PURPOSE:
During the COVID-19 surge months of March and April 2020, our New York multicenter health system experienced an influx of cases with COVID-19. We sought to study the impact of the surge period on patients with cancer prescribed radiation treatment (RT).
METHODS:
We reviewed our secure departmental quality assurance database for all patients who underwent RT planning simulations from March 6, 2020, through April 30, 2020. A priority level between 1 and 3 was prospectively assigned to each case based on faculty consensus to determine which patients required immediate RT. In May 2020, each faculty physician again retrospectively reviewed their patients from the database and provided additional commentary on how the COVID-19 pandemic had affected each patient's care. All statistics are descriptive.
RESULTS:
A total of 412 RT courses in 406 unique patients were simulated for linear accelerator–based external beam RT. The median age was 66 years. Treatment intent was curative in 70.6% and palliative in 29.4%. Of the 412 cases, 66.7% were priority 1, 25% priority 2, and 7.8% priority 3. Two hundred thirty-nine cases (58%) underwent standard-of-care diagnosis, workup, and treatment plan. Seventeen patients (4.1%) electively canceled their RT, and 17 others (4.1%) electively delayed RT start. Thirty-four (8.3%) were prescribed hypofractionation to shorten their RT course, and 22 (5.3%) had a change in modality. Incomplete or delayed workup was identified in 19 cases (4.6%).
CONCLUSION:
The COVID-19 pandemic surge resulted in 42% of our patients having a non–standard-of-care pathway. This outcome demonstrates a significant impact of the COVID-19 crisis on routine cancer care.
INTRODUCTION
Since December 2019, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)1 and its associated COVID-19 have led to a pandemic unprecedented in modern times. The pandemic has caused considerable morbidity, mortality, and healthcare resource strain.2 The New York area had its first confirmed case of COVID-19 on March 1, 2020; as of June 5, 2020, New York has confirmed 376,200 cases and 24,175 deaths.3
Our institution is the largest healthcare provider in New York State and based around the New York Metropolitan area. Most of our hospitals experienced a surge of COVID-19 cases, and throughout our health system, all nonemergent surgeries and procedures were temporarily canceled from mid-March to mid-May to provide capacity for COVID-19-related hospital admissions. Because delays in oncology care for many malignancies can pose worse survival and quality of life outcomes, efforts were made to triage patients and deliver standard-of-care (SOC) when possible. However, this had to be balanced with the knowledge that this patient population generally is older, may be immunosuppressed, and experiences an increased rate of SARS-CoV-2 infection and COVID-19 morbidity.4-10
In our department, we established two over-riding principles: (1) to maintain the safety of all staff and patients and (2) to maintain access for those patients requiring radiotherapy services. Our department implemented early policies to promote safety of staff and patients. These include physical distancing, use of telehealth, conversion to shorter fractionation schedules, prioritization of cases for treatment start, deferment of some treatments, use of alternate or safer treatment modalities, and a strict hospital avoidance guideline for care.21 Referring to working guidelines provided by oncology societies and institutions,11-15 we prioritized patients based on urgency to start and, where possible, suggested an abbreviated course of treatment.
In this study, we sought to analyze the impact of the COVID-19 pandemic on 412 radiation therapy (RT) courses among 406 patients, encompassing March and April 2020. Specifically, we review details of how care deviated from SOC practice in response to the pandemic.
