To the Editor:
Among patients hospitalized with coronavirus disease (COVID-19), 15–30% die during hospitalization (1–3). However, specific causes of death, the prevalence of organ system dysfunction before death, and features of end-of-life care in patients with COVID-19 remain unclear. Before the pandemic, in cohorts of patients who died during hospitalization for acute hypoxemic respiratory failure (AHRF), death was rarely due to refractory respiratory failure. Pulmonary dysfunction was the primary cause of death for only one in every five decedents and only 2% had insupportable oxygenation or ventilation (4, 5). It is unknown whether causes and circumstances of death differ in patients with COVID-19–related respiratory failure versus historical cohorts with non–COVID-19–related respiratory failure—and specifically whether death due to pulmonary dysfunction is more common with COVID-19.
Methods
We performed a retrospective cohort study of adult patients (aged ≥18 yr) hospitalized with a laboratory-confirmed severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection at Michigan Medicine (March 1 to June 30, 2020) who experienced in-hospital death. Michigan Medicine is a tertiary medical center with approximately 1,000 beds that treated hundreds of patients with COVID-19 during the 2020 spring surge. In April 2020, Michigan was the third leading state for COVID-19–related deaths. Throughout the pandemic, COVID-19 therapies were used at the discretion of the treating physician as supported by the best evidence available at the time; there was limited use of remdesivir, systemic corticosteroids, or therapeutic anticoagulation.
Clinical data for decedents were extracted from the medical record by two internal medicine–trained physicians using a structured abstraction tool. The data included organ system dysfunction, septic shock, the primary cause of death, and withdrawal of life support, using definitions adapted from previous studies (4, 5). The primary organ system responsible for death was defined as the organ system dysfunction that most directly resulted in the patient’s death or the decision to withdraw life support. This approach to adjudicating the primary cause of death had excellent interrater reliability in previous studies (5), and there was full agreement between our abstractors on an initial set of 10 charts reviewed independently. Data on coinfection, goals-of-care discussions, advanced directives, spiritual support, respiratory support, and family presence at the time of death were also collected (6). The study definitions are presented in Table 1.
Table 1.
Definitions
| Goals-of-care discussion | Documentation of a conversation with the patient and/or a surrogate decision-maker regarding the patient’s wishes for end-of-life care. |
| Advanced directive* | Documentation in the electronic medical record of a durable power of attorney, healthcare proxy, or living will. |
| Spiritual support visitation* | Documentation of visitation by spiritual care services, chaplain services, or pastoral care with patient or family member interaction. Visitation may have taken place face to face or by telephone. |
| Organ dysfunction and infection within 72 h before death or withdrawal of life support | |
| Pulmonary† | Inability to liberate from mechanical ventilation, noninvasive ventilation, or heated high-flow nasal cannula due to inadequate oxygenation or ventilation without aforementioned support. |
| Neurologic‡ | Glasgow coma scale <8, or <6 if intubated. |
| Renal‡ | Either creatinine >5.0 mg/dl or requiring hemodialysis. |
| Cardiac‡ | Either cardiac output <2.0 L/min/m2 or documented cardiogenic shock (or) reversible ventricular fibrillation or asystole. |
| Hematologic‡ | Either fibrinogen <100 mg/dl, prothrombin time and partial thromboplastin time >1.5 times the upper limit of normal, or platelets <60,000 μl. |
| Hemorrhagic‡ | Mean arterial pressure <65 mm Hg for >2 h (or requiring vasopressors) necessitating blood transfusions and excluding other causes of hypotension. |
| Gastrointestinal‡ | Resectable ruptured or necrotic bowel, or pancreatitis causing mean arterial pressure <65 mm Hg for >2 h (or requiring vasopressors). |
| Hepatic‡ | Bilirubin >5.0 mg/dl and albumin <3.0 g/dl and prothrombin time or partial thromboplastin time >1.5 times upper limit of normal. |
| Multiorgan failure† | Presence of at least 2 dysfunctional organ systems. |
| Septic shock† | Mean arterial pressure <65 mm Hg for >2 h (or requiring vasopressors) attributed to either COVID-19 or other documented infection. |
| Coinfection | Non–COVID-19 culture-confirmed or PCR-confirmed infection being treated at the time of death. |
Finally, we compared causes of death with a previous cohort (5) of 385 patients admitted to Michigan Medicine with AHRF (January 1, 2016, to December 31, 2017) who experienced in-hospital death. We compared characteristics of patients with COVID-19 with patients with non–COVID-19–related respiratory failure using chi-square tests and considered P < 0.05 significant. Data analysis was completed in R. The study was deemed exempt by the University of Michigan Institutional Review Board.
