Abstract
COVID-19 does not leave behind refugees. They are disproportionately affected during the current pandemic. The present study aimed to investigate the psychological impacts of COVID-19 related stressors -resource loss and perceived discrimination during the COVID-19 pandemic- on Syrian refugees in Turkey. Further, the buffering role of perceived social support against the detrimental impacts of such stressors was examined.
An online cross-sectional study was conducted between September-October 2020. A sample of 345 Syrian refugees in Turkey completed the questions about demographic characteristics, resource loss and perceived discrimination during the pandemic, perceived social support, and depressive and anxiety symptoms. A high level of depressive and anxiety symptoms was reported in our sample. Resource loss and perceived discrimination during the pandemic significantly and positively predicted depressive and anxiety symptoms. Perceived social support acted as a buffer against the detrimental effect of resource loss on mental health. For those with higher perceived social support, resource loss during the pandemic did not significantly predict depressive and anxiety symptoms. The results indicate the detrimental role of COVID-19 related stressors on refugee mental health. Social support is an important protective factor for mental health amidst the pandemic. Our findings highlight the importance of considering the precarious conditions of refugees in all COVID-19 responses and communications.
Keywords: COVID-19, Refugees, Mental health, Resource loss, Discrimination, Social support
Introduction
As of 31 March 2021, nearly 130 million have been infected with and 3 million died due to the novel coronavirus SARS-CoV-2 (COVID-19) globally (World Health Organization, 2021). To curb the spread of COVID-19, all countries have taken certain measures such as imposing travel restrictions and lockdowns which caused profound changes in our lives (Bavel et al., 2020). Considering the difficulty in controlling the spread of the virus, the United Nations’ pledge of leaving no one behind to achieve sustainable development goals could not be more vital for global health because COVID-19 does not leave behind the most vulnerable groups including refugees (Lancet, 2020; United Nations Sustainable Development Group, 2019).
According to the UN High Commissioner for Refugees, there are 26 million refugees who fled from their countries due to conflict, violence, and persecution (United Nations High Commissioner for Refugees, 2020a). Among them, approximately 6 million are Syrians who sought refuge in neighboring and Western countries. Currently, Turkey hosts the largest number of refugees with 3.6 million Syrians (United Nations High Commissioner for Refugees, 2020b). Refugees are especially at great risk of infection and mortality during the pandemic (Kluge, Jakab, Bartovic, d’Anna, & Severoni, 2020) because they mostly live in low- and middle-income countries with limited social and economic resources (United Nations High Commissioner for Refugees, 2020a). In such countries, COVID-19 puts an extra burden on already insufficient health care and economic infrastructure (Fouad, McCall, Ayoub, Abu-Raddad, & Mumtaz, 2021; Lancet, 2020). Further, refugees are exposed to potentially traumatic events such as torture, injury, and captivation before arriving to host countries (Steel et al., 2009), all of which might affect person’s physical and mental health leaving the person more vulnerable to disease. Once settled in, they also encounter ongoing displacement-related stressors such as impoverishment, social isolation, and discrimination (Miller & Rasmussen, 2010, 2017). Due to traumatic events and displacement-related stressors, refugees are at higher risk of having mental health problems than the general population (Porter & Haslam, 2005). The recent estimates of WHO for depression, PTSD, and anxiety are 10.8 %, 15.3 %, and 21.7 % among conflict-affected populations including refugees (Charlson et al., 2019). Unfortunately, COVID-19 poses another daunting challenge for refugees (Rees & Fisher, 2020). Most of them live in precarious conditions such as overcrowded camps or shared houses which makes compliance to COVID-19 precautions (e.g., social distancing, hygiene, etc.) hardly possible (Kluge et al., 2020). Refugees also face serious economic hardships such as losing their job and income and legal barriers such as problems in issuance or renewal of residency status (Brickhill-Atkinson & Hauck, 2021). They have limited access to necessary information and health care services related to COVID-19 (Júnior et al., 2020). Although refugees are less likely to transmit communicable diseases to host communities (World Health Organization, 2018), they might become the target of discrimination and stigmatization during the current pandemic (Alemi, Stempel, Siddiq, & Kim, 2020). Taken together, it is imperative to assume that COVID-19 both exacerbates the risk of mental health problems and worsens the existing ones among refugees.
There are a limited number of studies investigating the psychological impacts of COVID-19 on refugee populations. Among them, a qualitative study with refugees in Uganda showed that COVID-19 brought significant changes in social and work life. It was also associated with fear, panic, and feeling of helplessness (Logie et al., 2021). In a longitudinal study with Yazidi refugees in Iraq, Kizilhan and Noll-Hussong (2020) showed that the prevalence of post-traumatic stress disorder (PTSD), depressive and anxiety disorders significantly increased during the COVID-19 compared to before the COVID-19 period. In another study, COVID-19 related traumatic stress predicted both the symptoms of PTSD and depression and deficits in working memory and inhibitory control among Syrian refugees in Turkey (Kira et al., 2021). Furthermore, given the limitation in making inferences for the general population, a study among hemodialysis patients showed that Syrian refugees had higher depressive symptoms than host community participants during the COVID-19 pandemic (Sevinc et al., 2021).
Although the aforementioned studies inform us about the adverse impacts of COVID-19 on mental health among refugees, they did not comprehensively examine the relationship between the stressors caused by COVID-19 and mental health. Since refugees are among the most vulnerable groups during the pandemic, there is an urgent need to uncover the impacts of COVID-19 related stressors on their mental health and identify the most important stressors for targeted interventions. Therefore, in the present study, we aimed to investigate the role of resource loss and perceived discrimination during COVID-19 on the mental health of Syrian refugees in Turkey.
According to the Conservation of Resources Theory (Hobfoll, 1989, 2001), there are different types of resources such as personal, social, and material which are fundamental for wellbeing and optimal human functioning. Psychological distress occurs if such resources are lost or are threatened to be lost. Several studies showed that in response to the events or circumstances leading to loss of resources or threatening resources, individuals are likely to report higher symptoms of PTSD, depression, and anxiety (Hobfoll, Tracy, & Galea, 2006; Hou, Law, Yin, & Fu, 2010; Zwiebach, Rhodes, & Roemer, 2010) and lower well-being (Topa, Jiménez, Valero, & Ovejero, 2017). Having acknowledged the personal, social, and material repercussions (Bavel et al., 2020), COVID-19 can be considered as a risk factor for resource loss and thereby mental health. Current findings corroborate this by showing that refugees in Turkey face loss of their already limited resources such as job, income, and obtaining basic needs during the pandemic (Ustubici & Karadag, 2020). Therefore, we hypothesized that COVID-19 related resource loss would predict higher psychological distress -higher level of depressive and anxiety symptoms- among Syrian refugees in Turkey.
