Abstract
Background
While it is known that sex and race/ethnic disparities persist for atherosclerotic cardiovascular disease (ASCVD), disparities in risk factor control have not been well-described in primary care where ASCVD can be prevented.
Methods
Adult patients with a hypertension diagnosis without ASCVD were included in this analysis of electronic health records from a large US healthcare system from 2018. Patients were categorized based on risk factor control defined as blood pressure (BP) <130/80 mm Hg; statin prescription among patients with indications, HbA1c of <7%, and not smoking. Multivariable Poisson regressions were developed to explore associations with race/ethnicity. Results are presented as relative risk (RR), 95% confidence intervals (CIs).
Results
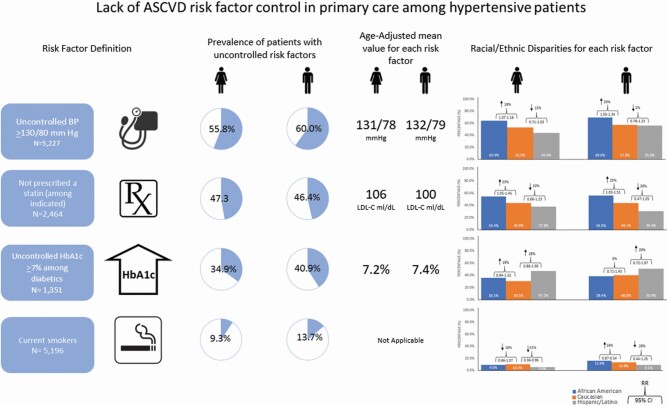
Among 5,227 patients, 55.8% women and 60.0% men had uncontrolled BP, 47.3% women and 46.4% men with statin therapy indication did not have a prescription, 34.9% women and 40.9% men had uncontrolled HbA1c values, and 9.3% women and 13.7% men were smokers. African Americans were more likely to have uncontrolled BP (women: RR 1.18, 95% CI 1.07–1.30; men: RR 1.20, 95% CI 1.05–1.34) and more likely to lack a statin prescription (women: RR 1.23, 95% CI 1.05–1.45; men: RR 1.25, 95% CI 1.03–1.51) compared to Caucasians. Differences in HbA1c control were not statistically significant among Hispanic/Latino compared to Caucasians (women: RR 1.28, 95% CI 0.86–1.90; men: RR 1.20, 95% CI 0.72–1.97).
Conclusions
Disparities in controlling ASCVD risk factors in primary care persist and were not fully explained by demographic or clinical characteristics. Monitoring changes in disparities is important to ensure equity as interventions to prevent ASCVD in primary care are developed and implemented.
Keywords: blood pressure, clinical practice guidelines, CVD, disparities, hypertension, risk factor control
Graphical Abstract
Graphical Abstract.
Atherosclerotic cardiovascular disease (ASCVD) remains the leading cause of mortality in the world with approximately 17.7 million deaths annually.1 Patients with hypertension are at higher risk of developing ASCVD if blood pressure (BP) and other risk factors are not controlled.1,2 There is evidence from randomized controlled trials that risk factors can be controlled and that reaching targets recommended by clinical practice guidelines reduces the risk of developing ASCVD.2–5 Over the last few decades, efforts to control risk factors, through pharmacotherapy and lifestyle changes have led to measurable reductions in ASCVD events and mortality.6 However, evidence for racial and ethnic disparities persists in the United States.7 Evaluating disparities prior to developing ASCVD, can help identify gaps in care and prevent augmentation of these disparities if and when ASCVD is diagnosed.
We used electronic health record (EHR) data from a large integrated healthcare system in Midwestern United States to describe disparities in concordance with clinical practice guideline for ASCVD risk factor control among patients diagnosed with hypertension and managed in primary care. Clinical practice guidelines for these risk factors were updated in 2017 for hypertension and 2018 for statin therapy. We report our results based on these updated guidelines. Recommendations include BP levels of <130/80 mm Hg among patients who have initiated BP lowering therapy regardless of ASCVD risk,8 statin therapy for patients at high risk of developing ASCVD (defined as low-density lipoprotein cholesterol [LDL-C] ≥190 mg/dl, patients 40–75 years old with diabetes or have a 10-year ASCVD risk ≥7.5%),9 glycemic control defined as HbA1c of <7%,10 and not smoking. The EHR of large healthcare systems provides an opportunity to examine to what extent these recommended targets are achieved in a diverse patient population attending primary care.
We describe sex and racial/ethnic disparities in risk factor control among patients who have been diagnosed with hypertension without ASCVD. Results can be used to develop tailored interventions at the primary care level aimed at primary ASCVD prevention.
