Abstract
Background
The aim of this paper was to examine the early impact of COVID-19 on substance use to assess implications for planning substance use treatment and support systems.
Method
A systematic review of literature published up to March 2021 was conducted to summarize changes in prevalence, incidence, and severity of substance use associated with COVID-19 and the accompanying public health measures, including lockdown, stay-at-home orders, and social distancing.
Results
We identified 53 papers describing changes to substance use at the population level. The majority of papers described changes related to alcohol use and most relied on self-reported measures of consumption during the COVID-19 pandemic, compared with pre-pandemic use. There was less evidence to support changes in non-alcohol substance use. In general, risky pre-pandemic alcohol use, caregiving responsibilities, stress, depression, anxiety, and current treatment for a mental disorder were found to be associated with increased substance use.
Conclusion
This review provides preliminary data on changes in substance use, indicating that certain segments of the population increased their alcohol use early on in the COVID-19 pandemic and may be at greater risk of harm and in need of additional services. There is a need for additional population-level information on substance use to inform evidence-based rapid responses from a treatment system perspective.
Keywords: COVID-19, Pandemics, Substance-related disorders, Prevalence, Health services needs and demand, Systematic review
1. Introduction
In response to the COVID-19 pandemic, governments all over the world implemented physical distancing measures, canceled large gatherings, and closed businesses and schools as key strategies to manage the spread of infection. As a result, concerns were raised about the mental health impacts of fear, worry, and isolation related to COVID-19 and public health measures (Rajkumar, 2020, Vigo et al., 2020). Early in the outbreak, high rates of moderate or severe psychological impact as a result of COVID-19 were reported in China (Wang et al., 2020). Within the general context of mental health concerns, it is critical to bring attention to substance use (SU) and substance use disorders (SUD) given their associated global disease burden (Degenhardt et al., 2018) as well as the unique challenges that a pandemic may present for those using substances and the services they require (Dunlop et al., 2020, Ornell et al., 2020).
The impacts of pandemics and associated public health measures can increase negative emotions, which have been linked to SU/SUD and return to SUD, even among long-term abstainers (Da et al., 2020, Ornell et al., 2020, Rajkumar, 2020, Sinha et al., 2009). Early in the pandemic, national and international surveys reported increased rates of SU, particularly alcohol use. Among the respondents to the Global Drug Survey, 56% of respondents increased the number of days on which they drank alcohol since the start of COVID-19 (Winstock, 2020). Boredom, depression, worry, loneliness, and pandemic-related anxiety were reported as reasons for increased use. Surveys with national samples reported that 22% of Americans and 19% of Canadians were drinking more alcohol during COVID-19, and 6% of Canadians were smoking more cannabis (Canadian Centre on Substance Use and Addiction, NANOS Research, 2020, Sharecare, 2020). However, from the same study, 12% of Canadians decreased their alcohol use and 4% of Canadians decreased their cannabis use (CCSA and NANOS Research, 2020). In some high-income countries, especially at the beginning of COVID-19, alcohol sales increased. In the week of March 21, 2020 alcohol sales increased by 67% in the UK and 50% in the U.S., with a greater increase reported for economy brands and larger volume containers (Da et al., 2020, Eley, 2020). In some jurisdictions, governments have loosened alcohol restrictions and there may be longer-term effects of shifts in alcohol policy that may never be rolled back, including increases in off-site sales and home delivery (Finlay and Gilmore, 2020, Rehm et al., 2020). However, in other jurisdictions the opposite trend has occurred, with the implementation of policies to limit the availability of alcohol (Finlay and Gilmore, 2020, Rehm et al., 2020), including temporary alcohol prohibition in some countries (Chu et al., 2021, Mahadevan et al., 2021). It remains unclear how these policies will impact patterns of alcohol use, drug use, and resulting health and social outcomes.
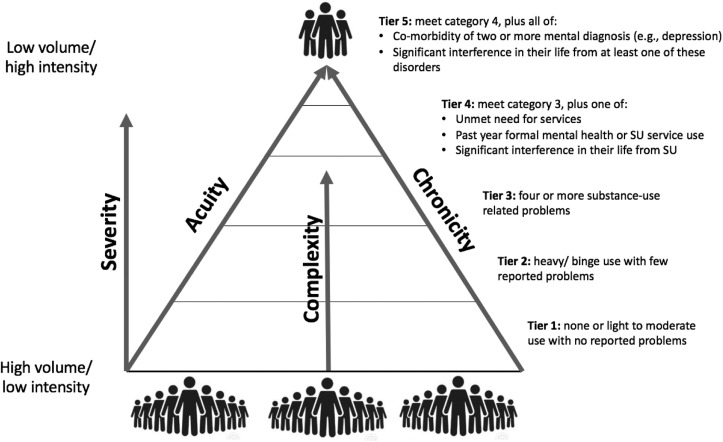
In recent years, the SU field has benefited from adopting a broad system perspective highlighting the importance of aligning public services to the population needs across varying levels of risk and severity (Barker et al., 2016, Rush, 2010, Rush et al., 2019a). Needs-based Planning (NBP) is an approach to health systems planning that uses population distributions to project the required capacity across treatment and support services (Barker et al., 2016, Rush, 2010). Rush et al.'s (2019b) Tiered NBP framework can be used to estimate the need for treatment capacity by accounting for variation in acuity, chronicity, and complexity of SU, and the corresponding type, duration, and intensity of care needed by each segment of the population. Within this five-category framework, Tier 1 and 2 includes people who abstain from or use substances moderately to heavily, but do not report significant problems related to their SU; Tier 3–5 include people with increasing intensity of problems related to their SU, comorbidity including mental health diagnoses, and/ or unmet need for services (Rush et al., 2019b). See Fig. 1 for a description of the five tier categories.
Fig. 1.
Needs based planning (NBP) tiered framework with five severity categories.
Adapted from Rush et al. (2019b) with permission.
For NBP, it is of considerable interest to measure the impact of COVID-19 and model the population-level impact to adjust resource requirements and service distribution across the full spectrum of community needs. In the context of our current work on treatment systems and NBP, we undertook a systematic review to examine the early impact of the COVID-19 pandemic and associated public health measures on SU and SUD in order to understand how these changes may impact the need for treatment and support systems. We were particularly interested in exploring the impact at different levels of risk and severity in the population.
2. Materials and methods
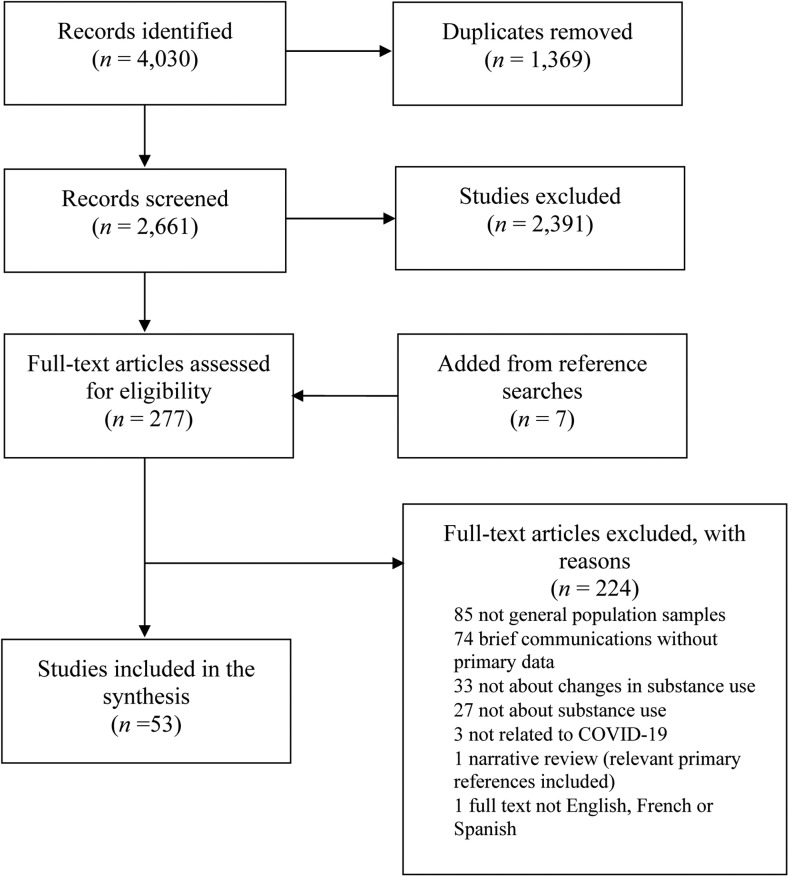
We conducted a systematic review of electronic databases in May and October of 2020 and March of 2021. We searched Medline, EMBASE, PsychInfo, and CINAHL using relevant Medical Subject Headings (MeSH) and key words corresponding to our PICO tool (See Table 1). The complete search strategy can be found in the Appendix. The 4030 identified papers were first screened by title and abstract using the software Covidence (https://www.covidence.org). Three reviewers (RS, JJ, RG) each coded the same random sample of 100 papers. As an acceptable level of agreement was obtained for this sample (> 80%), the subsequent papers were screened by only one reviewer. The full text of the remaining papers was then retrieved and screened for inclusion by two reviewers (RG, JJ), and any disagreements were resolved by discussion with RS. Reference lists of all included studies were screened for relevant articles. Two reviewers (RS, JJ) assessed the included studies using the National Institutes of Health quality assessment tools (https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tool) to identify potential biases in the studies related to our research question. Discrepancies on the quality assessment were resolved through discussions with a third reviewer (RG). The review methods were registered with the International Prospective Register of Systematic Reviews (CRD42020198670, https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=198670). Fig. 2 depicts our Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) diagrams of study selection.
Table 1.
PICO tool for guiding the search strategy.
| P (Problem or patient or population) | Substance use, substance use disorder, drug abuse and dependence (including alcohol, cannabis, opioids, cocaine and amphetamines, but excluding tobacco and nicotine) among general populations of adult human participants. |
| I (Intervention/indicator or exposure) | Exposure to or living in countries affected by the Coronavirus (COVID-19) or the impact of associated public health measures including lockdown, social distancing and stay-at-home orders. |
| C (Comparison) | Before the pandemic; to another population that did not experience the pandemic event; groups within a population; or no comparison. |
| O (Outcome of interest) | Changes substance use service need as identified by changes in prevalence, incidence, or severity of substance use and substance use disorders. |
Fig. 2.
Preferred reporting items for systematic reviews and meta-analyses (PRISMA) flow diagram of study selection.
We included peer-reviewed academic journal articles published up to March 2021 in English, French, or Spanish. We included studies that focused on the impact of living in countries affected by COVID-19, including those studying the impact of lockdown, physical distancing, stay-at-home orders, and other public health measures. Included studies had to report changes to SU service needs at a population level, as indicated by changes in prevalence, incidence, severity, or help-seeking behavior. We excluded papers and results related to tobacco use or that focused only on specific sub-populations (e.g., college students, health care workers). While we initially intended to include papers on the impact of previous respiratory pandemics in this review, we identified only a few papers (e.g., (Lau et al., 2005)) that fit this criterion. As such, we amended our inclusion criteria to include only papers on the impact of the COVID-19 pandemic. We did not make any exclusion by study design but excluded brief reports without original data.
3. Results
We identified 53 papers describing the impact of COVID-19 on substance use prevalence at the population level. Table 2 summarizes the details of the included studies and Table 3 summarizes the results and quality assessment. Most papers used a cross-sectional design with data collection occurring between March and May of 2020 (n = 49), and therefore the evidence presented describes changes that occurred early in the pandemic, during the first wave of COVID-19 infections.
Table 2.
