Abstract
Allostatic load refers to wear and tear on the body due to repeated activation of the stress response and, thus, may be an early subclinical indicator of future disease and mortality risk. To date, few studies of allostatic load have focused on young adults, racial/ethnic comparisons that include Mexican Americans, or the interplay between race/ethnicity, gender, and educational attainment. To fill these gaps, we used data on non-Hispanic Black, non-Hispanic White, and Mexican-origin respondents from Waves I (1994–1995) and IV (2007–2008) of the National Longitudinal Study of Adolescent to Adult Health (Add Health; N = 11,807). We calculated allostatic load scores based on respondents’ values for 10 metabolic, cardiovascular, and inflammatory biomarkers measured at Wave IV, when respondents were 24–34 years old. We then used negative binomial regression models to assess the combined effects of race/ethnicity, gender, and educational attainment on allostatic load, while controlling for key covariates. We found that Black women had significantly higher allostatic load scores than White women and Black men, net of educational attainment and other covariates. Yet, education modified the relationship between race/ethnicity, gender, and allostatic load. Obtaining a college education was protective for White males and females but no more or less protective for other women and deleterious for Black males. In other words, by the time they reach young adulthood, the cumulative physiological burden of stress on Black women and college-educated Black men is already greater than it is among their similarly or less educated White counterparts. These findings provide important information about the intermediate physiological dysregulation that underlies social inequalities in stress-related health outcomes, especially those that occur at the intersections of race/ethnicity, gender, and educational attainment. They also suggest that research on its antecedents should focus on earlier life periods.
Keywords: Race, Gender, Education, Intersectionality, Allostatic load, Health disparities
Highlights
-
•
In a nationally representative sample of young adults, allostatic load varies by race/ethnicity, gender, and educational attainment.
-
•
Black women have higher allostatic load scores than others, net of educational attainment.
-
•
Educational attainment modifies the effects of race/ethnicity and gender on allostatic load.
-
•
College-educated Black men have higher allostatic load than less educated Black men.
1. Introduction
A large body of scholarly literature documents racial/ethnic, gender, and socioeconomic disparities in morbidity and mortality. In the social sciences and beyond, it is widely accepted that these disparities are rooted in broader social inequalities. Given this connection and the related conclusion that health disparities are, thus, avoidable and unfair, many scholars now use the term “health inequities” instead (Carter-Pokras 2002). Moreover, a growing amount of research has been devoted to uncovering the processes and mechanisms through which social inequalities translate into health inequities. A leading candidate is the stress process—i.e., the process whereby exposure to stress produces deleterious effects on mental and physical well-being if not mitigated by adaptive coping and social resources (Pearlin, 1989, Pearlin, 1999). Specifically, sociology of health scholars argue that differential exposure to stressful experiences is a key contributor to racial/ethnic, gender, and socioeconomic inequities in health (Thoits, 2010; Turner, 2013). This argument is rooted in sociological theories regarding the social patterning of the stress process (Pearlin, 1989, Pearlin, 1999). These theories posit that macro- and meso-level structural conditions perpetuate social inequalities that, in turn, generate differences in both exposure to stressors and access to stress buffers (Gee et al., 2019). Ample research provides support for these theories, frequently finding that members of disadvantaged social status groups (e.g., low socioeconomic status (SES), racial/ethnic minorities) experience greater exposure to chronic stress and have fewer adaptive coping and social resources to buffer the negative effects of stress on health (Thoits, 2010; Turner, 2013).1
An intersectionality perspective on this social stress process requires that we also consider the ways in which social statuses, e.g., race/ethnicity and gender, simultaneously structure exposure to social stressors and the lived experience2 of them (Collins 2000; Crenshaw, 1989). For example, Black women are simultaneously located at the bottom of both the race/ethnicity and gender hierarchies, which together contribute to their experience of “a double load of discrimination” (Borrell et al., 2006) and their lower class status (Elemelch and Lu 2004; Chang, 2006). These burdens are compounded by the social and economic consequences of being the daughters, partners, and mothers of Black men, who have disproportionately high rates of unemployment, incarceration, and premature mortality (U.S. Bureau of Labor Statistics, 2018; DeVuono-Powell et al., 2015; Xu et al., 2010). Moreover, the absence of personal and social resources to meet the demands of these stressors often leads Black women to engage in high effort coping which, together with the stressors themselves, could hasten the higher rates of stress-related health outcomes we find among them (Geronimus, 1992; Mullings & Wali, 2001; Read & Gorman, 2006; Warner & Brown, 2011). Interestingly, recent studies are beginning to find that the intersection of race/ethnicity and gender similarly disadvantages women of Mexican origin in the U.S., although the effects on their health are less pronounced than they are for Black women (Hummer & Gutin, 2018; Richardson & Brown, 2016). While some of the stressors experienced by Mexican-origin women overlap with those of Black women (e.g., racism- and SES-related stressors), they experience a unique set of stressors related to immigration and family matters (Viruell-Fuentes, 2007; Goodkind et al., 2008).
The assertions stemming from this intersectionality perspective on stress-related illness are consistent with Geronimus' (1992, 1996, 2001) weathering hypothesis, which was proposed to account for the observation that Black women's health begins to decline earlier in the life course than White women's health. Specifically, she argues that a number of race-related stressors (or “insults to health”), such as discrimination, racial differences in exposures to psychosocial or environmental hazards, and low SES, lead to accelerated aging (“weathering”)—i.e., an earlier onset and more rapid progression of health decline—among Black women compared to White women. Multiple studies have confirmed the age pattern described by the weathering hypothesis (e.g., Geronimus et al., 2006); however, tests of the hypothesized stressors or other pathogenic processes that precipitate the pattern are lacking. Nonetheless, the biological plausibility of such theories is widely acknowledged, given the known involvement of multiple physiological regulatory systems when the body responds to stress—i.e., the same systems in which dysregulation precipitates illness. However, operationalizing them—and, more specifically, confirming the process through which social stressors are theorized to “get under the skin” and produce health inequities—has been a challenge for social scientists and public health scholars alike.
The concept of allostatic load offers a response to this challenge. Indeed, allostatic load is now conceptualized to be a key mechanism by which the chronic stress of social disadvantage/discrimination translates into adverse health outcomes and inequities (Rodriquez, Kim, Sumner, Nápoles, & Pérez-Stable, 2019). Introduced over 20 years ago, allostatic load refers to physiological wear and tear on the body due to repeated activation of the stress response. When operationalized, it is considered to be a measure of the cumulative impact of social, psychological, or environmental stressors on the regulatory systems involved in the generalized physiological stress response (Crimmins & Seeman, 2004; McEwen, 1998; McEwen & Stellar, 1993). These systems include primary mediators of stress (i.e., cortisol, noradrenaline, epinephrine, and dehydroepiandrosterone sulfate (DHEA-S), which are rapidly released by the hypothalamic-pituitary-adrenal (HPA) axis in response to stress. Under normal conditions, the release of these primary mediators ceases after the response (i.e., after adaptation to the stressor is achieved). In the case of chronic or repeated stress, however, this adaptation process may fail, resulting in the continuous release of primary mediators. This flood, in turn, leads to the dysregulation of metabolic, inflammatory, and cardiovascular biomarkers, as evidenced by elevated blood pressures, cholesterol levels, and glycated hemoglobin levels (McEwen & Seeman, 1999). These secondary outcomes are antecedent to tertiary outcomes, such as cardiovascular disease, diabetes, decreased cognitive and physical functioning (Seeman et al., 1997, 2001), and increased risk for mortality (Juster et al., 2010). Thus, a high allostatic load level prior to the onset of secondary or tertiary outcomes may represent an early subclinical indicator of future disease and mortality risk. In fact, ample empirical support for this assertion has amassed during the last two decades (Beckie, 2012; Borrell et al., 2020).
The findings of prior research on social inequalities in allostatic load also overwhelmingly support the theory that chronic exposure to social stress increases physiological wear and tear on the body as evidenced by higher levels of allostatic load. Previous studies of racial/ethnic differences in allostatic load, for example, have consistently found higher allostatic load levels among non-Hispanic Blacks than among non-Hispanic Whites and people of Mexican origin (Peek et al., 2010; Rainisch & Upchurch, 2013)—a difference that persists when SES is taken into account (e.g., Chyu & Upchurch, 2018). Research on racial/ethnic differences in allostatic load also suggests that they are gendered. For example, in a nationally representative sample of women over 18 years old, Chyu and Upchurch (2011) found that Black women had the highest predicted allostatic load levels relative to women in other racial/ethnic groups; and foreign-born Mexican women had lower predicted allostatic load levels than U.S.-born Mexican women. Similarly, in Geronimus et al.’s (2006) study of age patterns of allostatic load scores among Black and White working-aged adults in the U.S., they found that Black females had the highest probability of high allostatic load compared to their same race male counterparts, White males, and White females. Bird et al. (2010) also found that Black females had higher allostatic load levels than their White and male counterparts.
A separate body of literature on SES differences in allostatic load also exists. Most studies have found a social gradient in allostatic load (i.e., an inverse graded relationship between SES and allostatic load) or simply that individuals with low SES have higher allostatic load levels than individuals with higher SES (Seeman et al., 2004, 2008; Gustafsson et al., 2011; Chyu & Upchurch, 2018). Bird et al. (2010) identified the same pattern, using a neighborhood-level measure of SES. Another study found that people who were persistently poor throughout their lives had higher allostatic load levels than others who had any periods of high SES in their lives (Gruenewald et al., 2012). However, the relationship between SES and allostatic load may be complicated by race/ethnicity (or vice versa). For example, in their analysis of racial/ethnic differences in allostatic load by education level, Howard and Sparks (2015) found that the largest differences were between college-educated Mexican Americans and Whites, and between college-educated non-Hispanic Blacks and Whites, and that there were no racial/ethnic differences at low levels of education.