METHODS
Quality and safety are critically important for the delivery of RT and are cornerstones of our previously reported Smarter Radiation Oncology program.16,17 As part of our departmental culture, new patient radiation cases are peer-reviewed in prospective daily contouring rounds before treatment planning begins.18,19 Our departmental quality assurance (QA) program also tracks data on patient hospitalization and discontinuation of RT.20
Prioritization System
A tiered system of prioritization was developed to stagger radiation starts and purposefully reduce machine treatment volume.21,22 We classified cases as follows: priority 1 includes patients who need treatment immediately, priority 2 can begin within 30 days, and priority 3 can begin beyond 30 days. Twenty faculty physicians from 10 radiation facilities met virtually on two separate occasions, March 20 and April 3, 2020, to prospectively determine the urgency and priority of all pending RT cases, including pending simulations and treatment starts. Group consensus was required to assign each patient's priority. Priority decisions were communicated to the patient by the departmental supervisors or by the attending physician. When patients were in priority 2 or 3 categories, we took great efforts to explain the rationale for treatment delay and to reassure the patient that treatment delay would likely not affect their outcome. After those initial meetings, all cases presented at our daily peer-review rounds required a priority assignment before proceeding to treatment planning.
Data Collection and Statistics
We reviewed our secure departmental QA database for all patients who underwent radiation planning computed tomography simulations (CT sim) from March 6, 2020, through April 30, 2020. Data included in the QA database included name, age, date of birth, diagnosis, disease site, treatment intent, radiation prescription (dose, fractionation, and