Characteristics of studies included in the systematic review: study design, and participants.
| Studies | Country | Focus of the paper | Participants | Study design | Time frame | Sample |
|---|---|---|---|---|---|---|
| Ahmed et al. (2020) | China | Psychosocial problems, including hazardous and harmful alcohol use | Convenience sample of Chinese population aged 14+ | Online survey of 12-month and lifetime prevalence of mental health problems, comparing results from Hubei province to other provinces | Following public health measures in February 2020 | N = 1074 (46.8% women; mean age 33.5) |
| Alomo et al. (2020) | Argentina | Attitudes and fears towards COVID-19, depression and alcohol use | Convenience sample of Argentinian adults aged 18+ | Online survey on the pattern of alcohol use during quarantine | April 23–30, 2020 | N = 759 (76% women; ages 18 and above) |
| Alpers et al. (2021) | Norway | Alcohol use | Convenience sample of Norwegian adults 18+ | Online survey of changes in alcohol use | April 15–30, 2020; 5 weeks after COVID-19 restrictions were introduced in Norway | N = 25,708 (56% women; median age 50) |
| Ammar et al. (2020) | International (40% Northern Africa, 36% Western Asia, 21% European, 3% other countries) | Eating behaviors and physical activity, including alcohol binge drinking | Convenience sample of multi-country adults aged 18+ | Online survey of mental health and lifestyle behaviors | April 6–11, 2020 | N = 1047 (54% women; 55% 35 years of age or less) |
| Barbosa et al. (2020) | United States | Alcohol drinking patterns | Representative sample of U.S. adults aged 21+ | Online survey to compare drinking behaviors in February and April 2020 | May 8–15, 2020 | N = 555 (52.3% women; ages 21 and above) |
| Bartoszek et al. (2020) | Poland | Mental well-being, including alcohol use | Convenience sample of Polish adults 18+ | Online survey examining symptoms of depression, loneliness, insomnia, and fatigue | Two weeks following April 3, 2020; 1.5 weeks after home confinement restrictions were introduced | N = 471 (85.6% women; mean age 25.5) |
| Błaszczyk-Bębenek et al. (2020) | Poland | Eating habits, including alcohol use | Convenience sample of Polish adults 18+ | Online survey examining eating behaviors | April 29- May 19, 2020; 6 weeks after lockdown was introduced in Poland | N = 312 (64.1% women; mean age 41.12) |
| Boschuetz et al. (2020) | United States | Alcohol use | Convenience sample of U.S. adults 18+ | Online surveys on alcohol use | April 5–12, 2020; 3.5 weeks after confinement measures were introduced | N = 417 (83% women; 44% between 35 and 44 years of age) |
| Callinan et al. (2020) | Australia | Alcohol use | Convenience sample of Australians 18+ who drank at least monthly | Online survey on alcohol use | April 16-May 11, 2020 | N = 1684 (64.6% women; age range 18–65) |
| Callinan et al. (2021) | Australia | Alcohol use | Convenience sample of Australians 18+ who drank at least monthly | Online survey on alcohol use in 2019 and during COVID-19 | April 29- May 16, 2020 | N = 2307 (55.1% women; mean age 46.5) |
| Chodkiewicz et al. (2020) | Poland | Alcohol use | Convenience sample of Polish adults 18+ | A two-stage online survey; the results presented are from the baseline in April 2020 | April 10–20, 2020 | N = 443 (78.6% women; mean age 31.9) |
| Constant et al. (2020) | France | Lifestyle changes, including alcohol use | Convenience sample of French adults 18+, stratified to reflect the distribution of the general population | Online survey on lifestyle changes since the start of COVID | April 8–20, 2020; 3 weeks after lockdown measures were introduced | N = 4005 (51.2% women; age distribution representative of French population) |
| Czeisler et al. (2020) | United States | Mental health, substance use (alcohol, legal or illegal drugs or prescription drugs) and suicidal ideation | Representative sample of U.S. adults 18+ | Panel online survey on the impact of physical distancing and stay-at-home order | April 2–8, 2020 | N = 5412 (50.9% women; ages 18 and above) |
| Czeisler et al. (2020) | United States | Mental health, substance use (not defined) and suicidal ideation | Representative sample of U.S. adults 18+ | Panel online survey on the impact of physical distancing and stay-at-home order | August 28-September 6, 2020 | N = 5470 (50.9% women; ages 18 and above) |
| Đogaš et al. (2020) | Croatia | Lifestyle and mood, including alcohol use | Convenience sample of Croatian adults aged 18+ | Online survey on the impact of lockdown on lifestyle and mood | April 25-May 5, 2020 | N = 3027 (79.7% women; median age 30) |
| Dozois (2021) | Canada | Anxiety and depression, including measures of alcohol and cannabis | Nationally representative sample of Canadian adults aged 18+ | Online survey on depression, anxiety and changes in alcohol and cannabis use | April 22–28, 2020 | N = 1803 (51.4% women; mean age 47.9) |
| Every-Palmer et al. (2020) | New Zealand | Psychological distress, anxiety, family violence, suicidality, wellbeing and alcohol use | Representative sample of New Zealand adults 18+ | Panel online survey on alcohol use, distress, anxiety, and family violence | April 15–18, 2020, which corresponded with Alert Level 4 lockdown days 19–22 | N = 2010 (53% women; age range 18–90) |
| Ferrante et al. (2020) | Italy | Lifestyle changes, including alcohol use | Convenience sample of Italians 14+ | Online survey on alcohol use | April 21- June 7, 2020 | N = 7847 (71% women; mean age 48.6) |
| Gadermann et al. (2021) | Canada | Mental health, including alcohol use | Nationally representative sample of Canadian adults 18+ | Panel online survey comparing mental health, stress, emotional responses, substance use, and suicidality/self-harm among families with children < 18 to those without | May 14–29, 2020; 8.5 weeks after lockdown measures were introduced | N = 618 (52.4% women; mean age 43.0) |
| Garnett et al. (2021) | United Kingdoms | Alcohol use | Representative sample of UK adults aged 18+ | Online survey on alcohol use | March 21-April 4, 2020 | N = 30,375 (49.6% women; mean age 47.8) |
| Glowacz and Schmits (2020) | International (85% Belgium, 14.8% Canada or France) | Psychological distress, including alcohol use | Multi-country convenience sample of adults 18+ | Online surveys about psychological distress | April 17-May 1, 2020 | N = 2871 (79% women; mean age 33.67) |
| Górnicka et al. (2020) | Poland | Dietary changes, including alcohol use | Convenience sample of Polish adults 18+ | Online survey examining dietary changes | April 30- May 23, 2020; 6 weeks after lockdown was implemented in Poland | N = 2381 (89.8% women; largest group aged 30–39 years old) |
| Grossman et al. (2020) | United States | Alcohol use | A convenience sample of U.S. adults 21+ | Online survey on alcohol use | May 2020 | N = 832 (84% women; age range 26–49) |
| Huckle et al. (2020) | New Zealand | Alcohol purchasing and drinking behavior | Convenience sample of New Zealand adults 18+ | Online survey examining alcohol purchasing and drinking behavior | April 30- May 28, 2020 | N = 2173 (79% women; median age 43) |
| Jackson et al. (2021) | United Kingdom | Alcohol and tobacco use | Representative sample of England adults aged 16+ | Monthly cross‐sectional telephone surveys on tobacco and alcohol use (Smoking and Alcohol Toolkit Studies) | April 2020 | N = 1674 (50.9% women; ages 16 and above) |
| Jacob et al. (2021) | United Kingdoms | Alcohol use and mental health | Convenience sample of UK residents aged 18+ | Online survey on alcohol use | March 2020 | N = 691 (61.1% women; 48.8% aged 35–64) |
| Killgore et al. (2021) | United States | Alcohol use | Convenience sample of U.S. adults aged 18+ | Online survey on alcohol use | Six time points between April–September 2020 | N = 5931 (53.7% women; mean age 36.3) |
| Koopmann et al. (2020) | Germany | Alcohol use | Convenience sample of German adults | Online survey on changes in alcohol use | Date not reported | N = 2102 (sex not reported) |
| Kriaucioniene et al. (2020) | Lithuania | Diet and health behaviors, including alcohol use | Convenience sample of Lithuanian adults 18+ | Online survey on changes health behavior | April 14–28, 2020; 1 month after COVID-19 quarantine started in Lithuania | N = 2447 (88% women; majority aged 18–35) |
| López-Bueno et al. (2020) | Spain | Health risk behaviors, including alcohol use | Representative sample of Spanish adults aged 18+ | Online survey on changes health behavior | March 22-April 5, 2020 | N = 2741 (51.8% women; mean age 34.2) |
| McKnight-Eily et al. (2021) | United States | Stress, Mental health and substance use | Representative sample of U.S. adults aged 18+ | Panel online survey on mental health and changes in substance use | April and May 2020 | N = 1004 (gender not reported) |
| Neill et al. (2020) | Australia | Alcohol use | Convenience sample of Australian adults aged 18+ | Online survey on alcohol use during the first month of social isolation measures | April 1, 2020 for 72 h | N = 4462 (80.9% women; 67% age 25–49) |
| Newby et al. (2020) | Australia | Mental health impacts and alcohol use | Convenience sample of Australian adults 18+ | Online surveys about alcohol use | March 27-April 7, 2020 | N = 5070 (86% women; ages 18 and above) |
| Niedzwiedz et al. (2021) | United States | Mental health and health behaviors | Representative sample of UK adults aged 16+ | Longitudinal household panel study on mental health and health behaviors | April 24–30, 2020; compared with waves conducted in 2015–2017, 2016–2018, 2017–2019 | N = 9748 (52% women; mean age 49.5) |
| Oksanen et al. (2021) | Finland | Drinking behavior and psychological stressors | Nationally representative sample of Finnish workers 19+ | Longitudinal National Survey Study | Pre-COVID-19: September 16-October 15, 2019 (Timepoint 1). Participants re-contacted during COVID-19: March 16-April 9, 2020 (Timepoint 2). | N = 1042 (48.2% women; mean age 43.1) |
| Pollard et al. (2020) | United States | Alcohol use | Nationally representative sample of adults 18+ | Online panel surveys on alcohol use with RAND Corporation American Life Panel | Baseline survey: April 29-June 9, 2019; Wave 2: May 28-June 16, 2020 | N = 1540 (57.3% women; age range 30–59) |
| Rodriguez et al. (2020) | United States | Alcohol use as a coping mechanism and psychological distress | Convenience sample of U.S. adults aged 18+ | Online panel survey on the perceived threat, psychological distress and associated drinking behaviors | April 17–23, 2020 | N = 754 (50% women; mean age 41.7) |
| Rodriguez et al. (2020) | Spain | Dietary behavior, including alcohol use | Convenience sample of Spanish adults 18+ | Online survey examining changes in food use and weight gain | March 20, 2020 for 3 weeks; 1 week after confinement was introduced | N = 7514 (70.6% women; 92% were aged between 31 and 65 years) |
| Rolland et al. (2020) | France | Eating behaviors, screen use and substance use | A representative sample of French adults 16+ | Online survey on the impact of the first two weeks of containment measures on diet, screen use and substance use | March 25, 2020 | N = 11,391 (52% women; mean age 47.5) |
| Rossinot et al. (2020) | France | Behavioral changes, including alcohol use | Weighted sample of French adults 24+ | Online survey on behavior changes and mental state during confinement | April 23- May 7, 2020 | N = 1454 (63.5% women; age 24–65) |
| Sallie et al. (2020) | International (85 countries, 32% UK, 26% U.S.) | Alcohol and tobacco use and internet use | Multi-country convenience sample of adults 18+ | Online surveys on changes in alcohol and tobacco use and internet use | May 12–28, 2020 | N = 1346 (24% women; mean age 28.9) |
| Scarmozzino and Visioli (2020) | Italy | Food consumption, including alcohol use | Convenience sample of Italian adults | Online survey on changes in food consumption | April 3–15, 2020; 3.5 weeks after confinement was introduced | N = 1929 (67% women; 63.1% within 21–35 years of age) |
| Sidor and Rzymski (2020) | Poland | Dietary choices, including alcohol use | Convenience sample of Polish adults aged 18+ | Online surveys about the effect of lockdown on diet | April 17-May 1, 2020 | N = 1097 (95.1% women; age range 18–71) |
| Stanton et al. (2020) | Australia | The impact of depression, anxiety and stress on lifestyle changes, including alcohol | Convenience sample of Australian adults aged 18+ | Online surveys about physical activity, sleep, tobacco and alcohol use | April 9-May 19, 2020 | N = 1491 (67% women; mean age 50.5) |
| Szajnoga et al. (2020) | Poland | Alcohol use | Convenience sample of Polish individuals 11+ | Online survey examining alcohol use | April 8–18, 2020; 4 weeks after lockdown restrictions introduced | N = 4072 (84.4% women; mean age 29.6) |
| Taylor et al. (2021) | United States and Canada | Alcohol and drug use | Representative sample of Canadian and U.S. adults 18+ | Online survey on alcohol use and COVID-19 related stress | May 6–19, 2020 | N = 3075 (51% women; mean age 51) |
| Tran et al. (2020) | Australia | Alcohol use and mental health | Representative sample of Australian adults 18+ | Online survey on alcohol use and mental health | April 3- May 2, 2020; four days after COVID-19 restrictions were implemented in Australia | N = 10,596 (75% women; ages 18 and above) |
| Vanderbruggen et al. (2020) | Belgium | Alcohol, tobacco and cannabis use | Convenience sample of Belgium adults aged 18+ | Online survey on substance use during lockdown measures | April 9–29, 2020 | N = 3632 (70% women; mean age 42.1) |
| Villanueva et al. (2021) | Spain | Alcohol use | Convenience sample of Spanish adults | Online survey on alcohol use | April 14-May 29, 2020 | N = 3779 (70% women; age range 18–64) |
| Wardell et al. (2020) | Canada | Alcohol use as a coping mechanism | Convenience sample of Canadian adults aged 18+ | Online survey on external and internal factors in coping motive pathways to alcohol use, solitary drinking and alcohol problems | April 30-May 4, 2020 following | N = 320 (45.3% women; mean age 32) |
| Weerakoon et al. (2020) | United States | Alcohol use | Convenience sample of U.S. adults aged 18+ | Online surveys about alcohol use | Mid-March to mid-April 2020 | N = 1982 (69% women; mean age 42) |
| Winkler et al. (2020) | Czech Republic | Mental health disorders, including alcohol use | Representative sample of Czech adults aged 18+ | Online surveys about prevalence of mental health disorders | May 6–20, 2020 | N = 3021 (52% women; mean age 46.8) |
| Zajacova et al. (2020) | Canada | Health behaviors including alcohol use, junk food, screen time and cannabis | Representative sample of Canadian adults aged 25+ | Online surveys on health behavior | March 29-April 3, 2020 | N = 4383 (51% women) |
Table 3.
