Abstract
Background
Electronic medical records (EMRs) can improve the quality of health care and patient safety. Various countries have gone through the local application of EMRs to various health care organizations in national implementation and integration of EMRs. Ethiopia lags far in the back in this regard, as solely some hospitals have implemented EMR.
Objective
This study aimed to identify barriers to the adoption of EMRs in Ethiopia through a systematic review of the literature.
Methods
PubMed, Semantic Scholar, and Google Scholar have been searched for applicable articles. The search method focuses on peer-reviewed, empirical research conducted in Ethiopia. The ultimate set that met the inclusion standards was 9 studies. The authors extracted, analyzed, and summarized empirical results associated with EMR barriers in these studies.
Results
This systematic review identified the following 17 barriers to EMR adoption: absence of EMR training, limited access to computers, insufficient computer literacy, deficiency of EMR knowledge, inadequate technical help, absence of EMR manual, negative attitude to EMR, limited internet access, lack of management support, electric power interruption, absence of perceived system quality, absence of perceived information quality, lack of willingness, the complexity of the system, performance expectancy, effort expectancy, and lack of IT qualification.
Conclusion
The most common barriers for EMR adoption are absence of EMR training, limited access to a computer, poor computer literacy, poor EMR knowledge, lack of technical support, and absence of an EMR manual. As this study summarizes the available evidence regarding barriers to adopting EMR in Ethiopia, future research will rest on this evidence and specialize in building a proper framework for EMR implementation in Ethiopia.
Keywords: electronic medical record, electronic health record, barriers, adoption, Ethiopia, systematic review
Introduction
Electronic Medical Records (EMRs) is a computerized electronic file system used to capture, store, and share information between health care providers in an organization, which supports the delivery of patient health services.1 It helps to enhance healthcare quality through enhancing workflow, lowering medical malpractice, minimizing price and therapy time, increasing revenue, improving patient care through creating a stronger linkage to all caregivers, lowering the want for file hose and people for the retrieval and filing of medical records.2,3
Despite the high expectations and activity in EMR as a principal pressure to enhance the standard, quality, continuity, safety, and effectiveness of healthcare worldwide, the adoption rate is incredibly low.4–6 Over 50% of EMRs may fail or fail to be used effectively within the world.5,7
Over the previous few decades, many countries are dedicated themselves to the countrywide implementation of EMRs to boost healthcare systems and better control human health needs.8 As in many countries, the Ethiopian Ministry of Health has acknowledged the importance of EMRs for quality enhancement in healthcare delivery. In 2013, the Ethiopian Ministry of Health adopted the EMR and planned to extend it to succeed in all hospitals, however, few health facilities have implemented EMRs.9
Given the massive quantity of resources supplied for the implementation of EMR, figuring out barriers to the adoption of EMR is vital to its effective implementation. Although researches are being carried out to recognize the barriers to the adoption of EMRs in Ethiopia, there has been no systematic review of those studies. Thus, our study aimed to identify barriers to the adoption of EMRs in Ethiopia through a systematic review of the literature. The findings of this study will aid policymakers in planning and developing strategies to extend EMR adoption.
Methods
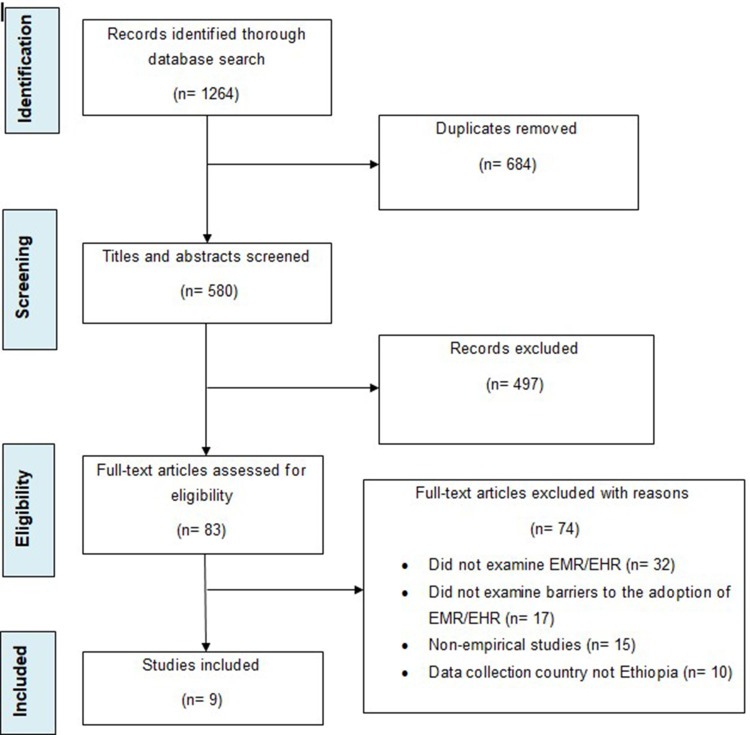
A systematic literature review was carried out based on the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA).10 PRISMA was used to show the flow of the study at each stage of the review process. The PRISMA flow diagram is also used to map the number of records identified, included, and excluded and the reasons for exclusion.