energy), plan type, priority score, and any other comments at the time of peer-review rounds. This study was approved under the Northwell Health COVID-19 Research Policy Institutional Review Board protocol for noninterventional research. In early May 2020, we asked each faculty physician to review their patients from the database and comment in detail on how the COVID-19 pandemic had affected patient care. We performed this step to collect additional clinical details regarding the case that were not available in the QA database. Possible comments on each case included the following categories: change in fractionation, change in treatment modality, inadequate or delayed workup, delay in simulation or radiation start, treatment cancellation, or no change. These comments were further categorized into those that were patient-driven versus physician or department-driven. All statistics are descriptive.
RESULTS
Demographics
A total of 412 radiation treatment courses were simulated in 406 patients for linear accelerator–based external beam RT during this time period (Table 1). The median age was 66 years (range, 11-93). Treatment intent was curative in 70.6% and palliative in 29.4%. Most common disease sites were breast (19.9%), metastasis (19.9%), head and neck (H&N, 14.0%), genitourinary (9.5%), lungs (9.0%), gynecologic (8.7%), GI (8.0%), and brain (6.8%).
TABLE 1.
Characteristics of Radiation Therapy Cases During Coronavirus Disease 2019 Surge
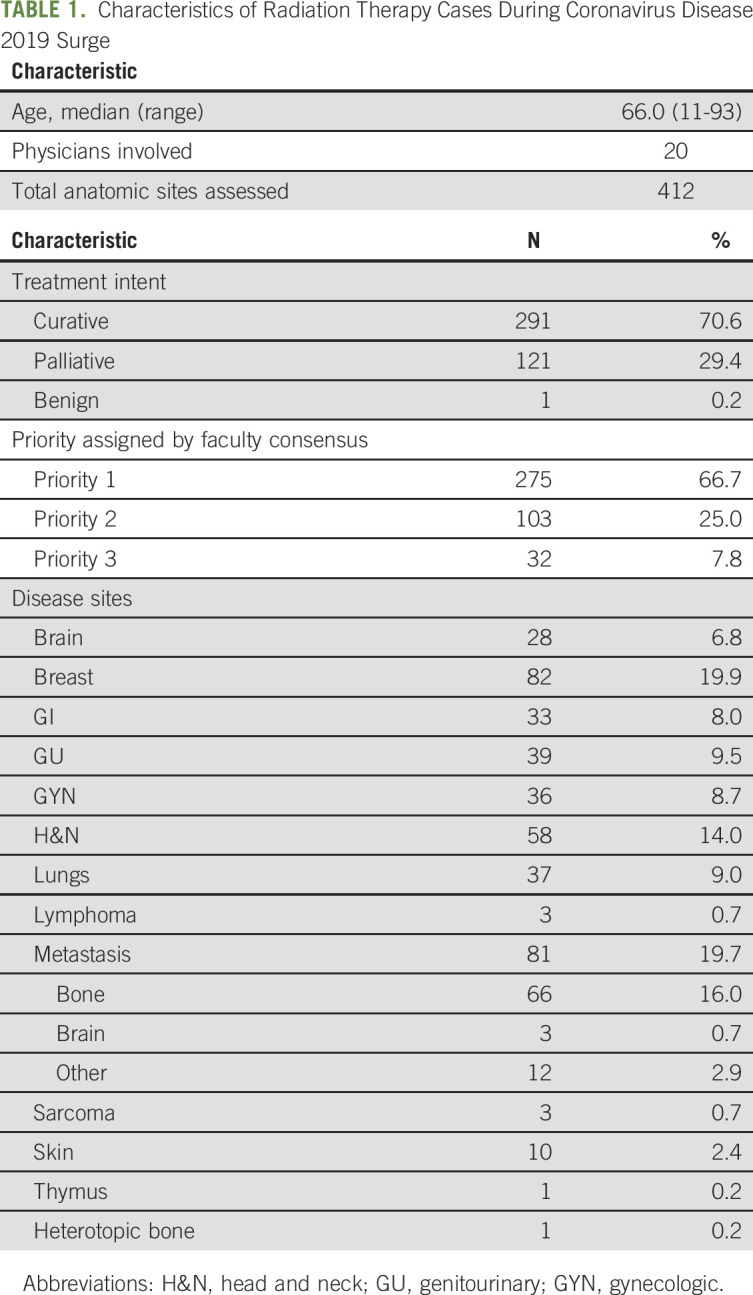
Prioritization of Cases
Of the 412 cases identified and discussed among the faculty, 66.7% were categorized as priority 1, 25% priority 2, and 7.8% priority 3 (Table 1). The median time from consultation visit to CT sim was 5.0 days (range, 1-120) for priority 1, 8.0 days (range, 1-121) for priority 2, and 14.5 days (range, 1-125) for priority 3. The median time from CT sim to RT start was 10 days (range, 1-49) for priority 1, 15 days (range, 1-83) for priority 2, and 25 days (range, 3-49) for priority 3.
