Abstract
Background
Anemia remains a major public health issue, particularly for children and women in low- and middle-income countries (LMICs). However, the current prevalence and recent changes of anemia among young children and women of reproductive age, particularly for pregnant women in different trimesters are unclear. We examined the current prevalence of anemia among children aged less than 5 years by age (6-35 months vs. 36-59 months) and women of reproductive age by pregnant status (pregnant vs. non-pregnant) and trimesters (the third vs. the second vs. the first trimester) between 2010 and 2018 and further examined changes in the prevalence from 2000-2009 to 2010-2018.
Methods
Data were from the cross-sectional Demographic and Health Surveys performed between 2000 and 2018. A total of 47 countries were included to examine the current prevalence of anemia (weighted prevalence and 95% confidence interval [CI]) among young children aged less than 5 years (N = 459,785) and 46 countries among women of reproductive age (N = 1,079,805) between 2010 and 2018. To examine changes in the prevalence of anemia, a total of 29 countries with at least two Demographic and Health Surveys performed between 2000 and 2009 (children: N = 130,772; women: N = 371,845) and 2010-2018 (children: N = 386,202; women: N = 928,889) were included. Modified Poisson regression analyses with robust error variance were used to examine changes in anemia between 2000-2009 and 2010-2018 in participants by child age (6-5 months vs. 36-59 months), women pregnant status (pregnant vs. non-pregnant), trimesters (the second or third trimester vs. the first trimester) with the adjustment for potential covariates.
Findings
In 47 LMICs for children aged less than 5 years between 2010 and 2018, the total prevalence of anemia was 56.5% (95% CI 56.2, 56.8). Younger children aged 6-35 months were more likely to have anemia than older children aged 36-59 months (adjusted odds ratio [OR] 1.38, 95% CI 1.36-1.39, P < 0.001). In 46 LMICs for women of reproductive age, the total prevalence was 40.4% (95% CI 40.1, 40.7). Pregnant women were more likely to have anemia than non-pregnant women (adjusted OR 1.14, 1.12-1.16, P < 0.001). Moreover, pregnant women in the third trimester (adjusted OR 1.55, 1.48-1.62, P < 0.001) and the second trimester (adjusted OR 1.51, 1.45-1.58, P < 0.001) were more likely to have anemia than those in the first trimester. Among 29 included countries, although there was a decreasing change (absolute change, relative change, and average annual rate of reduction) in young children and women between 2000-2009 and 2010-2018 in a majority of countries, the current prevalence of anemia remained at a high level.
Interpretation
The prevalence of anemia among children aged less than 5 years and women of reproductive age was still high in LMICs, particularly for younger children and pregnant women. The relative change among women of reproductive age was far away from the WHO goal of reduction of anemia by 50% by 2025 (i.e., prevalence reduction to about 15.2% by 2025 from 30.3% at 2012 baseline). Continued and effective efforts, particularly for high-risk populations, are needed to improve the general health of the population.
Funding
Innovation Team of “Climbing” Program of Shandong University, and the Youth Team of Humanistic and Social Science of Shandong University (20820IFYT1902)
Research in context.
Evidence before this study
Several previous publications have examined the prevalence of anemia among non-pregnant women and children less than 5 years in low- and middle-income countries (LMICs). However, most studies were based on old data before 2011 or did not focus on specific populations, like pregnant women in different trimesters and infants and toddlers within the period from conception to 2 years of life.
Added value of this study
We examined the recent prevalence of anemia during 2010-2018 and found that 56.5% of children aged less than 5 years and 40.4% of women of reproductive age had anemia in 47 LMICs. The anemia was more prevalent and severe among younger children aged 6–35 months and pregnant women (particularly for the second and third trimesters vs. the first trimester) in most LMICs compared with older children aged 36-59 months and non-pregnant women. The relative decrease among women was far from the WHO goal of reduction by 50% by 2025 (i.e., prevalence reduction to about 15.2% by 2025 from 30.3% at 2012 baseline).
Implications of all the available evidence
Although some achievements have been made, the current situation of anemia in both children and women of reproductive age remains poor, and that in women is far below the WHO target. Continued efforts, particularly targeting high-risk populations including younger children and pregnant women, are needed to improve the anemia status in LMICs.
Alt-text: Unlabelled box
1. Introduction
Anemia, defined as the reduction of hemoglobin, contributes substantially to the global burden of chronic diseases. The World Health Organization (WHO) estimated that anemia affected 42% of young children aged less than 5 years and 40% of women of reproductive age globally in 2016 [1]. In recent decades, anemia has been a leading cause of years lived with disability among children aged less than 5 years and women [2,3].
Young children and women of reproductive age are two critical populations vulnerable to anemia. As a major cause of maternal and child morbidity and mortality, [4] anemia can cause adverse pregnancy outcomes (e.g., prematurity and fetal death), [5] impaired neurological development, impaired cardiac function, and undergrowth [6,7]. The World Health Assembly has established a nutrition goal that anemia in women should reduce by 50% by 2025 (i.e., prevalence reduction to about 15.2% by 2025 from 30.3% at 2012 baseline) [8].
Although previous studies have assessed the prevalence of anemia in non-pregnant women and children aged less than 5 years in low- and middle-income countries (LMICs), [9,10] relatively old data were used or specific populations were not targeted, like infants and toddlers within the period from conception to 2 years of life and different trimesters of pregnant women. The first 2 years of life are critical periods for child development when nutrients are easily deficient [11] and demands for iron are higher in the later trimester than former trimester among pregnant women [12]. In addition, children and pregnant women are more infected by malaria particularly in the region of African, which might be the main cause of iron deficiency [13,14]. Therefore, regular surveillance of the global epidemic status of anemia among children in the early years and pregnant women is needed to inform the development of intervention strategies.
In this study, we evaluated the prevalence of anemia among children aged less than 5 years and women of reproductive age in 47 LMICs, stratified by child age, pregnancy status of women, and pregnant trimesters using data from the Demographic and Health Surveys during 2010 and 2018. We further examined changes in the prevalence from 2000-2009 to 2010-2018.
2. Methods
2.1. Study design and study population
Data were from the nationally representative and cross-sectional Demographic and Health Surveys, which were available at https://dhsprogram.com/. This study adheres to the guidelines of the Strengthening the Reporting of Observational Studies in Epidemiology. Oral informed consent was provided by all participants or their guardians. The non-identifiable data are publicly available and there is no need for the ethical committee of Shandong University to grant access for use of these data.
We assessed the prevalence of anemia in children aged 6 to 59 months and women of reproductive age in 47 LMICs with complete data (1 country in 2010, 6 in 2011, 4 in 2012, 6 in 2013, 6 in 2014, 7 in 2015, 8 in 2016, 5 in 2017, 4 in 2018, respectively). In addition, to determine changes in the prevalence of anemia, we included 29 of the 47 countries (for the beginning of survey years: 6 countries in 2000, 2 in 2001, 1 in 2002, 2 in 2003, 4 in 2004, 8 in 2005, 2 in 2006, 1 in 2007, 2 in 2008, and 1 in 2009, respectively) which had two Demographic and Health Surveys during 2000–2009 and 2010–2018.
2.2. Information on hemoglobin and definition of anemia
Hemoglobin was tested through finger prick or heel prick blood tests among participants using the HemoCue blood hemoglobin testing system. The detailed process has been shown on the website: https://dhsprogram.com/topics/Anemia.cfm. Anemia was defined as the concentration of blood hemoglobin less than 110 g/L for pregnant women and children, and less than 120 g/L for non-pregnant women according to recommendations from the WHO [15]. The severity of anemia was classified as mild (children aged 6-59 months: 100-109 g/L; non-pregnant women: 110-119 g/L; pregnant women: 100-109 g/L), moderate (children aged 6-59 months: 70-99 g/L; non-pregnant women: 80-109 g/L; pregnant women: 70-99 g/L), and severe (children aged 6-59 months: less than 70 g/L; non-pregnant women: less than 80 g/L; pregnant women: less than 70 g/L) status based on age-specific cut-offs according to recommendations from the WHO [15].
