Abstract
In the midst of the COVID-19 pandemic, we report two cases of children presenting with typical diagnosis of pediatric inflammatory multisystem syndrome temporally associated with SARS-CoV-2 (PIMS-TS) who suffered from complete heart block requiring pacemaker placement which is an unusual presentation of PIMS-TS. We also compared it with the already existing data with similar manifestations. PIMS-TS is reported to occur in children with predominantly gastrointestinal symptoms, hemodynamic instability, and myocardial dysfunction. The implications of development of atrioventricular block during critical illness in PIMS-TS are yet unknown. Both patients had an otherwise normal cardiac structure and had no gastrointestinal symptoms but suffered complete heart block without any other identifiable etiology, both requiring temporary pacemaker placement. While one child recovered completely with medical management, the other child required permanent pacemaker placement. While we cannot be certain that COVID-19 was the cause, complete heart block appeared to be temporally related to COVID-19 infection in both patients, and hence, it is important for pediatricians to be aware of the potential manifestation of this disease.
Keywords: COVID-19, heart block, pacemaker, pediatric inflammatory multisystem syndrome temporally associated with SARS-CoV-2, SARS-CoV-2
INTRODUCTION
The Royal College of Pediatrics and Child Health has published a guidance and case definition of pediatric inflammatory multisystem syndrome temporally associated with SARS-CoV-2 (PIMS-TS) on May 1, 2020.[1] PIMS-TS typically affects children with an average age group around 9–15 years.[2] It is postulated that PIMS-TS is not an acute COVID-19 infection but is likely a postimmunological reaction.[3] Various cardiac manifestations of PIMS-TS have been reported, namely pericardial effusion, ventricular arrhythmia, myocarditis, valvular regurgitation, and pericarditis. Although cardiac involvement in PIMS-TS is well described including various conduction abnormalities, advanced atrioventricular block (AVB) in these patients is not common and few cases of heart block suffering from SARS-CoV-2 have been reported.[4,5,6]
Here, we report two children with PIMS-TS requiring pacemaker placement. Of note, none of the children in this discussion suffered from the usual manifestations of rash, gastrointestinal symptoms, diarrhea, or respiratory distress.
CASE REPORTS
Case 1
A 6-year-old boy presented in the emergency room with complaints of sudden syncopal attacks. He had fever for the past 4 days. Examination revealed that he had a heart rate of 32 beats/min, poor peripheral perfusion, and normal sensorium. Electrocardiogram (ECG) showed complete heart block with a ventricular rate of 30/min and echocardiogram showed a structurally normal heart with thin rim of pericardial effusion and mild ventricular dysfunction. Oxygen saturation was normal and he did not require any respiratory support. He was started on isoprenaline and adrenaline infusion and was immediately taken up for temporary pacemaker implantation (TPI). His laboratory work-up was remarkable for neutrophilic leukocytosis (22,000 cells/mm3, 77% polymorphs), elevated serum urea/creatinine (63/1.7), transaminitis (aspartate transaminase [AST]: 1493 U/L and alanine aminotransferase: 2501 U/L), elevated inflammatory markers (C-reactive protein [CRP]: 33 mg/dL, lactate dehydrogenase [LDH]: 1751 U/L, and ferritin: 2227), elevated creatinine phosphokinase (1306 U/L), troponin I (46.5 ng/mL), and NT-Pro-B-type natriuretic peptide (BNP) (12,148 pg/ml). A nasopharyngeal swab test for COVID-19 on real-time reverse transcriptase-polymerase chain reaction (RT-PCR) assay was negative, but SARS-CoV-2 immunoglobulin G (IgG) antibody to S-protein was positive (5.04). Nasopharyngeal swab for respiratory viral panel to rule out other causes of myocarditis was sent as a part of routine work-up for suspected viral myocarditis, which turned out to be negative. Overall clinical and laboratory parameters of this child fulfilled the criteria for PIMS-TS. The child was treated with intravenous gamma globulin (IVIg) at a dose of 2 g/kg and pulse methylprednisolone at a dose of 30 mg/kg considering the disease as life-threatening PIMS. Rhythm was found to be predominantly sinus with intermittent junctional escapes 2 days after TPI. The rhythm reverted to sinus after 5 days. The temporary pacemaker lead was removed and the child was discharged without any residual cardiac morbidity. The child was found to have sinus rhythm during his routine follow-up at 2 months after the illness. Figure 1 shows ECG findings of this child.
Figure 1.