To our knowledge, no previous studies of allostatic load have simultaneously treated measures of race/ethnicity, gender, and SES as focal variables in the analysis; they have either controlled for at least one of these three social status variables analytically or restricted its variability via exclusion (for example, samples that focus exclusively on women (e.g., Chyu & Upchurch, 2011, 2018), Hispanics/Latinos (e.g., Yellow Horse & Santos-Lozada, 2019 or Blacks (e.g., Doamekpor & Dinwiddie, 2015; Hickson et al., 2012). In addition, the vast majority of the aforementioned allostatic load studies have relied on data from the National Health and Nutrition Examination Survey (NHANES), a nationally representative sample of adults spanning the late teens, young adult years, and middle to late ages (see reviews by Duong et al., 2017; Juster et al., 2010; Beckie, 2012; Johnson et al., 2017). In their study of age patterns of allostatic load in NHANES, however, Geronimus et al. (2006) convincingly showed that young adulthood (or perhaps the period immediately prior to it) may be a critical period for the differential accumulation of biological risk due to social stress; it is during and after this period that health inequities appeared to widen dramatically. Thus, our study focuses squarely on young adulthood and seeks to contribute new knowledge about the associations between race/ethnicity, gender, SES, and allostatic load using data from a nationally representative sample of young adult men and women in the U.S.
Though narrowing the age period of interest obviates our ability to examine age patterns of allostatic load, we extend Geronimus et al.'s (2006) study by including people of Mexican origin and using educational attainment—a more consistent and reliable predictor of health than income-based measures of SES like the one they used (Winkleby et al., 1992). We also aimed to further test the utility of an intersectional approach to research on stress-related health inequities by investigating whether and how race/ethnicity, gender, and educational attainment combine to produce differences in the physiological dysregulation that underlies them. Toward this end, we used data on a nationally representative sample of non-Hispanic Black, non-Hispanic White, and Mexican-origin young adults to test hypotheses associated with two main research questions: (1) How do race/ethnicity and gender combine to produce inequities in allostatic load? and (2) How does educational attainment influence the relationships among race/ethnicity, gender, and allostatic load? We hypothesized an intersectional effect of race/ethnicity and gender, as well as race/ethnicity, gender, and educational attainment, on allostatic load, which would be indicated by variation in allostatic load across groups and by higher allostatic load scores among people with intersecting disadvantages (e.g., Black × female or Black × less educated × female) than other race/ethnicity-gender or race/ethnicity-education-gender groups.
2. Materials and methods
2.1. Sample
We used restricted-use data from Waves I and IV of the National Longitudinal Study of Adolescent to Adult Health (Add Health), a longitudinal study of a nationally representative sample of adolescents in grades 7 through 12 during the 1994–1995 school year in the U.S. In Wave I, data were collected from 20,745 adolescents ages 11–19 through in-home interviews between April and December 1995 (response rate = 79%). Wave IV data were collected in 2007–2008 from 15,701 respondents (response rate = 80%) ages 24–34 through in-home interviews, physical examinations, and collection of blood spots. See Harris et al. (2019) for further details about the study design.
Our initial sampling frame consisted of male and female respondents who self-identified as non-Hispanic White, non-Hispanic Black, or Mexican-origin in Wave I and had valid sampling weights in Wave IV. Other racial/ethnic groups were excluded due to their substantially smaller sample sizes. Respondents who reported more than one race also were excluded from the study because there were far too few of them to conduct meaningful analysis. We then excluded female respondents who were pregnant at their Wave IV examination because pregnancy may impact several biomarkers for allostatic load (especially BMI and waist circumference) toward levels that would be considered high risk (n = 519). Thus, our final analytic sample consisted of 11,807 non-Hispanic White, non-Hispanic Black, and Mexican-origin men and non-pregnant women.
2.2. Measures
Allostatic Load. We calculated an allostatic load score for respondents based on their values for 10 biomarkers of stress, use of biomarker-regulating medications, and reports of being diagnosed with a health condition related to the biomarkers—all three of which were measured at Wave IV. First, we established a high-risk threshold for each biomarker and assigned respondents a point for each biomarker value beyond that threshold, consistent with previous research (e.g., Crimmins et al., 2003). Specifically, respondents received a point for having values of diastolic blood pressure (DBP), systolic blood pressure (SBP), pulse rate, body mass index (BMI), waist circumference, hemoglobin A1c (HbA1c), or C-reactive protein (CRP) above the 75th percentile of all values in the Add Health Wave IV sample; above the 80th percentile for triglycerides and total cholesterol; and below the 20th percentile for high-density lipoprotein (HDL) cholesterol.3 Five of the biomarkers—namely, DBP, SBP, pulse rate, BMI, and waist circumference—were collected through physical examination. The other five biomarkers—i.e., HbA1c, CRP, total cholesterol, triglycerides, and HDL cholesterol—were collected from blood samples. (See Add Health documentation for greater detail on measurement and biomarker assays; Harris et al., 2019).
Second, among respondents who were not already identified as high risk on a particular biomarker using the sample-based cutoffs, we gave a point for use of a biomarker-regulating medication or a self-reported history of a condition related to the biomarker. Specifically, for respondents who were taking medication to manage hypertension, diabetes, hyperlipidemia, or inflammation, and/or who self-reported having been diagnosed with hypertension, diabetes, or hyperlipidemia, we assigned a point for SBP, DBP, HbA1c, total cholesterol, triglycerides, HDL, or CRP, respectively. This approach to accounting for biomarker-related medication usage reflects our assumption that respondents who were on medication and had biomarker values within healthy ranges were successful in controlling them but would have otherwise experienced the same wear and tear on their regulatory systems as unmedicated respondents who had biomarker values in the unhealthy ranges.
To calculate allostatic load, we summed the points assigned due to biomarker levels, medication use, and self-reported diagnoses related to each biomarker, resulting in a single score ranging from 0 to 10 for each respondent.
Social Status. We combined responses to questions asking respondents to self-identify their race and Hispanic/Latino origin in Wave I and dummy-coded them to classify respondents as non-Hispanic White, non-Hispanic Black, or Mexican-origin (hereafter referred to simply as White, Black, or Mexican). Whites were selected as the reference category because they are the largest and most socially advantaged racial/ethnic group in the United States. As such, the estimated health inequities reflect the extent to which Blacks and Mexicans are disadvantaged relative to the most privileged and numerically dominant group. We used Add Health's pre-loaded gender variable at Wave IV, which classified respondents as male (reference) or female based on their self-reports at earlier waves. To capture respondents' educational attainment, we collapsed and dummy-coded responses to a question about the highest level of education obtained at Wave IV into three categories – high school diploma or less (reference), some college or vocational/technical training, and college degree or more.
Covariates. We included covariates from Wave IV that have a known or suspected association with allostatic load or with one's likelihood of receiving a diagnosis and/or being prescribed a biomarker-regulating medication. Specifically, we included: mean-centered age (in years), nativity (foreign born vs. U.S.-born), recency of a doctor visit (last 12 months vs. 1–2 years vs. 2+ years or never), smoking behavior (non-smoker vs. current smoker), and alcohol consumption in the past 12 months (non-drinkers vs. 1–2 drinks per week or less vs. greater than 2 drinks per week). In previous studies, the relationships among race/ethnicity, gender, SES, and allostatic load were stable in the presence of controls for smoking, alcohol consumption, and health care utilization (e.g., Doamekpor & Dinwiddie, 2015; Yellow Horse & Santos-Lozada, 2019; Hickson et al., 2012; Kaestner et al., 2009; Peek et al., 2010). However, smoking and alcohol consumption are believed to decelerate the reactivity of the physiological stress system or attenuate the stress response (Wiggert et al., 2016), and a known association between health care utilization and receipt of treatment for health conditions precipitated by physiological dysregulation also exists (Zhang et al., 2012). Thus, we considered it wise to include these behavioral factors in our analyses as controls.
2.3. Statistical Analysis
We examined the distributions of allostatic load scores across racial/ethnic, gender, and educational categories using univariate and multivariate statistics. Then, we used negative binomial regression to estimate the main effects of, and interactions among, race/ethnicity, gender, and educational attainment on allostatic load, net of controls. Given the complexity of interpreting three-way interactions (and for presentation purposes), we stratified our analyses of the effects of race/ethnicity, educational attainment, and their interaction by gender and used Chow tests from a full, gender-interacted model to assess the statistical significance of the gender differences. This approach produces identical point estimates to those yielded from a full sample model with two- and three-way interactions (Landry, 2007), and it has been used in previous tests of intersectionality hypotheses (e.g., Brown et al., 2016; Hinze et al., 2012). Thus, for each gender, we estimated racial/ethnic differences in allostatic load (Model 1) and then added educational attainment (Model 2), covariates (Model 3), and an interaction term for race/ethnicity and educational attainment (Model 4). Statistical significance of the interaction among these variables, suggesting that their effects are conditional on each other, was considered support for intersectionality.
For consistency with previous studies of allostatic load (e.g., Chyu & Upchurch, 2011; Yellow Horse & Santos-Lozada, 2019; Graves & Nowakowski, 2017; Rainisch & Upchurch, 2013), we report incidence rate ratios (IRRs) instead of the log-rate coefficients we estimated. An IRR, which is calculated by exponentiating a log-rate coefficient, is the ratio of the allostatic load scores for one group (e.g., Blacks) compared to the scores of another group, typically the reference group (e.g., Whites). We recognize, however, that the improvements in interpretability of our findings gained from stratifying our results by gender (rather than estimating and reporting the results from 3-way interactions) and reporting IRRs (instead of log-rate coefficients) come at a small cost. Specifically, because we stratified our analysis by gender, the IRRs generated from our analytic models are useful for comparisons within each gender but not between them. A comparison of the IRRs for Black males and Black females, for example, would provide insight only on how much each group's allostatic load score differs from that of their same-gender reference group (i.e., White males and White females, respectively), not how Black males' and females' allostatic load scores differ from each other. This means that a difference in IRRs between them could be a result of differences between the allostatic load scores of their same-gender reference group (which are the denominators for the IRRs) rather than a result of a real difference in allostatic load between Black men and women. Given this possibility, we conducted supplemental analysis in which we re-normalized the model intercepts to allow for estimation and direct comparisons of the raw allostatic load scores of each racial/ethnic-gender group across analytic models. This approach (described in more detail and presented alongside its results in Appendix A) improves interpretability of the Chow test results for gender differences within each of the three racial/ethnic groups while also facilitating the identification of any intersectional effects across racial/ethnic-gender and racial/ethnic-gender × education groups.
We used Stata version 15 (StataCorp, College Station, TX) and accounted for Add Health's complex survey design (including sampling weights) in all analyses (Harris et al., 2019). Aside from race/ethnicity and gender for which we had complete data, missing values on all covariates and components of allostatic load, which ranged from less than 1%–13%, were imputed using multiple imputation. The findings were not sensitive to the use of imputed versus non-imputed data. Therefore, we report the results for the imputed data here. (Results of complete case analysis are provided in Appendix B).
