Abstract
Introduction
In the ongoing COVID-19 global pandemic, compliance to governmental orders is a challenge in the effort to contain the spread of the virus. A cross-sectional study of the Israeli population during the first wave of the outbreak is utilized to elucidate factors that enhance or impede public compliance to the governmental regulation of lockdown and illustrate the practical complexities of staying at home for an elongated time duration.
Methods
A structured questionnaire was utilized to investigate compliance with home isolation, factors that enhance and impede compliance, activities engaged during lockdown, personal resilience, and level of individual distress during the first wave of COVID-19 in Israel.
Results
The most salient factors for enhanced compliance were concern for family or self-health (63.4 % and 56.3 % respectively), while deterrence played little role (18.5 %). Desire to maintain a normal life and fear of economic loss were the most significant factors that impeded compliance. A negative correlation between the levels of resilience and distress symptoms (r = 0.318 p < .001), and a positive correlation between resilience and enhanced compliance with home isolation (r = 0.225 p < .001) were identified.
Conclusions
Utilizing tools for empowering the population rather than instilling fear or other deterrence measures are more effective approaches to increase compliance with governmental directives during the COVID-19 pandemic. Public health officials and authorities need to engage the public in resilience building activities, in order to promote compliance to isolation measures. These findings have valuable implications for authorities in ensuring compliance to current and potential future stay-at-home orders for outbreaks.
Keywords: COVID-19, Compliance, Lockdown, Pandemics, The public
1. Introduction
Management of pandemics and epidemics is dependent on the adherence of the civil societies to the rules, regulations and directives issued by the governmental and public health authorities. As pandemics may rapidly spread globally, the international community has a vested interest in understanding the factors that enhance or impede on the compliance with the varied measures directed at containing the spread of communicable diseases.
Originating in December 2019 in Wuhan, China, Coronavirus Disease 2019 (COVID-19), a viral respiratory disease, has quickly been transmitted in 188 countries. As of June 22, 2021,179 million [179, 171, 152] cases have been confirmed globally, and 3.8 million [3,882,709] reported deaths [1]. This novel and emerging illness was declared a pandemic by the World Health Organization (WHO) on March 11, 2020 [2] and has been characterized by its unique clinical features of varying severity, most frequently including fever, cough, fatigue and myalgia [3].
To respond to this outbreak, authorities worldwide have invoked rigorous and unprecedented public health measures to contain the virus from further spread. A vital component of the COVID-19 efforts is enforced home-isolation for non-essential workers [4]. To ensure the success and effectiveness of measures such as this, it is well acknowledged that governments and crisis managers rely fundamentally on the public's compliance [5,6]. While action taken top-down by a government, such as banning large gatherings, closing workplaces and educational institutions, establishing diagnostic facilities, and isolation of localities are imperative, these actions will have limited effect without the individuals' cooperation [[6], [7], [8], [9]]. Part of planning a successful disease-control response, is recognizing that all individuals must be willing and able to comply [9]. Without such considerations, high rates of noncompliance will undermine the possible benefits of any lockdown [9]. For this reason, it is essential to understand the factors that influence the public's behavior and compliance. Different theoretical frameworks, such as the health belief model (HBM) and protection motivation theory (PMT) offer insights into the mediation process of compliance [[10], [11], [12]].
Lessons from the implementation of large-scale home-isolations during the current and previous outbreaks, indicate that potential motivations and obstacles to compliance are many-fold. In Toronto, Canada during the Severe Acute Respiratory Syndrome (SARS) epidemic in early 2003, DiGiovanni et al. elucidated that compliance to isolation was often motivated by the aim to protect and reduce risk of transmission to loved ones and the community, while fear of the law played only a small role in encouraging individuals to comply with directives [13]. An additional study that similarly evaluated the self-isolated population in Toronto during the SARS outbreak, indicated that legal reasons were at play (such as receiving a fine), along with risk perception (a key construct from HBM and PMT), and socio-cultural factors (social pressure and “Civic Duty”) when deciding to comply. Nonetheless, the findings also revealed that preoccupation with ill health of loved ones impeded adherence, as the individuals felt obliged to attend to the medical and other vital needs of their loved one [14]. Fear of loss of income was a paramount obstacle discussed in both studies [13,14]. Similar findings were established in relation to compliance in Israel during the COVID-19 outbreak, in which the researchers Bodas and Peleg (2020), found that self-isolation compliance is highly influenced by compensation, where if a household's income during the self-isolation period is guaranteed, compliance with public health regulation can be expected to increase [15]. There was mixed evidence in regard to whether employment characteristics affected adherence to home-isolation for non-essential workers. For parents, who had taken leave from work to care for children, adherence was higher, and it was found that unemployed or low-waged people were more likely to adhere to isolation guidelines [16]. One of the most salient factors associated with adherence to isolation during SARS in Taiwan was higher awareness and knowledge about the pandemic and its respective protocols for isolation [17]. In response to the 2009 H1N1 outbreak in Australia, individuals who comprehended what isolation entailed had significantly higher compliance rates [18]. This study further signified that individuals comply when others are complying. When individuals started hearing rumors that others were not complying with the guidelines, they were more likely to proceed to break isolation measures themselves [18]. Differences in factors affecting adherence behavior amongst these populations may be a function of the unique backdrop of additional contributing factors, such as differences in cultural, social, economic, and political contexts which must be considered for a complete understanding to generate conclusions.