2.3. Statistical analysis
The global, WHO regional, and national prevalence with 95% confidence intervals (95% CI) of anemia during 2010 and 2018 among children aged 6 to 59 months and women of reproductive age were calculated by considering sampling weights, strata, and primary sampling units from the Demographic and Health Surveys, as well as the subgroup analyses stratified by child age and pregnant status of women. The weighted national prevalence was calculated according to original sampling weights for each country, and the weighted global and regional prevalence was calculated by the rescaled weights to reduce the influence of large samples in the Demographic and Health Surveys with the consideration of the arbitrary differences in sample sizes across surveys. Chi-square test was used to compare the prevalence between groups. P-value < 0.0011 and < 0.0017 based on Bonferroni-adjusted alpha value of 47 countries and 29 countries (calculation of changes in the prevalence of anemia) respectively with non-overlapped 95% CIs indicate significant difference [16,17]. A modified Poisson regression analysis with robust error variance that used new indicators for strata, cluster, and sampling weight and the equation of “average annual rate of reduction [AARR]=1-EXP(β)” derived by United Nations International Children's Emergency Fund [UNICEF] (available at: https://data.unicef.org/resources/technical-note-calculate-average-annual-rate-reduction-aarr-underweight-prevalence/) were applied to estimate changes in prevalence of anemia between 2000-2009 and 2010-2018 in participants by child age, women pregnant status, and trimesters with the adjustment for potential variables including age, sex, wealth index (i.e., an indicator related to the socioeconomic status such as availability of community-level services and household ownership of selected assets), gross domestic product per capita on purchasing power parity, residence, country, and survey time and to estimate the association between periods and anemia at a national level with the adjustment for age and survey time. SAS version 9.4 (SAS Institute Inc, Cary, North Carolina) was used for all data analyses.
2.4. Role of funding sources
The funder of the study had no role in study design, data collection, data analyses, data interpretation, or writing of the report. The corresponding author (BX) had full access to all of the data and the final responsibility to submit for publication.
3. Results
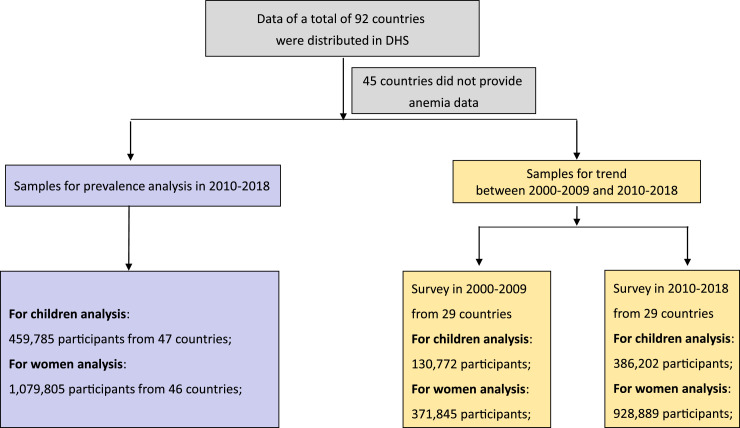
A total of 459,785 children aged 6 to 59 months and 1,079,805 women of reproductive age in the 47 countries were included in the analysis of prevalence during 2010–2018. 130,772 children aged 6 to 59 months and 371,845 women of reproductive age in 29 LMICs from 2000 to 2009 and 386,202 children and 928,889 women from 2010 to 2018 were included to examine changes in the prevalence of anemia (Fig. 1).
Fig. 1.
Flowchart of samples included in this study.
A total of 47 countries from 5 WHO regions were included in this study with 29 countries from the African region, 4 countries from the American region, 3 countries from the Eastern Mediterranean region, 4 countries from the European region, and 7 countries from the South-East Asia/Western Pacific region (Table S1).
3.1. Prevalence of anemia among children aged 6 to 59 months of age, 2010-2018
During 2010 and 2018, among 47 LMICs, the overall prevalence of anemia among children aged 6 to 59 months was 56.5%, higher among those aged 6 to 35 months (64.3%) than those aged 36 to 59 months (46.8%, P < 0.001). Younger children were more likely to have anemia than older children (adjusted odds ratio [OR] 1.38, 95% confidence intervals (CIs) 1.36-1.39, P < 0.001) (Table 1).
Table 1.
The weighted prevalence of anemia in children aged less than 5 years by age during 2010–2018 in 47 low- and middle-income countries.
| Group | % (95% CI) | Standard deviation | ORadj (95%CI) | P-valueadj |
|---|---|---|---|---|
| Children aged less than 5 years | ||||
| Total | 56.5 (56.2–56.8) | 17.1 | ||
| 6–35 months | 64.3 (63.9–64.7) | 16.5 | 1.38 (1.36–1.39) | <0.001 |
| 36–59 months (ref.) | 46.8 (46.3–47.3) | 18.2 | ||
| Women of reproductive age | ||||
| Total | 40.4 (40.1–40.7) | 14.8 | ||
| Pregnant women | 48.7 (47.9–49.5) | 15.4 | 1.14 (1.12–1.16) | <0.001 |
| Non-pregnant women(ref.) | 39.7 (39.4–40.0) | 14.8 | ||
| First trimester(ref.) | 35.2 (33.9–36.5) | 15.1 | ||
| Second trimester | 53.2 (52.0–54.4) | 16.9 | 1.51 (1.45–1.58) | <0.001 |
| Third trimester | 54.5 (53.2–55.8) | 15.9 | 1.55 (1.48–1.62) | <0.001 |
Adjusted OR (95%CI) and P-value adj were calculated with adjustment for sex, age, wealth index, residence, gross domestic product per capita on purchasing power parity, country, and survey time, with the group of 36–59 months as the reference. Data are shown as mean prevalence estimates and 95% confidence intervals.
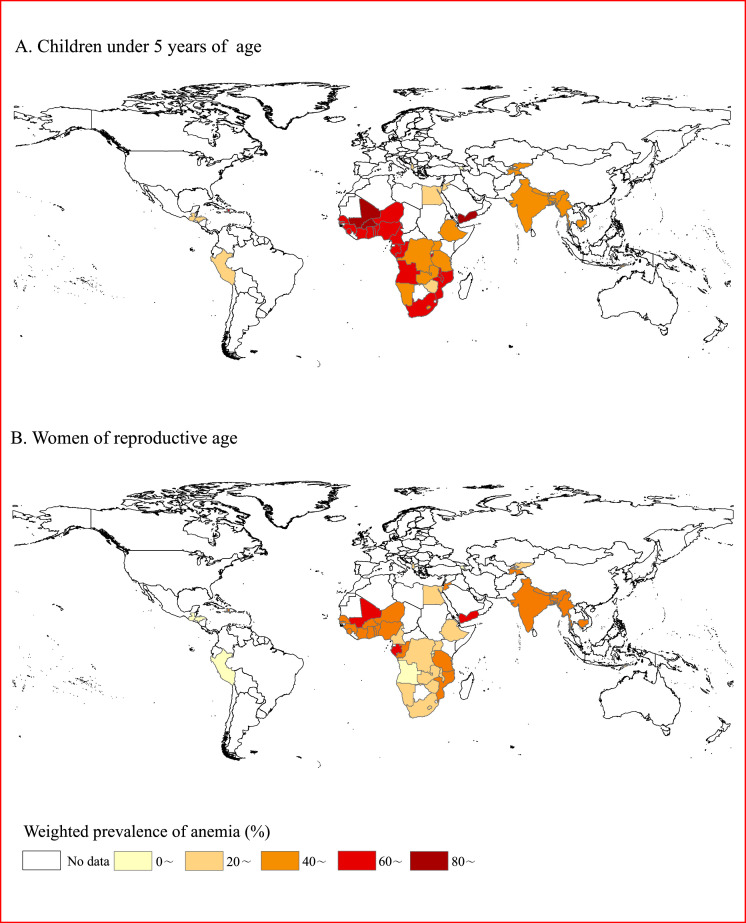
There was substantial heterogeneity across countries for the prevalence of anemia in children aged less than 5 years (African region: highest in Burkina Faso [87.7%] and lowest in Rwanda [36.5%]; American region: highest in Haiti [66.4%] and lowest in Honduras [29.1%]; Eastern Mediterranean: highest in Yemen [86.4%] and lowest in Egypt [27.2%]; European region: highest in the Kyrgyz Republic [42.5%] and lowest in Armenia [15.6%]; South-East Asia/Western Pacific: highest in India [58.5%] and lowest in Timor-Leste [40.3%], Fig. 2A and Table 2). When stratified by child age, more countries (32 countries: from 62.0% in Bangladesh to 92.8% in Burkina Faso) had a prevalence of anemia above 60% in younger children (aged 6–35 months) compared with older children (aged 36-59 months, 12 countries: from 60.2% in Nigeria to 81.4% in Burkina Faso, Table S1). The prevalence of anemia among children aged 6 to 59 months across different regions, income levels, and severity levels has been shown in Table S2.
