method of alerting FR-types may influence OHCA survival-rates.[5] For example, if an FR-type is based at the EMS station (which is the case in some European regions) it may not be worthwhile to dispatch that particular FR-type. Being stationed at the same location as the EMS thus may result in that FR-type being rarely dispatched.
4.4. FR-systems and OHCA survival-rate
We found that survival-rates after dispatching FRs were higher both in the total population and in the Utstein comparator group. Previous findings from Sweden indicated that the main impact of FR treatment on OHCA survival was seen in patients with a shockable initial rhythm.[13]
We studied survival-rates at hospital discharge and were not able to study survival-rates at hospital admission. Differences in survival-rate at hospital discharge may be partly due to differences in in-hospital treatment. Yet, a previous Swedish study showed that a higher proportion of patients was admitted to the hospital alive when FRs were dispatched, indicating that higher OHCA survival-rates are likely achieved, at least in part, through prehospital actions by FRs.[13]
To reduce possible effects of differences in in-hospital treatment on differences in survival to discharge in our present analysis, we also investigated ROSC. In line with the observed higher survival-rates, regions dispatching FRs also showed higher ROSC-rates. However, the difference in ROSC-rate between regions where FRs are dispatched and regions where FRs are not dispatched was much smaller when compared to the difference in survival-rate at hospital discharge (a relative increase in ROSC-rate of 50% was observed in regions dispatching FRs, while a relative increase in survival-rate of 160% was observed). This may, for example, suggest that regions with a dispatched FR-system in place could transfer OHCA-patients to hospitals that provide better post resuscitation care than those in locations without FRs. Another possibility is that in regions with an FR-system the time interval between the start of OHCA to ROSC is shorter or that OHCA-patients receive higher CPR-quality from FRs.[23] Patients who achieve ROSC earlier will arrive in a better condition and thus may have a higher chance of survival once admitted to the hospital.[24] However, we have no data available to explore the possibilities as mentioned above.
4.5. Implementation of a first responder system and raising awareness of CPR
Our calculations regarding the theoretical change in survival for regions without an FR-system may suggest that, if an FR-system would be implemented, this might result in a higher OHCA survival-rate in all regions, assuming that having an FR-system is associated with survival.
Public health programs for raising awareness of CPR in the community have been implemented in many countries.[25,26] Among others, the following public programs were associated with increased bystander-CPR provision: mandatory CPR-education in elementary schools and voluntary CPR-training in the community.[26]
It could also be that introducing an FR-system is a proxy for increased public awareness of the need of bystander-CPR in case of OHCA. Higher awareness (after implementation of an FR-system) might be associated with a higher likelihood of bystander-CPR and subsequently, favourable survival outcomes after OHCA.[25] Our post-hoc analysis suggesting a higher rate of bystander-CPR in regions with an FR- system may support this line of thinking.
Implementation of an FR-system may be part of a combined approach of several initiatives to improve the OHCA-chain of care. [27] Therefore, the benefit of the presence of an FR-system may also be a result of other beneficial improvements in the chain of care (for example, having an organization goal).[28]
4.6. Strengths and limitations
This study has several strengths. First, data harmonization within the ESCAPE-NET project and EuReCa-TWO study made it possible to analyse the association between FR-systems and OHCA survival-rates.[9] Second, all analyses were weighted based on the number of included patients per region in order to take account of the variation by chance in regional estimates.
Nonetheless, multiple limitations need to be considered. First, we used aggregate data only, since patient-level data were not available. This limited our possibilities to address confounding. Furthermore, our aggregate data originated from different registries. Hence, differences in inclusion criteria may exist, which may hamper the comparability of ROSC and survival-rates (i.e. differences in % CPR initiated across the registries). We addressed this issue by using the Utstein comparator group. Second, the effectiveness of FRs depends among others on the response time of the EMS. In a system with short EMS response times, dispatched FRs may have less added value than in a system with longer EMS response times. Also, the effectiveness of a system might be better assessed by AED-connection rate. However, EMS response intervals and AED-connection rates were not available in each of the participating regions. Nonetheless, our analysis of the Utstein comparator group only includes OHCA-patients with an initial shockable rhythm. A shockable initial rhythm eliminates most cases (>50%) with more than 10-12 minutes delay from call EMS to connection to AED or manual defibrillator, thus rendering more comparable groups.[29] Third, other unmeasured differences between the included regions may have affected the results of this study, such as differences in population characteristics or in-hospital treatment. The association found in this study should prompt further research to determine the size of the effect of FR-systems when other differences between regions are adjusted for. Also, we have no information on the proportion of FRs being first on scene and the actual percentage of AED-connection rate by FRs. Finally, as with all observational studies, we were only able to study associations. A causal relation between FR-systems and survival could therefore not be determined; inference and quantification of the effect of implementing an FR-system must be done with caution.
