Abstract
Abstract
Background:
Reduced respiratory muscle strength leads to reduced pulmonary function, chest wall movements in the affected side, and increased chest infections, which thereby reduces oxygenation and ventilation. Respiratory muscle training can be used in acute stroke subjects to increase their pulmonary function.
Purpose:
To compare the short-term effects of diaphragmatic breathing exercise, flow, and volume-oriented incentive spirometry on respiratory function following stroke.
Methods:
A non-randomized hospital-based study was conducted at Kasturba Medical College Hospitals, Mangalore, India. Forty-two sub-acute subjects of either gender, with the first episode of stroke within six months, were assigned to three groups by the consultant, i.e., diaphragmatic breathing group (DBE), Flow oriented-incentive spirometry group (FIS), and volume oriented-incentive spirometry group (VIS; N = 14) each. All subjects received intervention thrice daily, along with conventional stroke rehabilitation protocols throughout the study period. Pre- and post-intervention values were taken on alternate days until day 5 for all the three groups.
Results:
The pulmonary function and maximal respiratory pressures were found to be significantly increased by the end of intervention in all three groups, but FIS and DBE groups had better results than VIS (FVC = FIS group, 13.71%; VIS group, 14.89%; DBE group, 21.27%, FEV1 = FIS group, 25.97%; VIS group, 22.52%; DBE group, 19.38%, PEFR = FIS group, 38.76%; VIS group,9.75%; DBE group, 33.16%, MIP = FIS group, 28.23%; VIS group, 19.36%; DBE group, 52.14%, MEP = FIS group, 43.00%; VIS group, 22.80%; DBE group, 28.68%).
Conclusion:
Even though all interventions had positive outcomes in all variables, flow incentive spirometry had better results across all outcomes (pulmonary function and maximal respiratory pressures) when compared to the other two interventions making it a valuable tool for stroke rehabilitation.
Keywords: Volume and flow incentive spirometry, Diaphragmatic breathing exercise, Acute stroke, Pulmonary function, Maximal respiratory pressures
Introduction
Stroke is one of the prominent causes of death globally and the primary cause of long-term disability worldwide.1 Annually, about 11 million people suffer stroke worldwide, and India is projected to have over 1 million strokes per year.2, 3
Stroke interferes with various respiratory processes depending on the size and severity of the neurological damage.4 Muscular weakness is a prominent deficit in individuals with stroke, which is also seen in respiratory muscles, like the diaphragm,5 which is the primary muscle of inspiration. Stroke survivors have been reported to have reduced diaphragmatic excursion with a higher position of the affected diaphragm, and they showed a reduction in both maximal inspiratory pressure and maximal expiratory pressure.5, 6
The central weakness of the respiratory muscles can adversely affect cough function, which is linked with low thorax expansion and postural trunk defect/malfunction.7 This abnormality is paired with altered chest wall kinematics, which leads to a decline in cardiovascular function and affects oxygen delivery, thereby reducing exercise capacity for activities of daily living.4–9
Stroke survivors demonstrate altered breathing mechanisms and reduction in respiratory efficiency depending on chest wall asymmetry, degree of loss in the chest wall movement, and the extent of muscular paralysis.10, 11 Abnormal breathing patterns have been reported in 18% to 88% of patients with stroke, particularly ones with more severe neurological impairment and depressed consciousness. This is presumed to be because of increased muscle tone and spasticity of the chest wall muscles caused by hemiplegia on the affected side restricting the chest wall.4 Thus they classically present with a restrictive pattern in which there is a reduction in forced expiratory volume in 1 s (FEV1), forced vital capacity (FVC), and total lung capacity (TLC).12, 13 Specifically, expiratory muscle weakness leads to the impairment of cough capacity and expectoration, further leading to the retention of copious secretions resulting in several respiratory complications including aspiration pneumonia and dysphagia that are essential triggers of nonvascular fatality after stroke.14, 15
Stroke patients receive respiratory care that involves use of numerous chest physiotherapy techniques like diaphragmatic breathing exercises, mechanical breathing devices such as volume and flow-oriented incentive spirometry, and use of inspiratory muscle training clinically as part of routine preventive and therapeutic regimen.
Diaphragmatic breathing exercise helps in the diaphragmatic descent during inspiration and its ascent during expiration.16 The benefits include decreased work of breathing, improved oxygenation, ventilation, inflation of the alveoli, the reversal of hypoxemia, and an increase in the diaphragm excursion.16, 17 The volume and flow-oriented incentive spirometer aims to promote adequate alveoli ventilation and increase transpulmonary pressure. The benefits include improved lung volumes and reduced pulmonary complications.18–23 These techniques help in enhanced lung ventilation by increasing the expansion of chest wall, helping maintain or increase appropriate lung volumes and capacities, and eventually reduce the incidence of pulmonary function loss and its eventual complications. Therefore, it aids in the preservation of airway patency by increasing muscle activity.13, 24
Volume-oriented incentive spirometry was found to be effective in improving pulmonary function in acute stroke subjects.25 Therefore, the study aims to compare the effects of diaphragmatic breathing exercises, flow, and volume-oriented incentive spirometry on pulmonary function and maximum respiratory pressures in acute stroke subjects.