METHODS
Study population and data sources
The study sample was selected from EHR data of adult patients in a large integrated not-for-profit community-based healthcare system in the Midwestern United States over a 12-month period covering 1/1/2018 to 12/31/2018. Patients 18 years and older, with a hypertension diagnosis and who were prescribed at least 1 BP lowering medication and visited a primary care provider for BP management at one of 143 outpatient sites at least once in 2018 were included. Primary care providers were defined as family medicine, internal medicine, or geriatricians. Patients diagnosed with hypertension for less than 6 months were excluded as medications may be modified and titrated for newly diagnosed patients and BP values may vary accordingly. Hypertension diagnosis was based on the International Classification of Diseases, tenth Revision (ICD-10) codes (I10.x).11 Patients who were pregnant during their visit were excluded. Patients with preexisting chronic kidney disease or ASCVD, defined as acute coronary syndromes, myocardial infarction, stable or unstable angina, arterial revascularization, stroke, transient ischemic attack, or peripheral arterial disease of atherosclerotic origin, identified by ICD-10 codes were excluded (Appendix I online).12 Diabetes status was identified by ICD-10 code E11.x.
Race and ethnicity were identified from self-reported data in the EHR. Patients are asked to choose from a list of race options, including but not limited to Caucasian, African American, Asian, American Indian or Alaskan Native, Native Hawaiian or other Pacific Islander, unknown, or declined to answer. Among patients eligible for our analysis only 273 (5%) did not report race or reported races other than Caucasian or African American and were excluded. Patients were also asked to choose from a list of ethnicity options, including Hispanic/Latino or non-Hispanic/Latino. Race and ethnicity were combined, referred to hereon as race/ethnicity, and patients who reported to be Hispanic/Latino were categorized as Hispanic/Latino regardless of selected race.
ASCVD risk and risk factors
Ten-year ASCVD risk was calculated using the American College of Cardiology/American Heart Association (ACC/AHA) ASCVD pooled cohort risk equations.13 The equations do not specify Hispanic/Latino race/ethnicity category, therefore, these patients were grouped with the Caucasian category for purposes of calculating ASCVD risk as recommended in the literature.14 We report the most recent available value for systolic BP, diastolic BP, LCL-C, HbA1c, and reported smoking status. If more than 1 value was recorded on the same encounter, the lowest value is reported in these analyses. All patients had at least 1 systolic and 1 diastolic BP reading given that the sample was limited to patients with hypertension and prescribed at least 1 BP lowering medication. LDL-C values were available for all eligible patients. HbA1c values were not recorded for all patients in the sample and results are limited to records where these values were reported. BP lowering medications and statin therapy are reported based on prescriptions recorded in the EHR. Nonsmoking status reflects smoking data captured in the EHR.
ASCVD risk factor control
We used recommendations from clinical practice guidelines to determine the proportion of patients with uncontrolled risk factors. Results are presented separately for each risk factor. BP control was defined as a systolic/diastolic BP of <130/80 mm Hg for patients with confirmed hypertension who have initiated BP lowering therapy regardless of ASCVD risk based on ACC/AHA 2017 guidelines.8 In a sensitivity analysis, we report control of BP using earlier Eighth Joint National Committee guidelines.15 Controlled LDL-C levels were defined as LDL-C <100 mg/dl based Adult Treatment Panel III (ATP) recommendations.16 We also report appropriate statin therapy based on indication as recommended by ACC/AHA guidelines.9 These guidelines recommend moderate- or high-intensity statin therapy for patients with LDL-C ≥190 mg/dl or patients 40–75 years old with diabetes or with a 10-year ASCVD risk ≥7.5. We use these categorizations but expand the age limit to 40 years or older without limiting to 75 years. This is based on clarifications on the guideline suggesting continuing statin therapy if initiated before 75 years and the recommendation that for adults above 75, clinician and patient should engage in a discussion about the possible benefits of preventive therapies appropriate to the age group in the context of comorbidities and life expectancy.17 Patients without an indication for moderate- or high-dose statin were excluded from this target measure. We therefore report the proportion of patients on a statin among the subgroup of patients who are indicated for statin therapy.9 Control of HbA1c values were defined as a level <7.0% based on the American Diabetes Association’s 2020 standards of medical care in diabetes and were reported among patients with an HbA1c value.10 Evidence indicates that any level of smoking is harmful and increases the risk of ASCVD, therefore, we report the proportion of current smokers in the sample.
Statistical analysis
Patient characteristics are presented with means and SDs or medians and interquartile ranges as applicable for continuous variables, and as proportions and absolute numbers for categorical variables. Least square means were used to present age-adjusted means for systolic and diastolic BP, LDL-C levels, and HbA1c levels. The proportion of patients with controlled risk factors is presented and multivariable Poisson regressions were developed to explore associations between each target and sex and race/ethnicity. Model results are presented as adjusted relative risk (RR) and 95% confidence intervals (CIs). Models were adjusted for age, preferred language, diabetes, obesity, years of hypertension diagnosis, and insurance type. Analyses were completed using SAS statistical package (release 9.4; SAS Institute, Cary, NC).
RESULTS
Patient characteristics
A total of 15,990 adult patients with a hypertension for at least 6 months, and had an ambulatory encounter in 2018. After excluding patients who did not attend primary care, patients who are not taking any BP medications, patients with history of ASCVD and patients with CKD, we include 5,227 patients diagnosed with hypertension in our analysis who attended one of 143 primary care clinics in 2018 (Appendix I online). We intended to exclude patients with ASCVD and CKD as these patients may be managed for hypertension and other risk factors outside of primary care.