Conclusion
European regions dispatching FRs after OHCA (either dispatching one single FR-type or more than one FR-type) have significantly higher rates of ROSC and survival to hospital discharge than regions that do not dispatch FRs. Having a dispatched FR-system, dispatching at least one FR-type (firefighters, police officers, citizen-responders) for OHCA might increase survival-rate in Europe, but further prospective or randomized research is required.
Declaration of Competing Interest
The authors have nothing to declare.
Acknowledgments
Acknowledgements
We thank the European Union's Horizon 2020 research and innovation programme for funding the ESCAPE-NET project. Furthermore, we are greatly indebted to Nikolaos Nikolaou (MD, PhD, from Greece), Simone Savastano (MD, from Italy), Michael Baubin (MD, PhD) and Maximilian Mörtl (MD, ) from Austria, Cristina Granja (MD, PhD, from Portugal), Ari Salo (MD, from Finland), Linn Andelius (MD, from Denmark), Mark Biancardi (MD, from Malta), Veronika Reinhard (MD, from Estonia), Marios Ioannidis (MD, PhD, from Cyprus), Violetta Raffay (MD, PhD, from Serbia), Emma Scott and Nicola Dunbar (from the United Kingdom), Martin Quinn (MA) from Ireland, Fernando Rosell Ortiz (MD, PhD from Spain), Nagy Enikő (from Hungary), Pascal Stammet (MD, PhD from Luxembourg), Andrej Markota (MD, PhD) and Janez Strnad (MD, PhD) (from Slovenia), Craig Hunter (from Scotland), Monika Praunova and Jaroslava Krencikova (MD, from the Czech Republic), and Xavier Jouven (MD, PhD, from France) for their cooperation and data collection. Also, we would like to thank all other OHCA experts who so generously shared their expert opinion and knowledge to make this study possible.
Roll of the funding source
The funder of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report. The corresponding author had full access to all of the data and the final responsibility to submit for publication.
Author contribution statement
Iris Oving*: study design, data collection, data analysis, data interpretation, writing manuscript, figures and tables.
Corina de Graaf*: data analysis, data interpretation, writing manuscript, figures and tables
Siobhan Masterson: data collection, data interpretation, review manuscript
Rudolph Koster: data interpretation, review manuscript
Aeilko Zwinderman: statistical analysis, review manuscript
Remy Stieglis: data interpretation, review manuscript
Hajriz AliHodzic: data collection, review manucript
Enrico Baldi: data collection, review manucript
Susanne Betz: data collection, review manucript
Diana Cimpoesu: data collection, review manucript
Fredrik Folke: data collection, review manucript
Dennis Rupp: data collection, review manucript
Federico Semeraro: data collection, review manucript
Anatolij Truhlar: data collection, review manucript
Hanno Tan: study supervisor, study design, data interpretation, writing and review of manuscript
Marieke Blom*: study supervisor, study design, data analysis, data interpretation, writing and review of manuscript
*Author verified the underlying data
Data sharing agreement
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.lanepe.2020.100004.