Characteristics of studies included in the systematic review: exposure, outcomes and quality assessment.
| Studies | Description of exposure | Measure of substance use | Increased substance use | Decreased substance use | No change | Quality assessmenta |
|---|---|---|---|---|---|---|
| Ahmed et al. (2020) | Full lockdown implemented with restricted transportation related to COVID-19 pandemic | AUDIT | Overall, hazardous drinking increased to 29.1%, harmful drinking increased to 9.5% and alcohol dependency reached to 1.6%. | Not reported | Not reported | Fair |
| Alomo et al. (2020) | Social isolation related to COVID-19 pandemic | Self-reported increase or decrease in alcohol use | 13% reported increases in alcohol use. | Not reported | Not reported | Poor |
| Alpers et al. (2021) | Social distancing, closure of schools, cultural and fitness facilities, related to COVID-19 pandemic | AUDIT-C | 13% increased alcohol use; 54% reported hazardous drinking. | 23% decreased alcohol use. | 64% did not change their alcohol use. | Good |
| Ammar et al. (2020) | Public health measures during COVID-19 including lockdown, closed gyms, no group gatherings, curfews and increased social distancing | Diet questionnaire including self-reported increase or decrease of drinking alcohol "out of control" | Not reported | Binge alcohol drinking decreased: 10.1–5.4% sometimes, 1.8–1.2% most of the time and 0.4% vs 0.2% always drank alcohol "out of control." | Not reported | Poor |
| Barbosa et al. (2020) | COVID-19 stay-at-home orders | Self-reported alcohol use behavior | 29% increased their average drinks per day; average drinks per day increased by 10%; 20% increase of those exceeding drinking limits; and 21% increase in binge drinking in April 2020 compared with February 2020. | Not reported | Not reported | Fair |
| Bartoszek et al. (2020) | Home confinement related to COVID-19 pandemic | Self-reported change in alcohol use since home confinement | 11.9% increased their alcohol use. | None | 38.6% reported no change; 49.5% reported no alcohol use. | Poor |
| Błaszczyk-Bębenek et al. (2020) | Home confinement related to COVID-19 pandemic | Frequency of alcohol use (never, 1–3 times a month, once a week, few times a week, once a day and few times a day) before and after home confinement | Alcohol was consumed more frequently during social isolation. | Not reported | Not reported | Poor |
| Boschuetz et al. (2020) | Social isolation, stay-at-home orders and social distancing related to COVID-19 pandemic | AUDIT-C | Increase in frequency, quantity consumed per day, and frequency consumed before 5 PM. Overall AUDIT scores increased from a median value of 3–4 (Statistically significant only among women). | Abstinence increased from 6.1% to 12.5%; binge drinking (>6 drinks) reduced from 45% to 30%. | Not reported | Good |
| Callinan et al. (2020) | Social distancing and isolation measures related to COVID-19 pandemic | AUDIT | 23.5% increased their AUDIT score. | 48.2% decreased their AUDIT score; mean score decreased from 8.16 to 7.33. | All groups significantly decrease their harmful drinking except for women aged 35 and older. | Good |
| Callinan et al. (2021) | Social distancing related to COVID-19 pandemic | Self-reported frequency, amount and location of alcohol use. Respondents categorized into low-risk (< 2 drinks per day), risky (2–4.99) or high risk (5 or more drinks per day). | 15% moved into a higher risk category. | 15.4% of respondents reported moving into a lower risk category. High-risk drinkers who drank 90% or more alcohol at home reported decreasing their use and were the only group who had less home alcohol use during the lockdown. | Overall, the mean number of drinks per day did not change. 69.5% remained in the same risk category. | Good |
| Chodkiewicz et al. (2020) | Enforcement of the COVID-19 public health measures which included lockdown, business shutdowns, and school closures | AUDIT; Self-reported recreational or designer drugs use | 13.8% increased alcohol use and 1.4% increased drug use. | 17.4% reduced alcohol use and 1.1% reduced drug use. | 27.8% already did not use alcohol and 93.7% did not use drugs. | Good |
| Constant et al. (2020) | Physical distancing, quarantine, school closures and banning gatherings related to COVID-19 pandemic | Self-reported alcohol use behavior | 14.8% of regular drinkers increased alcohol use. | 21.1% of regular drinkers decreased alcohol use. | Not reported | Fair |
| Czeisler et al. (2020) | COVID-19 physical distancing and stay-at-home orders | Self-reported initiation or increase of substance use to cope with stress | 13.3% reported increasing substance use to cope with stress or emotions related to COVID-19. | Not reported | Not reported | Fair |
| Czeisler et al. (2020) | COVID-19 physical distancing and stay-at-home orders | Self-reported increase of substance use | 15.1% reported increases in substance use. | Not reported | Not reported | Fair |
| Đogaš et al. (2020) | Lockdown, social distancing, and home confinement related to COVID-19 pandemic | Self-reported frequency of weekly alcohol use | Proportion of people who drank 7 drinks or more increased from 16.7% to 18.4%. | Proportion of people who did not drink alcohol increased from 19.1% to 32.1%; who drank occasionally (once per month) decreased from 31.9% to 22.3%; and who drank up to 3 drinks a week decreased from 32.3% to 27.2% | Not reported | Fair |
| Dozois (2021) | COVID-19 physical distancing and isolation measures | Self-reported increase or decrease in alcohol use and cannabis use | 28% increased alcohol use and 29% increase in cannabis use. | Not reported | 56% reported no change in alcohol use and 48% reported no change in cannabis | Fair |
| Every-Palmer et al. (2020) | Stay-at-home orders, school closures and travel bans related to COVID-19 pandemic | Self-reported number of standard drinks of alcohol per day | 22% increased alcohol use. | 18.9% decreased alcohol use. | 59.1% did not change their alcohol use. | Fair |
| Ferrante et al. (2020) | Lock down measures related to COVID-19 pandemic | Self-reported increase or decrease in alcohol use | 17.3% increased their alcohol use. | Not reported | Not reported | Poor |
| Gadermann et al. (2021) | Social isolation, school/childcare closures and employment instability related to COVID-19 pandemic | Self-reported change in alcohol use since home confinement | 27.7% of parents increased their alcohol use compared to 16.1% of those without children at home. | Not reported | Not reported | Poor |
| Garnett et al. (2021) | Social distancing and business closures related to COVID-19 pandemic | Self-reported number of drinks consumed in the past week, and changes in alcohol use | 26.2% reported increasing alcohol use over the past week. | 25.7% reported decreasing alcohol use over the past week. | 48.1% reported alcohol use the same as usual. | Good |
| Glowacz and Schmits (2020) | Self-isolation and social distancing related to COVID-19 pandemic | AUDIT-C; self-reported change in alcohol use | A larger percentage of middle-aged and older people increased their alcohol use. | 18–30-year olds reported significantly less use of alcohol, compared with other age groups. | Half the population did not change their alcohol use during lockdown. | Fair |
| Górnicka et al. (2020) | Isolation, social distancing, and home confinement related to COVID-19 pandemic | Self-reported change in alcohol use since home confinement | 18.1% increased their alcohol use. | 10.7% decreased their alcohol use. | 71.3% did not change their alcohol use. | Poor |
| Grossman et al. (2020) | Shelter-at-home orders related to COVID-19 pandemic | Self-reported change and motivation for alcohol use | 60.1% increased alcohol use compared to pre-COVID. | 12.8% reported that their alcohol use had decreased from pre-post COVID-19. | 27.0% did not change their alcohol use. | Fair |
| Huckle et al. (2020) | Home confinement, social distancing related to COVID-19 pandemic | Typical occasion quantity in the past week and self-reported change in alcohol use since home confinement | 47% of males and 53% of females reported drinking more alcohol during COVID-19 restrictions. | 26% of males and 22% of females reported drinking less alcohol during COVID-19 restrictions. | 28% of males and 25% of females reported drinking the same amount of alcohol. | Fair |
| Jackson et al. (2021) | Stay-at-home orders and social distancing related to COVID-19 pandemic | AUDIT-C and self-reported quit attempts | The prevalence of high-risk drinking (38.3%) was significantly higher during compared with before lockdown (25.1%). | Among high-risk drinkers, the odds of making a serious attempt to reduce alcohol use was 2.16 times higher after lockdown as compared to before lockdown. | Not reported | Good |
| Jacob et al. (2021) | Physical distancing related to COVID-19 pandemic | Self-reported change in alcohol use behavior | 17% increased alcohol use. | Not reported | Not reported | Poor |
| Killgore et al. (2021) | Stay-at-home orders related to COVID-19 pandemic | AUDIT-C | Higher levels of hazardous alcohol use among people in areas with lockdowns. AUDIT scores increased month-by-month for those under lockdown. | Not reported | Not reported | Fair |
| Koopmann et al. (2020) | Quarantining and social isolation related to COVID-19 pandemic | Self-reported changes in alcohol use | 34.7% increased alcohol use. | 19.4% decreased alcohol use. | 37.7% did not change their alcohol use. | Poor |
| Kriaucioniene et al. (2020) | Quarantining related to COVID-19 pandemic | Self-reported changes in alcohol use | 14.2%. increased alcohol use. | 15.9% decreased alcohol use. | 69.9% remained the same as before the COVID-19 quarantine. | Poor |
| López-Bueno et al. (2020) | Quarantining related to COVID-19 pandemic | Self-reported alcohol use | Not reported | Percent of the population that reported alcohol use decreased every week over the first three weeks of confinement (70.5% before, 53.4% week 1, 46.5% week 2% and 43.3% week 3). | Not reported | Poor |
| McKnight-Eily et al. (2021) | COVID-19 social isolation measures | Self-reported changes in substance use | 18.2% increased or newly initiated substance use. | Not reported | Not reported | Poor |
| Neill et al. (2020) | Social distancing related to COVID-19 pandemic | Self-reported changes to past week amount of alcohol use | 30.8% reported drinking a lot more than normal. | None | 69.2% reported no change or reducing their alcohol use. | Fair |
| Newby et al. (2020) | Border closures, lockdowns, social distancing and isolation related to COVID-19 | AUDIT-C | 52.7% met criteria for hazardous drinking; higher than the 42% found in previous primary care samples in Australia. | Not reported | Not reported | Fair |
| Niedzwiedz et al. (2021) | Physical distancing related COVID-19 | AUDIT-C | Binge drinking increased from 10.8% in 2017–2019 to 16.2% during lockdown, and dinking four or more times per week increased from 13.7% to 22%. | 5.6% consumed 5 or more drinks on a typical occasion during lockdown, compared with 13.6% 2017–2019. | Not reported | Good |
| Oksanen et al. (2021) | Social distancing related to COVID-19 pandemic | AUDIT-C | 25.4% increased their alcohol use; 53.4% of those who increased their alcohol use during COVID-19 had hazardous (5 or more) AUDIT scores. | 26.62% decreased their alcohol use. | 48.02% did not change their alcohol use behavior. | Good |
| Pollard et al. (2020) | Social distancing related to COVID-19 pandemic | Self-reported number of drinking days, heavy alcohol use and average number of drinks in past 30 days: 15- Item Short Inventory of Problems | Frequency of alcohol use increased by 0.74 days; a 14% increase over the baseline of 5.48 days in 2019. | Not reported | Not reported | Fair |
| Rodriguez et al. (2020) | Stay-at-home orders, social distancing, quarantine, and school closures related to COVID-19 pandemic. | Quantity/Frequency/Peak alcohol use index, in past month | Psychological distress was associated with a 7% increase in the maximum number of drinks consumed, 8% increase in the drinks consumed on a typical occasion and 8% increase in the number of past months drinking days. | Not reported | Not reported | Good |
| Rodriguez et al. (2020) | Home confinement related to COVID-19 pandemic | PREDIMED MedDiet (Mediterranean Diet) Adherence Screener which assesses weekly intake of seven or more glasses of wine | 10.4% increased alcohol use. | 57.3% decreased alcohol use. | 32.3% did not change alcohol use. | Poor |
