Abstract
Context:
Follicular keratotic disorder is an abnormal keratinization affecting the follicular orifices and clinically characterized by hyperkeratotic follicular papules affecting various sites. Dermoscopy is a non-invasive diagnostic tool and differentiates closely resembling diseases as well as possibly prevents need for an invasive biopsy.
Aim:
This study was aimed to find the correlation between clinical, dermoscopic and histopathological findings in follicular keratotic diseases and to establish the dermoscopic criteria in the diagnosis of primary follicular keratotic diseases.
Materials and Methods:
This was a hospital-based prospective cross-sectional study of 30 consecutive patients clinically diagnosed with follicular keratotic diseases, irrespective of age and duration of the disease.
Results:
The study consisted of 30 patients with a mean age of 19.57 ± 9.69 years. The most common primary follicular keratotic disease observed was phrynoderma and secondary follicular keratotic disease was follicular lichen planus (lichen planopilaris). The predominant dermoscopic finding among all the follicular keratotic diseases was perifollicular scaling 29 (96.7%) followed by keratotic plug 28 (93.3%). The most common histopathological feature was dilated follicular infundibulum 22 (73.3%) followed by follicular plug 15 (50%) and dermal perivascular infiltration 22 (73.3%). The clinical and dermoscopic features showed a significant statistical association with the histopathological findings.
Conclusion:
Dermoscopy is a simple, non-invasive diagnostic tool that helps in differentiating and diagnosing the closely resembling follicular keratotic diseases.
Keywords: Dermoscopy, follicular keratotic diseases, histopathology
Introduction
Follicular keratotic disease is an abnormal keratinization affecting the follicular orifices. It clinically presents as hyperkeratotic papules with prominent keratin plug affecting various sites and histologically characterized by orthokeratosis of follicular ostium and infundibulum. Follicular keratotic diseases can be grouped as (a) primary follicular keratotic diseases – phrynoderma, keratosis pilaris, lichen spinulosis and pityriasis rubra pilaris and (b) follicular variants of psoriasis, lichen planus, eczema, etc.[1,2]
This study was carried out to find the correlation between clinical, histopathological and dermoscopic findings in follicular keratotic diseases and propose diagnostic dermoscopic criteria. Formulating objective and reproducible dermoscopic criteria would assert the clinical diagnosis and differentiate closely resembling diseases and possibly prevent the need for an invasive biopsy.
Materials and Methods
The study was a hospital-based cross-sectional study of 30 patients clinically diagnosed with follicular keratotic diseases, irrespective of age, sex or duration of the disease. Patients with ongoing or having received treatment in the past 4 weeks were not included. Informed consent was obtained from all the participating subjects. Institutional ethical committee clearance was obtained for the study.
Biodata of the patients, relevant history, clinical and dermoscopic examination findings were recorded. The skin lesions were evaluated using DermLite™ DL3 (3Gen Inc., San Juab Capistrano, CA, USA) under polarized mode. Skin biopsy for histopathological examination was performed. Dermoscopic and histopathological features of individual follicular keratotic disorders were studied. The data obtained were subjected to statistical analysis using the SPSS software version 23 (IBM Statistics, Chicago, USA). Results were presented as mean ± SD, counts and percentages. Categorical variables were compared using Chi-square test while the quantitative variables were compared using independent t test. For all the tests, significance was achieved at P < 0.05. All statistical tests performed were two tailed.
Results
Among the 30 patients clinically diagnosed with follicular keratotic diseases, primary follicular keratotic diseases were observed in 22 (73.3%) and secondary follicular keratotic diseases in 8 (26.7%). All the patients had follicular keratotic papules distributed in a discrete [26 (86.7%)], or grouped manner [4 (13.3%)]. Majority had the lesions confined to upper extremities and trunk.
Dermoscopy and histopathological findings
The predominant dermoscopic finding observed was perifollicular scaling in 29 (96.7%) patients followed by keratotic plug in 28 (93.3%), and majority of the patients showed white scales 29 (96.7%). The dermoscopic findings of individual follicular keratotic diseases observed were perifollicular white halo, interfollicular hyperpigmentation with prominent skin markings in phrynoderma; perifollicular erythema, coiled and twisted hair in keratosis pilaris; perifollicular erythema with irregularly arranged red dots in pityriasis rubra pilaris; perifollicular white areas with normal interfollicular area in lichen spinulosis; perifollicular erythema and white halo, interfollicular area blue-gray dots, white dots and reduced follicular ostia in follicular lichen planus; regular arrangement of follicular red dots in follicular psoriasis; and interfollicular hyperpigmentation with prominent skin markings and irregularly arranged red dots were observed in one case of follicular eczema [Table 1].
