Abstract
Background
The Affordable Care Act (ACA) Medicaid expansion improved access to health insurance and health care services. This study assessed whether the rate of patients with undiagnosed hypertension and the rate of patients with hypertension without anti-hypertensive medication decreased post-ACA in community health center (CHC).
Methods
We analyzed electronic health record data from 2012 to 2017 for 126,699 CHC patients aged 19–64 years with ≥1 visit pre-ACA and ≥1 post-ACA in 14 Medicaid expansion states. We estimated the prevalence of patients with undiagnosed hypertension (high blood pressure reading without a diagnosis for ≥1 day) and the prevalence of patients with hypertension without anti-hypertensive medication by year and health insurance type (continuously uninsured, continuously insured, gained insurance, and discontinuously insured). We compared the time to diagnosis or to anti-hypertensive medication pre- vs. post-ACA.
Results
Overall, 37.3% of patients had undiagnosed hypertension and 27.0% of patients with diagnosed hypertension were without a prescribed anti-hypertensive medication for ≥1 day during the study period. The rate of undiagnosed hypertension decreased from 2012 through 2017. Those who gained insurance had the lowest rates of undiagnosed hypertension (2012: 14.8%; 2017: 6.1%). Patients with hypertension were also more likely to receive anti-hypertension medication during this period, especially uninsured patients who experienced the largest decline (from 47.0% to 8.1%). Post-ACA, among patients with undiagnosed hypertension, time to diagnosis was shorter for those who gained insurance than other insurance types.
Conclusions
Those who gained health insurance were appropriately diagnosed with hypertension faster and more frequently post-ACA than those with other insurance types.
Clinical trials registration
Trial Number NCT03545763.
Keywords: Affordable Care Act, blood pressure, community health center, hypertension, Medicaid expansion, medication
Graphical Abstract
Graphical Abstract.
Uncontrolled hypertension is the largest single contributor to all-cause and cardiovascular mortality.1 Annually, hypertension—as a primary or contributing cause—leads to about 500,000 US deaths2 and to high medical spending, estimated at >$50 billion yearly.3 Currently, about 108 million US adults (nearly 1 in 2) have hypertension.2,3 In 2017, only 43.7% of patients with hypertension had blood pressure <140/90 and 19.0% had blood pressure <130/80.4 Additionally, Wall et al.5 noted that up to 30% of clinic patients with sustained high blood pressure are “hiding in plain sight” with multiple documented elevated blood pressure measurements, but no hypertension diagnosis or anti-hypertensive medications.
Patients with hypertension must engage in daily management activities such as taking medications or adhering to diet and exercise regimens.6 Access to health insurance is a critical aspect of hypertension detection, treatment, and control7 and a lack of insurance can greatly exacerbate barriers to successful hypertension care and management.8 Adults without insurance have lower prevalence of known hypertension (<20%) relative to Medicaid recipients (~30%),9 as they are more likely to be undiagnosed; an estimated 30% of uninsured adults have undiagnosed hypertension.10,11 Health insurance may be especially beneficial for patients with lower income and hypertension, who may be unable to afford health care services without coverage.
The Affordable Care Act (ACA) Medicaid expansion substantially improved access to health insurance and health care services for patients, including preventive services, especially among adults with lower income.12–16 To date, several studies have focused specifically on changes to hypertension care following the ACA and found improvement in blood pressure screening and fewer barriers to accessing care.17–19 One study showed a significant reduction in access barriers for young adults (19–25 years of age) with hypertension and a subsequent increase in access to health care services following the ACA.18 There was no evidence, however, whether this improved access to care led to decreases in undiagnosed hypertension. As noted above, individuals without health insurance are more likely to have undiagnosed hypertension. As such, it is hypothesized that gaining health insurance could lead to increased rates of appropriate hypertension diagnosis as well as adequate treatment (i.e., receiving anti-hypertensive medications). Thus, we sought to investigate whether the rate of patients with undiagnosed hypertension and the rate of patients with diagnosed hypertension without anti-hypertensive medication would decrease post-ACA among patients with lower income who receive care in community health centers (CHCs).
METHODS
Data source
Electronic health record (EHR) data were obtained from the OCHIN community health information network, a multistate collaboration of CHCs.20 Eligible clinics (n = 93) were primary care clinics or local health departments that were “live” on OCHIN’s EHR before 1 January 2012 and remained live throughout the entire period and were in a state that expanded its Medicaid program following the ACA. We analyzed data from 2012 to 2017 (pre-ACA: 2012–2013; post-ACA: 2014–2017) for patients who were 19–64 years of age throughout the study period, had at least 2 ambulatory visits within 2 years of each other at an eligible clinic, and had at least 1 visit pre-ACA and at least 1 visit post-ACA. Patients who were pregnant during the study period, those with a documented diagnosis for end-stage renal disease, and patients with a Medicare-financed visit during the study period were excluded. Our final sample included 126,699 patients from 14 states (Alaska, California, Hawaii, Indiana, Maryland, Minnesota, Montana, New Mexico, Nevada, Ohio, Oregon, Rhode Island, Washington, and Wisconsin).
Definitions of patients with no hypertension, diagnosed hypertension, undiagnosed hypertension, and patients with diagnosed hypertension without hypertensive medication
No hypertension was defined as those without a diagnosis or any indication of undiagnosed hypertension as defined below.