In addition to resource loss during the pandemic, stigmatization and discrimination towards refugees and immigrants are rather alarming (Alemi et al., 2020). A large body of research shows that perceived discrimination is detrimental for both mental and physical health (Panza et al., 2019; Schmitt, Postmes, Branscombe, & Garcia, 2014 for reviews). Similar findings were obtained about perceived discrimination among refugees and immigrants during the pandemic too. A study conducted with Asian originated refugees in the United States showed that one-third of the participants experienced at least one type of discrimination during the pandemic such as feeling that other people were afraid of them and as if they had been treated with less respect than others. Experiencing discrimination was associated with increased stress (Zhang, Gurung, Anglewicz, Baniya, & Yun, 2021). In a similar vein, Asian immigrants reported higher discrimination which was related to higher depressive symptoms and lower life satisfaction (Litam & Oh, 2020). Although the existing studies might point out racial discrimination due to erroneously blaming Asians for spreading the coronavirus (Zhang et al., 2021), discrimination towards other refugee and immigrant groups are also likely to happen amidst the current pandemic. Behavioral immune system theory suggests that pathogenic threats active a set of behavioral and psychological mechanisms to avoid diseases (Schaller & Park, 2011). Activation of such mechanisms results in ingroup favoritism (Murray & Schaller, 2012; Navarrete & Fessler, 2006) and negative attitudes and behaviors towards outgroup members including immigrants (Faulkner, Schaller, Park, & Duncan, 2004). Given that COVID-19 is a serious pathogenic threat, it is not unexpected to see that discrimination towards refugees and immigrants increases and adversely affects mental health. Therefore, we hypothesized that perceived discrimination during the COVID-19 would predict higher psychological distress among Syrian refugees in Turkey.
Due to the high prevalence of mental health problems among refugees, the extant studies tend to focus on the identification of risk factors. However, it is crucial to be cognizant that many do not develop mental health problems. Refugees are, in fact, resilient referring to either being shielded against the adversities or finding equilibrium more rapidly despite the challenges (Bonanno, 2004). Thus, to facilitate the adjustment of refugees, it is of critical importance to investigate resilience promoting factors. According to the socio-ecological model of resilience, resilience is conceptualized as a dynamic and multifaceted process through which individuals restore or maintain psychological well-being to the extent that they access psychological, social, cultural, and physical resources. Compared to traditional person-centered conceptualizations, the socio-ecological model defines resilience as the interplay between personal and contextual characteristics rather than a solely personal trait (Ungar, 2008, 2011). A growing number of studies show the utility of this model to elucidate the refugee resilience process (e.g., Schlechter et al., 2021; von Haumeder, Ghafoori, & Retailleau, 2019; Spatrisano, Robinson, Eldridge, & Rosich, 2020). Among many resilience promoting factors, social support appears to be among the most important ones for refugee mental health (Wachter et al., 2021). According to the stress-buffering model (Cohen & Wills, 1985), social support provides necessary social resources such as instrumental support, practical support, and companionship to individuals to cope with the stressors so that they become protected against the detrimental effects of stressful life events. Two distinct mechanisms are suggested to delineate the process behind this protection or buffering effect. One is via alleviating stress appraisal response whereby individuals perceive the stressful situation more benign and feel capable of coping with it. The other is via reducing stress reaction so that individuals become physiologically and psychologically less reactive to stressful situations (Cohen & Wills, 1985). Since social support is conducive to the acquisition of other resources such as material goods, information, and guidance, it can be considered as one of the key facilitative factors of well-being in the resilience process of refugees (Spatrisano et al., 2020). A systematic review (Siriwardhana, Ali, Roberts, & Stewart, 2014) indicated that social support was an important protective factor against psychological distress. It was associated with increased resilience and lower symptoms of PTSD, depression, and anxiety among conflict-affected populations including refugees. In a more recent systematic review among refugees and asylum seekers, it was found that social support from family, friends, organizations, and the local community was conducive to well-being (Posselt, Eaton, Ferguson, Keegan, & Procter, 2019). Considering resilience among refugees, we investigated whether social support act as a buffer against psychological distress during the pandemic, especially given restrictions that the pandemic has imposed on peoples’ social lives. We assumed that social support would moderate the relationship between resource loss and perceived discrimination during the pandemic and psychological distress, such that resource loss and perceived discrimination would positively predict depressive and anxiety symptoms if social support is low.
Method
Participants and procedure
The current sample consisted of 345 participants (165 female, 180 male) with an average age of 33.40 (SD = 9.11). Participants were mostly university (45 %) or high school graduates (24 %). Most of the participants were married (74 %) and under temporary protection status (75 %). The average length of stay in Turkey was 6.5 years (SD = 1.19). Over half of the participants (54 %) were unemployed. 25 % were working from office while 10 % were working from home. The majority of the participants’ monthly household income (73 %) was between 185 US dollars to 615 US dollars.
Almost one-third of the participants (27 %) had chronic diseases such as respiratory illnesses and high blood pressure. 8% reported having a previously diagnosed psychiatric problem. 30 % were smokers. 18 % received financial or in-kind support from several organizations due to COVID-19. More than half of the participants adhered to the COVID-19 measures imposed by the government (58 %) and followed the news about COVID-19 (63 %). 14 % had been infected with COVID-19. 43 % knew someone infected with COVID-19 and 34 % lost someone due to COVID-19 (mainly friends, neighbors, and second-degree relatives), which indicated a high rate of exposure to COVID related stress and loss in their community.
An online cross-sectional study which was reviewed and approved by the university’s ethics committees (2020.200.IRB3.080) was conducted between September and October 2020. Participants were recruited through social media advertisements on Facebook. In the advertisements, we specified the following inclusion criteria for the participation: 1) being 18 years or older, 2) migrating to Turkey due to the ongoing conflict in Syria since 2011, 3) being literate in the Arabic language. Those who did not meet these criteria were excluded from the study. They were asked to answer a series of questions about demographic characteristics, COVID-19 related factors, resource loss, perceived discrimination, social support, anxiety, and depressive symptoms, respectively. Only those who migrated to Turkey due to the conflict in Syria were included in the study. Completion of the survey took approximately 20 min. To compensate for their time and effort, each participant was given an equal chance to win a grocery check of 6 US dollars upon their completion of the study.
Measures
The conservation of resources evaluation (modified version)
Resource loss during the COVID-19 pandemic was assessed by the modified version of The Conservation of Resources Evaluation (COR-Evaluation) (Hobfoll & Lilly, 1993). Participants were asked to indicate the resource loss since the start of COVID-19. It has 15 items (e.g., personal health, stable employment, adequate food, and hope) rated on a 3-point Likert scale (0 = no decrease, 2 = decreased a lot). Higher scores indicate higher resource loss since the start of COVID-19. The scale was translated from English into Arabic and then back-translated into English by bilingual speakers. The Cronbach’s alpha was 0.81 in the present study.
Everyday discrimination scale (short version)
Perceived discrimination during the COVID-19 pandemic was assessed by the Everyday Discrimination Scale-Short version (Sternthal, Slopen, & Williams, 2011) which includes 5 items rated on a 5-point Likert scale (1 = never, 5 = always). Items were re-worded to refer to the discrimination experiences since the outbreak (e.g., “People act as if they are afraid of you since coronavirus outbreak”). It was previously used with Syrian refugees in Turkey (Çelebi, Verkuyten, & Bagci, 2017). Higher scores indicate higher perceived discrimination since the COVID-19 outbreak. In the present study, Cronbach’s alpha of 0.84 was reported.
Multidimensional scale of perceived social support (MSPSS)
The multidimensional scale of perceived social support (MSPSS) was used to assess perceived social support from different sources (family, friends, and significant others) (Zimet, Dahlem, Zimet, & Farley, 1988). It was previously used in the Arabic population (Dambi et al., 2018). It has 12 items rated on a 7-point Likert scale ranging from 1 (very strongly disagree) to 7 (very strongly agree). Higher scores indicate higher perceived social support. The internal consistency was 0.90 in the present study.