Table 1.
Dermoscopic findings of follicular keratotic diseases
| Dermoscopic findings | Phrynoderma (n=7) n (%) | Keratosis pilaris (n=6) n (%) | PRP (n=5) n (%) | Lichen spinulosis (n=4) n (%) | Follicular LP (n=5) n (%) | Follicular psoriasis (n=2) n (%) | Follicular eczema (n=1) n (%) | P |
|---|---|---|---|---|---|---|---|---|
| Follicular & perifollicular features | ||||||||
| Perifollicular scaling | 7 (100%) | 5 (83.3%) | 5 (100%) | 4 (100%) | 5 (100%) | 2 (100%) | 1 (100%) | 0.658 |
| Keratotic plug | 7 (100%) | 6 (100%) | 4 (80%) | 3 (75%) | 5 (100%) | 2 (100%) | 1 (100%) | 0.535 |
| Perifollicular erythema | 1 (14.28) | 5 (83.3%) | 3 (60%) | 0 (0.0) | 3 (60%) | 0 (0.0) | 0 (0.0) | 0.0437* |
| Perifollicular fibrosis | 5 (71.48%) | 0 (0.0) | 0 (0.0) | 2 (50%) | 3 (60%) | 0 (0.0) | 0 (0.0) | 0.036* |
| Perifollicular | 0 (0.0) | 0 (0.0) | 0 (0.0) | 3 (75%) | 0 (0.0) | 0 (0.0) | 0 (0.0) | <0.001* |
| White areas | ||||||||
| Interfollicular area | ||||||||
| Normal | 2 (28.57%) | 3 (50%) | 2 (40%) | 4 (100%) | 1 (20%) | 2 (100%) | 0 (0.0) | 0.117 |
| Hyperpigmentation | 4 (57.14%) | 3 (50%) | 1 (20%) | 0 (0.0) | 4 (80%) | 0 (0.0) | 1 (100%) | 0.109 |
| Erythema | 0 (0.0) | 1 (16.7%) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0.658 |
| Prominent skin markings | 4 (57.14%) | 0 (0.0) | 1 (20%) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (100%) | 0.026* |
| White area | 0 (0.0) | 0 (0.0) | 1 (20%) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0.522 |
| Blue-gray dots | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 5 (100%) | 0 (0.0) | 0 (0.0) | <0.001* |
| White dots | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 5 (100%) | 0 (0.0) | 0 (0.0) | <0.001* |
| Reduced follicular ostia | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 5 (100%) | 0 (0.0) | 0 (0.0) | <0.001* |
| Color of scales | ||||||||
| White | 7 (100%) | 5 (83.3%) | 5 (100%) | 4 (100%) | 5 (100%) | 2 (100%) | 1 (100%) | 0.658 |
| Type of hair | ||||||||
| Coiled | 3 (42.86%) | 6 (100%) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 2 (100%) | 0 (0.0) | 0.007* |
| Twisted | 1 (14.28%) | 4 (66.7%) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 2 (100%) | 0 (0.0) | 0.007* |
| Type of vessel | ||||||||
| Red dots | 0 (0.0) | 0 (0.0) | 3 (60%) | 0 (0.0) | 0 (0.0) | 2 (100%) | 1 (100%) | 0.001* |
| Total | 7 (100%) | 6 (100%) | 5 (100%) | 4 (100%) | 5 (100%) | 2 (100%) | 1 (100%) |
The predominant histopathological findings observed among all the patients were dilated hair follicle [22 (73.3)], follicular plugs [15 (50%)], keratin [9 (30%)], and perivascular [22 (73.3%)] and perifollicular [17 (56.7%)] lymphocytic infiltration. Additionally, follicular lichen planus showed basal cell vacuolization and pigment incontinence. Elongated, club-shaped rete ridges and dilated capillaries were seen in one patient each of follicular psoriasis. Perifollicular spongiosis, perifollicular orthokeratosis and dilated capillaries were seen in follicular eczema [Table 2]. The dermoscopic-histologic correlation observed has been outlined in Table 3.