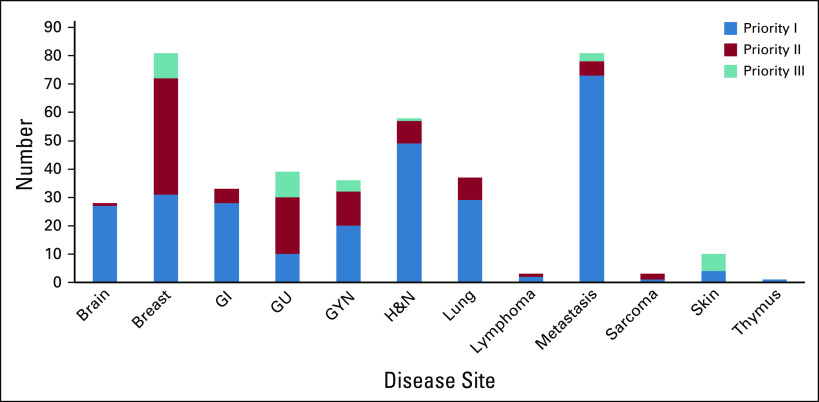
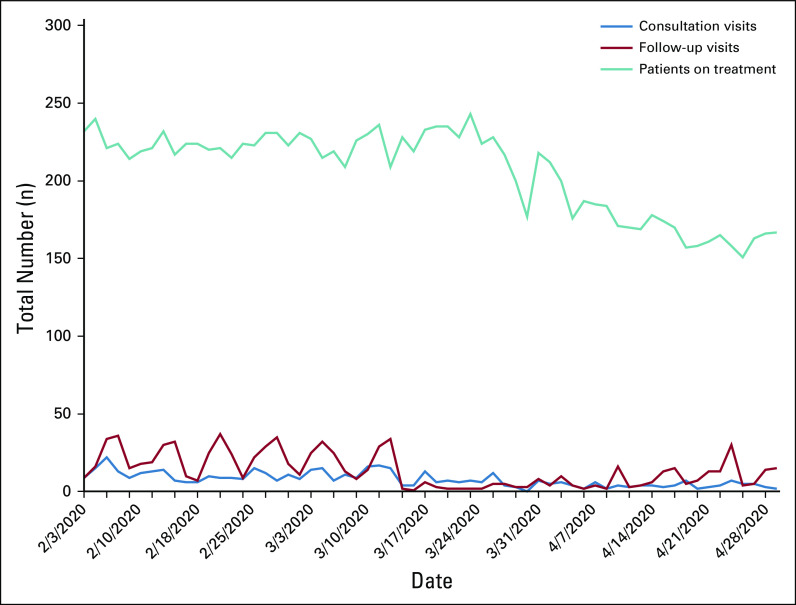
The majority of cases in priority 1 were in curative disease settings. Breast and genitourinary cancers made up the majority of priority 2 and 3 categories. Figure 1 shows the priority groupings for each disease site. Additional data are available in the Data Supplement (online only). Our prioritization system reduced the number of patients on treatment by approximately 27% during the months of March and April (Appendix Figure A1, online only).
FIG 1.
Priority distribution by disease site. GU, genitourinary; GYN, gynecologic; H&N, head and neck.
Impacts of COVID-19 on Care Plan
Table 2 outlines the impact of the pandemic on the 406 patients. In 58% of cases, there was no change in workup, treatment, or care plan. In 42% of cases, there was an impact of the pandemic on at least one aspect of the patient's radiation treatment; changes in treatment or care plan can broadly be placed into three categories: (1) unplanned impact on workup and modalities available, (2) patient decisions to delay or cancel treatment, and (3) proactive physician-initiated changes to the radiation timing and prescription. This third category includes change in radiation prescription, number of fractions, modalities of treatment, and prioritization system categorization of two or three to delay start date.
TABLE 2.
Effect of Coronavirus Disease 2019 Surge on Radiation Oncology Component of Treatment Plan
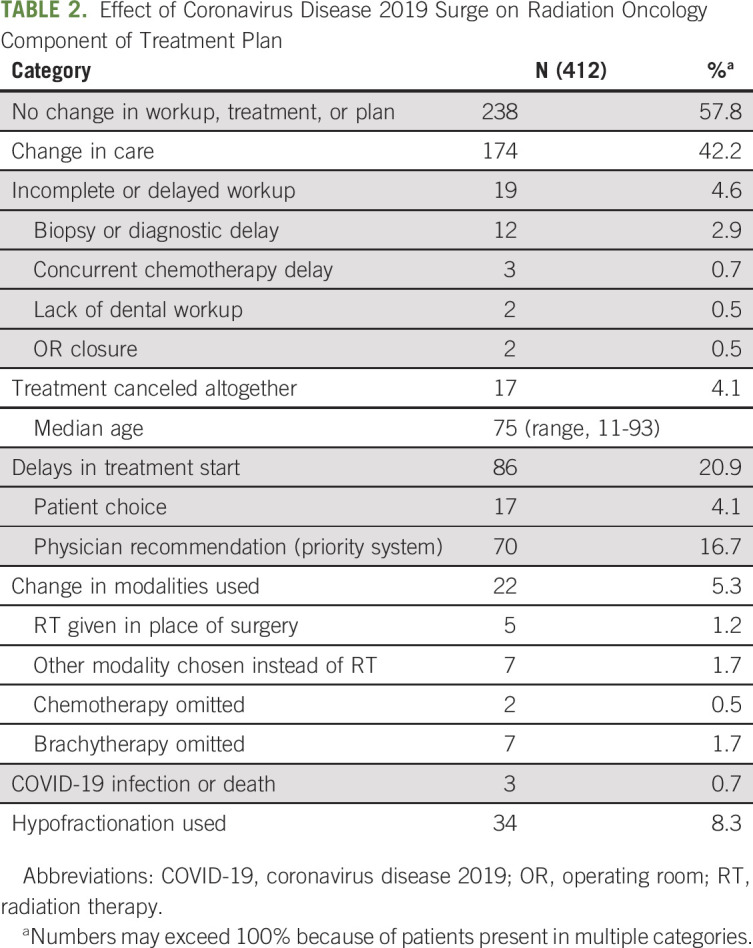
Before treatment began, incomplete or delayed workup was present in 19 cases (4.6%): most were biopsy or diagnostic delay (n = 12). Treatment intent was palliative in 10 cases, and a variety of disease sites were affected, including eight metastasis, three H&N, and two lung and brain. A change in treatment modality was present in 22 cases (5.3%).