Appendix. Supplementary materials
References
- 1.Holmgren C, Bergfeldt L, Edvardsson N. Analysis of initial rhythm, witnessed status and delay to treatment among survivors of out-of-hospital cardiac arrest in Sweden. Heart (British Cardiac Society) 2010;96(22):1826–1830. doi: 10.1136/hrt.2010.198325. [DOI] [PubMed] [Google Scholar]
- 2.Rajan S, Folke F, Hansen SM. Incidence and survival outcome according to heart rhythm during resuscitation attempt in out-of-hospital cardiac arrest patients with presumed cardiac etiology. Resuscitation. 2017;114:157–163. doi: 10.1016/j.resuscitation.2016.12.021. [DOI] [PubMed] [Google Scholar]
- 3.Hansen CM, Kragholm K, Granger CB. The role of bystanders, first responders, and emergency medical service providers in timely defibrillation and related outcomes after out-of-hospital cardiac arrest: results from a statewide registry. Resuscitation. 2015;96:303–309. doi: 10.1016/j.resuscitation.2015.09.002. [DOI] [PubMed] [Google Scholar]
- 4.Berdowski J, Blom MT, Bardai A, Tan HL, Tijssen JG, Koster RW. Impact of onsite or dispatched automated external defibrillator use on survival after out-of-hospital cardiac arrest. Circulation. 2011;124(20):2225–2232. doi: 10.1161/CIRCULATIONAHA.110.015545. [DOI] [PubMed] [Google Scholar]
- 5.Oving I, Masterson S, Tjelmeland IBM. First-response treatment after out-of-hospital cardiac arrest: a survey of current practices across 29 countries in Europe. Scand J Trauma Resusc Emerg Med. 2019;27(1):112. doi: 10.1186/s13049-019-0689-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Grasner JT, Wnent J, Herlitz J. Survival after out-of-hospital cardiac arrest in Europe - results of the EuReCa-TWO study. Resuscitation. 2020;148:218–226. doi: 10.1016/j.resuscitation.2019.12.042. [DOI] [PubMed] [Google Scholar]
- 7.Zijlstra JA, Stieglis R, Riedijk F, Smeekes M, van der Worp WE, Koster RW. Local lay rescuers with AEDs, alerted by text messages, contribute to early defibrillation in a Dutch out-of-hospital cardiac arrest dispatch system. Resuscitation. 2014;85(11):1444–1449. doi: 10.1016/j.resuscitation.2014.07.020. [DOI] [PubMed] [Google Scholar]
- 8.Sayre MR, Evans J, White LJ, Brennan TD. Providing automated external defibrillators to urban police officers in addition to a fire department rapid defibrillation program is not effective. Resuscitation. 2005;66(2):189–196. doi: 10.1016/j.resuscitation.2005.02.006. [DOI] [PubMed] [Google Scholar]
- 9.Empana JP, Blom MT, Bttiger BW. Determinants of occurrence and survival after sudden cardiac arrest-A European perspective: the ESCAPE-NET project. Resuscitation. 2018;124:7–13. doi: 10.1016/j.resuscitation.2017.12.011. [DOI] [PubMed] [Google Scholar]
- 10.Perkins GD, Jacobs IG, Nadkarni VM. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update of the utstein resuscitation registry templates for out-of-hospital cardiac arrest: a statement for healthcare professionals from a task force of the international liaison committee on resuscitation (American Heart Association, European Resuscitation Council, Australian and New Zealand Council on Resuscitation, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Council of Southern Africa, Resuscitation Council of Asia); and the American Heart Association Emergency Cardiovascular Care Committee and the Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation. Circulation. 2015;132(13):1286–1300. doi: 10.1161/CIR.0000000000000144. [DOI] [PubMed] [Google Scholar]
- 11.Fletcher D, Chamberlain D, Handley A. Utstein-style audit of Protocol C: a non-standard resuscitation protocol for healthcare professionals. Resuscitation. 2011;82(10):1265–1272. doi: 10.1016/j.resuscitation.2011.06.012. [DOI] [PubMed] [Google Scholar]
- 12.van Alem AP, Vrenken RH, de Vos R, Tijssen JG, Koster RW. Use of automated external defibrillator by first responders in out of hospital cardiac arrest: prospective controlled trial. Bmj. 2003;327(7427):1312. doi: 10.1136/bmj.327.7427.1312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hasselqvist-Ax I, Nordberg P, Herlitz J. Dispatch of firefighters and police officers in out-of-hospital cardiac arrest: a nationwide prospective cohort trial using propensity score analysis. J Am Heart Ass. 2017;6(10) doi: 10.1161/JAHA.117.005873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nichol G, Detsky AS, Stiell IG, O'Rourke K, Wells G, Laupacis A. Effectiveness of emergency medical services for victims of out-of-hospital cardiac arrest: a metaanalysis. Ann Emerg Med. 1996;27(6):700–710. doi: 10.1016/s0196-0644(96)70187-7. [DOI] [PubMed] [Google Scholar]