Fig. 2.
Weighted national prevalence of anemia during 2010-2018; A, children aged less than 5 years; B, women of reproductive age. Note: deeper color represents a higher prevalence of anemia.
Table 2.
Weighted prevalence of anemia in children aged 6–59 months and women of reproductive age during 2010–2018 in each country.
| WHO Region, Country | World Bank Income | Survey year | Young children aged 6–59 months |
Women of reproductive age |
||||
|---|---|---|---|---|---|---|---|---|
| Sample size | No. of cases | Prevalence,% | Sample size | No. of cases | Prevalence,% | |||
| African | ||||||||
| Angola | UM | 2015 | 6854 | 4392 | 64.6 (62.5–66.7) | ― | ― | ― |
| Burkina Faso | LI | 2010 | 6286 | 5545 | 87.7 (86.6–88.8) | 8376 | 4033 | 48.8 (47.2–50.4) |
| Benin | LI | 2017 | 6253 | 4477 | 71.5 (69.9–73.1) | 8011 | 4618 | 57.7 (56.2–59.2) |
| Burundi | LI | 2016 | 5767 | 3410 | 61.0 (59.2–62.8) | 8539 | 3176 | 39.3 (37.7–40.9) |
| Congo Democratic Republic | LI | 2013 | 8266 | 5189 | 59.9 (57.6–62.2) | 9328 | 3775 | 38.4 (36.2–40.6) |
| Congo | LM | 2011 | 4457 | 2943 | 66.8 (64.1–69.5) | 5562 | 2941 | 54.2 (52.1–56.3) |
| Cote d'Ivoire | LM | 2011 | 3403 | 2547 | 74.9 (73.0–76.8) | 4678 | 2471 | 53.7 (51.4–56.0) |
| Cameroon | LM | 2011 | 5476 | 3365 | 60.4 (58.6–62.2) | 7815 | 3128 | 39.5 (37.9–41.1) |
| Ethiopia | LI | 2016 | 8525 | 5107 | 56.8 (54.3–59.3) | 14,489 | 3929 | 23.6 (22.0–25.2) |
| Gabon | UM | 2012 | 3849 | 2420 | 60.2 (57.8–62.6) | 5484 | 3202 | 60.6 (58.3–62.9) |
| Ghana | LM | 2014 | 2736 | 1878 | 65.9 (63.1–68.7) | 4704 | 1984 | 42.4 (40.5–44.3) |
| Gambia | LI | 2013 | 3422 | 2502 | 70.8 (68.4–73.2) | 4558 | 2811 | 59.0 (56.3–61.7) |
| Guinea | LI | 2018 | 3610 | 2656 | 74.6 (72.8–76.4) | 5262 | 2363 | 45.8 (44.0–47.6) |
| Lesotho | LM | 2014 | 1766 | 901 | 51.0 (47.9–54.1) | 3349 | 866 | 27.3 (25.3–29.3) |
| Mali | LI | 2018 | 4349 | 3464 | 81.8 (80.3–83.3) | 5090 | 3199 | 63.4 (61.4–65.4) |
| Malawi | LI | 2015 | 5276 | 3301 | 62.5 (60.6–64.4) | 7970 | 2690 | 32.7 (31.3–34.1) |
| Mozambique | LI | 2011 | 4923 | 3222 | 68.5 (66.4–70.6) | 13,537 | 7100 | 54.0 (52.4–55.6) |
| Nigeria | LM | 2018 | 11,230 | 7708 | 67.9 (66.5–69.3) | 14,750 | 8557 | 57.8 (56.7–58.9) |
| Niger | LI | 2012 | 4827 | 3590 | 73.4 (71.6–75.2) | 5050 | 2238 | 45.8 (43.5–48.1) |
| Namibia | UM | 2013 | 2342 | 1143 | 47.5 (44.9–50.1) | 4327 | 899 | 20.7 (19.3–22.1) |
| Rwanda | LI | 2014 | 3532 | 1264 | 36.5 (34.7–38.3) | 6692 | 1281 | 19.2 (18.0–20.4) |
| Sierra Leone | LI | 2013 | 5290 | 4229 | 79.9 (78.4–81.4) | 7848 | 3573 | 44.8 (42.4–47.2) |
| Senegal | LI | 2017 | 10,896 | 7991 | 70.9 (69.6–72.2) | 8013 | 4293 | 54.1 (52.2–56.0) |
| Togo | LI | 2013 | 3240 | 2277 | 70.2 (68.2–72.2) | 4802 | 2210 | 48.1 (46.3–49.9) |
| Tanzania | LI | 2015 | 9323 | 5358 | 57.8 (56.2–59.4) | 13,102 | 6092 | 44.8 (43.4–46.2) |
| Uganda | LI | 2016 | 4806 | 2578 | 52.9 (50.8–55.0) | 6031 | 1945 | 31.7 (30.2–33.2) |
| South Africa | UM | 2016 | 1160 | 705 | 61.5 (57.5–65.5) | 2974 | 945 | 33.2 (30.5–35.9) |
| Zambia | LM | 2018 | 8707 | 5004 | 58.0 (56.5–59.5) | 13,226 | 4020 | 31.1 (29.7–32.5) |
| Zimbabwe | LI | 2015 | 5326 | 1946 | 36.5 (34.8–38.2) | 9265 | 2531 | 26.8 (25.5–28.1) |
| American | ||||||||
| Guatemala | LM | 2014 | 10,943 | 3664 | 32.4 (31.0–33.8) | 25,422 | 3733 | 13.6 (12.9–14.3) |
| Honduras | LM | 2011 | 9560 | 2865 | 29.1 (27.8–30.4) | 21,594 | 3331 | 15.1 (14.4–15.8) |
| Haiti | LI | 2016 | 6092 | 4022 | 66.4 (64.6–68.2) | 9513 | 4561 | 49.0 (47.4–50.6) |
| Peru | UM | 2012 | 8974 | 3190 | 32.6 (31.2–34.0) | 24,273 | 4642 | 17.6 (16.8–18.4) |
| Eastern Mediterranean | ||||||||
| Egypt | LM | 2014 | 4702 | 1337 | 27.2 (25.4–29.0) | 7189 | 1720 | 25.2 (23.8–26.6) |
| Jordan | UM | 2017 | 8815 | 2934 | 31.6 (29.8–33.4) | 7110 | 3183 | 43.5 (41.3–45.7) |
| Yemen | LM | 2013 | 3892 | 3435 | 86.4 (84.9–87.9) | 4904 | 3674 | 71.4 (69.5–73.3) |
| European | ||||||||
| Albania | LM | 2017 | 2057 | 573 | 24.4 (21.9–26.9) | 10,461 | 2427 | 22.7 (21.4–24.0) |
| Armenia | LM | 2015 | 1373 | 220 | 15.6 (13.4–17.8) | 5807 | 788 | 13.4 (11.9–14.9) |
| Kyrgyz Republic | LI | 2012 | 4213 | 1822 | 42.5 (40.0–45.0) | 8048 | 2768 | 35.2 (33.5–36.9) |
| Tajikistan | LI | 2017 | 5496 | 2221 | 41.5 (39.2–43.8) | 10,618 | 4366 | 41.1 (39.3–42.9) |
| South-East Asia/Western Pacific | ||||||||
| Bangladesh | LI | 2011 | 2432 | 1254 | 51.2 (48.7–53.7) | 5666 | 2364 | 42.4 (40.6–44.2) |
| India | LM | 2015 | 220,487 | 126,602 | 58.5 (58.1–58.9) | 684,904 | 352,570 | 53.1 (52.9–53.3) |
| Myanmar | LM | 2015 | 4003 | 2181 | 57.8 (55.8–59.8) | 12,516 | 5629 | 46.5 (45.1–47.9) |
| Maldives | UM | 2016 | 2064 | 977 | 49.7 (47.1–52.3) | 6867 | 4016 | 63.0(61.1–64.9) |
| Nepal | LI | 2016 | 2232 | 1162 | 52.9 (50.2–55.6) | 6423 | 2609 | 40.8 (38.6–43.0) |
| Timor-Leste | LM | 2016 | 2041 | 794 | 40.3 (37.2–43.4) | 4268 | 887 | 22.7 (21.1–24.3) |
| Cambodia | LI | 2014 | 4512 | 2463 | 55.5 (53.5–57.5) | 11,390 | 4988 | 45.4 (44.2–46.6) |
LI: low-income countries; LM: low-middle-income countries; UM: upper-middle-income countries.