The analysis included 3,445 women (55.6% Caucasian, 34.5% African American, 10.0% Hispanic/Latino) and 1,782 men (65.0% Caucasian, 24.5% African American, 10.4% Hispanic/Latino). The mean age for women was 61.0 ± 13.5 years and 58.8 ± 13.1 years for men. Most patients were diagnosed with hypertension in the past 2 years (79.2% women and 80.9% men), 59.0% of women and 58.0% of men were obese, 30.3% of women and 32.2% of men were diagnosed with diabetes, 41.3% of women and 58.5% of men had an indication for statin therapy, and 9.3% of women and 13.7% of men reported being current smokers (Table 1).
Table 1.
Characteristics of patients diagnosed with hypertension and managed in primary care
| Women | Men | |||||||
|---|---|---|---|---|---|---|---|---|
| Caucasian | African American | Hispanic or Latino | Overall | Caucasian | African American | Hispanic or Latino | Overall | |
| N = 1,915 | N = 1,187 | N = 343 | N = 3,445 | N = 1,159 | N = 437 | N = 186 | N = 1,782 | |
| Age | 62.7 ± 13.3 | 58.3 ± 13.4 | 60.3 ± 13.0 | 61.0 ± 13.5 | 59.5 ± 13.1 | 58.5 ± 12.6 | 56.1 ± 14.0 | 58.8 ± 13.1 |
| HTN diagnosis <2 years | 1,517 (79.2%) | 873 (73.6%) | 276 (80.5%) | 2,727 (79.2%) | 941 (81.2%) | 341 (78.0%) | 160 (86.0%) | 1,442 (80.9%) |
| 2+ blood pressure lowering medications | 1,243 (64.9%) | 873 (73.6%) | 224 (65.3%) | 2,340 (67.9%) | 719 (62.0%) | 325 (74.4%) | 111 (58.7%) | 1,155 (64.8%) |
| Mean ASCVD risk score (SD) | 15.7 ± 19.6 | 14.0 ± 13.2 | 13.6 ± 17.3 | 14.9 ± 17.3 | 17.2 ± 15.8 | 19.9 ± 11.0 | 16.3 ± 15.8 | 17.8 ± 14.8 |
| Indicated for statin therapya | 709 (37.0%) | 557 (46.9%) | 156 (45.5%) | 1,422 (41.3%) | 605 (52.2%) | 325 (74.4%) | 112 (60.2%) | 1,042 (58.5%) |
| LDL-C >190 | 20 (1.0%) | 18 (1.5%) | 2 (0.6%) | 40 (1.2%) | 6 (0.5%) | 4 (0.9%) | 1 (0.5%) | 11 (0.6%) |
| Age ≥40 and diabetic | 410 (21.4%) | 341 (28.7%) | 117 (34.1%) | 868 (25.2%) | 273 (23.6%) | 133 (30.4%) | 78 (41.9%) | 484 (27.2%) |
| Age ≥40 and ASCVD score ≥7.5 | 540 (28.2%) | 484 (40.8%) | 102 (29.7%) | 1,126 (32.7%) | 539 (46.5%) | 320 (73.2%) | 96 (51.6%) | 955 (53.6%) |
| Current smokers | 195 (10.2%) | 106 (8.9%) | 19 (5.5%) | 320 (9.3%) | 156 (13.5%) | 69 (15.8%) | 17 (9.0%) | 242 (13.7%) |
| Obesity | 1,018 (53.2%) | 809 (68.2%) | 206 (60.1%) | 2,033 (59.0%) | 648 (55.9%) | 264 (60.4%) | 122 (65.6%) | 1,034 (58.0%) |
| Diabetes | 494 (25.8%) | 408 (34.4%) | 143 (41.7%) | 1,045 (30.3%) | 326 (28.1%) | 155 (35.5%) | 93 (50.0%) | 574 (32.2%) |
| Language, non-English | 42 (2.2%) | 2 (0.3%) | 104 (30.5%) | 149 (4.3%) | 20 (1.7%) | 2 (0.5%) | 53 (28.7%) | 75 (4.2%) |
| Insurance | ||||||||
| Commercial | 997 (52.1%) | 701 (59.2%) | 164 (47.8%) | 1,862 (54.1%) | 727 (63.0%) | 280 (64.1%) | 126 (67.7%) | 1,133 (63.8%) |
| Medicare | 763 (39.9%) | 309 (26.1%) | 105 (30.6%) | 1,177 (34.2%) | 352 (30.5%) | 112 (25.6%) | 38 (20.4%) | 502 (28.3%) |
| Medicaidb | 129 (6.7%) | 156 (13.2%) | 70 (20.4%) | 355 (10.3%) | 64 (5.6%) | 42 (9.6%) | 19 (10.2%) | 125 (7.0%) |
| Uninsured | 24 (1.3%) | 19 (1.6%) | 4 (1.2%) | 47 (1.4%) | 11 (1.0%) | 3 (0.7%) | 3 (1.6%) | 17 (1.0%) |
Abbreviations: ASCVD, atherosclerotic cardiovascular disease; HTN, hypertension; LDL-C, low-density lipoprotein cholesterol.
aPatients indicated for statin therapy included patients with LDL-C >190 and patients ages 40 and above who are diabetic or who have an ASCVD score ≥7.5, patients may fall into multiple categories.
bIncludes Medicaid, Medicaid/Medicare, and Other government programs.
