To the Editor:
Recent studies have uncovered remarkably elevated rates of allergic disease among Asian immigrants to Australia,1 and previous studies in the United Studies suggest that children of Asian immigrants may have higher risks of eczema and food allergy but lower rates of asthma.2,3 However, because nationally representative surveys typically have small numbers of Asian participants, there is little population-level data on the prevalence of allergic diseases among Asian children in the United States. The National Health Interview Survey provides a unique data source to explore the effect of Asian race on allergy as Asians were oversampled beginning in 2006. Using National Health Interview Survey data from 2007 to 2016, we sought to determine the prevalence of allergic disease among Asian-American children and to examine the contribution of child and parental migration to estimates of disease burden.
Children 17 years and younger were included. Allergic conditions and race were defined on the basis of self-report. Children of Asian race were further questioned about Asian subcategory, and data on Asian-Indian, Chinese, and Filipino subcategories were made available. Other Asian subpopulations were grouped for purposes of analysis on the basis of small sample size. Survey weights, sampling units, and strata were used in all analyses to create a nationally representative sample and account for the complex survey design. We first examined the overall prevalence of allergic diseases by race. Next, to understand the effects of race independent of age, sex, family income relative to federal poverty level, and parental and child nativity, we used multivariable logistic regression models that included these factors. Interaction terms and stratification were used to evaluate for effect modification by race and age (see this article’s Methods section in the Online Repository at www.jacionline.org), and analyses of Asian subpopulations were performed. All analyses used Stata/IC version 14.2 (Stata Corporation, College Station, Tex), and non-Hispanic white children were used as the reference population, except for subpopulation analyses, in which non-Asian children were used as the reference population because of constraints of sampling methodology (see this article’s Methods section in the Online Repository).
Sample size and demographic information are presented in Tables E1 and E4 in this article’s Online Repository at www.jacionline.org. In unadjusted analyses, Asian children had somewhat higher rates of food allergy (6.2% vs 5.5%) and eczema (11.8% vs 11.2%), and lower rates of asthma (5.7% vs 9.0%), than non-Hispanic white children (see Tables E1 and E5 in this article’s Online Repository at www.jacionline.org). This was true even though Asian children had much higher rates of birth outside the United States (20.3% vs1.5%) and foreign-born parents (76.9% vs 6.2%) than did white children, factors that were both found to be protective against all 3 allergic diseases. Thus, in analyses adjusted for the protective effects of nativity, Asians had even higher risk of food allergy and eczema, and also had a higher risk of asthma, compared with non-Hispanic white children, with odds ratios (ORs) of 1.22 (95% CI, 1.05-1.42), 1.47 (95% CI, 1.31-1.64), and 1.15 (95% CI, 1.00-1.32), respectively (Table I).
TABLE I.
Effect of race and nativity on odds of allergic diseases*
| OR (95% CI) |
|||
|---|---|---|---|
| Variable | Food allergy (6,209; 5.3%, 5.4%) |
Eczema (13,700; 11.8%, 11.8%) |
Asthma (10,725; 9.2%, 9.0%) |
| Race | |||
| Non-Hispanic white (54,896; 48.7%, 66.0%)† | Reference | Reference | Reference |
| Non-Hispanic black (18,352; 16.3%, 12.8%) | 1.11 (1.00-1.23) | 1.65 (1.54-1.76) | 1.97 (1.84-2.12) |
| Hispanic (31,829; 28.3%, 16.0%) | 0.82 (0.73-0.92) | 1.03 (0.96-1.11) | 1.28 (1.18-1.39) |
| Asian (7,571; 6.7%, 5.2%) | 1.22 (1.05-1.42) | 1.47 (1.31-1.64) | 1.15 (1.00-1.32) |
| Nativity category | |||
| Child US-born | Reference | Reference | Reference |
| Parent US-born (83,520; 72.0%, 77.7%) | |||
| Child US-born | 0.93 (0.83-1.03) | 0.67 (0.62-0.72) | 0.59 (0.55-0.64) |
| Parent foreign-born (26,603; 22.9%, 18.2%) | |||
| Child foreign-born | 0.72 (0.58-0.89) | 0.44 (0.37-0.52) | 0.28 (0.22-0.34) |
| Parent foreign-born (4,941; 4.3%, 3.3%) | |||
| Child foreign-born | 1.12 (0.81-1.57) | 0.77 (0.57-1.03) | 0.70 (0.51-0.95) |
| Parent US-born‡ (928; 0.8%, 0.8%) | |||
| Age (y) | 0.99 (0.99-1.00) | 0.97 (0.97-0.98) | 1.06 (1.05-1.06) |
| Sex | |||
| Female (56,628; 48.6%, 51.1%) | 0.99 (0.93-1.06) | 1.03 (0.98-1.08) | 0.77 (0.73-0.82) |
| Income§ | 0.99 (0.95-1.04) | 0.98 (0.95-1.02) | 0.79 (0.77-0.82) |
Odds ratios in boldface represent statistically significant comparisons.