3. Results
3.1. Sample characteristics
Descriptive statistics for the 10 components of our allostatic load measure are shown in Table 1. Aside from the three lipids (i.e., total cholesterol, triglycerides, and HDL) which, as previously noted, were reported in deciles in the Add Health dataset, we list the range, mean, and high-risk threshold (75th percentile of our analytic sample) for each biomarker. Also, we report the overall percentage of the sample identified as “at risk” based on their biomarker measurements, self-reports, or use of biomarker-regulating medication. The percentages for high risk are consistent with those reported by other Add Health-based studies of these biomarkers (Nguyen et al, 2011, 2014; Yang et al., 2020).
Table 1.
Descriptive Statistics of the 10 Measures Comprising Allostatic Load, Wave IV of the National Longitudinal Study of Adolescent to Adult Health (N = 11,807)*.
| Biomarker | Range | Mean (SD) | High Risk Threshold‡ | % High Risk, Biomarker only | Overall % High Risk§ | |
|---|---|---|---|---|---|---|
| Blood pressure, systolic (mm Hg) | 74.00–222.50 | 125.41 (12.97) | 133.00 | 25.79 | 33.86 | |
| Blood pressure, diastolic (mm Hg) | 31.00–147.00 | 79.70 (9.70) | 85.50 | 25.69 | 33.88 | |
| Pulse rate (beats/min) | 40.00–196.00 | 73.92 (11.34) | 81.50 | 27.37 | 27.37 | |
| C-reactive protein (mg/L) | 0.08–205.00 | 4.68 (7.93) | 5.26 | 25.01 | 53.33 | |
| Body mass index (kg/m2) | 14.40–97.40 | 29.09 (7.31) | 32.50 | 26.28 | 26.28 | |
| Waist circumference (cm) | 50.00–197.00 | 98.30 (16.56) | 106.00 | 29.44 | 29.44 | |
| Glycated hemoglobin (%) | 3.80–23.10 | 5.58 (0.76) | 5.80 | 27.63 | 37.53 | |
| Total cholesterol (deciles) | 1–10 | – | ≥8th decile | 20.00 | 37.08 | |
| Triglycerides (deciles) | 1–10 | – | ≥8th decile | 20.00 | 37.61 | |
| High-density lipoprotein (deciles) | 1–10 | – | <2nd decile | 20.00 | 33.53 | |
Abbreviations:%, weighted percent; SD, standard deviation
*Descriptive statistics are based on weighted data.
‡ The high-risk threshold denotes values greater than or equal to the 75th percentile of the sample, except in the case of high-density lipoprotein (HDL), total cholesterol, and triglycerides. These lipids are reported by deciles in Add Health. Thus, the high-risk threshold marks values above the 80th percentile for total cholesterol and triglycerides and below the 20th percentile for HDL.
§ Percentage listed for systolic blood pressure, diastolic blood pressure, C-reactive protein (CRP), glycated hemoglobin, total cholesterol, triglycerides, and HDL includes self-report and medication flags deeming the respondent high risk regardless of whether the biomarker measurement from the Add Health physical examination resulted in a value above the high risk threshold.
Table 2 presents descriptive statistics for the study sample overall and by race/ethnicity and gender. Overall, respondents had an average allostatic load score of 3.13 (95%CI = 3.05, 3.20). Of all the race/ethnicity-gender groups, Mexican men exhibited the highest average allostatic load score (3.50 [95%CI = 3.12, 3.87]), followed by Black women (3.39 [95%CI = 3.24, 3.54]). Within racial/ethnic groups, White (2.79 [95%CI = 2.66, 2.91]) and Mexican (3.12 [95%CI = 2.83, 3.41)] women had lower mean allostatic load scores than their male counterparts (3.29 [95%CI = 3.19, 3.40] for White men), while the reverse was true for Blacks, among whom women had a higher mean allostatic load score than men (3.39 vs. 3.27 [95%CI = 3.09, 3.45], respectively). Table 2 also reveals considerable variation in demographic, socioeconomic, and behavioral characteristics across the racial/ethnic-gender groups. Notably, women in each racial/ethnic group exhibited higher levels of educational attainment than men. Comparing within and across racial/ethnic groups, White women had the most favorable educational attainment distribution (with 36.6% having a college degree or more [95%CI = 0.32, 0.41]), while Black and Mexican men had the least favorable distributions (with only 17.7% [95%CI = 0.13, 0.22] and 14.1% [95%CI = 0.11, 0.21], respectively, having a college degree or more).
Table 2.
Characteristics of the Study Population, Overall and by Race/Ethnicity and Gender, Wave IV of the National Longitudinal Study of Adolescent to Adult Health.
| Non-Hispanic White |
Non-Hispanic Black |
Mexican Origin |
|||||
|---|---|---|---|---|---|---|---|
| Variable | Total (N = 11,807) |
Male (n = 3733) |
Female (n = 3840) |
Male (n = 1390) |
Female (n = 1730) |
Male (n = 548) |
Female (n = 566) |
| Allostatic load score, mean (SE) [95% CI] | 3.13 (0.04)[3.05,3.20] | 3.30 (0.05) [3.19,3.40] | 2.79 (0.06) [2.67,2.91] | 3.27 (0.09) [3.09,3.45] | 3.39 (0.08) [3.24,3.54] | 3.49 (0.19) [3.12,3.87] | 3.12 (0.14) [2.84,3.41] |
| Age (years), mean (SE) [95% CI] | 28.34 (0.12) [28.10,28.58] | 28.37 (0.14) [28.10,28.65] | 28.16 (0.13) [27.90,28.43] | 28.70 (0.23) [28.25,29.16] | 28.49 (0.20) [28.09,28.89] | 28.38 (0.28) [27.81,28.95] | 28.26 (0.31) [27.64,28.88] |
| Educational attainment,% [95% CI] | |||||||
| H.S. diploma or less | 7.5 [0.24,0.31] | 28.6 [0.25,0.32] | 19.9 [0.17,0.23] | 42.1 [0.17,0.23] | 26.4 [0.22,0.31] | 2.6 [0.36,0.49] | 36.5 [0.30,0.43] |
| Some college | 42.9 [0.41,0.45] | 41.6 [0.39,0.44] | 43.5 [0.41,0.46] | 40.2 [0.35,0.45] | 47.9 [0.44,0.52] | 43.3 [0.36,0.50] | 47.4 [0.41,0.54] |
| College degree or more | 29.6 [0.26,0.33] | 29.8 [0.25,0.34] | 36.6 [0.32,0.41] | 17.7 [0.13,0.22] | 25.7 [0.19,0.32] | 14.1 [0.10,0.18] | 16.1 [0.11,0.21] |
| Nativity, % [95% CI] | |||||||
| U.S.-born | 97.4 [0.96,0.98] | 98.9 [0.98,0.99] | 98.8 [0.98,0.99] | 98.7 [0.98,1.00] | 98.1 [0.97,0.99] | 81.2 [0.76,0.87] | 80.5 [0.74,0.87] |
| Foreign-born | 2.6 [0.02,0.04] | 1.1 [0.01,0.02] | 1.2 [0.01,0.02] | 1.3 [0.00,0.02] | 1.9 [0.01,0.03] | 18.8 [0.13,0.24] | 19.5 [0.13,0.26] |
| Recency of doctor visit, % [95% CI] | |||||||
| Last year | 58.5 [0.57,0.60] | 45.3 [0.43,0.47] | 66.8 [0.65,0.69] | 60.1 [0.56,0.64] | 79.7 [0.76,0.83] | 52.4 [0.46,0.59] | 68.6 [0.62,0.75] |
| 1–2 years ago | 14.5 [0.14,0.15] | 15.7 [0.14,0.17] | 13.9 [0.12,0.15] | 15.2 [0.13,0.18] | 10.7 [0.09,0.12] | 15.7 [0.11,0.19] | 15.1 [0.11,0.19] |
| >2 years ago or never | 27.0 [0.25,0.28] | 39.0 [0.37,0.41] | 19.3 [0.17,0.21] | 24.7 [0.21,0.28] | 9.6 [0.06,0.13] | 31.9 [0.27,0.37] | 16.3 [0.11,0.22] |
| Smoking behavior, % [95% CI] | |||||||
| Non-smoker | 80.7 [0.79,0.82] | 78.7 [0.77,0.81] | 82.8 [0.81,0.85] | 72.7 [0.69,0.76] | 84.2 [0.80,0.87] | 82.3 [0.77,0.86] | 91.6 [0.87,0.95] |
| Current smoker | 19.3 [0.17,0.21] | 21.3 [0.18,0.24] | 17.2 [0.15,0.20] | 27.3 [0.23,0.32] | 15.8 [0.12,0.20] | 17.7 [0.13,0.25] | 8.4 [0.05,0.13] |
| Alcohol consumption past 12 mos, % [95% CI] | |||||||
| Non-drinker | 25.9 [0.24,0.28] | 19.7 [0.17,0.22] | 23.5 [0.21,0.26] | 38.9 [0.35,0.44] | 43.8 [0.40,0.48] | 24.7 [0.19,0.32] | 40.1 [0.32,0.49] |
| 1-2 drinks/week or less | 61.7 [0.60,0.63] | 61.2 [0.59,0.63] | 68.4 [0.66, 0.71] | 49.3 [0.45,0.53] | 51.9 [0.48,0.56] | 62.3 [0.56,0.69] | 57.2 [0.49,0.65] |
| >2 drinks/week | 12.4 [0.11,0.14] | 19.1 [0.17,0.21] | 8.1 [0.07,0.10] | 11.8 [0.10,0.14] | 4.3 [0.03,0.07] | 13.0 [0.09,0.18] | 2.7 [0.01,0.05] |
Abbreviations:%, weighted percent; SE, standard error of the mean; CI, confidence interval; H.S., high school
3.2. Multivariate results
Table 3 displays the results from negative binomial regression analysis of the relationships among race/ethnicity, educational attainment, allostatic load, and covariates, stratified by gender. Model 1 reveals racial/ethnic differences in allostatic load among women, but not men. Specifically, the allostatic load scores of Black women were 22% higher on average than those of White women (IRR [95%CI] = 1.22 [1.15, 1.29]), while those of Mexican women were 12% higher (IRR [95%CI] = 1.12 [1.01, 1.24]). Conversely, the IRRs of Black and Mexican men were not statistically significant, indicating that their allostatic load scores did not differ from those of White men. Results from the Chow tests for Model 1 suggest that, not only are the allostatic load scores of Black women significantly higher than those of White women, but they also are significantly higher than those of their Black male counterparts (see Table A.1, Model 1 in Appendix A). Conversely, White females had lower allostatic load scores than White men.
