Abstract
Background
The treatment of arterial hypertension can be monitored by office blood pressure (office BP), home blood pressure (home BP), or 24 hours ambulatory blood pressure (ABPM). In this review, we present current recommendations from Germany and from international guidelines as well as the findings of the main studies on the use of these methods to guide treatment.
Methods
This review is based on pertinent publications retrieved by a selective search in PubMed up to and including March 2020. Special attention was paid to guidelines and position papers.
Results
The guidelines offer heterogeneous recommendations for treatment monitoring. Home BP is the most reproducible method, with test-retest correlation coefficients of 0.91/0.86 (systolic/diastolic), in comparison to office BP (0.77/0.76). Two meta-analyses revealed better blood pressure control with home measurement than with usual care (systolic, -3.2 to -8.9 mmHg). A meta-analysis of randomized controlled trials also suggests that home measurement promotes adherence. In the randomized and controlled TASMINH4 trial, the home BP group with telemetric surveillance achieved better blood pressure control than the group with treatment titration based on office BP (systolic -4.7 [CI: -7; -2.4] mmHg, diastolic -1.3 [-2.5; 0.02] mmHg). With ABPM, patients frequently reported moderate to severe discomfort, limiting its practical applicability.
Conclusion
Blood pressure measurement at home is recommended for treatment monitoring, using validated, automatic upper arm devices with data storage and trend analysis. Changes of treatment should be based on average values (28 home measurements) from seven days (two morning and two evening measurements per day). Office BP is mainly used for for screening purposes. There have not yet been any randomized trials comparing the three measuring methods in terms of hard cardiovascular endpoints.
cme plus
This article has been certified by the North Rhine Academy for Continuing Medical Education. The CME questions on this article can be found at http://daebl.de/RY95. Answers must be submitted by 11 July 2022.
Participation is possible at cme.aerztebatt.de
The treatment of arterial hypertension can essentially be monitored by occasional office blood pressure (office BP) measurements or by out-of-office measurements, such as ambulatory blood pressure monitoring (ABPM) and home blood pressure (home BP) measurements performed by the patients themselves. The various measuring methods should not be viewed as alternatives but as complementary, and decisions on which method to use are based on the individual clinical scenario (1).
Numerous studies evaluating the advantages and disadvantages of these three methods have been conducted over the last 50 years. They have demonstrated a clear prognostic advantage of out-of-office measurements for the diagnosis of arterial hypertension, but not for treatment monitoring. The fundamental question whether a treatment strategy based on out-of-office measurements results in greater reductions in morbidity and mortality compared to office blood pressure measurements has yet to be answered.
Besides addressing the question which blood pressure targets would be most appropriate for the treatment of arterial hypertension, the SPRINT trial stimulated a variety of scientific discussions concerning the method used for measuring blood pressure (2, 3). Adjustments to the antihypertensive regimen made to achieve the blood pressure targets were based on automated office blood pressure measurements taken without involvement of medical staff. Even though the method of automated office blood pressure measurement is scientifically well described and blood pressure measuring devices using this technology are commercially available, these systems have virtually not been adopted in clinical practice in Germany and worldwide (4).
The majority of antihypertensive therapy milestone trials used office blood pressure measurements for treatment monitoring and adjustment (5). However, the office blood pressure measurement methods used in these studies varied significantly, e.g. with regard to the examiner (physician, study nurse, medical staff), blood pressure monitor (mercury, oscillometric, fully automatic, semi-automatic, aneroid, random-zero), number of measurements (1– 6), and statistical analysis (5).
The current guidelines of the specialist societies increasingly highlight the importance of out-of-office measurements for treatment monitoring. For the monitoring and adjustment of antihypertensive therapy, however, consistent and uniform national and international recommendations for out-of-office blood pressure measurement are still lacking.
Methods
PubMed was searched up to and including March 2020, using the following keywords: “ambulatory blood pressure“, “home blood pressure“, “out of office blood pressure“, “self-measured blood pressure“, and “self-measurement of blood pressure“. The focus was on prospective follow-up studies with cardiovascular endpoints. In addition, reviews, meta-analyses, blood pressure guidelines, scientific statements, and position papers were included in the analysis.
What recommendations are made in the current guidelines and what is the actual clinical practice?
The current guidelines of the major medical societies, such as the American Heart Association (AHA/ACC 2017 [6]), the European Society of Hypertension and the European Society of Cardiology (ESH/ESC 2018 [7]), the UK’s National Institute for Health and Care Excellence (NICE 2019 [8]) and the position paper of the German Hypertension Society (DHL, Deutsche Hochdruckliga [9]) make widely varying recommendations regarding how antihypertensive therapy should best be monitored (table 1). The German Hypertension Society has not issued its own guidelines on this subject, but essentially translated the European guidelines. In a 2017 statement on the SPRINT trial and blood pressure targets, however, the DHL made a recommendation for blood pressure self-measurement (9). Given the greater patient acceptance of blood pressure self-measurement compared to 24-hour ambulatory blood pressure measurement, it recommended blood pressure self-measurement as the preferred method of treatment monitoring. However, these definite proposals were not incorporated into official DHL guidelines.