ASCVD risk factors
Table 2 presents age-adjusted mean values for each risk factor by sex and race/ethnicity. Women and men diagnosed with hypertension, had BP readings with an age-adjusted mean of 131.0/78.0 and 132.0/79.0 mm Hg, respectively. BP values were highest among African American men at 135.2/81.3 mm Hg. Mean age-adjusted LDL-C values were 105.9 mg/dl among women and 99.7 mg/dl among men and were highest among African American women (107.1 mg/dl). HbA1c values were available for 1,351 (25.8%) patients. Mean HbA1c values among patients with diabetes were highest among Hispanic/Latino men (7.7%) and were well below 7.0% among patients without diabetes across all sex and race/ethnic categories.
Table 2.
Blood pressure, LDL, and HbA1c levels in patients with hypertension by sex and race
| SBP (mm Hg) | DBP (mm Hg) | LDL-C (ml/dl) | HbA1c (%), diabetic | HbA1c (%), nondiabetic | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | Age-adjusted mean (95% CI) | P value | N | Age-adjusted mean (95% CI) | P value | N | Age-adjusted mean (95% CI) | P value | N | Age-adjusted mean (95% CI) | P value | N | Age-adjusted mean (95% CI) | P value | |
| Overall | |||||||||||||||
| Women | 3,445 | 131 (130.4–131.5) |
Ref. | 3,445 | 78.0 (77.7–78.3) |
Ref. | 2,896 | 105.9 (104.7–107.1) |
Ref. | 598 | 7.2 (7.1–7.3) |
Ref. | 306 | 5.7 (5.6–5.8) |
Ref. |
| Men | 1,782 | 132 (131.3–132.8) |
0.02 | 1,782 | 79.0 (78.6–79.5) |
<0.01 | 1,508 | 99.7 (98.0–101.4) |
<0.01 | 308 | 7.4 (7.2–7.5) |
0.17 | 139 | 5.6 (5.5–5.7) |
0.12 |
| Women | |||||||||||||||
| Caucasian | 1,915 | 129.6 (128.9–130.3) |
Ref. | 1,915 | 77.2 (76.8–77.6) |
Ref. | 1,540 | 105.4 (103.8–107.1) |
Ref. | 260 | 7.0 (6.9–7.2) |
Ref. | 153 | 5.6 (5.6–5.7) |
Ref. |
| African American | 1,187 | 134 (133.1–134.9) |
<0.01 | 1,187 | 79.4 (78.9–79.9) |
<0.01 | 1,054 | 107.1 (105.1–109.1) |
0.22 | 258 | 7.2 (7.1–7.4) |
0.14 | 127 | 5.8 (5.5–5.9) |
0.03 |
| Hispanic or Latino | 343 | 128.5 (126.9–130.2) |
0.26 | 343 | 75.5 (74.5–76.4) |
<0.01 | 302 | 102.6 (98.8–106.3) |
0.17 | 80 | 7.4 (7.1–7.8) |
0.05 | 26 | 5.7 (5.5–5.9) |
0.41 |
| Men | |||||||||||||||
| Caucasian | 1,159 | 131.2 (130.3–132.0) |
Ref. | 1,159 | 78.8 (78.2–79.4) |
Ref. | 949 | 100.7 (98.5–102.9) |
Ref. | 169 | 7.2 (6.9–7.4) |
Ref. | 86 | 5.7 (5.5–5.8) |
Ref. |
| African American | 437 | 135.2 (133.7–136.6) |
<0.01 | 437 | 81.3 (80.4–82.3) |
<0.01 | 397 | 99.8 (96.5–103.2) |
0.67 | 90 | 7.5 (7.2–7.9) |
0.11 | 43 | 5.7 (4.9–5.5) |
0.84 |
| Hispanic or Latino | 186 | 129.5 (127.3–131.7) |
0.17 | 186 | 78.3 (76.9–79.7) |
0.54 | 162 | 96.9 (91.7–102.2) |
0.19 | 49 | 7.7 (7.3–8.2) |
0.05 | 10 | 5.2 (5.6–5.8) |
0.01 |
Abbreviations: CI, confidence interval; DBP, diastolic blood pressure; HbA1c, hemoglobin A1c; LDL-C, low-density lipoprotein cholesterol; Ref., reference; SBP, systolic blood pressure.
