Abstract
Background
Hypertension is a major cause of morbidity and mortality. In community populations the prevalence of hypertension, both in diagnosed and undiagnosed states, has been widely reported. However, estimates for the prevalence of hospitalized patients with average blood pressures (BPs) that meet criteria for the diagnosis of hypertension are lacking. We aimed to estimate the prevalence of patients in a UK hospital setting, whose average BPs meet current international guidelines for hypertension diagnosis.
Methods
We performed a retrospective cross-sectional observational study of patients admitted to adult wards in 4 acute hospitals in Oxford, United Kingdom, between March 2014 and April 2018.
Results
We identified 41,455 eligible admitted patients with a total of 1.7 million BP measurements recorded during their hospital admissions. According to European ESC/ESH diagnostic criteria for hypertension, 21.4% (respectively 47% according to American ACC/AHA diagnostic criteria) of patients had a mean BP exceeding the diagnostic threshold for either Stage 1, 2, or 3 hypertension. Similarly, 5% had a mean BP exceeding the ESC/ESH (respectively 13% had a mean BP exceeding the ACC/AHA) diagnostic criteria for hypertension, but no preexisting diagnostic code for hypertension or a prescribed antihypertensive medication during their hospital stay.
Conclusions
Large numbers of hospital inpatients have mean in-hospital BPs exceeding diagnostic thresholds for hypertension, with no evidence of diagnosis or treatment in the electronic record. Whether opportunistic screening for in-hospital high BP is a useful way of detecting people with undiagnosed hypertension needs evaluation.
Keywords: blood pressure, hospital measurements, hypertension, undiagnosed hypertension
BACKGROUND
Hypertension is a major cause of morbidity and mortality.1 Early detection and management of hypertension is key to preventing end-organ damage.2 However, in the early stages, hypertension is usually asymptomatic. In the UK healthcare setting, hypertension is typically identified either opportunistically or through the National Health Service (NHS) Health Check in primary care.3,4 However, only half of those invited attend these health checks5 and 12% of the English adult population have undiagnosed hypertension.6 Internationally, hypertension awareness varies widely from 40% to 80% among high-income nations, with awareness and treatment rates of younger people being lower than older age groups.7 Furthermore, the Global Burden of Disease Study of 2013 estimated hypertension causes over 10 million deaths worldwide annually.8 Therefore, current approaches to identifying people with hypertension are not adequate and innovative approaches need to be considered to improve the detection of hypertension.
The inpatient hospital setting, in which multiple blood pressure (BP) measurements are performed for each admitted patient may provide an opportunity to detect people with undiagnosed hypertension. However, research in this field has so far, focused on the prevalence of hypertension in the emergency department setting and has largely excluded patients admitted to hospital.9
OBJECTIVES
The primary objective of this study is to estimate the prevalence of hypertension and undiagnosed hypertension in a UK hospital inpatient setting using a large hospital database of 1.7 million BP measurements. We also identify patient characteristics of those who appear to be at greatest risk of undiagnosed hypertension.
METHODS
Study design
This study is a retrospective cross-sectional analysis of in-hospital BP for adult hospital patients meeting the eligibility criteria described below.
Study setting
Patients were admitted between March 2014 and April 2018 to adult wards in 3 tertiary and 1 secondary referral centers in the Oxford University Hospitals NHS Foundation Trust, United Kingdom.
Participants
We included patients from all adult wards, with the exception of the maternity and intensive care units, of the 4 acute hospitals in the Oxford University Hospitals (OUH) NHS Foundation Trust. We included the first admission of each patient during which at least 3 BP measurements were recorded, with at least 1 being recorded during the nighttime (midnight to 5:59 am) and at least 1 recorded during the daytime (10:00 am to 7:59 pm), with 2 of these observations being at least 24 hours apart. Hospital day and night periods were defined in accordance with standard practice in the literature.10
Data sources
Patients had their vital observations, including heart rate and systolic and diastolic BP recorded using the System for Electronic Notification and Documentation (SEND). SEND is a software application that links vital sign monitoring devices including BP monitors, with a tablet computer for the manual recording of vital signs in patients.11 All vital-sign equipment used within the study was purchased and maintained (including regular calibration) in accordance with the Oxford University Hospitals NHS Foundation Trust Medical Devices Management Policy. Other data (date of birth, sex, ICD-10 codes and prescription information) were obtained from the Patient Administration System (PAS) in the hospitals’ electronic patient record (EPR) system, Cerner Millennium (https://www.cerner.com/, North Kansas City, MO).
Sample size
We examined all patients aged 16 years and over who were admitted between March 2014 and April 2018 with observations recorded electronically using the SEND system for eligibility.
Quantitative variables
Each patient’s BP data were averaged by hour of the day over their whole admission period, such that each individual only contributed averaged data for a maximum of 24 individual hourly periods. The computational details of this procedure have been described in our previous article.12
Classification of inpatients meeting clinic and ambulatory (daytime, nighttime, and 24 hours) hypertension diagnostic thresholds were made according to published guidelines for hypertension diagnosis and management from Europe (ESC/ESH guidelines of 201813) and America (ACC/AHA guidelines of 201714). The definitions of the corresponding hypertension diagnostic thresholds can be found in Supplementary Tables ST-1 and ST-2 online.
Undiagnosed hypertension was defined as having a mean BP above the diagnostic thresholds and no previous ICD-10 codes for hypertension (Supplementary Table ST-4 online) nor any of the prescribed antihypertensive medications listed by British National Formulary (Supplementary Table ST-3 online).15
In line with published diagnostic criteria, we define patients meeting the criteria for isolated nocturnal hypertension as elevated nighttime BP (average nighttime systolic BP ≥120 or diastolic BP ≥70) in the presence of normal daytime BP (average daytime systolic BP <135 and diastolic BP <85). As a proxy for the ambulatory BP monitoring, we applied these diagnostic criteria to patients’ 24-hour BP signature as explained above.
We investigated the prevalence of elevated BP in predefined patient subgroups according to (i) sex as recorded in the EPR, (ii) age, (iii) elective vs. emergency admission, and (iv) medical vs. surgical admission. We classified patients according to whether their electronic record did not contain previous ICD-10 codes for hypertension (Supplementary Table ST-8 online) or record of the antihypertensive drugs listed by British National Formulary15 (Supplementary Table ST-7 online).
RESULTS
Descriptive data
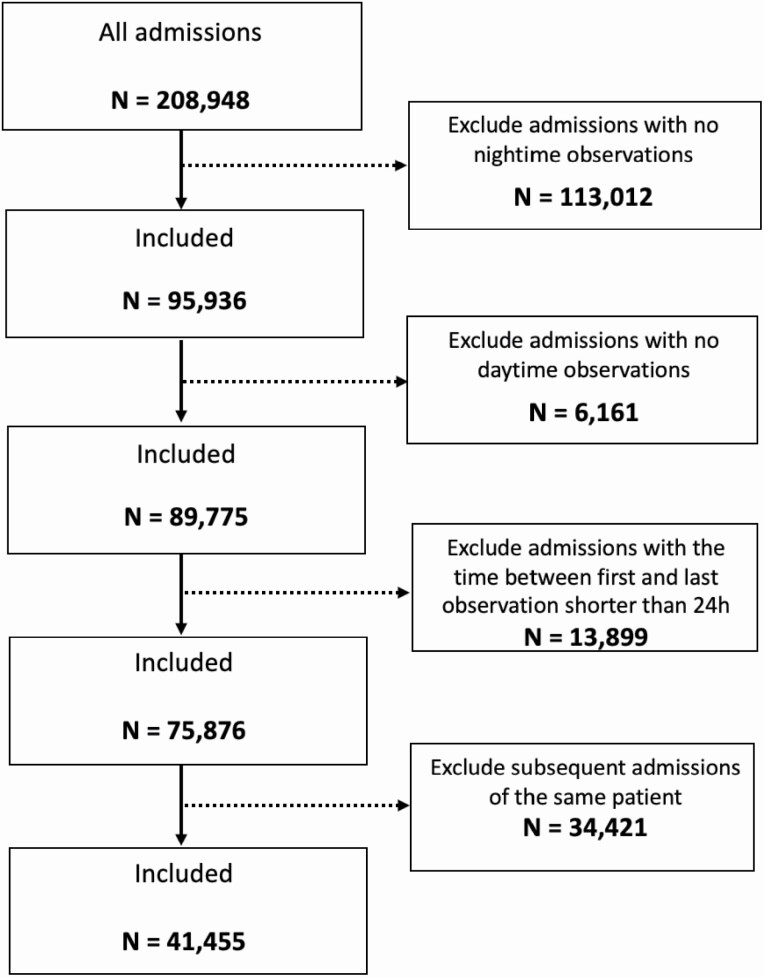
Between March 2014 and April 2018, 208,948 patients 16 years of age and over were admitted to Oxford University Hospitals NHS Foundation Trust and had their BP recorded using the SEND system. After excluding patients with no nighttime observations (113,012), those with no daytime observation (6,161), those in whom the time between first and last observation was less than 24 hours (13,899), and any subsequent admissions of the same patient (34,421), 41,455 patients were eligible for inclusion in the study (see Figure 1 for an inclusion/exclusion criteria flowchart). A total of 1,701,812 BP measurements were recorded for these patients. Patient demographics are shown in Table 1. Mean patient age was 64 years (SD 19) and 51% were female. Median length of stay was 4.7 days (interquartile range 7.4) and 63% were admitted as an emergency, whilst 33% were admitted electively and 4% classified as “other” (e.g., transfer from other hospital provider other than in an emergency).
Figure 1.
Inclusion/exclusion criteria flowchart.
Table 1.
Patient demographics
| Patients | Age | LOS | Number of BP measurements | SBP | DBP | |
|---|---|---|---|---|---|---|
| Percentage of total | Mean (SD) | Median (IQR) | Median (IQR) | Mean (SD) | Mean (SD) | |
| All | 41,455 (100%) | 64 (19) | 4.7 (7.4) | 27 (34) | 127 (16) | 69 (9) |
| Sex | ||||||
| Men | 20,169 (49%) | 64 (19) | 4.9 (7.5) | 28 (34) | 128 (15) | 70 (9) |
| Women | 21,286 (51%) | 65 (20) | 4.6 (7.2) | 26 (33) | 126 (17) | 67 (9) |
| Age groups | ||||||
| 18–29 | 2,833 (7%) | 24 (4) | 2.8 (3.9) | 17 (19) | 118 (12) | 66 (8) |
| 30–39 | 2,722 (7%) | 35 (3) | 3.2 (4.5) | 19 (23) | 119 (14) | 69 (9) |
| 40–49 | 3,714 (9%) | 45 (3) | 3.6 (5.1) | 22 (26) | 122 (14) | 71 (10) |
| 50–59 | 5,674 (14%) | 55 (3) | 4.1 (5.8) | 25 (28) | 125 (15) | 71 (9) |
| 60–69 | 7,071 (17%) | 65 (3) | 4.5 (6.4) | 27 (32) | 127 (15) | 69 (9) |
| 70–79 | 8,680 (21%) | 74 (3) | 5.2 (7.9) | 30 (35) | 130 (16) | 68 (8) |
| 80–89 | 7,861 (19%) | 84 (3) | 6.8 (10.9) | 34 (44) | 132 (17) | 68 (9) |
| 90+ | 2,714 (7%) | 91 (1) | 7.5 (12) | 34 (45) | 133 (18) | 68 (9) |
| NHS Admission Method | ||||||
| Emergency | 26,290 (63%) | 66 (21) | 5.1 (8.9) | 26 (37) | 125 (14) | 67 (8) |
| Elective | 13,490 (33%) | 61 (17) | 3.9 (4.7) | 27 (26) | 128 (17) | 69 (9) |
| Other | 1,675 (4%) | 64 (18) | 9.8 (11.9) | 46 (48) | 126 (16) | 68 (9) |
| NHS Specialty | ||||||
| Medical | 18,113 (44%) | 69 (19) | 4.9 (8.9) | 25 (36) | 127 (18) | 69 (10) |
| Surgical | 22,543 (54%) | 60 (19) | 4.6 (6.3) | 28 (31) | 127 (15) | 68 (8) |
| Other | 792 (2%) | 66 (15) | 5.5 (9.8) | 27 (41) | 125 (16) | 68 (9) |
Abbreviations: BP, blood pressure; DBP, diastolic BP; IQR, interquartile range; LOS, length of stay; SBP, systolic BP. “Other” in NHS Admission Method refers to any admission method, that is not Emergency or Elective (e.g., maternity admissions or transfer from other hospital provider other than in an emergency); “other” in NHS Specialty refers to any specialty that is not Medical or Surgical.
Prevalence of patients meeting criteria for hypertension
According to the European ESC/ESH diagnostic criteria for clinical hypertension, 18% patients had a mean BP equal to or greater than the diagnostic thresholds for Stage 1 hypertension, 3% had a mean BP equal to or greater than the diagnostic thresholds for Stage 2 hypertension, and 0.4% equal to or greater than the thresholds for Stage 3 hypertension (Table 2). Using the (lower) American ACC/AHA guidelines, the proportions of patients meeting the diagnostic thresholds for Stage 1, 2, and 3 hypertension were 26%, 18%, and 3%, respectively (Table 2). The prevalence of patients meeting the criteria for isolated nighttime hypertension was 39% according to ESC/ESH (45% according to ACC/AHA) guidelines. The prevalence of those meeting criteria for isolated systolic hypertension according to ESC/ESH thresholds was 19% (31% according to ACC/AHA thresholds). The prevalence for isolated diastolic and daytime hypertension was low (Supplementary Table ST-5 online). The prevalence of patients meeting the Ambulatory Blood Pressure Monitoring (ABPM) for daytime, nighttime, and 24-hour diagnostic thresholds (Supplementary Table ST-2 online) is stratified further by sex, age groups, NHS admission method, and NHS specialty and presented in Table 3.
Table 2.
Estimated prevalence of “clinic” hypertension
| Patients | Age | LOS | Number of BP measurements | |
|---|---|---|---|---|
| % of total | Mean (SD) | Median (IQR) | Median (IQR) | |
| Hypertension category (ESC/ESH) | ||||
| Normotensive | 32,788 (79%) | 62 (20) | 5 (7) | 27 (34) |
| Stage 1 | 7,504 (18%) | 72 (15) | 5 (8) | 27 (35) |
| Stage 2 | 1,297 (3%) | 74 (15) | 4 (6) | 23 (29) |
| Stage 3 | 144 (0.4%) | 72 (18) | 2 (3) | 19 (15) |
| Hypertension category (ACC/AHA) | ||||
| Normotensive | 24,158 (58%) | 60 (20) | 5 (7) | 27 (34) |
| Stage 1 | 10,858 (26%) | 68 (17) | 5 (8) | 27 (34) |
| Stage 2 | 7,504 (18%) | 72 (15) | 5 (8) | 28 (35) |
| Stage 3 | 1,417 (3%) | 74 (15) | 4 (6) | 23 (28) |
Estimated prevalence (%) of patients meeting the criteria for clinical hypertension stratified by stages of hypertension together with the corresponding mean age (years), median length of stay (days), median number of blood pressure observations according to European ESC/ESH and American ACC/AHA guidelines (Supplementary Table ST-1 online). Abbreviations: BP, blood pressure; IQR, interquartile range; LOS, length of stay.
Table 3.
Estimated ABPM daytime, ABPM nighttime, and ABPM 24-hour hypertension
| ESC/ESH | ACC/AHA | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ABPM | Daytime | Nighttime | 24 hours | Daytime | Nighttime | 24 hours | ||||||
| SBP/DBP ≥ | 135/85 | 120/70 | 130/80 | 130/80 | 110/65 | 125/75 | ||||||
| M | F | M | F | M | F | M | F | M | F | M | F | |
| Overall | 29 | 28 | 73 | 65 | 43 | 40 | 42 | 38 | 95 | 90 | 59 | 53 |
| Age groups | ||||||||||||
| 18–29 | 15 | 4 | 55 | 31 | 23 | 8 | 28 | 10 | 93 | 79 | 44 | 17 |
| 30–39 | 20 | 8 | 65 | 36 | 30 | 12 | 33 | 13 | 95 | 81 | 48 | 21 |
| 40–49 | 26 | 15 | 74 | 47 | 37 | 20 | 39 | 22 | 97 | 87 | 55 | 33 |
| 50–59 | 29 | 22 | 76 | 59 | 43 | 31 | 43 | 33 | 97 | 91 | 60 | 45 |
| 60–69 | 31 | 29 | 74 | 66 | 45 | 41 | 44 | 40 | 97 | 91 | 60 | 55 |
| 70–79 | 31 | 35 | 76 | 74 | 47 | 50 | 43 | 47 | 96 | 92 | 62 | 64 |
| 80–89 | 34 | 39 | 76 | 80 | 51 | 58 | 46 | 51 | 94 | 95 | 64 | 70 |
| 90+ | 31 | 41 | 77 | 82 | 49 | 61 | 43 | 52 | 94 | 95 | 62 | 72 |
| NHS Admission method | ||||||||||||
| Elective | 26 | 22 | 71 | 55 | 41 | 32 | 40 | 32 | 96 | 87 | 57 | 45 |
| Emergency | 30 | 31 | 74 | 70 | 45 | 45 | 43 | 41 | 95 | 92 | 60 | 57 |
| Other | 26 | 29 | 70 | 65 | 40 | 41 | 38 | 38 | 94 | 91 | 56 | 51 |
| NHS Specialty | ||||||||||||
| Medical | 29 | 31 | 72 | 69 | 43 | 45 | 40 | 41 | 94 | 91 | 57 | 56 |
| Surgical | 29 | 25 | 74 | 61 | 43 | 37 | 43 | 35 | 96 | 90 | 60 | 50 |
| Other | 28 | 23 | 72 | 60 | 41 | 36 | 40 | 34 | 95 | 88 | 54 | 49 |
Estimated prevalence (%) of patients meeting the criteria for “clinic,” daytime, nighttime, and 24-hour hypertension stratified by sex, age groups, NHS Admission Method, and NHS Specialty according to the European ESC/ESH and American ACC/AHA guidelines (Supplementary Table ST-2 online). Abbreviations: DBP, diastolic blood pressure; F, female; M, male; SBP, systolic blood pressure. Daytime SBP (DBP) is the mean systolic (diastolic) blood pressure measurements taken during daytime hours (10:00 am to 7:59 pm). Nighttime SBP (DBP) is the mean systolic (diastolic) blood pressure measurements taken during night hours (midnight to 5:59 am).
Estimated undiagnosed hypertension in the hospital setting
The prevalence of patients meeting the diagnostic criteria for clinic hypertension and no previous or existing ICD-10 codes for hypertension nor any of the prescribed antihypertensive drugs listed by British National Formulary (referred to here as “undiagnosed hypertension”) was 5% for men and for 5% women according to European ESC/ESH (140/90 threshold) and 14% men and 12% for women according to American ACC/AHA (130/80 threshold) guidelines. The analogous estimated prevalence of undiagnosed hypertension using the ABPM thresholds stratified by sex, age, NHS admission method, and NHS Specialty is given in Table 4.
Table 4.
Estimated undiagnosed ABPM daytime, ABPM nighttime, and ABPM 24-hour hypertension
| ESC/ESH | ACC/AHA | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ABPM | Daytime | Nighttime | 24 hours | Daytime | Nighttime | 24 hours | ||||||
| SBP/DBP ≥ | 135/85 | 120/70 | 130/80 | 130/80 | 110/65 | 125/75 | ||||||
| M | F | M | F | M | F | M | F | M | F | M | F | |
| Overall | 9 | 8 | 29 | 25 | 14 | 12 | 15 | 12 | 42 | 42 | 22 | 18 |
| Age groups | ||||||||||||
| 18–29 | 13 | 3 | 50 | 28 | 20 | 6 | 25 | 8 | 86 | 74 | 39 | 15 |
| 30–39 | 13 | 5 | 52 | 30 | 22 | 8 | 25 | 9 | 79 | 71 | 37 | 16 |
| 40–49 | 14 | 9 | 50 | 34 | 22 | 12 | 23 | 14 | 69 | 67 | 35 | 22 |
| 50–59 | 12 | 11 | 36 | 34 | 18 | 16 | 20 | 18 | 50 | 58 | 28 | 25 |
| 60–69 | 9 | 10 | 26 | 28 | 14 | 16 | 14 | 16 | 36 | 43 | 20 | 23 |
| 70–79 | 7 | 8 | 19 | 21 | 10 | 14 | 10 | 12 | 25 | 29 | 15 | 18 |
| 80–89 | 6 | 7 | 16 | 17 | 10 | 11 | 9 | 10 | 21 | 21 | 13 | 14 |
| 90+ | 6 | 7 | 19 | 17 | 11 | 11 | 10 | 9 | 25 | 20 | 15 | 15 |
| Admission method | ||||||||||||
| Elective | 8 | 8 | 29 | 24 | 14 | 11 | 15 | 12 | 42 | 46 | 22 | 18 |
| Emergency | 10 | 8 | 30 | 26 | 15 | 13 | 16 | 14 | 42 | 41 | 23 | 19 |
| Other | 6 | 6 | 20 | 19 | 9 | 9 | 9 | 9 | 28 | 32 | 15 | 13 |
| Specialty | ||||||||||||
| Medical | 8 | 8 | 24 | 24 | 12 | 12 | 12 | 12 | 35 | 38 | 18 | 18 |
| Surgical | 10 | 8 | 33 | 26 | 16 | 12 | 17 | 13 | 46 | 46 | 25 | 19 |
| Other | 11 | 11 | 34 | 28 | 17 | 15 | 17 | 16 | 49 | 49 | 24 | 21 |
Estimated undiagnosed hypertension prevalence (%) in-hospital population stratified by sex, age category, NHS Admission Method, and NHS Specialty according to the European ESC/ESH and American ACC/AHA guidelines (Supplementary Table ST-2 online). Abbreviations: DBP, diastolic blood pressure; F, female; M, male; SBP, systolic blood pressure. Daytime SBP (DBP) is the mean systolic (diastolic) blood pressure measurements taken during daytime hours (10:00 am to 7:59 pm). Nighttime SBP (DBP) is the mean systolic (diastolic) blood pressure measurements taken during night hours (midnight to 5:59 am).
The prevalence of those meeting the criteria for “undiagnosed” isolated nighttime hypertension was 17% according to ESC/ESH (22% according to ACC/AHA). The prevalence for those meeting the criteria for “undiagnosed” isolated systolic hypertension was lower at 5% according to ESC/ESH (9% according to ACC/AHA). The prevalence for undiagnosed isolated diastolic and daytime hypertension was nearly zero (Supplementary Table ST-6 online).
Estimated age-dependent trends of hypertension
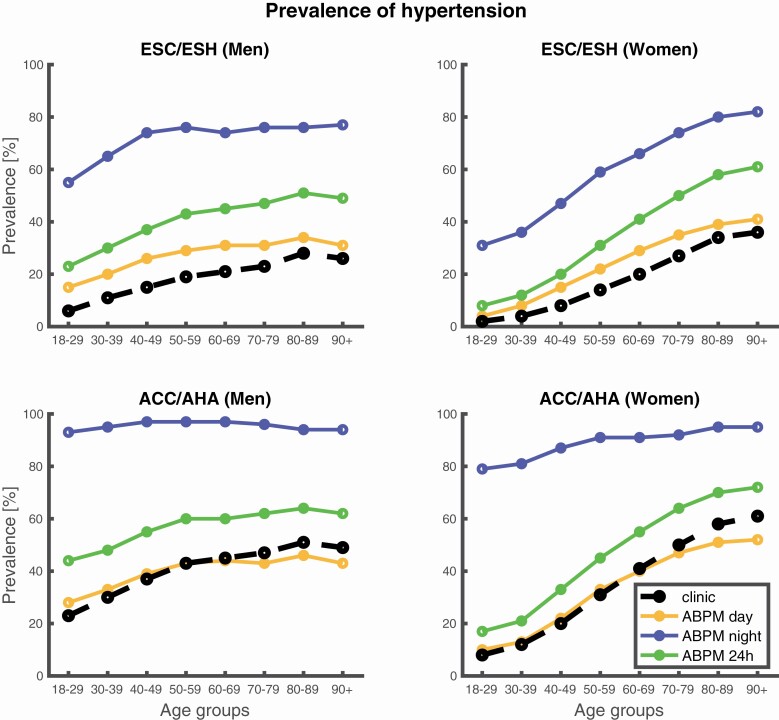
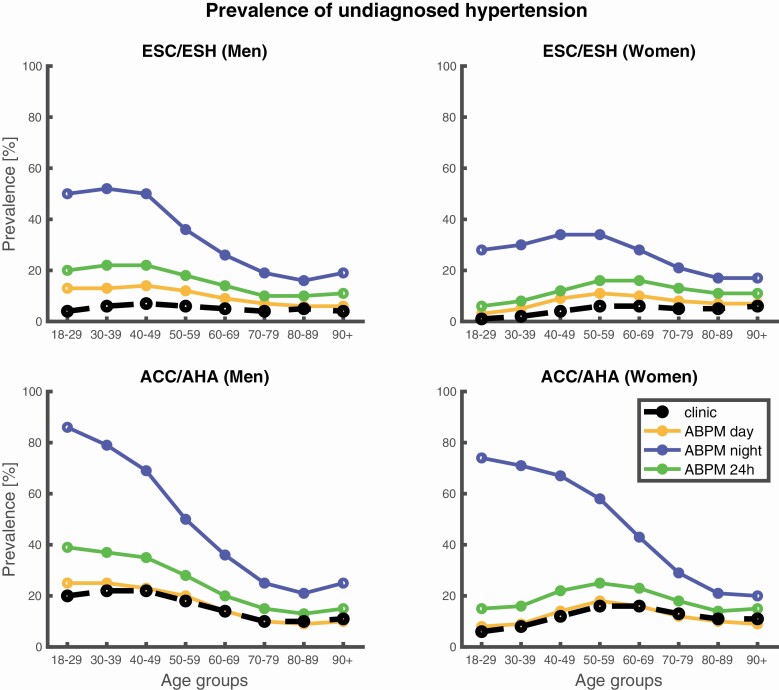
The estimated age-dependent prevalence of hypertension trends for men and women according to the European ESC/ESH and American ACC/AHA definitions of thresholds is shown in Figure 2, with underlying numbers in Table 3. The analogous estimated prevalence trends for undiagnosed hypertension, shown in Figure 3, with the underlying data presented in Table 4.
Figure 2.
Estimated age-dependent hypertension trends. Estimated prevalence trends of patients meeting the criteria for “clinic,” ABPM day, ABPM night, and ABPM 24-hour hypertension for different age groups according to the European ESC/ESH (top panel) and American ACC/AHA (bottom panel) guidelines (Supplementary Tables ST-2 online).
Figure 3.
Estimated undiagnosed age-dependent hypertension trends. Estimated prevalence of undiagnosed hypertension trends for different age groups according to the European ESC/ESH (top panel) and American ACC/AHA (bottom panel) guidelines.
Discussion
Key results
We estimated the prevalence of patients with average in-hospital BP meeting criteria for hypertension and undiagnosed hypertension according to the European 2018 ESC/ESH guidelines13 and American 2017 ACC/AHA guidelines,14 using a large hospital database of 1.7 million BP measurements. The proportion of patients meeting the diagnostic criteria for Stage 1, 2, or 3 hypertension was 21.4% when the European guidelines were applied and 47% when the American guidelines were applied. Overall, the proportion of patients meeting diagnostic criteria for hypertension increased with age, whilst number with “undiagnosed” hypertension decreased with age.
Interpretation
Although the prevalence of hypertension and specifically undiagnosed hypertension in the community has been well established, it is rarely reported in the hospital setting. Literature regarding the prevalence of elevated in-hospital BP in the absence of a diagnosis of hypertension and its diagnostic ability and association with a persistently raised BP postdischarge and the future development of hypertension are also lacking; a recent systematic review that investigated the extent to which elevated in-hospital BP can predict undiagnosed hypertension identified 12 studies of emergency department populations but none of inpatient populations.9
Prevalence of hypertension
The prevalence of undiagnosed hypertension in emergency departments has been reported to be about 3%–15% of adult patients, of which nearly 50% being categorized as having Stage 1 hypertension, 25%–36% Stage 2 hypertension, and 12%–30% Stage 3 hypertension.16 In comparison, the current study shows that the estimated prevalence of patients undiagnosed hypertension (see Methods section for a definition) was 5% using ESC/ESH and 13% using ACC/AHA criteria. We note that using lower ABPM daytime, nighttime, and 24-hour thresholds yields higher estimated prevalences (Table 4).
Screening for hypertension in hospital
Hospital admission allows for opportunistic screening of BP and potential identification of undiagnosed hypertension. The accumulation of multiple measurements during hospital admission may also allow more accurate detection of patients who have hypertension. The prevalence of nocturnal high BP suggests a single normotensive screening measurement obtained in a primary care appointment might falsely classify some patients reaching hypertension criteria in hospital as being normotensive.
Figure 2 shows that the prevalence of elevated BP increases with age. This patient group includes those with and without an existing diagnosis of hypertension. Although many of those with diagnosed hypertension had elevated BP in hospital, this may result from decreased antihypertensive treatment during the hospital stay, rather than reflecting uncontrolled hypertension in the community.
Figure 3 illustrates that there is a decrease in prevalence of patients meeting criteria for “undiagnosed” hypertension with advancing age. It is unlikely that this is solely attributable to physiological aging and may reflect increased pick-up as age increases. The marked prevalence of patients meeting criteria for “undiagnosed” hypertension suggests in-hospital screening may be worthwhile.17 Whilst elevated or labile BP in hospital may be attributed to stress and anxiety, previous studies have suggested increased BP lability under stress is a predictor of future cardiovascular events.18
A particularly interesting aspect of hospital screening is the finding that 17% patients met the ESC/ESH (22% ACC/AHA) criteria for undiagnosed isolated nighttime hypertension. These patients would not be identified for 24-hour ABPM by office measurements, but may have increased cardiovascular risk.19
Present guidelines on the management of elevated BP in hospital are only applicable to patients who have markedly elevated BP in the emergency department setting.20 Internationally, hypertension guidelines provide diagnostic criteria for the clinic, home, or ambulatory setting (Supplementary Tables ST-1 and ST-2 online) but do not suggest diagnostic thresholds for the in-hospital setting. This may be owing to a lack of studies upon which hospital thresholds could be defined. Indeed, the emergency department guidelines draw on evidence from few studies which are limited in sample size and representativeness.9 However, studies conducted in Emergency Departments suggest that between 25% and 76% of those with high BP in the emergency department meet criteria for the diagnosis of hypertension in the community.9 As our hospitalized patients contributed more BP readings than patients with brief hospital attendances in the emergency departments studies9 classification of BP using in-hospital measurements may prove more predictive.
Study limitations
This was a retrospective study with inherent limitations. The study used measurements recorded on the wards by nursing staff as part of their regular observations of in-hospital patients. This poses 2 potential limitations. Firstly, patients who have longer hospital stays will contribute more data to a hospital database of vital-sign observations. We compensated for this by generating 1 24-hour BP profile per patient, regardless of their length of hospital stay with details of this procedure described in ref. 12. Secondly, the question of selection bias arises. The patients who are clinically less stable may have their BP taken more frequently during nighttime hours. However, observations may also be measured at night as a result of admission time or clinical protocols. Our predefined inclusion criteria based on earlier work in which we defined a method for 24-hour BP profiling of patients meant we excluded the majority of patients admitted to hospital. The greatest number of patients was excluded due to having no nighttime BP measurements. This may have caused us to underestimate the prevalence of daytime hypertension.
This study included patients from 4 hospitals (3 tertiary and 1 secondary) within a single University Hospital Trust in the United Kingdom. Further work is needed to discover whether our results are generalizable to hospitalized patients in different regions of the world. Finally, our work includes only in-hospital BPs. Further research investigating the diagnostic performance of in-hospital BP measurements for reliably detecting community hypertension is required.
A substantial number of hospitalized patients have an average in-hospital BP that exceeds international criteria for the diagnosis of hypertension, with many demonstrating isolated nocturnal hypertension that are unlikely to be picked up with clinic or home BP measurements. In-hospital BPs may present an opportunity to detect patients with previously undiagnosed hypertension.
Supplementary Material
ACKNOWLEDGMENTS
The views expressed are those of the authors and not necessarily those of the National Health Service (NHS), the National Institute for Health Research, or the Department of Health. This research would not have been possible without the help of Dr Marco Pimentel, who was instrumental in compiling the anonymized patient data.
FUNDING
The research was supported by the National Institute for Health Research (NIHR) Oxford Biomedical Research Centre and by an EPSRC grant (EP/EP/N024966/1—Intelligent Wearable Sensors for Predictive Patient Monitoring).
ETHICAL APPROVAL
This study was approved by the Oxfordshire Research Ethics Committee (reference: 16/SC/0264), with Confidential Advisory Group approval to process patient data without consent (reference: 16/CAG/0066).
DISCLOSURE
A.M. was funded by an EPSRC grant (EP/EP/N024966/1—Intelligent Wearable Sensors for Predictive Patient Monitoring). L.C.A. is funded by a Wellcome Trust Doctoral Research Fellowship [203921/Z/16/Z]. For the purpose of open access, the author has applied a CC BY public copyright license to any Author Accepted Manuscript version arising from this submission. L.T. is a nonexecutive Director of Sensyne Health and holds share options in the company. P.W. was Chief Medical Officer for Sensyne Health and holds shares in the company.
REFERENCES
- 1. Lewington S, Clarke R, Qizilbash N, Peto R, Collins R; Prospective Studies Collaboration . Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 2002; 360:1903–1913. [DOI] [PubMed] [Google Scholar]
- 2. Reibis RK, Huber M, Karoff M, Kamke W, Kreutz R, Wegscheider K, Völler H. Target organ damage and control of cardiovascular risk factors in hypertensive patients. Evidence from the multicenter ESTher registry. Herz 2015; 40(Suppl 2):209–216. [DOI] [PubMed] [Google Scholar]
- 3. Fleming S, Atherton H, McCartney D, Hodgkinson J, Greenfield S, Hobbs FD, Mant J, McManus RJ, Thompson M, Ward A, Heneghan C. Self-screening and non-physician screening for hypertension in communities: a systematic review. Am J Hypertens 2015; 28:1316–1324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Public Health England. NHS Health Check: Our Approach to the Evidence (PHE number: 2013097). 2013. [Google Scholar]
- 5. Martin A, Saunders CL, Harte E, Griffin SJ, MacLure C, Mant J, Meads C, Walter FM, Usher-Smith JA. Delivery and impact of the NHS Health Check in the first 8 years: a systematic review. Br J Gen Pract 2018; 68:e449–e459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Public Health England. Hypertension Prevalence Estimates in England for Local Populations (PHE number GW-1181). 2016. [Google Scholar]
- 7. NCD Risk Factor Collaboration (NCD-RisC), Danaei G, Stevens GA, Bixby H, Taddei C, Carrillo-Larco RM, Solomon B, Riley LM, Cesare M Di, Iurilli MLC, Rodriguez-Martinez A, Zhu A, Hajifathalian K, Amuzu A, Banegas JR, Bennett JE, Cameron C, Cho Y, Clarke J, Craig CL, Cruz JJ, Gates L, Giampaoli S, Gregg EW, Hardy R, Hayes AJ, Ikeda N, Jackson RT, Jennings G, Joffres M, Khang Y-H, Koskinen S, Kuh D, Kujala UM, Laatikainen T, Lehtimäki T, Lopez-Garcia E, Lundqvist A, Maggi S, Magliano DJ, Mann JI, McLean RM, McLean SB, Miller JC, Morgan K, Neuhauser HK, Niiranen TJ, Noale M, Oh K, Palmieri L, Panza F, Parnell WR, Peltonen M, Raitakari O, Rodríguez-Artalejo F, Roy JG, Salomaa V, Sarganas G, Servais J, Shaw JE, Shibuya K, Solfrizzi V, Stavreski B, Tan EJ, Turley ML, Vanuzzo D, Viikari-Juntura E, Weerasekera D, Ezzati M. Long-term and recent trends in hypertension awareness, treatment, and control in 12 high-income countries: an analysis of 123 nationally representative surveys. Lancet (London, England) 2019; 394:639–651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Forouzanfar MH, Alexander L, Anderson HR, Bachman VF, Biryukov S, Brauer M, Burnett R, Casey D, Coates MM, Cohen A, Delwiche K, Estep K, Frostad JJ, KC A, Kyu HH, Moradi-Lakeh M, Ng M, Slepak EL, Thomas BA, Wagner J, Aasvang GM, Abbafati C, Ozgoren AA, Abd-Allah F, Abera SF, Aboyans V, Abraham B, Abraham JP, Abubakar I, Abu-Rmeileh NME, Aburto TC, Achoki T, Adelekan A, Adofo K, Adou AK, Adsuar JC, Afshin A, Agardh EE, Al Khabouri MJ, Al Lami FH, Alam SS, Alasfoor D, Albittar MI, Alegretti MA, Aleman A V, Alemu ZA, Alfonso-Cristancho R, Alhabib S, Ali R, Ali MK, Alla F, Allebeck P, Allen PJ, Alsharif U, Alvarez E, Alvis-Guzman N, Amankwaa AA, Amare AT, Ameh EA, Ameli O, Amini H, Ammar W, Anderson BO, Antonio CAT, Anwari P, Cunningham SA, Arnlöv J, Arsenijevic VSA, Artaman A, Asghar RJ, Assadi R, Atkins LS, Atkinson C, Avila MA, Awuah B, Badawi A, Bahit MC, Bakfalouni T, Balakrishnan K, Balalla S, Balu RK, Banerjee A, Barber RM, Barker-Collo SL, Barquera S, Barregard L, Barrero LH, Barrientos-Gutierrez T, Basto-Abreu AC, Basu A, Basu S, Basulaiman MO, Ruvalcaba CB, Beardsley J, Bedi N, Bekele T, Bell ML, Benjet C, Bennett DA, Benzian H, Bernabé E, Beyene TJ, Bhala N, Bhalla A, Bhutta ZA, Bikbov B, Abdulhak AA Bin, Blore JD, Blyth FM, Bohensky MA, Başara BB, Borges G, Bornstein NM, Bose D, Boufous S, Bourne RR, Brainin M, Brazinova A, Breitborde NJ, Brenner H, Briggs ADM, Broday DM, Brooks PM, Bruce NG, Brugha TS, Brunekreef B, Buchbinder R, Bui LN, Bukhman G, Bulloch AG, Burch M, Burney PGJ, Campos-Nonato IR, Campuzano JC, Cantoral AJ, Caravanos J, Cárdenas R, Cardis E, Carpenter DO, Caso V, Castañeda-Orjuela CA, Castro RE, Catalá-López F, Cavalleri F, Çavlin A, Chadha VK, Chang J, Charlson FJ, Chen H, Chen W, Chen Z, Chiang PP, Chimed-Ochir O, Chowdhury R, Christophi CA, Chuang T-W, Chugh SS, Cirillo M, Claßen TK, Colistro V, Colomar M, Colquhoun SM, Contreras AG, Cooper C, Cooperrider K, Cooper LT, Coresh J, Courville KJ, Criqui MH, Cuevas-Nasu L, Damsere-Derry J, Danawi H, Dandona L, Dandona R, Dargan PI, Davis A, Davitoiu D V, Dayama A, de Castro EF, De la Cruz-Góngora V, De Leo D, de Lima G, Degenhardt L, del Pozo-Cruz B, Dellavalle RP, Deribe K, Derrett S, Jarlais DC Des, Dessalegn M, deVeber GA, Devries KM, Dharmaratne SD, Dherani MK, Dicker D, Ding EL, Dokova K, Dorsey ER, Driscoll TR, Duan L, Durrani AM, Ebel BE, Ellenbogen RG, Elshrek YM, Endres M, Ermakov SP, Erskine HE, Eshrati B, Esteghamati A, Fahimi S, Faraon EJA, Farzadfar F, Fay DFJ, Feigin VL, Feigl AB, Fereshtehnejad S-M, Ferrari AJ, Ferri CP, Flaxman AD, Fleming TD, Foigt N, Foreman KJ, Paleo UF, Franklin RC, Gabbe B, Gaffikin L, Gakidou E, Gamkrelidze A, Gankpé FG, Gansevoort RT, García-Guerra FA, Gasana E, Geleijnse JM, Gessner BD, Gething P, Gibney KB, Gillum RF, Ginawi IAM, Giroud M, Giussani G, Goenka S, Goginashvili K, Dantes HG, Gona P, de Cosio TG, González-Castell D, Gotay CC, Goto A, Gouda HN, Guerrant RL, Gugnani HC, Guillemin F, Gunnell D, Gupta R, Gupta R, Gutiérrez RA, Hafezi-Nejad N, Hagan H, Hagstromer M, Halasa YA, Hamadeh RR, Hammami M, Hankey GJ, Hao Y, Harb HL, Haregu TN, Haro JM, Havmoeller R, Hay SI, Hedayati MT, Heredia-Pi IB, Hernandez L, Heuton KR, Heydarpour P, Hijar M, Hoek HW, Hoffman HJ, Hornberger JC, Hosgood HD, Hoy DG, Hsairi M, Hu G, Hu H, Huang C, Huang JJ, Hubbell BJ, Huiart L, Husseini A, Iannarone ML, Iburg KM, Idrisov BT, Ikeda N, Innos K, Inoue M, Islami F, Ismayilova S, Jacobsen KH, Jansen HA, Jarvis DL, Jassal SK, Jauregui A, Jayaraman S, Jeemon P, Jensen PN, Jha V, Jiang F, Jiang G, Jiang Y, Jonas JB, Juel K, Kan H, Roseline SSK, Karam NE, Karch A, Karema CK, Karthikeyan G, Kaul A, Kawakami N, Kazi DS, Kemp AH, Kengne AP, Keren A, Khader YS, Khalifa SEAH, Khan EA, Khang Y-H, Khatibzadeh S, Khonelidze I, Kieling C, Kim D, Kim S, Kim Y, Kimokoti RW, Kinfu Y, Kinge JM, Kissela BM, Kivipelto M, Knibbs LD, Knudsen AK, Kokubo Y, Kose MR, Kosen S, Kraemer A, Kravchenko M, Krishnaswami S, Kromhout H, Ku T, Defo BK, Bicer BK, Kuipers EJ, Kulkarni C, Kulkarni VS, Kumar GA, Kwan GF, Lai T, Balaji AL, Lalloo R, Lallukka T, Lam H, Lan Q, Lansingh VC, Larson HJ, Larsson A, Laryea DO, Lavados PM, Lawrynowicz AE, Leasher JL, Lee J-T, Leigh J, Leung R, Levi M, Li Y, Li Y, Liang J, Liang X, Lim SS, Lindsay MP, Lipshultz SE, Liu S, Liu Y, Lloyd BK, Logroscino G, London SJ, Lopez N, Lortet-Tieulent J, Lotufo PA, Lozano R, Lunevicius R, Ma J, Ma S, Machado VMP, MacIntyre MF, Magis-Rodriguez C, Mahdi AA, Majdan M, Malekzadeh R, Mangalam S, Mapoma CC, Marape M, Marcenes W, Margolis DJ, Margono C, Marks GB, Martin R V, Marzan MB, Mashal MT, Masiye F, Mason-Jones AJ, Matsushita K, Matzopoulos R, Mayosi BM, Mazorodze TT, McKay AC, McKee M, McLain A, Meaney PA, Medina C, Mehndiratta MM, Mejia-Rodriguez F, Mekonnen W, Melaku YA, Meltzer M, Memish ZA, Mendoza W, Mensah GA, Meretoja A, Mhimbira FA, Micha R, Miller TR, Mills EJ, Misganaw A, Mishra S, Ibrahim NM, Mohammad KA, Mokdad AH, Mola GL, Monasta L, Hernandez JCM, Montico M, Moore AR, Morawska L, Mori R, Moschandreas J, Moturi WN, Mozaffarian D, Mueller UO, Mukaigawara M, Mullany EC, Murthy KS, Naghavi M, Nahas Z, Naheed A, Naidoo KS, Naldi L, Nand D, Nangia V, Narayan KV, Nash D, Neal B, Nejjari C, Neupane SP, Newton CR, Ngalesoni FN, de Dieu Ngirabega J, Nguyen G, Nguyen NT, Nieuwenhuijsen MJ, Nisar MI, Nogueira JR, Nolla JM, Nolte S, Norheim OF, Norman RE, Norrving B, Nyakarahuka L, Oh I-H, Ohkubo T, Olusanya BO, Omer SB, Opio JN, Orozco R, Pagcatipunan RS, Pain AW, Pandian JD, Panelo CIA, Papachristou C, Park E-K, Parry CD, Caicedo AJP, Patten SB, Paul VK, Pavlin BI, Pearce N, Pedraza LS, Pedroza A, Stokic LP, Pekericli A, Pereira DM, Perez-Padilla R, Perez-Ruiz F, Perico N, Perry SAL, Pervaiz A, Pesudovs K, Peterson CB, Petzold M, Phillips MR, Phua HP, Plass D, Poenaru D, Polanczyk G V, Polinder S, Pond CD, Pope CA, Pope D, Popova S, Pourmalek F, Powles J, Prabhakaran D, Prasad NM, Qato DM, Quezada AD, Quistberg DAA, Racapé L, Rafay A, Rahimi K, Rahimi-Movaghar V, Rahman SU, Raju M, Rakovac I, Rana SM, Rao M, Razavi H, Reddy KS, Refaat AH, Rehm J, Remuzzi G, Ribeiro AL, Riccio PM, Richardson L, Riederer A, Robinson M, Roca A, Rodriguez A, Rojas-Rueda D, Romieu I, Ronfani L, Room R, Roy N, Ruhago GM, Rushton L, Sabin N, Sacco RL, Saha S, Sahathevan R, Sahraian MA, Salomon JA, Salvo D, Sampson UK, Sanabria JR, Sanchez LM, Sánchez-Pimienta TG, Sanchez-Riera L, Sandar L, Santos IS, Sapkota A, Satpathy M, Saunders JE, Sawhney M, Saylan MI, Scarborough P, Schmidt JC, Schneider IJC, Schöttker B, Schwebel DC, Scott JG, Seedat S, Sepanlou SG, Serdar B, Servan-Mori EE, Shaddick G, Shahraz S, Levy TS, Shangguan S, She J, Sheikhbahaei S, Shibuya K, Shin HH, Shinohara Y, Shiri R, Shishani K, Shiue I, Sigfusdottir ID, Silberberg DH, Simard EP, Sindi S, Singh A, Singh GM, Singh JA, Skirbekk V, Sliwa K, Soljak M, Soneji S, Søreide K, Soshnikov S, Sposato LA, Sreeramareddy CT, Stapelberg NJC, Stathopoulou V, Steckling N, Stein DJ, Stein MB, Stephens N, Stöckl H, Straif K, Stroumpoulis K, Sturua L, Sunguya BF, Swaminathan S, Swaroop M, Sykes BL, Tabb KM, Takahashi K, Talongwa RT, Tandon N, Tanne D, Tanner M, Tavakkoli M, Te Ao BJ, Teixeira CM, Téllez Rojo MM, Terkawi AS, Texcalac-Sangrador JL, Thackway S V, Thomson B, Thorne-Lyman AL, Thrift AG, Thurston GD, Tillmann T, Tobollik M, Tonelli M, Topouzis F, Towbin JA, Toyoshima H, Traebert J, Tran BX, Trasande L, Trillini M, Trujillo U, Dimbuene ZT, Tsilimbaris M, Tuzcu EM, Uchendu US, Ukwaja KN, Uzun SB, van de Vijver S, Van Dingenen R, van Gool CH, van Os J, Varakin YY, Vasankari TJ, Vasconcelos AMN, Vavilala MS, Veerman LJ, Velasquez-Melendez G, Venketasubramanian N, Vijayakumar L, Villalpando S, Violante FS, Vlassov VV, Vollset SE, Wagner GR, Waller SG, Wallin MT, Wan X, Wang H, Wang J, Wang L, Wang W, Wang Y, Warouw TS, Watts CH, Weichenthal S, Weiderpass E, Weintraub RG, Werdecker A, Wessells KR, Westerman R, Whiteford HA, Wilkinson JD, Williams HC, Williams TN, Woldeyohannes SM, Wolfe CDA, Wong JQ, Woolf AD, Wright JL, Wurtz B, Xu G, Yan LL, Yang G, Yano Y, Ye P, Yenesew M, Yentür GK, Yip P, Yonemoto N, Yoon S-J, Younis MZ, Younoussi Z, Yu C, Zaki ME, Zhao Y, Zheng Y, Zhou M, Zhu J, Zhu S, Zou X, Zunt JR, Lopez AD, Vos T, Murray CJ. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015; 386:2287–2323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Armitage LC, Whelan ME, Watkinson PJ, Farmer AJ. Screening for hypertension using emergency department blood pressure measurements can identify patients with undiagnosed hypertension: a systematic review with meta-analysis. J Clin Hypertens (Greenwich) 2019; 21:1415–1425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Staessen JA, Bieniaszewski L, O’Brien E, Gosse P, Hayashi H, Imai Y, Kawasaki T, Otsuka K, Palatini P, Thijs L, Fagard R. Nocturnal blood pressure fall on ambulatory monitoring in a large international database. The “Ad Hoc” Working Group. Hypertension 1997; 29:30–39. [DOI] [PubMed] [Google Scholar]
- 11. Wong D, Bonnici T, Knight J, Morgan L, Coombes P, Watkinson P. SEND: a system for electronic notification and documentation of vital sign observations. BMC Med Inform Decis Mak 2015; 15:68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Mahdi A, Watkinson P, McManus RJ, Tarassenko L. Circadian blood pressure variations computed from 1.7 million measurements in an acute hospital setting. Am J Hypertens 2019; 32:1154–1161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, Clement DL, Coca A, de Simone G, Dominiczak A, Kahan T, Mahfoud F, Redon J, Ruilope L, Zanchetti A, Kerins M, Kjeldsen SE, Kreutz R, Laurent S, Lip GYH, McManus R, Narkiewicz K, Ruschitzka F, Schmieder RE, Shlyakhto E, Tsioufis C, Aboyans V, Desormais I, De Backer G, Heagerty AM, Agewall S, Bochud M, Borghi C, Boutouyrie P, Brguljan J, Bueno H, Caiani EG, Carlberg B, Chapman N, Cífková R, Cleland JGF, Collet J-P, Coman IM, de Leeuw PW, Delgado V, Dendale P, Diener H-C, Dorobantu M, Fagard R, Farsang C, Ferrini M, Graham IM, Grassi G, Haller