Source of Information and Search Strategy
PubMed, Semantic Scholar, and Google Scholar were searched from 2 to 15 March 2021. To amplify the possibilities of finding all researches carried out in Ethiopia, two common search terms, separated by using operator “OR”, were used: “electronic medical record” AND “Ethiopia” OR “electronic health record” AND “Ethiopia”.
Eligibility Criteria
The inclusion and exclusion criteria’s were: 1) articles focusing solely on EMR or EHR, but no longer other electronic systems used in healthcare (for instance on IT systems, or Personal Health Records (PHRs)), 2) articles assessing barriers to the implementation and/or adoption of EMR/EHR, 3) articles published in scientific journals-conference articles and unpublished work were excluded, 4) articles primarily based on empirical studies, and 5) articles where the country of data collection was in Ethiopia.
Selection Process
Initially, two independent reviewers screened all titles and abstracts for probably eligible articles. Articles that failed to meet the inclusion criteria were removed from the list. Discrepancies about exclusions between the two reviewers were resolved through discussion. Finally, all reviewers assessed the full text of each article individually to create the ultimate selection of important studies to include.
Data Extraction and Analysis
Articles that met the eligibility criteria were further analyzed and therefore the following items had been extracted from each article: research methods, data collection methods, sample size, and sampling techniques. Finally, the empirical results associated with EMR adoption barriers were extracted from each article.
Meta-analysis of results was not attempted because of variations between studies in terms of research approaches and type of participants. For instance, research11 used a qualitative method to understand the hindering factors for EMR adoption, while the remaining studies used quantitative methods. Statistical interpretation supported the findings of11 was not feasible, so meta-analysis was not possible. But, the analytical method employed by previous systematic reviews12,13 were used in the current study. In this manner, the barriers were analyzed based on the rate of existence within the studies. This method can yield trustworthy results in our study.
Results
Study Selection
The selection process and the associated inclusion criteria are presented in Figure 1. A total of 1264 studies had been recognized for the first screening. Then, 684 studies have been removed after being marked as duplicates. After being managed for duplicates, the titles and abstracts of 580 studies have been examined. Subsequently, 83 studies had been placed for a full-text review. A total of 74 studies have been excluded based on the full-text assessment. Finally, 9 studies were included in the review.
Figure 1.
PRISMA flowchart showing the selection process and the associated inclusion criteria.
Notes: PRISMA adapted from Liberati A, Altman D, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Journal of Clinical Epidemiology. 2009;62(10)e1-e34. Creative Commons.42
Abbreviations: PRISMA, preferred reporting items for systematic reviews and meta-analysis; EMR, electronic medical record; EHR, electronic health record.
Study Characteristics
Included articles varied across some areas, as shown in Table 1. Six studies used a quantitative research method, two using a mixed approach and one remaining using a qualitative approach. All of these studies were conducted in hospital areas, except this one, which was conducted in hospital and primary care.14 Different types of respondents have been included in the studies. All studies involved a mix of different health professionals such as laboratory staff, pharmacists, midwives, and others,14 doctors, nurses, pharmacists, and health management information system (HMIS) staff.9
Table 1.