Table 2.
Histopathological findings of follicular keratotic diseases
| Histopathological findings | Phrynoderma (n=7) n (%) | Keratosis pilaris (n=6) n (%) | PRP (n=5) n (%) | Lichen spinulosis (n=4) n (%) | Follicular LP (n=5) n (%) | Follicular psoriasis (n=2) n (%) | Follicular eczema (n=1) n (%) | P |
|---|---|---|---|---|---|---|---|---|
| Epidermal changes | ||||||||
| Hyperkeratosis | 4 (57.14%) | 0 (0.0) | 1 (20%) | 0 (0.0) | 1 (20%) | 2 (100%) | 1 (100%) | 0.0273* |
| Parakeratosis | 1 (14.28%) | 0 (0.0) | 4 (80%) | 0 (0.0) | 0 (0.0) | 1 (50%) | 0 (0.0) | 0.001* |
| Orthokeratosis | 0 (0.0) | 1 (16.67%) | 1 (20%) | 1 (25%) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0.7415 |
| Acanthosis | 2 (28.7%) | 0 (0.0) | 1 (20%) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0.5137 |
| Spongiosis | 1 (14.28%) | 0 (0.0) | 3 (60%) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0.0477* |
| Basal layer | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 2 (40%) | 0 (0.0) | 0 (0.0) | 0.097 |
| a) Vacuolization | ||||||||
| b) Pigment incontinence | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 5 (100%) | 0 (0.0) | 0 (0.0) | <0.001* |
| Reteridges | 0 (0.0) | 0 (0.0) | 3 (60%) | 0 (0.0) | 0 (0.0) | 1 (50%) | 0 (0.0) | 0.018* |
| Epidermal thinning | 1 (14.28%) | 2 (33.3%) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (50%) | 0 (0.0) | 0.374 |
| Dermal changes | ||||||||
| a) Hair changes | 6 (85.71%) | 6 (100%) | 1 (20%) | 3 (75%) | 5 (100%) | 1 (50%) | 1 (100%) | 0.0326* |
| Dilated hair follicle | ||||||||
| Keratin | 4 (57.14%) | 2 (33.3%) | 0 (0.0) | 0 (0.0) | 2 (40%) | 0 (0.0) | 1 (100%) | 0.041* |
| Follicular plug | 4 (57.14%) | 4 (66.67%) | 1 (20%) | 1 (25.0) | 4 (80%) | 0 (0.0) | 1 (100%) | 0.163 |
| Perifollicular parakeratosis | 0 (0.0) | 1 (16.67%) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0.658 |
| Perifollicular orthokeratosis | 0 (0.0) | 1 (16.67%) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (100%) | 0.0108* |
| Perifollicular spongiosis | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (100%) | <0.001* | |
| b) Blood vessels | 0 (0.0) | |||||||
| c) Sebaceous glands | 0 (0.0) | 0 (0.0) | 2 (40%) | 0 (0.0) | 0 (0.0) | 1 (50%) | 0 (0.0) | 0.085 |
| d) Inflammation | 0 (0.0) | 1 (16.67%) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0.658 |
| Lymphocytic infiltration | 3 (42.86%) | 3 (50%) | 2 (40%) | 3 (75%) | 4 (80%) | 1 (50%) | 1 (100%) | 0.721 |
| i) perifoll nexal | 4 (57.14%) | 5 (83.33%) | 4 (80%) | 4 (100%) | 2 (40%) | 2 (100%) | 1 (100%) | 0.418 |
| Lymphohistiocytic | 5 (71.42%) | 2 (33.33%) | 2 (40%) | 2 (50.0%) | 3 (60%) | 0 (0.0) | 1 (100%) | 0.499 |
| Infiltration | ||||||||
| i) perifollicular | 1 (14.28) | 1 (16.67%) | 0 (0.0) | 0 (0.0) | 1 (20%) | 0 (0.0) | 0 (0.0) | 0.207 |
| ii) perivascular | 1 (14.28) | 1 (16.67%) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0.082 |
| e) Fibrosis | 0 (0.0) | 1 (16.67%) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0.6580 |
Table 3.