H, Hobbs FDR, Jelakovic B, Jennings C, Katus HA, Kroon AA, Leclercq C, Lovic D, Lurbe E, Manolis AJ, McDonagh TA, Messerli F, Muiesan ML, Nixdorff U, Olsen MH, Parati G, Perk J, Piepoli MF, Polonia J, Ponikowski P, Richter DJ, Rimoldi SF, Roffi M, Sattar N, Seferovic PM, Simpson IA, Sousa-Uva M, Stanton A V, van de Borne P, Vardas P, Volpe M, Wassmann S, Windecker S, Zamorano JL, Windecker S, Aboyans V, Agewall S, Barbato E, Bueno H, Coca A, Collet J-P, Coman IM, Dean V, Delgado V, Fitzsimons D, Gaemperli O, Hindricks G, Iung B, Jüni P, Katus HA, Knuuti J, Lancellotti P, Leclercq C, McDonagh TA, Piepoli MF, Ponikowski P, Richter DJ, Roffi M, Shlyakhto E, Simpson IA, Sousa-Uva M, Zamorano JL, Tsioufis C, Lurbe E, Kreutz R, Bochud M, Rosei EA, Jelakovic B, Azizi M, Januszewics A, Kahan T, Polonia J, van de Borne P, Williams B, Borghi C, Mancia G, Parati G, Clement DL, Coca A, Manolis A, Lovic D, Benkhedda S, Zelveian P, Siostrzonek P, Najafov R, Pavlova O, De Pauw M, Dizdarevic-Hudic L, Raev D, Karpettas N, Linhart A, Olsen MH, Shaker AF, Viigimaa M, Metsärinne K, Vavlukis M, Halimi J-M, Pagava Z, Schunkert H, Thomopoulos C, Páll D, Andersen K, Shechter M, Mercuro G, Bajraktari G, Romanova T, Trušinskis K, Saade GA, Sakalyte G, Noppe S, DeMarco DC, Caraus A, Wittekoek J, Aksnes TA, Jankowski P, Polonia J, Vinereanu D, Baranova EI, Foscoli M, Dikic AD, Filipova S, Fras Z, Bertomeu-Martínez V, Carlberg B, Burkard T, Sdiri W, Aydogdu S, Sirenko Y, Brady A, Weber T, Lazareva I, De Backer T, Sokolovic S, Jelakovic B, Widimsky J, Viigimaa M, Pörsti I, Denolle T, Krämer BK, Stergiou GS, Parati G, Trušinskis K, Miglinas M, Gerdts E, Tykarski A, de Carvalho Rodrigues M, Dorobantu M, Chazova I, Lovic D, Filipova S, Brguljan J, Segura J, Gottsäter A, Pechère-Bertschi A, Erdine S, Sirenko Y, Brady A. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J 2018; 39:3021–3104. [DOI] [PubMed] [Google Scholar]
- 14. Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, DePalma SM, Gidding S, Jamerson KA, Jones DW, MacLaughlin EJ, Muntner P, Ovbiagele B, Smith SC Jr, Spencer CC, Stafford RS, Taler SJ, Thomas RJ, Williams KA Sr, Williamson JD, Wright JT Jr. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol 2018; 71:e127–e248. [DOI] [PubMed] [Google Scholar]
- 15. Joint Formulary Committee. British National Formulary (BNF) No. 72. Pharmaceutical Press: London, UK, 2016, p. 1424. [Google Scholar]
- 16. Svenson JE, Repplinger M. Hypertension in the ED: still an unrecognized problem. Am J Emerg Med 2008; 26:913–917. [DOI] [PubMed] [Google Scholar]
- 17. Armitage LC, Mahdi A, Lawson BK, Roman C, Fanshawe T, Tarassenko L, Farmer AJ, Watkinson PJ. Screening for Hypertension in the INpatient Environment (SHINE): a protocol for a prospective study of diagnostic accuracy among adult hospital patients. BMJ Open 2019; 9:e033792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Chida Y, Steptoe A. Greater cardiovascular responses to laboratory mental stress are associated with poor subsequent cardiovascular risk status: a meta-analysis of prospective evidence. Hypertension 2010; 55:1026–1032. [DOI] [PubMed] [Google Scholar]
- 19. Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, Amann M, Anderson HR, Andrews KG, Aryee M, Atkinson C, Bacchus LJ, Bahalim AN, Balakrishnan K, Balmes J, Barker-Collo S, Baxter A, Bell ML, Blore JD, Blyth F, Bonner C, Borges G, Bourne R, Boussinesq M, Brauer M, Brooks P, Bruce NG, Brunekreef B, Bryan-Hancock C, Bucello C, Buchbinder R, Bull F, Burnett RT, Byers TE, Calabria B, Carapetis J, Carnahan E, Chafe Z, Charlson F, Chen H, Chen JS, Cheng AT, Child JC, Cohen A, Colson KE, Cowie BC, Darby S, Darling S, Davis A, Degenhardt L, Dentener F, Des Jarlais DC, Devries K, Dherani M, Ding EL, Dorsey ER, Driscoll T, Edmond K, Ali SE, Engell RE, Erwin PJ, Fahimi S, Falder G, Farzadfar F, Ferrari A, Finucane MM, Flaxman S, Fowkes FG, Freedman G, Freeman MK, Gakidou E, Ghosh S, Giovannucci E, Gmel G, Graham K, Grainger R, Grant B, Gunnell D, Gutierrez HR, Hall W, Hoek HW, Hogan A, Hosgood HD III, Hoy D, Hu H, Hubbell BJ, Hutchings SJ, Ibeanusi SE, Jacklyn GL, Jasrasaria R, Jonas JB, Kan H, Kanis JA, Kassebaum N, Kawakami N, Khang YH, Khatibzadeh S, Khoo JP, Kok C, Laden F, Lalloo R, Lan Q, Lathlean T, Leasher JL, Leigh J, Li Y, Lin JK, Lipshultz SE, London S, Lozano R, Lu Y, Mak J, Malekzadeh R, Mallinger L, Marcenes W, March L, Marks R, Martin R, McGale P, McGrath J, Mehta S, Mensah GA, Merriman TR, Micha R, Michaud C, Mishra V, Mohd Hanafiah K, Mokdad AA, Morawska L, Mozaffarian D, Murphy T, Naghavi M, Neal B, Nelson PK, Nolla JM, Norman R, Olives C, Omer SB, Orchard J, Osborne R, Ostro B, Page A, Pandey KD, Parry CD, Passmore E, Patra J, Pearce N, Pelizzari PM, Petzold M, Phillips MR, Pope D, Pope CA III, Powles J, Rao M, Razavi H, Rehfuess EA, Rehm JT, Ritz B, Rivara FP, Roberts T, Robinson C, Rodriguez-Portales JA, Romieu I, Room R, Rosenfeld LC, Roy A, Rushton L, Salomon JA, Sampson U, Sanchez-Riera L, Sanman E, Sapkota A, Seedat S, Shi P, Shield K, Shivakoti R, Singh GM, Sleet DA, Smith E, Smith KR, Stapelberg NJ, Steenland K, Stöckl H, Stovner LJ, Straif K, Straney L, Thurston GD, Tran JH, Van Dingenen R, van Donkelaar A, Veerman JL, Vijayakumar L, Weintraub R, Weissman MM, White RA, Whiteford H, Wiersma ST, Wilkinson JD, Williams HC, Williams W, Wilson N, Woolf AD, Yip P, Zielinski JM, Lopez AD, Murray CJ, Ezzati M, AlMazroa MA, Memish ZA. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012; 380:2224–2260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Wolf SJ, Lo B, Shih RD, Smith MD, Fesmire FM; American College of Emergency Physicians Clinical Policies Committee . Clinical policy: critical issues in the evaluation and management of adult patients in the emergency department with asymptomatic elevated blood pressure. Ann Emerg Med 2013; 62:59–68. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.