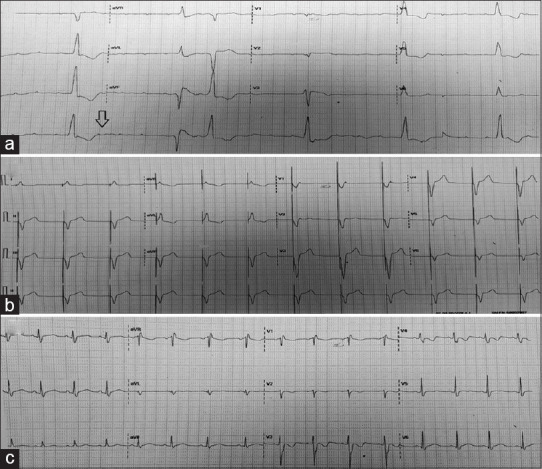
(a) Electrocardiogram during complete heart block with a heart rate of 30/min (black arrow points the P wave not conducted to produce QRS complex). (b) Electrocardiogram after temporary pacemaker insertion. (c) Complete return to sinus rhythm
Case 2
A 7½-year-old girl presented in the emergency room with fever for 6 days and recurrent convulsions, with a heart rate of 26 beats/min and poor peripheral perfusion, and was in postictal confusion state. Prior to admission at our center, she was admitted for 2 days at another facility. ECG showed complete heart block with a ventricular rate of 26/min. Echocardiogram showed structurally normal heart with mildly dilated left ventricle, mild left ventricular systolic dysfunction, moderate bilateral pleural effusion, and mild pericardial effusion. Oxygen saturation was found to be within normal limits and she did not require any respiratory support. She was started on isoprenaline and adrenaline infusion and was immediately taken up for TPI. Her laboratory work-up was remarkable for elevated urea/creatinine (89/0.9 units), transaminitis (AST: 332 U/L 321 U/L), elevated acute-phase reactants LDH (982 U/L), CRP (44 mg/dl), elevated NT-Pro-BNP (10,124 pg/ml), creatinine phosphokinase (1306 U/L), and troponin I (29,085 ng/mL). A nasopharyngeal swab test for COVID-19 on RT-PCR assay was negative, but SARS-CoV-2 IgG antibody to S-protein was positive (1.70), all pointing toward the diagnosis of PIMS-TS. Nasopharyngeal swab for respiratory viral panel to rule out other causes of myocarditis was sent for this child also which turned out to be negative. This child was also treated with IVIg at a dose of 2 g/kg and pulse methylprednisolone at a dose of 30 mg/kg/day. While all the inflammatory markers including CRP and LDH normalized, she remained completely pacemaker dependent even 10 days after TPI. Dual-chamber pacemaker was inserted via transvenous route on the 12th day of admission removing the temporary pacemaker lead. She remained pacemaker dependent during 1-month follow-up where the pacemaker was found to be functioning as A sensed V paced mode. Figure 2 shows ECG findings of this child.
Figure 2.
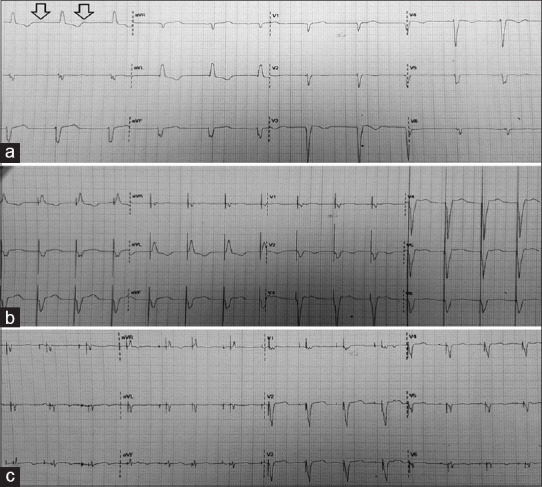
(a) Complete heart block (black arrow points the P waves not having any fixed relationship with QRS complexes with varying PR interval). (b) Electrocardiogram after temporary pacemaker implantation. (c) Electrocardiogram after permanent pacemaker implantation DDDR mode
DISCUSSION
Cardiac involvement in PIMS-TS is well described in the literature. Ventricular dysfunction, valvulitis, pericardial effusion, and coronary artery abnormalities are the predominant cardiac lesions found to be commonly associated with PIMS-TS. Conduction abnormality has been described in PIMS-TS, and ventricular ectopics, PR segment prolongation, ST-segment changes, and bundle branch blocks are the commonly described conduction abnormalities found in PIMS-TS. Advanced AVBs, though described in the literature, are rare and incidence of complete heart block requiring permanent pacemaker implantation is not described in PIMS-TS. We have summarized the common conduction abnormalities found in PIMS-TS and the requirement of pacemakers in Table 1.