Patient health questionnaire-9 (PHQ-9)
The Patient Health Questionnaire-9 (PHQ-9) was used to assess depressive symptoms (Kroenke, Spitzer, & Williams, 2001). 9 items (e.g., little interest or pleasure in doing things, feeling down, depressed, or hopeless) are rated on a 4-point Likert scale (0 = not at all, 3 = nearly every day). Higher scores indicate a higher level of depressive symptoms. The severity of the symptoms is determined based on the following criteria: a total score of 0–4 no depressive symptoms, 5–9 mild depressive symptoms, 10–14 moderate depressive symptoms, 15–19 moderate to severe depressive symptoms, and 20–27 severe depressive symptoms. A total of score 10 and above is considered probable depression (Kroenke, Spitzer, Williams, & Löwe, 2010). The Arabic version of the scale has been validated (Sawaya, Atoui, Hamadeh, Zeinoun, & Nahas, 2016) and widely used in conflict-affected populations including Syrians (Georgiadou, Zbidat, Schmitt, & Erim, 2018; Nesterko, Jäckle, Friedrich, Holzapfel, & Glaesmer, 2019). The Cronbach’s alpha was 0.91 in the present study.
Generalized anxiety scale (GAD-7)
To assess anxiety symptoms, the Generalized Anxiety Scale (GAD-7) was used (Spitzer, Kroenke, Williams, & Löwe, 2006). It has 7 items (e.g., feeling nervous, anxious or on edge, worry too much about different things) rated on a 4-point Likert scale (0 = not at all, 3 = nearly every day). Higher scores indicate higher anxiety symptoms. A total score of 5, 10, and 15 represent the mild, moderate, and severe level of anxiety, respectively. Scoring 10 and above is considered as having a probable generalized anxiety disorder (Kroenke et al., 2010). The Arabic version of the scale with good psychometric properties is available (Sawaya et al., 2016). The scale has been used in conflict-affected populations including Syrians as well (Georgiadou et al., 2018). In the present study, Cronbach’s alpha was 0.91.
Data analysis
The normality assumptions for each construct were tested by using skewness (|3|) and kurtosis (|8|) criteria (Kline, 2015). Preliminary analyses were conducted in SPSS Version 26. To estimate the parameters for the hypothesized relationships, path analysis with maximum likelihood estimator in the context of structural equation modeling was conducted in Mplus 8.5 (Muthén & Muthén, 1998–2021). Compared to multiple regression, path analysis takes into account variances and covariances of variables and thereby provide us with more accurate estimations for the hypothesized relationships between the variables. Therefore, this approach allows us to capture and test the complexity of the hypothesized model especially when there are several predictor and outcome variables in the model (Kline, 2015).The missing data were accounted for by using full information maximum likelihood estimation with robust standard errors (FIML) to prevent sample size reduction, thereby loss of power (Enders, 2010). In the model, age, sex (coded as 0 = male, 1 = female), education (0 = below bachelors’ degree, 1 = bachelors’ degree and above), marital status (dummy coded as 0 = unmarried, 1 = married), employment (dummy coded as 0 = unemployed, 1 = employed), and income (dummy coded as 0 = 240 US dollar and below, 1 = above 240 dollars) were considered as covariates. Nonsignificant paths were removed one at a time to preserve model parsimony (Wang & Wang, 2012). All the variables were centered to prevent multicollinearity before hypothesis testing. To test the moderating role of social support, interaction terms (social support*resource loss and social support*perceived discrimination) were computed (Aiken, West, & Reno, 1991). The moderating role of social support was inspected at -1 SD and +1 SD values of social support. Standardized path coefficients were reported.
Results
Preliminary analyses
Little’ MCAR test suggested that the data were missing at random (χ2/df = 1.38, p = .190) with the ratio of missingness of focal variables ranging from 0 % to 15 %. Bivariate correlations and descriptive statistics were presented in Table 1 . Depressive and anxiety symptoms were positively correlated with resource loss and perceived discrimination, but negatively correlated with education and social support. Age was positively associated with social support. Income was negatively correlated with anxiety symptoms. Of the participants, 52.9 % and 42.9 % scored above the cut-off value of probable depression and anxiety, respectively.
Table 1.
Descriptive statistics and bivariate correlations among study variables.
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 |
|---|---|---|---|---|---|---|---|---|---|---|---|
|
– | ||||||||||
|
.758** | – | |||||||||
|
.221** | .165** | – | ||||||||
|
.301** | .286** | .125* | – | |||||||
|
−.277** | −.247** | −.111* | −.089 | – | ||||||
|
−.029 | −.033 | .086 | −.111 | .136* | – | |||||
|
−.043 | −.066 | −.100 | −.095 | .018 | −.108 | – | ||||
|
−.169** | −.153** | .047 | −.042 | .116* | .087 | −.130 | – | |||
|
−.036 | .036 | .059 | .006 | .128* | .390** | −.058 | .068 | – | ||
|
−.191** | −.176** | −.065 | −.109 | .073 | .055 | −.235** | −.232** | −.069 | – | |
|
−.077 | −.143** | .106 | −.060 | .187** | .142* | −.074 | −.301** | −.001 | .169** | – |
| N | 344 | 343 | 345 | 293 | 332 | 273 | |||||
| M | 1.24 | 1.37 | 1.56 | 2.05 | 4.39 | 33.40 | |||||
| SD | .78 | .87 | .33 | .86 | 1.30 | 9.11 | |||||
| Range | 0−3 | 0−3 | .33−2 | 1−5 | 1−7 | 18−69 | |||||
| Skewness | .506 | .390 | −1.07 | 1.09 | −.377 | .541 | |||||
| Kurtosis | −.588 | −.842 | 1.13 | 1.43 | −.502 | .336 |
Note: *p < .05, **p < .001.