Table 1. Guidelines of the US (6), European (7) and UK (8) medical societies on treatment monitoring (2017 DHL statement [9]).
| Guidelines | Office blood pressure | Home blood pressure | 24h blood pressure |
| AHA (2017) | + | +++*1 | ++ |
| NICE (2019) | +++ | ++ *2, 3 | ++*2 |
| ESH/ESC (2018) | +++ | + | + |
| DHL (2017) | + | +++ | ++ |
*1 Potentially in conjunction with telemedicine case management
*2 If “white coat” effect or masked hypertension is suspected
*3 If patient preference
AHA, American Heart Association; DHL, German Hypertension Society (Deutsche Hochdruckliga);
ESC, European Society of Cardiology; ESH, European Society of Hypertension;
NICE, National Institute for Health and Clinical Excellence
The American Heart Association made the most specific statement, clearly preferring out-of-office measurements, such as ambulatory blood pressure monitoring or home blood pressure measurement, over conventional office blood pressure measurement. Before home blood pressure measurement is started, patients should be adequately educated in the use of systems which automatically store measurements for treatment monitoring, potentially in conjunction with telemedicine interventions (6).
The ESH/ESC guideline highlights the growing importance of out-of-office measurements for the diagnosis of hypertension. With respect to treatment monitoring, it draws attention to the lack of randomized trials on the prognostic significance of different methods of blood pressure measurement (gaps in evidence). Treatment targets derived from observational studies are stated for home blood pressure measurement and ABPM (7). The recommendation made for the targets of home blood pressure monitoring is very vague. In reference to the new office blood pressure target of 130/80 mmHg, which was introduced in 2018 and applies to most patients, the guideline specifies the same target for self-measured blood pressure.
The NICE guideline continues to primarily recommend office blood pressure measurement for treatment monitoring (8). While the authors discuss potential advantages of home blood pressure, they do not indicate a clear preference for this method because of gaps in the evidence base. If a patient prefers home blood pressure monitoring, they recommend to use this method, but only after adequate training.
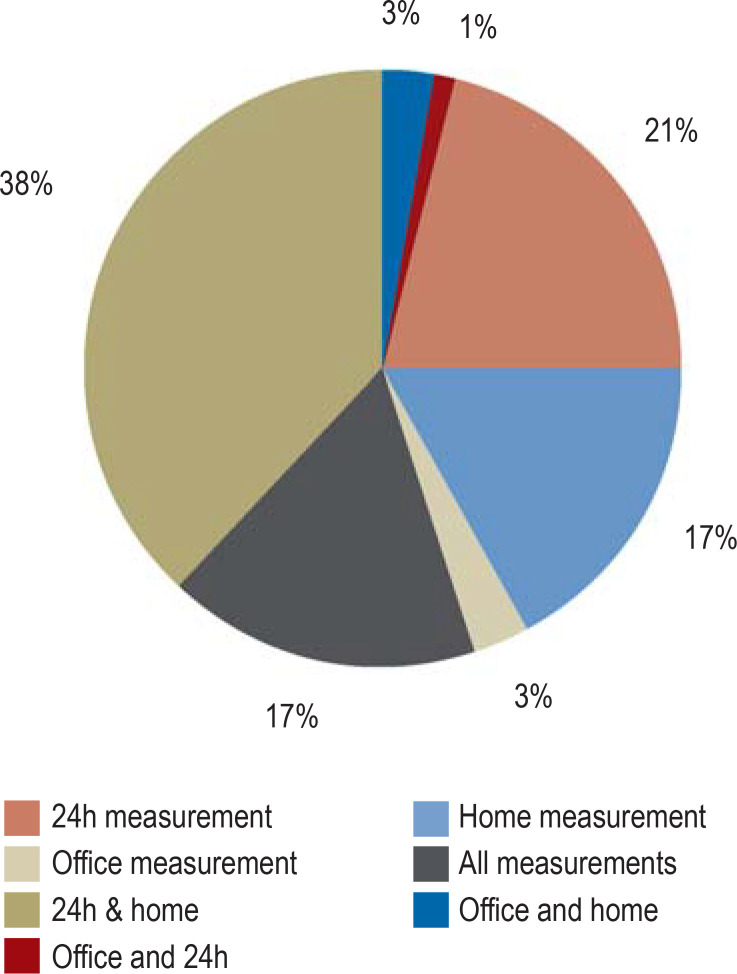
The results of an online survey on blood pressure measurement of the German Society of Internal Medicine are presented in the eMethods section. The use of the various measuring methods for treatment monitoring is very inconsistent. While 38% use both ABPM and home blood pressure, 21% use only ABPM and 17% only home blood pressure measurement (efigure 1a).
eFigure 1a.