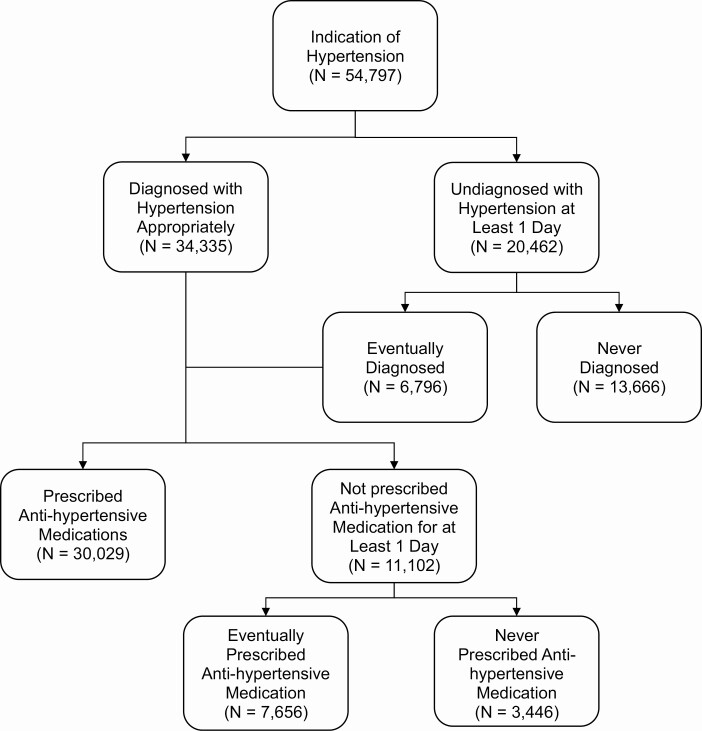
Patients with diagnosed hypertension had a documented problem list or visit diagnosis for hypertension any time before or during the study period (see Figure 1).
Figure 1.
Operationalization of patients defined as having undiagnosed hypertension and those with diagnosed hypertension without anti-hypertensive medication.
Following previous studies, patients with undiagnosed hypertension21 had an elevated blood pressure reading (defined below) at least 1 day before a documented diagnosis during the study period. Patients remained in the undiagnosed hypertension group until they were diagnosed with hypertension (see definition above) or until their last visit during the study period. Among patients with undiagnosed hypertension who eventually received a diagnosis, only 9.6% were diagnosed within the first month of their elevated blood pressure reading. Elevated blood pressure included: at least 1 blood pressure reading ≥160 mm Hg systolic or 100 mm Hg diastolic (stage 2 hypertension), 2 consecutive elevated blood pressure readings ≥140 mm Hg systolic or 90 mm Hg diastolic within 2 years of each other, or 2 consecutive elevated blood pressure readings ≥130 mm Hg systolic or 80 mm Hg diastolic within 2 years of each other for patients with a diagnosis for diabetes or chronic kidney disease.22 Patients with a documented diagnosis for white coat hypertension23 at any time before or during the study were excluded from the undiagnosed hypertension group (see Figure 1).
Patients with diagnosed hypertension without anti-hypertensive medication had a diagnosis of hypertension (documented problem list or visit diagnosis, N = 52,161) any time during the study period and were without a documented prescription for an anti-hypertensive medication for at least 1 day after a documented diagnosis. Patients remained in this group until they received a prescription for an anti-hypertensive medication or their last visit during the study period. Among patients with diagnosed hypertension without anti-hypertensive medication for at least 1 day, 17.0% received an anti-hypertensive prescription within the first month of their hypertension diagnosis. Because of data limitations, we focused only on anti-hypertension medications as a proxy for hypertension treatment as counseling or referral for lifestyle changes are not consistently available in EHR (see Figure 1).
Definition of health insurance coverage types
Our main independent variable of interest was health insurance coverage type during the time patients were either with undiagnosed hypertension or with diagnosed hypertension without anti-hypertensive medication. For the undiagnosed hypertension analysis, we used insurance from the date of the elevated blood pressure associated with the undiagnosed hypertension date to hypertension diagnosis date or end of the study period, whichever came first. For patients with diagnosed hypertension without anti-hypertensive medication, we utilized insurance coverage from the date of diagnosis to the first anti-hypertensive medication prescription date or end of the study period, whichever came first. Insurance types included continuously insured, continuously uninsured, gained insurance, or discontinuously insured, as described below:
Continuously insured patients had any type of health insurance (Medicaid or private insurance) at all visits during the time they had undiagnosed hypertension or were diagnosed with hypertension and without anti-hypertensive medication in the study period (2012–2017).
Continuously uninsured patients had no health insurance at any visit during the time they had undiagnosed hypertension or were diagnosed with hypertension and without anti-hypertensive medication in the study period (2012–2017).
Patients who gained insurance were uninsured at the first visit identifying them as having undiagnosed hypertension or as diagnosed with hypertension and without anti-hypertensive medication, but gained insurance (Medicaid or private insurance) at a subsequent visit, and kept health insurance for the remainder of their visits during the study period (2012–2017). Over 83% of patients who gained insurance were uninsured pre-ACA, and most gained Medicaid coverage post-ACA (80%).
Discontinuously insured patients fluctuated on and off health insurance throughout the time they had undiagnosed hypertension or were diagnosed with hypertension and without anti-hypertensive medication. In other words, some patients were uninsured at the first visit identifying them as having undiagnosed hypertension or with diagnosed hypertension without anti-hypertensive medication, were insured at a subsequent visit, and uninsured again at another follow-up visit. Other patients were insured at the first visit identifying them as having undiagnosed hypertension or with diagnosed hypertension without anti-hypertensive medication, and had subsequent visits that were either insured or uninsured.
Additional covariates included in our models were: age at the start of the study (19–26, 27–39, 40–59 years), sex (male, female), race (white, Black, other, unknown), ethnicity (Hispanic, non-Hispanic, unknown), number of visits to an eligible clinic during the undiagnosed hypertension or time without an anti-hypertensive for those diagnosed with hypertension, rurality (urban, urban cluster, rural, unknown), a modified Charlson comorbidity index score (0, 1–2, 3–5, 6+) that excluded hypertension diagnosis from the final score,24 and percent federal poverty level (≤138%, >138%, missing).