Characteristics of Included Studies
| Reference/ Year of Publication | Type of Research | Method of Data Collection | Number of Participants/ Sampling Strategy |
|---|---|---|---|
| Awol et al36/ 2020 | Mixed | Questionnaire & interview | 451/ Random sampling |
| Biruk et al37/ 2014 | Quantitative | Questionnaire | 606/ Random sampling |
| Ahmed et al38/ 2020 | Quantitative | Questionnaire | 420/ Random sampling |
| Berihun et al14/ 2020 | Quantitative | Questionnaire | 616/ Random sampling |
| Yehualashet et al39/ 2015 | Quantitative | Questionnaire | 428/ Random sampling |
| Tilahun and Fritz9/ 2015 | Quantitative | Questionnaire | 406/ Random sampling |
| Tilahun and Fritz40/ 2015 | Quantitative | Questionnaire | 332/ Random sampling |
| Gebre-Mariam et al11/ 2012 | Qualitative | Questionnaire & interview | 30/ Convenience sampling |
| Berhe et al41/ 2017 | Mixed | Questionnaire & FGD | 255/ Sampling strategy not provided |
Barriers to EMR Adoption in Ethiopia
A total of 17 barriers have been identified across the 9 studies as presented in Table 2. The identified barriers are lack of EMR training, limited access to computers at work, lack of computer literacy, lack of EMR knowledge, lack of technical support, lack of EMR manual, health professionals negative attitude towards EMR, limited internet access in the workplace, lack of management support, electric power interruption, lack of perceived system quality, lack of perceived information quality, lack of willingness, the complexity of the system, performance expectancy, effort expectancy, and lack of information technology (IT) qualification.
Table 2.
Barriers to the Adoption of EMR in Ethiopia and Frequency of Occurrences
| No. | Barriers | References | Frequency | % |
|---|---|---|---|---|
| 1 | Lack of EMR training | [9,11–37,39,40] | 7 | 77.8 |
| 2 | Limited computer access | [9,36,37,39,40] | 5 | 55.6 |
| 3 | Lack of computer literacy | [14,36,37,39,41] | 5 | 55.6 |
| 4 | Lack of knowledge on EMR | [14,36,37] | 3 | 33.3 |
| 5 | Lack of technical support | [11,38,40] | 3 | 33.3 |
| 6 | Absence of EMR manual | [14,39,40] | 3 | 33.3 |
| 7 | Negative attitude towards EMR | [36,37] | 2 | 22.2 |
| 8 | Limited internet access | [36,41] | 2 | 22.2 |
| 9 | Lack of management support | [14,39] | 2 | 22.2 |
| 10 | Electric power interruption | [39,41] | 2 | 22.2 |
| 11 | Lack of perceived system quality | [9,40] | 2 | 22.2 |
| 12 | Lack of perceived information quality | [9,40] | 2 | 22.2 |
| 13 | Lack of willingness | [37] | 1 | 11.1 |
| 14 | Complexity of the system | [37] | 1 | 11.1 |
| 15 | Performance expectancy | [38] | 1 | 11.1 |
| 16 | Effort expectancy | [38] | 1 | 11.1 |
| 17 | Lack of IT qualification | [9] | 1 | 11.1 |
The 17 barriers are organized by the frequency of occurrences among the studies, with the most frequently listed first. The frequency rates of the 17 barriers are: the “Lack of EMR training” appeared in seven of the nine studies (77.8%), “Limited access of computer” and “Lack of computer literacy” appeared in five of the nine studies (55.6%); “Lack of knowledge”, “Lack of technical support”, and “absence of EMR manual”, each appeared in three of the nine studies (33.3%); “Negative attitude towards EMR”, “Limited internet access”, “Lack of management support”, “Electric power interruption”, “Lack of perceived system quality” and “Lack of perceived information quality” each appeared in two of the nine studies (22.2%); five barriers, namely: “Lack of willingness to implement the system”, “Complexity of the system”, “Performance expectancy”, “Effort expectancy”, and “Lack of IT qualification” each appeared once in the nine articles (11.1%).
Discussion
Our systematic review found a variety of potential barriers to the adoption of EMR systems in Ethiopia. The most common barriers to EMR adoption are Lack of EMR training, limited access to computers, lack of computer literacy, lack of EMR knowledge, lack of technical support, and lack of EMR manuals.
Lack of EMR training is often declared as an obstacle. A systematic review of the perceptions of health care professionals about EMR adoption in the Gulf Cooperation Council countries has provided a lack of training as a major barrier to EMR adoption.15 Similarly, evidence from western Canada states that the lack of proper practical training and support for EMR systems has affected the success of EMR implementation.16 In another study from India, two-thirds of medical professionals cited a lack of EMR training as a barrier to EMR adoption.17 Accordingly, training should be considered as an important determinant for the successful implementation of EMR systems.
One of the most commonly reported barriers is the lack of a computer in the office. Similarly, a study by Norwegian physicians on the use of EMR systems reported that some of the computers and other hardware required to run EMR properly were not present in some practices and that this problem prevented EMR from being widely adopted.18 Implementing EMR systems requires considerable hardware, including computers, cable, and Internet connections. Therefore, the successful implementation of EMR by healthcare organizations should take into account the allocation of appropriate technical resources and a percentage of total revenue.