Methods
Design, Setting and Study Population
A nonrandomized study was conducted after receiving approval from the Institutional Ethics Committee, Kasturba Medical College, Mangalore, Manipal Academy of Higher Education (IEC KMC MLR 11-18/414), and registered with clinical trials registry of India (CTRI/2018/12/016651). The inclusion criteria were as follows: male and female subjects of the age group 18 to 80 years, diagnosed with the first episode of stroke (within last six months), National Institutes of Health Stroke Scale score 5 to 25 with motor impairment, preserved cognition according to the mini-mental state examination (score >22)26, 27 and able to follow researcher’s verbal commands. The exclusion criteria were as follows: subjects with BP >180/100 mmHg more than twice in 24 h, history of unstable angina, myocardial infarction, or acute heart failures within past one month or neurological conditions other than stroke present before or after their admission to ICU, presence of neurosurgical intervention in the past one month, non-cooperative subjects and pre-existing postural and musculoskeletal deformities affecting lung volumes.
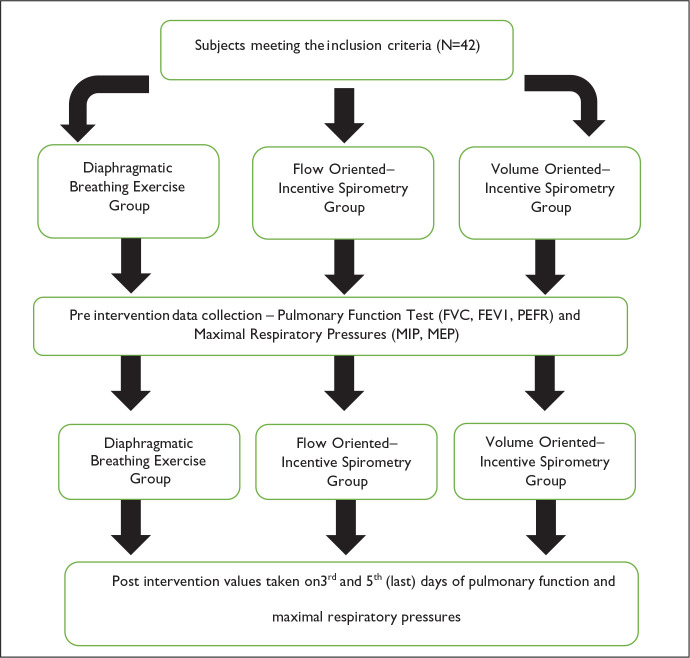
Diagnosed stroke subjects, referred by a neurologist to the Department of Physiotherapy, were approached from December 2018 to March 2020. The aim of the study was explained to the subjects, and those volunteering to participate were recruited after signing a written informed consent. Demographic details and baseline data like pulmonary assessment, including pulmonary function and maximum respiratory pressure values, were taken before the start of any intervention. The consultant allocated eligible subjects to three groups, i.e., diaphragmatic breathing exercise (DBE) group, flow-oriented incentive spirometry (FIS) group (respirometer), and volume-oriented incentive spirometry (VIS) group (Coach 2 device). All the subjects received treatment thrice daily which included three sets of 15 breaths each.26, 28–30 Caretakers were instructed that the given exercise should be performed by the subject once every waking hour for the rest of the day. All the subjects underwent conventional stroke rehabilitation for stroke motor impairments. Pulmonary function and maximum respiratory pressure values will be taken on the first, third, and fifth day (Figure 1).
Figure 1. Participants Recruitment Flowchart.
Methods to Perform Flow-Oriented and Volume-Oriented Incentive Spirometry
Subjects were placed in a semi-recumbent position with slight flexion of knees using pillows under them. They were then asked to take a deep inspiration, which is slow and sustained for a minimum 5 s and exhale passively. This is used to avoid any forceful exhalation. The subject was asked to hold the device upright and then take a slow inspiration such that the ball within the flow spirometer (respirometer–respiratory exerciser–Romsons; Figure 2) or the piston within the volume spirometer (Coach 2 device, Smiths Medical International Ltd, USA; Figure 3) is raised to the set target.31, 32 All techniques were demonstrated by the therapist for a clear understanding of the subject.17, 21 The therapist administered the exercise thrice daily of three sets with 15 repetitions in each session.26–33
Figure 2. Participant Using Flow-Oriented Incentive Spirometry.

Figure 3. Participant Using Volume-Oriented Incentive Spirometry.

Method to Perform Diaphragmatic Breathing Exercise
The subjects were placed in semi-fowler’s position with head and back fully supported, and the abdominal wall relaxed. They were asked to take a slow deep breath through their nose, i.e., from functional residual capacity to total lung capacity with a hold of a minimum of 3 s. They had to be relaxed so that they could appreciate the raised abdomen during breathing. While exhaling, the subject should breathe out through his/her mouth (Figure 4). This movement of the abdomen during breathing in and out has to be felt by the subject by placing his/her hand just below the anterior costal margin on the rectus abdominis.16, 34
Figure 4. Participant Performing Diaphragmatic Breathing Exercise.