ASCVD risk factor control
BP control was assessed among the entire patient population with a hypertension diagnosis (n = 5,227), statin prescriptions were assessed among patients with indication for therapy, representing 47% of patients, HbA1c values were assessed among patients with an HbA1c value, representing 26% (n = 1,351) of patients. Overall, 55.8% of women and 60.0% of men had uncontrolled BP (see Appendix II online for proportion of patients with uncontrolled BP using JNC8 recommendations). 47.3% and 46.4% of women and men, respectively, with indication for statin therapy were not prescribed a statin, 34.9% women and 40.9% men had uncontrolled HbA1c values, and 9.3% of women and 13.7% of men reported being current smokers.
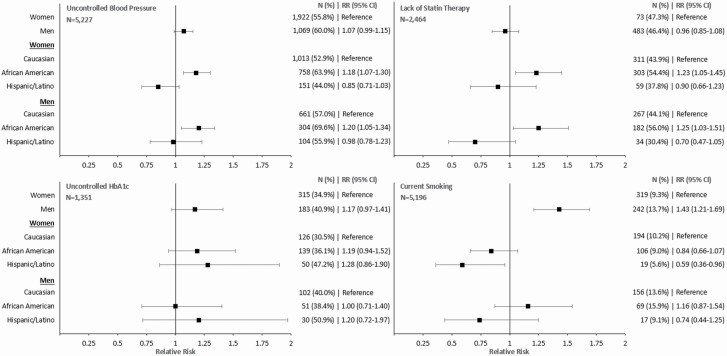
Figure 1 presents the proportion and RR for control of each risk factor by sex and race/ethnicity. In fully adjusted analyses, African American women and men with hypertension were 1.18 (95% CI 1.07–1.30) and 1.20 (95% CI 1.05–1.34) times more likely to have uncontrolled BP values compared with Caucasian women and men, respectively. African American women and men with hypertension and a statin therapy indication were 1.23 (95% CI 1.05–1.45) and 1.25 (95% CI 1.03–1.51) times more likely lack a statin prescription compared with Caucasian women and men. There was no evidence of disparities among Hispanic/Latino patients in BP control and statin prescriptions. Although not statistically significant, there was a trend for worse HbA1c control among African American women compared with Caucasian women (RR 1.19, 95% CI 0.94–1.52) and among Hispanic women (RR 1.28, 95% CI 0.86–1.90) and men (RR 1.20, 95% CI 0.72–1.97) compared with Caucasian women and men. Hispanic/Latino women were 0.59 (95% CI 0.36–0.96) times less likely to report being current smokers than Caucasian women. There was no evidence of disparities among African Americans men and women or Hispanic/Latino men in reported smoking status.
Figure 1.
Proportion and relative risk of uncontrolled blood pressure, lack of statin prescription, uncontrolled HbA1c, and current smoking targets in patients with hypertension, by sex and race/ethnicity. Uncontrolled blood pressure: ≥130/80 mm Hg; lack of statin therapy: lack of medium- or high-dose statin therapy among patients with indication (LDL-C >190 or patients ages 40 or more who have diabetes or have a 10-year ASCVD score ≥7.5; glycemic control: uncontrolled HbA1c: ≥7%, and current smoking. Models presented by sex are adjusted for: race, age, language, years of diagnosis, obesity, and insurance. Models presented by sex and race are adjusted for: age, language, years of diagnosis, obesity, and insurance. Abbreviations: ASCVD, atherosclerotic cardiovascular disease; HbA1c, hemoglobin A1c; LDL-C, low-density lipoprotein cholesterol.
DISCUSSION
We observed differences in ASCVD risk factor control by sex and racial/ethnic groups in this sample of patients diagnosed and managed for hypertension in primary care. Results indicate poorer control in risk factors among African Americans, which is consistent with higher prevalence of ASCVD in this racial group. African American men and women were more likely to have uncontrolled BP values and lack a statin prescription if indicated for statin therapy compared with their Caucasian counterpart. These gaps persisted after adjusting for multiple confounders. Hispanic/Latino men and women were less likely to achieve HbA1c control compared with their Caucasian counterpart, although differences were not statistically significant likely due to the fewer number of Hispanic/Latino patients with HbA1c values in our analysis.
There are several potential explanations for the observed racial/ethnic disparities. These include access to primary care,18 in terms of how often patients follow up with their primary care providers,19 access to specialty care when patient risk factors were poorly controlled in the primary care setting,20 underlying social determinants of health,21 as well as how adherent they are to BP lowering medications.22 The literature suggests that African American men are less likely to follow up with providers regularly compared with African American women.23 Moreover, clinical bias and variations in the clinical management of patients with sex and racial/ethnic differences were not explored at the individual provider or practice level and may warrant further investigation. Other explanations include variations in treatment intensification.15 Our analysis indicates that the proportion of patients receiving at least 2 BP lowering medications is higher among African American men and women compared with other races. Other treatment patterns such as type of BP lowering medication and time to intensification were not explored and warrant further analysis.