The limited capacity of health professionals in computer literacy is also a persistent obstacle. The study was supported by a study conducted in Malaysia,19 Taiwan,20 and Iran.21 Consistently, several systematic reviews22–25 suggest that a lack of computer literacy is the most common barrier to EMR adoption. Three studies conducted in Saudi Arabia report that computer literacy is closely related to health care professionals’ EHR acceptance,26 health care professionals’ EHR use,27 and health professionals’ satisfaction with HER.28 Furthermore, studies conducted in developing countries have shown that poor computer skills of health professionals are related to poor implementation of EMR systems.29–31
The present study also found that lack of EMR knowledge is a major barrier to EMR adoption. Similarly, a study conducted in Iran on nurse readiness to implement EMR found that lack of knowledge was a major obstacle to the success of EMR implementation.32 A similar study in northern Ghana found that EHR knowledge was an important determinant of healthcare provider’s readiness to adopt EHRs.33 Another important issue is the negative attitude of health care professionals towards the EMR system. This exploration is consistent with a systematic review of the perceptions of health care professionals on EHR adoption in the Gulf Cooperation Council countries, in which negative perception is a major challenge to adopt an EHR.15 This is a good explanation for the need for professionals to be aware of the EMR system before implementing it so that they have a good attitude and develop their readiness for better adaptation of the system.
Lack of management support has also been identified as a major problem hindering the implementation of EMR systems. Whether managers support EMR adoption and trust the benefits of EMR will have an impact on clinicians’ level of EMR adoption.6,34,35 Therefore, managers at all levels of the health care system must be committed to supporting EMR implementation.
Overall, this study summarizes the results of current empirical studies and identifies barriers to the widespread adoption of the EMR system in Ethiopia. To promote health care delivery and patient care quality, managers and other stakeholders in healthcare organizations need to be aware of these barriers that hinder EMR implementation. There are some important limitations to this study. Although the authors did a thorough search, only a limited number of articles (n = 9) were found. This may be due to limited research on e-health in Ethiopia.
Conclusion
In this paper, barriers to the adoption of the EMR system in Ethiopia are identified through a systematic review of the literature. Lack of EMR training, limited access to computers, health professional’s limited computer literacy, deficiency of EMR knowledge, absence of technical support, and absence of EMR manual were the most common barriers to the adoption of EMR. This knowledge update about EMR barriers is important for policymakers, health informatics professionals, academics, clinicians, and EMR vendors. EMR policymakers and implementers, such as hospital managers and project leaders, can use this information to understand what barriers exist in their specific situation to identify appropriate interventions to address these barriers. From a practical point of view, policymakers can use the results of this study to plan and design policies to increase EMR adoption. Additionally, EMR vendors can use the findings in system development and marketing. Researchers can also use this information to investigate reported barriers in various settings and regions (eg investigating type and frequency of technical issues with EMR systems). As this study summarizes the available evidence regarding barriers to adopting EMR in Ethiopia, future studies will rest on this evidence and specialize in building an appropriate framework for EMR adoption in Ethiopia.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Hamilton C. The WHO-ITU national eHealth strategy toolkit as an effective approach to national strategy development and implementation. Stud Health Technol Inform. 2013;192:913–916. [PubMed] [Google Scholar]
- 2.Bagayoko CO, Anne A, Fieschi M, Geissbuhler A. Can ICTs contribute to the efficiency and provide equitable access to the health care system in Sub-Saharan Africa? The Mali experience. Yearb Med Inform. 2011;6(1):33–38. [PubMed] [Google Scholar]
- 3.Williams F, Boren SA. The role of the electronic medical record (EMR) in care delivery development in developing countries: a systematic review. Inform Prim Care. 2008;16(2):139–145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Terry AL, Brown JB, Bestard Denomme L, Thind A, Stewart M. Perspectives on electronic medical record implementation after two years of use in primary health care practice. J Am Board Fam Med. 2012;25(4):522–527. doi: 10.3122/jabfm.2012.04.110089 [DOI] [PubMed] [Google Scholar]
- 5.Willyard C. Focus on electronic health records: electronic records pose dilemma in developing countries. Nat Med. 2010;16(3):249. doi: 10.1038/nm0310-249a [DOI] [PubMed] [Google Scholar]
- 6.Miller RH, Sim I. Physicians? use of electronic medical records: barriers and solutions. Health Aff. 2004;23(2):116–126. doi: 10.1377/hlthaff.23.2.116 [DOI] [PubMed] [Google Scholar]
- 7.Ketikidis P, Dimitrovski T, Lazuras L, Bath PA. Acceptance of health information technology in health professionals: an application of the revised technology acceptance model. Health Informatics J. 2012;18(2):124–134. doi: 10.1177/1460458211435425 [DOI] [PubMed] [Google Scholar]
- 8.AlJarullah A, El-Masri S. A novel system architecture for the national integration of electronic health records: a semi-centralized approach. J Med Syst. 2013;37(4):1–20. doi: 10.1007/s10916-013-9953-4 [DOI] [PubMed] [Google Scholar]
- 9.Tilahun B, Fritz F. Comprehensive evaluation of EMR system use and user satisfaction at five low-resource setting hospitals in Ethiopia. JMIR Med Inform. 2015;3(2):e22. doi: 10.2196/medinform.4106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. [PubMed PMID: 19621072]. doi: 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gebre-Mariam M, Borycki E, Kushniruk A, Purkis MAn Electronic Medical Record (EMR) implementation framework for HIV care and treatment facilities in Ethiopia. 2012;11.