A DGIM online survey on blood pressure measurement of 15 884 office-based and hospital physicians; personal communication L. Unger, response rate 4% (n = 731)
a) Strategies in selecting measuring methods for treatment monitoring
Blood pressure variability
Essentially, two types of blood pressure variability are important for treatment monitoring: circadian variability over 24 hours and variability between blood pressure checks during physician visits.
Due to the significant circadian variability of blood pressure measurements, it is difficult to reliably establish control< of hypertension based on office blood pressure measurements alone. The mean daytime and nighttime ABPM values, by their very nature, better reflect the 24-hour period than office blood pressure measurements; however, they are not necessarily representative for prolonged observation over weeks and months. Home blood pressure measurements performed as described in Box 1 better reflect prolonged observation periods and can be used both in the dose-titration period and for long-term monitoring (10).
BOX 1. Home measurement procedure*.
Structured patient education recommended
Automatic validated upper-arm device (seal of approval, www.hochdruckliga.de; www.stridebp.org) with memory function, mean and trend analyses
Select cuff size based on upper-arm circumference according to manufacturer‘s specifications
Sitting position; cuff at the level of the heart
First measurement after 5-minute rest; second measurement after 1–2 minutes
4-times-daily self-measurements over 7 days (2 in morning, 2 in the evening; before intake of medication) before each physician visit and after adjustment of treatment
Treatment evaluation is based on the mean blood pressure from the 7 days (28 measurements) before each physician visit
Telemetry indications: examples include gestational hypertension, heart failure, stroke, reduction of physician contacts during a pandemic
* Recommendations of the authors in line with the 2011 clinical practice guideline of the German Hypertension Society (26), 2017 AHA guideline (6), 2019 NICE guideline (8), and 2010 ESH guideline (10)
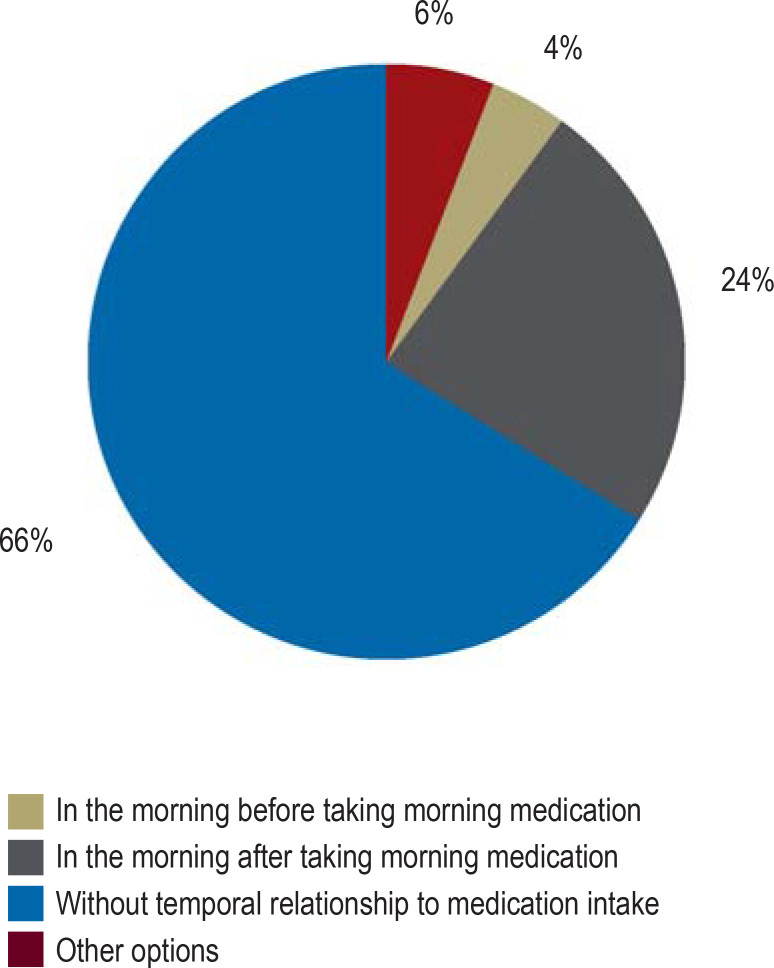
Thus, in the monitoring of antihypertensive therapy, the role of office blood pressure measurements is, at best, that of a screening tool. They only reflect the blood pressure situation at the time of the measurement. Typically, no consideration is given to the temporal relationship between office blood pressure measurement and the intake of medication (efigure 1b). This also applies, for example, to the above-mentioned SPRINT trial in which the timing of measurement is not stated in either the study protocol or the original publication. Thus, it is likely that in the SPRINT trial the office blood pressure readings were not obtained as trough values (before the intake of medication in the morning). This would also explain why in the SPRINT substudy the mean daytime ABPM readings were 7 mmHg higher than the office blood pressure readings.
eFigure 1b.
b) Temporal relationship between medication intake and blood pressure measurement
In most patients, home blood pressure monitoring is a low-stress alternative to ABPM, offering the additional advantage that it can be repeated as often as desired. However, ABPM is still indicated to answer certain questions (box 2).
