One of the most encountered complications of ESKD, especially for patients undergoing maintenance hemodialysis, is the subtle but clinically important progressive deterioration of nutritional status. This unique state of metabolic and nutritional derangements, termed protein-energy wasting (PEW), is closely associated with major adverse clinical outcomes, such as higher rates of hospitalization and death in these patients. The etiology of PEW is complex and includes multiple factors that affect nutritional and metabolic status simultaneously (1). Among these, the content and composition of dietary nutrient intake are important determinants of nutritional and metabolic states of these patients.
Dietary nutrient intake encompasses a cadre of macro- and micronutrients, and its appropriate management requires attention to these specific groups. The combination and the quantity of macronutrients in the diet define the total dietary energy intake. In patients on maintenance hemodialysis, it is believed that inappropriately low dietary energy intake relative to the actual demand is considered to lead to PEW in the long term. Of note, inappropriately low dietary energy intake is not only easy to define and diagnose, but also believed to be treatable. In adults with CKD, nutrition in CKD guidelines recommend prescribing a dietary energy intake of 25–35 kcal/kg body weight per day to maintain normal nutritional status (2). The guideline suggests adjusting the energy intake on the basis of age, sex, level of physical activity, body composition, weight status goals, CKD stage, and concurrent illness or presence of inflammation. In individuals who are unable to achieve sufficient energy intake to meet their relative nutritional requirements despite aggressive dietary counseling, a trial of oral nutritional supplements to improve nutritional status is also recommended. Notably, the evidence behind these recommendations is not strong (1C and 2D, respectively), indicating the need for additional research.
In this issue of CJASN, Yang et al. (3) report their findings regarding the effects of a fat-based energy-dense nutritional supplement on various measures of nutritional status in patients receiving maintenance hemodialysis who have low dietary energy intake. They randomized 240 nondiabetic patients who had dietary energy intake <30 kcal/kg per day in a 1:1 ratio to receive supplemental oral fat-based energy-dense supplement (300 kcal daily) or routine care for 12 weeks (n=120 per group). The additional energy intake provided by the oral nutritional supplement was 4.9±1.4 kcal/kg per day. Although the researchers were blinded to the data, the participants were not. The primary outcome was the change in phase angle measured by bioelectrical impedance analysis (BIA) over the 12 weeks, and the secondary outcome was the quality of life using the Kidney Disease Quality of Life Short Form (KDQOL-SF). Other exploratory outcomes included serum concentrations of albumin, prealbumin, transferrin, and hemoglobin; body mass index (BMI); handgrip strength; midarm muscle circumference; and lean and fat tissue indices by BIA.
What did the study show? At the end of 12 weeks, 112 (93%) participants in the control group and 116 (97%) participants in the intervention group were included in the complete case analysis. Adherence to intervention was reported as 88% during the study. As expected, the intervention led to a higher energy intake than in those in the control group (28.2±6.3 versus 23.0±6.5 kcal/kg per day; P<0.001).
In terms of the primary outcome, there was no significant difference in the change in phase angle over 12 weeks between groups (0.0±0.5 versus 0.0±0.6; P=0.82). All domains of quality of life did not differ between the groups, including sleep domain. In terms of the exploratory outcomes, the most notable findings were statistically significant increases in fat tissue index (0.6±1.1 versus 0.1±1.1 kg/m2) and BMI (0.1±0.6 versus 0±0.5 kg/m2), all in favor of the intervention group; however, the differences were clinically minute. None of the other outcomes showed any difference between intervention and control groups. A notable difference was also seen in reported adverse outcomes between groups, specifically in gastrointestinal issues such as nausea, vomiting, abdominal pain, bloating, and diarrhea (33% in the intervention group versus 19% in the control group). Despite the high fat content of the intervention, there were no significant differences in the changes in serum triglycerides, total cholesterol, HDL cholesterol, and LDL cholesterol between groups.