- 12.Khan SU, Niazi M, Ahmad R. Barriers in the selection of offshore software development outsourcing vendors: an exploratory study using a systematic literature review. Inf Softw Tech. 2011;53(7):693–706. doi: 10.1016/j.infsof.2010.08.003 [DOI] [Google Scholar]
- 13.Kruse CS, Goetz K. Summary and frequency of barriers to adoption of CPOE in the U.S. J Med Syst. 2015;39(2):15. doi: 10.1007/s10916-015-0198-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Berihun B, Atnafu DD, Sitotaw G. Willingness to use Electronic Medical Record (EMR) system in healthcare facilities of Bahir Dar City, Northwest Ethiopia. Biomed Res Int. 2020;2020:3827328. doi: 10.1155/2020/3827328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Alanazi B, Butler-Henderson K, Alanazi M. Perceptions of healthcare professionals about the adoption and use of EHR in Gulf cooperation council countries: a systematic review. BMJ Health Care Inform. 2020;27(1):e100099. doi: 10.1136/bmjhci-2019-100099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ludwick DA, Doucette J. Primary care physicians’ experience with electronic medical records: barriers to implementation in a fee-for- service environment. Int J Telemed Appl. 2009;853524. doi: 10.1155/2009/853524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Loomis GA, Ries S, Saywell RM, Thakker NR. If electronic medical records are so great, why aren’t family physicians using them? J Fam Pract. 2002;51(7):636–641. [PubMed] [Google Scholar]
- 18.Laerum H, Ellingsen G, Faxvaag A. Doctors’ use of electronic medical records systems in hospitals: cross sectional survey. Br Med J. 2001;323(7325):1344–1348. doi: 10.1136/bmj.323.7325.1344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mukred M, Yusof ZM, Alotaibi FM, Mokhtar UMIA, Fauzi F. The key factors in adopting an electronic records management system (ERMS) in the educational sector: a UTAUT-based framework. IEEE Access. 2019;7:35963–35980. doi: 10.1109/ACCESS.2019.2904617 [DOI] [Google Scholar]
- 20.Huang W-M, Chen T, Hsieh C-WAn empirical study on the physicians’ behavioral intention with electronic medical record systems in Taiwan. PACIS; 2014:160.