Table 1.
Various electrophysiologic changes in children suffering from pediatric inflammatory multisystem syndrome temporally associated with severe acute respiratory syndrome coronavirus 2
| Study | ECG changes (number of patients) | Recovery to normal (yes/no) | Pacemaker requirement (yes/no) |
|---|---|---|---|
| Valverde et al.[7] | Abnormal ST or T wave segment (63) | Yes | No |
| Prolonged PR interval (18) | Yes | No | |
| Bundle branch block (11) | Yes | No | |
| Prolonged QT interval (9) | Yes | No | |
| AVB (6) | Yes | No | |
| Tachyarrhythmias (5) | Yes | No | |
| Abnormal Q waves (3) | Yes | No | |
| Clark et al.[8] | Complete atrioventricular block (1) | Yes | No |
| Transient second-degree AVB (1) | Yes | No | |
| Sinus pause (1) | Yes | No | |
| Ventricular tachycardia (2) | Yes | No | |
| Idioventricular rhythm (1) | Yes | No | |
| Dionne et al.[9] | First-degree AVB (1) | Yes | No |
| Mobitz Type I (2) | Yes | No | |
| Mobitz Type II in (1) | Yes | No | |
| Third-degree AVB (1) | Yes | No | |
| QTc prolongation (7) | Yes | No | |
| Nonspecific ST-segment changes (14) | Yes | No | |
| Atrial ectopy (2) | Yes | No | |
| Sustained ectopic atrial tachycardia (1) | Yes | No | |
| Choi et al.[10] | First-degree AVB (6) | Yes | No |
| Prolonged QTc interval (4) | Yes | No | |
| Ectopic atrial rhythm (1) | Yes | No | |
| ST elevation or depression (3) | Yes | No | |
| T wave inversions (5) | Yes | No | |
| Nonspecific ST and/or T wave abnormalities (14) | Yes | No | |
| Nonspecific intraventricular conduction delay or right ventricular conduction delay (5) | Yes | No | |
| Right axis deviation (5) | Yes | No | |
| Intermittent premature ventricular complexes (1) | Yes | No | |
| Domico et al.[11] | Second-degree Type II heart block (1) | Yes | Yes (temporary pacing was removed on D-6) |
AVB: Atrioventricular block, ECG: Electrocardiogram
The mechanism of cardiac involvement in PIMS-TS is speculative. Immune-mediated myocardial damage, direct myocardial invasion by the virus, and systemic inflammation-mediated myocardial damage are described as the possible mechanisms of myocardial involvement in PIMS-TS.[7,12,13] Based on the facts that coronavirus not being a cardiotropic virus, negative result of COVID-19 virus on RT-PCR assay, elevated inflammatory markers, and beneficial response to immunomodulators, majority of the authors have suggested that the immune-mediated myocardial involvement is the probable mechanism for cardiac manifestation in PIMS-TS. In both the cases, inflammatory markers were elevated. In one of our cases, the AVB resolved with IVIg and steroids, indicating that the mechanism of complete heart block is probably immune mediated. The other patient required permanent pacemaker placement, suggesting that although the mechanism is immune mediated, the damage can be permanent and irreversible. In our series, we encountered an advanced heart block as the major involvement in PIMS rather than gastrointestinal symptoms or pneumonia, and following the administration of IVIg and steroid, there was a significant recovery of myocardial dysfunction.
It may be postulated that the AV node can get involved in PIMS and early institution of IVIg and steroid may prevent permanent damage of the AV node.
Limitation
We did not perform the endomyocardial biopsy for both the children which might have helped in postulating the cause of conduction abnormality in patients with PIMS-TS.
CONCLUSIONS
PIMS is expanding its clinical spectrum and has been reported to affect the cardiovascular system in different patterns. This is a rare presentation of PIMS with new-onset complete heart block in the setting of COVID-19 infection. Our case series shows that COVID-19-associated PIMS may be associated with acute-onset complete heart block. Prompt recognition and management is important. Children suspected to have COVID-19-associated PIMS should have their heart rhythm monitored so that changes in cardiac rhythm can be detected as early as possible. These children have high values of cardiac enzymes and NT-Pro-BNP levels, so any children with elevation in these should be closely monitored for their rhythm.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the guardians have given their consent for images and other clinical information to be reported in the journal. The guardians understand that names and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We would like to thank the patients for allowing to publish.