Table 3.
Incidence Rate Ratios of Allostatic Load Scores from Negative Binomial Regression Models, Wave IV of the National Longitudinal Study of Adolescent to Adult Health (N = 11,807)*.
| Model 1 (IRR; 95% CI) |
Model 2 (IRR; 95% CI) |
Model 3 (IRR; 95% CI) |
Model 4 (IRR; 95% CI) |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Variable | Men | Women | Men | Women | Men | Women | Men | Women | |
| Race/Ethnicity | |||||||||
| Non-Hispanic White | 1.00 [Referent] | 1.00 [Referent] | 1.00 [Referent] | 1.00 [Referent] | 1.00 [Referent] | 1.00 [Referent] | 1.00 [Referent] | 1.00 [Referent] | |
| Non-Hispanic Black | 0.99 [0.93,1.06] | 1.22 [1.15,1.29] ‡ | 0.98 [0.92,1.04] | 1.18 [1.12,1.25] ‡ | 0.94 [0.88,1.00] | 1.15 [1.09,1.21] ‡ | 0.91 [0.81,1.03] | 1.12 [0.97,1.29] ‡ | |
| Mexican Origin | 1.06 [0.95,1.18] | 1.12 [1.01,1.24] | 1.04 [0.93,1.15] | 1.06 [0.95,1.17] | 1.04 [0.93,1.16] | 1.06 [0.95,1.18] | 1.09 [0.93,1.28] | 1.00 [0.88,1.13] | |
| Educational Attainment | |||||||||
| H.S. diploma or less | 1.00 [Referent] | 1.00 [Referent] | 1.00 [Referent] | 1.00 [Referent] | 1.00 [Referent] | 1.00 [Referent] | |||
| Some college | 1.02 [0.97,1.09] | 0.87 [0.82,0.92] ‡ | 1.03 [0.97,1.10] | 0.88 [0.83,0.94] ‡ | 1.05 [0.98,1.12] | 0.87 [0.80,0.95] ‡ | |||
| College degree or more | 0.85 [0.79.0.91] | 0.72 [0.67,0.77] ‡ | 0.86 [0.80,0.93] | 0.73 [0.68,0.79] ‡ | 0.83 [0.76,0.90] | 0.71 [0.65,0.78] ‡ | |||
| Race/Ethnicity × Education | |||||||||
| White H.S. diploma or less | 1.00 [Referent] | 1.00 [Referent] | |||||||
| Black some college | 0.96 [0.82,1.13] | 1.01 [0.85,1.21] | |||||||
| Black college degree or more | 1.28 [1.06,1.56] | 1.08 [0.92,1.27] ‡ | |||||||
| Mexican some college | 0.87 [0.71,1.07] | 1.03 [0.87,1.23] | |||||||
| Mexican college degree or more | 1.05 [0.82,1.36] | 1.27 [0.99,1.63] | |||||||
| Age (referent is age 24) | 1.03 [1.02,1.05] | 1.03 [1.01,1.04] | 1.03 [1.02,1.05] | 1.03 [1.01,1.04] | |||||
| Nativity | |||||||||
| U.S.-born | 1.00 [Referent] | 1.00 [Referent] | 1.00 [Referent] | 1.00 [Referent] | |||||
| Foreign-born | 0.91 [0.79,1.05] | 0.90 [0.77,1.04] | 0.90 [0.78,1.03] | 0.91 [0.78,1.06] | |||||
| Recency of doctor visit | |||||||||
| Last year | 1.00 [Referent] | 1.00 [Referent] | 1.00 [Referent] | 1.00 [Referent] | |||||
| 1–2 years ago | 0.99 [0.92,1.06] | 0.96 [0.90,1.03] | 0.99 [0.92,1.06] | 0.96 [0.90,1.03] | |||||
| >2 years ago or never | 0.91 [0.87,0.96] | 0.95 [0.89,1.02] | 0.91 [0.87,0.96] | 0.95 [0.89,1.02] | |||||
| Smoking behavior | |||||||||
| Non-smoker | 1.00 [Referent] | 1.00 [Referent] | 1.00 [Referent] | 1.00 [Referent] | |||||
| Current smoker | 0.99 [0.94,1.05] | 1.00 [0.93,1.07] | 0.99 [0.94,1.05] | 1.00 [0.93,1.07] | |||||
| Alcohol consumption past 12 mos. | |||||||||
| Non-drinker | 1.00 [Referent] | 1.00 [Referent] | 1.00 [Referent] | 1.00 [Referent] | |||||
| 1-2 drinks/week or less | 0.91 [0.86,0.97] | 0.93 [0.89,0.98] | 0.91 [0.86,0.97] | 0.93 [0.89,0.98] | |||||
| >2 drinks/week | 0.88 [0.81,0.96] | 0.83 [0.73,0.95] | 0.88 [0.81,0.96] | 0.84 [0.74,0.95] | |||||
| Constant | 3.30 [3.20,3.40] | 2.79 [2.67,2.91] | 3.42 [3.27,3.57] | 3.32 [3.13,3.51] | 1.60 [1.07,2.40] | 1.65 [1.05,2.60] | 1.61 [1.08,2.40] | 1.67 [1.06,2.62] | |
| F (2, 123.8) = 0.72 | F (2, 123.8) = 25.6 | F (4, 124.4) = 7.7 | F (4, 125.1) = 37.9 | F (11, 125.6) = 7.1 | F (11,125.6) = 18.8 | F (15, 125.6) = 6.6 | F (15, 125.6) = 14.3 | ||
| Prob > F = 0.49 | Prob > F = 0.00 | Prob > F = 0.00 | Prob > F = 0.00 | Prob > F = 0.00 | Prob > F = 0.00 | Prob > F = 0.00 | Prob > F = 0.00 | ||
Abbreviations: IRR = Incidence Rate Ratio; CI = Confidence Interval, H.S. = High School
∗IRRs are based on weighted data.
‡ Denotes variable's effect on the IRR significantly differs by gender at the p < .05 level.
The inclusion of educational attainment in Model 2 attenuated the difference in allostatic load between White and Mexican women. However, Black women's allostatic load scores remained significantly higher than those of White women (IRR [95%CI] = 1.18 [1.12, 1.25]). They also remained significantly higher than those of their Black male counterparts and surpassed those of Mexican men, making Black women the group with the largest allostatic load in the sample (see Table A.1, Model 2 in Appendix A). Moreover, the protective effect of gender for White females was largely eliminated once we controlled for educational attainment.
These results are attributable to the overall protective effect of educational attainment that is evident in Model 2 and the compositional differences in educational attainment across racial/ethnic-gender groups identified in our descriptive statistics. As Model 2 shows, both men and women with a college degree or more exhibited allostatic load scores that were roughly 15% and 30% lower, respectively, than the scores of their counterparts with a high school diploma or less ([IRR [95%CI] = 0.85 [0.79, 0.91] for college-educated men; IRR [95%CI] = 0.72 [0.67, 0.77] for college-educated women). Women who completed some college had allostatic load scores that were 13% lower than women with a high school diploma or less (IRR [95%CI] = 0.87 [0.82, 0.92]). Taken together with the findings for race/ethnicity-gender, it is therefore clear that parsing the benefits of their favorable educational attainment distribution and the stress-mitigating effects of education from the model resulted in the loss of White women's health advantage over White men and Black women's health advantage over Mexican men, whose allostatic load scores were high due to their relatively low levels of education (see Table A.1, Model 2 in Appendix A). The addition of all other covariates to this model resulted in little change in the pattern of results (Model 3), owing perhaps to the lack of statistically significant associations between most of the covariates and allostatic load.
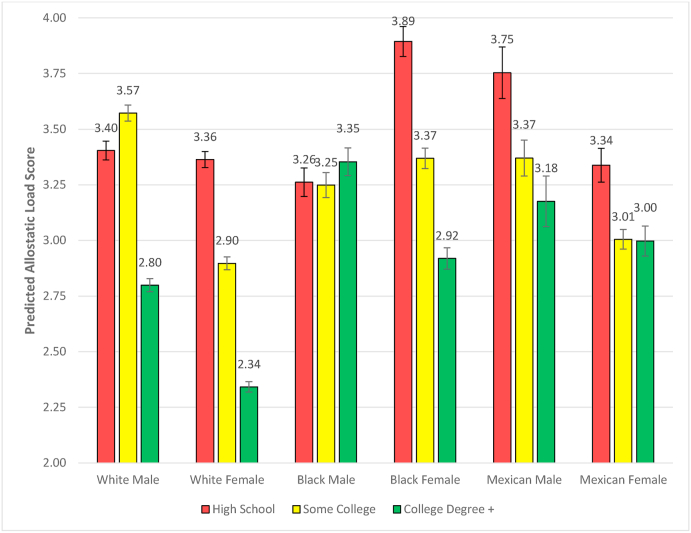
However, adding an interaction term for race/ethnicity × educational attainment in Model 4 makes clear that the overall protective effect of college education found in Model 3 did not hold true for all racial/ethnic-gender groups. Specifically, college education was associated with significantly lower allostatic load scores than obtaining only a high school diploma or less for White men and women (IRR [95%CI] = 0.83 [0.76, 0.90] for White men; IRR [95%CI] = 0.71 [0.65, 0.78] for White women). Similarly, attending at least some college was protective for White women (IRR [95%CI] = 0.87 [0.80, 0.95]). Yet for Black men, not only does a college degree provide no net protection, but it actually has the opposite effect (IRR [95%CI] = 1.28 [1.06, 1.56]). The statistically significant Chow test for gender differences among Black college degree recipients in Model 4 also indicates that there is a 3-way interaction among race/ethnicity, gender, and educational attainment. This interaction effect on allostatic load is visually depicted in Fig. 1, where it is evident that every racial/ethnic-gender group benefits from a college education except for Black males, whose allostatic load is larger at this level of education than at lower levels of education. In fact, this figure shows that college education renders Black males no better off than White males who have obtained only a high school diploma or dropped out of high school.
