To the Editor
Since it was first identified as a novel viral strain in late 2019, SARS-CoV-2 (COVID-19) has infected over 38 million Americans and claimed the lives of over 600,000.1 The Centers for Disease Control and Prevention (CDC) closely monitors the evolving landscape of COVID-19 and tracks various metrics in each U.S. County and State. Examination of this data has revealed heterogeneity in COVID-19 burden, testing and vaccination rates.2 It is important to identify communities that are particularly susceptible to the effects of COVID-19 in order to adequately prepare for any contingencies and to design measures to counteract them.
The CDC has developed the social vulnerability index (SVI) as a tool that public health officials can use to identify communities that may be at high risk for hazardous events such as disease outbreak and natural disasters.3 However, few studies have evaluated whether the SVI is associated with COVID-19 cases and deaths and also counteractive measures including testing and vaccinations.
We abstracted SVI data from the CDC Agency for Toxic Substances and Disease Registry (ATSDR), which outlines every US census tract on 15 social factors using the American Community Survey (ACS) data.4 These social attributes are further grouped into 4 related themes: socioeconomic status (below poverty, unemployed, income, and no high school diploma); household composition and disability (age ≥ 65 years, age ≤ 17 years, age > 5 years with a disability, and single-parent households), minority status and language (minority and individual speak English “less than well”), and housing type and transportation (multi-unit structure, mobile home, crowding, no vehicle, and group quarters) and ranked according to percentiles. These four percentiles are summed, and the census tracts are sorted again to calculate an overall percentile ranking for each census tract. High SVI corresponds to more unfavorable metrics related to the four themes mentioned above. To derive state-level SVI percentiles, census tracts within each state were ranked against one another. Data on COVID-19 was obtained from the CDC COVID Data Tracker (data accessed on 8/19/2021) and presented per 100,000 people to facilitate comparisons between U.S. states.1
COVID-19 cases, deaths, vaccinations, and testing were summarized by tertiles of SVI, presented as means (standard deviation), and compared using ANOVA testing. Pearson's correlation coefficient and linear regression analysis was used to study the relationship between SVI and each COVID-19 measure. All analyses were conducted using Stata version 16.1 (StataCorp, College Station, Texas). Graphs were created using Excel version 16.41. A p-value <0.05 was considered to be statistically significant.
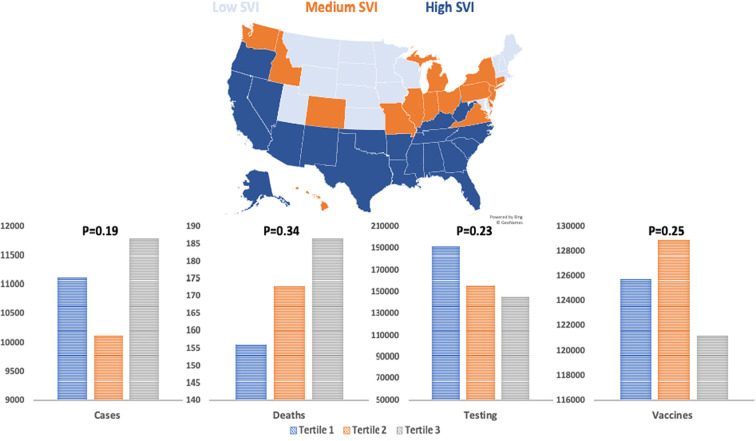
Compared to the first tertile of SVI, U.S. states in the third tertile had higher COVID-19 cases (mean [standard deviation]) (11,799 [2207] versus 11,115 [3278]; p = 0.19) and deaths (187 [55] versus 156 [66]; p = 0.34) but lower number of COVID-19 tests (145,313 [79,277] versus 191,981 [91,835]; p = 0.23) and vaccines administered (121,272 [12,866] versus 125,735 [20,465]; p = 0.25) (Fig. 1 ). There was a positive correlation between SVI and COVID-19 cases and deaths (r = 0.18 [p = 0.21] and 0.25 [p = 0.07], respectively) and a negative correlation with testing and vaccines (r = −0.33 [p = 0.03] and − 0.19 [p = 0.17], respectively). In regression analyses, there was a significant association between 1-unit higher SVI and COVID-19 tests performed [B coefficient − 109,999 95% confidence interval (−206,560, −13,438; p = 0.03, adjusted R2 = 0.09). There was no significant association with other COVID-19 measures.
Fig. 1.
Distribution of social vulnerability index across U.S. states and average number of COVID-19 cases, deaths, tests, and vaccinations (per 100,000) according to social vulnerability index tertiles.
The present analysis found that the SVI might be associated with number of COVID-19 infections and deaths but inversely associated with number of tests and vaccinations performed though the strength of this association appears to be modest. The SVI is a holistic measure that encompasses multiple facets related to social determinants of health. The variables comprising the SVI provide both a biologic basis for COVID-19 transmission rates (more vulnerable age groups, living in overcrowded households) and a social basis (lack of access to health care, systemic racism, medical literacy, poor public health policies), which suggests the mechanisms for the observed results in our study.
COVID-19 has exacerbated already existing disparities in access to medical care and disease outcomes. Minority racial groups are disproportionately affected by COVID-19.5 These same groups may also be more hesitant to get vaccinated.6, 7 Furthermore, U.S. states have differed in their preparedness for COVID-19 hospitalizations and deaths. The SVI could potentially be used to mitigate such disparities through advanced preparedness (public health education on testing and vaccination including the upcoming booster shots) and planning by allocating resources to communities that are already at high risk according to SVI metrics.
In summary, we believe the SVI is a valuable tool that can be used for resource allocation and health policy design to combat the ongoing COVID-19 pandemic. Our results emphasize the importance of advanced strategic planning so that the healthcare system and workers are not overwhelmed in states with higher social vulnerability.
Declaration of Competing Interest
Salim S. Virani.
Research support: Department of Veterans Affairs, World Heart Federation, Tahir and Jooma Family.
Honorarium: American College of Cardiology (Associate Editor for Innovations, acc.org).
The remaining coauthors report no relevant conflicts of interest.
References
- 1.Centers for Disease Control and Prevention COVID Data Tracker. United States COVID-19 Cases and Deaths by State. https://covid.cdc.gov/covid-data-tracker/#datatracker-home Published 2021.
- 2.Reitsma Marissa, Artiga Samantha, Goldhaber-Fiebert Jeremy, et al. Disparities in Reaching COVID-19 Vaccination Benchmarks: Projected Vaccination Rates by Race/Ethnicity as of July 4. https://www.kff.org/racial-equity-and-health-policy/issue-brief/disparities-in-reaching-covid-19-vaccination-benchmarks-projected-vaccination-rates-by-race-ethnicity-as-of-july-4/ Published 2021. [DOI] [PMC free article] [PubMed]
- 3.Flanagan B.E., Hallisey E.J., Adams E., Lavery A. Measuring community vulnerability to natural and anthropogenic hazards: the Centers for Disease Control and Prevention’s social vulnerability index. J Environ Health. 2018;80(10):34–36. https://pubmed.ncbi.nlm.nih.gov/32327766 [PMC free article] [PubMed] [Google Scholar]
- 4.CDC/ATSDR Social Vulnerability Index https://www.atsdr.cdc.gov/%0D%0Aplaceandhealth/svi/index.html%0D%0A Accessed June 12, 2020.
- 5.Gross C.P., Essien U.R., Pasha S., Gross J.R., Wang S., Nunez-Smith M. Racial and ethnic disparities in population level covid-19 mortality. medRxiv. 2020 doi: 10.1101/2020.05.07.20094250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lu D., Qiao Y., Brown N.E., Wang J. Racial and ethnic disparities in influenza vaccination among adults with chronic medical conditions vary by age in the United States. PLoS One. 2017;12(1) doi: 10.1371/journal.pone.0169679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hall L.L., Xu L., Mahmud S.M., Puckrein G.A., Thommes E.W., Chit A. A map of racial and ethnic disparities in influenza vaccine uptake in the Medicare fee-for-service program. Adv Ther. 2020;37(5):2224–2235. doi: 10.1007/s12325-020-01324-y. [DOI] [PMC free article] [PubMed] [Google Scholar]