Laminin-521 as a Novel Target in Anti-GBM Disease
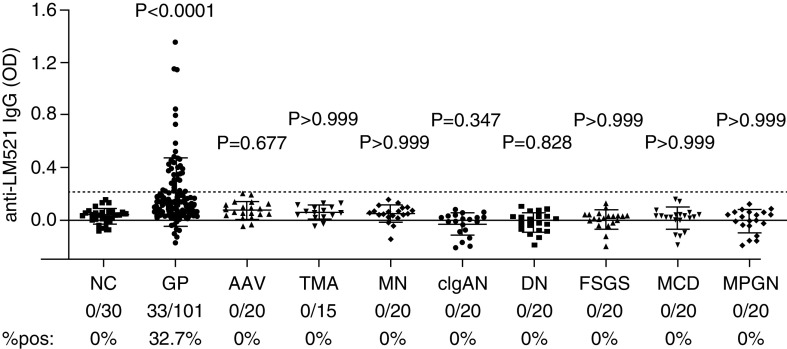
Antiglomerular basement membrane (anti-GBM) disease clinically presents as rapidly progressive glomerulonephritis, often accompanied by pulmonary hemorrhage. The autoantibodies that mediate the disease typically recognize cryptic epitopes within a345(IV) collagen in the glomerular and alveolar basement membranes. In a retrospective study of circulating autoantibodies from 101 patients with anti-GBM/Goodpasture's disease and 85 controls, Shen et al. detected autoantibodies to laminin-521, another major autoantigen in anti-GBM disease, in 51.5% of patients with both kidney and lung involvement versus 23.5% of patients with isolated kidney disease. Seropositivity for antilaminin autoantibodies was significantly associated with lung hemorrhage, hemoptysis, and smoking. These autoantibodies may contribute to lung injury in anti-GBM disease by increasing the amount of IgG bound to the alveolar basement membrane. See Shen et al., pages 1887–1897.
Iron Biomarkers and Mortality in Nondialysis Kidney Disease
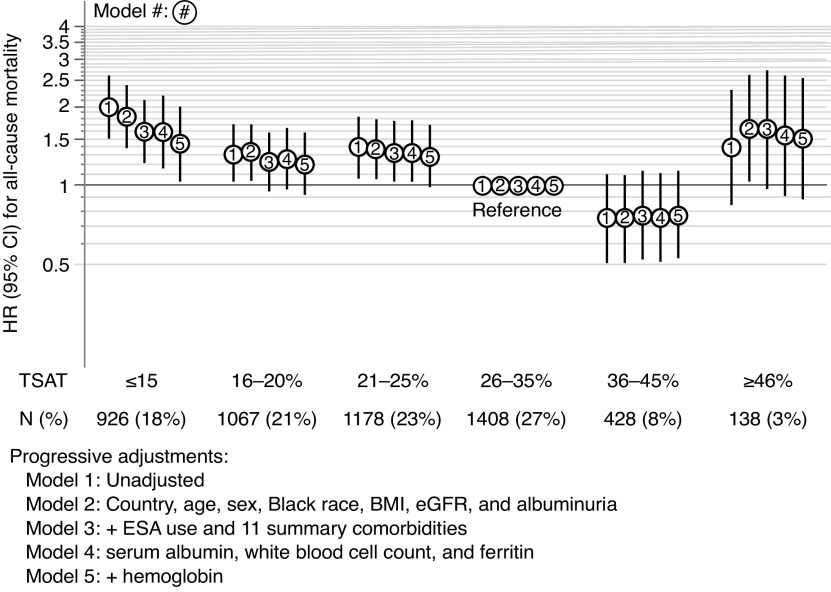
Managing iron deficiency in patients with nondialysis CKD focuses on improving erythropoiesis. Studies in heart failure patients with iron deficiency found that treating iron deficiency improves cardiovascular outcomes regardless of anemia. To evaluate a possible anemia-independent association of iron stores with outcomes, the authors studied patients with nondialysis CKD in nephrology-based clinics from a multinational cohort. They show that iron deficiency, as reflected by the transferrin saturation index, associates with higher risk of mortality and cardiovascular events in CKD patients with or without anemia. Intervention studies of the effects of treating iron deficiency beyond effects on erythropoiesis are needed to test the current anemia-focused paradigm of iron deficiency management in nondialysis CKD and to develop better strategies for improving outcomes. See Guedes et al., pages 2020–2030.
Disparities among Hemodialysis Patients with COVID-19
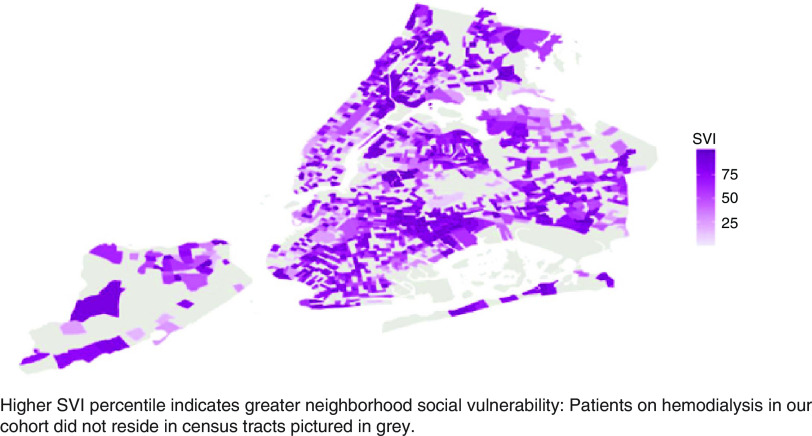
COVID-19 has disproportionately affected socially disadvantaged populations. Whether racial/ethnic and socioeconomic disparities in COVID-19 incidence exist in the hemodialysis population is unknown. The authors examined the association of race/ethnicity and a validated neighborhood-level index of social vulnerability (the Social Vulnerability Index) with acquiring symptomatic COVID-19 among patients receiving in-center hemodialysis from a New York City dialysis organization. They found substantial racial/ethnic disparities in COVID-19 incidence, with Black and Hispanic patients on hemodialysis more likely than non-Hispanic White patients to acquire COVID-19. Neighborhood-level socioeconomic status, minority status and language, and housing crowding were positively associated with COVID-19 acquisition among non-Hispanic white patients but did not explain racial/ethnic disparities. These findings indicate that targeted strategies are needed to mitigate excess COVID-19 risk among socially vulnerable patients on dialysis. See Tummalapalli et al., pages 2048–2056.