BOX 2. Indication for 24-hour ambulatory blood pressure measurement (ABPM)*.
-
Patients with high cardiovascular risk (10-year mortality >5%, according to ESC/ESH) should undergo ABPM once a year and for specific queries:
Conspicuous discrepancy between home measurement and office measurement
(e.g., to rule out “white coat“ effect)
Suspected masked uncontrolled hypertension
Advanced hypertensive end organ damage, e.g. renal failure or hypertensive heart disease
Night-time blood pressure behavior
(e.g., in patients with sleep-related breathing disorders or glaucoma)
Chronotherapy
Refractory hypertension
Very high blood pressure variability
Intermittent hypotension
Gestational hypertension
* Recommendations of the authors in line with DHL 2013 (28), AHA 2017 (6)
ESC, European Society of Cardiology; ESH, European Society of Hypertension
The “black box” of blood pressure variability between two physician visits is not reliably captured by either an office blood pressure measurement or an ABPM.
Treatment adherence and blood pressure measurement
Due to known treatment adherence issues, non-compliant patients often experience an increase in blood pressure in periods with no or inadequate intake of medication. Furthermore, it is known that medication compliance improves in anticipation of an upcoming blood pressure check visit—an effect also referred to as white-coat compliance or tooth-brush effect (11). If white-coat compliance is suspected, reliable treatment monitoring can only be achieved by daily home blood pressure measurements (11, 12). A treatment study with electronic adherence monitoring found that home blood pressure measurements were the only way to identify days without intake of medication (“drug holidays”) (12). For this reason, home blood pressure monitoring may also promote adherence, as shown in a meta-analysis of 6 of 11 randomized controlled trials (13). Due to complex adherence interventions, it was not possible to reliably determine the independent effect of home blood pressure measurement alone (13).
Reproducibility of the various measuring methods
The inherent blood pressure variability between two blood pressure measurements (“background noise”) should be considerably below the expected therapeutic effect. In statistical terms, the mean difference between two measurements should be close to 0 mmHg in case of no or unchanged medication and the standard deviation (SD) of this mean difference should be as low as possible. Thus, it is of interest to find out which of the three measuring methods has the least impact on measurement-related and inherent blood pressure variability and consequently offers the best reproducibility.
The results of two studies addressing this question were largely comparable (14, 15). In the first study (n = 133), the test-retest correlation coefficients (systolic/diastolic) between two measurements were highest for home blood pressure measurements (0.91/0.86) compared to office blood pressure measurements (0.77/0.76) and 24h ABPM (0.80/0.84) (14). The variability, expressed as standard deviation (SD) of the mean systolic/diastolic differences, was highest for office blood pressure (11/6.6) and daytime ABPM (10/6.6) and lowest for home blood pressure (6.9/4.7).
A second study (n = 97) largely confirmed these results (15). The variability (SD) was lowest for home blood pressure and highest for office blood pressure measurement. For systolic home blood pressure, ABPM and office blood pressure, the values (SD and [95% CI]) were 3.81 [3.34; 4.44], 7.83 [6.9; 9.17] and 8.1 [7.1; 9.43], respectively.
For clinical practice, this means that even small treatment-induced reductions in blood pressure of 5 mm Hg and less are best detected by means of home blood pressure measurement (14).
Comparison of office blood pressure, ABPM and home blood pressure in treatment studies
Randomized trials, comparing all three measuring methods with regard to blood pressure control and hard cardiovascular endpoints have not yet been conducted.
Two meta-analyses found that home blood pressure-based treatment monitoring improved blood pressure control (systolic -3.2 to -8.9 mmHg), especially in conjunction with therapeutic co-interventions such as case management (16, 17). In the most recent meta-analysis, the mean systolic blood pressure in the self-monitoring group was found reduced by 3.2 mmHg [-4.9; –1.6 mmHg] (16).
In pharmacological efficacy studies, direct (head-to-head) comparisons of all three measuring methods yielded in summary the following results:
In comparison to the gold standard ABPM, home self-measurements taken 12 to 24 hours after intake of medication allowed a conclusion to be drawn about the 24-hour efficacy of the treatment (18, 19).
Furthermore, the pharmacodynamic effects of variable adherence were captured by home blood pressure measurement (12, 18).
Hypertension management-evaluating dose titration studies reported the following results:
A Finnish trial compared ABPM directly to home blood pressure measurements with regard to the adjustment of antihypertensive therapy in a clinical setting (20). The primary endpoint of the study after 24 weeks was blood pressure control determined with all three measuring methods. Management of hypertension based on ABPM versus home blood pressure resulted in a comparable blood pressure control without significant differences (ABPM group -17.9/-12.3 mmHg; home blood pressure group -17.3/ -10.8 mmHg).