Fig. 1.
Fitted Allostatic Load Scores and 95% CIs by Race/Ethnicity, Gender, and Educational Attainment from Model 4 of Table 3.
4. Discussion
This study applied an intersectionality perspective to investigate whether and how race/ethnicity, gender, and educational attainment combine to produce differences in the physiological dysregulation that underlies stress-related illness, as measured by allostatic load. It is among only a few intersectionality-informed studies of health inequities that have examined interactions between more than two social statuses and focused on racial/ethnic comparisons beyond the Black-White binary. Importantly, the study is based on data from a nationally representative sample of non-Hispanic Black, non-Hispanic White, and Mexican adults ages 24–34 because previous analyses of racial/ethnic differences in allostatic load have often excluded the latter racial/ethnic group and have suggested that young adulthood may represent a critical period for the differential accumulation of biological risk due to social stress.
We had two primary aims. First, we sought to determine whether race/ethnicity and gender combine to produce inequities in allostatic load. In particular, we hypothesized that people with intersecting disadvantages would fare worse than people without them. Consistent with this hypothesis, we found that Black women had higher allostatic load scores than either Black men or White women. In fact, Black women were the only group of women who were disadvantaged compared to their male counterparts. These findings offer support for intersectionality and are consistent with previous research (e.g., Geronimus et al., 2006). Somewhat surprisingly, we found that Mexican women exhibited no higher allostatic load than either Mexican men or White women. While our analyses could not explain why these patterns emerged, they suggest that the stress-related health of young adult Mexican women (over 80 percent of whom are U.S.-born in Add Health) is more similar to Whites than to Blacks, consistent with the longstanding epidemiologic paradox (Markides and Coreil, 1986). Future work should further investigate reasons behind the relatively favorable health of Mexican women in Add Health, in comparison to both Mexican men and to Black and White women.
Second, we aimed to assess whether and how educational attainment influences the relationship between race/ethnicity and gender. We found an overall protective effect of educational attainment that, when taken into account, did little to attenuate the higher allostatic load scores for Black women compared to White women. It also resulted in a mean allostatic load score for Black women that was even higher than that of Mexican men, whose unadjusted score was highest owing to their relatively low education levels. This set of findings clearly demonstrates that allostatic load varies along racial/ethnic, gender, and education lines. However, the additive model of race/ethnicity and education masked substantial heterogeneity in the effect of education across racial/ethnic-gender groups, as we discovered when we added an interaction term for race/ethnicity × education which, in turn, revealed further support for intersectionality. Most notably, albeit contrary to our hypothesis regarding the more detrimental effect for people with intersecting disadvantages, we found that the intersectional effect of educational attainment and race/ethnicity on allostatic load was most pronounced among men. Black men with a college education experienced significantly higher allostatic load scores than college-educated White men, as well as White men with a high school diploma or less. Moreover, Black men were the only racial/ethnic-gender group who were not protected by a college education. Among other racial/ethnic-gender groups, the health returns to college education were highest among both White men and women. These findings are consistent with other research demonstrating that the health benefits associated with higher education are not experienced equally among different racial/ethnic groups (Gaydosh et al., 2018; Howard & Sparks, 2015).
As hypothesized and consistent with previous research (e.g., Doamekpor & Dinwiddie, 2015; Yellow Horse & Santos-Lozada, 2019; Hickson et al., 2012; Kaestner et al., 2009; Peek et al., 2010), our results were stable in the presence of behavioral covariates, such as smoking and health care utilization. This suggests that such factors do not confound the relationships among race/ethnicity, gender, educational attainment, and allostatic load. It also means that, despite high levels of unhealthy behavior among young adult men (Olson et al., 2017) and higher levels of poorly managed chronic conditions and delayed health care-seeking among Black men compared to other population subgroups (Griffith & Thorpe, 2016; Warner & Hayward, 2006; Williams, 2003), smoking and drinking do not explain the higher allostatic load levels of college-educated Black men relative to others. It is possible, however, that other unmeasured behaviors—particularly maladaptive coping responses to the stressors these highly motivated men encounter—may explain this finding. A related explanation comes from the extant literature on Black men's health, in which there has been an increasing amount of attention paid to the multiplicative (i.e., intersectional) effects of race/ethnicity and gender (Gilbert et al., 2016; Griffith, 2012) with emphasis on the chronic stressors they face and must find ways to cope with. Like their female counterparts, Black men also have been the victims of gendered racism at every level of society that has shaped their contemporary social and economic realities. For example, the disproportionate incarceration, unemployment, and premature mortality of Black men is attributable to structural and institutional racism. Black men also tend to be judged, and interacted with, based on a wide range of negative race-, and race-and-gender-based stereotypes (Pieterse & Carter, 2007; Williams, 2003) that are the basis for interpersonal racism (Gilbert et al., 2016). These experiences may be particularly toxic to young adult Black men who pursue higher education, especially if it means they must navigate more White spaces. It is during college that it may become clear to them that improvements in SES will offer little protection against strongly held stereotypes about them and the interpersonal discrimination, blocked opportunities, and other threats to their lives and livelihoods that stem from these stereotypes, including the threat of unjustified victimization and murder by individuals charged with protecting and serving the citizenry (i.e., the police). It is difficult to imagine a stressor more severe and chronic for any person than certain knowledge that, despite their best efforts, they are completely unable to be free of or to defend against these threats (except perhaps for the stress associated with being their mother).
Of course, a few limitations of our study are worth noting. First, we were limited in the number and type of biomarkers we could use to measure allostatic load by their availability (or lack thereof) in the Add Health dataset. As a result, we included no primary mediators, i.e., cortisol, noradrenaline, epinephrine, and dehydroepiandrosterone sulfate (DHEA-S), and only one marker of inflammation (C-reactive protein). Moreover, the lipid measures in Add Health are less precise than desirable. Nonetheless, it is not uncommon to find variation in the number and types of biomarkers used in research on allostatic load (Beckie, 2012; Duong et al., 2017; Johnson et al., 2017; Juster et al., 2010). Second, our method for establishing biomarker thresholds (i.e., using sample-based cutoffs) is only one of several methods that can be found in the extant literature on allostatic load. It is, however, the most widely used approach and is preferred over clinical guidelines, which are unavailable nationally and rarely age-specific (Duong et al., 2017). Fortunately, although research on social inequalities in allostatic load is rife with debates about the best way to operationalize it (Beckie, 2012), the findings tend to be robust to variations in measurement and analytic technique (Seeman et al., 1997; Santos-Lozada & Daw, 2018). Third, we also are aware of recent debates about how best to conduct quantitative intersectionality research, including how to distinguish between intersectional and statistical multiplicativity and whether intersectionality can be captured without a qualitative component (Bauer, 2014, Hankivsky, Doyal, Einstein, Kelly, & Shim, 2017). Thus, our study has other potential limitations vis-à-vis this debate.
By design, our study does not offer insights regarding the stress exposures that contribute to the racial/ethnic, gender, and educational differences in allostatic load we found. Nonetheless, we believe it still provides important clues about the intermediate physiological dysregulation that underlies social inequalities in stress-related health in later life. In particular, our results add to the growing bodies of evidence showing differential stress exposure and outcomes, as well as differential health returns to education. Indeed, our findings about the lack of protection conferred by college education on Black males suggests that educational improvement policies are a necessary but woefully insufficient strategy for addressing racial/ethnic health inequities. Even more upstream policies that focus on the structural roots of health inequities are needed instead (Gee & Ford, 2011). This is further supported by the stability of our findings in the presence of behavioral controls, which suggests that lifestyle-based strategies for reducing health inequities are not tenable, despite the fact that they are still far too frequently recommended and pursued.
Future research must, therefore, identify other life course-based stress exposures that differ across racial/ethnic-gender groups and matter for allostatic load. As we have suggested elsewhere in the paper, the identification of gendered racism-related stressors should be a top priority. Based on our findings in a young adult population, this research also should focus on exposures during earlier life periods. For this reason and because allostatic load is intended to capture a cumulative process and, thus, will change over time as stress burdens accumulate, future research should rely on longitudinal data instead of the cross-sectional data (like NHANES) that has been frequently used in previous research on allostatic load. This frequency is largely attributable to the fact that biomarker data have not been consistently collected in major longitudinal social surveys. Fortunately, Add Health repeated biospecimen collection in its fifth wave of data collection, which will open up new opportunities for longitudinal analyses of allostatic load and its contributing stressors in a nationally representative cohort. It is imperative that other major social surveys follow Add Health's lead, given the differences between them in terms of cohort factors (ages and years of data collection, for example) and the types of stressors that are captured.
Importantly, it should be recognized that further research on social status differences in allostatic load, and especially the early life race-, gender-, and SES-related stressors that combine to create them, would be consistent with a syndemics approach to health (Singer et al., 2017). Particularly as the COVID-19 pandemic in the United States continues to shine a spotlight on a syndemic—i.e., the clustering of multiple diseases (especially stress-related diseases) within Black, Native, and Latino populations, the interactions among the diseases and COVID-19, and the social, economic, environmental, and political stressors that give rise to them—research on how these stressors combine to accelerate the physiological wear and tear on the bodies of racial/ethnic minorities seems ever more critical and timely. We suspect that the findings of such research will inevitably signal the need for aggressive health and social policy efforts to reduce the elevated levels of stress exposure and simultaneous degradation of stress-buffering social and personal resources that they experience throughout their lives.
Ethical statement
This research used data from the National Longitudinal Study of Adolescent to Adult Health (Add Health), a program project directed by Kathleen Mullan Harris and designed by J. Richard Udry, Peter S. Bearman, and Kathleen Mullan Harris at the University of North Carolina at Chapel Hill (UNC–CH). Both Add Health and this secondary analysis of data from Add Health were approved by UNC-CH's Institutional Review Board.
Credit author statement
Liana Richardson: Conceptualization, Methodology, Writing – original draft, Writing – review & editing, Project administration, Visualization; Andrea Goodwin: Formal analysis, Data curation, Writing – original draft, Visualization; Robert Hummer: Methodology, Writing – review & editing, Supervision, Funding acquisition.
Declaration of competing interest
None.