3.2. The weighted prevalence of anemia among women of reproductive age, 2010-2018
During 2010 and 2018, among 46 LMICs, the prevalence of anemia among women of reproductive age was 40.4%. Pregnant women (48.7%) were more likely to have anemia than non-pregnant women (39.7%) (adjusted OR 1.14, 95% CI 1.12–1.16, P < 0.001, Table 1). Pregnant women in the third trimester (54.5%, adjusted OR 1.55, 95% CI 1.48–1.62) and the second trimester (53.2%, adjusted OR 1.51, 95% CI 1.45–1.58, P < 0.001, Table 1) were more likely to have anemia than those in the first trimester (35.2%). Similar changes were observed at the national level (Fig. S1).
There was substantial heterogeneity across countries for the prevalence of anemia in women of reproductive age (African region: highest in Mali [63.4%] and lowest in Rwanda [19.2%]; American region: highest in Haiti [49.0%] and lowest in Honduras [15.1%]; Eastern Mediterranean: highest in Yemen [71.4%] and lowest in Egypt; European region: highest in Tajikistan [41.1%] and lowest in Armenia [13.4%]; South-East Asia/Western Pacific: highest in Maldives [63.0%] and lowest in Timor-Leste [22.7%] Fig. 2B and Table 2). When stratified by pregnancy status of women, more counties (9 countries: from 61.1% in Nigeria to 78.2% in Yemen) had a prevalence of anemia above 60% in pregnant women compared with non-pregnant women (4 countries including Yemen [70.4%], Maldives [63.1%], Mali [62.6%], and Gabon [60.9%]) (Table S1). The prevalence of anemia among women of reproductive age across different regions, income levels, and severity levels has been shown in Tables S3, S4.
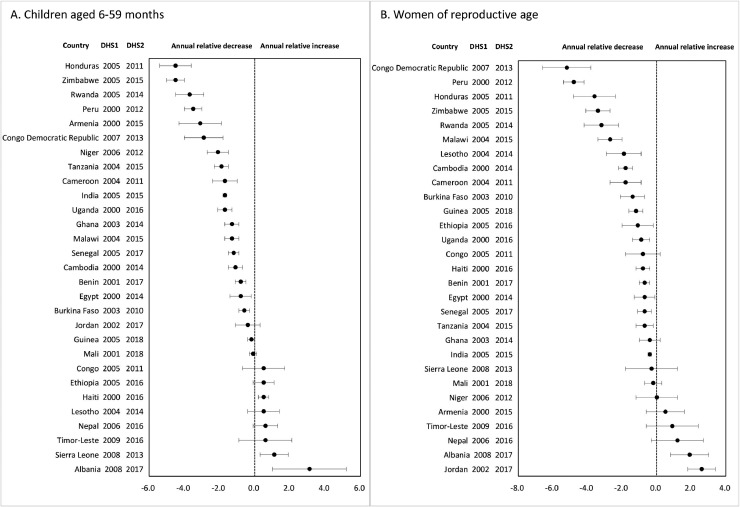
3.3. Changes in the prevalence of anemia among children less than 5 years of age and women of reproductive age in 29 LMICs, 2000-2009 to 2010-2018
At a national level, there were downward changes in the prevalence of anemia among children in 21 (of 29) LMICs and among women in 23 (of 29) LMICs. The AARR changed from 0.1% in Mali to 4.5% in Zimbabwe and Honduras among children, and from 0.2% in Mali and 0.3% in Sierra Leone to 5.2% in the Congo Democratic Republic among women (Table 3 and Fig. 3), which were similar to results of absolute downward change and relative change between 2000-2009 and 2010–2018. The AARR in anemia from 2000-2009 to 2010–2018 among children aged 6-35 months (ranging from −0.1% in Nepal to −4.3% in Honduras) and those aged 36–59 months (ranging from −0.4% in Mali to −6.3% in Zimbabwe) at the national level were shown in Fig. S2, changes among pregnant women (ranging from −0.1% in Mali to −5.3% in Congo Democratic Republic) and non-pregnant women (ranging from −0.2% in Mali to −5.2% in Congo Democratic Republic) shown in Fig. S3, and changes among pregnant women in different trimesters shown in Fig. S4 (first trimester: ranging from −0.3% in Mali to −10.3% in Zimbabwe; second trimester: from −0.1% in Benin to −6.0% in Congo Democratic Republic; third trimester: from −0.1% in Tanzania and Lesotho to −4.1% in Congo Democratic Republic). The change in anemia among children aged less than 5 years and women of reproductive age across different regions, income levels, and severity levels has been shown in Table S5 and Fig. S5.
Table 3.
Change in weighted prevalence of anemia in children aged 6–59 months and women of reproductive age from 2000 to 2009 to 2010–2018 in each country.