Statistical analysis
We summarized demographic characteristics of our CHC patient study population by hypertension status (no hypertension, diagnosed hypertension, undiagnosed hypertension, diagnosed hypertension without anti-hypertensive medication). We estimated the unadjusted prevalence of undiagnosed hypertension and of patients with diagnosed hypertension without anti-hypertensive medication by year and insurance type and reported those graphically.
Since provisions were established within the ACA that eliminated cost sharing for preventive care and a large number of patients gained insurance coverage after implementation of the ACA, we estimated time to diagnosis for undiagnosed hypertension and time to prescription among patients with diagnosed hypertension without anti-hypertensive medication in both the pre- and post-ACA periods using Cox proportional hazard models, adjusting for the covariates noted above. For each period (pre- and post-ACA), time to diagnosed hypertension was the time, in months, from the date they were first noted to have undiagnosed hypertension to a documented diagnosis. For those who never received a documented diagnosis, the censoring data point was set as their last visit to a study clinic. Time to prescription among patients with diagnosed hypertension without anti-hypertensive medication was the time, in months, from the first documented hypertension diagnosis until the first documented prescription for an anti-hypertensive medication. For patients who never received a documented anti-hypertensive medication prescription, it was the time until their last visit to a study clinic. For these analyses, gained insurance was the referent category, as we were interested in the effect of gaining insurance on diagnosis of hypertension and prescription of anti-hypertensive medications for patients with diagnosed hypertension compared with the other insurance types. Analyses were performed in SAS Enterprise Guide version 7.1 and Stata version 15.1. This study was approved by the Oregon Health & Science University Institutional Review Board. The data that support the findings of this study may be made available, upon reasonable request.
RESULTS
Overall, 37.3% of patients had undiagnosed hypertension for at least 1 day during the study period, and 27.0% of patients with diagnosed hypertension were without an anti-hypertensive medication for at least 1 day after their diagnosis. A greater percentage of patients with undiagnosed hypertension were male, non-Hispanic, lived in an urban cluster, and had continuous insurance compared with those with no hypertension. A greater percentage of patients with diagnosed hypertension without anti-hypertensive medication were Black, non-Hispanic, lived in rural areas, and were continuously insured (Table 1).
Table 1.
Patient characteristics by hypertension status
| No hypertension (N = 71,902) | Diagnosed hyperensiona (N = 54,797) | Undiagnosed hypertension (N = 20,462) | Diagnosed hypertension without anti-hypertensive medication (N = 11,102) | |
|---|---|---|---|---|
| Sex, % | ||||
| Male | 34.6 | 46.1 | 45.6 | 46.0 |
| Female | 65.4 | 53.9 | 54.4 | 54.0 |
| Age at study start, mean (SD) | 35.1 (10.4) | 44.1 (9.7) | 40.8 (10.3) | 44.6 (9.5) |
| Race, % | ||||
| White | 81.1 | 78.0 | 83.8 | 79.5 |
| Black | 8.9 | 13.9 | 8.0 | 12.7 |
| Other Race | 5.4 | 5.1 | 5.0 | 5.2 |
| Unknown Race | 4.6 | 3.0 | 3.3 | 2.6 |
| Ethnicity, % | ||||
| Non-Hispanic | 64.3 | 73.5 | 71.5 | 75.3 |
| Hispanic | 34.3 | 25.1 | 27.0 | 23.2 |
| Unknown | 1.4 | 1.5 | 1.5 | 1.5 |
| Federal poverty level, % | ||||
| ≤138% | 70.6 | 72.9 | 72.3 | 70.7 |
| >138% | 25.3 | 24.0 | 24.6 | 24.9 |
| Missing | 4.1 | 3.1 | 3.1 | 4.3 |
| Urban/rural location, % | ||||
| Urban | 72.5 | 71.4 | 64.4 | 68.1 |
| Urban cluster | 19.9 | 19.2 | 24.5 | 20.8 |
| Rural | 6.5 | 8.3 | 9.7 | 10.2 |
| Unknown | 1.1 | 1.1 | 1.4 | 0.9 |
| Ambulatory visits, mean (SD) | 11.5 (11.4) | 19.8 (18.0) | 19.8 (19.1) | 19.1 (17.5) |
| Charlson comorbidity index score 2012, % | ||||
| 0 | 62.0 | 35.3 | 37.2 | 37.4 |
| 1–2 | 17.3 | 27.8 | 27.8 | 26.8 |
| 3–5 | 17.3 | 29.0 | 27.4 | 28.3 |
| 6+ | 3.4 | 8.0 | 7.6 | 7.5 |
| Insurance groups, % | ||||
| Continuously insured | 42.6 | 40.7 | 56.8 | 54.4 |
| Continuously uninsured | 14.6 | 9.2 | 14.3 | 22.3 |
| Gained insurance | 21.9 | 27.5 | 12.9 | 9.0 |
| Discontinuously insured | 20.9 | 22.7 | 16.0 | 14.3 |
aInclude patients receiving care in community health centers with elevated blood pressure (never diagnosed = 13,666) or diagnosis of hypertension (n = 41,131) by the end of the study period (2012–2017). Patients with diagnosed hypertension without anti-hypertensive medication were those with a diagnosis of hypertension that did not have a documented prescription for a hypertension medication for at least 1 day. Patients with diagnosed hypertension without anti-hypertensive medication had a diagnosis of hypertension any time during the study period and were without a documented prescription for an anti-hypertensive medication for at least 1 day after a documented diagnosis. Patients remained in this group until they received a prescription for an anti-hypertensive medication or their last visit during the study period. Continuously uninsured patients had no health insurance at any visit during the time they had undiagnosed hypertension or were diagnosed with hypertension and without anti-hypertensive medication in the study period (2012–2017). Patients who gained insurance were uninsured at the first visit identifying them as diagnosed with hypertension and without anti-hypertensive medication but gained insurance at a subsequent visit, and kept health insurance for the remainder of their visits during the study period (2012–2017). Discontinuously insured patients fluctuated on and off health insurance throughout the time they had undiagnosed hypertension or were diagnosed with hypertension and without anti-hypertensive medication.