Patients canceled or delayed treatment in reaction to the pandemic. Seventeen patients canceled their radiation treatment altogether. Treatment intent of these patients was curative in 12 and palliative in four; one treatment was for benign heterotopic bone. Disease sites included breast (n = 4), metastasis (2), H&N (3), skin (3), gynecologic (2), and one each of brain and GI. Treatment start date was electively delayed by the patient in 17 cases (4.1%); the average time elapsed was 22.8 days (range, 6-83) from CT sim to treatment start date.
Hypofractionation was used by the attending physician to shorten the treatment plan in 34 cases (8.3%). Most common disease sites for hypofractionation were metastasis (n = 13); brain, breast, and GI (n = 4 each); and lungs (n = 3). Three patients developed COVID-19 after CT sim, and one died as a result.
DISCUSSION
In this study, we aimed to review how the acute surge phase of the COVID-19 pandemic from March to April of 2020 affected the care of our Northwell Health radiation medicine patients.23 We were forced to quickly adjust our oncology patient management to keep our patients and staff safe while maintaining access to RT. During this time period, we continued to treat patients with standard-of-care treatments. We found that over 50% of patients experienced no change in their care plan or radiation treatments. However, 42% of patients deviated from standard-of-care in some way. These deviations could be categorized into two distinct categories: proactive or planned changes to care versus unplanned or reactive changes. For this study, we relied on physicians to provide detailed commentary on each patient case, rather than the study team independently reviewing medical records to identify delays. We found that physicians provided additional nuances of patient care than were initially present in the otherwise comprehensive QA database, and we are grateful for their detailed contributions to this study.
Proactive changes to care are reflected in (1) our prioritization system and (2) physician decisions to shorten or modify treatment plans. These proactive decisions were based on best available evidence regarding safe deferrals of radiotherapy. We achieved a notably diminished volume of outpatients entering our department for treatment and routine outpatient visits (Appendix Figure A1). Our departmental approach to priority groupings has evolved. Once we achieved a reduced treatment census on each machine, we began to allow all priority 2 and 3 patients in the queue to schedule treatment start appointments. By the end of May 2020, operating rooms were opening and routine workup was readily available. At the time of this writing, we are close to normal operations with respect to treatment workups and availability of all modalities of care. We are no longer delaying patient starts, and the prioritization system is on hold.