Statistical association between dermoscopic and histopathological correlation
| Dermoscopy features | HPE findings | P |
|---|---|---|
| Perifollicular scaling | Hyperkeratosis | 0.611 |
| Prominent skin markings with hyperpigmentation | hyperkeratosis and acanthosis with melanin | 0.014* |
| Perifollicular white halo | Dermal fibrosis | 0.472 |
| Keratotic plug | Keratin-filled follicular infundibula | 1.000 |
| Blue-gray dots | Pigment incontinence into the dermis | <0.001* |
| Red dots | Dilated dermal blood vessels | 0.001* |
Regarding the dermoscopic-histopathologic correlation [Table 3], follicular features like keratotic plugs observed on dermoscopy correspond to keratin-filled follicular infundibula in histology; perifollicular features like erythema and white halo correspond to dilated perifollicular dilated dermal vessels and fibrosis, respectively. The perifollicular pigmentation with prominent skin markings seen in phrynoderma correspond to the hyperkeratosis and acanthosis of the interfollicular epidermis, and the interfollicular red dots and blue-gray dots correspond to the dilated dermal vessels and pigment incontinence.
Discussion
Follicular keratotic disease is an abnormal keratinization affecting the follicular orifices, clinically presenting as hyperkeratotic papules with prominent keratin plug affecting various sites of the body and histologically characterized by orthokeratosis of follicular ostium and infundibulum.[1,2] Dermoscopy is a non-invasive imaging technique that serves as a useful rapid diagnostic tool.[3] The use of dermoscopy to assert the clinical diagnosis and differentiate closely resembling follicular keratotic diseases is the highlight of this study.
In this cross-sectional study, we report findings in 30 patients with follicular keratotic diseases. Among 30 patients, 14 (46.7%) were males and 16 (53.3%) were females (F:M ratio 1.14:1). The age of patients ranged from 4 years to 40 years with a mean age of 19.57 ± 9.69 years. Adolescents in the age group of 10-19 years constituted the majority of study population with a maximum of 12 (40%) patients followed by adult population 8 (26.7%) in the age group 20-29 years.
Dermoscopy and histopathology findings in primary follicular keratotic diseases
Phrynoderma
Phrynoderma is a type of follicular keratosis that occurs due to multiple nutritional deficiencies such as vitamin A, vitamin B-complex, vitamin E and essential fatty acid deficiency and protein-calorie malnutrition. It is clinically characterized by follicular papules with keratotic plug predominantly distributed over extensor aspects of elbows, knees, gluteal area, extensor arms and forearms, thighs and back [Figure 1a].[4]
Figure 1.

Phrynoderma: discrete and confluent, skin colored and hyperpigmented follicular papules with central keratinous plug over elbows and forearms [a]. Dermoscopy shows perifollicular scaling (black arrow), keratin plug (yellow arrow), perifollicular gray-white halo indicative of fibrosis (black star), and hyperpigmentation with prominent skin markings of the interfollicular area (yellow stars) [b]. [Dermoscopy, polarized non-contact, x10]
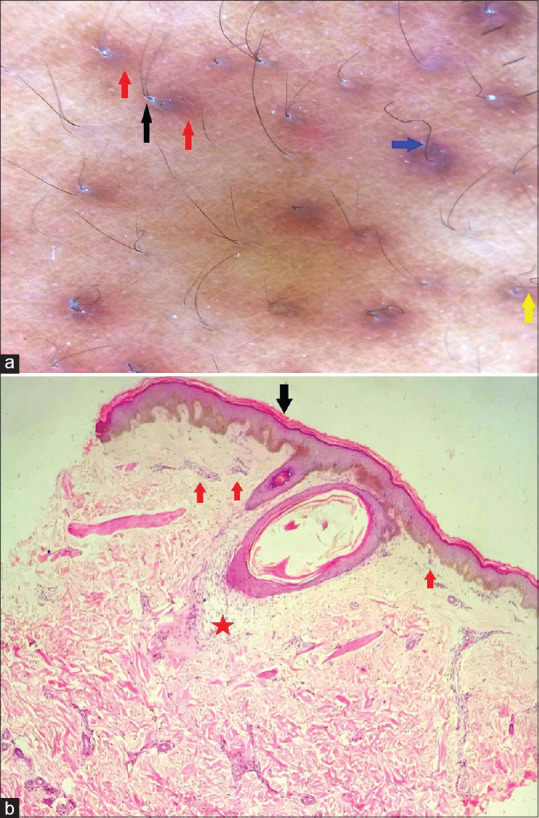
Among the 7 (23.3%) cases of phrynoderma, dermoscopy revealed perifollicular white halo in 5 (71.42%), and interfollicular hyperpigmentation with prominent skin markings in 4 (57.14%) patients each. Also, coiled hair were seen in 3 (42.86%) patients followed by twisted hair in one (14.28%) patient [Figure 1b]. The dermoscopic features of phrynoderma have not been reported in the literature thus far. The predominant histopathological findings were epidermal hyperkeratosis, dilated hair follicles, follicular plug and keratin, and periadnexal, perivascular and perifollicular lymphocytic infiltration. These observations were similar to those made in a study by Raghunatha et al.[4] The dermoscopic-histopathologic correlation is depicted in Figure 2a and b.
