Sir,
Potassium permanganate (KMnO4) is a commonly used topical therapeutic agent in dermatology. It is readily available and widely used as a disinfectant and astringent. Due to its antiseptic and astringent properties, it is used for acute and sub-acute eczematous dermatitis with exudation in dilution of 0.010.0001%. It also has antifungal and deodorant property. If used in higher concentration, it causes severe chemical irritation and burning of skin. In this article, we report a unique case of accidental ocular injury in a 6 year old female child by potassium permanganate crystals. This type of ocular injury is fortunately rare; however, when it occurs, it may lead to severe complications. The aim of this case report is to sensitize the dermatologists regarding adverse effects of the commonly used topical agent, i.e. KMnO4, and to enhance the awareness of this condition for prompt management. It also highlights the importance of proper history taking in the OPD or the emergency.
A 6-year-old girl was brought by her father in emergency to eye department of our hospital with severe pain, redness, and swelling of right eye [Figure 1]. According to her father, he was using KMnO4 crystals [Figure 2] for his acute eczema. The child had been playing alone in a room where KMnO4 crystals were kept in a box. The child opened the box and accidentally, the loose crystals fell inside her eye. She was immediately brought to the hospital. At the emergency room, on examination, general physical condition was normal. Her vitals were within normal limit and there were no signs of systemic toxicity. On local examination, her right eyelid was grossly swollen and tender. Left eye was not involved. Brown staining was seen over the tongue and neck [Figure 3(a) and 3(b)]. Considering it as a chemical ocular injury, she was immediately taken to the minor OT. Copious irrigation was done with a balanced salt solution for approximately 30 min. Balanced saline solution was used in this condition because it is a sterile cleansing solution that provides the cells with water and inorganic ions while maintaining a physiological pH and osmotic pressure. The loose impacted crystals were removed from the inferior fornix with the help of sterile cotton buds [Figure 4(a) and 4(b)]. Few brown splotches could not be flushed out. The staining of neck and tongue was cleaned with normal saline.
Figure 1.

Pain, redness, and swelling in the right eye
Figure 2.
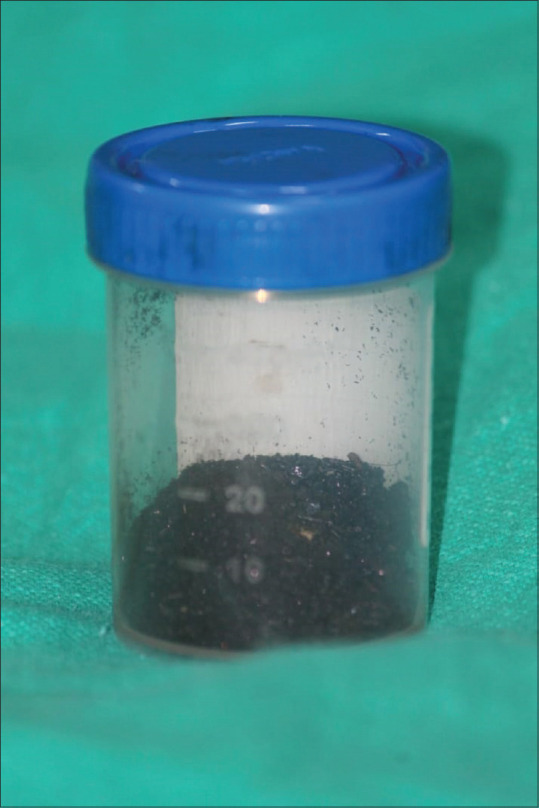
Potassium permanganate crystals
Figure 3.