Results
We identified 82 decedents with COVID-19 who were 32.9% female and 43.9% Black and had a median age 71 (61–81) years (Table 2). The most common organ dysfunctions before death were pulmonary (81.7%), neurologic (57.3%), and renal (39.0%). Out of the total, 74.4% of patients were mechanically ventilated during hospitalization. A multiorgan failure occurred in 67.1% and coinfection occurred in 41.5%. Septic shock was present in 40.2% (24.3% with coinfection and 15.9% without coinfection).
Table 2.
Circumstances of death in patients hospitalized with COVID-19 (N = 82)
| Parameter | n (%) | |
|---|---|---|
| Location of death | |
|
| ICU |
62 (75.6) | |
| General care |
20 (24.4) | |
| Goals-of-care discussion | ||
| Documented discussion |
80 (97.6) | |
| Face to face |
35 (42.7) | |
| Telephone |
73 (89.0) | |
| Virtual |
2 (2.4) | |
| Held within 72 h of admission to ICU, no./total no. ever admitted to ICU (%) |
43/72 (59.7) | |
| Held within 24 h of death or decision to withdraw life support |
75 (91.5) | |
| Advanced directives documented |
26 (31.7) | |
| Spiritual support visitation | ||
| Spiritual support visit was offered |
72 (87.8) | |
| Offered before intubation, no./total no. intubated and offered spiritual support (%) |
5/55 (9.1) | |
| Spiritual support visitation occurred |
66 (80.5) | |
| Visitation occurred before intubation, no./total no. intubated with visit (%) |
5/51 (9.8) | |
| Presence of friends and family before death | ||
| Physically present at bedside |
28 (34.1) | |
| Virtual visit within 24 h before death or withdrawal of life support |
13 (15.9) | |
| Both physically presence at bedside and virtual visit within 24 h |
4 (4.9) | |
| Neither presence at bedside nor virtual visit within 24 h |
45 (54.9) | |
| Respiratory support at time of death or decision to limit/withdraw life support | ||
| Room air |
4 (4.9) | |
| Nasal cannula oxygen |
11 (13.4) | |
| High-flow nasal cannula oxygen |
9 (11.0) | |
| Noninvasive positive pressure ventilation |
0 (0) | |
| IMV |
58 (70.7) | |
| IMV discontinued before death, no./total no. on IMV (%) |
37/58 (63.8) | |
| Patient on IMV at time of death, no./total no. on IMV (%) |
21/58 (36.2) | |
| Organ system dysfunction within 72 h of death | ||
| Pulmonary |
67 (81.7) | |
| Neurologic |
47 (57.3) | |
| Renal |
32 (39.0) | |
| Cardiac |
10 (12.2) | |
| Hematologic |
5 (6.1) | |
| Hemorrhagic |
3 (3.7) | |
| Gastrointestinal |
1 (1.2) | |
| Hepatic |
0 (0) | |
| Multiorgan failure |
55 (67.1) | |
| Septic shock |
33 (40.2) | |
| Other features at end of life | ||
| Coinfection |
34 (41.5) | |
| Withdrawal or limitation of life-sustaining interventions |
63 (76.8) | |
| Receiving cardiopulmonary resuscitation in last hour of life | 6 (7.3) | |
Definition of abbreviations: COVID-19 = coronavirus disease; ICU = intensive care unit; IMV = invasive mechanical ventilation.
The most common primary causes of death were pulmonary dysfunction (56.1%) and septic shock (26.8%). Compared with the historic cohort with non–COVID-19–related respiratory failure (who had a median age of 63 [55–73] yr and were 43% female and 82% white), patients with COVID-19 were more likely to die of pulmonary dysfunction (56.1% vs. 21.6%; P < 0.01) and less likely to die of cardiac (7.3% vs. 16.1%; P = 0.04) or neurologic (6.1% vs. 19.5%; P < 0.01) dysfunction (Figure 1).
Figure 1.