The loss of usual routine, and the reduction of social and physical contact with others during self-isolation has frequently been shown to have a myriad of detrimental psychosocial impacts [18], among them are a documented increase in distress, a feeling of loneliness, and boredom [13,19]. Boredom has specifically been cited as a disincentive to comply with regulations to self-isolate [19]. To occupy time and adapt to changes of routine, it has previously been acknowledged that social networking activities increase [20], and children spend less time doing physical activities and spend a greater allocation of time sleeping [21]. The experience of adults in terms of the practical complexities as well as the pastime activities during self-isolation remains under-researched. There is varied evidence for whether length of prescribed isolation affected compliance to protocols. The median isolation period for the SARS outbreak was 14 days, similar to that of the current pandemic [22].
In this study, we investigate the factors that most powerfully enhance and impede compliance to public health regulations, such as self-isolation in relation to the COVID-19 outbreak, as well as assess the practical complexities of staying at home for extended durations of time, among an adult population. We focus our analysis specifically on the state of Israel, which has been afflicted by eight hundred forty-eight thousand [840,079] confirmed cases and over 6000 deaths [6428] deaths as of June 22, 2020 [1].
2. Methods
2.1. Study design
Considering the importance of understanding the factors affecting public compliance with government regulations concerning the current COVID-19 crisis, a study was conducted during the first wave of the pandemic, in March 2020, when the population was directed to maintain lockdown. A sample of the Israeli population (N = 503) was employed to assess elements affecting compliance during the COVID-19 pandemic, as well as how individuals allocated their time during home-isolation. Recruiting participants to the study was conducted through an online internet panel company that consists of over 100,000 members, representing all geographic and demographic sectors of the Israeli population (http://www.ipanel.co.il/). A stratified sampling method was used, based on data published by the Israeli Central Bureau of Statistics in regard to age, gender, religiosity and geographic zones.
2.2. Participants
The sample size was determined based on OpenEpi (https://www.openepi.com/SampleSize), requiring 384 respondents. This was calculated based on the size of the Israeli population, accounting for 9 million people, as presented by the Israeli bureau of statistics. The study was conducted using a random internet sample of 503 participants who consented to participate voluntarily in the research. To partake in the study, the participants had to confirm their willingness to voluntarily participate in the study. The data was collected anonymously, following approval of the Ethics Committee of the Tel Aviv University (number 0001196-1 from March 23rd, 2020).
2.3. The study tool
The study was based on a structured questionnaire that included items and indices that were developed specifically for this study, except for two main elements: distress symptoms and personal resilience. The newly developed components of the questionnaire were designed based on a literature review of prior pandemics (such as SARS, Avian flu and H1N1 pandemic), as well as consultation with experts in the field of behavior of civil society. The developed scales were validated by 7 content experts, pilot tested among 25 individuals and revised prior to their distribution.
2.4. Type of isolations and levels of adherence
The components of the questionnaire consisted of several elements: 1) One item assessing individual association into one of the following groups: a) put in home isolation in light of Ministry of Health guidance for people returning from abroad or coming in contact with a confirmed COVID-19 patient, b) Maintain home isolation in light of the lockdown policy of all, except for essential workers, or c) Individual is an “essential worker” and therefore leaves for work. 2) One item assessing level of compliance with home isolation (“Extent to which you follow the instructions to stay at home” by a 5 point Likert scale, scaling from 1 = to a very small extent, to 5 = to a great extent.
2.5. Factors that enhance and impede compliance
Nine items assessing factors that enhanced compliance on a 5 point Likert scale, scaling from 1 = to a very small extent, to 5 = to a great extent (e.g. “directive from the Ministry of Health instructing to remain under lockdown” or “belief that lockdown protects my health”). Cronbach's Alpha for this index was α = 0.783.4) Nine items measuring factors that impeded compliance (e.g. “the fear of economic loss” or “lack of faith in the effectiveness of staying at home”). Cronbach's Alpha for this index was α = 0.795.