Hypothesis testing
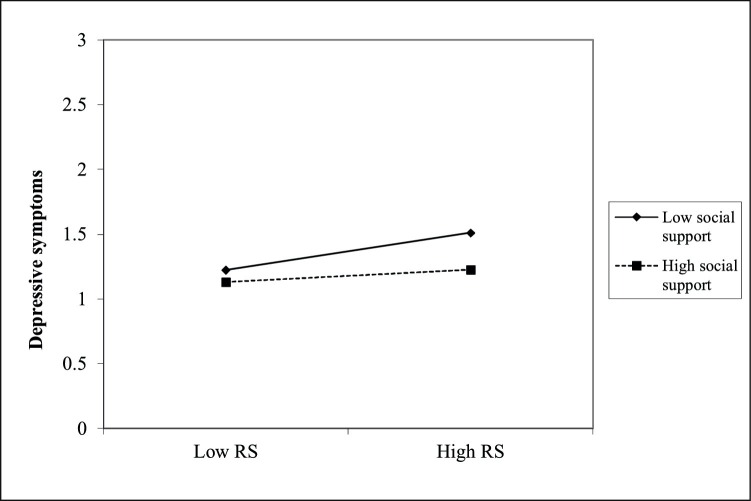
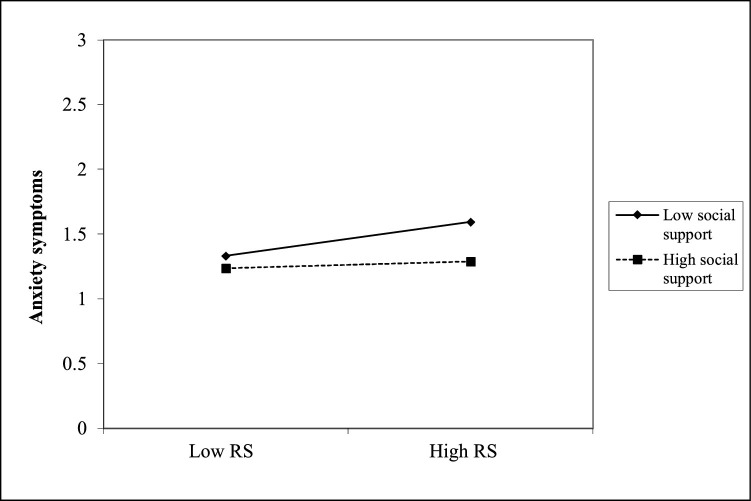
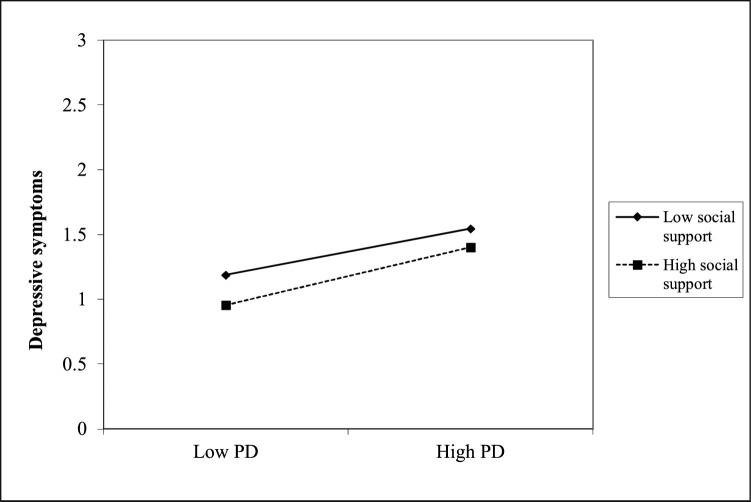
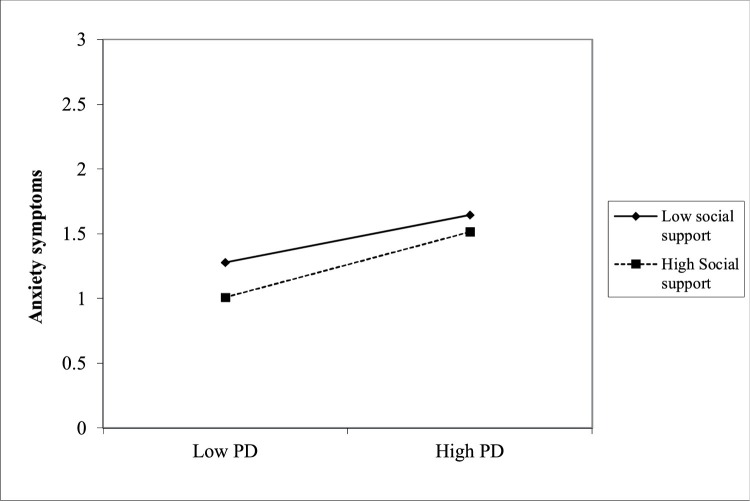
The results showed that resource loss and perceived discrimination during the COVID-19 significantly and positively predicted both depressive (β = .179, p < .01, β = .223, p < .001) and anxiety symptoms (β = .151, p < .01, β = .211, p < .001). On the other hand, social support significantly and negatively predicted depressive (β = -0.233, p < .001) and anxiety symptoms (β = -0.231, p < .001). The interaction between social support and resource loss was significant both for depressive (β = -0.119, p < .05) and anxiety symptoms (β = -0.121, p < .05). When social support was low (-1 SD below the mean), resource loss significantly predicted both depressive (β = .298, p < .001, [95 % CI: .151, .446]) and anxiety symptoms (β = .272, p < .001, [95 % CI: .122, .422]). However, when social support was high (1 SD above the mean), the effect of resource loss on those symptoms was not significant (β = .060, p = .405 for depressive symptoms, β = .031, p = .677 for anxiety symptoms). On the other hand, the interaction between social support and perceived discrimination was not significant either for depressive (β = .056, p = .257) or anxiety symptoms (β = .080, p = .111) (see Table 2 for all path coefficients and Fig. 1, Fig. 2, Fig. 3, Fig. 4 for interaction effects).
Table 2.
Standardized path coefficients.
| 95 % CI |
|||
|---|---|---|---|
| β (SE) | LLCI | ULCI | |
| Paths | |||
| RS → DEP | .179** (.053) | .076 | .283 |
| RS → ANX | .151** (.054) | .046 | .257 |
| PD → DEP | .223*** (.053) | .119 | .327 |
| PD → ANX | .211*** (.054) | .105 | .317 |
| SS → DEP | −.233*** (.052) | −.336 | −.131 |
| SS → ANX | −.231*** (.053) | −.336 | −.127 |
| INT1→ DEP | −.119* (.052) | −.220 | −.018 |
| INT1 → ANX | −.121* (.053) | −.223 | −.018 |
| INT2→ DEP | .056 (.049) | −.041 | .153 |
| INT2→ ANX | .080 (.050) | −.018 | .179 |
Note: * p < .05; ** p < .01; ***p < .001. RS: Resource loss during the COVID-19. PD: Perceived discrimination during the COVID-19. SS: Social support.
DEP: Depressive symptoms. ANX: Anxiety symptoms. INT1: Interaction term between resource loss and social support. INT2: Interaction term between perceived discrimination and social support.
LLCI: Lower-Level Confidence Interval. ULCI: Upper-Level Confidence Interval.
Fig. 1.
Interaction plot of resource loss with social support on depressive symptoms.
Fig. 2.
Interaction plot of resource loss with social support on anxiety symptoms.
Fig. 3.
Interaction plot of perceived discrimination with social support on depressive symptoms.
Fig. 4.
Interaction plot of perceived discrimination with social support on anxiety symptoms.
Discussion
In the present study, we investigated the relationship between COVID-19 related stressors and mental health among Syrian refugees in Turkey. We also examined the buffering role of social support against the detrimental impacts of such stressors. To the best of our knowledge, this is one of the very few studies examining the psychological impacts of COVID-19 on refugees as one of the most vulnerable groups. We found a high level of depressive and anxiety symptoms in our sample. Nearly half of the participants met the criteria for probable depression (52.9 %) and anxiety (42.9 %), which is higher than the previously reported prevalence rates among Syrian refugees in Turkey (Acarturk et al., 2018, 2021) and other hosting countries (Javanbakht et al., 2019; Poole, Hedt-Gauthier, Liao, Raymond, & Bärnighausen, 2018; Tinghög et al., 2017). Lower education level and unemployment were found to be risk factors to mental health problems as in the other studies (Porter & Haslam, 2005; von Haumeder et al., 2019).