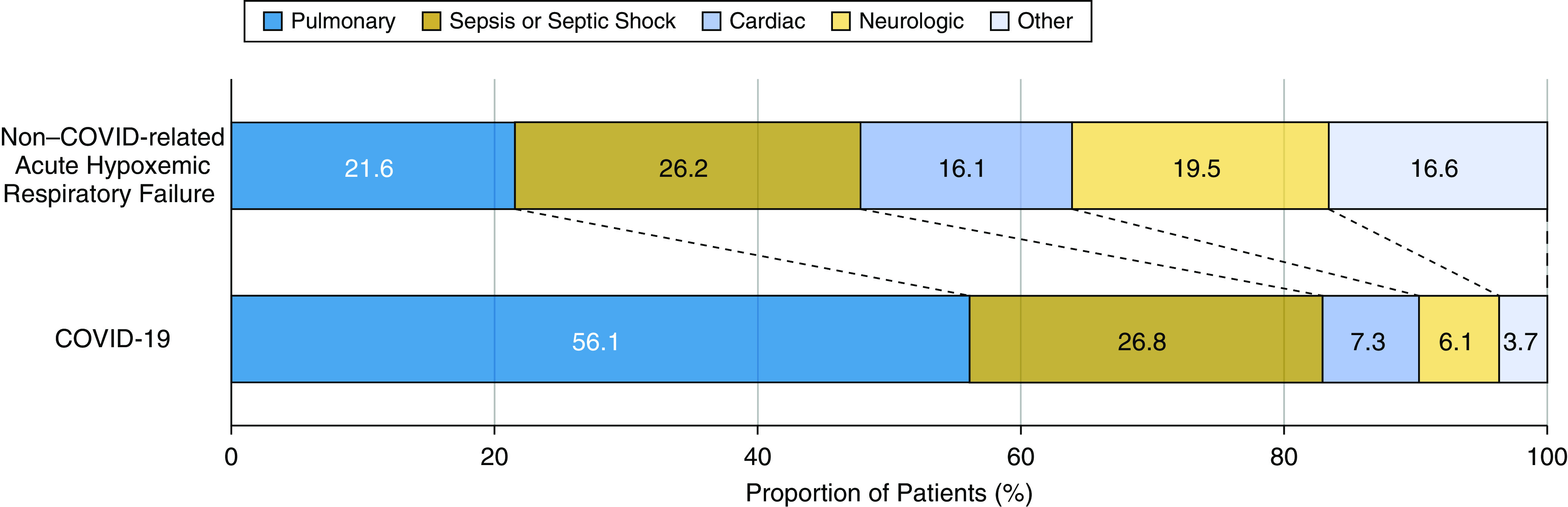
Primary cause of death in patients hospitalized with coronavirus disease (COVID-19) versus non–COVID-19–related acute hypoxemic respiratory failure. The figure shows that pulmonary dysfunction was the most common primary cause of death in patients with COVID-19 (N = 82). The proportion of patients with pulmonary dysfunction as the primary cause of death was more than twofold higher than recent cohorts of decedents with acute hypoxemic respiratory failure (N = 385). Death due to cardiac or neurologic dysfunction was less common among decedents with COVID-19.
Among decedents with COVID-19, at least one goals-of-care discussion was documented in 97.6%. Among the 72 patients ever treated in an intensive care unit, 59.7% had a goals-of-care discussion within 72 hours after the first intensive care unit admission. Discussions occurred by telephone (91.3% of discussions), in person (43.8%), or by videoconference (2.5%). Advanced directives were documented in 31.7%. Spiritual support was offered to 87.8% and a spiritual support visit occurred in 80.5%. Among the 51 patients who received both mechanical ventilation and a spiritual support visit, a visit occurred before intubation in 9.8%. Family/friends were physically present at the time of death for 34.1%, a virtual visit with family/friends occurred within 24 hours of death for 15.9%, and 4.9% had both family/friends physically present and a virtual visit, whereas 54.9% had neither family/friends present at death nor a virtual visit within 24 hours of death. Withdrawal or limitation of life-sustaining interventions occurred in 76.8%, including 37 (45.1%) who were terminally extubated before death. A total of 21 patients (25.6%) were receiving invasive mechanical ventilation at the time of death.
Discussion
In this cohort of patients who died during hospitalization for COVID-19, the most common causes of death were pulmonary dysfunction and septic shock from COVID-19 or a confirmed coinfection. Pulmonary dysfunction was the primary cause of death for 56% of decedents with COVID-19, compared with only 22% in a recent cohort of decedents with acute hypoxic respiratory failure due to other causes (5). However, sepsis was the primary cause of death in approximately one-fourth of both patients with COVID-19 and those with non–COVID-19–related respiratory failure. These two most common causes of death underscore the importance of appropriate delivery of invasive respiratory support and early recognition and treatment of infection. In addition, these findings suggest that although patients with non–COVID-19–related AHRF often die of downstream complications, patients with COVID-19–related respiratory failure more often die as a direct consequence of their infection. As such, the development of new therapeutic strategies that reduce the severity of lung injury in COVID-19 may improve survival.