Outcome Measures
Pulmonary Function Test
Pulmonary function test was done using a portable machine–a spirometer by COSMED technologies, USA. Variables that were used for this study included the following –forced vital capacity (L), forced expiratory volume in the first second (L), peak expiratory flow rate (L/s), and three tests were taken. The best value was entered in the datasheet.33
Maximum Respiratory Pressure
Two maximum pressures were taken namely maximum inspiratory pressure (cmH2O) where the participant made an inspiratory effort from residual volume to their total lung capacity. Maximum expiratory pressure (cmH2O), was a reverse procedure.35 Each maneuver was maintained for at least 1 s, and three efforts were made. Only the best value was entered in the datasheet.35, 36
Data Analysis
Data were entered and analyzed into a statistical package for the social sciences (SPSS) version 25. Demographic and baseline data were compared across groups using analysis of variance. p-value < .05 will be considered as statistically significant.
Results
This study included 42 acute stroke subjects that met the inclusion criteria. Table 1 describes the baseline anthropometric values of all subjects such as age, gender, height, weight, mini-mental state examination score, and National Institutes of Health Stroke Scale. Table 2 gives a summary of forced vital capacity within the interventional groups before the intervention and the third day and last day for comparison of all groups. Table 3 gives a summary of forced expiratory volume in 1-s values of all interventional groups before and after intervention for comparison. Table 4 gives a summary of peak expiratory flow rate values for comparison of all groups. Table 5 gives a brief of maximal inspiratory pressure values for comparison of all groups. Table 6 summarizes maximal expiratory pressure values for comparison of all groups. Table 7 summarizes the difference between baseline and fifth day between the three intervention groups of forced expiratory volume in 1 s, forced vital capacity, peak expiratory flow rate. Table 8 summarizes the difference between baseline and fifth day between the three intervention groups of maximal inspiratory pressure and maximal expiratory pressure.
Table 1. Demographic Characteristics of Subjects Who Participated in the Study.
| Variables | Diaphragmatic Breathing Exercise (DBE) n = 14 | Flow-Incentive Spirometry (FIS) n = 14 | Volume-Incentive Spirometry (VIS) n = 14 | p Value(p < .05) |
| Age (years)(mean ± SD) | 63.40 ± 7.83 | 56.07 ± 13.10 | 55.79 ± 13.79 | .15 |
| Gender (M:F) | 11:3 | 8:6 | 9:5 | .54 |
| Height (m)(mean ± SD) | 1.61 ± 0.13 | 1.64 ± 0.07 | 1.64 ± 0.07 | .59 |
| Weight (kg)(mean ± SD) | 59.20 ± 9.05 | 67.00 ± 9.29 | 64.14 ± 6.11 | .05 |
| Lesion type (ischemic:hemorrhagic) | 8:6 | 8:6 | 9:5 | |
| Paretic side (right:left) | 6:8 | 8:6 | 7:7 | |
| Duration because stroke(days) | 9.07 ± 9.53 | 5.28 ± 3.66 | 9.92 ± 14.57 | |
| MMSE | 27.53 ± 1.64 | 27.36 ± 1.86 | 27.36 ± 2.31 | .96 |
| NIHSS | 5.60 ± 0.91 | 5.21 ± 0.43 | 5.86 ± 0.86 | .09 |
Abbreviations: MMSE, mini mental state examination; NIHSS, national institute of health stroke scale.
Table 2. Comparison of Forced Vital Capacity Before and After Intervention in Post-stroke Subjects.
| Forced Vital Capacity [Liters (L)] | Baseline (Mean ± SD) | Third Day (Mean ± SD) | Fifth Day (Mean ± SD) |
| Diaphragmatic breathing exercise group (n = 14) | 1.79 ± 0.63 | 1.95 ± 0.85 | 2.17 ± 0.90 |
| Flow incentive spirometry group (n = 15) | 2.05 ± 0.80 | 2.17 ± 0.71 | 2.33 ± 0.70 |
| Volume incentive spirometry group(n = 14) | 1.95 ± 0.75 | 2.20 ± 0.71 | 2.24 ± 0.70 |
| Mean Difference Between Baseline and Fifth Day | |||
| Baseline to Third Day | Third to Fifth Day | Baseline to Fifth Day | |
| Diaphragmatic Breathing exercise group | -0.158.75% | -0.2211.51% | -0.3821.27% |
| p value | 0.27 | 0.04* | 0.01* |
| Flow incentive spirometry group | -0.115.81% | -0.167.47% | -0.2813.71% |
| p value | 0.77 | 0.17 | 0.03* |
| Volume incentive spirometry group | -0.2513.05% | -0.031.62% | -0.2914.89% |
| p value | 0.00** | 1.00 | 0.04* |
Note: *p < .05 statistically significant; **highly significant.