The present results corroborated most of our initial assumptions. In line with the basic premises of COR theory (Hobfoll, 2001), we found that resource loss during the COVID-19 significantly predicted higher symptoms of depression and anxiety among Syrian refugees in Turkey. These results are congruent with the previous studies showing the adverse impacts of the loss of resources such as food, sleep, health, optimism, and sense of control on mental health among survivors of human-made and natural disasters, disadvantaged groups including refugees, and those going through significant changes in their lives (Betancourt et al., 2015; Hobfoll, Johnson, Ennis, & Jackson, 2003; Hobfoll, Tracy, & Galea, 2006; Smith & Freedy, 2000; Topa, Jiménez, Valero, & Ovejero, 2017; Zwiebach, Rhodes, & Roemer, 2010) . Yet, the present study goes well beyond the existing ones by showing that due to being actual cause of resource loss, COVID-19 seems to compound the existing vulnerabilities of refugees caused by conflict-related traumatic experiences and post-displacement related stressors and thereby deteriorates well-being. In a survey study investigating the impacts of COVID-19 on refugees across 48 cities in Turkey, it was found that more than half of the participants had difficulty in accessing basic needs such as food and hygienic materials. The majority were unemployed and unable to afford their rent and bills (Association for Solidarity with Asylum Seekers and Migrants (SGDD-ASAM) (2020)). Therefore, several humanitarian organizations expanded their work to respond to the precarious conditions of refugees during the pandemic in Turkey (United Nations High Commissioner for Refugees, 2020c). Nevertheless, their responses could not meet the excessive amount of need. In line with the vulnerability criteria applied by UNHCR, those organizations have to prioritize the most vulnerable groups (single parent, single woman, elderly, and LGBTI persons) while allocating their limited resources. Like other underserved populations with low resources, unfortunately, COVID-19 affects refugees disproportionally where they face an exceptional threat to their already insufficient resources. Since initial scarcity of resources precipitates further losses (Hobfoll, 2001), this situation calls an urgent attention. Due to the resource scarcity and current losses, disadvantaged groups like refugees might get in the trap of cycle of resource loss which makes their recovery from the aftermath of the pandemic more difficult. Thus, it becomes vital to intervene resource loss earlier.
We found a protective role for social support for refugee mental health amidst the pandemic. Higher perceived social support predicted a lower level of anxiety and depressive symptoms. Further, among those with lower perceived social support, resource loss during the pandemic significantly predicted psychological distress. On the other hand, for those with higher perceived social support, resource loss was not a significant predictor of psychological distress. Our results support the stress-buffering model asserting that social support immunizes individuals against the adverse impacts of stressful events (Cohen & Wills, 1985). Furthermore, as shown in the previous studies, social support is an indispensable resilience asset for mental health among refugees (Siriwardhana et al., 2014 for a review) including Syrians in Turkey and other countries (Böge, Karnouk, Hahn, Demir, & Bajbouj, 2020; Yildirim, Isik, Yildirim-Firat, & Aylaz, 2020). Having acknowledged the limited capacity and resources of organizations to provide necessary assistance for refugees, this finding is of paramount importance. Humanitarian organizations can consider either implementing psychosocial programs for refugees or including certain elements in their existing programs in a way that refugees can use and enhance their social support system. Furthermore, refugees might be encouraged to benefit from internet-mediated social support which is one of the most feasible options during the pandemic. Using online platforms can help refugees to maintain social relations and thereby promote mental health in the face of adversities (Mancini, Sibilla, Argiropoulos, Rossi, & Everri, 2019 for a review). However, the present findings should be interpreted with caution. As stated by the socio-ecological model of resilience, the process of and factors related to resilience are shaped by the social context (Ungar & Liebenberg, 2011). Both the availability and use of social support among refugees depends on the social, cultural, and political atmosphere of both the host and home country (Wachter et al., 2021). Therefore, strategies to promote social support during the pandemic should be carefully tailored according to the specific needs and conditions of the resettlement context of refugees.
Lastly, in line with the cumulative evidence for adverse impacts of perceived discrimination on physical and mental health (Panza et al., 2019; Schmitt et al., 2014), we found that perceived discrimination during the pandemic significantly predicted a higher level of depressive and anxiety symptoms among Syrian refugees in Turkey. To the best of our knowledge, this is one of the first studies to show the impact of discrimination during the pandemic on the mental health of non-Asian refugees. Previous studies found that Asian immigrants and refugees are likely to experience discrimination because they are erroneously blamed for the current pandemic (Litam & Oh, 2020; Zhang et al., 2021). However, our results espoused the behavioral immune system theory suggesting that pathogenic threat triggers negative behaviors and attitudes towards outgroup members (Schaller & Park, 2011). In a similar vein, a study among Italian participants found that COVID-19 threat and fear was associated with the lower sense of common belonging with disadvantaged groups such as addicts and immigrants as well as other nationalities such as Chinese, French, and Dutch (Fuochi, Boin, Voci, & Hewstone, 2021), which might increase prejudice and discrimination (Bavel et al., 2020). These findings offer several caveats about the psychological and social aftermath of the current pandemic. It is necessary to consider the lingering effects of COVID-19 on intergroup relations as well as individuals, especially in countries like Turkey which is one of the major refugee hosting countries. Negative attitudes and behaviors towards Syrian refugees have dramatically increased over years in Turkey (Erdogan, 2018; Erdogan, 2019). Considering that host society’ attitudes play a critical role in shaping refugees’ displacement related experiences (Hynie, 2018), COVID-19 poses another roadblock for refugee mental health and harmonious society. However, COVID-19 might offer a unique opportunity to create a sense of humanity and thereby active coordinated effort to combat the pandemic. In a study among Turkish participants, Adam-Troian and Bagci (2021) showed that perceived threat due to COVID-19 predicted positive attitudes towards Syrian refugees such as higher level of helping intention, positive attitudes, and pro-migration policy support. The relationship between COVID-19 related perceived threat and positive outgroup attitudes was explained by the common victimhood in the face of the current pandemic. These findings highlight the possibility of more inclusive intergroup relations during the COVID-19 pandemic caused by the perception of “togetherness” against the common threat. Therefore, to foster this perception, media and political leaders have a great responsibility in including all segments of society in their COVID-19 responses and persuading the public to perceive COVID-19 as a threat to the whole of humanity (Bavel et al., 2020).
Although the present study provides important insights about the psychological impacts of COVID-19 on refugees, it has several limitations. First of all, participants were recruited via social media advertisements. Since we conducted this study during the pandemic, face-to-face data collection was not a viable option. Yet, collecting data via social media might have been biased our sample in a way to include those with electronic devices (e.g., smartphones and tablets), social media accounts, and higher technology literacy. This limits our ability to draw a comprehensive conclusion about the conditions of Syrian refugees in Turkey. To test the validity of our findings, future studies should try to reach out to those who do not use social media as well. Secondly, it is a cross-sectional study that does not allow us to make causal inferences about the relationship between COVID-19 related stressors and mental health outcomes. Longitudinal studies focusing on the change in COVID-19 related stressors and psychological impacts are warranted. Such studies might be also informative to see long-term impacts of COVID-19 if they are extended to cover after the COVID-19 period. Thirdly, we included the measurements of depressive and anxiety symptoms as the indicators of mental health among refugees. Future studies might focus on different indicators such as well-being and quality of life. Lastly, we only focused on the mental health aspect of refugee experiences during COVID-19. Yet, the adaptation process of refugees might be also hindered during the current pandemic. The relationship between COVID-19 related stressors and the adaptation process requires further investigation.
Conclusion
Our findings show that COVID-19 related stressors -resource loss and perceived discrimination during the current pandemic- adversely impact the mental health of refugees. Social support might act as a buffer against mental health problems in response to resource loss during the pandemic. These findings support the notion that COVID-19 does not leave behind the refugees. In stark contrast, they are severely affected. It is important to acknowledge that there is no public health without refugee health. Therefore, in light of the current findings, humanitarian organizations and government bodies need to arrange their activities to best respond to the needs of refugees during the COVID-19 pandemic.
Funding
This study was funded by Scientific and Technological Research Council of Turkey (TUBITAK) under the project number of 120K440. The funding agency did not involve in research design, collection, analysis, and interpretation of data, writing of an article and decision to submit it for publication.
Declarations of interest
None.