What do the results mean? The primary outcome measure in this well-executed study (i.e., phase angle measured by BIA) was found to be insignificant. The results also suggest that an energy-dense nutritional supplement efficiently improved dietary energy intake in patients on maintenance hemodialysis who were considered to have low dietary energy intake, and there were statistically significant, albeit clinically miniscule, increases in BMI and fat mass. The additional data showed that fat-based energy-dense supplementation did not have a significant effect on a list of well-recognized markers of nutrition status, including but not limited to visceral and somatic protein stores and anthropometric measures, and markers of systemic inflammation. Although these results can be considered as disappointing overall, they are not necessarily surprising. For example, on a positive note, it is well established that increased energy intake leads to weight gain and fat deposition, and this study confirms that this is also possible in patients on maintenance hemodialysis (4). On the other hand, it is not surprising that markers of visceral and somatic protein stores did not improve by providing purely fat-based energy supplements without any other macronutrients, especially supplemental amino acids. Although improvements in protein stores can be best achieved by a combination of macronutrient supplementation, amino acids are the mandatory ingredient, and fat and carbohydrate supplementation is usually provided for added benefit (5).
Similar arguments can be made for the secondary outcome of the study (i.e., measures of quality of life). Lower dietary nutrient intake, especially if associated with a chronic illness such as ESKD, is known to be associated with low quality of life and depressive symptoms. The question that remains to be answered is whether a condensed supplement rather than actual food will be able to improve these symptoms. The data by Yang et al. (3) suggest that this is unlikely to happen, at least with the specific supplement used and the timing and length of which it was provided in this study. It is notable that although adherence was excellent in the study, the side effect profile was notably worse in the intervention arm, especially related to gastrointestinal symptoms. These side effects are reported in multiple previous studies using a variety of nutritional supplements. It is again unrealistic to expect that an intervention that is known to be associated with significant inconvenience would improve quality of life by simply increasing energy intake.
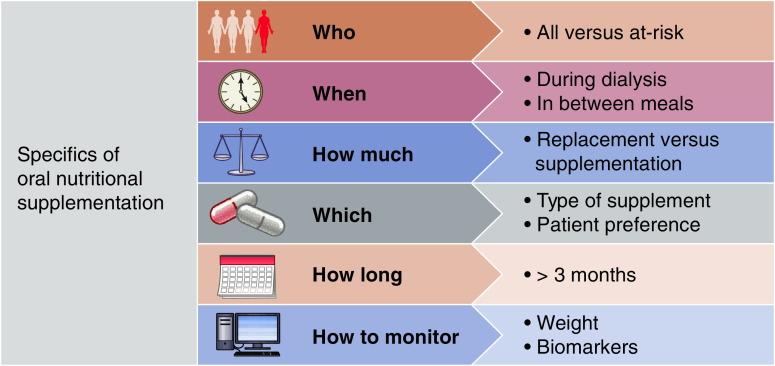
What are the implications of these findings for further research and clinical care? There are several important lessons that can be learned from this study. First and foremost, these observations emphasize the need for precision nutrition in patients on maintenance hemodialysis (6). Precision nutrition can be achieved by multiple strategies in these patients (Figure 1); some are directly related to the results of the study by Yang et al. (3). For example, the matching of the appropriate choice of outcome with the dietary intervention is crucial for assessment of efficacy. In that sense, this study confirms the basic proof of concept (i.e., extra energy intake leads to increases in fat mass and body weight). Whether this effect on these intermediate outcomes is beneficial in the longer term is also debatable because actual body weight is closely related to hospitalization and death in patients on maintenance hemodialysis (7). On the other hand, expecting changes in protein stores with fat supplementation only is a rather ambitious goal.
Figure 1.
Nutritional supplementation in patients on maintenance hemodialysis: a model for precision nutrition.
Another important aspect of precision nutrition is selection of the patient population. Yang et al. (3) targeted patients with dietary energy intake <30 kcal/kg body weight per day, a threshold that does not necessarily indicate clinically significant low levels, especially given the overall nutrition profile of the study patients. It is possible that the benefits of an energy-dense supplement would have been more noticeable if the threshold was lower and the adverse effects of low dietary energy intake, such as weight loss, were noticeable in the study patients. A similar argument can be made for other nutritional markers, such as serum albumin and prealbumin, because these markers were within normal ranges in the study patients. Likewise, patients with barriers to adequate energy intake or ones with obvious reasons to require more than usual would be more suitable to observe the likely effects. Hospitalized patients with acute illnesses (8) or ones who do not have direct or easy access to regular meals, such as the elderly, are good examples of these high-risk patients.