Table 3. Comparison of Forced Expiratory Volume in 1 s (FEV1) Before and After Intervention.
| Forced Expiratory Volume in 1 s [Litres (L)] | Baseline (Mean ± SD) | Third Day (Mean ± SD) | Fifth Day (Mean ± SD) |
| Diaphragmatic breathing exercise group (n = 14) | 1.37 ± 0.51 | 1.47 ± 0.66 | 1.63 ± 0.61 |
| Flow incentive spirometry group(n = 14) | 1.56 ± 0.48 | 1.69 ± 0.57 | 1.97 ± 0.57 |
| Volume incentive spirometry group (n = 14) | 1.39 ± 0.75 | 1.64 ± 0.58 | 1.70 ± 0.68 |
| Mean Difference Between First and Fifth Day | |||
| FEV1 | Baseline to Third Day | Third Day to Fifth Day | Baseline to Fifth Day |
| Diaphragmatic breathing exercise group | -0.107.81% | -0.1510.73% | -0.2619.38% |
| p value | 1.00 | 0.29 | 0.18 |
| Flow incentive spirometry group | -0.128.28% | -0.2716.34% | -0.4025.97% |
| p value | 0.90 | 0.11 | 0.00** |
| Volume incentive spirometry group | -0.2518.15% | -0.063.70% | -0.3122.52% |
| p value | 0.23 | 1.00 | 0.17 |
Note: *p < .05 statistically significant; **highly significant.
Table 4. Comparison of Peak Expiratory Flow Rate (PEFR) Before and After Intervention.
| Peak Expiratory Flow Rate (PEFR)[Litres(L/s)] | Baseline (Mean ± SD) | Third Day (Mean ± SD) | Fifth Day (Mean ± SD) |
| Diaphragmatic breathing exercise group (n = 14) | 2.09 ± 0.97 | 2.36 ± 1.10 | 2.78 ± 1.43 |
| Flow incentive spirometry group (n = 14) | 2.06 ± 0.62 | 2.76 ± 1.30 | 2.85 ± 1.20 |
| Volume incentive spirometry group (n = 14) | 2.10 ± 1.12 | 2.16 ± 0.81 | 2.31 ± 1.19 |
| Mean Difference Between First and Fifth Day | |||
| Baseline to Third Day | Third Day to Fifth Day | Baseline to Fifth Day | |
| Diaphragmatic breathing exercise group | -0.2712.96% | -0.4217.89% | -0.6933.16% |
| p value | 1.00 | 0.41 | 0.16 |
| Flow incentive spirometry group | -0.7034.25% | -0.093.36% | -0.7938.76% |
| p value | 0.04* | 1.00 | 0.04* |
| Volume incentive spirometry group | -0.052.58% | -0.156.99% | -0.209.75% |
| p value | 1.00 | 1.00 | 1.00 |
Note: *p < .05 statistically significant.
Table 5. Comparison of Maximal Inspiratory Pressure Before and After Intervention.
| Maximal Inspiratory Pressure [cmH2O] | Baseline (Mean ± SD) | Third Day (Mean ± SD) | Fifth Day (Mean ± SD) |
| Diaphragmatic breathing exercise group(n = 14) | 24.93 ± 14.51 | 32.20 ± 19.50 | 37.93 ± 19.81 |
| Flow incentive spirometry group(n = 14) | 32.64 ± 15.39 | 39.14 ± 15.69 | 41.86 ± 11.64 |
| Volume incentive spirometry group(n = 14) | 33.57 ± 14.01 | 37.21 ± 14.35 | 40.07 ± 13.06 |
| Mean Differences Compared on Fifth Day in Between Groups | |||
| Maximal Inspiratory Pressure | Baseline to Third Day | Third Day to Fifth Day | Baseline to Fifth Day |
| Diaphragmatic breathing exercise group | -7.2629.14% | -5.7317.81% | -13.0052.14% |
| p value | 0.00** | 0.06 | 0.00** |
| Flow incentive spirometry group | -6.5019.91% | -2.716.93% | -9.2128.23% |
| p value | 0.00** | 1.00 | 0.01* |
| Volume incentive spirometry group versus | -3.6410.85% | -2.857.68% | -6.5019.36% |
| p value | 0.04* | 0.31 | 0.04* |
Note: *p < .05 statistically significant; **highly significant.
Table 6. Comparison of Maximal Expiratory Pressure Before and After Intervention.
| Maximal Expiratory Pressure [cmH2O] | Baseline (Mean ± SD) | Third Day (Mean ± SD) | Fifth Day (Mean ± SD) |
| Diaphragmatic breathing exercise group (n = 14) | 35.80 ± 17.10 | 41.73 ± 16.36 | 46.07 ± 17.46 |
| Flow incentive spirometry group(n = 14) | 36.71 ± 16.34 | 48.79 ± 19.18 | 52.50 ± 17.18 |
| Volume incentive spirometry group(n = 14) | 38.21 ± 13.46 | 43.79 ± 13.49 | 46.93 ± 13.91 |
| Mean Differences | |||
| MEP | Baseline to Third Day | Third Day to Fifth Day | Baseline to Fifth Day |
| Diaphragmatic breathing exercise group | -5.9316.57% | -4.3310.38% | -10.2628.68% |
| p value | 0.03* | 0.00* | 0.01* |
| Flow incentive spirometry group | -12.0732.88% | -3.717.61% | -15.7843.00% |
| p value | 0.00* | 0.41 | 0.00* |
| Volume incentive spirometry group versus | -5.5714.58% | -3.147.18% | -8.7122.80% |
| p value | 0.01* | 0.26 | 0.00* |
Note: *p < .05 statistically significant; **highly significant.