Focusing on cardiovascular events, the PLUR study compared blood pressure management based on office measurements with ABPM-based management (21). It found that ABPM-based management improved the cardiovascular prognosis. However, the acceptance of repeated ABPM investigations was low.
The randomized, controlled TASMINH4 trial (n = 1 003 [22]) showed superior blood pressure control in the home blood pressure group with telemonitoring compared to the control group (means and confidence intervals systolic/diastolic of -4.7 [-7; -2.4 mmHg]/-1.3 [-2.5; -0.02 mmHg]). In the control group, a study nurse performed the office blood pressure measurements. In addition, it was shown for the telemetry group that treatment escalation by the primary care physicians was more effective and faster than in the group with office blood pressure monitoring (22).
Repeated ABPM investigations are limited by the very high discomfort factor of ABPM, especially among professionals. In a study with 104 patients, 55% reported moderate to severe discomfort and 30% severe restriction of their daily activities related to ABPM (23). Consequently, ABPM is of limited clinical use in the dose titration period.
In summary, these studies present a strong argument for the use of home blood pressure measurements for treatment monitoring; yet, there is still a lack of studies with hard endpoints. Besides scientific considerations, the patient preference for home blood pressure measurements should be taken into account as this is essential for ensuring long-term collaboration (24, 25).
How should home blood pressure measurements be obtained and analyzed?
While for ABPM technical aspects, such as measurement frequency, measurement intervals and statistical analysis, are largely standardized by guidelines and manufacturer software, this level of standardization is far from being achieved for home blood pressure measurement in a clinical setting. While the current guidelines and position papers on home blood pressure measurement provide comparatively precise guidance on measurement frequencies and intervals as well as on statistical analysis, only few software systems have so far implemented these recommendations in a consistent manner (10). For example, the German Hypertension Society recommends in a clinical practice guideline and a position paper on the SPRINT trial to use validated upper-arm devices, standardized measurements as well as automatic data storage and analysis for home blood pressure monitoring (9, 26).
With regard to measurement accuracy of home blood pressure measuring devices, reference is made to the recommendations of the German Hypertension Society (seal of approval, www.hochdruckliga.de) and the European Hypertension Society (www.stridebp.org).
Our recommendations for home blood pressure measurement are summarized in Box 1.
The advantage of telemetry in low-risk populations lies primarily in the fast and standardized transmission of home blood pressure measurements directly into the patient records. In addition, telemetry offers advantages for high-risk populations, such as patients with gestational hypertension or heart failure and patients with stroke (27).
In 2017, the blood pressure target for office measurements was still at 140/90 mmHg; at that time, the DHL stated a target of 135/85 mmHg for home blood pressure measurement (9). With the 2017 and 2018 guidelines (AHA, ESH, ESC, and DHL), the target for most patients is now lower (130/80 mmHg, office blood pressure). The differences between the three measuring methods become smaller the lower the blood pressure level, i.e. for blood pressure readings of 120/80 or 130/80 mmHg, the targets are similar for office blood pressure measurement, home blood pressure measurement and daytime ABPM (table 2).
Table 2. 2017 AHA analog values for office, home and 24-hour ambulatory blood pressure (ABPM) measurements. The corresponding analog values of the ESH/ESC and NICE are marked.
| Office measurement | Home measurement | ABPM 24-h total period | ABPM daytime period |
| 120/80 mmHg | 120/80 mmHg | 115/75 mmHg | 120/80 mmHg |
| 130/80 mmHg | 130/80 mmHg*1 | 125/75 mmHg*1 | 130/80 mmHg |
| 140/90 mmHg | 135/85 mmHg*1, 2 | 130/80 mmHg*1 | 135/85 mmHg*1, 2 |
*1 ESH/ESC analog values
*2 NICE analog values
AHA, American Heart Association; ESC, European Society of Cardiology;
ESH, European Society of Hypertension; NICE, National Institute for Health and Clinical Excellence
The target analog value recommendations of the AHA, the ESH/DHL and of NICE for office blood pressure measurements, home blood pressure measurements and ABPM are listed in Table 2. The AHA is the only organization to provide analog values for the various measuring methods across the full range of blood pressure readings.
Conclusions
Despite the lack of prognosis studies comparing office, home and ambulatory blood pressure measurements, in our opinion the studies discussed above show a clear advantage for home blood pressure measurement over the other methods of treatment monitoring. However, the current AHA, NICE and ESH/ESC/DHL guidelines and position papers support this preference to considerably varying extent.
The reasons for the preference of home blood pressure measurement for treatment monitoring include:
Best blood pressure measurement reproducibility of all methods
Revealing adherence issues
Overcoming “therapeutic inertia“
Detection even of small therapeutic effects
Unlimited repeatability compared to ABPM
Patient preference.