Overall, Hispanic/Latino men and women were more likely to have controlled risk factors while African American men and women were less likely to have controlled risk factors compared with Caucasians. An exception was HbA1c control; although not statistically significant, Hispanic/Latino women were less likely to have controlled HbA1c values. Further, the prevalence of diabetes was higher among Hispanic/Latino men and women compared with other races which is consistent with the literature for the general Hispanic/Latino population.24,25
It is important to note that over half of the patients in this sample did not have controlled BP values based on ACC/AHA 2017 guidelines, despite having a hypertension diagnosis and having visited a primary care clinic at least once in the past year. Similarly, close to half of the patients, who are indicated for statin therapy were not prescribed a statin. These results indicate a lag between clinical practice guidelines and clinical practice.26 This may be due to provider’s lack of agreement with the guidelines, lack of knowledge, or clinical inertia.27 This gap may also be due to feasibility of implementing these guidelines in a clinical setting. For example, appropriate statin prescription based on AHA/ACC practice guidelines requires calculating ASCVD which may not be feasible and limits its widespread utility and adoption. Our sample was restricted to patients with hypertension and explored adherence to the updated ACC/AHA 2017 guidelines on BP control, which were issued 1 year prior to the study period (2018). In concordance with the literature, we show that adherence to these guidelines in community primary care settings is low.28 More research is warranted in future years to evaluate adhering to these guidelines more closely.
Our analysis has several notable enhancements from prior literature. While other studies have focused on disparities in BP control, we were able to include data on other ASCVD risk factors that tend to aggregate in this patient population.29 The literature focuses on racial/ethnic disparities among patients with established ASCVD. Conversely, we evaluated patients at risk of ASCVD who had not yet developed the disease. We have demonstrated that disparities exist in primary care and that interventions should start upstream rather than after the disease is established.30 Additionally, we evaluated disparities using the latest clinical practice guidelines for BP and statin therapy as well as earlier guidelines. We observed that disparities persist while using the previous practice guidelines. Further, we aggregated a large sample size from 143 primary care clinics in both an urban and suburban setting which is larger than many other studies exploring disparities in primary care. Finally, our results are based on EHR data for diagnoses, prescriptions, and BP and lab measurements, rather than relying on self-reporting.
Our study has several limitations. Our analysis included patients with at least 1 visit to the healthcare system and therefore is not restricted to those who receive continuous care at this healthcare system. Therefore, information on risk factor control based on measurements outside of the healthcare system are not accounted for. Similarly, details on medications prescribed at another healthcare system are not available. Information on medication was limited to prescriptions and did not cover actual use or adherence which may partially explain lack of ASCVD risk factor control. We did not have data on lifestyle health behaviors which may be influenced by sex and race/ethnicity explaining some of the disparities observed. We included patients who manage their hypertension with a primary care provider. Information on whether these patients also see a specialist was not available. Although we were able to include a diverse patient population to evaluate difference in risk factor control, the Hispanic/Latino patient population was small which prevented conducting further analyses especially regarding HbA1c. We defined lack of BP control using the last available BP measurement, where guidelines usually recommend evaluating the 2 most recent measurements. Finally, our patient population is limited to patients with hypertension who have visited a primary care provider at least once during the 1-year study period. These patients may not be representative of the general US population.
Our results have implications for developing interventions to control hypertension and other risk factors to prevent ASCVD in primary care settings of large healthcare systems serving a diverse patient population. Several effective interventions exist to improve risk factor control in racial and ethnic minorities. For example, the combination of health promotion by barbers and medication management in barbershops by specialty-trained pharmacists appears to be effective in controlling BP among African American men.31,32 Culturally tailored education and peer support interventions show effectiveness in HbA1c control among African Americans and Latino/Hispanics.33 These types of interventions require further understanding of how they can be implemented on a broader scale. More recently, health information technology interventions such as mobile apps have been explored to improve risk factor control. High-quality evidence of their effectiveness is limited and effectiveness in reducing disparities has not been well explored.34,35
In conclusion, barriers to reducing disparities in ASCVD risk factor control are complex and require intervening at the patient level, provider level, regional geographic level, and healthcare system level.27,36 Interventions need to be multidisciplinary to evaluate and target multiple barriers. Continued monitoring of progress across sex, racial, and ethnic groups at the healthcare system level is also important to ensure effectiveness of interventions as well as preventing the development of further disparities.
FUNDING
Research reported in this publication was supported in part by the NIH National Institute On Minority Health And Health Disparities (R01MD014874).
DISCLOSURE
The authors declared no conflict of interest.