Figure 2.

Dermoscopic-histopathologic correlat ion in phrynoderma [a and b]: The follicular plugging on dermoscopy corresponds to the dilated follicular infundibulum filled with keratin debris (yellow arrow), perifollicular scaling to the hyperkeratosis of stratum corneum (black arrow), perifollicular white halo to the dermal fibroplasias around the follicles (black star) and the interfollicular hyperpigmentation with prominent skin markings to the acanthosis, papillomatosis and elongation of rete ridges of the epidermis (yellow star). [Dermoscopy, polarized non-contact, x10; H and E, x10]
Keratosis pilaris
Keratosis pilaris is characterized by keratin plugs in the follicular orifices with or without perifollicular erythema.[5] It is characterized by minute, gooseflesh-like, horny plugs at the follicular orifices distributed predominantly on the posterolateral aspect of the thighs, upper arms, gluteal area and legs [Figure 3a].[6]
Figure 3.

Keratosis pilaris: discrete erythematous and hyperpigmented follicular keratotic papules over upper arms and back [a]. Dermoscopy shows perifollicular scaling (black arrow), perifollicular erythema (red arrows), coiled (yellow arrow) and twisted (blue arrow) hair [b]. [Dermoscopy, polarized non-contact, x10]
The predominant dermoscopic findings observed among the six cases were perifollicular erythema, interfollicular hyperpigmentation and coiled and twisted hair [Figure 3b]. Our observations were in concurrence with the study by Thomas et al.[5] and Sonthalia et al.[7] wherein they observed perifollicular erythema, perifollicular scaling and coiled and twisted hair. Histopathology in our study revealed epidermal orthokeratosis, dilated hair follicles, follicular plug, keratin, perifollicular parakeratosis and orthokeratosis, and perivascular and periadnexal lymphocytic infiltrate as predominant findings. These features were in line with those observed by Sonthalia et al.[7] The dermoscopic-histopathologic correlation is depicted in Figure 4a and b.
Figure 4.
Dermoscopic-histopathologic correlation in keratosis pilaris [a and b]: The perifollicular scaling on dermoscopy corresponds to the hyperkeratosis around the follicles (black arrow) and the perifollicular erythema to the inflammatory reaction around the follicles as shown by dilated vessels with perivascular infiltrate (red arrows) and perifollicular infiltrate (red star). [Dermoscopy, polarized non-contact, x10; H and E, x5]
Pityriasis rubra pilaris
Pityriasis rubra pilaris (PRP) is a rare chronic disorder of keratinization characterized by keratotic follicular papules, palmoplantar keratoderma and reddish orange scaly plaques that coalesce to form widespread lesions with islands of normal skin (nappes claires).[8]
In this present study, follicular plugging was the most frequent observation on dermoscopy followed by perifollicular erythema. Interfollicular hyperpigmentation and lichenification were observed in one patient each. Red dots arranged in irregular pattern were seen in 3 (60%) patients [Table 1]. A similar dermoscopic pattern was observed by Moretta et al.,[9] Kumar et al.[10] and Nair et al.[11]
The predominant histopathological findings were epidermal parakeratosis, hyperkeratosis, orthokeratosis and acanthosis. Spongiosis and broad and shortened rete ridges were observed in 3 (60%) patients each. This was in line with the observations made by Sehgal et al.[12] and Nair et al.[11]
Lichen spinulosus
Lichen spinulosus (LS) is a disorder of keratinization of hair follicles usually seen in association with atopy, infections, id reaction to fungal infection or drug reactions. It is characterized by the development of grouped, asymptomatic minute, flesh colored, follicular horny papules, with central spinous process distributed symmetrically on the trunk, limbs and buttocks with sparing of face, hands and feet [Figure 5a].[13]
Figure 5.