| Rolland et al. (2020) | Lockdown and only continuing essential services such as medical visits and food supply related to COVID-19 pandemic | Self-reported increase or decrease of alphol and cannabis | 15.5% increased alcohol use. Among drinkers 24.8% increased their alcohol use, and among those who used cannabis 31.2% increased their use. | 10.9% decreased alcohol use. Among those that drank before the lockdown, 17.4% reduced or stopped. Among those who used cannabis before the lockdown, 29.3 reduced or stopped. | 57.8% did not change their alcohol use (36.1% stayed the same, and 37.6% already did not use), and 39.5% did not change their cannabis use. | Fair |
| Rossinot et al. (2020) | Travel bans and restricted trips outside of homes related to COVID-19 pandemic | Self-reported changes in alcohol use | 22.7% increased alcohol use. | 12.2% of decrease in their alcohol use. | 39.1% did not change their alcohol use. | Fair |
| Sallie et al. (2020) | Self-isolation related to COVID-19 pandemic | Self-reported units amount, frequency of alcohol use and AUDIT-C | 36% increased weekly alcohol use. | Units consumed during quarantine decreased, except in the UK; 45% decreased weekly alcohol use. | 19% did not change weekly alcohol use. | Good |
| Scarmozzino and Visioli (2020) | Home confinement related to COVID-19 pandemic | Self-reported change in alcohol use | 10.1% increased alcohol use. | 36.8% decreased alcohol use. | Not reported | Poor |
| Sidor and Rzymski (2020) | Social distancing measures related to COVID-19 | Self-reported frequency of alcohol use | 14.6% increased alcohol use. | Not reported | 77% reported no change in alcohol use. | Fair |
| Stanton et al. (2020) | Social distancing, travel bans and mass gathering cancellations related to COVID-19 pandemic | Self-reported frequency of alcohol use and change since pre-pandemic | 26.6% made "negative changes" (Drink much more, or a little more than usual). | 18.1% made "positive changes" (drank less or much less than usual, or have ceased drinking all together). | 55.3% reported no change in alcohol use. | Fair |
| Szajnoga et al. (2020) | School closures, travel bans, and social distancing related to COVID-19 pandemic | Self-reported frequency of alcohol use before and during home confinement | 17.9% used alcohol more often. | 39.3% used alcohol less often. | 42.8% reported the same amount of alcohol use. | Fair |
| Taylor et al. (2021) | Social distancing and stay-at-home orders related to COVID-19 pandemic | AUDIT and a COVID-19-related alcohol, the drug scales adapted from the AUDIT and self-reported yes/no increase in use | 23% of those who drank prior to the pandemic increased use; 31% reported of those who used drugs increased use; 23% increase in alcohol abuse and 16% increase in drug abuse. | Not reported | Not reported | Fair |
| Tran et al. (2020) | Social distancing related to COVID-19 pandemic | Self-reported changes in alcohol use | About one in five adults reported that they had been drinking more alcohol than usual since the COVID-19 pandemic began (20.9% weighted prevalence). | 10.5% reported less alcohol use. | 43.9% reported about the same alcohol use. | Fair |
| Vanderbruggen et al. (2020) | Lockdown and social distancing related to COVID-19 pandemic | Self-reported average number of standard drinks consumed in the prior week, number of joints consumed per day, and self-reported increase or decrease in use. | 5.8% of the population said they did not drink before but started during social distancing. 30.3% of the population said they drank more and 2.1% used more cannabis. There was a significant increase in the number of drinks per day from one (range 0–15) before to 1.4 during (Range 0–21). | 9.4% of the population quit drinking, 13.7% said used less alcohol and 1.1% used less cannabis. | Not reported | Good |
| Villanueva et al. (2021) | Confinement related to COVID-19 pandemic | AUDIT-C | Not reported | 15.1% reduction in people classified as risky alcohol consumers. | Not reported | Good |
| Wardell et al. (2020) | School closures, work closures, business closures, physical distancing, and stay-at-home recommendations related to COVID-19 pandemic | Quantity/ Frequency (QF) alcohol use index, in past month | Overall frequency of alcohol use was higher compared to 30 days prior to pandemic. | Overall amount per occasion was lower, which resulted in a stable QF score pre and during the pandemic. | Not reported | Good |
| Weerakoon et al. (2020) | Stay-at-home measures related to COVID-19 pandemic | Self-reported change in alcohol use and binge drinking during pandemic | 32.2% had more alcohol use. People who binge drank were more likely to increase alcohol use during the pandemic (60%) than non-binge drinkers (28%). | 10.2% had less alcohol use. | 34.9% had the same amount of alcohol use. | Good |
| Winkler et al. (2020) | Reduced hours for non-essential businesses and stay-at-home orders related to COVID-19 pandemic | Self-reported alcohol frequency and amount of alcohol use and binge drinking | There was a significant increase in number of drinks per drinking session and number of individuals who binge drank at least once per week. | Not reported | The prevalence of alcohol use disorder in 2020 was approximately the same as in 2017. | Fair |
| Zajacova et al. (2020) | Physical distancing and self-isolation related to COVID-19 pandemic | Self-reported alcohol use and cannabis use | 14% increased their alcohol use and 5.5% increased their cannabis use. | 9% decreased their alcohol use. | Not reported | Fair |
Assessed using the NIH quality assessment tools. Possible outcomes of these tools include Poor, Fair or Good, and the quality of evidence described relates to our research question (e.g., measures of change in substance use).
3.1. Percentage of the population that changed their alcohol use
Thirty-two studies reported percent population changes in alcohol use behavior during the COVID-19 pandemic compared with pre-pandemic behavior. Twenty of these papers included a single question such as, “Since the start of the pandemic, has your alcohol use increased, decreased, or stayed the same?” In general, most papers (n = 24) reported both increased and decreased alcohol use among different segments of the population. An equal number of papers (n = 11) reported that more people increased their drinking (Bartoszek et al., 2020, Every-Palmer et al., 2020, Górnicka et al., 2020, Grossman et al., 2020, Huckle et al., 2020, Rolland et al., 2020, Stanton et al., 2020, Tran et al., 2020, Vanderbruggen et al., 2020, Weerakoon et al., 2020, Zajacova et al., 2020), and decreased their drinking during the pandemic at the population level (Alpers et al., 2021, Chodkiewicz et al., 2020, Constant et al., 2020, Dozois, 2021, Koopmann et al., 2020, Kriaucioniene et al., 2020, Oksanen et al., 2021, Rodriguez et al., 2020, Scarmozzino and Visioli, 2020, Sidor and Rzymski, 2020, Szajnoga et al., 2020).
3.2. Changes in frequency, amount, or severity of alcohol used
Twenty studies reported a change in frequency, amount, or severity of alcohol use during the COVID-19 pandemic compared to pre-pandemic use (Alpers et al., 2021, Ammar et al., 2020, Barbosa et al., 2021, Błaszczyk-Bębenek et al., 2020, Boschuetz et al., 2020, Callinan et al., 2021, Callinan et al., 2021, Đogaš et al., 2020, Huckle et al., 2020, Jackson et al., 2021, Newby et al., 2020, Niedzwiedz et al., 2021, Oksanen et al., 2021, Rolland et al., 2020, Sallie et al., 2020, Vanderbruggen et al., 2020, Villanueva et al., 2021, Wardell et al., 2020, Weerakoon et al., 2020, Winkler et al., 2020), two studies compared alcohol use at two or more time points during the pandemic (Killgore et al., 2021, Pollard et al., 2020), and one study compared the severity of alcohol use in Hubei province, the epicenter of COVID-19, compared with respondents from other provinces in China (Ahmed et al., 2020).
3.2.1. Amount and frequency
Four papers reported an increase in number of drinks consumed per day or per occasion during the pandemic (Barbosa et al., 2021, Boschuetz et al., 2020, Vanderbruggen et al., 2020, Winkler et al., 2020). A multi-country study reported that, overall, the units of alcohol consumed during quarantine decreased across their sample, except among participants from the UK who reported an increase (Sallie et al., 2020).
Seven studies reported an increase in how often people consumed alcohol during the pandemic (Błaszczyk-Bębenek et al., 2020, Boschuetz et al., 2020, Pollard et al., 2020), four of which found that despite the increase in frequency there was either no change or a reduction in drinks consumed on each drinking occasion (Callinan et al., 2021, Callinan et al., 2021, Niedzwiedz et al., 2021, Wardell et al., 2020). Boschuetz et al. (2020) also reported an increase in frequency of drinking before 5 PM.
Three studies reported an increase in both the proportion of people who did not drink any alcohol and those who used alcohol heavily or frequently (Błaszczyk-Bębenek et al., 2020, Boschuetz et al., 2020, Đogaš et al., 2020). In these studies, the results indicated that some occasional drinkers shifted into higher or lower risk categories during the pandemic.
3.2.2. Severity
Five studies found that COVID-19 significantly increased AUDIT scores (Ahmed et al., 2020, Jackson et al., 2021, Killgore et al., 2021, Newby et al., 2020), although in one study this was only significant among women (Boschuetz et al., 2020). Killgore et al. (2021) found a positive interaction between the length of lockdown and mean AUDIT score. Four studies did not find increased AUDIT scores during the pandemic (Callinan et al., 2021, Oksanen et al., 2021, Sallie et al., 2020, Villanueva et al., 2021).
Although Oksanen et al. (2021) did not find an overall change in AUDIT scores, among the 37% of the population that did increase their alcohol use, 53.4% of them had hazardous ( 5) AUDIT scores, indicating that those who already drank at risky levels were more likely to increase their use. Similarly, Sallie et al. (2020) found that overall AUDIT scores decreased, but those that did increase their weekly units consumed during COVID-19 had the highest current drinking severity scores, and Weerakoon et al. (2020) found that binge drinkers were more likely to increase alcohol consumption during the pandemic compared with non-binge drinkers (60% vs. 28%).
3.2.3. Binge/hazardous use
Compared to before the pandemic, two studies reported an increased proportion of people reporting binge drinking (Niedzwiedz et al., 2021, Winkler et al., 2020). However, two studies reported a decrease in the percentage of the population that reported binge-drinking (Ammar et al., 2020, Boschuetz et al., 2020), and Alpers et al. (2021) reported that rates of binge and hazardous drinking were similar to pre-pandemic rates from other studies.
3.3. Changes in cannabis use
Four studies reported changes in cannabis use behaviors. Rolland et al. (2020) found that among French adults who used cannabis, 60.5% had made changes to their use; 24.3% had moderately increased, 6.9% had increased in a way that was “difficult to control,” 22.5% had reduced or stopped without cravings or withdrawal, and 6.7% had reduced or stopped but did experience cravings or withdrawal. Vanderbruggen et al. (2020) reported that 2.1% of their Belgian sample reported using more cannabis, while 1.1% reported using less, and there was no significant change in number of joints smoked per day. In Canadian samples, Dozois (2021) found that 29% had increased and 48% reported no change in cannabis use, and Zajacova et al. (2020) found that 5.5% reported increased cannabis use, but they did not report the proportion that decreased or stayed the same.
3.4. Changes in other substance use
Chodkiewicz et al. (2020) found that 1.4% of their Polish sample increased their use of “recreational drugs” and 1.1% decreased their use. A significant majority of their sample, 93.7%, already did not use these drugs. Taylor et al. (2021) found that 31% of their sample who reported drug use prior to the pandemic (16%) had increased their use.
Czeisler et al. (2020) investigated if people in the U.S. had started or increased their SU as a way of coping with COVID-19 stress, including the use of alcohol, legal or illegal drugs, or prescription drugs taken in a way not recommended by a doctor (Czeisler et al., 2020). They found that 13.3% had started or increased SU to cope with stress, however they did not report the number of people who had reduced their SU (Czeisler et al., 2020). Similarly, McKnight-Eily et al. (2021) found that 18.2% increased or initiated substance use during the pandemic.