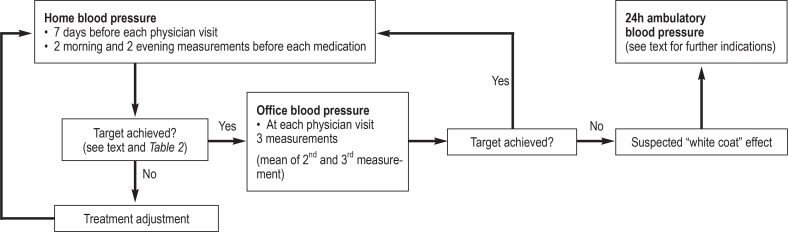
In the period of dose titration and treatment escalation, home blood pressure measurement should be performed in a standardized way for at least seven days before the next physician visit. Based on the mean blood pressure measurements of the last seven days before the next physician visit, the treating physician can decide on the type and extent of further treatment (Figure).
Figure 1.
The authors’ recommendation for the use of home blood pressure, office blood pressure and 24-hour ambulatory blood pressure measurements for treatment monitoring
Office blood pressure measurement, as it is commonly practiced in Germany, is limited by examiner error, poor reproducibility and white-coat effect. Due to methodological issues, singular, repeated or automated office blood pressure measurements are only used for screening purposes and in patients in whom home blood pressure monitoring is contraindicated, for example because of neurotic fixation (Figure) (1). In comparison to ABPM, home blood pressure measurement enjoys greater acceptance by patients and, consequently, measurement repeatability is greater. The indications for ABPM are listed in the AHA, ESH guidelines and in a DHL position paper (28) and summarized in the Figure and Box 2.
Shortly after completion of this review article, the 2021 Practice Guidelines of the European Society of Hypertension were published (29); their content is in line with the authors’ recommendations.
Randomized trials with hard endpoints are needed to determine which measuring method for treatment monitoring provides the best prognostic data.
Supplementary Material
eMethods
The results depicted in eFigure 1a and 1b are intended to illustrate that in Germany the approaches to treatment monitoring in patients with hypertension vary significantly, both in internal medicine practices and in hospitals.
A total of 731 internists responded in this online survey of members of the German Society of Internal Medicine (DGIM, Deutsche Gesellschaft für Innere Medizin). With 4%, this is a typical response rate in online surveys. As shown in eFigure 1a, in 38% ABPM and home blood pressure measurement, in 21% only ABPM and in 17% only home measurement were used, besides many other combinations. Although there is no claim to representativeness for the individual proportions in this survey, the great heterogeneity of the approaches is obvious.
The timing of the office blood pressure measurement is another issue, as false low readings may be obtained shortly after the intake of antihypertensive medication.
Questions on the article in issue 27–28/2021:
Monitoring of Treatment for Arterial Hypertension
The submission deadline is 11 July 2022. Only one answer is possible per question.
Please select the answer that is most appropriate.
Question 1
The authors recommend to analyze the home blood pressure measurement data during the physician visit for dose titration. What minimum data collection period is required for the calculation of the mean?
the last 2 days
the last 3 days
the last 5 days
the last 7 days
the last 14 days
Question 2
What is meant by the term trough values?
Values obtained after the intake of morning medication
Values obtained after the intake of evening medication
Values obtained after lunch
Values obtained after dinner
Values obtained before the intake of morning medication
Question 3
The guidelines recommend the use of analog values to compare the results of office blood pressure measurements and home blood pressure measurements. Which analog value in office blood pressure measurement corresponds to a home measurement of 135/85 mmHg?
145/90 mmHg
140/90 mmHg
130/80 mmHg
120/80 mmHg
125/75 mmHg
Question 4
If home blood pressure measurement is arranged with a patient, how many measurements per day should patients typically perform?
four measurements (two in the morning, two in the evening)
six measurements (two in the morning, two at noon, two in the evening)
two measurements (one in the morning, one in the evening)
five measurements (two in the morning, one at noon, two in the evening)
three measurements (one in the morning, one at noon, one in the evening)
Question 5
Two studies evaluated the reproducibility of various blood pressure measurement methods. For which measurement method was the lowest variability reported?
Automated office blood pressure measurement
Office blood pressure measurement by medical staff
24-hour ambulatory blood pressure measurement (ABPM)
Home blood pressure measurement
Blood pressure measurement in a pharmacy
Question 6
What is the “tooth brush” effect?
Growing accustomed to regular home blood pressure measurement
Falling adherence to home blood pressure measurement
Increase in blood pressure associated with upcoming blood pressure check
Development of aversion to blood pressure measurement
Increased medication adherence along with upcoming blood pressure check
Question 7
Which potential issue of the SPRINT trial is highlighted by the authors?
The trial was not randomized.
Information about the timing of the office blood pressure measurement is missing.
The patient sample was too small.
The duration of the trial was too short.
The trial was conducted as a monocentric study.
