Abstract
Cross-reactions with Fusobacterium necrophorum were found in a PCR designed for detection of a wide range of mycoplasma species. Twenty-five strains of Fusobacterium were examined; all 14 F. necrophorum strains reacted positively, whereas all 7 Fusobacterium nucleatum strains reacted negatively. Two strains that were not F. necrophorum yielded variable results.
Detection of growth in blood cultures without subsequent growth on subculture represents a diagnostic dilemma. During an attempt to solve this problem we encountered the highly unexpected outcome of the blood cultures yielding growth of Fusobacterium necrophorum but not of mycoplasmas, while the same blood cultures were strongly reactive in a PCR assay designed for detection of a wide range of mycoplasma species. Thereafter laboratory investigations were performed in order to elucidate the cross-reactions.
A 15-year-old girl was admitted to the hospital because of fever and coughing that had persisted for several weeks. A chest radiograph revealed a pleural exudate, emphysema, and multiple abscesses in the right lower lobe. Growth from sputum and exudate was negative, whereas the anaerobic bottles of two blood culture sets (ESP; Difco) gave positive signals. Initial subcultures after 2 days’ incubation were, however, negative. Since growth of mycoplasmas was suspected, inter alia, the blood cultures were sent to the national reference laboratory, where the following two avenues of investigation were pursued: renewed prolonged subcultivation for anaerobic bacteria and examination for mycoplasmas by culture and by a PCR method (11) designed and evaluated for detection of a wide range of Mollicutes (mycoplasmas) in cell cultures including Mycoplasma pneumoniae, Mycoplasma hominis, and Ureaplasma urealyticum. Broth from the anaerobic bottles was strongly reactive in the Mollicutes PCR; at about the same time anaerobic subcultures from the bottles yielded growth of F. necrophorum after 3 days’ incubation. Attempts to isolate mycoplasmas were unsuccessful, and tests for M. pneumoniae antibodies by complement fixation test, as well as cold agglutinins, were negative (titer of <16). The patient was treated with clindamycin for 3 weeks and recovered uneventfully.
The 25 Fusobacterium strains examined in this study are listed in Table 1. The strains were grown on anaerobic agar from the Statens Serum Institut (5) and identified by means of standard methods, including gas-liquid chromatography (4, 10).
TABLE 1.
Results of Mollicutes PCR on 25 strains of Fusobacterium spp.
| Strain | Mollicutes PCRa (MGSO/GPO-3) |
|---|---|
| F. necrophorum | |
| F22 | + |
| F24 | + |
| F25 | + |
| F29 | + |
| F30 | + |
| F32 | + |
| F33 | + |
| F34 | + |
| F35 | + |
| F36 | + |
| F37 | + |
| F38 | + |
| F39 | + |
| TJ9-17 | + |
| F. gonidiaformans | |
| F11 | − |
| F. naviforme | |
| F1 | (+) |
| F21 | − |
| F. nucleatum | |
| F13 | − |
| F14 | − |
| F20 | − |
| F40 | − |
| TJ 62-2 | − |
| TJ 62-11 | − |
| TJ 62-12 | − |
| Fusobacterium sp. | |
| AB 04012b | + |
+, positive reaction; (+), weakly positive reaction; −, negative reaction.
This strain biochemically most resembled F. mortiferum (see text).
Isolation of mycoplasmas was attempted by inoculation of SP4, Hayflick, U10C (9), and modified Friis (6), quality-controlled broth, and agar media with subsequent blind passage. Cultures were kept for 5 weeks without showing any signs of growth.
For PCR, broth medium from the anaerobic blood culture bottle or bacterial growth corresponding to one-quarter to one-half of a colony was boiled with a 20% (wt/vol) Chelex 100 slurry (Bio-Rad, Richmond, Calif.) in Tris-EDTA buffer (10 mM Tris-HCl [pH 8.0], 1 mM EDTA). Ten microliters of the supernatant was used for PCR. A 270-bp fragment of the 16S rRNA gene was amplified with primers GPO-3 and MGSO, deduced from an alignment of 16S rRNA sequences (11). In control experiments primer GPO-1 (11) was used in combination with MGSO. All reactions were carried out with an internal process control in order to control for inhibition. A manual hot-start procedure (1) and thermocycling including a “touchdown” procedure (2, 3) during the first 10 cycles was used in order to increase amplification specificity. The amplified samples were subjected to agarose gel electrophoresis.
All isolates of F. necrophorum, including two initially identified as Fusobacterium pseudonecrophorum (F29 and F38), gave a positive reaction in the Mollicutes PCR (Table 1). One Fusobacterium isolate (AB 04012), identified only to the genus level and biochemically not in accordance with F. necrophorum (it was lipase negative, esculin hydrolysis positive, and β-galactosidase positive) but resembling Fusobacterium mortiferum except for being indole positive, also gave a positive result. All isolates of Fusobacterium nucleatum and the single isolate of Fusobacterium gonidiaformans were negative, while one of two isolates of Fusobacterium naviforme gave a weak positive reaction. In control experiments with the MGSO/GPO-1 primer set, all strains of Fusobacterium as well as the anaerobic blood culture gave negative results.
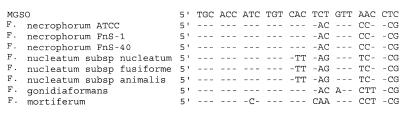
As can be seen in Fig. 1, several mismatches were present in the 3′ end of the MGSO primer. These mismatches should theoretically make amplification impossible. Furthermore, the touchdown procedure and the increased annealing temperature (from 55°C in the method described by van Kuppeveld et al. [11] to 57°C in our assay) should increase the specificity of the primer annealing.