References
- Acarturk C., Cetinkaya M., Senay I., Gulen B., Aker T., Hinton D. Prevalence and predictors of posttraumatic stress and depression symptoms among Syrian refugees in a refugee camp. The Journal of Nervous and Mental Disease. 2018;206(1):40–45. doi: 10.1097/NMD.0000000000000693. [DOI] [PubMed] [Google Scholar]
- Acarturk C., McGrath M., Roberts B., Ilkkursun Z., Cuijpers P., Sijbrandij M.…Fuhr D.C. Prevalence and predictors of common mental disorders among Syrian refugees in Istanbul, Turkey: A cross-sectional study. Social Psychiatry and Psychiatric Epidemiology. 2021;56(3):475–484. doi: 10.1007/s00127-020-01941-6. [DOI] [PubMed] [Google Scholar]
- Adam-Troian J., Bagci S.C. The pathogen paradox: Evidence that perceived COVID-19 threat is associated with both pro- and anti-immigrant attitudes. International Review of Social Psychology. 2021;34(1):1–15. doi: 10.5334/irsp.469. [DOI] [Google Scholar]
- Aiken L.S., West S.G., Reno R.R. California: Sage; Thousand Oaks: 1991. Multiple regression: Testing and interpreting interactions. [Google Scholar]
- Alemi Q., Stempel C., Siddiq H., Kim E. Refugees and covid-19: Achieving a comprehensive public health response. Bulletin of the World Health Organization. 2020;98(8) doi: 10.2471/BLT.20.271080. 510-510A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Association for Solidarity with Asylum Seekers and Migrants (SGDD-ASAM) 2021. COVID-19 salgınının Türkiye'deki mülteciler üzerindeki etkilerinin sektörel analizi. Retrieved from https://www.sivilsayfalar.org/wp-content/uploads/2020/05/asam_covid_anket_raporu_200518_2_TR-1.pdf. Accessed March 31. [Google Scholar]
- Bavel J.J.V., Baicker K., Boggio P.S., Capraro V., Cichocka A., Cikara M., Crockett M.J., Crum A.J., Douglas K.M., Druckman J.N., Drury J., Dube O., Ellemers N., Finkel E.J., Fowler J.H., Gelfand M., Han S., Haslam S.A., Jetten J.…Willer R. Using social and behavioural science to support COVID-19 pandemic response. Nature Human Behaviour. 2020;4(5):460–471. doi: 10.1038/s41562-020-0884-z. [DOI] [PubMed] [Google Scholar]
- Betancourt T.S., Abdi S., Ito B.S., Lilienthal G.M., Agalab N., Ellis H. We left one war and came to another: Resource loss, acculturative stress, and caregiver–child relationships in Somali refugee families. Cultural Diversity & Ethnic Minority Psychology. 2015;21(1):114. doi: 10.1037/a0037538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Böge K., Karnouk C., Hahn E., Demir Z., Bajbouj M. On perceived stress and social support: Depressive, anxiety and trauma-related symptoms in Arabic-speaking refugees in Jordan and Germany. Frontiers in Public Health. 2020;8 doi: 10.3389/fpubh.2020.00239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonanno G.A. Loss, trauma, and human resilience: Have we underestimated the human capacity to thrive after extremely aversive events? The American Psychologist. 2004;59(1):20–28. doi: 10.1037/0003-066X.59.1.20. [DOI] [PubMed] [Google Scholar]
- Brickhill-Atkinson M., Hauck F.R. Impact of COVID-19 on resettled refugees. Primary Care. 2021;48(1):57–66. doi: 10.1016/j.pop.2020.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Çelebi E., Verkuyten M., Bagci S.C. Ethnic identification, discrimination, and mental and physical health among Syrian refugees: The moderating role of identity needs. European Journal of Social Psychology. 2017;47(7):832–843. doi: 10.1002/ejsp.2299. [DOI] [Google Scholar]
- Charlson F., van Ommeren M., Flaxman A., Cornett J., Whiteford H., Saxena S. New WHO prevalence estimates of mental disorders in conflict settings: A systematic review and meta-analysis. The Lancet. 2019;394(10194):240–248. doi: 10.1016/S0140-6736(19)30934-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S., Wills T.A. Stress, social support, and the buffering hypothesis. Psychological Bulletin. 1985;98(2):310. doi: 10.1037/0033-2909.98.2.310. [DOI] [PubMed] [Google Scholar]
- Dambi J.M., Corten L., Chiwaridzo M., Jack H., Mlambo T., Jelsma J. A systematic review of the psychometric properties of the cross-cultural translations and adaptations of the Multidimensional Perceived Social Support Scale (MSPSS) Health and Quality of Life Outcomes. 2018;70(5):AB195. doi: 10.1016/j.jaad.2014.01.810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Enders C.K. Guilford Press; 2010. Applied missing data anlysis. [Google Scholar]
- Erdogan M.M. İstanbul Bilgi University Press; 2018. Suriyeliler Barometresi: Suriyelilerle Uyum İçinde Yaşamanın Çerçevesi. [Google Scholar]
- Erdogan M.M. 2019. Suriyeliler Barometresi 2019: Suriyelilerle Uyum İçinde Yaşamanın Çerçevesi.https://www.unhcr.org/tr/wp-content/uploads/sites/14/2020/09/SB2019-TR-04092020.pdf Retrieved from. [Google Scholar]
- Faulkner J., Schaller M., Park J.H., Duncan L.A. Evolved disease-avoidance mechanisms and contemporary xenophobic attitudes. Group Processes & Intergroup Relations. 2004;7(4):333–353. doi: 10.1177/1368430204046142. [DOI] [Google Scholar]
- Fouad F.M., McCall S.J., Ayoub H., Abu-Raddad L.J., Mumtaz G.R. Vulnerability of Syrian refugees in Lebanon to COVID-19: Quantitative insights. Conflict and Health. 2021;15(1):1–6. doi: 10.1186/s13031-021-00349-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuochi G., Boin J., Voci A., Hewstone M. COVID-19 threat and perceptions of common belonging with outgroups: The roles of prejudice-related individual differences and intergroup contact. Personality and Individual Differences. 2021;175(January):110700. doi: 10.1016/j.paid.2021.110700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Georgiadou E., Zbidat A., Schmitt G.M., Erim Y. Prevalence of mental distress among Syrian refugees with residence permission in Germany: A registry-based study. Frontiers in Psychiatry. 2018;9(AUG):1–12. doi: 10.3389/fpsyt.2018.00393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hobfoll S.E., Lilly R.S. Resource conservation as a strategy for community psychology. Journal of Community Psychology. 1993;21(2):128–148. doi: 10.1002/1520-6629(199304)21:2<128::AID-JCOP2290210206>3.0.CO;2-5. [DOI] [Google Scholar]
- Hobfoll S.E. Conservation of resources: A new attempt at conceptualizing stress. American Psychologist. 1989;44(3):513–524. doi: 10.1037/0003-066X.44.3.513. [DOI] [PubMed] [Google Scholar]
- Hobfoll S.E. The influence of culture, community, and the nested-self in the stress process: Advancing conservation of resources theory. Applied Psychology. 2001;50(3):337–421. doi: 10.1111/1464-0597.00062. [DOI] [Google Scholar]
- Hobfoll S.E., Johnson R.J., Ennis N., Jackson A.P. Resource loss, resource gain, and emotional outcomes among inner city women. Journal of Personality and Social Psychology. 2003;84(3):632–643. doi: 10.1037/0022-3514.84.3.632. [DOI] [PubMed] [Google Scholar]
- Hobfoll S.E., Tracy M., Galea S. The impact of resource loss and traumatic growth on probable PTSD and depression following terrorist attacks. Journal of Traumatic Stress. 2006;19(6):867–878. doi: 10.1002/jts. [DOI] [PubMed] [Google Scholar]