Family or friends were physically present for only one-third of deaths, compared with 80% in past cohorts (6). In addition, patients and families had minimal face-to-face interaction with their healthcare team, with less than half of patients and families having face-to-face goals-of-care discussions. These findings likely reflect the impact of restricted visitation policies established during the pandemic, both in Michigan and elsewhere (7, 8). In addition, despite the wide availability of videoconferencing tools (9), videoconferencing was rarely used for discussing goals of care. This represents a potential opportunity to improve patient and family interaction when physical presence is limited (10). The generalizability of our findings may be limited by a small sample size, single-center design, and potential changes in causes of death as COVID-19 management continues to evolve.
Acknowledgments
Acknowledgment
The authors thank Elizabeth McLaughlin, program manager for Michigan–COVID-19 registry for assistance with identifying Michigan Medicine patients in the Michigan–COVID-19 registry.
Footnotes
Supported by the Ann Arbor Veterans Medical Center and the Blue Cross Blue Shield/Blue Care Network of Michigan.
Author Contributions: All authors made substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work; and to drafting the work or revising it critically for important intellectual content; and provided final approval of the version submitted for publication; and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work.
Author disclosures are available with the text of this letter at www.atsjournals.org.
References
- 1. Wiersinga WJ, Rhodes A, Cheng AC, Peacock SJ, Prescott HC. Pathophysiology, transmission, diagnosis, and treatment of coronavirus disease 2019 (COVID-19): a review. JAMA. 2020;324:782–793. doi: 10.1001/jama.2020.12839. [DOI] [PubMed] [Google Scholar]
- 2. Ruan Q, Yang K, Wang W, Jiang L, Song J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med. 2020;46:846–848. doi: 10.1007/s00134-020-05991-x. [Published erratum appears in Intensive Care Med 46:1294–1297.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kim L, Garg S, O’Halloran A, Whitaker M, Pham H, Anderson EJ, et al. Risk factors for intensive care unit admission and in-hospital mortality among hospitalized adults identified through the U.S. coronavirus disease 2019 (COVID-19)-associated hospitalization surveillance network (COVID-NET) Clin Infect Dis [online ahead of print] 16 Jul 202010.1093/cid/ciaa1012 [DOI] [PMC free article] [PubMed]
- 4. Stapleton RD, Wang BM, Hudson LD, Rubenfeld GD, Caldwell ES, Steinberg KP. Causes and timing of death in patients with ARDS. Chest. 2005;128:525–532. doi: 10.1378/chest.128.2.525. [DOI] [PubMed] [Google Scholar]
- 5. Ketcham SW, Sedhai YR, Miller HC, Bolig TC, Ludwig A, Co I, et al. Causes and characteristics of death in patients with acute hypoxemic respiratory failure and acute respiratory distress syndrome: a retrospective cohort study. Crit Care. 2020;24:391. doi: 10.1186/s13054-020-03108-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kruser JM, Aaby DA, Stevenson DG, Pun BT, Balas MC, Barnes-Daly MA, et al. Assessment of variability in end-of-life care delivery in intensive care units in the United States. JAMA Netw Open. 2019;2:e1917344. doi: 10.1001/jamanetworkopen.2019.17344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Valley TS, Schutz A, Nagle MT, Miles LJ, Lipman K, Ketcham SW, et al. Changes to visitation policies and communication practices in Michigan ICUs during the COVID-19 pandemic. Am J Respir Crit Care Med. 2020;202:883–885. doi: 10.1164/rccm.202005-1706LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kitano T, Piché-Renaud P-P, Groves HE, Streitenberger L, Freeman R, Science M.Visitor restriction policy on pediatric wards during novel coronavirus (COVID-19) outbreak: a survey study across North America J Pediatric Infect Dis Soc [online ahead of print] 22 Oct 202010.1093/jpids/piaa126 [DOI] [PMC free article] [PubMed]
- 9.Pew Research Center. Washington, DC: Pew Research Center; 2019. Demographics of mobile device ownership and adoption in the United States Pew Research Center. [accessed 2020 Oct 22]. Available from: https://www.pewresearch.org/internet/fact-sheet/mobile/ [Google Scholar]
- 10. Humphreys J, Schoenherr L, Elia G, Saks NT, Brown C, Barbour S, et al. Rapid implementation of inpatient telepalliative medicine consultations during COVID-19 pandemic. J Pain Symptom Manage. 2020;60:e54–e59. doi: 10.1016/j.jpainsymman.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]