Lichen spinulosus: Clusters of grouped follicular keratotic papules with central spinous process present over arm [a]. Dermoscopy of lichen spinulosis shows perifollicular scaling (red arrow), follicular plug (black arrow), perifollicular white halo (yellow arrows) with normal interfollicular area [b]. [Dermoscopy, polarized non-contact, x10]
Dermoscopy showed perifollicular scaling and normal interfollicular area in all the patients. Keratotic plug and perifollicular white areas were the other findings [Figure 5b]. The dermoscopic features of LS have not been reported in the literature as yet.
Histopathology showed no significant changes in the epidermis. The dermis showed dilated follicular infundibulum, follicular plug, perivascular, perifollicular and periadnexal lymphocytic infiltration. This was in accordance with the findings of Kim et al.[13] The dermoscopic-histologic correlation is described in Figure 6a and b.
Figure 6.

Dermoscopic-histopathologic correlation in lichen spinulosus [a and b]: Perifollicular scaling corresponds to the perifollicular hyperkeratosis (red arrow), follicular plug to the keratinous material in the follicular orifice (black arrow) and the perifollicular white halo to the acanthosis of the perifollicular epidermis (black star). [Dermoscopy, polarized non-contact, x10; H and E, x5]
Secondary follicular keratotic diseases
Follicular lichen planus (lichen planopilaris)
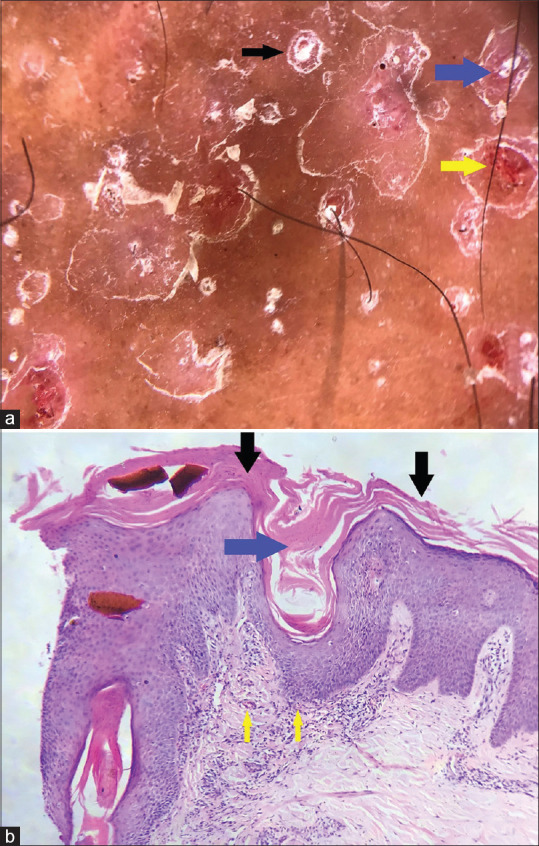
Lichen planopilaris is the most common form of follicular LP and is characterized by inflammation of the upper portion of the hair follicle that results in follicular scarring and irreversible hair loss.[14] The dermoscopic findings in our study revealed follicular keratin plug, perifollicular scaling, interfollicular blue-gray and white dots, and reduced follicular ostia in all the patients. Perifollicular erythema and perifollicular white halo were seen in 3 (60%) patients each [Figure 7a]. Nirmal et al.[15] have observed similar features.
Figure 7.

Lichen planopiaris: Dermoscopy shows perifollicular scaling (black arrows), follicular fibrosis (red arrow), areas of absent follicles (black circle) and interfollicular blue-gray dots (blue arrows) [a]. Histologically, the blue-gray dots correspond to the upper dermal melanin incontinence (blue arrows) and perifollicular scaling to the infundibular hyperkeratosis (black arrows) [b]. [Dermoscopy, polarized non-contact, x10; H and E, x5]
The predominant histopathological findings were epidermal hyperkeratosis, basal cell vacuolization, pigment incontinence in the basal layer, dilated follicular infundibulum, follicular plugging and band-like lymphocytic infiltration in the upper dermis [Figure 7b]. These observations were in accordance with those made by Nirmal et al.[15]
Follicular psoriasis
Follicular psoriasis is an underrecognized entity and affects adults more commonly than children. In adults, it presents as multiple, discrete and follicular hyperkeratotic papules predominantly, and in children as asymmetric, grouped, follicular and keratotic papules predominantly affecting the trunk, axilla and extensor aspects of limbs and resembling PRP [Figure 8a].[16]
Figure 8.