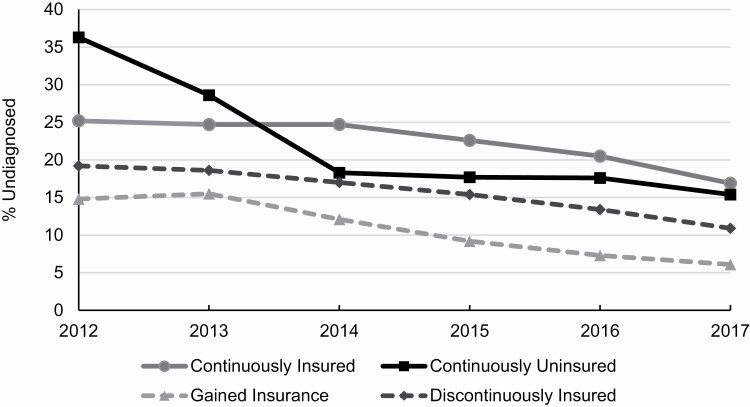
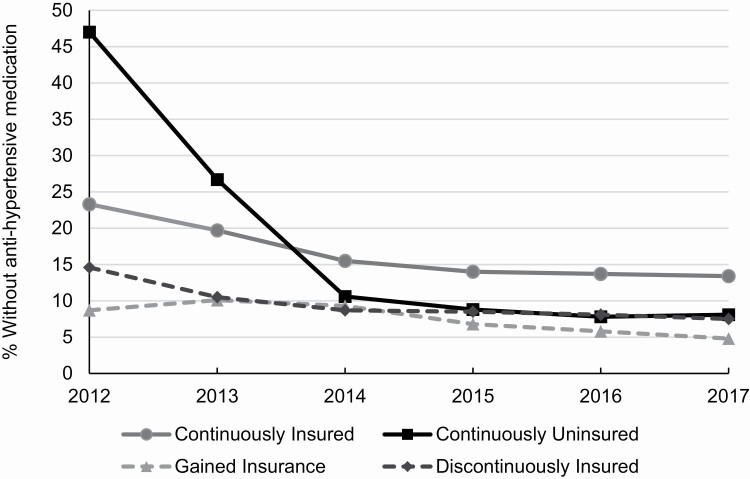
The rate of undiagnosed hypertension steadily decreased from 2012 (22.4%) through 2017 (12.9%). These trends were seen across all insurance types (Figure 2). Those who gained insurance had the lowest rate of undiagnosed hypertension in all years. Those who were continuously uninsured had the highest rate of undiagnosed hypertension at the start of the study period, but saw the largest decline in rate over the study period, a 20.9 percentage point drop. Among patients with undiagnosed hypertension at any point in the study period, 24.9% remained undiagnosed at the end of the study period. A significantly greater percentage of continuously insured patients never received a diagnosis (31.1%) compared with the other insurance types (25.9% for continuously uninsured, 22.1% for discontinuously insured, and 14.5% for gained insurance; results not shown). Rates of patients with diagnosed hypertension without anti-hypertensive medication decreased across all insurance groups (Figure 3); with uninsured experienced the largest decline. Among patients with diagnosed hypertension without anti-hypertensive medication, 8.4% remained without a documented prescription at the end of the study period.
Figure 2.
Trends in the proportions of patients with undiagnosed hypertension by insurance type, 2012–2017. Patients with diagnosed hypertension without anti-hypertensive medication were those with a diagnosis of hypertension that did not have a documented prescription for a hypertension medication for at least 1 day. Continuously insured patients had any type of health insurance (Medicaid or private insurance) at all visits during the time they had undiagnosed hypertension in the study period (2012–2017). Continuously uninsured patients had no health insurance at any visit during the time they had undiagnosed hypertension in the study period (2012–2017). Patients who gained insurance were uninsured at the first visit identifying them as having undiagnosed hypertension but gained insurance (Medicaid or private insurance) at a subsequent visit, and kept health insurance for the remainder of their visits during the study period (2012–2017). Discontinuously insured patients fluctuated on and off health insurance throughout the time they had undiagnosed hypertension.
Figure 3.
Trends in the proportions of patients with diagnosed hypertension without anti-hypertensive medication by insurance type, 2012–2017. Patients with diagnosed hypertension without anti-hypertensive medication had a diagnosis of hypertension any time during the study period and were without a documented prescription for an anti-hypertensive medication for at least 1 day after a documented diagnosis. Patients remained in this group until they received a prescription for an anti-hypertensive medication or their last visit during the study period. Continuously insured patients had any type of health insurance (Medicaid or private insurance) at all visits during the time they were diagnosed with hypertension and without anti-hypertensive medication in the study period (2012–2017). Continuously uninsured patients had no health insurance at any visit during the time they were diagnosed with hypertension and without anti-hypertensive medication in the study period (2012–2017). Patients who gained insurance were uninsured at the first visit identifying them as diagnosed with hypertension and without anti-hypertensive medication but gained insurance (Medicaid or private insurance) at a subsequent visit, and kept health insurance for the remainder of their visits during the study period (2012–2017). Discontinuously insured patients fluctuated on and off health insurance throughout the time they were diagnosed with hypertension and without anti-hypertensive medication.