- Hou W.K., Law C.C., Yin J., Fu Y.T. Resource loss, resource gain, and psychological resilience and dysfunction following cancer diagnosis: A growth mixture modeling approach. Health Psychology. 2010;29(5):484–495. doi: 10.1037/a0020809. [DOI] [PubMed] [Google Scholar]
- Hynie M. Refugee integration: Research and policy. Peace and Conflict. 2018;24:265–276. [Google Scholar]
- Javanbakht A., Amirsadri A., Abu Suhaiban H., Alsaud M.I., Alobaidi Z., Rawi Z.…Arfken C.L. Prevalence of possible mental disorders in syrian refugees resettling in the United States screened at primary care. Journal of Immigrant and Minority Health. 2019;21(3):664–667. doi: 10.1007/s10903-018-0797-3. [DOI] [PubMed] [Google Scholar]
- Júnior J.G., de Sales J.P., Moreira M.M., Pinheiro W.R., Lima C.K.T., Neto M.L.R. A crisis within the crisis: The mental health situation of refugees in the world during the 2019 coronavirus (2019-nCoV) outbreak. Psychiatry Research. 2020;288:113000. doi: 10.1016/j.psychres.2020.113000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kira I.A., Alpay E.H., Turkeli A., Shuwiekh H.A.M., Ashby J.S., Alhuwailah A. The effects of COVID-19 traumatic stress on executive functions: The case of Syrian refugees in Turkey. Journal of Loss & Trauma. 2021;(January) doi: 10.1080/15325024.2020.1869444. [DOI] [Google Scholar]
- Kizilhan J.I., Noll-Hussong M. Psychological impact of COVID-19 in a refugee camp in Iraq. Psychiatry and Clinical Neurosciences. 2020;74(12):659–660. doi: 10.22028/D291-33374. [DOI] [PubMed] [Google Scholar]
- Kline R.B. Guilford publications; New York: 2015. Principles and practice of structural equation modeling. [Google Scholar]
- Kluge H.H.P., Jakab Z., Bartovic J., d’Anna V., Severoni S. Refugee and migrant health in the COVID-19 response. The Lancet. 2020;395(10232):1237–1239. doi: 10.1016/S0140-6736(20)30791-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B.W. The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B., Löwe B. The patient health questionnaire somatic, anxiety, and depressive symptom scales: A systematic review. General Hospital Psychiatry. 2010;32(4):345–359. doi: 10.1016/j.genhosppsych.2010.03.006. [DOI] [PubMed] [Google Scholar]
- Lancet T. COVID-19 will not leave behind refugees and migrants. Lancet (London, England) 2020;395(10230):1090. doi: 10.1016/S0140-6736(20)30758-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Litam S.D.A., Oh S. Ethnic identity and coping strategies as moderators of COVID-19 racial discrimination experiences among Chinese Americans. Counseling Outcome Research and Evaluation. 2020:1–15. doi: 10.1080/21501378.2020.1814138. [DOI] [Google Scholar]
- Logie C.H., Okumu M., Latif M., Musoke D.K., Lukone S.O., Mwima S.…Kyambadde P. Exploring resource scarcity and contextual influences on wellbeing among young refugees in Bidi Bidi refugee settlement, Uganda: Findings from a qualitative study. Conflict and Health. 2021;15(1):1–11. doi: 10.1186/s13031-020-00336-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mancini T., Sibilla F., Argiropoulos D., Rossi M., Everri M. The opportunities and risks of mobile phones for refugees’ experience: A scoping review. PloS One. 2019;14(12):1–24. doi: 10.1371/journal.pone.0225684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller K.E., Rasmussen A. The mental health of civilians displaced by armed conflict: An ecological model of refugee distress. Epidemiology and Psychiatric Sciences. 2017;26(2):129–138. doi: 10.1017/S2045796016000172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller K.E., Rasmussen A. War exposure, daily stressors, and mental health in conflict and post-conflict settings: Bridging the divide between trauma-focused and psychosocial frameworks. Social Science & Medicine. 2010;70(1):7–16. doi: 10.1016/j.socscimed.2009.09.029. [DOI] [PubMed] [Google Scholar]
- Murray D.R., Schaller M. Threat (s) and conformity deconstructed: Perceived threat of infectious disease and its implications for conformist attitudes and behavior. European Journal of Social Psychology. 2012;42(2):180–188. doi: 10.1002/ejsp.863. [DOI] [Google Scholar]
- Muthén L.K., Muthén B.O. eighth edition. Muthén & Muthén; Los Angeles, CA: 1998–2017. Mplus user’s guide. [Google Scholar]
- Navarrete C.D., Fessler D.M. Disease avoidance and ethnocentrism: The effects of disease vulnerability and disgust sensitivity on intergroup attitudes. Evolution and Human Behavior. 2006;27(4):270–282. doi: 10.1016/j.evolhumbehav.2005.12.001. [DOI] [Google Scholar]
- Nesterko Y., Jäckle D., Friedrich M., Holzapfel L., Glaesmer H. Prevalence of post-traumatic stress disorder, depression and somatisation in recently arrived refugees in Germany: An epidemiological study. Epidemiology and Psychiatric Sciences. 2019;(May) doi: 10.1017/S2045796019000325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Panza G.A., Puhl R.M., Taylor B.A., Zaleski A.L., Livingston J., Pescatello L.S. Links between discrimination and cardiovascular health among socially stigmatized groups: A systematic review. PloS One. 2019;14(6):1–27. doi: 10.1371/journal.pone.0217623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poole D.N., Hedt-Gauthier B., Liao S., Raymond N.A., Bärnighausen T. Major depressive disorder prevalence and risk factors among Syrian asylum seekers in Greece. BMC Public Health. 2018;18(1):1–10. doi: 10.1186/s12889-018-5822-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Porter M., Haslam N. Predisplacement and post displacement of refugees and internally displaced persons. Journal of the American Medical Association. 2005;294(5):610–612. doi: 10.1001/jama.294.5.602. [DOI] [PubMed] [Google Scholar]
- Posselt M., Eaton H., Ferguson M., Keegan D., Procter N. Enablers of psychological well-being for refugees and asylum seekers living in transitional countries: A systematic review. Health & Social Care in the Community. 2019;27(4):808–823. doi: 10.1111/hsc.12680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rees S., Fisher J. COVID-19 and the mental health of people from refugee backgrounds. International Journal of Health Services. 2020;50(4):415–417. doi: 10.1177/0020731420942475. [DOI] [PubMed] [Google Scholar]
- Sawaya H., Atoui M., Hamadeh A., Zeinoun P., Nahas Z. Adaptation and initial validation of the Patient Health Questionnaire - 9 (PHQ-9) and the Generalized Anxiety Disorder - 7 Questionnaire (GAD-7) in an Arabic speaking Lebanese psychiatric outpatient sample. Psychiatry Research. 2016;239:245–252. doi: 10.1016/j.psychres.2016.03.030. [DOI] [PubMed] [Google Scholar]
- Schaller M., Park J.H. The behavioral immune system (and why it matters) Current Directions in Psychological Science. 2011;20(2):99–103. doi: 10.1177/0963721411402596. [DOI] [Google Scholar]
- Schlechter P., Rodriguez I.M., Morina N., Knausenberger J., Wilkinson P.O., Hellmann J.H. Psychological distress in refugees: The role of traumatic events, resilience, social support, and support by religious faith. Psychiatry Research. 2021;304(July):114121. doi: 10.1016/j.psychres.2021.114121. [DOI] [PubMed] [Google Scholar]