Follicular psoriasis: Grouped follicular white scaly keratotic papules on the shin [a]. Dermoscopy shows follicular keratotic plugging (blue arrows), perifollicular white scaling (black arrows), and follicular red dots (yellow arrow) [b]. [Dermoscopy, polarized non-contact, x10]
The predominant dermoscopic observations in the two cases were perifollicular scaling, keratotic plug with normal interfollicular area and twisted hair. Regular arrangement of follicular red dots was observed in both the patients [Figure 8b]. Similar features have been reported by Behera et al.[17] The histopathological features seen were epidermal hyperkeratosis, parakeratosis, elongated club-shaped rete ridges, dilated hair follicle, and perivascular and perifollicular lymphocytic infiltration with dilated papillary dermal capillaries. The dermoscopic findings of perifollicular scaling and regularly arranged blood vessels correspond to hyperkeratosis and dilated capillaries histologically. The dermoscopic-histologic correlation is described in Figure 9a and b.
Figure 9.
Dermoscopic-histopathologic correlation in follicular psoriasis [a and b]: The follicular plugging corresponds to keratin-filled follicular infundibulum (blue arrows), perifollicular scaling to the hyperkeratosis and parakeratosis around the follicles (black arrows), and the follicular red dots to the perifollicular dilated vessels (yellow arrows). [Dermoscopy, polarized non-contact, x10; H and E, x5]
Follicular eczema
Follicular eczema is usually seen on the extensor aspect of the extremities [Figure 10a].[18] The dermoscopic features observed were follicular keratotic plug with perifollicular scaling, interfollicular hyperpigmentation with prominent skin markings and irregularly arranged red dots [Figure 10b]. Dermoscopic features of follicular eczema have not yet been reported in the literature. Histopathology revealed epidermal hyperkeratosis and spongiosis; dilated follicular infundibulum with keratin plug, perifollicular spongiosis, perifollicular orthokeratosis, and perifollicular; perivascular, periadnexal and lymphocytic infiltration. Sardana et al.[18] in their study noted a similar finding of spongiotic dermatitis localized to the upper portion of hair follicle.
Figure 10.

Follicular eczema: Follicular and non-follicular erythematous papules on the extensor forearms [a]. Dermoscopy shows follicular keratotic plugging (black arrows), perifollicular white scaling (white arrows), interfollicular red dots (red arrow), and interfollicular hyperpigmentation and prominent skin markings (black star) [b]. [Dermoscopy, polarized non-contact, x10]
Limitations of the study
The main limitation of the study is the low sample size, and hence, the proposed algorithm for dermoscopic diagnosis of primary follicular keratotic disorders needs further validation.
Conclusion
Our study describes the utility of dermoscopy is a non-invasive, quick and office-based diagnostic tool to differentiate closely resembling follicular keratotic diseases.
Dermoscopically, perifollicular white areas in lichen spinulosis; the coiled and twisted hair in keratosis pilaris, phrynoderma and follicular psoriasis; interfollicular area blue-gray dots, white dots, reduced follicular ostia in lichen planopilaris, and the interfollicular red dots in PRP, follicular eczema and follicular psoriasis showed a strong statistical association as outlined in Table 1. Figure 11 depicts the proposed dermoscopic algorithm for primary follicular keratotic diseases.
Figure 11.

