To the Editor:
Chronic lower respiratory diseases, including chronic obstructive pulmonary disease (COPD) and asthma, comprised the fourth leading cause of death in the United States in 2018 (1). Total age-adjusted mortality rates (AAMRs) from chronic lower respiratory diseases declined between 2000 and 2011, although geographic differences across the United States have been reported (2). Higher mortality rates from chronic lower respiratory diseases and higher prevalence of COPD have been observed in rural compared with urban areas (2, 3). However, temporal patterns related to urbanization in mortality rates for chronic lower respiratory diseases have not been assessed. The NHLBI and the Health Resources and Services Administration recently convened a workshop to discuss the COPD National Action Plan. The resulting plan established several priorities, including the need to quantify the burden of COPD and focus on community-level interventions in rural areas in the United States (4). To inform population-level prevention and policy strategies, we evaluated trends in chronic lower respiratory disease mortality between 1999 and 2019 in the United States stratified by county-level urbanization.
We obtained data from Multiple Cause of Death 1999–2019 on CDC WONDER, which aggregates all death certificates filed in the United States (5). We queried for deaths and AAMRs (standardized according to the 2000 U.S. population) with chronic lower respiratory diseases as the underlying cause (J40–J47). Deaths classified using International Statistical Classification of Diseases and Related Health Problems (ICD)-9 codes prior to local ICD-10 implementation were adjusted internally by the CDC using ICD-10 codes for the CDC WONDER database. We stratified deaths by six county urbanization categories according to the 2013 National Center for Health Statistics Urban–Rural Scheme for Counties (6). Four categories contain metropolitan areas classified from most to least urban: large central, large fringe, medium, and small. Two categories describe rural areas: micropolitan areas may contain an urban cluster and noncore areas are the most rural. We characterized temporal trends in AAMRs by fitting linear regression models using R version 4.0.2. We calculated AAMR ratios and respective 95% confidence intervals (CIs) to represent the number of deaths in less urbanized counties for every 1 death in the large central metro counties per 100,000 population. This study was exempt from institutional review board approval.
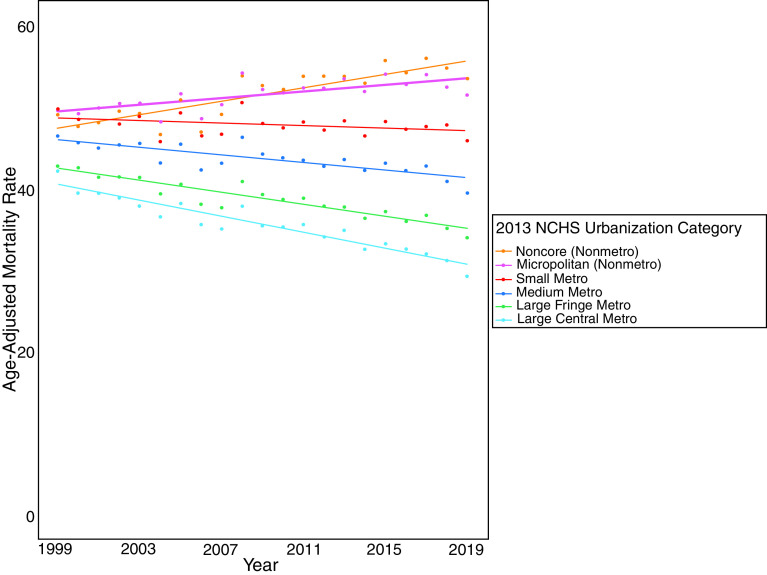
Between 1999 and 2019, there were 2,911,392 deaths from chronic lower respiratory diseases, including 669,637 in large central metropolitan, 630,341 in large fringe metropolitan, 643,229 in medium metropolitan, 328,634 in small metropolitan, 355,925 in micropolitan, and 283,626 in noncore counties. Total AAMRs (SE) declined from 45.4 (0.1) to 38.2 (0.1) from 1999 to 2019. AAMRs (SE) in large central metro areas were lowest in 1999 (42.3 [0.2] per 100,000) and declined the fastest (regression coefficient for annual change in AAMR, −0.49; 95% CI, −0.56 to −0.41) compared with all other urbanization categories (Table 1 and Figure 1). In contrast, micropolitan and noncore counties had higher AAMRs in 1999 and experienced increases in AAMRs (coefficients: 0.20 [0.11 to 0.30] and 0.41 [0.29 to 0.53], respectively). AAMR ratios increased in a dose-dependent relationship for all less urbanized counties when compared with large central metro counties, with the greatest increase among noncore counties between 1999 and 2019 (1.16 [95% CI, 1.14 to 1.19] to 1.83 [95% CI, 1.79 to 1.86]).
Table 1.