Table 7. Difference Between Baseline and Fifth Day Between the Three Intervention Groups of Forced Expiratory Volume in 1 s, Forced Vital Capacity, Peak Expiratory Flow Rate.
| Baseline Minus Fifth Day (Mean Difference) | Forced Vital Capacity [Liters (L)] | Forced Expiratory Volume in 1 s [Liters (L)] | Peak Expiratory Flow Rate [Liters/s (L/s)] |
| Flow incentive spirometry group versus diaphragmatic breathing exercise group | 0.1 | 0.15 | 0.11 |
| p value | 0.77 | 0.74 | 0.39 |
| Flow incentive spirometry group versus volume incentive spirometry group | 0.00 | 0.1 | 0.59 |
| p value | 0.77 | 0.74 | 0.39 |
| Volume incentive spirometry group versus diaphragmatic breathing exercise group | 0.09 | 0.05 | 0.48 |
| p value | 0.77 | 0.74 | 0.39 |
Note: *p < .05 statistically significant.
Table 8. Difference Between Baseline and Fifth Day Between the Three Intervention Groups of Maximal Inspiratory Pressure and Maximal Expiratory Pressure.
| Baseline Minus Fifth Day (Mean Difference) | Maximal Inspiratory Pressure | Maximal Expiratory Pressure |
| Flow incentive spirometry group versus diaphragmatic breathing exercise group | 3.79 | 5.52 |
| p value | 0.20 | 0.26 |
| Flow incentive spirometry group versus volume incentive spirometry group | 2.71 | 7.08 |
| p value | 0.20 | 0.26 |
| Volume incentive spirometry group versus diaphragmatic breathing exercise group | 6.5 | 1.56 |
| p value | 0.20 | 0.26 |
Note: *p < .05 statistically significant.
Discussion
It is the first study to our knowledge that evaluates the effects of diaphragmatic breathing exercises, volume and flow-oriented incentive spirometry on pulmonary function and maximal respiratory pressures in patients with stroke compared to the effects of the three interventions. The study revealed that all three interventions were successful in enhancing the pulmonary function and maximal respiratory pressures when respiratory muscle training is given for five days in acute stroke subjects.
Pulmonary function tests such as forced expiratory volume in 1 s (L), forced vital capacity (L), and peaked expiratory flow rate (L/s) improved in all three interventions. However, flow-oriented incentive spirometry showed better improvement in forced vital capacity values when compared to others. One of the reasons could be the higher baseline value at the start of the intervention in this group. Although these interventions showed clinical significance in pulmonary function of forced vital capacity, higher statistical significance and percentage change were observed in the diaphragmatic breathing exercise group (21.27%) when compared to flow and volume-oriented incentive spirometry (13.71% and14.89%, respectively).
Forced expiratory volume in 1 s also exhibited improvement clinically in all the three groups by the end of this study. However, statistically significant improvement was found in flow-oriented incentive spirometry (25.97%) when compared to diaphragmatic (19.38%) and volume-oriented incentive spirometry (22.52%).
Peaked expiratory flow rate values improved in flow-oriented incentive spirometry (38.76%) with statistical significance than in the other two groups. Even though peaked expiratory flow rate values were not statistically significant, clinically, we noticed an improvement in the other two groups. The present study suggests that flow-oriented incentive spirometry has shown more improvement in pulmonary function overall than in the other two interventions, though all interventions had shown an increase from baseline.
Our study was in line with the results given by Joo et al.28 who, in his study, showed a 27.89% increase in forced expiratory volume in 1 s and 26% increase in forced vital capacity value after administering game-based exercise as an intervention to stroke subjects for five weeks. A study done by Jung et al.34used inspiratory muscle training as an intervention in stroke and found a 9.6% increase in forced expiratory volume in 1 s and 6.56% increase in forced vital capacity. Possible reasons for reduced pulmonary function in stroke are because of reduced activity of the rib cage muscles and diaphragm. The diaphragm of the affected side also tends to attain a higher position, thereby reducing the pulmonary capacity of that side. Similar interventions were given to patients with open abdominal surgery by Kumar et al.37 and a significant increase in forced expiratory volume in 1 s and forced vital capacity (18% to 25%) was found.
In the overall pulmonary function, the flow-oriented incentive spirometry group has shown better improvement than volume-oriented incentive spirometry. Possible reasons for flow-oriented incentive spirometry showing better improvement are as follows: (a) there is visual feedback with this device, and it is easy to follow, which motivates the patient and thereby increases the adherence to this device.
Earlier studies have already highlighted that the flow-oriented incentive spirometry device does not facilitate the diaphragm but causes increased use of accessory muscles of the rib-cage.38 It also imposes more significant work of breathing in this device.39, 40 We postulate that the mechanism by which it was useful primarily in the stroke population is that as there is the weakness of the abdominal muscle and respiratory muscles, the affected side of hemi diaphragm is even more elevated than the nonaffected side.41 It shows a reduced diaphragmatic motion of the paretic side.42 Therefore, stroke patients are unable to generate negative pressure and hence show reduced forced vital capacity and maximal inspiratory pressure. Because the diaphragm is the primary muscle and cannot be used for normal respiration because of the stroke, these patients find it easier to use accessory muscle for respiration, as promoted by this device.38 This group, hence, has shown better results than others. This might be the reason why our results do not reflect the findings from the previous studies that have used these interventions in abdominal surgery patients where volume-oriented incentive spirometry was proven to be better.