- 21.Gagnon M, Kebir E, Kengne P, et al. Electronic health record acceptance by physicians: testing an integrated theoretical model. J Biomed Inform. 2014;48:17–27. doi: 10.1016/j.jbi.2013.10.010 [DOI] [PubMed] [Google Scholar]
- 22.Gagnon MP, Desmartis M, Labrecque M, et al. Systematic review of factors influencing the adoption of information and communication technologies by healthcare professionals. J Med Syst. 2012;36(1):241–277. doi: 10.1007/s10916-010-9473-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Li J, Talaei-Khoei A, Seale H, Ray P, Macintyre CR. Health care provider adoption of eHealth: systematic literature review. Interact J Med Res. 2013;2(1):e7. doi: 10.2196/ijmr.2468 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McGinn CA, Grenier S, Duplantie J, et al. Comparison of user groups’ perspectives of barriers and facilitators to implementing electronic health records: a systematic review. BMC Med. 2011;9(1):1–10. doi: 10.1186/1741-7015-9-46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Najaftorkaman M, Ghapanchi AH, Talaei-Khoei A, Ray P. A taxonomy of antecedents to user adoption of health information systems: a synthesis of thirty years of research. J Assoc Inf Sci Technol. 2015;66(3):576. doi: 10.1002/asi.23181 [DOI] [Google Scholar]
- 26.Hasanain RA, Vallmuur K, Clark M. Electronic medical record systems in Saudi Arabia!: knowledge and preferences of healthcare professionals. J Health Inform Dev Ctries. 2015;9(1):23–31. [Google Scholar]
- 27.Nour El Din MM. Physicians’ use of and attitudes toward electronic medical record system implemented at a teaching hospital in Saudi Arabia. J Egypt Public Health Assoc. 2007;82(5–6):347–364. [PubMed] [Google Scholar]
- 28.Alasmary M, El Metwally A, Househ M. The association between computer literacy and training on clinical productivity and user satisfaction in using the electronic medical record in Saudi Arabia. J Med Syst. 2014;38(8):1–13. doi: 10.1007/s10916-014-0069-2 [DOI] [PubMed] [Google Scholar]
- 29.Kgasi MR, Kalema BM. Assessment E-health readiness for rural South African areas. J Ind Intell Inf. 2014;2(2):131–135. doi: 10.12720/jiii.2.2.131-135 [DOI] [Google Scholar]
- 30.Yogeswaran P, Wright G. EHR implementation in South Africa: how do we get it right? Stud Health Technol Inform. 2010;160(Pt 1):396–400. [PubMed] [Google Scholar]
- 31.Fraser HS, Biondich P, Moodley D, Choi S, Mamlin BW, Szolovits P. Implementing electronic medical record systems in developing countries. Inform Prim Care. 2005;13(2):83–95. [DOI] [PubMed] [Google Scholar]
- 32.Mahdi H-K, Reza S, Hamid B. Nurses readiness and electronic health records. Acta Inform Med. 2015;23(2):105. doi: 10.5455/aim.2015.23.105-107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Adjorlolo S, Ellingsen G. Readiness assessment for implementation of electronic patient record in Ghana: a case of university of Ghana hospital. J Health Inform Dev Ctries. 2013;7(2):128–140. [Google Scholar]
- 34.Vishwanath A, Scamurra SD. Barriers to the adoption of electronic health records: using concept mapping to develop a comprehensive empirical model. Health Informatics J. 2007;13(2):119–134. doi: 10.1177/1460458207076468 [DOI] [PubMed] [Google Scholar]
- 35.Reardon JL, Davidson E. An organisational learning perspective on the assimilation of electronic medical records among small physician practices. Eur J Inf Syst. 2007;16(6):681–694. doi: 10.1057/palgrave.ejis.3000714 [DOI] [Google Scholar]
- 36.Awol SM, Birhanu AY, Mekonnen ZA, et al. Health professionals’ readiness and its associated factors to implement electronic medical record system in four selected primary hospitals in Ethiopia. Adv Med Educ Pract. 2020;11:147–154. doi: 10.2147/AMEP.S233368 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Biruk S, Yilma T, Andualem M, Tilahun B. Health Professionals ‘ readiness to implement electronic medical record system at three hospitals in Ethiopia: a cross-sectional study. BMC Med Inform Decis Mak. 2014;14(1):115. doi: 10.1186/s12911-014-0115-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ahmed MH, Bogale AD, Tilahun B, et al. Intention to use electronic medical record and its predictors among health care providers at referral hospitals, north-West Ethiopia, 2019: using unified theory of acceptance and use technology 2(UTAUT2) model. BMC Med Inform Decis Mak. 2020;20(1):207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yehualashet G, Asemahagn M, Tilahun B. The attitude towards and use of electronic medical record system by health professionals at a referral hospital in Northern Ethiopia: a cross-sectional study. J Health Inform Afr. 2015;3(1):19–29. [Google Scholar]
- 40.Tilahun B, Fritz F. Modeling antecedents of electronic medical record system implementation success in low resource setting hospitals. BMC Med Inform Decis Mak. 2015;15(1):61. doi: 10.1186/s12911-015-0192-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Berhe M, Gebremariam K, Gebregergs GB, Gebrehiwot T. Evaluation of electronic medical record implementation from user’s perspectives in Ayder referral hospital Ethiopia. J Health Med Inform. 2017;8(1):2. doi: 10.4172/2157-7420.1000249 [DOI] [Google Scholar]
- 42.Liberati A, Altman D, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. ournal of Clinical Epidemiology. 2009;62(10)e1-e34. [DOI] [PubMed] [Google Scholar]