(a) Brown staining of tongue. (b) Brown staining of neck
Figure 4.
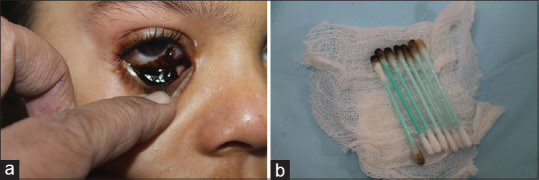
(a) Impacted crystals in conjunctiva. (b) Crystals removed with the help of earbuds
After removal of the debris, her visual acuity was 6/24. Slit-lamp examination revealed stained and congested conjunctival mucosa with debris and mucus shreds. According to Dua classification, there was more than 30% of conjunctival involvement and more than 3-6 clock hours of limbal involvement (Grade III). Cornea was hazy due to corneal edema.
The patient was put on 0.5% moxifloxacin eye drops 4 times a day, 1% prednisolone eye drops every 2 hours for the initial 10 days to reduce inflammation, and preservative-free lubricant eye drop hourly. Along with this, the patient also received tablet vitamin C 500 mg three times a day. Doxycycline was not considered due to her age.
Gradually, all KMnO4 stains had disappeared. The child started showing signs of improvement with the medications but her ocular movements were restricted due to pseudomembrane formation between globe and lid margin. After 7 days of injury, the pseudomembrane was removed under general anesthesia. There was no requirement for amniotic grafting in this case. Following surgery, the child showed speedy recovery with the healing of conjunctiva [Figure 5]. After 4 weeks of regular treatment and follow up, the corneal edema subsided, complete epithelialization of conjunctiva was seen, and the patient recovered completely with visual acuity 6/6 [Figure 6].
Figure 5.

Early recovery of eye
Figure 6.

Complete recovery of the eye
Across the world, chemical burn injury constitutes about 515% of the total ocular injuries.[1] Over the last three decades, there are multiple publications in which KMnO4 toxicity has been reported like ocular burns, hepatic failure, gastric mucosa injury, pancreatitis, and methaemoglobinaemia.[2,3,4] Majority of the ocular chemical injury are usually mild and accidental. The chemicals commonly responsible for such injuries are fertilizers, detergents, acids like sulfuric acid, acetic acid, nitric acid, and alkalis like sodium hydroxide and ammonium hydroxide. The severity of the burns is directly related to the type of causative agents (acids or alkali) and the duration of exposure.
Chemical injuries due to potassium permanganate are rarely reported injury because of its minimal household and industrial use. In our case, the patient sustained eye injury by accidental instillation of KMnO4 crystals. It is a powerful caustic chemical that leads to coagulative necrosis of tissue. Its probable lethal dose is 10 g4.[5] Clinically, it presents with brown staining of the surrounding skin, severe pain, redness, and burning sensation in eye. Rarely, it can cause permanent loss of vision also.
Immediate management of such injuries is important as it prevents complications and improves the outcome. They can be managed on the same lines of burn and other chemical injuries. The mainstay of treatment is immediate and adequate decontamination. It is necessary to immediately wash out the offending agents by extensive irrigation. The most ideal fluid is ringer lactate as its osmolarity is similar to aqueous humour. Any residual granular material should be removed carefully. In acute stages, topical steroid plays an important role in controlling inflammation. If required, topical antibiotics are given in order to prevent secondary infection. In severe cases, where there are ocular surface deformation and early development of symblepharon, amniotic membrane is used as an adjunctive treatment.
Limitation
In our case, the patient could not be followed up for a longer duration. Longer follow-ups are required to ensure the presence or absence of side effects of such injuries.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient's father has given his consent for publication of the information in this journal. The parents understand that names and initials will not be published and due efforts will be made to conceal their child identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Herr RD, White GL, Bernhisel K, Mamalis N, Swanson E. Clinical comparison of ocular irrigation fluids following chemical injury. Am J Emerg Med. 1991;9:228–31. doi: 10.1016/0735-6757(91)90082-u. [DOI] [PubMed] [Google Scholar]
- 2.Baron S, Moss C. Caustic burn caused by potassium permanganate. Arch Dis Child. 2003;88:96. doi: 10.1136/adc.88.2.96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ong KL, Tan TH, Cheung WL. Potassium permanganate poisoning--A rare cause of fatal self-poisoning. J Accid Emerg Med. 1997;14:43–5. doi: 10.1136/emj.14.1.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chirapapaisan C, Prabhasawat P, Srivannaboon S, Roongpoovapatr V, Chitsuthipakorn P. Ocular injury due to potassium permanganate granules. Case Rep Ophthalmol. 2018;9:132–7. doi: 10.1159/000486922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Younan L, Eloubeidi M, Barada K. A rare cause of caustic gastric injury in a young man. Gastroenterology. 2013;145:60–260. doi: 10.1053/j.gastro.2013.04.017. [DOI] [PubMed] [Google Scholar]