REFERENCES
- 1.Paediatric Multisystem Inflammatory Syndrome Temporally Associated with COVID-19 (PIMS) - Guidance for Clinicians. RCPCH. [Last accessed on 2021 Apr 20]. Available from: https://www.rcpch.ac.uk/resources/paediatric-multisystem-inflammatorysyndrome-temporally-associated-covid-19-pimsguidance .
- 2.Whittaker E, Bamford A, Kenny J, Kaforou M, Jones CE, Shah P, et al. Clinical characteristics of 58 children with a pediatric inflammatory multisystem syndrome temporally associated with SARS-CoV-2. JAMA. 2020;324:259–69. doi: 10.1001/jama.2020.10369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Davies P, Evans C, Kanthimathinathan HK, Lillie J, Brierley J, Waters G, et al. Intensive care admissions of children with paediatric inflammatory multisystem syndrome temporally associated with SARS-CoV-2 (PIMS-TS) in the UK: A multicentre observational study. Lancet Child Adolesc Health. 2020;4:669–77. doi: 10.1016/S2352-4642(20)30215-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kaushik S, Aydin SI, Derespina KR, Bansal PB, Kowalsky S, Trachtman R, et al. Multisystem inflammatory syndrome in children associated with severe acute respiratory syndrome coronavirus 2 infection (MIS-C): A multi-institutional study from New York City. J Pediatr. 2020;224:24–9. doi: 10.1016/j.jpeds.2020.06.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Haddadin FI, Mahdawi TE, Hattar L, Beydoun H, Fram F, Homoud M. A case of complete heart block in a COVID-19 infected patient. J Cardiol Cases. 2021;23:27–30. doi: 10.1016/j.jccase.2020.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lawrensia S, Henrina J, Wijaya E, Suciadi LP, Saboe A, Cool CJ. Pediatric inflammatory multisystem syndrome temporally associated with SARS-CoV-2: A new challenge amid the pandemic. SN Compr Clin Med. 2020:1–9. doi: 10.1007/s42399-020-00602-8. doi: 10.1007/s42399-020-00602-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Valverde I, Singh Y, Sanchez-de-Toledo J, Theocharis P, Chikermane A, Di Filippo S, et al. Acute cardiovascular manifestations in 286 children with multisystem inflammatory syndrome associated with COVID-19 infection in Europe. Circulation. 2021;143:21–32. doi: 10.1161/CIRCULATIONAHA.120.050065. [DOI] [PubMed] [Google Scholar]
- 8.Clark BC, Sanchez-de-Toledo J, Bautista-Rodriguez C, Choueiter N, Lara D, Kang H, et al. Cardiac abnormalities seen in pediatric patients during the SARS-CoV2 Pandemic: An international experience. J Am Heart Assoc JAHA. 2020;9:e018007. doi: 10.1161/JAHA.120.018007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dionne A, Mah DY, Son MB, Lee PY, Henderson L, Baker AL, de Ferranti SD, et al. Atrioventricular block in children with multisystem inflammatory syndrome. Pediatrics. 2020;146:e2020009704. doi: 10.1542/peds.2020-009704. [DOI] [PubMed] [Google Scholar]
- 10.Choi NH, Fremed M, Starc T, Weller R, Cheung E, Ferris A, et al. MIS-C and cardiac conduction abnormalities. Pediatrics. 2020;146:e2020009738. doi: 10.1542/peds.2020-009738. [DOI] [PubMed] [Google Scholar]
- 11.Domico M, McCanta AC, Hunt JL, Ashouri N, Nugent D, Kelly RB. High-grade heart block requiring transvenous pacing associated with multisystem inflammatory syndrome in children during the COVID-19 pandemic. Heart Rhythm Case Rep. 2020;6:811–4. doi: 10.1016/j.hrcr.2020.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Oudit GY, Kassiri Z, Jiang C, Liu PP, Poutanen SM, Penninger JM, et al. SARS-coronavirus modulation of myocardial ACE2 expression and inflammation in patients with SARS. Eur J Clin Invest. 2009;39:618–25. doi: 10.1111/j.1365-2362.2009.02153.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Persistent Complete Heart Block in a Patient with COVID-19 Infection: A Case Report | SpringerLink. [Last accessed on 2021 Apr 14]. Available from: https://link.springer.com/article/100.1007/s42399-020-00712-3 . [DOI] [PMC free article] [PubMed]