Our department already heavily uses hypofractionation where high-level evidence exists.24 In this study, our physicians made the decision to use a more hypofractionated treatment regimen in 34 cases; these decisions were driven entirely by the COVID-19 pandemic. Our physicians' actions are in line with multiple publications that have suggested ways to modify treatment fractionations in the COVID-19 era.25
Unplanned or reactive impacts on patient cancer care were observed in a minority of cases. Prior to analyzing our data, we anticipated that we would observe a number of cases where workup and diagnosis were inadequate or delayed. We were heartened to see that only 19 of the 412 cases had an inadequate or delayed workup, primarily as a result of closures of interventional radiology, endoscopy services, operating rooms, and dental offices during the surge phase of the pandemic. Similarly, changes in modalities used or offered represent an additional unplanned, or reactive, impact of the pandemic on cancer care. Brachytherapy was omitted in seven cases because of operating room closures. In 8% of cases, patients made the choice to cancel or delay their radiation treatment plan. We believe that fear of nosocomial infection played a major role in patient choice to delay or cancel care. Fear and anxiety are well-documented deterrents to compliance in RT.26 During this pandemic, we hypothesize that many of the patients who canceled treatment were concerned with limiting exposure to the virus, even if that meant avoiding a necessary part of their cancer treatment. Early in the pandemic, there was a paucity of data regarding the risks and impacts of COVID-19 on patients with cancer. Center for Disease Control and Prevention guidelines grouped patients with cancer under the umbrella of persons with underlying conditions. Therefore, in addition to fear, many patients lacked adequate guidance from national and multinational organizations. Unfortunately, this decision to cancel or delay treatment was often done against medical advice. In curative settings, we anticipate that cancellations or delays will have an adverse impact on patient outcomes. These patients represent an opportunity for better counseling and intervention.
Recommendations for Radiation Oncology Practices
Our data highlighted that more than 40% of patient treatments deviated from SOC in some way, whether proactively by physician decision, or reactively by patient choice or as a result of resource limitation. We intend to learn from this experience so that fewer patients would deviate from SOC in future pandemics. Disease models of COVID-19 uniformly indicate the persistence of the virus with various surges of disease until herd immunity is attained by vaccination.27,28 We must plan ahead for these future scenarios where resources may again be limited and patients avoid healthcare settings. We offer the following recommendations to practices based on our experience.
1. Educate physicians and staff about the purpose and goals of prioritization system.
A large proportion of patients (66%) were given priority 1 status. We believe that faculty chose this category for patients who wanted to begin treatment quickly or for patients who were being treated in our locations where treatment census was low enough to allow physical distancing without a need to delay patient start dates. If and when we encounter a need for prioritization of patients in the future, we will clearly educate physicians regarding the meaning of each priority category. Triage systems have no value if categorization is not performed correctly. In a situation where treatment volume is low enough to allow for priority 2 and 3 patients to begin treatment, they would warrant a different categorization such as Priority 2—Ready to Start, rather than incorrectly grouping into priority 1.
2. Provide counseling, reassurance, and support to patients who require timely care.
Fear of exposure to COVID-19 has kept many patients from obtaining necessary cancer care. As a medical field, we have now learned how to safely offer cancer care using proper sanitary measures, universal masking, telemedicine, and physical distancing. We have an urgent opportunity to communicate these safety steps clearly to our patients and thereby rebuild their trust in healthcare settings. We must maintain strict protocols that stop the spread of virus. These new policies should remain in effect until public health authorities convey definitive guidance that the spread of this virus has been controlled.
3. Use of multidisciplinary teams to allocate resources effectively in future pandemics.
When determining optimal treatment pathways during the pandemic, we would have benefited from having multidisciplinary input about resource and facility availability. Therefore, we propose that multidisciplinary teams during pandemic times contain members with up-to-date knowledge of available resources. These personnel can offer guidance to patient-facing providers who face closure of operating rooms or other necessary resources.
4. Closely follow those patients whose care has deviated from standard protocols.
All patients whose care deviated from standard protocols will need to be followed prospectively to assess the impact on their disease outcomes. In our department, we continuously reach out to patients who have delayed or deferred care until they resume care or indicate an informed desire to cancel care entirely. This information is then tracked in our QA database. It is our responsibility as clinicians and providers to learn from this experience and publish our results for the benefit of other practices.