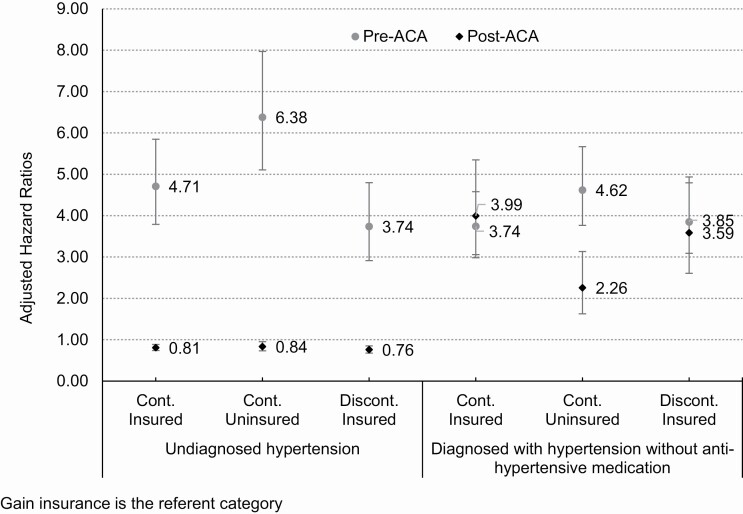
In the pre-ACA period, the time to diagnosis among patients with undiagnosed hypertension was longer for those who gained insurance than it was for patients in all other insurance types (Figure 4 and Supplementary Table S1 online). For instance, those continuously insured received a diagnosis 4 times faster than those who gained insurance (hazard ratio = 4.71; 95% confidence interval = 3.79–5.85). In the post-ACA period, the time to diagnosis was shorter for those who gained insurance than it was for the other insurance types. Time to hypertension diagnosis in both the pre- and post-ACA periods was shorter for those who were female, older, non-Hispanic, and had fewer visits. Time to diagnosis was shorter for Black than white patients in the post-ACA period (Supplementary Table S1 online). Additionally, there was some indication that those who were more medically complex (measured via the Charlson comorbidity index score) had a faster time to hypertension diagnosis pre-ACA, but these differences disappeared in the post-ACA period.
Figure 4.
Adjusted time to diagnosis among undiagnosed hypertension and those with diagnosed hypertension without anti-hypertensive medication pre- and post-ACA by insurance type. Hazard ratios were adjusted for sex, ethnicity, race, age at the study starts, urban/rural location, number of visits, Charlson comorbidity index score, and federal poverty level. Error bars represent the 95% confidence intervals. Referent insurance type is gained insurance. Time to diagnosed hypertension was the time, in months, from the date of their elevated blood pressure to a documented diagnosis. For those who never had a documented diagnosis, it was the time until their last visit to a study clinic. Time to prescription among patients with diagnosed hypertension without anti-hypertensive medication was the time, in months, from the first documented hypertension diagnosis until the first documented prescription for an anti-hypertensive medication. For patients who never received a documented anti-hypertensive medication, it was the time until their last visit to a study clinic. Continuously insured (Cont. Ins) patients had any type of health insurance at all visits during the time they had undiagnosed hypertension or were diagnosed with hypertension and without anti-hypertensive medication in the study period (2012–2017). Continuously uninsured (Cont. Unins) patients had no health insurance at any visit during the time they had undiagnosed hypertension or were diagnosed with hypertension and without anti-hypertensive medication in the study period (2012–2017). Discontinuously insured (Discont. Ins) patients fluctuated on and off health insurance throughout the time they had undiagnosed hypertension or were diagnosed with hypertension and without anti-hypertensive medication. Abbreviation: ACA, Affordable Care Act.
Among patients with diagnosed hypertension without anti-hypertension medication, the time to anti-hypertensive medication prescription was significantly longer for patients who gained insurance in both the pre- and post-ACA periods compared with other insurance types, after adjusting for covariate. In both the pre- and post-ACA periods, the time to anti-hypertensive medication prescription was longer for men, patients who were less medically complex, those with more visits, and patients with a higher federal poverty level compared with their counterparts. In the pre-ACA period, time to anti-hypertensive medication prescription was longer for younger patients. In the post-ACA period, time to anti-hypertensive medication prescription was longer for Hispanic than non-Hispanic patients (Supplementary Table S1 online).
Discussion
The purpose of this study was to evaluate the impact of gaining insurance on rates of undiagnosed hypertension and anti-hypertensive medication prescriptions among patients with lower income receiving care in CHCs. Our findings are consistent with other studies that showed CHC patients and CHCs themselves benefited from the ACA.25,26 We observed that the prevalence of undiagnosed hypertension decreased over time, and decreased more rapidly following the ACA Medicaid expansion. Further, the differences between insurance types among patients with undiagnosed hypertension were significantly reduced post-ACA, suggesting that patients who gained insurance were more likely to get a diagnosis post-compared with pre-ACA. Post-ACA, the time to hypertension diagnosis was shorter for patients who gained insurance than other insurance types. These results showcase the importance of supporting and sustaining health insurance expansion to ensure detection of chronic conditions among low-income individuals. This is particularly relevant following the COVID-19 pandemic, which led to a dramatic increase in unemployment likely associated with substantial losses of health insurance. As such, reductions in barriers to obtaining health insurance, such as the Medicaid expansion, are critical. Our findings also stress the need to expand health insurance access to those who remain uninsured to ensure they are able to receive timely diagnoses and treatment. One possible strategy is universal health care coverage for all.