| WHO Region, Country | Survey year | Income | Children aged 6–59 months |
Women of reproductive age |
||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sample size | No. of cases | Prevalence,% | Absolute change,% | Relative change,% | P-value | Average annual rate of reduction (95%CI) | P-valuead | Sample size | No. of cases | Prevalence,% | Absolute change,% | Relative change,% | P-value | Average annual rate of reduction (95%CI) | P-cvalueadj | |||
| African | ||||||||||||||||||
| Benin | 2001 | LI | 2292 | 1876 | 81.9 (79.9–83.9) | 3124 | 2010 | 64.3 (62.0–66.6) | ||||||||||
| 2017 | LI | 6253 | 4477 | 71.5 (69.9–73.1) | −10.4 | −12.70% | <0.001 | −0.8 (−1.1,−0.6) | <0.001 | 8011 | 4618 | 57.7 (56.2–59.2) | −6.6 | −10.30% | <0.001 | −0.7 (−1.0,−0.4) | <0.001 | |
| Burkina Faso | 2003 | LI | 2770 | 2535 | 91.5 (90.1–92.9) | 4211 | 2244 | 53.7 (51.7–55.7) | ||||||||||
| 2010 | LI | 6286 | 5545 | 87.7 (86.6–88.8) | −3.8 | −4.20% | <0.001 | −0.6 (−0.9,−0.3) | <0.001 | 8376 | 4033 | 48.8 (47.2–50.4) | −4.9 | −9.10% | <0.001 | −1.4 (−2.1,−0.6) | <0.001 | |
| Cameroon | 2004 | LI | 3572 | 2461 | 68.2 (66.1–70.3) | 5137 | 2318 | 44.9 (43.1–46.7) | ||||||||||
| 2011 | LM | 5476 | 3365 | 60.4 (58.6–62.2) | −7.8 | −11.40% | <0.001 | −1.7 (−2.4,−1.1) | <0.001 | 7815 | 3128 | 39.5 (37.9–41.1) | −5.4 | −12.00% | <0.001 | −1.8 (−2.7,−0.9) | <0.001 | |
| Congo | 2005 | LM | 2021 | 1320 | 64.6 (61.0–68.2) | 3246 | 1856 | 57.0 (54.5–59.5) | ||||||||||
| 2011 | LM | 4457 | 2943 | 66.8 (64.1–69.5) | 2.2 | 3.40% | 0.353 | 0.5 (−0.7,1.7) | 0.404 | 5562 | 2941 | 54.2 (52.1–56.3) | −2.8 | −4.90% | 0.091 | −0.8 (−1.8,0.2) | 0.100 | |
| Congo Democratic Republic | 2007 | LI | 3566 | 2516 | 71.8 (68.2–75.4) | 4632 | 2316 | 53.0 (49.6–56.4) | ||||||||||
| 2013 | LI | 8266 | 5189 | 59.9 (57.6–62.2) | −11.9 | −16.60% | <0.001 | −2.9 (−4.0,−1.9) | <0.001 | 9328 | 3775 | 38.4 (36.2–40.6) | −14.6 | −27.50% | <0.001 | −5.2 (−6.6,−3.8) | <0.001 | |
| Ethiopia | 2005 | LI | 3616 | 1969 | 53.3 (51.0–55.6) | 5963 | 1654 | 26.6 (24.6–28.6) | ||||||||||
| 2016 | LI | 8525 | 5107 | 56.8 (54.3–59.3) | 3.5 | 6.60% | 0.04 | 0.5 (−0.1,1.1) | 0.102 | 14,489 | 3929 | 23.6 (22.0–25.2) | −3 | −11.30% | 0.026 | −1.1 (−2.0,−0.1) | 0.031 | |
| Ghana | 2003 | LI | 3240 | 2497 | 76.0 (74.2–77.8) | 5278 | 2395 | 44.6 (42.8–46.4) | ||||||||||
| 2014 | LM | 2736 | 1878 | 65.9 (63.1–68.7) | −10.1 | −13.30% | <0.001 | −1.3 (−1.7,−0.8) | <0.001 | 4704 | 1984 | 42.4 (40.5–44.3) | −2.2 | −4.90% | 0.089 | −0.4 (−1.0,0.1) | 0.117 | |
| Guinea | 2005 | LI | 2591 | 1969 | 76.6 (74.6–78.6) | 3881 | 2069 | 53.3 (51.2–55.4) | ||||||||||
| 2018 | LI | 3610 | 2656 | 74.6 (72.8–76.4) | −2 | −2.60% | 0.153 | −0.2 (−0.4,0.1) | 0.258 | 5262 | 2363 | 45.8 (44.0–47.6) | −7.5 | −14.10% | <0.001 | −1.2 (−1.6,−0.7) | <0.001 | |
| Lesotho | 2004 | LI | 1553 | 735 | 48.6 (45.3–51.9) | 3061 | 955 | 32.9 (30.6–35.2) | ||||||||||
| 2014 | LM | 1766 | 901 | 51.0 (47.9–54.1) | 2.4 | 4.90% | 0.31 | 0.5 (−0.4,1.5) | 0.260 | 3349 | 866 | 27.3 (25.3–29.3) | −5.6 | −17.00% | <0.001 | −1.9 (−2.9,−0.8) | <0.001 | |
| Malawi | 2004 | LI | 2303 | 1689 | 73.3 (71.0–75.6) | 2749 | 1234 | 44.3 (41.9–46.7) | ||||||||||
| 2015 | LI | 5276 | 3301 | 62.5 (60.6–64.4) | −10.8 | −14.70% | <0.001 | −1.3 (−1.7,−0.9) | <0.001 | 7970 | 2690 | 32.7 (31.3–34.1) | −11.6 | −26.20% | <0.001 | −2.7 (−3.4,−2.1) | <0.001 | |
| Mali | 2001 | LI | 2791 | 2321 | 82.8 (79.6–86.0) | 118,728 | 80,276 | 65.5 (61.3–69.7) | ||||||||||
| 2018 | LI | 4349 | 3464 | 81.8 (80.3–83.3) | −1 | −1.20% | 0.588 | −0.1 (−0.3,0.2) | 0.630 | 5090 | 3199 | 63.4 (61.4–65.4) | −2.1 | −3.20% | 0.377 | −0.2 (−0.7,0.2) | 0.316 | |
| Niger | 2006 | LI | 3589 | 2957 | 83.9 (82.0–85.8) | 4276 | 1885 | 45.8 (43.3–48.3) | ||||||||||
| 2012 | LI | 4827 | 3590 | 73.4 (71.6–75.2) | −10.5 | −12.50% | <0.001 | −2.1 (−2.7,−1.6) | <0.001 | 5050 | 2238 | 45.8 (43.5–48.1) | 0 | 0.00% | 0.981 | 0.0 (−1.2,1.3) | 0.990 | |
| Rwanda | 2005 | LI | 3583 | 1855 | 51.7 (49.5–53.9) | 5638 | 1428 | 25.6 (24.0–27.2) | ||||||||||
| 2014 | LI | 3532 | 1264 | 36.5 (34.7–38.3) | −15.2 | −29.40% | <0.001 | −3.7 (−4.5,−3.0) | <0.001 | 6692 | 1281 | 19.2 (18.0–20.4) | −6.4 | −25.00% | <0.001 | −3.2 (−4.2,−2.1) | <0.001 | |
| Senegal | 2005 | LI | 2742 | 2284 | 82.6 (80.5–84.7) | 4355 | 2609 | 59.1 (56.9–61.3) | ||||||||||
| 2017 | LI | 10,896 | 7991 | 70.9 (69.6–72.2) | −11.7 | −14.20% | <0.001 | −1.2 (−1.5,−0.9) | <0.001 | 8013 | 4293 | 54.1 (52.2–56.0) | −5 | −8.50% | 0.001 | −0.7 (−1.1,−0.3) | <0.001 | |
| Sierra Leone | 2008 | LI | 2516 | 1891 | 75.7 (73.2–78.2) | 3364 | 1509 | 45.2 (42.9–47.5) | ||||||||||
| 2013 | LI | 5290 | 4229 | 79.9 (78.4–81.4) | 4.2 | 5.50% | 0.004 | 1.1 (0.3,2.0) | 0.006 | 7848 | 3573 | 44.8 (42.4–47.2) | −0.4 | −0.90% | 0.796 | −0.3 (−1.8,1.3) | 0.738 | |
| Tanzania | 2004 | LI | 7284 | 5230 | 71.9 (70.1–73.7) | 10,132 | 5066 | 48.4 (46.3–50.5) | ||||||||||
| 2015 | LI | 9323 | 5358 | 57.8 (56.2–59.4) | −14.1 | −19.60% | <0.001 | −1.9 (−2.3,−1.6) | <0.001 | 13,102 | 6092 | 44.8 (43.4–46.2) | −3.6 | −7.40% | 0.007 | −0.7 (−1.2,−0.1) | 0.012 | |
| Uganda | 2000 | LI | 5403 | 3709 | 71.0 (68.7–73.3) | 6485 | 2250 | 36.7 (34.3–39.1) | ||||||||||
| 2016 | LI | 4806 | 2578 | 52.9 (50.8–55.0) | −18.1 | −25.50% | <0.001 | −1.7 (−2.1,−1.4) | <0.001 | 6031 | 1945 | 31.7 (30.2–33.2) | −5 | −13.60% | <0.001 | −0.9 (−1.4,−0.4) | 0.001 | |
| Zimbabwe | 2005 | LI | 4436 | 2561 | 58.4 (56.3–60.5) | 7893 | 2944 | 37.7 (35.8–39.6) | ||||||||||