3.5. Factors associated with changes in substance use
3.5.1. Gender
Thirty studies investigated the impact of gender. Gender differences were noted in nineteen studies (Ahmed et al., 2020, Alpers et al., 2021, Barbosa et al., 2021, Boschuetz et al., 2020, Callinan et al., 2021, Callinan et al., 2021, Đogaš et al., 2020, Ferrante et al., 2020, Gadermann et al., 2021, Garnett et al., 2021, Grossman et al., 2020, Huckle et al., 2020, Killgore et al., 2021, Neill et al., 2020, Niedzwiedz et al., 2021, Pollard et al., 2020, Rodriguez et al., 2020, Rossinot et al., 2020, Sallie et al., 2020), with no significant differences reported in eleven (Bartoszek et al., 2020, Chodkiewicz et al., 2020, Czeisler et al., 2020, Oksanen et al., 2021, Rolland et al., 2020, Sidor and Rzymski, 2020, Szajnoga et al., 2020, Vanderbruggen et al., 2020, Villanueva et al., 2021, Wardell et al., 2020, Zajacova et al., 2020). The impact of gender was mixed. Two papers found men increased their drinking more than women (Ferrante et al., 2020, Gadermann et al., 2021), and that change in drinking amount was positively correlated with being male (Sallie et al., 2020). However, other studies found that being a man was protective for increased alcohol consumption during the pandemic (OR = 0.71 [95% CI: 0.56. 0.90]; Rossinot et al., 2020), and that a larger percentage of men had decreased their alcohol consumption (29.2%) compared with increased consumption (13.1%) or staying the same (12.5%, X 2 p = 0.002; Grossman et al., 2020).
Other studies found significant changes among women’s drinking, with more women reporting increased drinking compared with men (Alpers et al., 2021, Garnett et al., 2021, Neill et al., 2020), and women significantly increasing the frequency of alcohol use during the pandemic (Pollard et al., 2020). Three papers found a significant increase in hazardous drinking among women. Barbosa et al. (2020) found that the proportion of people who increased their use to exceed drinking limits during COVID-19 was larger for women than men; although there was no difference in the number of drinks per day. Boschuetz et al. (2020) also found that women were more likely to develop high-risk behavior during social distancing (63% vs. 25%, p = 0.03). A large increase in the number of women who increased their AUDIT score did so based only on the question regarding frequency of alcohol consumption per week. Niedzwiedz et al. (2021) found that women had a higher risk of binge drinking during COVID-19 compared to before (relative risk [RR] = 1.49 [95% CI: 1.31, 1.69]), and of drinking four or more times per week (RR = 1.34 [95% CI: 1.23, 1.47]). Rodriguez et al. (2020), found the impact of distress on the maximum number and typical number of drinks consumed per occasion was moderated by gender, and that psychological distress was associated with greater drinking in women but not in men.
Looking at the interaction of age and gender, Callinan et al. (2021) found no overall significant difference between men and women's change in alcohol use, but the interaction between age and gender showed young men decreased their use more than other groups. They also found that women aged 30–50 increased both frequency and quantity of consumption and were the only group to not decrease their harmful drinking (Callinan et al., 2020).
3.5.2. Age
Twenty-eight papers looked at the impact of age on SU and reported different trends, with four papers reporting no significant changes based on age (Barbosa et al., 2021, Boschuetz et al., 2020, Sidor and Rzymski, 2020, Szajnoga et al., 2020). Garnett et al. (2021) reported that younger people changed their drinking behavior most often, whether increased or decreased, whereas Sallie et al. (2020) reported that changes were positively associated with age.
Fourteen papers highlighted an increase in SU use based on age. Four reported the greatest increase among the younger groups included in their studies (Alomo et al., 2020 [18–44 years]; Czeisler et al., 2020 [18–24 years]; Jacob et al., 2021 [18–34 years]; Oksanen et al., 2021 [less than 30 years, compared with 30–45 years]). Nine papers reported an increase among the middle-aged group of adults in their studies, aged from 25 up to 50 years old (Alpers et al., 2021 [30–39 years]; Callinan et al., 2021 [30–49 years]; Callinan et al., 2020 [36–50 years]; Czeisler et al., 2020 [25–44 years]; Neill et al., 2020 [25–49 years]; Pollard et al., 2020 [30–59 years]; Rolland et al., 2020 [30–59 years]; Sallie et al., 2020 [25+ years]; Zajacova et al., 2020 [35–44 years, compared to 25–34 years]). Niedzwiedz et al. (2021) reported a higher risk of binge drinking in the 25–44 years age group (when compared to the 65+ age group).
Seven papers reported a decrease in SU related to age. Two papers reported that increasing age was associated with a decrease in drinking (Constant et al., 2020, Vanderbruggen et al., 2020), and five papers found decreased drinking among people younger than 34 years old (Alpers et al., 2021 [18–29 years]; Chodkiewicz et al., 2020 [less than 26 years]; Glowacz and Schmits, 2020 [18–30 years]; Rossinot et al., 2020 [25–34 years]; Villanueva et al., 2021 [18–24 and 25–29 years]). Callinan et al. (2020) found that all ages decreased their risky drinking, except for men aged 26–35 years old, with the largest decrease of risky behavior seen among the youngest people.
3.5.3. Race
Ten studies reported the impact of race on SU. Three found a non-significant impact on SU (Boschuetz et al., 2020, Niedzwiedz et al., 2021, Wardell et al., 2020). Four studies found that racialized groups were more likely to increase their SU or exceed drinking limits during the pandemic (Barbosa et al., 2021, Czeisler et al., 2020, Huckle et al., 2020, McKnight-Eily et al., 2021). However, Garnett et al. (2021) found racialized groups were drinking less during COVID-19.
3.5.4. Mental health
In 13 studies, mental health was associated with increased SU (Bartoszek et al., 2020, Chodkiewicz et al., 2020, Czeisler et al., 2020, Dozois, 2021, Garnett et al., 2021, Jacob et al., 2021, Neill et al., 2020, Rolland et al., 2020, Sallie et al., 2020, Stanton et al., 2020, Tran et al., 2020, Wardell et al., 2020, Weerakoon et al., 2020). Higher rates of depression (Bartoszek et al., 2020, Czeisler et al., 2020, Dozois, 2021, Neill et al., 2020, Stanton et al., 2020, Tran et al., 2020, Wardell et al., 2020, Weerakoon et al., 2020), anxiety (Czeisler et al., 2020, Dozois, 2021, Garnett et al., 2021, Sallie et al., 2020, Stanton et al., 2020, Tran et al., 2020, Weerakoon et al., 2020), overall poor mental health (Jacob et al., 2021), and current treatment for a mental disorder (Rolland et al., 2020), were all found to be associated with increased SU during COVID-19. Wardell et al. (2020) reported that depression was positively associated with greater coping motives for drinking. While Chodkiewicz et al. (2020) found no significant difference in rates of treatment for mental health conditions between low-risk and hazardous drinkers, people who drank more reported coping less well with everyday functioning, and those who were currently having suicidal thoughts (10.7%) were more likely to report increased alcohol use.
3.5.5. Prior substance use
Five studies found an association between the severity of alcohol use and increased drinking during the pandemic. Increased alcohol use was significantly correlated with AUDIT abuse scores (Sallie et al., 2020, Taylor et al., 2021). Taylor et al. (2021) also reported a change in the degree of severity of SU, with pandemic-related increased SU tending to result in hazardously high increases. Sidor and Rzymski (2020) found that alcohol use most frequently increased among people who reported having an “alcohol addiction.” Weerakoon et al. (2020) found that those who reported ever binge drinking reported a greater increase in drinking, Neill et al. (2020) found that heavy drinking prior to the pandemic was associated with increased COVID-19-related drinking, and Boschuetz et al. (2020) found that people drinking 5–6 drinks daily before the pandemic had more significantly increased use during the pandemic.
3.5.6. Caregiving responsibilities
Caregiving responsibilities were associated with increased pandemic SU in nine studies (Boschuetz et al., 2020, Callinan et al., 2021, Czeisler et al., 2020, Gadermann et al., 2021, Grossman et al., 2020, Rodriguez et al., 2020, Rossinot et al., 2020, Sallie et al., 2020, Vanderbruggen et al., 2020), and less reduction in SU in another (Zajacova et al., 2020). Having children at home was related to increased overall consumption (Callinan et al., 2021, Gadermann et al., 2021, Grossman et al., 2020, Rodriguez et al., 2020, Rossinot et al., 2020, Sallie et al., 2020, Vanderbruggen et al., 2020), higher AUDIT scores (Boschuetz et al., 2020, Sallie et al., 2020), number of drinks per occasion (Rodriguez et al., 2020), number of drinks consumed weekly (Sallie et al., 2020), and greater number of heavy drinking episodes (Rodriguez et al., 2020). The odds of consuming more alcohol during lockdown also increased as the number of children at home increased (OR = 1.22 for every one child [CI: 1.15, 1.30], p < 0.001) (Vanderbruggen et al., 2020). Having a child under 18 at home was also associated with more coping-related motives for drinking alcohol (Wardell et al., 2020). Among Americans who did not report SU in May 2020, unpaid caregivers for adults had 3.33 times the odds of reporting having started to use substances than others to cope with stress in June 2020 (CI: 1.75, 6.31, p < 0.001; Czeisler et al., 2020). Contrary to these results Chodkiewicz et al. (2020) found that people with children were more likely to reduce than increase their alcohol use and Weerakoon et al. (2020) found that households with children at home had 0.74 lower odds of binge drinking compared with households with no children (95% CI: 0.58, 0.94).
3.5.7. Employment
The impact of employment also demonstrated mixed results. No significant differences were found in six studies by employment status (Chodkiewicz et al., 2020, Rolland et al., 2020, Sidor and Rzymski, 2020, Villanueva et al., 2021, Weerakoon et al., 2020, Zajacova et al., 2020). Income loss, job loss, economic worries, and unemployment were found to be associated with increased rates of SU in five studies (Alpers et al., 2021, Killgore et al., 2021, Neill et al., 2020, Vanderbruggen et al., 2020, Wardell et al., 2020). Contrary to these results, two studies found unemployment was a protective factor for increased alcohol use (Rossinot et al., 2020, Szajnoga et al., 2020); Czeisler et al. (2020) reported that more employed people compared with unemployed people started or increased their use to cope with stress; and Grossman et al. (2020) reported that people stressed by spending more time at work increased their alcohol use. Two studies found that working or studying from home was associated with increased alcohol use (Alpers et al., 2021, Szajnoga et al., 2020), while another did not find a significant effect (Boschuetz et al., 2020).
3.5.8. COVID-19 infection and public health measures
Experiencing a COVID-19 infection (Garnett et al., 2021) or worrying about a relative’s health was associated with reduced alcohol use (Rossinot et al., 2020). However, the perceived threat of COVID-19 infection was positively associated with multiple measures of drinking (e.g., frequency, amount, severity; Rodriguez et al., 2020). Two studies found non-significant impacts of quarantine on alcohol use (Chodkiewicz et al., 2020, Sallie et al., 2020), while one found it was associated with increased alcohol use (Alpers et al., 2021) and one found those who were self-isolating alone had lower alcohol use than those not in isolation (Newby et al., 2020). The severity of and amount of time spent under public health measures, such as lockdown or social isolation appears to affect alcohol use. Huckle et al. (2020) found that drinkers consumed 13% more in the more severe Level 3 lockdown restrictions in the UK compared with Level 2, and Killgore et al. (2021) found that AUDIT scores increased month by month as lockdown continued with the lowest AUDIT scores observed during the first month. Conversely, López-Bueno et al. (2020) found that each week of lockdown in Spain was associated with a reduction in alcohol use.
3.5.9. Stress and coping
Ten studies found that psychological stress levels were associated with increased alcohol use (Alpers et al., 2021, Callinan et al., 2021, Grossman et al., 2020, Kriaucioniene et al., 2020, Neill et al., 2020, Oksanen et al., 2021, Rodriguez et al., 2020, Rossinot et al., 2020, Stanton et al., 2020, Taylor et al., 2021), while two studies found no association (Chodkiewicz et al., 2020, Đogaš et al., 2020). Garnett et al. (2021) found that significant stress about becoming sick with COVID-19 was independently associated with both drinking less (adjusted odds ratio (aOR) 1.26 [95%CI: 1.08, 1.48], p = 0.004) and drinking more (aOR 1.28 [95% CI: 1.10, 1.48], p < 0.001). However, significant stress about finances was only associated with more drinking (aOR 1.43 [95% CI: 1.24, 1.66], p < 0.001).