Adjusted for age, sex, and income.
N, unweighted proportion, weighted proportion (accounting for complex survey structure).
Foreign-birth to US-born parents is a small group with likely varying backgrounds.
Income-to-poverty ratio is an ordinal variable, with categories of ≤Federal Poverty Level, 1-2 times Federal Poverty Level, ≥2 times Federal Poverty Level.
Thirty-nine percent of reporting parents were males and 61% were females, and there was no interaction between sex of reporting parent and parental nativity on the allergic outcomes (data not shown). There was no significant interaction between race and nativity (see Table E3 in this article’s Online Repository at www.jacionline.org) or race and age on the odds of food allergy or eczema. There was evidence that the relationship between race and asthma did differ by age category but not by nativity, with Asian race conferring higher odds of asthma in all but the 12- to 17-year-old group (see Table E2 in this article’s Online Repository at www.jacionline.org).
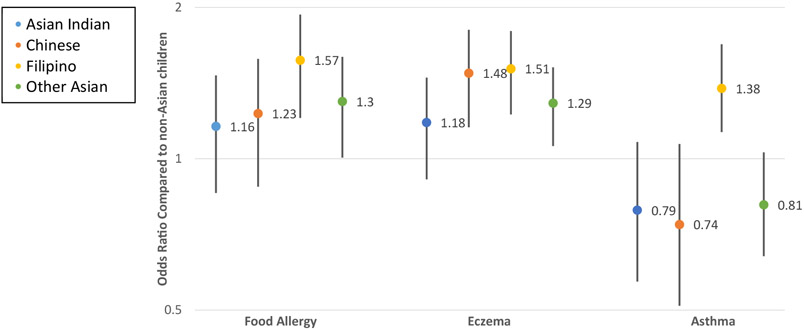
We then examined Asian subpopulations, finding markedly higher rates of all allergic diseases in Filipino children compared with non-Asian children in adjusted models: OR, 1.57 (95% CI, 1.25-1.98) for food allergy, 1.51 (95% CI, 1.25-1.82) for eczema, and 1.38 (95% CI 1.13-1.69) for asthma (Fig 1). There were trends toward increased odds in the remaining Asian subpopulations for food allergy (Asian Indian: OR, 1.16, 95% CI, 0.89-1.47; Chinese: OR, 1.23, 95% CI, 0.88-1.58; and Other Asian: OR, 1.30, 95% CI, 1.01-1.60), and eczema (Asian Indian: OR, 1.18, 95% CI, 0.91-1.45; Chinese: OR, 1.48, 95% CI, 1.16-1.81; and Other Asian: OR, 1.29, 95% CI, 1.06-1.52). Of the Asian subpopulations, only Filipinos demonstrated an elevated rate of asthma compared with non-Asian populations (Asian Indian: OR, 0.79, 95% CI, 0.57-1.08; Chinese: OR, 0.74, 95% CI, 0.51-1.07; and Other Asian: OR, 0.81, 95% CI, 0.64-1.03).
FIG 1.
Odds of allergic diseases among Asian subpopulations compared with non-Asian children, adjusted for age, sex, and income. Other Asian includes Asian subpopulations without sufficient numbers for reporting, such as Korean, Japanese, and mixed Asian children.
Taken together, these findings suggest an increased propensity for allergic diseases among Asian populations in the United States that fully emerges only after accounting for the protective effect of foreign child and parental birth. With subsequent generations, the increased risk of allergic disease in immigrant populations may become more pronounced as the protective effect of foreign birth wanes. This increased propensity for allergic disease may reflect gene by environment interaction or epigenetic modification. Environmental exposures in this population, as well as in-country rates of allergic diseases, should be further studied.