Acknowledgments
This work was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) [grant numbers P2C HD050924 and T32 HD091058], and by the Carolina Women's Center. The content is solely the responsibility of the authors and does not necessarily represent the official views of NICHD or the Carolina Women's Center. The research used data from Add Health, a program project directed by Kathleen Mullan Harris and designed by J. Richard Udry, Peter S. Bearman, and Kathleen Mullan Harris at the University of North Carolina at Chapel Hill, and funded by grant P01-HD31921 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD), with cooperative funding from 23 other federal agencies and foundations. Information on how to obtain the Add Health data files is available on the Add Health website (http://www.cpc.unc.edu/addhealth). No direct support was received from grant P01-HD31921 for this analysis. An earlier version of this paper was presented at the 2019 annual meeting of the Interdisciplinary Association for Population Health Science in Seattle, WA. The authors would like to thank Cathy Zimmer and Anthony Perez for their statistical and programming advice.
Footnotes
A large literature documents the relatively favorable health of immigrants in the United States, including those of Mexican origin (Kaestner et al., 2009; Viruell-Fuentes, 2007). This has been described as an epidemiologic paradox because of the low socioeconomic status and stressful social conditions in which immigrant populations tend to live. Explanations for this paradox focus on healthy selection of immigrants upon arrival in the United States, healthy behavior, and strong supportive family and social networks. Given the complexity of the issues, we do not focus on the health of immigrant populations in the United States. We urge future researchers to consider focusing on the stress-health relationship among immigrants and especially so given the stressful social and political context in which immigrants live in the 21st century United States.
Of particular relevance here are feminist perspectives on lived experience that conceptualize it in terms of how social structural arrangements shape individual subjectivities and intersubjective meanings and experiences (e.g., Beauvoir, 1989), and that consider it a point of entry into larger questions of power and knowledge (Collins, 1990).
Although previous research has used 75th and 25th percentile cutoffs for lipids, we were unable to adhere to this approach because raw data for the lipids are not provided in the Add Health dataset. Instead, they are reported in deciles.
Appendix A. Supplemental Analysis Technique and Results
We conducted supplemental analysis to allow direct comparisons of the allostatic load scores of each gender group, thereby improving interpretability of the Chow test results for gender differences and facilitating identification of intersectional effects that include gender. We accomplished this analysis by first constraining the model intercept to zero, which allowed us to estimate raw (log rate) coefficients for all three racial/ethnic groups. Then, we exponentiated the coefficients to obtain IRRs, which transformed the (now implicit) intercept to exp (0) = 1, allowing the IRRs to conveniently reduce to exp(B)/1 = exp(B), i.e., incidence rates in the original allostatic load scale (meaning: the allostatic load scores) of each racial/ethnic-gender group. Thus, the underlying models for this analysis and the primary analysis (from which results in Table 3 were generated) are identical; the difference between them is simply a difference in normalization.
Results of this supplemental analysis are presented in Table A.1 below. For simplicity, we present only the allostatic load scores for race/ethnicity by gender. It should be noted, however, that these scores, as well as the effect sizes of other variables in the analytic models, are calculable (although without confidence intervals) from information in Table 3: The allostatic load scores for Whites in Table A.1 are equivalent to the constants in Table 3. These values are the denominators for the IRRs in Table 3; thus, the allostatic load scores for the other racial/ethnic groups can be obtained by multiplying each of their IRRs with its corresponding constant/intercept from Table 3. Then, all other IRRs listed in Table 3 except for those in Model 4 can be multiplied by the racial/ethnic- and gender-specific allostatic load scores in Table A.1 to determine their effects in the original allostatic load scale. For the interaction effects on allostatic load scores in Model 4, one must multiply the racial/ethnic- and gender-specific allostatic load scores by the IRRs for education and race/ethnicity × education.
Thus, we provide the results of the supplemental analysis as a courtesy to readers who would otherwise need to perform these calculations on their own. And, as we explained in our rationale for this analysis (in the Statistical Analysis section), Table 3 enables identification of statistically significant effects within gender. Table A.1 facilitates identification and interpretation of statistically significant effects between genders.
Table A.1.
Raw/Calculated Allostatic Load Scores for Race/Ethnicity by Gender from Negative Binomial Regression Models, Wave IV of the National Longitudinal Study of Adolescent to Adult Health (N = 11,807)*
| Variable | Model 1 (AL Score; 95% CI) |
Model 2 (AL Score; 95% CI) |
Model 3 (AL Score; 95% CI) |
Model 4 (AL Score; 95% CI) |
||||
|---|---|---|---|---|---|---|---|---|
| Men | Women | Men | Women | Men | Women | Men | Women | |
| Race/Ethnicity | ||||||||
| Non-Hispanic White | 3.30 [3.19,3.40] | 2.79 [2.67,2.91] ‡ | 3.43 [3.28,3.57] | 3.31 [3.13,3.50] | 3.84 [3.59,4.10] | 3.56 [3.33,3.79] | 3.85 [3.61,4.09] | 3.61 [3.32,3.90] |
| Non-Hispanic Black | 3.28 [3.09,3.45] | 3.39 [3.24,3.54] ‡ | 3.35 [3.12,3.58] | 3.92 [3.69,4.16] ‡ | 3.61 [3.32,3.89] | 4.09 [3.84,4.35] ‡ | 3.51 [3.11,3.91] | 4.03 [3.64,4.42] ‡ |
| Mexican Origin | 3.51 [3.12,3.87] | 3.13 [2.84,3.41] | 3.56 [3.20,3.90] | 3.51 [3.20,3.83] | 4.01 [3.55,4.48] | 3.78 [3.39,4.18] | 4.21 [3.59,4.84] | 3.63 [3.20,4.06] |
Abbreviations: AL = Allostatic Load; CI = Confidence Interval
∗Allostatic load scores of each racial/ethnic-gender group when covariates are held constant for all X; based on weighted data
‡ Denotes variable's effect on allostatic load significantly differs by gender at the p < .05 level.
Appendix B. Complete Case Analysis Results
Table B.1.
Incidence Rate Ratios of Allostatic Load Scores from Negative Binomial Regression Models for Complete Case (i.e., non-imputed) Data Only, Wave IV of the National Longitudinal Study of Adolescent to Adult Health*
| Model 1 (IRR; 95% CI) |
Model 2 (IRR; 95% CI) |
Model 3 (IRR; 95% CI) |
Model 4 (IRR; 95% CI) |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Variable | Men | Women | Men | Women | Men | Women | Men | Women | |
| Race/Ethnicity | |||||||||
| Non-Hispanic White | 1.00 [Referent] | 1.00 [Referent] | 1.00 [Referent] | 1.00 [Referent] | 1.00 [Referent] | 1.00 [Referent] | 1.00 [Referent] | 1.00 [Referent] | |
| Non-Hispanic Black | 0.98 [0.92,1.06] | 1.20 [1.13,1.27]‡ | 0.97 [0.91,1.04] | 1.16 [1.09,1.24] ‡ | 0.93 [0.87,1.00] | 1.13 [1.06,1.20]‡ | 0.92 [0.80,1.07] | 1.12 [0.96,1.29]‡ | |
| Mexican Origin | 1.03 [0.92,1.15] | 1.15 [1.04,1.27] | 1.00 [0.90,1.12] | 1.09 [0.98,1.21] | 1.01 [0.91,1.13] | 1.09 [0.98,1.22] | 1.06 [0.90,1.25] | 1.07 [0.93,1.23] | |
| Educational Attainment | |||||||||
| H.S. diploma or less | 1.00 [Referent] | 1.00 [Referent] | 1.00 [Referent] | 1.00 [Referent] | 1.00 [Referent] | 1.00 [Referent] | |||
| Some college | 1.03 [0.96,1.09] | 0.89 [0.83,0.95]‡ | 1.03 [0.97,1.10] | 0.89 [0.84,0.96]‡ | 1.06 [0.99,1.12] | 0.89 [0.82,0.97]‡ | |||
| College degree or more | 0.85 [0.79,0.92] | 0.73 [0.68,0.79]‡ | 0.86 [0.80,0.93] | 0.75 [0.69,0.81]‡ | 0.84 [0.77,0.91] | 0.73 [0.67,0.81]‡ | |||
| Race/Ethnicity × Education | |||||||||
| White H.S. diploma or less | 1.00 [Referent] | 1.00 [Referent] | |||||||
| Black some college | 0.92 [0.76,1.11] | 1.00 [0.83,1.20] | |||||||
| Black college degree or more | 1.24 [1.00,1.55] | 1.06 [0.89,1.26]‡ | |||||||
| Mexican some college | 0.87 [0.71,1.07] | 0.99 [0.84,1.16] | |||||||
| Mexican college degree or more | 1.06 [0.80,1.41] | 1.16 [0.89,1.50] | |||||||
| Age (referent is age 24) | 1.03 [1.01,1.05] | 1.03 [1.01,1.05] | 1.03 [1.01,1.05] | 1.03 [1.01,1.04] | |||||
| Nativity | |||||||||
| U.S.-born | 1.00 [Referent] | 1.00 [Referent] | 1.00 [Referent] | 1.00 [Referent] | |||||
| Foreign-born | 0.89 [0.76,1.04] | 0.91 [0.78,1.07] | 0.88 [0.76,1.02] | 0.92 [0.79,1.08] | |||||
| Recency of doctor visit | |||||||||
| Last year | 1.00 [Referent] | 1.00 [Referent] | 1.00 [Referent] | 1.00 [Referent] | |||||
| 1–2 years ago | 0.97 [0.91,1.04] | 0.95 [0.89,1.02] | 0.97 [0.91,1.04] | 0.95 [0.89,1.03] | |||||
| >2 years ago or never | 0.89 [0.76,1.04] | 0.94 [0.88,1.02] | 0.89 [0.84,0.94] | 0.96 [0.94,0.99] | |||||
| Smoking behavior | |||||||||
| Non-smoker | 1.00 [Referent] | 1.00 [Referent] | 1.00 [Referent] | 1.00 [Referent] | |||||
| Current smoker | 0.98 [0.92,1.04] | 1.00 [0.93,1.07] | 0.98 [0.92,1.04] | 1.00 [0.93,1.07] | |||||
| Alcohol consumption past 12 mos. | |||||||||
| Non-drinker | 1.00 [Referent] | 1.00 [Referent] | 1.00 [Referent] | 1.00 [Referent] | |||||
| 1-2 drinks/week or less | 0.90 [0.84,0.97] | 0.94 [0.89,0.99] | 0.90 [0.84,0.97] | 0.94 [0.89,0.99] | |||||
| >2 drinks/week | 0.86 [0.78,0.94] | 0.83 [0.71,0.95] | 0.86 [0.78,0.94] | 0.83 [0.72,0.96] | |||||
| Constant | 3.44 [3.32,3.55] | 2.88 [2.76,3.01] | 3.55 [3.39,3.71] | 3.38 [3.17,3.60] | 1.75 [1.09,2.80] | 1.62 [1.01,2.59] | 1.73 [1.08,2.77] | 1.62 [1.01,2.60] | |
| F (2, 127) = 18.51 | F (2, 127) = 2.06 | F (4, 125) = 6.01 | F (4, 125) = 29.84 | F (11, 118) = 5.93 | F (11,118) = 14.23 | F (15, 114) = 5.08 | F (15, 114) = 10.62 | ||
| Prob > F = 0.00 | Prob > F = 0.00 | Prob > F = 0.03 | Prob > F = 0.00 | Prob > F = 0.00 | Prob > F = 0.00 | Prob > F = 0.00 | Prob > F = 0.00 | ||
Abbreviations:IRR = Incidence Rate Ratio; CI = Confidence Interval, H.S. = High School
∗IRRs are based on weighted data. Sample size varies by variable.