Finally, one should consider the right prescription for nutritional supplementations. In doing so, considering the actual need of daily energy of each subject, patient preference and acceptance, ability to assess the efficacy, and determining the duration of the intervention are crucial aspects of precision nutrition. These are hard-to-implement features in a randomized clinical trial that limits our ability to generalize the findings, such as reported by Yang et al. (3). Accordingly, the subsequent studies testing the efficacy of this particular or some other form of nutritional supplementations, such as ones incorporating several macronutrients, must consider the patient characteristics. Nevertheless, the investigators should be commended for designing and executing this informative study. We must continue to perform similar high-quality research that can be translated into clinical care to provide the most optimal nutrition care for our patients.
Disclosures
T.A. Ikizler reports consultancy agreements with Abbott Renal Care, Corvidia, Fresenius-Kabi, International Society of Nephrology, La Renon, and Nestle; receiving honoraria from La Renon and Nestle; patents and inventions with Vanderbilt University Medical Center; and serving as a scientific advisor or member of Fresenius-Kabi and Kidney International.
Funding
This work was supported by National Institute of Diabetes and Digestive and Kidney Diseases grant P30 DK079341.
Acknowledgments
The content of this article reflects the personal experience and views of the author(s) and should not be considered medical advice or recommendation. The content does not reflect the views or opinions of the American Society of Nephrology (ASN) or CJASN. Responsibility for the information and views expressed herein lies entirely with the author(s).
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
See related article, “The Effects of Oral Energy-Dense Supplements on Nutritional Status in Nondiabetic Maintenance Hemodialysis Patients: A Randomized Controlled Trial,” on pages 1228–1236.
References
- 1.Carrero JJ, Stenvinkel P, Cuppari L, Ikizler TA, Kalantar-Zadeh K, Kaysen G, Mitch WE, Price SR, Wanner C, Wang AY, ter Wee P, Franch HA: Etiology of the protein-energy wasting syndrome in chronic kidney disease: A consensus statement from the International Society of Renal Nutrition and Metabolism (ISRNM). J Ren Nutr 23: 77–90, 2013 [DOI] [PubMed] [Google Scholar]
- 2.Ikizler TA, Burrowes JD, Byham-Gray LD, Campbell KL, Carrero JJ, Chan W, Fouque D, Friedman AN, Ghaddar S, Goldstein-Fuchs DJ, Kaysen GA, Kopple JD, Teta D, Yee-Moon Wang A, Cuppari L: KDOQI clinical practice guideline for nutrition in CKD: 2020 update. Am J Kidney Dis 76: S1–S107, 2020 [DOI] [PubMed] [Google Scholar]
- 3.Yang Y, Qin X, Chen J, Wang Q, Kong Y, Wan Q, Tao H, Liu A, Li Y, Lin Z, Huang Y, He Y, Lei Z, Liang M: The effects of oral energy-dense supplements on nutritional status in nondiabetic maintenance hemodialysis patients: A randomized controlled trial [published online ahead of print June 21, 2021]. Clin J Am Soc Nephrol 16: 1228–1236, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Theilade S, Christensen MB, Vilsbøll T, Knop FK: An overview of obesity mechanisms in humans: Endocrine regulation of food intake, eating behaviour and common determinants of body weight. Diabetes Obes Metab 23: 17–35, 2021 [DOI] [PubMed] [Google Scholar]
- 5.Garibotto G, Picciotto D, Saio M, Esposito P, Verzola D: Muscle protein turnover and low-protein diets in patients with chronic kidney disease. Nephrol Dial Transplant 35: 741–751, 2020 [DOI] [PubMed] [Google Scholar]
- 6.Wang AY, Kalantar-Zadeh K, Fouque D, Wee PT, Kovesdy CP, Price SR, Kopple JD: Precision medicine for nutritional management in end-stage kidney disease and transition to dialysis. Semin Nephrol 38: 383–396, 2018 [DOI] [PubMed] [Google Scholar]
- 7.Stenvinkel P, Zoccali C, Ikizler TA: Obesity in CKD--What should nephrologists know? J Am Soc Nephrol 24: 1727–1736, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ikizler TA: Nutrition support for the chronically wasted or acutely catabolic chronic kidney disease patient. Semin Nephrol 29: 75–84, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]