| 2015 | LI | 5326 | 1946 | 36.5 (34.8–38.2) | −21.9 | −37.50% | <0.001 | −4.5 (−5.0,−3.9) | <0.001 | 9265 | 2531 | 26.8 (25.5–28.1) | −10.9 | −28.90% | <0.001 | −3.4 (−4.1,−2.7) | <0.001 | |
| American | ||||||||||||||||||
| Haiti | 2000 | LI | 3030 | 1804 | 62.1 (59.5–64.7) | 4778 | 2644 | 55.5 (52.8–58.2) | ||||||||||
| 2016 | LI | 6092 | 4022 | 66.4 (64.6–68.2) | 4.3 | 6.90% | 0.007 | 0.5 (0.2,0.8) | 0.002 | 9513 | 4561 | 49.0 (47.4–50.6) | −6.5 | −11.70% | <0.001 | −0.8 (−1.2,−0.4) | <0.001 | |
| Honduras | 2005 | LM | 9284 | 3537 | 37.2 (35.7–38.7) | 18,883 | 3457 | 18.7 (17.7–19.7) | ||||||||||
| 2011 | LM | 9560 | 2865 | 29.1 (27.8–30.4) | −8.1 | −21.80% | <0.001 | −4.5 (−5.4,−3.5) | <0.001 | 21,594 | 3331 | 15.1 (14.4–15.8) | −3.6 | −19.30% | <0.001 | −3.6 (−4.8,−2.3) | <0.001 | |
| Peru | 2000 | LM | 2334 | 1147 | 49.6 (46.8–52.4) | 6211 | 1929 | 31.6 (29.9–33.3) | ||||||||||
| 2012 | UM | 8974 | 3190 | 32.6 (31.2–34.0) | −17 | −34.30% | <0.001 | −3.5 (−4.0,−2.9) | <0.001 | 24,273 | 4642 | 17.6 (16.8–18.4) | −14 | −44.30% | <0.001 | −4.8 (−5.4,−4.2) | <0.001 | |
| Eastern Mediterranean | ||||||||||||||||||
| Egypt | 2000 | LM | 4786 | 1463 | 30.3 (28.6–32.0) | 7584 | 2109 | 27.7 (26.3–29.1) | ||||||||||
| 2014 | LM | 4702 | 1337 | 27.2 (25.4–29.0) | −3.1 | −10.20% | 0.014 | −0.8 (−1.4,−0.1) | 0.021 | 7189 | 1720 | 25.2 (23.8–26.6) | −2.5 | −9.00% | 0.014 | −0.7 (−1.3,−0.1) | 0.019 | |
| Jordan | 2002 | LM | 1510 | 531 | 34.5 (31.1–37.9) | 1831 | 530 | 29.1 (26.0–32.2) | ||||||||||
| 2017 | UM | 8815 | 2934 | 31.6 (29.8–33.4) | −2.9 | −8.40% | 0.134 | −0.4 (−1.1,0.4) | 0.350 | 7110 | 3183 | 43.5 (41.3–45.7) | 14.4 | 49.50% | <0.001 | 2.6 (1.8,3.4) | <0.001 | |
| European | ||||||||||||||||||
| Albania | 2008 | UM | 1404 | 263 | 17.4 (14.8–20.0) | 7467 | 1330 | 19.0 (17.5–20.5) | ||||||||||
| 2017 | LM | 2057 | 573 | 24.4 (21.9–26.9) | 7 | 40.20% | <0.001 | 3.1 (1.0,5.2) | 0.004 | 10,461 | 2427 | 22.7 (21.4–24.0) | 3.7 | 19.50% | <0.001 | 1.9 (0.8,3.1) | 0.001 | |
| Armenia | 2000 | LI | 1384 | 341 | 24.0 (21.7–26.3) | 6137 | 802 | 12.4 (11.4–13.4) | ||||||||||
| 2015 | LM | 1373 | 220 | 15.6 (13.4–17.8) | −8.4 | −35.00% | <0.001 | −3.1 (−4.3,−1.8) | <0.001 | 5807 | 788 | 13.4 (11.9–14.9) | 1 | 8.10% | 0.269 | 0.5 (−0.6,1.6) | 0.363 | |
| South-East Asia/Western Pacific | ||||||||||||||||||
| India | 2005 | LI | 37,999 | 24,486 | 69.4 (68.6–70.2) | 112,714 | 58,650 | 55.3 (54.7–55.9) | ||||||||||
| 2015 | LM | 220,487 | 126,602 | 58.5 (58.1–58.9) | −10.9 | −15.70% | <0.001 | −1.7 (−1.8,−1.6) | <0.001 | 684,904 | 352,570 | 53.1 (52.9–53.3) | −2.2 | −4.00% | <0.001 | −0.4 (−0.5,−0.3) | <0.001 | |
| Nepal | 2006 | LI | 4995 | 2388 | 48.6 (46.4–50.8) | 10,661 | 3718 | 36.2 (31.8–40.6) | ||||||||||
| 2016 | LI | 2232 | 1162 | 52.9 (50.2–55.6) | 4.3 | 8.80% | 0.014 | 0.6 (−0.1,1.4) | 0.090 | 6423 | 2609 | 40.8 (38.6–43.0) | 4.6 | 12.70% | 0.085 | 1.2 (−0.3,2.7) | 0.105 | |
| Timor-Leste | 2009 | LM | 2591 | 1070 | 38.5 (36.2–40.8) | 4117 | 911 | 21.3 (19.8–22.8) | ||||||||||
| 2016 | LM | 2041 | 794 | 40.3 (37.2–43.4) | 1.8 | 4.70% | 0.358 | 0.6 (−0.9,2.1) | 0.433 | 4268 | 887 | 22.7 (21.1–24.3) | 1.4 | 6.60% | 0.199 | 0.9 (−0.6,2.5) | 0.226 | |
| Cambodia | 2000 | LI | 1587 | 1015 | 63.4 (60.5–66.3) | 3666 | 2146 | 58.8 (56.7–60.9) | ||||||||||
| 2014 | LI | 4512 | 2463 | 55.5 (53.5–57.5) | −7.9 | −12.50% | <0.001 | −1.1 (−1.5,−0.6) | <0.001 | 11,390 | 4988 | 45.4 (44.2–46.6) | −13.4 | −22.80% | <0.001 | −1.8 (−2.2,−1.5) | <0.001 | |
P-Valueadj was calculated with adjustment for child or women age, child sex, wealth index, residence, gross domestic product per capita on purchasing power parity, country, and survey time.
LI: low-income countries; LM: low-middle-income countries; UM: upper-middle-income countries.
Fig. 3.
National change in weighted prevalence of anemia from 2000 to 2009 to 2010-2018; A, children aged less than 5 years; B, women of reproductive age.
4. Discussion
The prevalence of anemia was high among both children aged less than 5 years and women of reproductive age in 47 LMICs, particularly for younger children aged 6 to 35 months and pregnant women. Additionally, moderate and severe anemia was more prevalent among younger children and pregnant women in the second and third trimesters. The prevalence of anemia among children and women varied across countries. Although the prevalence decreased or did not change from 2000-2009 to 2010–2018 in both children and women in most LMICs, the absolute, relative, or AARR varied across countries and the relative change among women was far from the WHO goal.
In this study, the prevalence of anemia among women (40.4%) in the 47 LMICs was similar to the global prevalence in 2016 (40.0%); however, in children aged less than 5 years, it was higher (56.5%) than the global prevalence (42.0%) [1]. We further found that anemia was more prevent among younger children and pregnant women. The countries with a high prevalence of anemia (more than 60%) in this study were mainly from the African and South-East Asia/Western Pacific regions, which might be due to endemic schistosomiasis in the African region [18] and the Asian-Pacific region [19], [20], [21]. Besides, sickle cell disease is a common health problem for children living in Saharan Africa [22,23] and Asian, amplified by those with malaria susceptibility candidate locus [24] or migration [22]. Therefore, schistosomiasis and sickle cell disease might be the core mission of anemia mitigation in these two regions.