Limitations
The included patients for this study came from a database of patients who underwent CT simulation for radiation treatment planning. This database does not include patients who were seen for consultations and for whom radiation simulation was deferred until the acute surge phase of the COVID-19 pandemic had passed. Therefore, we do not include patients with priority 3 type cancer, early stage prostate cancers, breast cancers being bridged with endocrine therapy, and early stage skin cancers. We believe that studying those patients who were simulated for radiation is useful for everyday radiation practice because it reflects more accurately patients who had agreed to proceed with treatment and then had a change in that plan. It is these patients in particular who are using valuable healthcare resources that need to be managed in real time. In addition, the database excludes patients who elected a different modality of treatment, such as prostate cancer active surveillance and rectal cancers starting with neoadjuvant chemotherapy rather than neoadjuvant chemoradiation therapy. Our study under-reports the impact of patient choice on delays in care during the COVID-19 pandemic. Anecdotally, all authors saw patients during this time period who elected to delay treatment because of their own fears regarding coronavirus exposure. Healthcare usage is considerably lower this year than in prior years, and the impact of patients' deferral of cancer screenings will not be recorded until they return to the medical setting.
In conclusion, the COVID-19 global pandemic had the potential to make a profound impact on care of outpatient oncology patients. During the resource-constrained New York surge phase of this pandemic lasting from March to April 2020, we found that the majority (58%) of patients simulated for RT were able to complete their care without change in their treatment plans. Still, 42% of patients experienced a deviation from standard care. We suggest four main recommendations for future pandemic scenarios: (1) educate physicians and staff about the purpose and intent of prioritization systems, (2) provide counseling and support to patients who require timely care, (3) use multidisciplinary teams to allocate resources effectively in future pandemics, and (4) closely follow patients whose treatment has deviated from standard-of-care.
APPENDIX
FIG A1.
Radiation medicine departmental treatment volume before and during the coronavirus disease 2019 crisis—office visits and patients on treatment.
Louis Potters
Stock and Other Ownership Interests: SRO Health LLC
No other potential conflicts of interest were reported.
AUTHOR CONTRIBUTIONS
Conception and design: Sewit Teckie, William Chun-Ying Chen, Anuj Goenka, Daniel Koffler, Louis Potters
Collection and assembly of data: Sewit Teckie, William Chun-Ying Chen, Anuj Goenka, Nilda Adair
Data analysis and interpretation: Sewit Teckie, Janna Zeola Andrews, William Chun-Ying Chen, Anuj Goenka, Daniel Koffler
Manuscript writing: Sewit Teckie, Janna Zeola Andrews, William Chun-Ying Chen, Anuj Goenka, Daniel Koffler, Nilda Adair
Final approval of manuscript: Sewit Teckie, Janna Zeola Andrews, William Chun-Ying Chen, Anuj Goenka, Daniel Koffler, Nilda Adair, Louis Potters
Accountable for all aspects of the work: Sewit Teckie, Janna Zeola Andrews, William Chun-Ying Chen, Anuj Goenka, Daniel Koffler, Nilda Adair, Louis Potters
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
Impact of the COVID-19 Pandemic Surge on Radiation Treatment: Report From a Multicenter New York Area Institution
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated unless otherwise noted. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/op/authors/author-center.
Open Payments is a public database containing information reported by companies about payments made to US-licensed physicians (Open Payments).
Louis Potters
Stock and Other Ownership Interests: SRO Health LLC
No other potential conflicts of interest were reported.