Proposed dermoscopic algorithm for diagnosis of primary follicular keratotic disorders
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Hsiao JL, Leslie KS, McMichael AJ, Curtis AR, Sanchez DG. Folliculitis and other follicular disorders. In: Bolognia JL, Schaffer JV, Cerroni L, editors. Dermatology. 4th ed. Philadelphia: Elsevier Saunders; 2018. pp. 615–32. [Google Scholar]
- 2.Bruckner AL. Keratosis Pilaris and other follicular keratotic disorders. In: Kang S, Amagai M, Bruckner AL, Enk AH, Margolis DJ, McMichael AJ, Orringer JS, editors. Fitzpatrick's Dermatology in General Medicine. 9th ed. McGraw-Hill; 2019. pp. 867–76. [Google Scholar]
- 3.Zalaudek I, Argenziano G, Di Stefani A, Ferrara G, Marghoob AA, Hofmann- Wellenhof R, et al. Dermoscopy in general dermatology. Dermatology. 2006;212:7–18. doi: 10.1159/000089015. [DOI] [PubMed] [Google Scholar]
- 4.Ragunatha S, Kumar VJ, Murugesh SB. A clinical study of 125 patients with phrynoderma. Indian J Dermatol. 2011;56:389–92. doi: 10.4103/0019-5154.84760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Thomas M, Khopkar US. Kerotosis pilaris revisited: Is it more than just a Follicular Keratosis? Int J Trichology. 2012;4:255–8. doi: 10.4103/0974-7753.111215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chu AC, Teixeira F. Acquired disorders of epidermal keratinization. In: Griffiths C, Barker J, Bleiker T, Chalmers R, Creamer D, editors. Rook's Textbook of Dermatology. 9th ed. London: Blackwell Science; 2016. pp. 87.1–87.30. [Google Scholar]
- 7.Sonthalia S, Bhatia J, Thomas M. Dermoscopy of keratosis pilaris. Indian Dermatol Online J. 2019;10:613–4. doi: 10.4103/idoj.IDOJ_279_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chu AC. Pityriasis rubra pilaris. In: Griffiths C, Barker J, Bleiker T, Chalmers R, Creamer D, editors. Rook's Textbook of Dermatology. 9th ed. London: Blackwell Science; 2016. pp. 36.1–36.7. [Google Scholar]
- 9.Moretta G, De Luca EV, Di Stefani A. Management of refractory pityriasis rubra pilaris: Challenges and solutions. Clin Cosmet Investig Dermatol. 2017;10:451–7. doi: 10.2147/CCID.S124351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kumar S, Vinay K, Radotra BD. Dermoscopy of erythrodermic pityriasis rubra pilaris. Indian Dermatol Online J. 2019;10:500–1. doi: 10.4103/idoj.IDOJ_156_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nair PA, Sheth N. Dermoscopy of juvenile circumscribed pityriasis rubra pilaris. Indian Dermatol Online J. 2018;9:474–6. doi: 10.4103/idoj.IDOJ_334_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sehgal VN, Srivastava G, Dogra S. Adult onset pityriasis rubra pilaris. Indian J Dermatol Venereol Leprol. 2008;74:311–21. doi: 10.4103/0378-6323.42889. [DOI] [PubMed] [Google Scholar]
- 13.Kim SH, Kang JH, Seo JK, Hwang SW, Sung HS, Lee D. Successful treatment of lichen spinulosis with topical tacalcitol cream. Pediatr Dermatol. 2010;27:546–7. doi: 10.1111/j.1525-1470.2010.01275.x. [DOI] [PubMed] [Google Scholar]
- 14.Messenger AG, Sinclair RD, Farrant P, Berker DAR. Acquired disorders of hair. In: Griffiths C, Barker J, Bleiker T, Chalmers R, Creamer D, editors. Rook's Textbook of Dermatology. 9th ed. London: Blackwell Science; 2016. pp. 89.1–89.77. [Google Scholar]
- 15.Nirmal B, George R, Kodiatte TA. Invisible lichen planopilaris unmasked by dermatoscopy. Int J Trichology. 2017;9:76–8. doi: 10.4103/ijt.ijt_81_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Souza BC, Bandeira LG, Cunha TAC, Valente NYS. Follicular psoriasis: An underdiagnosed entity? An Bras Dermatol. 2018;94:116–8. doi: 10.1590/abd1806-4841.20197987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Behera B, Gochhait D, Remya R, Resmi MR, Kumari R, Thappa DM. Follicular psoriasis - dermoscopic features at a glance. Indian J Dermatol Venereol Leprol. 2017;83:702–4. doi: 10.4103/ijdvl.IJDVL_12_17. [DOI] [PubMed] [Google Scholar]
- 18.Sardana K, Arora P, Mishra D. Follicular eczema: A commonly misdiagnosed dermatosis. Indian Pediatr. 2012;49:599. doi: 10.1007/s13312-012-0111-8. [DOI] [PubMed] [Google Scholar]