Supplementary Material
REFERENCES
- 1. World Health Organization. Cardiovascular Diseases (CVDs) Key Facts. 2017. https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds). [Google Scholar]
- 2. Mons U, Müezzinler A, Gellert C, Schöttker B, Abnet CC, Bobak M, de Groot L, Freedman ND, Jansen E, Kee F, Kromhout D, Kuulasmaa K, Laatikainen T, O’Doherty MG, Bueno-de-Mesquita B, Orfanos P, Peters A, van der Schouw YT, Wilsgaard T, Wolk A, Trichopoulou A, Boffetta P, Brenner H; CHANCES Consortium . Impact of smoking and smoking cessation on cardiovascular events and mortality among older adults: meta-analysis of individual participant data from prospective cohort studies of the CHANCES consortium. BMJ 2015; 350:h1551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Brunström M, Carlberg B. Association of blood pressure lowering with mortality and cardiovascular disease across blood pressure levels: a systematic review and meta-analysis. JAMA Intern Med 2018; 178:28–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Giugliano D, Maiorino MI, Bellastella G, Chiodini P, Esposito K. Glycemic control, preexisting cardiovascular disease, and risk of major cardiovascular events in patients with type 2 diabetes mellitus: systematic review with meta-analysis of cardiovascular outcome trials and intensive glucose control trials. J Am Heart Assoc 2019; 8:e012356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Zhang XL, Lan RF, Zhang XW, Xu W, Wang L, Kang LN, Xu B. Association between baseline, achieved, and reduction of CRP and cardiovascular outcomes after LDL cholesterol lowering with statins or ezetimibe: a systematic review and meta-analysis. J Am Heart Assoc 2019; 8:e012428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. GBD 2013 Mortality and Causes of Death Collaborators. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015; 385:117–171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Pool LR, Ning H, Lloyd-Jones DM, Allen NB. Trends in racial/ethnic disparities in cardiovascular health among US adults from 1999–2012. J Am Heart Assoc 2017; 6:e006027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, DePalma SM, Gidding S, Jamerson KA, Jones DW, MacLaughlin EJ, Muntner P, Ovbiagele B, Smith SC Jr, Spencer CC, Stafford RS, Taler SJ, Thomas RJ, Williams KA Sr, Williamson JD, Wright JT Jr. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 2018; 138:e484–e594. [DOI] [PubMed] [Google Scholar]
- 9. Grundy SM, Stone NJ, Bailey AL, Beam C, Birtcher KK, Blumenthal RS, Braun LT, de Ferranti S, Faiella-Tommasino J, Forman DE, Goldberg R, Heidenreich PA, Hlatky MA, Jones DW, Lloyd-Jones D, Lopez-Pajares N, Ndumele CE, Orringer CE, Peralta CA, Saseen JJ, Smith SC Jr, Sperling L, Virani SS, Yeboah J. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the management of blood cholesterol: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol 2019; 73:e285–e350. [DOI] [PubMed] [Google Scholar]
- 10. American Diabetes Association. 6. Glycemic targets: standards of medical care in diabetes-2020. Diabetes Care 2020; 43:S66–S76. [DOI] [PubMed] [Google Scholar]
- 11. Shuey MM, Gandelman JS, Chung CP, Nian H, Yu C, Denny JC, Brown NJ. Characteristics and treatment of African-American and European-American patients with resistant hypertension identified using the electronic health record in an academic health centre: a case-control study. BMJ Open 2018; 8:e021640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Arnett DK, Khera A, Blumenthal RS. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: part 1, lifestyle and behavioral factors. JAMA Cardiol 2019; 4:1043–1044. [DOI] [PubMed] [Google Scholar]
- 13. Muntner P, Colantonio LD, Cushman M, Goff DC Jr, Howard G, Howard VJ, Kissela B, Levitan EB, Lloyd-Jones DM, Safford MM. Validation of the atherosclerotic cardiovascular disease Pooled Cohort risk equations. JAMA 2014; 311:1406–1415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Goff DC Jr, Lloyd-Jones DM, Bennett G, Coady S, D’Agostino RB, Gibbons R, Greenland P, Lackland DT, Levy D, O’Donnell CJ, Robinson JG, Schwartz JS, Shero ST, Smith SC Jr, Sorlie P, Stone NJ, Wilson PW, Jordan HS, Nevo L, Wnek J, Anderson JL, Halperin JL, Albert NM, Bozkurt B, Brindis RG, Curtis LH, DeMets D, Hochman JS, Kovacs RJ, Ohman EM, Pressler SJ, Sellke FW, Shen WK, Smith SC Jr, Tomaselli GF; American College of Cardiology/American Heart Association Task Force on Practice Guidelines . 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 2014; 129:S49–S73. [DOI] [PubMed] [Google Scholar]
- 15. James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, Lackland DT, LeFevre ML, MacKenzie TD, Ogedegbe O, Smith SC Jr, Svetkey LP, Taler SJ, Townsend RR, Wright JT Jr, Narva AS, Ortiz E. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA 2014; 311:507–520. [DOI] [PubMed] [Google Scholar]
- 16. National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III) final report. Circulation 2002; 106:3143–3421. [PubMed] [Google Scholar]
- 17. Arnett DK, Blumenthal RS, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ, Himmelfarb CD, Khera A, Lloyd-Jones D, McEvoy JW, Michos ED. ACC/AHA guideline on the primary prevention of cardiovascular disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol 2019; 74:e177–e232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Manuel JI. Racial/ethnic and gender disparities in health care use and access. Health Serv Res 2018; 53:1407–1429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Bardach NS, Doupnik SK, Rodean J, Zima BT, Gay JC, Nash C, Tanguturi Y, Coker TR. ED visits and readmissions after follow-up for mental health hospitalization. Pediatrics 2020; 145:e20192872. [DOI] [PubMed] [Google Scholar]
- 20. Bellinger JD, Hassan RM, Rivers PA, Cheng Q, Williams E, Glover SH. Specialty care use in US patients with chronic diseases. Int J Environ Res Public Health 2010; 7:975–990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Braveman PA, Cubbin C, Egerter S, Williams DR, Pamuk E. Socioeconomic disparities in health in the United States: what the patterns tell us. Am J Public Health 2010; 100(Suppl 1):S186–S196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Ritchey M, Chang A, Powers C, Loustalot F, Schieb L, Ketcham M, Durthaler J, Hong Y. Vital signs: disparities in antihypertensive medication nonadherence among Medicare part D beneficiaries—United States, 2014. MMWR Morb Mortal Wkly Rep 2016; 65:967–976. [DOI] [PubMed] [Google Scholar]
- 23. Kotchen JM, Shakoor-Abdullah B, Walker WE, Chelius TH, Hoffmann RG, Kotchen TA. Hypertension control and access to medical care in the inner city. Am J Public Health 1998; 88:1696–1699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Center for Disease Control and Precention. National Center for Health Statistics. Table A-4a. Age-Adjusted Percentages (With Standard Errors) of Selected Diseases and Conditions Among Adults Aged 18 and Over, by Selected Characteristics: United States, National Health Interview Survey, 2018. https://ftp.cdc.gov/pub/Health_Statistics/NCHS/NHIS/SHS/2018_SHS_Table_A-4.pdf. [Google Scholar]
- 25. CDC. Hispanic/Latino Americans and Type 2 Diabetes. 2019. https://www.cdc.gov/diabetes/library/features/hispanic-diabetes.html. [Google Scholar]
- 26. Cabana MD, Rand CS, Powe NR, Wu AW, Wilson MH, Abboud PA, Rubin HR. Why don’t physicians follow clinical practice guidelines? A framework for improvement. JAMA 1999; 282:1458–1465. [DOI] [PubMed] [Google Scholar]
- 27. Khatib R, Schwalm JD, Yusuf S, Haynes RB, McKee M, Khan M, Nieuwlaat R. Patient and healthcare provider barriers to hypertension awareness, treatment and follow up: a systematic review and meta-analysis of qualitative and quantitative studies. PLoS One 2014; 9:e84238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Al Kibria GM. Racial/ethnic disparities in prevalence, treatment, and control of hypertension among US adults following application of the 2017 American College of Cardiology/American Heart Association guideline. Prev Med Rep 2019; 14:100850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Sripipatana A, Pourat N, Chen X, Zhou W, Lu C. Exploring racial/ethnic disparities in hypertension care among patients served by health centers in the United States. J Clin Hypertens (Greenwich) 2019; 21:489–498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, Das SR, de Ferranti S, Després JP, Fullerton HJ, Howard VJ, Huffman MD, Isasi CR, Jiménez MC, Judd SE, Kissela BM, Lichtman JH, Lisabeth LD, Liu S, Mackey RH, Magid DJ, McGuire DK, Mohler ER III, Moy CS, Muntner P, Mussolino ME, Nasir K, Neumar RW, Nichol G, Palaniappan L, Pandey DK, Reeves MJ, Rodriguez CJ, Rosamond W, Sorlie PD, Stein J, Towfighi A, Turan TN, Virani SS, Woo D, Yeh RW, Turner MB; Writing Group Members; American Heart Association Statistics Committee; Stroke Statistics Subcommittee . Heart disease and stroke statistics-2016 update: a report from the American Heart Association. Circulation 2016; 133:e38–360. [DOI] [PubMed] [Google Scholar]
- 31. Victor RG, Lynch K, Li N, Blyler C, Muhammad E, Handler J, Brettler J, Rashid M, Hsu B, Foxx-Drew D, Moy N, Reid AE, Elashoff RM. A cluster-randomized trial of blood-pressure reduction in black barbershops. N Engl J Med 2018; 378:1291–1301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Victor RG, Blyler CA, Li N, Lynch K, Moy NB, Rashid M, Chang LC, Handler J, Brettler J, Rader F, Elashoff RM. Sustainability of blood pressure reduction in black barbershops. Circulation 2019; 139:10–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Peek ME, Cargill A, Huang ES. Diabetes health disparities: a systematic review of health care interventions. Med Care Res Rev 2007; 64:101S–156S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Thangada ND, Garg N, Pandey A, Kumar N. The emerging role of mobile-health applications in the management of hypertension. Curr Cardiol Rep 2018; 20:78. [DOI] [PubMed] [Google Scholar]
- 35. Persell SD, Peprah YA, Lipiszko D, Lee JY, Li JJ, Ciolino JD, Karmali KN, Sato H. Effect of home blood pressure monitoring via a smartphone hypertension coaching application or tracking application on adults with uncontrolled hypertension: a randomized clinical trial. JAMA Netw Open 2020; 3:e200255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Mueller M, Purnell TS, Mensah GA, Cooper LA. Reducing racial and ethnic disparities in hypertension prevention and control: what will it take to translate research into practice and policy? Am J Hypertens 2015; 28:699–716. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.