REFERENCES
- 1.Guan W Ni Z Hu Y, et al. : Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 382:1708-1720, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.WHO Director-General's opening remarks at the media briefing on COVID-19. 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020
- 3.COVID-19 map. Johns Hopkins Coronavirus Resource Center. https://coronavirus.jhu.edu/map.html
- 4.Liang W Guan W Chen R, et al. : Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Lancet Oncol 21:335-337, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang H, Zhang L: Risk of COVID-19 for patients with cancer. Lancet Oncol 21:e181, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Xia Y Jin R Zhao J, et al. : Risk of COVID-19 for patients with cancer. Lancet Oncol 21:e180, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Onder G, Rezza G, Brusaferro S: Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. JAMA 323:1775-1776, 2020 [DOI] [PubMed] [Google Scholar]
- 8.Remuzzi A, Remuzzi G: COVID-19 and Italy: What next? Lancet 395:1225-1228, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sidaway P: COVID-19 and cancer: What we know so far. Nat Rev Clin Oncol 17:336, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yu J Ouyang W Chua MLK, et al. : SARS-CoV-2 transmission in patients with cancer at a tertiary care hospital in Wuhan, China. JAMA Oncol 6:1108-1110, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Papachristofilou A Finazzi T Kohler G, et al. : Contingency plans in a radiation oncology department amid the 2019-nCoV outbreak in Switzerland. Adv Radiat Oncol 5:577-581, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Braunstein LZ Gillespie EF Hong L, et al. : Breast radiotherapy under COVID-19 pandemic resource constraints—Approaches to defer or shorten treatment from a Comprehensive Cancer Center in the United States. Adv Radiat Oncol 5:582-588, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yerramilli D Xu AJ Gillespie EF, et al. : Palliative radiotherapy for oncologic emergencies in the setting of COVID-19: Approaches to balancing risks and benefits. Adv Radiat Oncol 5:589-594, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zaorsky NG Yu JB McBride SM, et al. : Prostate cancer radiotherapy recommendations in response to COVID-19. Adv Radiat Oncol 5:659-665, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Achard V, Tsoutsou P, Zilli T: Radiotherapy in the time of the coronavirus pandemic: When less is better. Int J Radiat Oncol Biol Phys 107, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Potters L, Kapur A: Implementation of a “No Fly” safety culture in a multicenter radiation medicine department. Pract Radiat Oncol 2:18-26, 2012 [DOI] [PubMed] [Google Scholar]
- 17.Potters L, Bloom B: Our pledge to achieve safety. Int J Radiat Oncol Biol Phys 82:1310-1311, 2012 [DOI] [PubMed] [Google Scholar]
- 18.Cox BW Kapur A Sharma A, et al. : Prospective contouring rounds: A novel, high-impact tool for optimizing quality assurance. Pract Radiat Oncol 5:e431-e436, 2015 [DOI] [PubMed] [Google Scholar]
- 19.Cox BW Teckie S Kapur A, et al. : Prospective peer review in radiation therapy treatment planning: Long-term results from a longitudinal study. Pract Radiat Oncol 10:e199-e206, 2019 [DOI] [PubMed] [Google Scholar]
- 20.Puckett LL Luitweiler E Potters L, et al. : Preventing discontinuation of radiation therapy: Predictive factors to improve patient selection for palliative treatment. J Oncol Pract 13:e782-e791, 2017 [DOI] [PubMed] [Google Scholar]
- 21.Chen WC Teckie S Somerstein G, et al. : Guidelines to reduce hospitalization rates for patients receiving curative-intent radiation therapy during the COVID-19 pandemic: Report from a Multicenter New York Area Institution. Adv Radiat Oncol 5:621-627, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Leading a Radiation Medicine Department from the Epicenter of the COVID-19 Pandemic in the United States. https://appliedradiationoncology.com/articles/leading-a-radiation-medicine-department-from-the-epicenter-of-the-covid-19-pandemic-in-the-united-states
- 23.Team IC-19 Health Service Utilization Forecasting, Murray CJ: Forecasting COVID-19 impact on hospital bed-days, ICU-days, ventilator-days and deaths by US state in the next 4 months. medRxiv, 2020. [Google Scholar]
- 24.Gilbo P, Potters L, Lee L: Implementation and utilization of hypofractionation for breast cancer. Adv Radiat Oncol 3:265-270, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Simcock R Thomas TV Estes C, et al. : COVID-19: Global radiation oncology's targeted response for pandemic preparedness. Clin Transl Radiat Oncol 22:55-68, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Guidolin K, