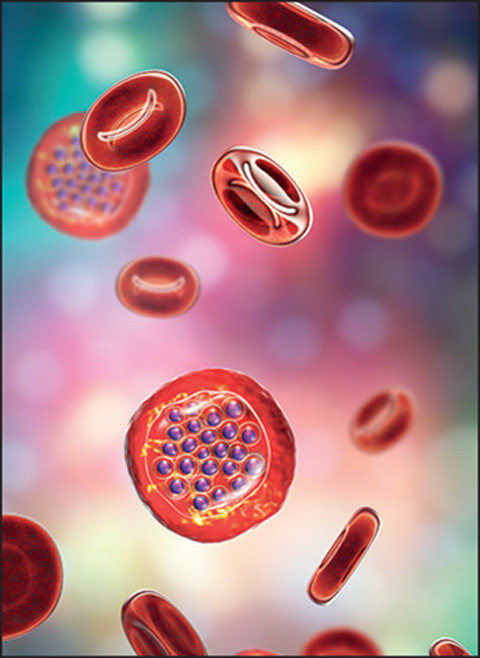
As we reported in an Editorial in January, the goals set to reduce malaria incidence and mortality by 2030 seem unlikely to be met at current rates of progress. Furthermore, COVID-19 could have a damaging effect on malaria control by delaying prevention measures designed to combat seasonal peaks in disease transmission. However, amid concerns about missed targets and pandemic setbacks, recent results of clinical trials offer hope for reinvigorating the malaria response.
Firstly, a trial done among young children in Burkina Faso and Mali, where malaria is seasonal, and published in the New England Journal of Medicine on Aug 25, 2021, showed a striking reduction in malaria when chemoprevention was combined with vaccination against malaria. Daniel Chandramohan and colleagues randomly assigned children aged 5–17 months to chemoprevention alone with sulfadoxine–pyrimethamine and amodiaquine, vaccination alone with RTS,S/AS01, or a combination of the two interventions. About 2000 children in each group received at least the first dose of their assigned intervention and were followed up for 3 years. The primary outcome was incidence of uncomplicated clinical malaria. Overall, there were 1661 cases of malaria in the chemoprevention-alone group, 1540 in the vaccine-alone group, and 624 in the combined intervention group. These incidences equated to protective efficacies of 62·8% and 59·6% for the combination versus chemoprevention alone and vaccination alone, respectively. Findings were similar in Burkina Faso and Mali, although the protective efficacy of the combination did reduce somewhat between year 1 and year 3 of follow-up. Compared with either intervention alone, the protective efficacies of the combination against hospital admission for severe malaria and against death from malaria were at least 70%.
A second promising set of results came from a trial, also done in Burkina Faso, of a new vaccine against malaria and published in The Lancet on May 5, 2021, by Mehreen Datoo and colleagues. Children aged 5–17 months were randomly assigned to receive 5 μg of the circumsporozoite protein-based vaccine R21, plus either 25 μg or 50 μg of the adjuvant Matrix-M (MM), or to a placebo of rabies vaccine. Three vaccine doses were given at 4-week intervals before the malaria season, followed by a fourth dose 1 year later. 150 children in each group received at least one vaccine dose, and the primary objective was R21 vaccine protective efficacy against clinical malaria from 2 weeks after the third dose to 6 months. At 6 months, 43 (29%) of 146 participants in the R21/25 μg MM group, 38 (26%) of 146 in the R21/50 μg MM group, and 105 (71%) of 147 in the placebo group had developed clinical malaria, giving vaccine efficacies of 74% and 77% in low-dose and high-dose adjuvant groups, respectively. Whether efficacy will be sustained over a second malaria season is being assessed in a continuation of the trial.
A final—and far more preliminary—set of promising findings come from a phase 1 trial of an antimalarial monoclonal antibody called CIS43LS, published by Martin Gaudinski and colleagues in the New England Journal of Medicine on Aug 26, 2021. The primary objective was to assess safety and pharmacokinetics among 25 healthy volunteers, but some participants were challenged with malaria after CIS43LS administration. Up to 21 days after malaria infection, five of six participants who did not receive CIS43LS had parasitaemia compared with none of the nine who had been given monoclonal antibody.
Given issues around cost and distribution, routine monoclonal antibody prophylaxis might not be feasible in countries where malaria is most common, although a clinical trial of CIS43LS underway in Mali will address these issues. Similarly, a phase 3 clinical trial of R21/MM, scheduled to recruit 4800 children, will determine the efficacy of the vaccine at five African sites with differing malaria patterns. The combination intervention seems the most likely candidate for routine implementation, but whether protective efficacy is sustained over several years or the intervention is appropriate in settings of year-round, endemic transmission are unknown.
Malaria is a disease that has been treatable and preventable since at least the middle of the last century. Having the tools to do the job is less of an issue than having the finance and infrastructure to get drugs, bednets, and insecticides to the people and places that need them. When the COVID-19 pandemic fades, politicians and policy makers must renew efforts to minimise, and perhaps eliminate, an ancient disease for which we have a promising new set of interventions at-hand.
For the NEJM combination prevention article see N Engl J Med 2021; published online Aug 25. https://doi.org/10.1056/NEJMoa2026330
For the NEJM monoclonal antibody article see N Engl J Med 2021; 385: 803–14
© 2021 iStock