‡ Denotes variable's effect on the IRR significantly differs by gender at the p < .05 level.
References
- Bauer Greta. Incorporating intersectionality theory into population health research methodology: Challenges and the potential to advance health equity. Social Science & Medicine. 2014;110:10–17. doi: 10.1016/j.socscimed.2014.03.022. [DOI] [PubMed] [Google Scholar]
- Beauvoir S. Vintage Books; New York: 1989. The second sex. [Google Scholar]
- Beckie T.M. A systematic review of allostatic load, health, and health disparities. Biological Research For Nursing. 2012;14:311–346. doi: 10.1177/1099800412455688. [DOI] [PubMed] [Google Scholar]
- Bird C.E., Seeman T., Escarce J.J., Basurto-Dávila R., Finch B.K., Dubowitz T., Heron M., Hale L., Merkin S.S., Weden M., Lurie N. Neighbourhood socioeconomic status and biological “wear and tear” in a nationally representative sample of US adults. Journal of Epidemiology & Community Health. 2010;64:860–865. doi: 10.1136/jech.2008.084814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borrell L.N., Kiefe C.I., Williams D.R., Diez-Roux A.V., Gordon-Larsen P. Self-reported health, perceived racial discrimination, and skin color in African Americans in the CARDIA study. Social Science & Medicine. 2006;63:1415–1427. doi: 10.1016/j.socscimed.2006.04.008. [DOI] [PubMed] [Google Scholar]
- Borrell L.N., Rodriguez-Alvarez E., Dallo F.J. Racial/ethnic inequities in the associations of allostatic load with all-cause and cardiovascular-specific mortality risk in U.S. adults. PloS One. 2020;15(2) doi: 10.1371/journal.pone.0228336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown T.H., Richardson L.J., Hargrove T.W., Thomas C.S. Using multiple-hierarchy stratification and life course approaches to understand health inequalities: The intersecting consequences of race, gender, SES, and age. Journal of Health and Social Behavior. 2016;57:200–222. doi: 10.1177/0022146516645165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carter-Pokras O., Baquet C. What is a health disparity? Public Health Reports. 2002;117:426–434. doi: 10.1093/phr/117.5.426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang M.L. Wealth accumulation and communities of color: Current issues, edited by jessica gordon nembhard and ngina chitej. University of Michigan Press; Ann Arbor, MI: 2006. Women and wealth; pp. 112–132. [Google Scholar]
- Chyu L., Upchurch D.M. Racial and ethnic patterns of allostatic load among adult women in the United States: Findings from the national health and nutrition examination survey 1999–2004. J Womens Health (Larchmt) 2011;20:575–583. doi: 10.1089/jwh.2010.2170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chyu L., Upchurch D.M. A longitudinal analysis of allostatic load among a multi-ethnic sample of midlife women: Findings from the study of women's health across the nation. Women's Health Issues. 2018;28:256–266. doi: 10.1016/j.whi.2017.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins P.H. Routledge; New York: 1990. Black feminist thought: Knowledge, consciousness, and the politics of empowerment. [Google Scholar]
- Crenshaw K. University of Chicago Legal Forum: 139-167; 1989. Demarginalizing the intersection of race and sex: A Black feminist critique of antidiscrimination doctrine, feminist theory and antiracist politics. [Google Scholar]
- Crimmins E.M., Seeman T.E. Integrating biology into the study of health disparities. Population and Development Review. 2004;30:89–107. [Google Scholar]
- DeVuono-Powell S., Schweidler C., Walters A., Zohrabi A. Ella Baker Center; Oakland, CA: 2015. Who pays? The true cost of incarceration on families. [Google Scholar]
- Doamekpor L.A., Dinwiddie G.Y. Allostatic load in foreign-born and US-born blacks: Evidence from the 2001–2010 national health and nutrition examination survey. American Journal of Public Health. 2015;105:591–597. doi: 10.2105/AJPH.2014.302285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duong M.T., Bingham B.A., Aldana P.C., Chung S.T., Sumner A.E. Variation in the calculation of allostatic load score: 21 examples from NHANES. Journal of Racial and Ethnic Health Disparities. 2017;4:455–461. doi: 10.1007/s40615-016-0246-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elemelech Y., Lu H. Race, ethnicity, and the gender poverty gap. Social Science Research. 2004;33:158–182. [Google Scholar]
- Gaydosh L., Schorpp K.M., Chen E., Miller G.E., Harris K.M. College completion predicts lower depression but higher metabolic syndrome among disadvantaged minorities in young adulthood. Proceedings of the National Academy of Sciences. 2018;115:109–114. doi: 10.1073/pnas.1714616114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gee G.C., Ford C.L. Structural racism and health inequities: Old issues, new Directions1. Du Bois Review: Social Science Research on Race. 2011;8(1):115–132. doi: 10.1017/S1742058X11000130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gee G.C., Hing A., Mohammed S., Tabor D.C., Williams D.R. Racism and the life course: Taking time seriously. American Journal of Public Health. 2019;109(S1):S43–S47. doi: 10.2105/AJPH.2018.304766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geronimus A.T. The weathering hypothesis and the health of african-American women and infants: Evidence and speculations. Ethnicity & Disease. 1992;2:207–221. [PubMed] [Google Scholar]
- Geronimus A.T. Black/white differences in the relationship of maternal age to birthweight: A population-based test of the weathering hypothesis. Social Science & Medicine. 1996;42:589–597. doi: 10.1016/0277-9536(95)00159-x. [DOI] [PubMed] [Google Scholar]
- Geronimus A. Understanding and eliminating racial inequalitites in women's health in the United States: The role of the weathering conceptual framework. Journal of the American Women's Association. 2001;56:134. [PubMed] [Google Scholar]
- Geronimus A.T., Hicken M., Keene D., Bound J. Weathering" and age patterns of allostatic load scores among blacks and whites in the United States. American Journal of Public Health. 2006;96:826–833. doi: 10.2105/AJPH.2004.060749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilbert K.L., Ray R., Siddiqi A., Shetty S., Baker E.A., Elder K., Griffith D.M. Visible and invisible trends in Black men's health: Pitfalls and promises for addressing racial, ethnic, and gender inequities in health. Annual Review of Public Health. 2016;37:295–311. doi: 10.1146/annurev-publhealth-032315-021556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodkind J.R., Gonzales M., Malcoe L.H., Espinosa J. The hispanic women's social stressor scale: Understanding the multiple social stressors of U.S.- and Mexico-born hispanic women. Hispanic Journal of Behavioral Sciences. 2008;30(2):200–229. [Google Scholar]
- Graves K.Y., Nowakowski A.C.H. Childhood socioeconomic status and stress in late adulthood: A longitudinal approach to measuring allostatic load. Glob Pediatr Health. 2017;4 doi: 10.1177/2333794X17744950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffith D.M. An intersectional approach to men's health. Journal of Men's Health. 2012;9:106–112. [Google Scholar]
- Griffith D.M., Thorpe R.J., Jr. APA handbook of the psychology of men and masculinities. APA; Washington, DC: 2016. Men's physical health and health behaviors; pp. 709–730. [Google Scholar]
- Gruenewald T.L., Karlamangla A.S., Hu P., Stein-Merkin S., Crandall C., Koretz B., Seeman T.E. History of socioeconomic disadvantage and allostatic load in later life. SSM. 2012;74:75–83. doi: 10.1016/j.socscimed.2011.09.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gustafsson P.E., Janlert U., Theorell T., Westerlund H., Hammarstrom A. Socioeconomic status over the life course and allostatic load in adulthood: Results from the Northern Swedish Cohort. Journal of Epidemiology & Community Health. 2011;65:986–992. doi: 10.1136/jech.2010.108332. [DOI] [PubMed] [Google Scholar]
- Hankivsky O, Doyal L, Einstein G, Kelly U, Shim J. The odd couple: using biomedical and intersectional approaches to address health inequities. Global Health Action. 2017;10:73–86. doi: 10.1080/16549716.2017.1326686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris K.M., Halpern C.T., Whitsel E.A., Hussey J.M., Killeya-Jones L.A., Tabor J., Dean S.C. Cohort profile: The national longitudinal study of adolescent to adult health (add health) International Journal of Epidemiology. 2019;48(5):1415–1425. doi: 10.1093/ije/dyz115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hickson D.A., Diez Roux A.V., Gebreab S.Y., Wyatt S.B., Dubbert P.M., Sarpong D.F., Sims M., Taylor H.A. Social patterning of cumulative biological risk by education and income among African Americans. American Journal of Public Health. 2012;102:1362–1369. doi: 10.2105/AJPH.2011.300444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hinze S.W., Lin J., Andersson T.E. Can we capture the intersections? Older Black women, education, and health. Women's Health Issues. 2012;22:e91–e98. doi: 10.1016/j.whi.2011.08.002. [DOI] [PubMed] [Google Scholar]
- Howard J.T., Sparks P.J. The role of education in explaining racial/ethnic allostatic load differentials in the United States. Biodemography and Social Biology. 2015;61:18–39. doi: 10.1080/19485565.2014.937000. [DOI] [PubMed] [Google Scholar]
- Hummer R.A., Gutin I. Future directions for the demography of aging: Proceedings of a workshop. The National Academies Press; Washington, DC: 2018. Racial/ethnic and nativity disparities in health of older U.S. Men and women; pp. 31–66. [PubMed] [Google Scholar]