Although volume-oriented incentive spirometry provides visual feedback, it was a little difficult to follow for our patients when compared to the flow-oriented incentive spirometry device. Possible reasons for its group showing improvement from baseline might be that it produces more symmetrical expansion in the pulmonary rib cage during incentive spirometry, suggesting that it promotes an increase in ventilator output on the paretic side, resulting in more significant expansion. It also provides low-level resistance training to the diaphragm and minimizes fatigue.24, 43
Diaphragmatic breathing exercise works on the principle of increasing diaphragmatic descent during deep inspiration to increase collateral ventilation and diaphragmatic excursion, leading to an increase in pulmonary capacities,24 but the adherence to this technique is least because there is no visual feedback, and therefore, patients do not practice it as often as required.
Secondary outcome variables were maximal inspiratory pressure and maximal expiratory pressure under maximal respiratory pressures. They help us assess and monitor the weaknesses of inspiratory musculature.25 Maximal inspiratory pressure has shown an increasing trend with statistical significance in all three groups. However, the diaphragmatic breathing exercise group has shown high statistical significance with a higher percentage change of 52.14% in maximal inspiratory pressure when compared with flow-oriented incentive spirometry (28.23%) and volume-oriented incentive spirometry (19.36%). On the other hand, flow-oriented incentive spirometry has shown 43% of change with higher statistical significance in maximal expiratory pressure when compared to diaphragmatic breathing exercise and volume-oriented incentive spirometry.
Our study is in agreement with Britto et al., where they found a 50.7% increase in maximal inspiratory pressure after eight weeks of inspiratory muscle training in chronic stroke. A similar study that gave inspiratory training to one group of stroke patients and expiratory muscle training to another group found 55% and 38% improvement from baseline, respectively, in maximal inspiratory pressure values and 47% and 32% improvement in maximal expiratory pressure after four weeks of training.44 A study that provided high-intensity home-based respiratory muscle training also found 62% improvement in inspiratory muscle strength and 68% in that of expiratory muscles.45
Stroke not only involves upper and lower extremities but also affects the trunk and pulmonary musculature. The abdominal muscles contribute to diaphragmatic action and play an essential role during inspiration, for maintaining abdominal wall tonus.46Abdominal muscles help diaphragm function in a more favorable position on its length-tension curve.47 Stroke leads to weakness of the abdominal muscles, which may affect this synergy by weakening the capacity of the diaphragm to generate negative force.46 The decline of maximal inspiratory pressure in stroke according to a previous study includes weakness of the expiratory muscles and may influence the effectiveness of coughing and the airway clearance reduction thus increasing the risk of aspiration.25 We recommend further studies that may evaluate the molecular and genetic mechanisms behind the changes elicited in our study.
Conclusion
Our study concludes that acute stroke patients show improvement in pulmonary function and maximal respiratory pressures with a short duration intervention of five days. The present study determines that flow-oriented incentive spirometry was proven to be more effective in improving both primary and secondary outcomes with higher percentage change when compared to diaphragmatic breathing exercise group and volume-oriented incentive spirometry.
Acknowledgment
The authors would like to thank all their study participants for participating in the study.
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Footnotes
ORCID iDs: Stephen Rajan Samuel  https://orcid.org/0000-0002-4744-0180
https://orcid.org/0000-0002-4744-0180
Sampath Kumar Amaravadi  https://orcid.org/0000-0002-4744-0180
https://orcid.org/0000-0002-4744-0180
Authorship Contribution
Natasha Shetty, Gopala Krishna Alaparthi, and Stephen R Samuel were responsible for conceiving and designing the study, integrating the setup, collecting, analyzing, and interpreting the data, drafting and critically revising the article, and approving the final version of the article.
Natasha Shetty, Stephen R Samuel, Abraham M Joshua, Shivanand Pai, and Sampath Kumar Amaravadi were responsible for collecting, analyzing, and interpreting the data, critically revising the article, and approving the final version of the article.
Ethical Statement
This study was conducted after receiving approval from the Institutional Ethics Committee, Kasturba Medical College Mangalore, Manipal Academy of Higher Education (IEC KMC MLR 11-18/414), and registered with Clinical Trials Registry of India (CTRI/2018/12/016651).
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1.Mozaffarian D, Benjamin EJ, Go AS,. et al. Executive summary: Heart disease and stroke statistics-2016 update: A report from the American Heart Association. Circulation 2016; 133: 447–454. [DOI] [PubMed] [Google Scholar]
- 2.Jandt SR, da Sil Caballero RM, Junior LA,. et al. Correlation between trunk control, respiratory muscle strength and spirometry in subjects with stroke: An observational study. Physiother. Res. Int 2011; 16: 218–224. [DOI] [PubMed] [Google Scholar]
- 3.Mehndiratta MM, Singhal AB, Chaturvedi S,. et al. Meeting the challenges of stroke in India. Neurology 2013; 80: 2246–2247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rochester CL and Mohsenin V.. Respiratory complications of a stroke. Semin Respir Crit Care Med 2002; 23(03): 248–260. [DOI] [PubMed] [Google Scholar]
- 5.Cho JE, Lee HJ, Kim MK,. et al. The improvement in respiratory function by inspiratory muscle training is due to structural muscle changes in patients with stroke: A randomized controlled pilot trial. Top Stroke Rehabil 2018; 25: 37–43. [DOI] [PubMed] [Google Scholar]
- 6.Jo MR and Kim NS.. Combined respiratory muscle training facilitates expiratory muscle activity in stroke patients. J Phys Ther Sci 2017; 29: 1970–1973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yoo HJ and Pyun SB. Efficacy of bedside respiratory muscle training in patients with stroke: A randomized controlled trial. Am J Phys Med Rehabil 2018; 97: 691–697. [DOI] [PubMed] [Google Scholar]
- 8.Cabral EE, Resqueti VR, Lima IN,. et al. Effects of positive expiratory pressure on chest wall volumes in subjects with stroke compared to healthy controls: A case-control study. Braz J Phys Ther 2017; 21: 416–424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gomes-Neto M, Saquetto MB, Silva CM,. et al. Effects of respiratory muscle training on respiratory function, respiratory muscle strength, and exercise tolerance in patients poststroke: A systematic review with meta-analysis. Arch. Phys Med Rehabil 2016; 97: 1994–2001. [DOI] [PubMed] [Google Scholar]
- 10.Ferretti G, Girardis M, Moia C,. et al. Effects of prolonged bed rest on cardiovascular oxygen transport during submaximal exercise in humans. Eur J Appl Physiol Occup Physiol 1998; 78: 398–402. [DOI] [PubMed] [Google Scholar]
- 11.Seo KC, Lee HM, and Kim HA.. The effects of combination of inspiratory diaphragm exercise and expiratory pursed-lip breathing exercise on pulmonary functions of stroke subjects. J Phys Ther Sci 2013; 25: 241–244. [Google Scholar]
- 12.American Thoracic Society/European Respiratory Society. ATS/ERS Statement on respiratory muscle testing. Am J Respir Crit Care Med 2002; 166: 518–624. [DOI] [PubMed] [Google Scholar]
- 13.Pfeffer G and Povitz M.. Respiratory management of subjects with neuromuscular disease: Current perspectives. Degener Neurol Neuromuscul Dis 2016; 6: 111–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Billinger SA, Coughenour E, Mackay-Lyons MJ,. et al. Reduced cardiorespiratory fitness after stroke: Biological consequences and exercise-induced adaptations. Stroke Res Treat 2012; 2012: 959120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Katzan IL, Cebul RD, Husak SH,. et al. The effect of pneumonia on mortality among subjects hospitalized for acute stroke. Neurology 2003; 60: 620–625. [DOI] [PubMed] [Google Scholar]
- 16.Nancy H. and Tecklin JS.. “Respiratory treatment.” In: Irwin S., Tecklin J.S., eds Cardiopulmonary Physical Therapy: A Guide to Practice. Mosby, 1995: pp. 356–374. [Google Scholar]
- 17.Grams ST, Ono LM, Noronha MA,. et al. Breathing exercises in upper abdominal surgery: A systematic review and meta-analysis. Rev Bras Fisioter 2012; 16: 345–353. [DOI] [PubMed] [Google Scholar]
- 18.Tomich GM, França DC, Diório ACM,. et al. Breathing pattern, thoracoabdominal motion and muscular activity during three breathing exercises. Braz J Med Biol Res 2007; 40: 1409–1417. [DOI] [PubMed] [Google Scholar]
- 19.Renault JÁ, Costa-val R, Rossetti MB,. et al. Comparison between deep breathing exercises and incentive spirometry after CABG surgery. Rev Bras Cir Cardiovasc 2009; 24: 165–172. [DOI] [PubMed] [Google Scholar]
- 20.Yamaguti WPS, Sakamoto ET, Panazzolo D,. et al. Mobilidade diafragmática durante a espirometria de incentivo orientada a fluxo e a volume em indivíduos sadios. J Bras Pneumol 2010; 36: 738–745. [DOI] [PubMed] [Google Scholar]
- 21.Pasquina P, Tramèr MR, Granier JM,. et al. Respiratory physiotherapy to prevent pulmonary complications after abdominal surgery: A systematic review. Chest 2006; 130:1887–1899. [DOI] [PubMed] [Google Scholar]
- 22.Guimarães MM, El Dib R, Smith AF,. et al. Incentive spirometry for prevention of postoperative pulmonary complications in upper abdominal surgery. Cochrane Database Syst Rev 2009; 2009(3): CD006058. [DOI] [PubMed] [Google Scholar]
- 23.Paisani Dde M, Lunardi AC, da Silva CC,. et al. Volume rather than flow incentive spirometry is effective in improving chest wall expansion and abdominal displacement using optoelectronic plethysmography. Respir Care 2013; 58: 1360–1366. [DOI] [PubMed] [Google Scholar]
- 24.Alaparthi GK, Augustine AJ, Anand R,. et al. Comparison of diaphragmatic breathing exercise, volume and flow incentive spirometry, on diaphragm excursion and pulmonary function in patients undergoing laparoscopic surgery: A randomized controlled trial. Minim Invasive Surg 2016; 2016: 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Teixeira-Salmela LF, Parreira VF, Britto RR,. et al. Respiratory pressures and thoracoabdominal motion in community-dwelling chronic stroke survivors. Arch Phys Med Rehabil 2005; 86: 1974–1978. [DOI] [PubMed] [Google Scholar]
- 26.Lyden P.Using the national institutes of health stroke scale: A cautionary tale. Stroke 2017; 48: 513–519. [DOI] [PubMed] [Google Scholar]
- 27.Folstein MF, Folstein SE, and McHugh PR.. “Mini-mental state”: A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 1975; 12: 189–198. [DOI] [PubMed] [Google Scholar]
- 28.Joo S, Shin D, and Song C.. The effects of game-based breathing exercise on pulmonary function in stroke subjects: A preliminary study. Med Sci Monit 2015; 21: 1806–1811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kulnik ST, Birring SS, Moxham J,. et al. Does respiratory muscle training improve cough flow in acute stroke? Pilot randomized controlled trial. Stroke 2015; 46: 447–453. [DOI] [PubMed] [Google Scholar]
- 30.Messaggi-Sartor M, Guillen-Solà A, Depolo M,. et al. Inspiratory and expiratory muscle training in subacute stroke: A randomized clinical trial. Neurology 2015; 85: 564–572. [DOI] [PubMed] [Google Scholar]
- 31.American Association for Respiratory Care. AARC clinical practice guideline. Incentive spirometry. Respir Care 1991; 36: 1402–1405. [PubMed] [Google Scholar]
- 32.Dean RH and Richard DB.. Devices for chest physiotherapy, incentive spirometry and intermittent positive-pressure breathing. Respir Care Equip 1995; 1995: 245–263. [Google Scholar]
- 33.European RS;. American Thoracic Society. ATS/ERS statement on respiratory muscle testing. Am J Respir Crit Care Med 2002; 166: 518. [DOI] [PubMed] [Google Scholar]
- 34.Jung JH and Kim NS.. Effects of inspiratory muscle training on diaphragm thickness, pulmonary function, and chest expansion in chronic stroke patients. J Korean Soc Phys Med 2013; 8: 59–69. [Google Scholar]
- 35.Costa D, Gonçalves HA, Lima LP,. et al. New reference values for maximal respiratory pressures in the Brazilian population. J Bras Pneumol 2010; 36: 306–312. [DOI] [PubMed] [Google Scholar]
- 36.Evans JA and Whitelaw WA.. The assessment of maximal respiratory mouth pressures in adults. Respir Care 2009; 54: 1348–1359. [PubMed] [Google Scholar]
- 37.Kumar AS, Alaparthi GK, Augustine AJ,. et al. Comparison of flow and volume incentive spirometry on pulmonary function and exercise tolerance in open abdominal surgery: A randomized clinical trial. J Clin Diagn Res.2016; 10: KC01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bolina IC, Coelho RMR, Torres MMC,. et al. Effect of flow and volume-oriented incentive spirometry on diaphragmatic and scalenus muscles activation. Eur Respir J 2002; 20: 180s. [Google Scholar]
- 39.Weindler J and Kiefer T.. The efficacy of postoperative incentive spirometry is influenced by the device-specific imposed work of breathing. Chest 2001; 119: 1858–1864. [DOI] [PubMed] [Google Scholar]
- 40.Mang H and Obermayer A.. Imposed work of breathing during sustained maximal inspiration: Comparison of six incentive spirometers. Respir Care 1989; 34: 1122–1128. [Google Scholar]
- 41.de Almeida IC, Clementino AC, Rocha EH,. et al. Effects of hemiplegy on pulmonary function and diaphragmatic dome displacement. Resp Physiol Neurobi 2011; 178: 196–201. [DOI] [PubMed] [Google Scholar]
- 42.Cohen E, Mier A, Heywood P,. et al. Diaphragmatic movement in hemiplegic patients measured by ultrasonography. Thorax 1994; 49: 890–895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lima IN, Fregonezi GA, Melo R,. et al. Acute effects of volume-oriented incentive spirometry on chest wall volumes in patients after a stroke. Respir Care 2014; 59: 1101–1107. [DOI] [PubMed] [Google Scholar]
- 44.Kulnik ST, Birring SS, Moxham J,. et al. Does respiratory muscle training improve cough flow in acute stroke? Pilot randomized controlled trial. Stroke 2015; 46: 447–453. [DOI] [PubMed] [Google Scholar]
- 45.de Menezes KK Nascimento LR, Ada L,. et al. High-intensity respiratory muscle training improves strength and dyspnea poststroke: A double-blind randomized trial. Arch Phys Med Rehabil 2019; 100: 205–212. [DOI] [PubMed] [Google Scholar]
- 46.De Troyer A and Estenne M.. Functional anatomy of respiratory muscles. Clin Chest Med 1998; 9: 175–192. [PubMed] [Google Scholar]
- 47.Ewig JM, Griscom NT, and Wohl ME.. The effect of the absence of abdominal muscles on pulmonary function and exercise. Am J Respir Crit Care Med 1996; 153: 1314–1321. [DOI] [PubMed] [Google Scholar]