The worse status of anemia among younger children might be due to that the period from conception to 2 years of life is a critical window when the needs of nutrition must be ensured; if not, child morbidity or mortality may occur [11]. In the first 4–6 months of term-born infants, iron, as a major factor of anemia, is sufficient with unimpaired intrauterine supply, whereas after 6 months, owing to rapid growth (rapid brain development, physical growth, and early learning capacity), the iron supplied by intrauterine means becomes insufficient, that can cause absolute deficiency [25,26].
For women of reproductive age, we not only found a worse status of anemia among pregnant women compared with non-pregnant women (except for several countries, such as Jordan and Egypt in the Eastern Mediterranean region and Armenia in European region, which might be influenced by iron supplementation during pregnancy, socioeconomic factors, culture, and religion) but also observed that the prevalence was higher during the second and third trimesters than the first trimester. During pregnancy, the blood volume expands more than 1 liter [27] and the iron needs are tripled that of non-pregnancy [28]. The increase of plasma volume with the progress of pregnancy may greatly exceed change of red cell mass, leading to physiologic fall in hemoglobin concentration [29]. In addition, the demand for iron ensuring the growth of the placenta, fetus, and other maternal tissues increases from 0.8 mg/day during the first trimester to 7.5 mg/day during the third trimester [12]. On the other hand, the decrease of hepcidin (the regulator of iron bioavailability in the body) with the progress of pregnancy [30] might be the result of gradual iron deficiency to maximally absorb iron supplementation to maintain hemoglobin levels. The lower prevalence of anemia among pregnant women during the first trimester compared with that among non-pregnant women might be due to that most of those pregnant women may tend to adhere to iron supplementation [31] prescribed by clinical physician which partly mitigates anemia situation. However, iron supplementation might not meet the increased demands with the progress of pregnancy. Then, there will be a significant increase in anemia prevalence during the second and third trimesters. These findings suggest an urgent need for interventions targeting the cause of anemia in LMICs, particularly for infants and toddlers and pregnant women who have a high demand for iron.
Although there was an overall decline in the prevalence of anemia among women in LMICs, most countries maintained a high prevalence of anemia with the relative decrease of anemia far from the WHO goal of reduction by 50% by 2025 [8,32]. Besides, we found that the prevalence of anemia among children and women increased substantially in Albania (including absolute change and AARR), as well as that among women in Jordan. Albania faced urgent economical challenges that resulted in 57% of children under economic assistance failing to meet fundamental needs such as nutrition and cleaning drinking water [33]. Because of limited funding and ineffective management of supplies in most countries, interventions (e.g., iron-folic acid supplementation) might be not operating at scale [34] and the coverage of nutrition intervention in LMICs was low for women and young children [35]. These findings suggest that a comprehensive implementation plan of interventions should be strengthened and made a key component of a global nutrition framework in multiple sectors according to their specific situation.
Public health interventions that improve bioavailability and infant feeding practices, and increase dietary diversity recommended by the WHO include intake of micronutrients by supplementation or fortification with iron, vitamins, folic acid, and minerals, and delayed cord clamping [1,36]. Despite these recommendations, we observed only a minimal improvement in the prevalence of anemia in these LMICs. In all, co-operative efforts to establish interventions aimed at maintaining sufficient iron levels among women and children are needed to address the issues of basic causes like water, sanitation and hygiene, disease control, reproductive health, gender norms, lack of education, and poverty [1] to ensure effective, safe, and wide delivery to those at high risk.
This is the first study to examine the prevalence, and change in prevalence, of anemia among infants and toddlers and pregnant women across different trimesters in LMICs from 2010 onward. Moreover, the HemoCue blood hemoglobin testing system used in this study includes in-built quality control, ensuring the accuracy of the measurements. However, this study had several limitations. First, the prevalence of anemia was calculated based on 47 LMICs and changes of anemia from 2000-2009 to 2010–2018 were based on 29 LMICs; but further estimation with more LMICs is needed. Second, the information on serum ferritin, soluble transferrin receptor, and transferrin saturation was not available and information on iron status, malaria, inflammation, infection, sickle cell disease, and hemoglobinopathies was limited in the dataset, which may partly have affected the prevalence of anemia. Further surveys will be needed to better acquire the information using uniform questions. Third, results of changes in the prevalence of anemia between 2000-2009 and 2010–2018 in upper-middle-income countries should be interpreted with caution because of limited numbers of countries in these two periods (only 1 country in 2000–2009 and 2 countries in 2010–2018). Fourth, there might be heterogeneity between the two time periods when comparing the prevalence of anemia between 2000-2009 and 2010–2018. However, to ensure comparability and standardization across periods and countries, interviewers were well-trained and standardized measurement tools and questionnaires were applied to collect data [37]. Besides, we have used modified Poisson regression models to estimate changes in the prevalence at the national level with the adjustment for age and survey time to eliminate the effect. Fifth, the prevalence of anemia varied significantly across the WHO regions and the World Bank income levels; therefore, the comparisons across different levels should be interpreted with caution. Sixth, the information on iron supplementation was limited, which impeded us to explore the possible reasons for a higher prevalence of anemia among non-pregnant women than pregnant women in some countries. Further studies are needed to verify this issue.
The current prevalence of anemia in both young children and women among LMICs remains high, particularly for infants and toddlers and pregnant women in their second and third trimesters. Despite a decline in the prevalence of anemia among children and women in most LMICs, the relative decrease of anemia among women of reproductive age was well behind meeting the WHO goal. More effective intervention policies and programs in maintaining sufficient iron, especially targeting high-risk populations, are needed to improve the general health of the population.
Contributors
BX contributed to study design, interpretation of the data analysis and revised the manuscript. JS drafted the manuscript. HW analyzed the data and contributed to the interpretation of the data. CGM contributed to the interpretation of the data and revised the manuscript. MZ contributed to study design, the interpretation of the data and revised the manuscript. HW and JS accessed and verified the data. BX had full access to all the data in the study and had final responsibility for the decision to submit it for publication. The corresponding author BX has access to and responsibility for the raw data associated with the study.
Data sharing statement
Data from the Demographic and Health Surveys are publicly available online (https://dhsprogram.com/).
Declaration of Competing Interest
We declare no competing interests.
Acknowledgements
We thank US Agency for International Development and the DHS program team for sharing the valuable data.
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.eclinm.2021.101136.
Appendix. Supplementary materials
References
- 1.World Health Organization. Health Topic. Anemia. Geneva: World Health Organization; 2016. Available from: https://www.who.int/health-topics/anaemia#tab=tab_1. Accessed September 11, 2021.
- 2.Kassebaum N.J., Jasrasaria R., Naghavi M. A systematic analysis of global anemia burden from 1990 to 2010. Blood. 2014;123:615–624. doi: 10.1182/blood-2013-06-508325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.G. B.D., Disease and Injury Incidence and Prevalence Collaborators Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: a systematic analysis for the global burden of disease study 2017. Lancet. 2018;392:1789–1858. doi: 10.1016/S0140-6736(18)32279-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Smith C., Teng F., Branch E., Chu S., Joseph K.S. Maternal and perinatal morbidity and mortality associated with anemia in pregnancy. Obstet Gynecol. 2019;134:1234–1244. doi: 10.1097/AOG.0000000000003557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rahman M.M., Abe S.K., Rahman M.S. Maternal anemia and risk of adverse birth and health outcomes in low- and middle-income countries: systematic review and meta-analysis. Am J Clin Nutr. 2016;103:495–504. doi: 10.3945/ajcn.115.107896. [DOI] [PubMed] [Google Scholar]
- 6.Chaparro C.M., Suchdev P.S. Anemia epidemiology, pathophysiology, and etiology in low- and middle-income countries. Ann N Y Acad Sci. 2019;1450:15–31. doi: 10.1111/nyas.14092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Allali S., Brousse V., Sacri A.S., Chalumeau M., de Montalembert M. Anemia in children: prevalence, causes, diagnostic work-up, and long-term consequences. Expert Rev Hematol. 2017;10:1023–1028. doi: 10.1080/17474086.2017.1354696. [DOI] [PubMed] [Google Scholar]
- 8.World Health Organization. Global nutrition monitoring framework: operational guidance for tracking progress in meeting targets for 2025. Geneva: World Health Organization; 2017. Available from: https://www.who.int/publications/i/item/9789241513609. Accessed September 11, 2021.