2.6. Activities during lockdown
Eleven items assessing the extent to which activities were engaged in during the lockdown on a 5 point Likert scale, scaling from 1 = to a very small extent, to 5 = to a great extent (e.g. “sports activities” or “household care”).
2.7. Personal resilience
Personal resilience was assessed by 10 items of the Connor-Davidson Resilience scale portraying feelings of ability and strength in face of adversity [23]. This is a validated tool widely used for assessing personal resilience; see previous work [24,25] The scale ranged on a 5 point Likert scale, from 0 = not true at all, to 4 = true almost all the time. (e.g. “I manage to adapt to changes” or “I can achieve my goals”. Cronbach's Alpha for this index was α = 0.875.
2.8. Level of distress
The level of individual distress symptoms during the lockdown was determined by 15 items about anxiety, boredom and distress, extracted from the Brief Symptom Inventory [26], similarly a widely used inventory [24,27]. The inventory was scaled from 1 = not at all, to 5 = to a great extent, (e.g. “how much do you suffer from feelings of fear “or “anger” during the lockdown). Cronbach's Alpha for this index was α = 0.906.
2.9. Demographics
Demographics were assessed by 11 items including gender, year of birth, place of residence, marital status, number of children, number of dependents, education, religion, degree of religiosity, employment status, and income.
2.10. Statistical analysis
Descriptive statistics were used to analyze the characteristics of the sample. Pearson correlations were used for analyzing the associations between resilience, distress, factors that enhance or impede compliance during lockdown. Multiple logistic regressions were used for determining the factors affecting compliance for staying at home. All statistical analyses were performed using SPSS software version 25. P-values lower than 0.05 were considered to be statistically significant.
3. Results
Table 1 presents the demographic characteristics of the survey population. The average age of the sampled persons is 40.5, with the age range being 18–70, with approximately half of them men, about 52 % are in relationships with children and about half define themselves as secular. About half of the sample reported having 1 to 3 children and half have an academic degree. In terms of income level, about a quarter reported being above average.
Table 1.
Study population characteristics.
| N = 503 | |
|---|---|
| Age | 40.5 ± 14.4 |
| Sex | |
| Male | 246 (48.9 %) |
| Female | 257 (51.1 %) |
| Marital status | |
| In relationship without children | 100 (19.9 %) |
| In relationship with children | 264 (52.5 %) |
| Not in a relationship and without children | 97 (19.3 %) |
| Not in a relationship with children | 42 (8.3 %) |
| Religiosity | |
| Secular | 261 (51.9 %) |
| Traditional | 157 (31.2 %) |
| Religious | 71 (14.1 %) |
| Orthodox | 14 (2.8 %) |
| Children | |
| None | 186 (37.0 %) |
| 1–3 | 151 (50.0 %) |
| 4+ | 66 (13.0 %) |
| Level of education | |
| Elementary school | 5 (1.0 %) |
| 12 years | 121 (24.1 %) |
| Professional education | 132 (26.2 %) |
| Bachelor's Degree | 158 (31.4 %) |
| Master Degree or Higher | 87 (17.3 %) |
| Income Level | |
| Below average | 118 (43.3 %) |
| Average | 160 (31.8 %) |
| Above average | 125 (24.9 %) |
The majority (97 %) of participants reported that they stayed at home resulting from the directive of the overall lockdown, while only 3 % reported that they were in home isolation in light of Ministry of Health (MOH) guidance for people who came in contact with a COVID-19 patient and/or returned from abroad. More than half (53.9 %) of the participants reported that they were very highly compliant, following strict guidelines to stay at home, 40.6 % reported being highly compliant while only 2.2 % reported that they do not comply with the guideline.
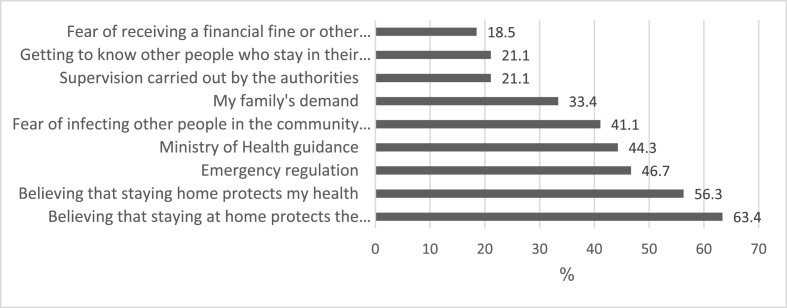
The major factor that enhanced compliance with the governmental directive to maintain home-isolation was the belief that staying at home protects the health of family (63.4 %) followed by the perception that staying home protects one's own health (56.3 %). The least common factor for compliance that was reported by the respondents was fear of receiving a financial fine or another type of punishment (18.5 %). See Fig. 1 .