Question 8
Regular 24-hour ambulatory blood pressure measurements are indicated in patients with high cardiovascular risk (10-year mortality >5% according to ESC/ESH). At what time interval should this examination usually be repeated?
once per month
once per quarter
once every six months
once per year
every second year
Question 9
Besides home blood pressure measurement, the authors recommend office blood pressure checks for treatment monitoring. Which measurement regimen is recommended here?
2 measurements per visit; value from second measurement is used
4 measurements per visit; mean from second, third and fourth measurement is used
3 measurements per visit; mean from second and third measurement is used
one measurement per visit
3 measurements per visit; mean from all measurements is used
Question 10
According to the specified analog values, which of the compared blood pressure measurement methods yields the lowest blood pressure levels for patients?
Daytime ABPM
Home blood pressure measurement
Office blood pressure measurement
Ergometry-based blood pressure measurement
24-hour ABPM – total period
Acknowledgments
Translated from the original German by Ralf Thoene, MD.
Acknowledgement
We would like to thank Jonna Goyert, research assistant at the Institute of Sports Science, Kiel University, for her support in the preparation of the manuscript with regard to formalities, figures and tables.
Footnotes
Conflict of interest statement
The authors declare that no conflict of interest exists.
References
- 1.Mengden T, Kraft K, Vetter H. Verbesserung der Langzeitkontrolle der arteriellen Hypertonie mit Blutdruckselbstmessung. Dtsch Arztebl. 1998;95, 45:2833–2842. [Google Scholar]
- 2.The SPRINT Research Group. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015;373:2103–2116. doi: 10.1056/NEJMoa1511939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Düsing R, Middeke M. SPRINT-Studie zur Blutdrucksenkung: Neuer Zündstoff für die Kontroverse. Deutsches Ärzteblatt. 2016;113 [Google Scholar]
- 4.Myers MG, Kaczorowski J, Godwin M. Automated office blood pressure measurement in primary care. Can Fam Physician. 2014;60:127–132. [PMC free article] [PubMed] [Google Scholar]
- 5.Chen Y, Lei L, Wang J-G. Methods of blood pressure assessment used in milestone hypertension trials. Pulse. 2018;6:112–123. doi: 10.1159/000489855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA. Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71:e13–e115. doi: 10.1161/HYP.0000000000000065. [DOI] [PubMed] [Google Scholar]
- 7.ESC/ESH. Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology (ESC) and the European Society of Hypertension (ESH) Eur Heart J. 2018;39:3021–3104. doi: 10.1093/eurheartj/ehy339. [DOI] [PubMed] [Google Scholar]
- 8.NICE. Hypertension in adults: diagnosis and management. NICE guideline. 2019 [Google Scholar]
- 9.Krämer BK, Hausberg M, Sanner B, et al. Blutdruckmessung und Zielblutdruck. Stellungnahme der Deutschen Hochdruckliga e. V. DHL /Deutschen Gesellschaft für Hypertonie und Prävention. Deutsche Medizinische Wochenschrift. 2017;142:1446–1447. doi: 10.1055/s-0043-117070. [DOI] [PubMed] [Google Scholar]
- 10.Parati G, Stergiou GS, Asmar R, et al. ESH Working Group on Blood Pressure Monitoring. European Society of Hypertension practice guidelines for home blood pressure monitoring. J Hum Hypertens. 2010;24:779–785. doi: 10.1038/jhh.2010.54. [DOI] [PubMed] [Google Scholar]
- 11.Mengden T, Ün S, Düsing R, Weisser B, Vetter H. Drug compliance decreases between clinic visits - the effect of „white-coat“ compliance on 24-h ambulatory blood pressure monitoring. J Hypertens. 2000;18 [Google Scholar]
- 12.Mengden T, Binswanger B, Grüne S, et al. The use of self-measured blood pressure determinations in assessing dynamics of drug compliance in a study with once daily morning vs evening amlodipine. J Hypertens. 1993;11:1403–1411. doi: 10.1097/00004872-199312000-00013. [DOI] [PubMed] [Google Scholar]
- 13.Ogedegbe G, Schoenthaler A. A systematic review of the effects of home blood pressure monitoring on medication adherence. J Clin Hypertens (Greenwich) 2006;8:174–180. doi: 10.1111/j.1524-6175.2006.04872.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stergiou G, Baibas N, Gantzarou A, et al. Reproducibility of home, ambulatory, and clinic blood opressure: Implications for the design of trials for the assessment of antihypertensive drug efficacy. Am J Hypertens. 2002;15:101–104. doi: 10.1016/s0895-7061(01)02324-x. [DOI] [PubMed] [Google Scholar]