Types of coping strategies were related to increased alcohol use in three papers. Chodkiewicz et al. (2020) reported that people in the hazardous drinking group more often used denial coping strategies, and Wardell et al. (2020) found that coping motives were associated with increased alcohol consumption in the past 30 days, controlling for pre-COVID-19 alcohol use. Taylor et al. (2021) found motives related to coping were associated with higher AUDIT alcohol abuse and drug abuse scores; 26% of their sample reported they tried to cope with self-isolation by consuming more drugs or alcohol.
4. Discussion
The goal of our review was to identify how COVID-19 impacted the distribution of SU-related risks and behaviors. We identified 53 studies published by March 2021 that described the early impacts of COVID-19 on SU at a population level. Our review found evidence that there has been increased frequency, quantity and severity of SU, particularly alcohol use, among certain segments of the population in certain countries. However, as also corroborated by studies which appeared after our search deadline, in many countries there were more people decreasing than increasing their use (see the large population-based survey studies in 21 European countries: Kilian et al. (2021) and Manthey et al. (2021)).
The impact of COVID-19 appears to be minimal, or at least variable for the people represented by Tier 1, 2 and 3 in our NBP model. The changes within these groups seem to be dependent on the sub-population and their pre-pandemic drinking patterns (e.g., mostly at home etc.). Multiple studies found that both the proportion not drinking alcohol and the proportion of people drinking heavily increased, while the proportion of people who drank occasionally decreased, which may indicate a polarization based on different mechanisms: reduced availability of alcohol and drinking occasions, together with fewer resources available due to economic constraints may have led to a reduction for many, while increased stress including mental stress may have led to an increase, in particular among people who already consumed at heavy levels (e.g., Rehm et al., 2020). This seems to be similar to the mechanisms observed in other crises, such as the last great recession (Bor et al., 2013). Consistent with such mechanisms, Callinan et al. (2021) reported the greatest reduction in alcohol use was among people who drank most of their alcohol outside their home prior to the pandemic.
The clearest negative SU outcomes in the context of COVID-19 are among people categorized as needing Tier 4 and 5 services who have history of problems related to their substance use and concurrent disorders. Across multiple measurements, the studies we reviewed indicated that people who already drank in risky ways before the pandemic were more likely to increase their substance use during the pandemic (see additionally Barrio et al., 2021 published after our search closure). This may have significant implications for service planning. Additionally, as drinking to cope with stressful and negative emotions is associated with risk for developing alcohol-related problems (McPhee et al., 2020, Rodriguez et al., 2020), the association between coping motives and increased pandemic alcohol use may also result in an upward shift in drinking patterns among pre-pandemic drinkers at a moderate level of risk. Given the evidence suggesting an increase in SU among those who are more vulnerable to harm and association with psychosocial distress, anxiety and depression, and overall poor mental health, these factors may complicate the process of treatment and support. During the pandemic, although health care visits for all reasons have decreased significantly, visits specifically for mental health and substance use concerns have increased (Yang et al., 2020). Significant collaboration and coordination among SU and other health and social service sectors, including mental health services are clearly indicated (Rush, 2014).
Increased substance use during COVID-19 among those currently having suicidal thoughts is an important finding to investigate in future studies (Chodkiewicz et al., 2020). Having an alcohol use disorder increases the risk of committing suicide, and acute alcohol use is associated with greater risks of suicide attempts (Flensborg-Madsen et al., 2008, Borges et al., 2017). Although preliminary evidence does not show a significant increase in suicide rates during the pandemic (Pirkis et al., 2021), since the use of substances can act as a trigger of suicidal behavior, health systems need to increase screening and offer appropriate prevention and treatment to those having suicidal thoughts (Vijayakumar et al., 2011).
In order to meet the changing needs of a population, it is important to monitor the impact of disease outbreaks such as COVID-19 and the resulting public health measures, including considerations of gender, race, and socioeconomic status (Rehm et al., 2020, Vigo et al., 2020). Maintaining a focus on diversity and equity is an essential and too often neglected principle of treatment system planning and evaluation (Rush and Urbanoski, 2019). In the papers we reviewed, increased SU was associated with caregiving responsibilities. Although not all studies showed a significant impact of gender on increased SU, higher stress is linked to unpaid caregiving for children and sick family members, which is often gendered (Rodriguez et al., 2020). The stress associated with caregiving and the increased risk of domestic violence during lockdown may lead to increased SU among women and the need for trauma and gender-informed services (Australian Bureau of Statistics, 2020, Finlay and Gilmore, 2020). SU, particularly alcohol use, is also a well-known risk factor for violence perpetration, and domestic violence may be both exacerbated and hidden by the social isolation mandated by public health measures (van Gelder et al., 2020).
4.1. Limitations
The evidence in our review only includes papers published prior to April 2021. The vast majority of these studies were conducted within the first month or two of the pandemic and the associated public health measures at that time. It is unclear if these changes in SU will be maintained. There is some evidence that the initial increase at the start of the pandemic has lessened over time (López-Bueno et al., 2020, Wright et al., 2020), while other studies associate increased substance with longer and more severe public health restrictions (Huckle et al., 2020, Killgore et al., 2021). In addition to being a clear limitation in answering our research questions, the sheer lack of empirical work related to non-alcohol SU also signals a need for more research and population surveillance on which to base prevention and treatment policies and programming. The included studies were all conducted in high and upper middle-income countries, and there is no information from low-income countries that have been particularly impacted by COVID-19. We were also unable to review materials published in languages other than English, French and Spanish, and it is possible that we missed literature published in other languages.
Additionally, more information is required to describe SU behavior across the entire population that includes standardized measures of frequency and quantity consumed, as would be accomplished with the use of the AUDIT. Most of the studies used non-representative samples gathered through convenience and snowball sampling methods. Very few papers tell us anything about severity, reporting only on the proportion of the population that increased or decreased use, but not providing any indication of the magnitude of the change. Although these studies provide preliminary data on changes in SU, without more information, the impact on treatment use is uncertain. It is also difficult to identify from the studies we reviewed the specific effect of different public health measures on SU. For example, in countries like Canada and Australia there was an increased availability of alcohol through delivery services despite decreased availability of on-site drinking. As a result, there is evidence of country-specific patterns of changes in SU due to the COVID-19 pandemic (Kilian et al., 2021).
Finally, the COVID-19 pandemic has been associated with increased opioid overdoses (Ali et al., 2021, Slavova et al., 2020, Special Advisory Committee on the Epidemic of Opioid Overdoses, 2021), and decreased access to harm-reduction services (Whitfield et al., 2020). Despite a number of brief communications on the converging public health crises of the opioid overdose epidemic and COVID-19 (see for example Alexander et al. (2020), Dunlop et al. (2020) and Khatri and Perrone (2020)), we did not identify any published evidence on the impact of the pandemic on the prevalence of opioid use or opioid use disorder at the population level.
5. Conclusions
Our review provides preliminary data on changes in substance use during the COVID-19 pandemic. This indicates that certain segments of the population increased their alcohol use, and may be at greater risk of harm and in need of additional services. In particular, people who already drank in risky ways before the pandemic were more likely to increase their substance use. Caregiving responsibilities, stress, depression, anxiety, and current treatment for a mental disorder were also found to be at associated with increased substance use. There continues to be a need for population-level information on SU and SUD by gender and age to inform evidence-based, rapid responses to the COVID-19 pandemic from a treatment system perspective.
Funding
This work was supported by Health Canada [Contribution Agreement #1920-HQ-000148].
CRediT authorship contribution statement
Rose A. Schmidt: conducted the systematic review and drafted the manuscript. Rosalie Genois: conducted the systematic review and drafted the manuscript. Jonathan Jin: conducted the systematic review and drafted the manuscript. Brian Rush: was instrumental in conceptualizing and directing the systematic review. Daniel Vigo: provided substantial comments and revisions. Jürgen Rehm: provided substantial comments and revisions. All authors discussed the results and contributed to the final manuscript.
Conflict of interest
No conflict declared.
Acknowledgments
This review was conducted as part of a project that received funding from Health Canada. The views represented here do not necessarily represent those of Health Canada.
Appendix. MHeS search strategy
Problem or patient or population
-
1.
addiction.mp. or substance abuse.mp. or exp Substance-Related Disorders/or drug dependance.mp.
-
2.
exp Drinking Behavior/or exp Alcohol Drinking/or exp Alcoholism/or alcohol.mp
-
3.
opioid.mp. or exp Analgesics, Opioid/or exp Heroin Dependence/or exp Heroin/or heroin.mp. or methadone.mp. or exp Methadone/or fentanyl.mp. or exp Fentanyl/
-
4.
marijuana.mp. or cannabis.mp. or exp Cannabis/
-
5.
cocaine.mp. or exp Cocaine-Related Disorders/or exp Cocaine/or exp Cocaine Smoking/or exp Crack Cocaine/or exp
-
6.
1 or 2 or 3 or 4 or 5
Exposure
-
7.
pandemic.mp. or exp Pandemics/or exp Coronavirus/or exp Coronavirus Infections/or Coronavirus.mp. or exp Middle East Respiratory Syndrome Coronavirus/or SARS virus.mp. or exp SARS Virus/or exp Severe Acute Respiratory Syndrome/or H1N1.mp. or Influenza A Virus, H1N1 Subtype or covid.mp
Outcome of interest
-
8.
exp Prevalence/or Prevalence.mp. or incidence.mp. or exp Incidence/or severity.mp.
-
9.
exp "Health Services Needs and Demand"/
-
10.
service planning.mp. or exp Health Planning/
-
11.
exp Substance Abuse Treatment Centers/ or addiction services.mp. or treatment.mp. or therapy.mp. or counseling.mp. or exp Counseling/
-
12.
opioid agonist treatment.mp. or exp Opiate Substitution Treatment/
-
13.
exp Substance Withdrawal Syndrome/ or withdrawal management.mp.
-
14.
exp "Utilization Review"
-
15.
8 or 9 or 10 or 11 or 12 or 13 or 14 or 15
Final search term
-
16.
6 and 7 and 15
References
- Ahmed M.Z., Ahmed O., Aibao Z., Hanbin S., Siyu L., Ahmad A. Epidemic of COVID-19 in China and associated psychological problems. Asian J. Psychiatry. 2020;51 doi: 10.1016/j.ajp.2020.102092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alexander G.C., Stoller K.B., Haffajee R.L., Saloner B. An epidemic in the midst of a pandemic: opioid use disorder and COVID-19. Ann. Intern. Med. 2020;173:57–58. doi: 10.7326/M20-1141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ali F., Russell C., Nafeh F., Rehm J., LeBlanc S., Elton-Marshall T. Changes in substance supply and use characteristics among people who use drugs (PWUD) during the COVID-19 global pandemic: a national qualitative assessment in Canada. Int. J. Drug Policy. 2021;93 doi: 10.1016/j.drugpo.2021.103237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alomo M., Gagliardi G., Peloche S., Somers E., Alzina P., Prokopez C.R. Psychological effects during the COVID-19 outbreak in Argentina. Rev. Fac. Cien. Med. Univ. Nac. Cordoba. 2020;77(3):176–181. doi: 10.31053/1853.0605.v77.n3.28561. [DOI] [PubMed] [Google Scholar]
- Alpers S.E., Skogen J.C., Mæland S., Pallesen S., Rabben Å.K., Lunde L.-H., Fadnes L.T. Alcohol consumption during a pandemic lockdown period and change in alcohol consumption related to worries and pandemic measures. Int. J. Environ. Res. Public Health. 2021;18(3):1220. doi: 10.3390/ijerph18031220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ammar A., Brach M., Trabelsi K., Chtourou H., Boukhris O., Masmoudi L., Bouaziz B., Bentlage E., How D., Ahmed M., Müller P., Müller N., Aloui A., Hammouda O., Paineiras-Domingos L.L., Braakman-Jansen A., Wrede C., Bastoni S., Pernambuco C.S., Mataruna L., Taheri M., Irandoust K., Khacharem A., Bragazzi N.L., Chamari K., Glenn J.M., Bott N.T., Gargouri F., Chaari L., Batatia H., Ali G.M., Bott O., Jarraya M., Abed K.E., Souissi N., Van Gemert-Pijnen L., Riemann B.L., Riemann L., Moalla W., Gómez-Raja J., Epstein M., Sanderman R., Schulz S.V., Jerg A., Al-Horani R., Mansi T., Jmail M., Barbosa F., Ferreira-Santos F., Šimunič B., Pišot R., Gaggioli A., Bailey S.J., Steinacker J.M., Souissi T., Hoekelmann A. Effects of COVID-19 home confinement on eating behaviour and physical activity: results of the ECLB-COVID19 international online survey. Nutrients. 2020:1583. doi: 10.3390/nu12061583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Australian Bureau of Statistics, 2020. 4940.0 – Household Impacts of COVID-19 Survey, 12–15 May 2020. 〈https://www.abs.gov.au/ausstats/abs@.nsf/mf/4940.0〉.