Asian populations are not homogeneous, and we found especially high rates of all 3 allergic diseases, including asthma, among Filipino-American children, which is notable given that asthma was less prevalent in Asian children overall. It remains unclear why certain Asian subpopulations are protected against asthma but have a much higher risk of eczema and food allergy, whereas others demonstrate increased risk of all 3. Further research into the genetic and environmental risk factors responsible for the different propensities to these diseases may provide broader insight into the mechanisms of these diseases.
The protective effect of birth outside the developed world has been previously demonstrated,4 but the effect of parental birth has been less consistent, with some studies demonstrating higher rates of allergic diseases in children of immigrants5-7 and others finding a protective effect of parental immigration on asthma and eczema.6 It is thought that microbial exposures may explain the protective effect of birth outside the United States on allergy, but how foreign parental birth may affect a child’s risk of allergy is much less clear, and may reflect cultural practices, dietary habits, or awareness of allergic diseases. Further research into the specific mechanisms by which child and parental nativity may affect the development of allergic disease is needed.
Limitations of this study include self-report of allergic disease,8 which lacks specificity, and which may be highly influenced by medical care and parental knowledge. In addition, self-reported place of birth and inability to discern more than 1 generation of immigration or duration of residence in the United States limit the specificity of analyses. Furthermore, because of survey design, data on only 1 parent were available, although nativity status concordance is greater than 80% in married couples.9 Granular data regarding children’s racial origin, particularly for those of mixed race, were not available nor were data on some smaller Asian subgroups. However, these limitations are balanced by the uncommon and distinctive nature of this nationally representative survey with detailed data about Asian populations and subpopulations, a group identified in previous studies to potentially be at a higher risk for allergic disease, yet one that has remained relatively unstudied in the United States. Data regarding immigration, an important modifier of allergic disease, were also available for both parents and children, allowing adjustment for this important and dynamic measure.
In conclusion, our study demonstrates increased prevalence of food allergy, eczema, and asthma among Asian children once adjusted for child and parental nativity, along with a pronounced risk of these diseases in the Filipino population, an important population for future study with 57% higher odds of food allergy, 51% higher odds of eczema, and 38% higher odds of asthma.
Supplementary Material
Acknowledgments
Disclosure of potential conflict of interest: J. H. Dunlop has received support from the National Institute of Allergy and Infectious Diseases T32AI007007. C. A. Keet has received research support from the National Institutes of Health, holds a patent on an immunotherapy delivery method, receives royalties from UpToDate, and is a member of the American Board of Allergy and Immunology.
REFERENCES
- 1.Wang Y, Allen KJ, Suaini NHA, Peters RL, Ponsonby AL, Koplin JJ. Asian children living in Australia have a different profile of allergy and anaphylaxis than Australian-born children: a state-wide survey. Clin Exp Allergy 2018;48:1317–24. [DOI] [PubMed] [Google Scholar]
- 2.Gupta RS, Springston EE, Warrier MR, Smith B, Kumar R, Pongracic J, et al. The prevalence, severity, and distribution of childhood food allergy in the United States. Pediatrics 2011;128:e9–17. [DOI] [PubMed] [Google Scholar]
- 3.Glick AF, Tomopoulos S, Fierman AH, Trasande L. Disparities in mortality and morbidity in pediatric asthma hospitalizations, 2007 to 2011. Acad Pediatr 2016;16:430–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Prescott SL, Pawankar R, Allen KJ, Campbell DE, Sinn J, Fiocchi A, et al. A global survey of changing patterns of food allergy burden in children. World Allergy Organ J 2013;6:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Koplin JJ, Peters RL, Ponsonby AL, Gurrin LC, Hill D, Tang ML, et al. Increased risk of peanut allergy in infants of Asian-born parents compared to those of Australian-born parents. Allergy 2014;69:1639–47. [DOI] [PubMed] [Google Scholar]
- 6.Keet CA, Wood RA, Matsui EC. Personal and parental nativity as risk factors for food sensitization. J Allergy Clin Immunol 2012;129:169–75, e1-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Leung RC, Carlin JB, Burdon JG, Czarny D. Asthma, allergy and atopy in Asian immigrants in Melbourne. Med J Australia 1994;161:418–25. [DOI] [PubMed] [Google Scholar]
- 8.Zablotsky B, Black LI. Concordance between survey reported childhood asthma and linked Medicaid administrative records. J Asthma 2019;56:285–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Larsen LJW, Nathan P. Married-couple households by nativity status: 2011. In: United States Department of Commerce, editor, Commerce. Suitland (MD): U.S. Census Bureau, Economics and Statistics Administration, United States Department of Commerce; 2013. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.