- 15.Uen S, Fimmers R, Brieger M, Nickenig G, Mengden T. Reproducibility of wrist home blood pressure measurement with position sensor and automatic data storage. BMC Cardiovasc Disord. 2009;9 doi: 10.1186/1471-2261-9-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tucker KL, Sheppard JP, Stevens R, et al. Self-monitoring of blood pressure in hypertension: a systematic review and individual patient data meta-analysis. PLoS Med. 2017;14 doi: 10.1371/journal.pmed.1002389. e1002389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Uhlig K, Patel K, Ip S, Kitsios GD, Balk EM. Self-measured blood pressure monitoring in the management of hypertension: a systematic review and meta-analysis. Ann Intern Med. 2013;159:185–194. doi: 10.7326/0003-4819-159-3-201308060-00008. [DOI] [PubMed] [Google Scholar]
- 18.Mengden T, Vetter W. Ambulatory 24-hour blood pressure vs self-measured blood pressure in pharmacological trials. J Cardiovasc Pharmacol. 1994;24:20–25. [PubMed] [Google Scholar]
- 19.Mengden T, Binswanger B, Weisser B, Vetter W. An evaluation of self-measured blood pressure in a comparative study with bisoprolol or nitrendipine. Am J Hypertension. 1992;5:154–160. doi: 10.1093/ajh/5.3.154. [DOI] [PubMed] [Google Scholar]
- 20.Niiranen T, Kantola IM, Vesalainen R, Johansson J, Ruuska MJ. Comparison of home measurement and ambulatory monitoring of blood pressure in the adjustment of antihypertensive treatment. Am J Hypertens. 2006;19:468–474. doi: 10.1016/j.amjhyper.2005.10.017. [DOI] [PubMed] [Google Scholar]
- 21.Schrader J, Lüders S, Züchner C, et al. Practice vs. ambulatory blood pressure measurement (ABPM) under treatment with ramipril - PLUR study - randomized, prospective long-term study to evaluate the benefits of ABPM in patients on antihypertensive treatment. J Hum Hypertens. 2000;14:435–440. doi: 10.1038/sj.jhh.1001052. [DOI] [PubMed] [Google Scholar]
- 22.McManus RJ, Mant J, Franssen M, et al. TASMINH4 investigators Efficacy of self-monitored blood pressure, with or without telemonitoring, for titration of antihypertensive medication (TASMINH4): an unmasked randomised controlled trial. Lancet. 2018;391:949–959. doi: 10.1016/S0140-6736(18)30309-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nasothimiou EG, Karpettas N, Dafni MG, Stergiou GS. Patients‘ preference for ambulatory versus home blood pressure monitoring. J Hum Hypertens. 2014;28:224–229. doi: 10.1038/jhh.2013.104. [DOI] [PubMed] [Google Scholar]
- 24.Little P, Barnett J, Barnsley L, et al. Comparison of acceptability of and preferences for different methods of measuring blood pressure in primary care. BMJ. 2002;325:258–259. doi: 10.1136/bmj.325.7358.258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McGowan N, Padfield PL. Self blood pressure monitoring: a worthy substitute for ambulatory blood pressure? J Hum Hypertens. 2010;24:801–806. doi: 10.1038/jhh.2010.15. [DOI] [PubMed] [Google Scholar]
- 26.Mengden T, Dechend R, Lüders S, Eckert S, Tholl U, Sanner B. [Practice guidelines for home blood pressure measurement] Dtsch Med Wochenschr. 2011;136:2374–2377. doi: 10.1055/s-0031-1292056. [DOI] [PubMed] [Google Scholar]
- 27.Kielblock B, Frye Ch, Kottmair S, et al. Einfluss einer telemedizinisch unterstützten Betreuung auf Gesamtbehandlungskosten und Mortalität bei chronischer Herzinsuffizienz. Dtsch Med Wochenschr. 2007;132:417–422. doi: 10.1055/s-2007-970350. [DOI] [PubMed] [Google Scholar]
- 28.Lüders S, Dechend R, Eckert S, et al. 24-h-Langzeitblutdruckmessung (ABDM) Statement der Deutschen Hochdruckliga e. V. DHL., Sektion Hochdruckdiagnostik. Kardiologe 3/2013 [Google Scholar]
- 29.Stergiou GS, Palatini P, Parati G, et al. European Society of Hypertension Council and the European Society of Hypertension Working Group on Blood Pressure Monitoring and Cardiovascular Variability 2021 European Society of Hypertension practice guidelines for office and out-of-office blood pressure measurement. J Hypertens. 2021;39:1293–1302. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods
The results depicted in eFigure 1a and 1b are intended to illustrate that in Germany the approaches to treatment monitoring in patients with hypertension vary significantly, both in internal medicine practices and in hospitals.
A total of 731 internists responded in this online survey of members of the German Society of Internal Medicine (DGIM, Deutsche Gesellschaft für Innere Medizin). With 4%, this is a typical response rate in online surveys. As shown in eFigure 1a, in 38% ABPM and home blood pressure measurement, in 21% only ABPM and in 17% only home measurement were used, besides many other combinations. Although there is no claim to representativeness for the individual proportions in this survey, the great heterogeneity of the approaches is obvious.
The timing of the office blood pressure measurement is another issue, as false low readings may be obtained shortly after the intake of antihypertensive medication.