Fig. 1.
Factors that enhance compliance to governmental directives during COVID-19 pandemic (to a great extent - 5).
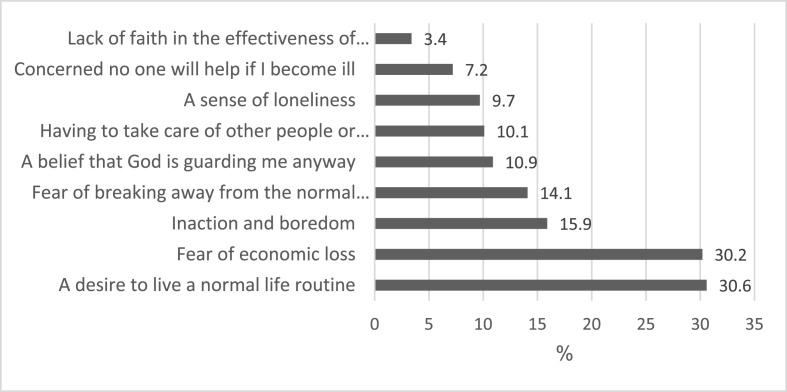
The major factors reported by the respondents that impeded compliance with the directive to maintain home-isolation was the desire to maintain a normal life routine (30.6 %), following by fear of economic loss (30.2 %). The least common factor was lack of faith in the effectiveness of the lockdown policy (3.4 %). See Fig. 2 .
Fig. 2.
Factors that impede compliance with governmental directive during COVID-19 pandemic (to a great extent - 5).
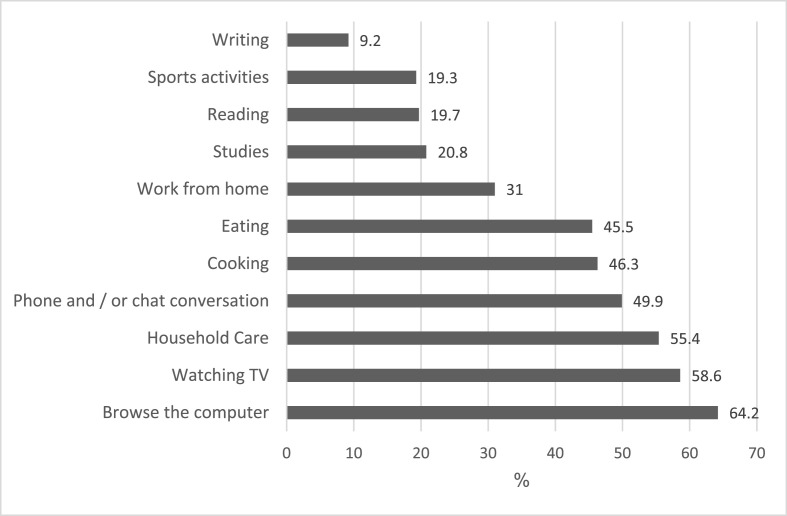
The participants were asked about the activities they performed during the lockdown. The most common activities were computer use (64.2 %), watching TV (58.6 %) and household care (55.4 %). See Fig. 3 .
Fig. 3.
Activities engaged in during home isolation (to a high or very high extent).
The mean levels of resilience and distress symptoms were found to be 2.65 ± 0.67 and 4.43 ± 0.74 respectively. A negative correlation was found between the levels of resilience and distress symptoms (r = 0.318 p < .001), while a positive correlation was identified between the resilience and factors that enhance compliance with home isolation (r = 0.225 p < .001). In addition, a positive correlation was found between distress symptoms and the factors that impede compliance with home isolation (r = 0.402 p < .001). This indicates that when the respondents reported higher levels of distress symptoms, they also reported a higher level of factors that impede their compliance with the directive to maintain home isolation. See Table 2 .
Table 2.
Correlations between resilience, distress symptoms, and factors that enhance or impede compliance with home isolation.1.
| Distress symptoms | Factors that enhance compliance | Factors that impede compliance | |
|---|---|---|---|
| Resilience | r = −.318 | r = .225 | r = .052 |
| p < .001 | p < .001 | p = .242 | |
| Distress symptoms | 1 | r = −.082 | r = .402 |
| p = .066 | p < .001 | ||
| Factors that enhance compliance | r = −.082 | 1 | r = .274 |
| p = .066 | p < .001 |
Notes: r value is the Pearson correlation coefficient measures that range from −1 to +1; p value or probability value of p < .05 indicates statistical significance.
Regression analysis was performed to predict the variables that impact the actual compliance with home isolation during lockdown. The following variables were entered into the model: age, gender, level of resilience, distress symptoms, factors that enhance compliance with home isolation and factors that impede with compliance with home isolation. The results of the regression analysis demonstrate that the only variable that predicted the actual compliance of maintaining home isolation is the index of the factors that enhance compliance (OR = 1.49,95 %CI 1.36–1.63). Nagelkerke R Square = 0.28 suggests that 28 % of the compliance with the directive to maintain home isolation is explained by the variables entered into the model. See Table 3 .
Table 3.
Results of regression analysis for predicting a high compliance to the guidelines to stay home.1.
| OR (95 %CI) | p-value | |
|---|---|---|
| Age | .99 (.98–1.00) | .49 |
| Gender | .72 (.49–1.08) | .12 |
| Resilience | .87 (.63–1.21) | .43 |
| Negative feeling | .75 (.54–1.04) | .09 |
| Factors that enhance compliance | 1.49 (1.36–1.63) | <.001 |
| Factors that impede compliance | .96 (.83–1.10) | .54 |
Nagelkerke R Square = 0.28.
OR refers to Odds Ratio, which is a measure of strength of association between two events in a population; CI, refers to confidence interval, which is a range of values that is likely to include a population parameter within a certain degree of confidence.
The strongest influencing components from which the measure of factors that enhance compliance to maintain home isolation was consisted of, were investigated. We found that the perception that maintaining home isolation protects the health of one's family is the strongest predictor (OR = 1.68, 95 %CI 1.09–2.58), followed by emergency regulation that requires oneself to stay home (OR = 1.64 95 %CI 1.17–2.31). The last component that was found as enhancing the compliance is the Ministry of Health's guidelines (OR 1.61 95 %CI 1.16–2.24). Nagelkerke R Square = 0.24 suggests that 24 % of complying to the directives of the authorities is explained by the variables entered to the model.
4. Discussion
Countries worldwide are facing remarkable challenges in implementing various measures to curb the spread of COVID-19. In light of global efforts to mitigate the impact of the pandemic, social isolation measures have been identified as a means to reduce the
likelihood of both contracting the virus and infecting others, and thus decelerating the spread of the virus [28]. Community-wide containment strategies of lockdown with stay-at-home orders have been invoked, however this tactic has proved complex to implement [29]. Therefore, it is of paramount importance to understand the factors that influence the public's compliance to isolation measures. To ensure the effectiveness of such measures, public compliance is key [[6], [7], [8], [9]]. With this agenda in mind, the current study investigates the contributing factors that influence compliance to isolation measures in Israel.
The findings of this investigation demonstrate several interesting phenomena. First, the results of the study suggest that the Israeli population tends to comply with isolation regulations. Similar findings were reported by Bodas and Peleg and de Brujin et al. [15,30]. This is an interesting finding as previous research has found that Israelis typically feel a lower sense of duty to be law abiding [31]. Furthermore, in line with the findings of DiGiovanni et al. from the SARS outbreak and more recently from research conducted in the United Kingdom during the COVID-19 outbreak, the results of this study indicate that compliance relies very little on deterrence or the threat of legal or financial repercussions by enforcement, but rather, the leading reason for complying to isolation measures is the belief that staying at home protects family health [12,13,32]. Concern for health of oneself similarly has proven to be a significant factor associated with willingness to comply with isolation measures. Both concern for family and self-health indicate that the naturally associated perceived fear of disease as a result of an outbreak may be sufficient to increase public compliance, without the need of additional fear induction or intimidation of the public. This is in line with the findings of Roma et al. (2020) which focused on the Italian population during the outbreak and found that compliance depended on individual's risk perception. Data from Hong Kong during the SARS outbreak and from the Netherlands during COVID-19 suggest similar conclusions [33,34]. These findings are in line with suggestions that empowerment over fear approaches are more effective for compliance [35].