- Barbosa C., Cowell A.J., Dowd W.N. Alcohol consumption in response to the COVID-19 pandemic in the United States. J. Addict. Med. 2021;15:341–344. doi: 10.1097/ADM.0000000000000767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barker S.F., Best D., Manning V., Savic M., Lubman D.I., Rush B. A tiered model of substance use severity and life complexity: potential for application to needs-based planning. Subst. Abus. 2016;37(4):526–533. doi: 10.1080/08897077.2016.1143907. [DOI] [PubMed] [Google Scholar]
- Barrio P., Baldaquí N., Andreu M., Kilian C., Rehm J., Gual A., Manthey J. Abstinence among alcohol use disorder patients during the COVID-19 pandemic: insights from Spain. Alcohol. Clin. Exp. Res. 2021;45(4):802–807. doi: 10.1111/acer.14555. [DOI] [PubMed] [Google Scholar]
- Bartoszek A., Walkowiak D., Bartoszek A., Kardas G. Mental well-being (depression, loneliness, insomnia, daily life fatigue) during COVID-19 related home-confinement—a study from Poland. Int. J. Environ. Res. Public Health. 2020;17(20):7417. doi: 10.3390/ijerph17207417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borges G., Bagge C., Cherpitel C.J., Conner K., Orozco R., Rossow I. A meta-analysis of acute alcohol use and the risk of suicide attempt. Psychol. Med. 2017;47(5):949–957. doi: 10.1017/S0033291716002841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bor J., Basu S., Coutts A., McKee M., Stuckler D. Alcohol use during the great recession of 2008–2009. Alcohol Alcohol. 2013;48(3):343–348. doi: 10.1093/alcalc/agt002. [DOI] [PubMed] [Google Scholar]
- Boschuetz N., Cheng S., Mei L., Loy V.M. Changes in alcohol use patterns in the United States during COVID-19 pandemic. WMJ. 2020;119:171–176. [PubMed] [Google Scholar]
- Błaszczyk-Bębenek E., Jagielski P., Bolesławska I., Jagielska A., Nitsch-Osuch A., Kawalec P. Nutrition behaviors in Polish adults before and during covid-19 lockdown. Nutrients. 2020;12(10):3084. doi: 10.3390/nu12103084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Callinan S., Mojica‐Perez Y., Wright C.J., Livingston M., Kuntsche S., Laslett A.M., Room R., Kuntsche E. Purchasing, consumption, demographic and socioeconomic variables associated with shifts in alcohol consumption during the COVID‐19 pandemic. Drug Alcohol Rev. 2021;40(2):183–191. doi: 10.1111/dar.13200. [DOI] [PubMed] [Google Scholar]
- Callinan S., Smit K., Mojica‐Perez Y., D’Aquino S., Moore D., Kuntsche E. Shifts in alcohol consumption during the COVID‐19 pandemic: early indications from Australia. Addiction. 2020;116:1381–1388. doi: 10.1111/add.15275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Canadian Centre on Substance Use and Addiction, NANOS Research, 2020. COVID-19 and Increased Alcohol Consumption: NANOS Poll Summary Report. CCSA, Ottawa, ON.
- Chodkiewicz J., Talarowska M., Miniszewska J., Nawrocka N., Bilinski P. Alcohol consumption reported during the COVID-19 pandemic: the initial stage. Int. J. Environ. Res. Public Health. 2020;17:4677. doi: 10.3390/ijerph17134677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chu K.M., Marco J.L., Owolabi E.O., Duvenage R., Londani M., Lombard C., Parry C.D.H. Trauma trends during COVID-19 alcohol prohibition at a South African regional hospital. Drug Alcohol Rev. 2021;74:287. doi: 10.1111/dar.13310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Constant A., Conserve D.F., Gallopel-Morvan K., Raude J. Socio-cognitive factors associated with lifestyle changes in response to the COVID-19 epidemic in the general population: results from a cross-sectional study in France. Front. Psychol. 2020;11:1. doi: 10.3389/fpsyg.2020.579460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Czeisler M.É., Howard M.E., Robbins R., Barger L.K., Facer-Childs E.R., Rajaratnam S.M.W., Czeisler C.A. COVID-19: public compliance with and public support for stay-at-home mitigation strategies. medRxiv. 2020 doi: 10.1186/s12889-021-10410-x. 2020.2004.2022.20076141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Da B.L., Im G.Y., Schiano T.D. COVID-19 hangover: a rising tide of alcohol use disorder and alcohol-associated liver disease. Hepatology. 2020 doi: 10.1002/hep.31307. (Baltimore, Md.) (gbz, 8302946) [DOI] [PubMed] [Google Scholar]
- Degenhardt L., Charlson F., Ferrari A., Santomauro D., Erskine H., Mantilla-Herrara A., Whiteford H., Leung J., Naghavi M., Griswold M., Rehm J., Hall W., Sartorius B., Scott J., Vollset S.E., Knudsen A.K., Haro J.M., Patton G., Kopec J., Carvalho Malta D., Topor-Madry R., McGrath J., Haagsma J., Allebeck P., Phillips M., Salomon J., Hay S., Foreman K., Lim S., Mokdad A., Smith M., Gakidou E., Murray C., Vos T. The global burden of disease attributable to alcohol and drug use in 195 countries and territories: a systematic analysis for the global burden of disease study 2016. Lancet Psychiatry. 2018;5(12):987–1012. doi: 10.1016/S2215-0366(18)30337-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Đogaš Z., Lušić Kalcina L., Pavlinac Dodig I., Demirović S., Madirazza K., Valić M., Pecotić R. The effect of COVID-19 lockdown on lifestyle and mood in Croatian general population: a cross-sectional study. Croat. Med. J. 2020;61(4):309–318. doi: 10.3325/cmj.2020.61.309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dozois D.J.A. Anxiety and depression in Canada during the COVID-19 pandemic: a national survey. Can. Psychol./Psychol. Can. 2021;62(1):136–142. [Google Scholar]
- Dunlop A., Lokuge B., Masters D., Sequeira M., Saul P., Dunlop G., Ryan J., Hall M., Ezard N., Haber P., Lintzeris N., Maher L. Challenges in maintaining treatment services for people who use drugs during the COVID-19 pandemic. Harm Reduct. J. 2020;17(1):74. doi: 10.1186/s12954-020-00370-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eley, J., 2020. Record month for UK supermarkets as consumers spend extra £1.9bn, Financial Times.
- Every-Palmer S., Jenkins M., Gendall P., Hoek J., Beaglehole B., Bell C., Williman J., Rapsey C., Stanley J. Psychological distress, anxiety, family violence, suicidality, and wellbeing in New Zealand during the COVID-19 lockdown: a cross-sectional study. PLOS One. 2020;15(11) doi: 10.1371/journal.pone.0241658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrante G., Camussi E., Piccinelli C., Senore C., Armaroli P., Ortale A., Garena F., Giordano L. Did social isolation during the SARS-CoV-2 epidemic have an impact on the lifestyles of citizens? Epidemiol. Prev. 2020;44:353–362. doi: 10.19191/EP20.5-6.S2.137. [DOI] [PubMed] [Google Scholar]
- Finlay I., Gilmore I. Covid-19 and alcohol-a dangerous cocktail. BMJ (Clin. Res. Ed.) 2020;369:m1987. doi: 10.1136/bmj.m1987. (8900488,bmj, 101090866) [DOI] [PubMed] [Google Scholar]
- Flensborg-Madsen T., Knop J., Mortensen E.L., Becker U., Sher L., Grønbæk M. Alcohol use disorders increase the risk of completed suicide — irrespective of other psychiatric disorders. A longitudinal cohort study. Psychiatry Res. 2008;167(1):123–130. doi: 10.1016/j.psychres.2008.01.008. [DOI] [PubMed] [Google Scholar]
- Gadermann A.C., Thomson K.C., Richardson C.G., Gagné M., McAuliffe C., Hirani S., Jenkins E. Examining the impacts of the COVID-19 pandemic on family mental health in Canada: findings from a national cross-sectional study. BMJ Open. 2021;11(1) doi: 10.1136/bmjopen-2020-042871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garnett C., Jackson S., Oldham M., Brown J., Steptoe A., Fancourt D. Factors associated with drinking behaviour during COVID-19 social distancing and lockdown among adults in the UK. Drug Alcohol Depend. 2021;219 doi: 10.1016/j.drugalcdep.2020.108461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Gelder N., Peterman A., Potts A., O’Donnell M., Thompson K., Shah N., Oertelt-Prigione S. COVID-19: reducing the risk of infection might increase the risk of intimate partner violence. EClinicalMedicine. 2020;21 doi: 10.1016/j.eclinm.2020.100348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glowacz F., Schmits E. Psychological distress during the COVID-19 lockdown: the young adults most at risk. Psychiatry Res. 2020;293 doi: 10.1016/j.psychres.2020.113486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Górnicka M., Drywień M.E., Zielinska M.A., Hamułka J. Dietary and lifestyle changes during COVID-19 and the subsequent lockdowns among Polish adults: a cross-sectional online survey PLifeCOVID-19 study. Nutrients. 2020;12(8):2324. doi: 10.3390/nu12082324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grossman E.R., Benjamin-Neelon S.E., Sonnenschein S. Alcohol consumption during the COVID-19 pandemic: a cross-sectional survey of US adults. Int. J. Environ. Res. Public Health. 2020;17(24):9189. doi: 10.3390/ijerph17249189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huckle T., Parker K., Romeo J.S., Casswell S. Online alcohol delivery is associated with heavier drinking during the first New Zealand COVID‐19 pandemic restrictions. Drug Alcohol Rev. 2020 doi: 10.1111/dar.13222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson S.E., Garnett C., Shahab L., Oldham M., Brown J. Association of the COVID‐19 lockdown with smoking, drinking and attempts to quit in England: an analysis of 2019–20 data. Addiction. 2021;116(5):1233–1244. doi: 10.1111/add.15295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacob L., Smith L., Armstrong N.C., Yakkundi A., Barnett Y., Butler L., McDermott D.T., Koyanagi A., Shin J.I., Meyer J. Alcohol use and mental health during COVID-19 lockdown: a cross-sectional study in a sample of UK adults. Drug Alcohol Depend. 2021;219 doi: 10.1016/j.drugalcdep.2020.108488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khatri U.G., Perrone J. Opioid use disorder and COVID-19: crashing of the crises. J. Addict. Med. 2020 doi: 10.1097/ADM.0000000000000684. (101306759) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kilian, C., Rehm, J., Allebeck, P., Braddick, F., Gual, A., Barták, M., Bloomfield, K., Gil, A., Neufeld, M., O'Donnell, A., 2021. Alcohol Consumption During the COVID-19 Pandemic in Europe: A Large-Scale Cross-Sectional Study in 21 Countries (preprint). [DOI] [PubMed]
- Killgore W.D., Cloonan S.A., Taylor E.C., Lucas D.A., Dailey N.S. Alcohol dependence during COVID-19 lockdowns. Psychiatry Res. 2021;296 doi: 10.1016/j.psychres.2020.113676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koopmann A., Georgiadou E., Kiefer F., Hillemacher T. Did the general population in germany drink more alcohol during the COVID-19 pandemic lockdown? Alcohol Alcohol. 2020;55(6):698–699. doi: 10.1093/alcalc/agaa058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kriaucioniene V., Bagdonaviciene L., Rodríguez-Pérez C., Petkeviciene J. Associations between changes in health behaviours and body weight during the COVID-19 quarantine in Lithuania: the Lithuanian COVIDiet study. Nutrients. 2020;12(10):3119. doi: 10.3390/nu12103119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lau J.T.F., Yang X., Pang E., Tsui H.Y., Wong E., Wing Y.K. SARS-related perceptions in Hong Kong. Emerg. Infect. Dis. 2005;11(3):417–424. doi: 10.3201/eid1103.040675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- López-Bueno R., Calatayud J., Casaña J., Casajús J.A., Smith L., Tully M.A., Andersen L.L., López-Sánchez G.F. COVID-19 confinement and health risk behaviors in Spain. Front. Psychol. 2020;11:1426. doi: 10.3389/fpsyg.2020.01426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahadevan J., Shukla L., Benegal V. Alcohol controls in the aftermath of the COVID-19 pandemic in India: commentary on Stockwell et al. Drug Alcohol Rev. 2021;40(1):10–12. doi: 10.1111/dar.13158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manthey J., Kilian C., Carr S., Bartak M., Bloomfield K., Braddick F., Gual A., Neufeld M., O’Donnell A., Petruzelka B., Rogalewicz V., Rossow I., Schulte B., Rehm J. Use of alcohol, tobacco, cannabis, and other substances during the first wave of the SARS-CoV-2 pandemic in Europe: a survey on 36,000 European substance users. Subst. Abus. Treat. Prev. Policy. 