- 9.Balarajan Y., Ramakrishnan U., Ozaltin E., Shankar A.H., Subramanian S.V. Anaemia in low-income and middle-income countries. Lancet. 2011;378:2123–2135. doi: 10.1016/S0140-6736(10)62304-5. [DOI] [PubMed] [Google Scholar]
- 10.Yang F., Liu X., Zha P. Trends in socioeconomic inequalities and prevalence of anemia among children and nonpregnant women in low- and middle-income countries. JAMA Netw Open. 2018;1 doi: 10.1001/jamanetworkopen.2018.2899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Christian P., Mullany L.C., Hurley K.M., Katz J., Black R.E. Nutrition and maternal, neonatal, and child health. Semin Perinatol. 2015;39:361–372. doi: 10.1053/j.semperi.2015.06.009. [DOI] [PubMed] [Google Scholar]
- 12.Milman N., Bergholt T., Byg K.E., Eriksen L., Graudal N. Iron status and iron balance during pregnancy. A critical reappraisal of iron supplementation. Acta Obstet Gynecol Scand. 1999;78:749–757. [PubMed] [Google Scholar]
- 13.Muriuki J.M., Mentzer A.J., Mitchell R. Malaria is a cause of iron deficiency in African children. Nat Med. 2021;27:653–658. doi: 10.1038/s41591-021-01238-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.van Eijk A.M., Hill J., Noor A.M., Snow R.W., Ter Kuile F.O. Prevalence of malaria infection in pregnant women compared with children for tracking malaria transmission in sub-Saharan Africa: a systematic review and meta-analysis. Lancet Glob Health. 2015;3:e617–e628. doi: 10.1016/S2214-109X(15)00049-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.World Health Organization . World Health Organization; Geneva: 2011. Haemoglobin concentrations for the diagnosis of anaemia and assessment of severity. Vitamin and mineral nutrition information system (VMNIS)https://www.who.int/vmnis/indicators/haemoglobin.pdf [Google Scholar]
- 16.Cumming G. Replication and p intervals: p values predict the future only vaguely, but confidence intervals do much better. Perspect Psychol Sci. 2008;3:286–300. doi: 10.1111/j.1745-6924.2008.00079.x. [DOI] [PubMed] [Google Scholar]
- 17.Hazra A., Gogtay N. Biostatistics series module 2: overview of hypothesis testing. Indian J Dermatol. 2016;61:137–145. doi: 10.4103/0019-5154.177775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.LoVerde P.T. Schistosomiasis. Adv Exp Med Biol. 2019;1154:45–70. doi: 10.1007/978-3-030-18616-6_3. [DOI] [PubMed] [Google Scholar]
- 19.Asundi A., Beliavsky A., Liu X.J. Prevalence of strongyloidiasis and schistosomiasis among migrants: a systematic review and meta-analysis. Lancet Glob Health. 2019;7:e236–ee48. doi: 10.1016/S2214-109X(18)30490-X. [DOI] [PubMed] [Google Scholar]
- 20.Buonfrate D., Bisanzio D., Giorli G. The global prevalence of strongyloides stercoralis Infection. Pathogens. 2020;9:468. doi: 10.3390/pathogens9060468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Paltridge M., Traves A. The health effects of strongyloidiasis on pregnant women and children: a systematic literature review. Trop Med Infect Dis. 2018;3:50. doi: 10.3390/tropicalmed3020050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rees D.C., Williams T.N., Gladwin M.T. Sickle-cell disease. Lancet. 2010;376:2018–2031. doi: 10.1016/S0140-6736(10)61029-X. [DOI] [PubMed] [Google Scholar]
- 23.Williams T.N. Sickle cell disease in Sub-Saharan Africa. Hematol Oncol Clin North Am. 2016;30:343–358. doi: 10.1016/j.hoc.2015.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gomez F., Tomas G., Ko W.Y. Patterns of nucleotide and haplotype diversity at ICAM-1 across global human populations with varying levels of malaria exposure. Hum Genet. 2013;132:987–999. doi: 10.1007/s00439-013-1284-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pizarro F., Yip R., Dallman P.R., Olivares M., Hertrampf E., Walter T. Iron status with different infant feeding regimens: relevance to screening and prevention of iron deficiency. J Pediatr. 1991;118:687–692. doi: 10.1016/s0022-3476(05)80027-7. [DOI] [PubMed] [Google Scholar]
- 26.Schumann K., Solomons N.W. Perspective: what makes it so difficult to mitigate worldwide anemia prevalence? Adv Nutr. 2017;8:401–408. doi: 10.3945/an.116.013847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.de Haas S., Ghossein-Doha C., van Kuijk S.M., van Drongelen J., Spaanderman M.E. Physiological adaptation of maternal plasma volume during pregnancy: a systematic review and meta-analysis. Ultrasound Obstet Gynecol. 2017;49:177–187. doi: 10.1002/uog.17360. [DOI] [PubMed] [Google Scholar]
- 28.Lopez A., Cacoub P., Macdougall I.C. Peyrin-Biroulet L. Iron deficiency anaemia. Lancet. 2016;387:907–916. doi: 10.1016/S0140-6736(15)60865-0. [DOI] [PubMed] [Google Scholar]
- 29.Sifakis S., Pharmakides G. Anemia in pregnancy. Ann N Y Acad Sci. 2000;900:125–136. doi: 10.1111/j.1749-6632.2000.tb06223.x. [DOI] [PubMed] [Google Scholar]
- 30.Achebe M.M., Gafter-Gvili A. How I treat anemia in pregnancy: iron, cobalamin, and folate. Blood. 2017;129:940–949. doi: 10.1182/blood-2016-08-672246. [DOI] [PubMed] [Google Scholar]
- 31.World Health Organization. Guideline: daily iron and folic acid supplementation in pregnant women. Geneva: World Health Organization; 2012. Available from: https://www.who.int/publications/i/item/9789241501996. Accessed September 11, 2021. [PubMed]
- 32.World Health Organization . World Health Organization; Geneva (Switzerland): 2014. Global nutrition targets 2025: anaemia policy brief.http://www.who.int/nutrition/globaltargets_indicators/en/ [Google Scholar]
- 33.Bali D., Kuli-Lito G., Ceka N., Godo A. Maternal and child health care services in Albania. J Pediatr. 2016;177S:S11–S20. doi: 10.1016/j.jpeds.2016.04.037. [DOI] [PubMed] [Google Scholar]
- 34.Trowbridge F., Martorell R. Summary and recommendations. J Nutr. 2002;132:875S–879S. doi: 10.1093/jn/132.4.875S. [DOI] [PubMed] [Google Scholar]
- 35.Lutter C.K., Daelmans B.M., de Onis M. Undernutrition, poor feeding practices, and low coverage of key nutrition interventions. Pediatrics. 2011;128:e1418–e1427. doi: 10.1542/peds.2011-1392. [DOI] [PubMed] [Google Scholar]
- 36.Sundararajan S., Rabe H. Prevention of iron deficiency anemia in infants and toddlers. Pediatr Res. 2020;89:63–73. doi: 10.1038/s41390-020-0907-5. [DOI] [PubMed] [Google Scholar]
- 37.ICF International . ICF International; Calverton. Maryland: 2012. Survey organization manual for demographic and health surveys. measure dhs. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.