FIG. 1.
Alignment of the MGSO primer used in the mollicutes PCR with selected available 16S rDNA sequences of Fusobacterium spp. Dashes indicate identity with the primer sequence.
We have previously used the primers MGSO and GPO-3 for detection of mycoplasmas in cell cultures with good results and attempted to extend their use to human clinical specimens obtained from usually sterile sites. Even though the specificity of the primers had been evaluated extensively by van Kuppeveld et al. (11) with particular emphasis on those genera most closely related to the Mollicutes, namely, Clostridium, Bacillus, Lactobacillus, and Streptococcus, unexpected cross-reactions were observed with the MGSO/GPO-3 primer combination when DNA from F. necrophorum was tested. Surprisingly, the cross-reactions were abolished when the GPO-3 primer was replaced with the GPO-1 primer. Both primers were designed from general prokaryotic 16S rDNA sequences, and consequently their specificities are expected to be the same. However, compared with the available 16S sequences from fusobacteria, primer GPO-1 had a 3′-terminal A:G mismatch. Such mismatches are known to be very efficient in terms of decreasing the yield of a PCR product (7). GPO-3 also had a single mismatch, but in the GPO-3 primer this mismatch (G:T) was located in the 5′ end of the primer and thus did not affect the amplification.
Our findings emphasize the need for thorough evaluation of all PCR methods before they are used for new categories of clinical specimens. Regardless of the efforts that have been put into validation, PCR methods cannot be accepted for diagnostic use exclusively on the basis of database searches for sequence homology of the primers and on specificity evaluations of cultures of phylogenetically related bacteria and of those which are commonly found in the specimens in question. Evaluations of specificity should always be performed on large panels of well-characterized clinical specimens. Whenever unexpected results are found, careful interpretation should be made. Testing with a set of unrelated primers in a confirmatory PCR assay (8) may help to avoid obtaining false-positive results on the basis of both cross-reactions and PCR product contamination and is therefore highly recommended.
Acknowledgments
Jette Nielsen and Birthe Dohn are thanked for expert technical assistance.
REFERENCES
- 1.Chou Q, Russell M, Birch D E, Raymond J, Bloch W. Prevention of pre-PCR mis-priming and primer dimerization improves low-copy-number amplifications. Nucleic Acids Res. 1992;20:1717–1723. doi: 10.1093/nar/20.7.1717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Don R H, Cox P T, Wainwright B J, Baker K, Mattick J S. ‘Touchdown’ PCR to circumvent spurious priming during gene amplification. Nucleic Acids Res. 1991;19:4008. doi: 10.1093/nar/19.14.4008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hecker K H, Roux K H. High and low annealing temperatures increase both specificity and yield in touchdown and stepdown PCR. BioTechniques. 1996;20:478–485. doi: 10.2144/19962003478. [DOI] [PubMed] [Google Scholar]
- 4.Holdeman L V, Cato E P, Moore W E C. Anaerobe laboratory manual. Blacksburg, Va: Virginia Polytechnic Institute and State University; 1977. [Google Scholar]
- 5.Jansen J E, Bremmelgaard A. Effect of culture medium and carbon dioxide concentration on growth of anaerobic bacteria and medium pH. Acta Pathol Microbiol Immunol Scand Sect B. 1986;94:319–323. doi: 10.1111/j.1699-0463.1986.tb03059.x. [DOI] [PubMed] [Google Scholar]
- 6.Jensen J S, Hansen H T, Lind K. Isolation of Mycoplasma genitalium strains from the male urethra. J Clin Microbiol. 1996;34:286–291. doi: 10.1128/jcm.34.2.286-291.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kwok S, Kellogg D E, McKinney N, Spasic D, Goda L, Levenson C, Sninsky J J. Effects of primer-template mismatches on the polymerase chain reaction: human immunodeficiency virus type 1 model studies. Nucleic Acids Res. 1990;18:999–1005. doi: 10.1093/nar/18.4.999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mahony J B, Luinstra K E, Jang D, Sellors J, Chernesky M A. Chlamydia trachomatis confirmatory testing of PCR-positive genitourinary specimens using a 2nd set of plasmid primers. Mol Cell Probes. 1992;6:381–388. doi: 10.1016/0890-8508(92)90031-r. [DOI] [PubMed] [Google Scholar]
- 9.Razin S, Tully J G. Methods in mycoplasmology. 1. Mycoplasma characterization. New York, N.Y: Academic Press, Inc.; 1983. [Google Scholar]
- 10.Summanen P, Baron E J, Citron D M, Strong C, Wexler H M, Finegold S M. Wadsworth anaerobic bacteriology manual. Belmont, Calif: Star Publishing Company; 1993. [Google Scholar]
- 11.van Kuppeveld F J M, van der Logt J T M, Angulo A F, van Zoest M J, Quint W G V, Niesters H G M, Galama J M D, Melchers W J G. Genus- and species-specific identification of mycoplasmas by 16S rRNA amplification. Appl Environ Microbiol. 1992;58:2606–2615. doi: 10.1128/aem.58.8.2606-2615.1992. . (Erratum, 59:655.) [DOI] [PMC free article] [PubMed] [Google Scholar]