Regarding patients with diagnosed hypertension without anti-hypertensive medication, those without insurance showed the greatest improvement in receiving prescriptions for anti-hypertensive medication when needed. This is likely because patients without insurance seen in CHCs benefit from the 340B drug pricing program,27 which allows clinics, hospitals, and affiliated pharmacies to obtain drugs at a significant discount and reduce the cost burden for patients. Although this program is available to all patients regardless of insurance status, it is critical for patients without insurance who might not otherwise be able to afford needed prescriptions. Following the ACA, this program grew, but especially so in Medicaid expansion states, which might explain the large decline in uninsured patients with diagnosed hypertension without anti-hypertensive medication. However, the US Centers for Medicare and Medicaid Services proposed to cut the program in 2020 by 22.5%,28 which could impact CHCs’ ability to assist patients who are uninsured or unstably insured with their medication needs. The continuity of this program and other medication cost containment efforts are imperative in the wake of the COVID-19 pandemic.
Although clinicians play a leading role in whether a patient receives a hypertension diagnosis or an anti-hypertensive medication prescription, there are many multilevel factors influencing diagnoses and treatment. For example, diagnosis is influenced by clinic workflows and how high blood pressure readings are communicated to the clinician prior to them seeing the patient. Treatment is influenced by whether or not a patient prefers to take a medication or prioritize nonpharmacological treatments. Importantly, the COVID-19 pandemic physical distancing policies and regulations may have had a large impact on the ability of clinics to screen for and document blood pressure readings and/or provide patients with timely treatment. Thus, more research is needed to understand the impact of COVID-19 on blood pressure screenings and health care utilization for hypertension treatment. Although health insurance facilitates access to care and treatment, it is only one of the many factors influencing when a chronic condition is diagnosed and what options are recommended for treating it.29
Our results highlight several demographic (race and ethnicity) and health-related factors (medical complexity and number of visits) that may influence receipt of a hypertension diagnosis and/or a prescription once diagnosed. We found that Hispanic patients experienced a longer time to diagnosis and treatment than non-Hispanic patients, while Black patients received diagnoses and prescriptions more rapidly than all other races. These results suggest that Hispanic CHC patients may experience unique barriers to hypertension diagnosis and treatment. We found that Hispanic patients were more likely to be uninsured pre-ACA and to remain uninsured post-ACA,30 which impacts health care access. Other studies focused on evaluating the barriers to hypertension treatment and control among Hispanic patients found income, ancestry, health literacy, access to transportation, family support, and physician communication skills impeded health care;19,29,31–33 we could not measure these factors with our data. We also found that patients with undiagnosed hypertension or with diagnosed hypertension without anti-hypertensive medication have medical complexity and numerous health care visits, suggesting competing health conditions may gain priority for time and attention34,35—leaving hypertension unaddressed, especially among continuously insured and those who gained insurance.
Additional mixed-methods research is needed to understand the barriers and facilitators to diagnosis and treatment of hypertension, especially among Hispanic populations, and identify strategies to improve adequate receipt of recommended care. For instance, there are numerous EHR tools21,36,37 and other population health tactics that successfully identify undiagnosed patients that could be implemented in CHCs. Other strategies may include recruiting a team to monitor a registry of patients with a hypertension diagnosis or consistently high blood pressure measurements; this team could expand beyond the clinician to include others, such as community health workers or patient navigators to assist with medication management and clinical pharmacists to reduce polypharmacy risk. Another approach could be to focus on cultural competency training, provider–patient communication, and increasing patient knowledge of health care benefits, wellness, and illness.
This study has some limitations: it includes CHCs who are part of the OCHIN community health network and therefore results may not be representative of all clinics, states, or expansion groups. This analysis is visit-based and does not assess the CHC population without visits and health insurance status is based on insurance at each visit. Inaccurate blood pressure measurements recorded in the EHR may have inaccurately categorized patients.38,39 Additionally, patients may seek care outside CHCs; however, evidence suggests that most established CHC patients continue to receive care from CHCs.40
In conclusion, those who gained health insurance had greater improvement in getting diagnosed with hypertension post-ACA than other insurance types. No such relationship was observed among patients with diagnosed hypertension without anti-hypertensive medication. More research is needed to untangle the barriers to hypertension diagnosis and treatment in CHC populations.
Supplementary Material
ACKNOWLEDGMENTS
OCHIN EHR data were from the Accelerating Data Value Across a National Community Health Center Network (ADVANCE) Clinical Research Network (CRN). OCHIN leads the ADVANCE network in partnership with Health Choice Network, Fenway Health, and Oregon Health & Science University. ADVANCE is funded through the Patient-Centered Outcomes Research Institute (PCORI), contract number RI-CRN-2020-001. The authors acknowledge the participation of our partnering community health centers. The views presented in this article are solely the responsibility of the authors and do not necessarily represent the views of the funding agencies.
FUNDING
This publication was supported by the National Health, Lung, and Blood Institute grant number R01HL136575 and by the National Cancer Institute grant number R01CA204267.
DISCLOSURE
The authors declared no conflict of interest.