In Israel, two additional national lockdowns had been instated (in September and December 2020). It is important to contextualize the conditions of the first Israeli lockdown as one where level of concern among the public was high, a consequence of the unfamiliarity and uncertainty with the crisis at hand. By government order, non-essential businesses were shut down and schools switched to distance teaching; many non-essential workers moved to work from home; sanctions were fines by the police (though only after repeated non-adherence fines were implemented); and the government issued an assurance that those that were on leave of absence will be financially compensated by the government for a temporary period of time [39]. The levels of compliance with the second and third lockdown, as reported by both the Israeli government and the media, were lower than what was seen in the first lockdown.
The most salient factors that impeded compliance were a desire to maintain a normal life routine and fear of economic loss. These results underscore the importance for authorities to take into consideration addressing people's concerns about their livelihood when putting in place restrictive measures such as lockdowns. Financial loss as a result of isolation measures may result in socioeconomic and psychological distress, including lasting anxiety and anger [6]. As similarly established by Bodas and Peleg, if authorities were to ensure monetary compensation for individuals in self-isolation due to lost wages, compliance can be significantly heightened. Additionally, as a result of the loss of usual routine and the necessary reduction in social and physical contact during self-isolation, boredom and inaction were a disincentive to comply with regulations. Similar findings have been identified during the SARS outbreak [13,14]. To ensure adaptation to changes in routine, individuals in self-isolation should be provided guidance on how to avoid boredom and with practical direction on how to cope with these changes. Our findings indicate that most individuals occupied their time through screen time (via the computer or television) and household care. While no other literature was found that evaluated comparatively what activities the adult population engages in during lockdowns, as expected, it has been found that during lockdown people increased their usage of digital media [36].
Lastly, the study identified that the higher the level of resilience of an individual, the less distress symptoms he or she felt. Correspondingly, when the individual felt less distress, they had more factors which resulted in compliance to stay at home during the lockdown. This observed positive association in this study is of utmost importance, as it is in line with the finding that resilience has been shown to play a significant role in the decision-making process for uptake of control measures [37,38]. Thus, there is sense in public health officials and authorities engaging the public in resilience building activities, in order to promote public compliance to isolation measures. Contrastingly, the found positive association between higher distress and the increased factors that impede compliance with home isolation indicate that authorities must take into consideration how to mitigate distress among the public. One such consideration may be addressing concerns of financial loss, as discussed above.
Three main limitations have been identified with regard to this study. The first is that participants were asked to self-report compliance levels, and thus the actual compliance cannot be verified. As in all studies based on questionnaires, social desirability bias cannot be ruled out with regard to the results found. In addition, because this study was conducted via the internet in order to ensure a rapid turnover of information collection, the study conclusions are limited to persons who have access to a source of internet and high computing skills and digital literacy. Lastly, because this study was conducted in Hebrew, members of the Israeli population who are not fluent in the language were unable to participate in this study.
5. Conclusion
The COVID-19 pandemic has substantially impacted on the global community, leading to prolonged and largely unprecedented measures of social distancing that were issued in the aim of containing the spread of the virus.
As the use of such a mechanism has substantial impacts on the civil society, socially, economically, psychologically and more, there is a need to understand the factors that most powerfully enhance and impede compliance to public health regulations, as well as assess the practical complexities of staying at home for extended durations of time, among an adult population. The study revealed that empowering the population and aiming to increase the resilience, in contrast to imposing fines or other types of ‘deterring” measures, are more effective in increasing compliance with governmental directives during the COVID-19 pandemic. Future research should explore additional factors that may influence compliance to mitigation strategies and identify the selection criteria adopted by individuals when deciding which measures to comply with.