Regression Coefficients for Annual Change in AAMRs and AAMR Ratios for Chronic Lower Respiratory Diseases in the United States Stratified by County-Level Urbanization, 1999–2019
| Coefficient for Annual Change in AAMR per 100,000 Population (95% CI) | AAMR Ratio (95% CI) | ||
|---|---|---|---|
| Overall | −0.24 (−0.32 to −0.16) | 1999 | 2019 |
| Large central metro* | −0.49 (−0.56 to −0.41) | Reference | Reference |
| Large fringe metro* | −0.36 (−0.44 to −0.29) | 1.01 (1.00 to 1.03) | 1.16 (1.14 to 1.18) |
| Medium metro† | −0.24 (−0.31 to −0.16) | 1.10 (1.08 to 1.12) | 1.35 (1.33 to 1.37) |
| Small metro‡ | −0.08 (−0.17 to 0.00) | 1.18 (1.16 to 1.20) | 1.56 (1.54 to 1.59) |
| Micropolitan (nonmetro)§ | 0.20 (0.11 to 0.30) | 1.17 (1.15 to 1.20) | 1.76 (1.72 to 1.79) |
| Noncore (nonmetro)‖ | 0.41 (0.29 to 0.53) | 1.16 (1.14 to 1.19) | 1.83 (1.79 to 1.86) |
Definition of abbreviations: AAMR = age-adjusted mortality rate; CI = confidence interval; MSA = metropolitan statistical area.
Large central and large fringe metropolitan counties were in MSAs with a population of at least 1 million. Large metro counties were assigned to either of these two categories using a discriminant model incorporating multiple factors, including population density and housing type and distribution.
Medium metropolitan counties were in MSAs with a population in the range of 250,000 to 999,999.
Small metropolitan counties were in MSAs with a population below 250,000.
Micropolitan counties were in micropolitan statistical areas. These include an urbanized area with a population of 2,500 to 49,999.
Noncore counties are the most rural, as they do not qualify as metropolitan or micropolitan areas.
Figure 1.
Cytokine production profiles in patients with coronavirus disease (COVID-19) (A) before and after 4, 12, and 48 hours on extracorporeal membrane oxygenation (ECMO) alone (n = 11), and (B) before and after 4 hours on ECMO and after 12 and 48 hours with the CytoSorb adsorber combined with ECMO (n = 11). Dots represent individual subjects; bars show the median. Statistical analyses were conducted using the Wilcoxon signed-rank test. Comparisons were performed between before ECMO and after 4 hours on ECMO as well as between after ECMO and either 48 hours on ECMO (control group) or 48 hours on CytoSorb (CytoSorb group).
Disparities in mortality from chronic lower respiratory diseases widened in a dose-dependent manner between more rural compared with more urban counties in the United States from 1999 to 2019. Limitations include the use of death certificate data, which may be subject to miscoding but represent the most comprehensive national assessment of mortality statistics. Potential contributing factors to these findings include different smoking rates, environmental air quality, socioeconomic factors, or occupational exposures between more or less urbanized counties over time (7, 8). Investigations focused on the main drivers of our findings are needed to identify opportunities for interventions at the community level to decrease the burden of deaths from chronic lower respiratory diseases in rural areas within the United States.
Footnotes
Supported by NHLBI grant K08 HL146943.
Author Contributions: Conception and design: P.A.R., D.A.M., M.R.C., R.K., and S.S.K. Analysis and interpretation: P.A.R., B.K., J.B.P., D.A.M., and S.S.K. Drafting the manuscript for important intellectual content: P.A.R., M.R.C., R.K., and S.S.K.
Originally Published in Press as DOI: 10.1164/rccm.202011-4150LE on February 9, 2021
Author disclosures are available with the text of this letter at www.atsjournals.org.
References
- 1. Xu J, Murphy SL, Kockanek KD, Arias E. Mortality in the United States, 2018. NCHS Data Brief . 2020;355:1–8. [PubMed] [Google Scholar]
- 2. Probst JC, Zahnd WE, Hung P, Eberth JM, Crouch EL, Merrell MA. Rural-urban mortality disparities: variations across causes of death and race/ethnicity, 2013-2017. Am J Public Health . 2020;110:1325–1327. doi: 10.2105/AJPH.2020.305703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Croft JB, Wheaton AG, Liu Y, Xu F, Lu H, Matthews KA, et al. Urban-rural county and state differences in chronic obstructive pulmonary disease - United States, 2015. MMWR Morb Mortal Wkly Rep . 2018;67:205–211. doi: 10.15585/mmwr.mm6707a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Moore P, Atkins GT, Cramb S, Croft JB, Davis L, Dolor RJ, et al. COPD and rural health: a dialogue on the national action plan. J Rural Health . 2019;35:424–428. doi: 10.1111/jrh.12346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention, National Center for Health Statistics. Multiple cause of death 1999-2018 on CDC WONDER online database [released 2020; accessed 2021 Jan 6]. Available from: https://wonder.cdc.gov/mcd-icd10.html.
- 6. Ingram DD, Franco SJ. 2013 NCHS urban-rural classification scheme for counties. Vital Health Stat . 2014:1–73. [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention. 2019. https://www.cdc.gov/tobacco/disparities/geographic/index.htm
- 8.Housing Assistance Council. 2012. [Google Scholar]