- Schmitt M.T., Postmes T., Branscombe N.R., Garcia A. The consequences of perceived discrimination for psychological well-being: A meta-analytic review. Psychological Bulletin. 2014;140(4):921–948. doi: 10.1037/a0035754. [DOI] [PubMed] [Google Scholar]
- Sevinc M., Hasbal N.B., Sakaci T., Basturk T., Ahbap E., Ortaboz M.…Unsal A. Frequency of depressive symptoms in Syrian refugees and Turkish maintenance hemodialysis patients during COVID-19 pandemic. PloS One. 2021;16(January):1–9. doi: 10.1371/journal.pone.0244347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siriwardhana C., Ali S.S., Roberts B., Stewart R. A systematic review of resilience and mental health outcomes of conflict-driven adult forced migrants. Conflict and Health. 2014;8(1):1–14. doi: 10.1186/1752-1505-8-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith B.W., Freedy J.R. Psychosocial resource loss as a mediator of the effects of flood exposure on psychological distress and physical symptoms. Journal of Traumatic Stress. 2000;13(2):349–357. doi: 10.1023/A:1007745920466. [DOI] [PubMed] [Google Scholar]
- Spatrisano J., Robinson R.V., Eldridge G.D., Rosich R.M. In: Contextualizing immigrant and refugee resilience. Gungor D., Strohmeimer D., editors. Springer; Cham: 2020. Conceptualizing refugee resilience across multiple contexts; pp. 163–182. [Google Scholar]
- Spitzer R.L., Kroenke K., Williams J.B.W., Löwe B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Steel Z., Chey T., Silove D., Marnane C., Bryant R.A., van Ommeren M. Association of torture and other potentially traumatic events with mental health outcomes among populations exposed to mass conflict and displacement a systematic review and meta-analysis. JAMA. 2009;302(5) doi: 10.1001/jama.2009.1132. [DOI] [PubMed] [Google Scholar]
- Sternthal M.J., Slopen N., Williams D.R. Racial disparities in health: How much does stress really matter? Du Bois Review. 2011;8(1):95–113. doi: 10.1017/S1742058X11000087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tinghög P., Malm A., Arwidson C., Sigvardsdotter E., Lundin A., Saboonchi F. Prevalence of mental ill health, traumas and postmigration stress among refugees from Syria resettled in Sweden after 2011: A population-based survey. BMJ Open. 2017;7(12) doi: 10.1136/bmjopen-2017-018899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Topa G., Jiménez I., Valero E., Ovejero A. Resource loss and gain, life satisfaction, and health among retirees in Spain. Journal of Aging and Health. 2017;29(3):415–436. doi: 10.1177/0898264316635589. [DOI] [PubMed] [Google Scholar]
- Ungar M. Resilience across cultures. British Journal of Social Work. 2008;38(2):218–235. doi: 10.1093/bjsw/bcl343. [DOI] [Google Scholar]
- Ungar M. The social ecology of resilience: Addressing contextual and cultural ambiguity of a nascent construct. The American Journal of Orthopsychiatry. 2011;81(1):1–17. doi: 10.1111/j.1939-0025.2010.01067.x. [DOI] [PubMed] [Google Scholar]
- Ungar M., Liebenberg L. Assessing resilience across cultures using mixed methods: Construction of the Child and youth resilience measure. Journal of Mixed Methods Research. 2011;5(2):126–149. doi: 10.1177/1558689811400607. [DOI] [Google Scholar]
- United Nations High Commissioner for Refugees . 2020. Figures at a glance. Retrieved from https://www.unhcr.org/figures-at-a-glance.html. Accessed March 31, 2021. [Google Scholar]
- United Nations High Commissioner for Refugees . 2020. UNHCR Türkiye İstatistikleri. Retrieved from https://www.unhcr.org/tr/unhcr-turkiye-istatistikleri. Accessed March 31, 2021. [Google Scholar]
- United Nations High Commissioner for Refugees . 2020. UNHCR Turkey response during the COVID-19 pandemic. Retrieved from https://www.unhcr.org/tr/wp-content/uploads/sites/14/2020/08/Flash-Update-UNHCR-Turkey-Response-During-COVID-Pandemic.pdf. Accessed March 31, 2021. [Google Scholar]
- United Nations Sustainable Development Group . 2019. Leaving No one behind: A UNSDG operational guide for UN country teams (Interim draft) Retrieved from https://unsdg.un.org/sites/default/files/Interim-Draft-Operational-Guide-on-LNOB-for-UNCTs.pdf. Accessed March 31, 2021. [Google Scholar]
- Ustubici A., Karadag S. 2020. Refugee protection in Turkey during the first phase of the COVID-19 pandemic, Turkey interim report. Retrieved from http://admigov.eu/upload/Ustubici_Karadag_2020_Turkey_Interim_Report.pdf. Accessed March 31, 2021. [Google Scholar]
- von Haumeder A., Ghafoori B., Retailleau J. Psychological adaptation and posttraumatic stress disorder among Syrian refugees in Germany: A mixed-methods study investigating environmental factors. European Journal of Psychotraumatology. 2019;10(1) doi: 10.1080/20008198.2019.1686801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wachter K., Bunn M., Schuster R.C., Boateng G.O., Cameli K., Johnson-Agbakwu C.E. A scoping review of social support research among refugees in resettlement: Implications for conceptual and empirical research. Journal of Refugee Studies. 2021;00(0) doi: 10.1093/jrs/feab040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J., Wang X. John Wiley & Sons; West Sussex: 2012. Structural equation modeling: applications Using Mplus. [Google Scholar]
- World Health Organization . 2021. WHO coronavirus (COVID-19) dashboard. Retrieved from https://covid19.who.int/. Accessed March 31, 2021. [Google Scholar]
- World Health Organization . 2018. Report on the health of refugees and migrants in the WHO European Region: No public health without refugees and migrant health. Retrieved from https://apps.who.int/iris/bitstream/handle/10665/311347/9789289053846-eng.pdf. Accessed March 31, 2021. [Google Scholar]
- Yildirim H., Isik K., Yildirim-Firat T., Aylaz R. Determining the correlation between social support and hopelessness of Syrian refugees living in Turkey. Journal of Psychosocial Nursing and Mental Health Services. 2020;58(7) doi: 10.3928/02793695-20200506-04. [DOI] [PubMed] [Google Scholar]
- Zhang M., Gurung A., Anglewicz P., Baniya K., Yun K. Discrimination and stress among Asian refugee populations during the COVID-19 pandemic: Evidence from Bhutanese and Burmese refugees in the USA. Journal of Racial and Ethnic Health Disparities. 2021 doi: 10.1007/s40615-021-00992-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimet G.D., Dahlem N.W., Zimet S.G., Farley G.K. The multidimensional scale of perceived social support. Journal of Personality Assessment. 1988;52(1):30–41. doi: 10.1207/s15327752jpa5201_2. [DOI] [PubMed] [Google Scholar]
- Zwiebach L., Rhodes J., Roemer L. The authors interviewed by phone 2,752 randomly selected individuals in New York City within 6 to 9 months after the attacks of September 11, 2001 on the World Trade Center, and 1,939 of these were reinterviewed at a 12- to 16-month follow-up. It was hypo. Journal of Traumatic Stress. 2010;23(6):751–758. doi: 10.1002/jts.20579.Resource. [DOI] [Google Scholar]