6. Practical applications
These findings have generalizable and valuable implications for authorities in ensuring compliance to current and potential future stay-at-home orders for outbreaks. Governments and other authorities need to strengthen and empower the resilience of the public, including through economic assurance, social support or emergency guidance, rather than try to increase their fear or concern from the virus or impose monetary fines. More so, they need to engage the public in resilience building activities, in order to promote compliance to isolation measures.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.COVID-19 Map. 2020. https://coronavirus.jhu.edu/map.html
- 2.World Health Organization; 11 March 2020. WHO Director-General's opening remarks at the media briefing on COVID-19.https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 [Google Scholar]
- 3.Huang C., Wang Y., Li X., et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi: 10.1016/s0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wilder-Smith A., Freedman D.O. Isolation, quarantine, social distancing and community containment: pivotal role for old-style public health measures in the novel coronavirus (2019-nCoV) outbreak. J. Trav. Med. 2020;27(2) doi: 10.1093/jtm/taaa020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Leppin A., Aro A.R. Risk perceptions related to SARS and Avian influenza: theoretical foundations of current empirical research. Int. J. Behav. Med. 2009;16(1):7–29. doi: 10.1007/s12529-008-9002-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Webster R., Brooks S., Smith L., Woodland L., Wessely S., Rubin G. How to improve adherence with quarantine: rapid review of the evidence. Publ. Health. 2020;182:163–169. doi: 10.1016/j.puhe.2020.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Anderson R.M., Heesterbeek H., Klinkenberg D., Hollingsworth T.D. How will country-based mitigation measures influence the course of the COVID-19 epidemic? Lancet. 2020;395(10228):931–934. doi: 10.1016/s0140-6736(20)30567-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rothstein M.A., Talbott M.K. Encouraging compliance with quarantine: a proposal to provide job security and income replacement. Am. J. Public Health. 2007;97(Supplement_1) doi: 10.2105/ajph.2006.097303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rothstein M.A., Coughlin C.N. Ensuring compliance with quarantine by undocumented immigrants and other vulnerable groups: public health versus politics. Am. J. Public Health. 2019;109(9):1179–1183. doi: 10.2105/ajph.2019.305201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Smith L.E., Amlȏt R., Lambert H., Oliver I., Robin C., Yardley L., Rubin G.J. Factors associated with adherence to self-isolation and lockdown measures in the UK: a cross-sectional survey. Publ. Health. 2020 Oct 1;187:41–52. doi: 10.1016/j.puhe.2020.07.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Al-Sabbagh M.Q., Al-Ani A., Mafrachi B., Siyam A., Isleem U., Massad F.I., Alsabbagh Q., Abufaraj M. Predictors of adherence with home quarantine during COVID-19 crisis: the case of health belief model. Psychol. Health Med. 2021 Jan 10:1–3. doi: 10.1080/13548506.2021.1871770. [DOI] [PubMed] [Google Scholar]
- 12.Roma P., Monaro M., Muzi L., Colasanti M., Ricci E., Biondi S., Napoli C., Ferracuti S., Mazza C. How to improve compliance with protective health measures during the covid-19 outbreak: testing a moderated mediation model and machine learning algorithms. Int. J. Environ. Res. Publ. Health. 2020 Jan;17(19) doi: 10.3390/ijerph17197252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Digiovanni C., Conley J., Chiu D., Zaborski J. Factors influencing compliance with quarantine in Toronto during the 2003 SARS outbreak. Biosecur. Bioterrorism Biodefense Strategy, Pract. Sci. 2004;2(4):265–272. doi: 10.1089/bsp.2004.2.265. [DOI] [PubMed] [Google Scholar]
- 14.Cava M.A., Fay K.E., Beanlands H.J., Mccay E.A., Wignall R. Risk perception and compliance with quarantine during the SARS outbreak. J. Nurs. Scholarsh. 2005;37(4):343–347. doi: 10.1111/j.1547-5069.2005.00059.x. [DOI] [PubMed] [Google Scholar]
- 15.Bodas M., Peleg K. Self-isolation compliance in the COVID-19 era influenced by compensation: findings from A recent survey in Israel. Health Aff. 2020;39(6):936–941. doi: 10.1377/hlthaff.2020.00382. [DOI] [PubMed] [Google Scholar]
- 16.Porten K., Faensen D., Krause G. SARS outbreak in Germany 2003: workload of local health departments and their compliance in quarantine measures—implications for outbreak modeling and surge capacity? J. Publ. Health Manag. Pract. 2006;12(3):242–247. doi: 10.1097/00124784-200605000-00004. [DOI] [PubMed] [Google Scholar]