2021;16(1):36. doi: 10.1186/s13011-021-00373-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKnight-Eily L.R., Okoro C.A., Strine T.W., Verlenden J., Hollis N.D., Njai R., Mitchell E.W., Board A., Puddy R., Thomas C. Racial and ethnic disparities in the prevalence of stress and worry, mental health conditions, and increased substance use among adults during the COVID-19 pandemic—United States, April and May 2020. Morb. Mortal. Wkly. Rep. 2021;70(5):162. doi: 10.15585/mmwr.mm7005a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McPhee M.D., Keough M.T., Rundle S., Heath L.M., Wardell J.D., Hendershot C.S. Depression, environmental reward, coping motives and alcohol consumption during the COVID-19 pandemic. Front. Psychiatry. 2020:11. doi: 10.3389/fpsyt.2020.574676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neill E., Meyer D., Toh W.L., van Rheenen T.E., Phillipou A., Tan E.J., Rossell S.L. Alcohol use in Australia during the early days of the COVID-19 pandemic: initial results from the COLLATE project. Psychiatry Clin. Neurosci. 2020;74(10):542–549. doi: 10.1111/pcn.13099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newby J.M., O’Moore K., Tang S., Christensen H., Faasse K. Acute mental health responses during the COVID-19 pandemic in Australia. PLOS One. 2020;15(7) doi: 10.1371/journal.pone.0236562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niedzwiedz C.L., Green M.J., Benzeval M., Campbell D., Craig P., Demou E., Leyland A., Pearce A., Thomson R., Whitley E., Katikireddi S.V. Mental health and health behaviours before and during the initial phase of the COVID-19 lockdown: longitudinal analyses of the UK household longitudinal study. J. Epidemiol. Community Health. 2021;75(3):224–231. doi: 10.1136/jech-2020-215060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oksanen A., Savolainen I., Savela N., Oksa R. Psychological stressors predicting increased drinking during the COVID-19 crisis: a longitudinal national survey study of workers in Finland. Alcohol Alcohol. 2021;56(3):299–306. doi: 10.1093/alcalc/agaa124. (Oxford, Oxfordshire) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ornell F., Moura H.F., Scherer J.N., Pechansky F., Kessler F., von Diemen L. The COVID-19 pandemic and its impact on substance use: implications for prevention and treatment. Psychiatry Res. 2020;7911385 doi: 10.1016/j.psychres.2020.113096. (qc4) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pirkis J., John A., Shin S., DelPozo-Banos M., Arya V., Analuisa-Aguilar P., Appleby L., Arensman E., Bantjes J., Baran A., Bertolote J.M., Borges G., Brečić P., Caine E., Castelpietra G., Chang S.-S., Colchester D., Crompton D., Curkovic M., Erlangsen A. Suicide trends in the early months of the COVID-19 pandemic: an interrupted time-series analysis of preliminary data from 21 countries. Lancet Psychiatry. 2021;8(7):579–588. doi: 10.1016/S2215-0366(21)00091-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollard M.S., Tucker J.S., Green H.D., Jr. Changes in adult alcohol use and consequences during the COVID-19 pandemic in the US. JAMA Netw. Open. 2020;3(9) doi: 10.1001/jamanetworkopen.2020.22942. e2022942-e2022942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rajkumar COVID-19 and mental health: a review of the existing literature. Asian J. Psychiatry. 2020;52 doi: 10.1016/j.ajp.2020.102066. 102066-102066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rehm J., Kilian C., Ferreira-Borges C., Jernigan D., Monteiro M., Parry C.D.H., Sanchez Z.M., Manthey J. Alcohol use in times of the COVID 19: implications for monitoring and policy. Drug Alcohol Rev. 2020;39(4):301–304. doi: 10.1111/dar.13074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodriguez L.M., Litt D.M., Stewart S.H. Drinking to cope with the pandemic: the unique associations of COVID-19-related perceived threat and psychological distress to drinking behaviors in American men and women. Addict. Behav. 2020;110 doi: 10.1016/j.addbeh.2020.106532. 106532-106532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rolland B., Haesebaert F., Zante E., Benyamina A., Haesebaert J., Franck N. Global changes and factors of increase in caloric/salty food intake, screen use, and substance use during the early COVID-19 containment phase in the general population in france: survey study. JMIR Public Health Surveill. 2020;6(3) doi: 10.2196/19630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rossinot H., Fantin R., Venne J. Behavioral changes during COVID-19 confinement in france: a web-based study. Int. J. Environ. Res. Public Health. 2020;17(22):8444. doi: 10.3390/ijerph17228444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rush B. Tiered frameworks for planning substance use service delivery systems: origins and key principles. Nord. Stud. Alcohol Drugs. 2010;27(6):617–636. [Google Scholar]
- Rush B. Evaluating the complex: alternative models and measures for evaluating collaboration among substance use services with mental health, primary care and other services and sectors. Nord. Stud. Alcohol Drugs. 2014;31(1):27–44. [Google Scholar]
- Rush B., Tremblay J., Babor T.F. Needs-based planning for substance use treatment systems: the new generation of principles, methods, and models. J. Stud. Alcohol Drugs Suppl. 2019;Suppl. 18:S5–S8. doi: 10.15288/jsads.2019.s18.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rush B., Tremblay J., Brown D. Development of a needs-based planning model to estimate required capacity of a substance use treatment system. J. Stud. Alcohol Drugs Suppl. 2019;Suppl. 18:S51–S63. doi: 10.15288/jsads.2019.s18.51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rush B., Urbanoski K. Seven core principles of substance use treatment system design to aid in identifying strengths, gaps, and required enhancements. J. Stud. Alcohol Drugs Suppl. 2019;18(Suppl. 18):S9–S21. doi: 10.15288/jsads.2019.s18.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sallie S.N., Ritou V., Bowden-Jones H., Voon V. Assessing international alcohol consumption patterns during isolation from the COVID-19 pandemic using an online survey: highlighting negative emotionality mechanisms. BMJ Open. 2020;10(11) doi: 10.1136/bmjopen-2020-044276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scarmozzino F., Visioli F. Covid-19 and the subsequent lockdown modified dietary habits of almost half the population in an Italian sample. Foods. 2020;9(5):675. doi: 10.3390/foods9050675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharecare, 2020. Flatten the Curve: Survey Results.
- Sidor A., Rzymski P. Dietary choices and habits during COVID-19 lockdown: experience from Poland. Nutrients. 2020;12(6):1657. doi: 10.3390/nu12061657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sinha R., Fox H.C., Hong K.A., Bergquist K., Bhagwagar Z., Siedlarz K.M. Enhanced negative emotion and alcohol craving, and altered physiological responses following stress and cue exposure in alcohol dependent individuals. Neuropsychopharmacology. 2009;34(5):1198–1208. doi: 10.1038/npp.2008.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slavova S., Rock P., Bush H.M., Quesinberry D., Walsh S.L. Signal of increased opioid overdose during COVID-19 from emergency medical services data. Drug Alcohol Depend. 2020;214 doi: 10.1016/j.drugalcdep.2020.108176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Special Advisory Committee on the Epidemic of Opioid Overdoses . Opioid- and Stimulant-Related Harms in Canada. Public Health Agency of Canada; Ottawa: 2021. [Google Scholar]
- Stanton R., To Q.G., Khalesi S., Williams S.L., Alley S.J., Thwaite T.L., Fenning A.S., Vandelanotte C. Depression, anxiety and stress during COVID-19: associations with changes in physical activity, sleep, tobacco and alcohol use in Australian adults. Int. J. Environ. Res. Public Health. 2020;17(11):4065. doi: 10.3390/ijerph17114065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szajnoga D., Klimek-Tulwin M., Piekut A. COVID-19 lockdown leads to changes in alcohol consumption patterns. Results from the Polish national survey. J. Addict. Dis. 2020:1–12. doi: 10.1080/10550887.2020.1848247. [DOI] [PubMed] [Google Scholar]
- Taylor S., Paluszek M.M., Rachor G.S., McKay D., Asmundson G.J. Substance use and abuse, COVID-19-related distress, and disregard for social distancing: a network analysis. Addict. Behav. 2021;114 doi: 10.1016/j.addbeh.2020.106754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tran T.D., Hammarberg K., Kirkman M., Nguyen H.T.M., Fisher J. Alcohol use and mental health status during the first months of COVID-19 pandemic in Australia. J. Affect. Disord. 2020;277:810–813. doi: 10.1016/j.jad.2020.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vanderbruggen N., Matthys F., Van Laere S., Zeeuws D., Santermans L., Van den Ameele S., Crunelle C.L. Self-reported alcohol, tobacco, and cannabis use during COVID-19 lockdown measures: results from a web-based survey. Eur. Addict. Res. 2020;26(6):309–315. doi: 10.1159/000510822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vigo D., Patten S., Pajer K., Krausz M., Taylor S., Rush B., Raviola G., Saxena S., Thornicroft G., Yatham L.N. Mental health of communities during the COVID-19 pandemic. Can. J. Psychiatry. 2020 doi: 10.1177/0706743720926676. 0706743720926676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vijayakumar L., Kumar M.S., Vijayakumar V. Substance use and suicide. Curr. Opin. Psychiatry. 2011;24(3):197–202. doi: 10.1097/YCO.0b013e3283459242. [DOI] [PubMed] [Google Scholar]
- Villanueva V.J., Motos P., Isorna M., Villanueva V., Blay P., Vázquez-Martínez A. Impact of confinement measures on the Covid-19 pandemic on alcohol risk consumption. Rev. Esp. Salud Publica. 2021:95. [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., Ho R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health. 2020;17(5):1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wardell J.D., Kempe T., Rapinda K.K., Single A., Bilevicius E., Frohlich J.R., Hendershot C.S., Keough M.T. Drinking to cope during COVID‐19 pandemic: the role of external and internal factors in coping motive pathways to alcohol use, solitary drinking, and alcohol problems. Alcohol. Clin. Exp. Res. 2020;44(10):2073–2083. doi: 10.1111/acer.14425. [DOI] [PubMed] [Google Scholar]
- Weerakoon S.M., Jetelina K.K., Knell G. Longer time spent at home during COVID-19 pandemic is associated with binge drinking among US adults. Am. J. Drug Alcohol Abus. 2020 doi: 10.1080/00952990.2020.1832508. [DOI] [PubMed] [Google Scholar]
- Whitfield M., Reed H., Webster J., Hope V. The impact of COVID-19 restrictions on needle and syringe programme provision and coverage in England. Int. J. Drug Policy. 2020;83 doi: 10.1016/j.drugpo.2020.102851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winkler P., Formanek T., Mlada K., Kagstrom A., Mohrova Z., Mohr P., Csemy L. Increase in prevalence of current mental disorders in the context of COVID-19: analysis of repeated nationwide cross-sectional surveys. Epidemiol. Psychiatr. Sci. 2020:29. doi: 10.1017/S2045796020000888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winstock, A., 2020. Global Drug Survey, Special Edition on COVID-19. 〈https://www.globaldrugsurvey.com/wp-content/themes/globaldrugsurvey/assets/GDS_COVID-19-GLOBAL_Interim_Report-2020.pdf〉.
- Wright C.J.C., Livingston M., Dwyer R., Callinan S. Second, third, fourth COVID-19 waves and the ‘pancession’: we need studies that account for the complexities of how the pandemic is affecting alcohol consumption in Australia. Drug Alcohol Rev. 2020 doi: 10.1111/dar.13188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang J., Landrum M.B., Zhou L., Busch A.B. Disparities in outpatient visits for mental health and/or substance use disorders during the COVID surge and partial reopening in Massachusetts. Gen. Hosp. Psychiatry. 2020;67:100–106. doi: 10.1016/j.genhosppsych.2020.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zajacova A., Jehn A., Stackhouse M., Denice P., Ramos H. Changes in health behaviours during early COVID-19 and socio-demographic disparities: a cross-sectional analysis. Can. J. Public Health. 2020;111(6):953–962. doi: 10.17269/s41997-020-00434-y. [DOI] [PMC free article] [PubMed] [Google Scholar]