- Johnson S.C., Cavallero F.L., Leon D.A. A systematic review of allostatic load in relation to socioeconomic position: Poor fidelity and major inconsistencies in biomarkers employed. SSM. 2017;192:66–73. doi: 10.1016/j.socscimed.2017.09.025. [DOI] [PubMed] [Google Scholar]
- Juster R.-P., McEwen B.S., Lupien S.J. Allostatic load biomarkers of chronic stress and impact on health and cognition. Neuroscience & Biobehavioral Reviews. 2010;35:2–16. doi: 10.1016/j.neubiorev.2009.10.002. [DOI] [PubMed] [Google Scholar]
- Kaestner R., Pearson J.A., Keene D., Geronimus A.T. Stress, allostatic load, and health of Mexican immigrants. Social Science Quarterly. 2009;90:1089–1111. doi: 10.1111/j.1540-6237.2009.00648.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landry B. Pearson Prentice Hall; Upper Saddle River, NJ: 2007. Race, gender, and class: Theory and methods of analysis. [Google Scholar]
- Markides K.S., Coreil J. The health of Hispanics in the southwestern United States: An epidemiologic paradox. Public Health Reports. 1986;101(3):253–265. [PMC free article] [PubMed] [Google Scholar]
- McEwen B.S. Stress, adaptation, and disease: Allostasis and allostatic load. Annals of the New York Academy of Sciences. 1998;840:33–44. doi: 10.1111/j.1749-6632.1998.tb09546.x. [DOI] [PubMed] [Google Scholar]
- McEwen B.S., Seeman T. Protective and damaging effects of mediators of stress: Elaborating and testing the concepts of allostasis and allostatic load. Annals of the New York Academy of Sciences. 1999;896:30–47. doi: 10.1111/j.1749-6632.1999.tb08103.x. [DOI] [PubMed] [Google Scholar]
- McEwen B.S., Stellar E. Stress and the individual: Mechanisms leading to disease. Archives of Internal Medicine. 1993;153:2093–2101. [PubMed] [Google Scholar]
- Mullings L., Wali A. Kluwer Academic/Plenum Publishers; New York: 2001. Stress and resilience: The social context of reproduction in harlem. [Google Scholar]
- Nguyen Q.C., Tabor J.W., Entzel P.P., Lau Y., Suchindran C., Hussey J.M., Halpern C.T., Harris K.M., Whitsel E.A. Discordance in national estimates of hypertension among young adults. Epidemiology. 2011;22(4):532–541. doi: 10.1097/EDE.0b013e31821c79d2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen Q.C., Whitsel E.A., Tabor J.W., Cuthbertson C.C., Wener M.H., Potter A.J., Halpern C.T., Killeya-Jones L.A., Hussey J.M., Suchindran C. Blood spot-based measures of glucose homeostasis and diabetes prevalence in a nationally representative population of young U.S. adults. Annals of Epidemiology. 2014;24(12):903. doi: 10.1016/j.annepidem.2014.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olson J.S., Hummer R.A., Harris K.M. Gender and health behavior clustering among U.S. Young adults. Biodemography and Social Biology. 2017;63:3–20. doi: 10.1080/19485565.2016.1262238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearlin L.I. The sociological study of stress. Journal of Health and Social Behavior. 1989;30:241–256. [PubMed] [Google Scholar]
- Pearlin L.I. Carol S. Aneshensel and jo C. Phelan. Kluwer Academic/Plenum; New York: 1999. The stress process revisited: Reflections on concepts and their interrelationshps; pp. 395–415. Handbook of the Sociology of Mental Health. [Google Scholar]
- Peek M.K., Cutchin M.P., Salinas J.J., Sheffield K.M., Eschbach K., Stowe R.P., Goodwin J.S. Allostatic load among non-hispanic whites, non-hispanic blacks, and people of Mexican origin: Effects of ethnicity, nativity, and acculturation. American Journal of Public Health. 2010;100:940–946. doi: 10.2105/AJPH.2007.129312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pieterse A., Carter R. An examination of the relationship between general life stress, racism-related stress, and psychological health among Black men. Journal of Counseling Psychology. 2007;54:101–109. [Google Scholar]
- Rainisch B.K.W., Upchurch D.M. Sociodemographic correlates of allostatic load among a national sample of adolescents: Findings from the national health and nutrition examination survey, 1999–2008. Journal of Adolescent Health. 2013;53:506–511. doi: 10.1016/j.jadohealth.2013.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Read J.G., Gorman B.K. Gender inequalities in U.S. Adult health: The interplay of race and ethnicity. Social Science & Medicine. 2006;62:1045–1065. doi: 10.1016/j.socscimed.2005.07.009. [DOI] [PubMed] [Google Scholar]
- Richardson L.J., Brown T.H. (En)gendering racial disparities in health trajectories: A life course and intersectional analysis. SSM-Population Health. 2016;2:425–435. doi: 10.1016/j.ssmph.2016.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodriquez E.J., Kim E.N., Sumner A.E., Nápoles A.M., Pérez-Stable E.J. Allostatic load: Importance, markers, and score determination in minority and disparity populations. Journal of Urban Health. 2019;96(Suppl 1):3–11. doi: 10.1007/s11524-019-00345-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santos-Lozada A.R., Daw J. The contribution of three dimensions of allostatic load to racial/ethnic disparities in poor/fair self-rated health. SSM-Population Health. 2018;4:55–65. doi: 10.1016/j.ssmph.2017.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seeman T.E., Crimmins E., Huang M.H., Singer B., Bucur A., Gruenewald T. Cumulative biological risk and socio-economic differences in mortality: MacArthur studies of successful aging. Social Science & Medicine. 2004;58:1985–1997. doi: 10.1016/S0277-9536(03)00402-7. [DOI] [PubMed] [Google Scholar]
- Seeman T.E., McEwen B.S., Rowe J.W., Singer B.H. Allostatic load as a marker of cumulative biological risk: MacArthur studies of successful aging. Proceedings of the National Academy of Sciences. 2001;98:4770–4775. doi: 10.1073/pnas.081072698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seeman T., Merkin S.S., Crimmins E., Koretz B., Charette S., Karlamangla A. Education, income, and ethnic differences in cumulative biological risk profiles in a national sample of U.S. Adults: Nhanes III (1988-1994) Social Science & Medicine. 2008;66:72–87. doi: 10.1016/j.socscimed.2007.08.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seeman T.E., Singer B.H., Rowe J.W., Horwitz R.I., McEwen B.S. Price of adaptation--allostatic load and its health consequences: MacArthur studies of successful aging. Archives of Internal Medicine. 1997;157:2259–2268. [PubMed] [Google Scholar]
- Singer M., Bulled N., Ostrach B., Mendenhall E. Syndemics and the biosocial conception of health. Lancet. 2017;389:941–950. doi: 10.1016/S0140-6736(17)30003-X. [DOI] [PubMed] [Google Scholar]
- Thoits P.A. Stress and health: Major findings and policy implications. Journal of Health and Social Behavior. 2010;51:S41–S53. doi: 10.1177/0022146510383499. [DOI] [PubMed] [Google Scholar]
- Turner R.J. Understanding health disparities: The relevance of the stress process model. Society and Mental Health. 2013;3:170–186. [Google Scholar]
- U.S. Bureau of Labor Statistics . U.S. Bureau of Labor Statistics; Washington, DC: 2018. Labor force characteristics by race and ethnicity, 2017. BLS Report 1076. [Google Scholar]
- Viruell-Fuentes E.A. Beyond acculturation: Immigration, discrimination, and health research among Mexicans in the United States. Social Science & Medicine. 2007;65:1524–1535. doi: 10.1016/j.socscimed.2007.05.010. [DOI] [PubMed] [Google Scholar]
- Warner D.F., Brown T.H. Understanding how race/ethnicity and gender impact age-trajectories of disability: An intersectionality approach. Social Science & Medicine. 2011;72:1236–1248. doi: 10.1016/j.socscimed.2011.02.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warner D.F., Hayward M.D. Early-life origins of the race gap in men's mortality. Journal of Health and Social Behavior. 2006;47:209–226. doi: 10.1177/002214650604700302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiggert N., Wilhelm F.H., Nakajima M., al'Absi M. Chronic smoking, trait anxiety, and the physiological response to stress. Substance Use & Misuse. 2016;51:1619–1628. doi: 10.1080/10826084.2016.1191511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams D.R. The health of men: Structured inequalities and opportunities. American Journal of Public Health. 2003;93:724–731. doi: 10.2105/ajph.93.5.724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winkleby M.A., Jatulis D.E., Frank E., Fortmann S.P. Socioeconomic status and health: How education, income, and occupation contribute to risk factors for cardiovascular disease. American Journal of Public Health. 1992;82:816–820. doi: 10.2105/ajph.82.6.816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu J., Kochanek K.D., Murphy S.L., Tejada-Vera B. Vol. 58. 2010. Deaths: Final data for 2007." national vital statistics reports. [PubMed] [Google Scholar]
- Yang C.Y., Schorpp K., Boen C., Johnson M., Harris K.M. Socioeconomic status and biological risks for health and illness across the life course. Journal of Gerontology: Serie Bibliographique. 2020;75(3):615–624. doi: 10.1093/geronb/gby108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yellow Horse A, Santos-Lozada A. Foreign-born hispanic women’s health patterns in allostatic load converge to U.S.-born hispanic women at a slower tempo compared with men. Women’s Health Issues. 2019;29(3):222–230. doi: 10.1016/j.whi.2019.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang X., Bullard K.M., Gregg E.W., Beckles G.L., Williams D.E., Barker L.E., Albright A.L., Imperatore G. Access to health care and control of ABCs of diabetes. Diabetes Care. 2012;35:1566–1571. doi: 10.2337/dc12-0081. [DOI] [PMC free article] [PubMed] [Google Scholar]