REFERENCES
- 1. Forouzanfar MH, Liu P, Roth GA, Ng M, Biryukov S, Marczak L, Alexander L, Estep K, Hassen Abate K, Akinyemiju TF, Ali R, Alvis-Guzman N, Azzopardi P, Banerjee A, Bärnighausen T, Basu A, Bekele T, Bennett DA, Biadgilign S, Catalá-López F, Feigin VL, Fernandes JC, Fischer F, Gebru AA, Gona P, Gupta R, Hankey GJ, Jonas JB, Judd SE, Khang YH, Khosravi A, Kim YJ, Kimokoti RW, Kokubo Y, Kolte D, Lopez A, Lotufo PA, Malekzadeh R, Melaku YA, Mensah GA, Misganaw A, Mokdad AH, Moran AE, Nawaz H, Neal B, Ngalesoni FN, Ohkubo T, Pourmalek F, Rafay A, Rai RK, Rojas-Rueda D, Sampson UK, Santos IS, Sawhney M, Schutte AE, Sepanlou SG, Shifa GT, Shiue I, Tedla BA, Thrift AG, Tonelli M, Truelsen T, Tsilimparis N, Ukwaja KN, Uthman OA, Vasankari T, Venketasubramanian N, Vlassov VV, Vos T, Westerman R, Yan LL, Yano Y, Yonemoto N, Zaki ME, Murray CJ. Global burden of hypertension and systolic blood pressure of at least 110 to 115 mm Hg, 1990–2015. JAMA 2017; 317:165–182. [DOI] [PubMed] [Google Scholar]
- 2. Centers for Disease Control and Prevention (CDC). Hypertension Cascade: Hypertension Prevalence, Treatment and Control Estimates Among US Adults Aged 18 Years and Older Applying the Criteria from the American College of Cardiology and American Heart Association’s 2017 Hypertension Guideline—NHANES 2013–2016. Atlanta, GA: US Department of Health and Human Services; 2019. [Google Scholar]
- 3. Virani SS, Alonso A, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP, Chamberlain AM, Chang AR, Cheng S, Delling FN, Djousse L, Elkind MSV, Ferguson JF, Fornage M, Khan SS, Kissela BM, Knutson KL, Kwan TW, Lackland DT, Lewis TT, Lichtman JH, Longenecker CT, Loop MS, Lutsey PL, Martin SS, Matsushita K, Moran AE, Mussolino ME, Perak AM, Rosamond WD, Roth GA, Sampson UKA, Satou GM, Schroeder EB, Shah SH, Shay CM, Spartano NL, Stokes A, Tirschwell DL, VanWagner LB, Tsao CW; American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee . Heart disease and stroke statistics—2020 update: a report from the American Heart Association. Circulation 2020; 141:e139–e596. [DOI] [PubMed] [Google Scholar]
- 4. Muntner P, Hardy ST, Fine LJ, Jaeger BC, Wozniak G, Levitan EB, Colantonio LD. Trends in blood pressure control among US adults with hypertension, 1999–2000 to 2017–2018. JAMA 2020; 324:1190–1200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Wall HK, Hannan JA, Wright JS. Patients with undiagnosed hypertension: hiding in plain sight. JAMA 2014; 312:1973–1974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. World Health Organization. A Global Brief on Hypertension: Silent Killer, Global Public Health Crisis. Geneva, Switzerland: WHO Press; 2013. [Google Scholar]
- 7. Ayanian JZ, Weissman JS, Schneider EC, Ginsburg JA, Zaslavsky AM. Unmet health needs of uninsured adults in the United States. JAMA 2000; 284:2061–2069. [DOI] [PubMed] [Google Scholar]
- 8. He J, Muntner P, Chen J, Roccella EJ, Streiffer RH, Whelton PK. Factors associated with hypertension control in the general population of the United States. Arch Intern Med 2002; 162:1051–1058. [DOI] [PubMed] [Google Scholar]
- 9. Gillespie CD, Hurvitz KA; Centers for Disease Control and Prevention (CDC) . Prevalence of hypertension and controlled hypertension—United States, 2007–2010. MMWR Suppl 2013; 62:144–148. [PubMed] [Google Scholar]
- 10. Paulose-Ram R, Gu Q, Kit B. Characteristics of U.S. adults with hypertension who are unaware of their hypertension, 2011–2014. NCHS Data Brief 2017; 278:1–8. [PubMed] [Google Scholar]
- 11. Ayanian JZ, Zaslavsky AM, Weissman JS, Schneider EC, Ginsburg JA. Undiagnosed hypertension and hypercholesterolemia among uninsured and insured adults in the Third National Health and Nutrition Examination Survey. Am J Public Health 2003; 93:2051–2054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Angier H, Ezekiel-Herrera D, Marino M, Hoopes M, Jacobs EA, DeVoe JE, Huguet N. Racial/ethnic disparities in health insurance and differences in visit type for a population of patients with diabetes after Medicaid expansion. J Health Care Poor Underserved 2019; 30:116–130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Huguet N, Angier H, Rdesinski R, Hoopes M, Marino M, Holderness H, DeVoe JE. Cervical and colorectal cancer screening prevalence before and after Affordable Care Act Medicaid expansion. Prev Med 2019; 124:91–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kaufman HW, Chen Z, Fonseca VA, McPhaul MJ. Surge in newly identified diabetes among Medicaid patients in 2014 within Medicaid expansion states under the Affordable Care Act. Diabetes Care 2015; 38:833–837. [DOI] [PubMed] [Google Scholar]
- 15. Wherry LR, Miller S. Early coverage, access, utilization, and health effects associated with the Affordable Care Act Medicaid expansions: a quasi-experimental study. Ann Intern Med 2016; 164:795–803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Huguet N, Springer R, Marino M, Angier H, Hoopes M, Holderness H, DeVoe JE. The impact of the Affordable Care Act (ACA) Medicaid expansion on visit rates for diabetes in safety net health centers. J Am Board Fam Med 2018; 31:905–916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hogan DR, Danaei G, Ezzati M, Clarke PM, Jha AK, Salomon JA. Estimating the potential impact of insurance expansion on undiagnosed and uncontrolled chronic conditions. Health Aff (Millwood) 2015; 34:1554–1562. [DOI] [PubMed] [Google Scholar]