- 17.Hsu C.-C., Chen T., Chang M., Chang Y.-K. Confidence in controlling a SARS outbreak: experiences of public health nurses in managing home quarantine measures in Taiwan. Am. J. Infect. Contr. 2006;34(4):176–181. doi: 10.1016/j.ajic.2005.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kavanagh A.M., Bentley R.J., Mason K.E., et al. Sources, perceived usefulness and understanding of information disseminated to families who entered home quarantine during the H1N1 pandemic in Victoria, Australia: a cross-sectional study. BMC Infect. Dis. 2011;11(1) doi: 10.1186/1471-2334-11-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Brooks S.K., Webster R.K., Smith L.E., et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(10227):912–920. doi: 10.1016/s0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jeong H., Yim H.W., Song Y.-J., et al. Mental health status of people isolated due to Middle East Respiratory Syndrome. Epidemiol. Health. 2016;38 doi: 10.4178/epih.e2016048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Orgilés M., Morales A., Delvecchio E., Mazzeschi C., Espada J.P. 2020. Immediate Psychological Effects of the COVID-19 Quarantine in Youth from Italy and Spain. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.2020. Quarantine During an Epidemic of SARS. Medscape.https://www.medscape.com/viewarticle/463805 October 1. [Google Scholar]
- 23.Campbell-Sills L., Stein M.B. Psychometric analysis and refinement of the connor–davidson resilience scale (CD-RISC): validation of a 10-item measure of resilience. J. Trauma Stress. 2007;20(6):1019–1028. doi: 10.1002/jts.20271. [DOI] [PubMed] [Google Scholar]
- 24.Kimhi S., Eshel Y., Marciano H., Adini B. Distress and resilience in the days of COVID-19: comparing two ethnicities. Int. J. Environ. Res. Publ. Health. 2020 Jan;17(11) doi: 10.3390/ijerph17113956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yu X., Zhang J. Factor analysis and psychometric evaluation of the Connor-Davidson Resilience Scale (CD-RISC) with Chinese people. SBP (Soc. Behav. Pers.) 2007 Jan 1;35(1):19–30. [Google Scholar]
- 26.Maruish M.E., Savitz K.L., Derogatis L.R. Handbook of Psychological Assessment in Primary Care Settings. Lawrence Erlbaum Associates, Publishers; Mahwah, NJ: 2000. The SCL-90-R and Brief symptom inventory (BSI) in primary care; pp. 297–334. [Google Scholar]
- 27.Silver R.C., Holman E.A., McIntosh D.N., Poulin M., Gil-Rivas V. Nationwide longitudinal study of psychological responses to September 11. Jama. 2002 Sep 11;288(10):1235–1244. doi: 10.1001/jama.288.10.1235. [DOI] [PubMed] [Google Scholar]
- 28.Meidan D., Cohen R., Haber S., Barzel B. April 2020. An Alternating Lock-Down Strategy for Sustainable Mitigation of COVID-19. arXiv preprint. [Google Scholar]
- 29.Bruijn A.L.D., Feldman Y., Kuiper M.E., et al. 2020. Why Did Israelis Comply with COVID-19 Mitigation Measures during the Initial First Wave Lockdown. [DOI] [Google Scholar]
- 30.Yagil D., Rattner A. Crime Law Soc. Change. 2002;38(2):185–209. doi: 10.1023/a:1020254631369. [DOI] [Google Scholar]
- 31.Simpson S.S., Rorie M., Alper M., Schell‐Busey N., Laufer W.S., Smith N.C. Corporate crime deterrence: a systematic review. Campbell Syst. Rev. 2014;10(1):1–105. doi: 10.4073/csr.2014.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kooistra E.B., Folmer C.R., Kuiper M.E., et al. Mitigating COVID-19 in a nationally representative UK sample: personal abilities and obligation to obey the law shape compliance with mitigation measures. SSRN Electr. J. 2020 doi: 10.2139/ssrn.3598221. [DOI] [Google Scholar]
- 33.Lau J.T.F. Monitoring community responses to the SARS epidemic in Hong Kong: from day 10 to day 62. J. Epidemiol. Community Health. 2003;57(11):864–870. doi: 10.1136/jech.57.11.864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kuiper M.E., Bruijn A.L.D., Folmer C.R., et al. 2020. The Intelligent Lockdown: Compliance with COVID-19 Mitigation Measures in the Netherlands. [DOI] [Google Scholar]
- 35.Martin C. Empathy, equity, empowerment: using restorative practices to build character and community while reducing suspensions. VUE (Voices in Urban Education) 2015;42(2):14–18. doi: 10.33682/ndqh-6he5. [DOI] [Google Scholar]
- 36.Cellini N., Canale N., Mioni G., Costa S. Changes in sleep pattern, sense of time and digital media use during COVID‐19 lockdown in Italy. J. Sleep Res. 2020;29(4) doi: 10.1111/jsr.13074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kaim A., Jaffe E., Siman-Tov M., Khairish E., Adini B. Impact of a Brief educational intervention on knowledge, perceived knowledge, perceived safety, and resilience of the public during COVID-19 crisis. Int. J. Environ. Res. Publ. Health. 2020;17(16) doi: 10.3390/ijerph17165971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Stirling B.V., Harmston J., Alsobayel H. An educational programme for nursing college staff and students during a MERS- coronavirus outbreak in Saudi Arabia. BMC Nurs. 2015;14(1) doi: 10.1186/s12912-015-0065-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Last M. The first wave of COVID-19 in Israel—initial analysis of publicly available data. PloS One. 2020 Oct 29;15(10) doi: 10.1371/journal.pone.0240393. [DOI] [PMC free article] [PubMed] [Google Scholar]