- 15.Nichol G, Laupacis A, Stiell IG. Cost-effectiveness analysis of potential improvements to emergency medical services for victims of out-of-hospital cardiac arrest. Ann Emerg Med. 1996;27(6):711–720. doi: 10.1016/s0196-0644(96)70188-9. [DOI] [PubMed] [Google Scholar]
- 16.Berdowski J, Kuiper MJ, Dijkgraaf MG, Tijssen JG, Koster RW. Survival and health care costs until hospital discharge of patients treated with onsite, dispatched or without automated external defibrillator. Resuscitation. 2010;81(8):962–967. doi: 10.1016/j.resuscitation.2010.04.013. [DOI] [PubMed] [Google Scholar]
- 17.Moran PS, Teljeur C, Masterson S, O'Neill M, Harrington P, Ryan M. Cost-effectiveness of a national public access defibrillation programme. Resuscitation. 2015;91:48–55. doi: 10.1016/j.resuscitation.2015.03.017. [DOI] [PubMed] [Google Scholar]
- 18.Nordberg P, Hollenberg J, Rosenqvist M. The implementation of a dual dispatch system in out-of-hospital cardiac arrest is associated with improved short and long term survival. Eu Heart J Acute Cardiovas Care. 2014;3(4):293–303. doi: 10.1177/2048872614532415. [DOI] [PubMed] [Google Scholar]
- 19.Shuster M, Keller JL. Effect of fire department first-responder automated defibrillation. Ann Emerg Med. 1993;22(4):721–727. doi: 10.1016/s0196-0644(05)81856-6. [DOI] [PubMed] [Google Scholar]
- 20.Smith KL, Peeters A, McNeil JJ. Results from the first 12 months of a fire first-responder program in Australia. Resuscitation. 2001;49(2):143–150. doi: 10.1016/s0300-9572(00)00355-5. [DOI] [PubMed] [Google Scholar]
- 21.Baekgaard JS, Viereck S, Moller TP, Ersboll AK, Lippert F, Folke F. The effects of public access defibrillation on survival after out-of-hospital cardiac arrest: a systematic review of observational studies. Circulation. 2017;136(10):954–965. doi: 10.1161/CIRCULATIONAHA.117.029067. [DOI] [PubMed] [Google Scholar]
- 22.Ringh M, Rosenqvist M, Hollenberg J. Mobile-phone dispatch of laypersons for CPR in out-of-hospital cardiac arrest. The New Eng J Med. 2015;372(24):2316–2325. doi: 10.1056/NEJMoa1406038. [DOI] [PubMed] [Google Scholar]
- 23.Yannopoulos D, Aufderheide TP, Abella BS. Quality of CPR: an important effect modifier in cardiac arrest clinical outcomes and intervention effectiveness trials. Resuscitation. 2015;94:106–113. doi: 10.1016/j.resuscitation.2015.06.004. [DOI] [PubMed] [Google Scholar]
- 24.Reynolds JC, Grunau BE, Rittenberger JC, Sawyer KN, Kurz MC, Callaway CW. Association between duration of resuscitation and favorable outcome after out-of-hospital cardiac arrest: implications for prolonging or terminating resuscitation. Circulation. 2016;134(25):2084–2094. doi: 10.1161/CIRCULATIONAHA.116.023309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ro YS, Shin SD, Song KJ. Public awareness and self-efficacy of cardiopulmonary resuscitation in communities and outcomes of out-of-hospital cardiac arrest: a multi-level analysis. Resuscitation. 2016;102:17–24. doi: 10.1016/j.resuscitation.2016.02.004. [DOI] [PubMed] [Google Scholar]
- 26.Wissenberg M, Lippert FK, Folke F. Association of national initiatives to improve cardiac arrest management with rates of bystander intervention and patient survival after out-of-hospital cardiac arrest. JAMA. 2013;310(13):1377–1384. doi: 10.1001/jama.2013.278483. [DOI] [PubMed] [Google Scholar]
- 27.Blewer AL, Ho AFW, Shahidah N. Impact of bystander-focused public health interventions on cardiopulmonary resuscitation and survival: a cohort study. Lancet Public Health. 2020;5(8):e428–ee36. doi: 10.1016/S2468-2667(20)30140-7. [DOI] [PubMed] [Google Scholar]
- 28.Dyson K, Brown SP, May S. Community lessons to understand resuscitation excellence (CULTURE): association between emergency medical services (EMS) culture and outcome after out-of-hospital cardiac arrest. Resuscitation. 2020 doi: 10.1016/j.resuscitation.2020.09.020. [DOI] [PubMed] [Google Scholar]
- 29.Oving I, de Graaf C, Karlsson L. Occurrence of shockable rhythm in out-of-hospital cardiac arrest over time: a report from the COSTA group. Resuscitation. 2020;151:67–74. doi: 10.1016/j.resuscitation.2020.03.014. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.