- 18. Fang J, Wang G, Ayala C, Lucido SJ, Loustalot F. Healthcare access among young adults: impact of the Affordable Care Act on young adults with hypertension. Am J Prev Med 2017; 53:S213–S219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Zhang D, Ritchey MR, Park C, Li J, Chapel J, Wang G. Association between Medicaid coverage and income status on health care use and costs among hypertensive adults after enactment of the Affordable Care Act. Am J Hypertens 2019; 32:1030–1038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Devoe JE, Sears A. The OCHIN community information network: bringing together community health centers, information technology, and data to support a patient-centered medical village. J Am Board Fam Med 2013; 26:271–278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Meador M, Osheroff JA, Reisler B. Improving identification and diagnosis of hypertensive patients hiding in plain sight (HIPS) in health centers. Jt Comm J Qual Patient Saf 2018; 44:117–129. [DOI] [PubMed] [Google Scholar]
- 22. American Diabetes Association. Cardiovascular disease and risk management: standards of medical care in diabetes—2018. Diabetes Care 2018; 41(Suppl 1):S86–S104. [DOI] [PubMed] [Google Scholar]
- 23. Viera AJ, Shimbo D. Ambulatory blood pressure phenotypes and the risk for hypertension. Curr Hypertens Rep 2014; 16:481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Charlson ME, Charlson RE, Peterson JC, Marinopoulos SS, Briggs WM, Hollenberg JP. The Charlson comorbidity index is adapted to predict costs of chronic disease in primary care patients. J Clin Epidemiol 2008; 61:1234–1240. [DOI] [PubMed] [Google Scholar]
- 25. Tilhou AS, Huguet N, DeVoe J, Angier H. The Affordable Care Act Medicaid expansion positively impacted community health centers and their patients. J Gen Intern Med 2020; 35:1292–1295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Paradise J, Rosenbaum S, Markus A, Sharac J, Tran C, Reynolds D. The Henry J. Kaiser Family Foundation. Community Health Centers: Recent Growth and the Role of the ACA. January 2017. https://www.kff.org/medicaid/issue-brief/community-health-centers-recent-growth-and-the-role-of-the-aca/. [Google Scholar]
- 27.McCaughan, M. The 340B Drug Discount Program, Health Affairs Health Policy Brief, September 14, 2017 (doi: 10.1377/hpb20171024.663441). [DOI] [Google Scholar]
- 28.US Department of Health and Human Services, Baltimore, MD. Available at https://www.govinfo.gov/content/pkg/FR-2019-11-12/pdf/2019-24138.pdf. [DOI] [PubMed] [Google Scholar]
- 29. Arredondo A, Recaman AL. New coverage schemes in health, income level, costs, and use of services in the management of hypertension. Am J Hypertens 2019; 32:932–934. [DOI] [PubMed] [Google Scholar]
- 30. Huguet N, Valenzuela S, Marino M, Angier H, Hatch B, Hoopes M, DeVoe JE. Following uninsured patients through Medicaid expansion: ambulatory care use and diagnosed conditions. Ann Fam Med 2019; 17:336–344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Borrell LN, Crawford ND. Disparities in self-reported hypertension in Hispanic subgroups, non-Hispanic black and non-Hispanic white adults: the National Health Interview Survey. Ann Epidemiol 2008; 18:803–812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Kendrick J, Nuccio E, Leiferman JA, Sauaia A. Primary care providers perceptions of racial/ethnic and socioeconomic disparities in hypertension control. Am J Hypertens 2015; 28:1091–1097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Lor M, Koleck TA, Bakken S, Yoon S, Dunn Navarra AM. Association between health literacy and medication adherence among Hispanics with hypertension. J Racial Ethn Health Disparities 2019; 6: 517–524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Angier H, Gregg J, Gold R, Crawford C, Davis M, DeVoe JE. Understanding how low-income families prioritize elements of health care access for their children via the optimal care model. BMC Health Serv Res 2014; 14:585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Bailey SR, O’Malley JP, Gold R, Heintzman J, Marino M, DeVoe JE. Receipt of diabetes preventive services differs by insurance status at visit. Am J Prev Med 2015; 48:229–233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Rakotz MK, Ewigman BG, Sarav M, Ross RE, Robicsek A, Konchak CW, Gavagan TF, Baker DW, Hyman DJ, Anderson KP, Masi CM. A technology-based quality innovation to identify undiagnosed hypertension among active primary care patients. Ann Fam Med 2014; 12:352–358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Ciemins EL, Ritchey MD, Joshi VV, Loustalot F, Hannan J, Cuddeback JK. Application of a tool to identify undiagnosed hypertension—United States, 2016. MMWR Morb Mortal Wkly Rep 2018; 67:798–802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Muntner P, Einhorn PT, Cushman WC, Whelton PK, Bello NA, Drawz PE, Green BB, Jones DW, Juraschek SP, Margolis KL, Miller ER III, Navar AM, Ostchega Y, Rakotz MK, Rosner B, Schwartz JE, Shimbo D, Stergiou GS, Townsend RR, Williamson JD, Wright JT Jr, Appel LJ; 2017 National Heart, Lung, and Blood Institute Working Group . Blood pressure assessment in adults in clinical practice and clinic-based research: JACC Scientific Expert Panel. J Am Coll Cardiol 2019; 73:317–335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Ringrose J, Padwal R. The ongoing saga of poor blood pressure measurement: past, present, and future perspectives. J Clin Hypertens (Greenwich) 2017; 19:611–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Huguet N, Kaufmann J, O’Malley J, Angier H, Hoopes M, DeVoe JE, Marino M. Using electronic health records in longitudinal studies: estimating patient attrition. Med Care 2020; 58(Suppl 6, Suppl 1):S46–S52. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.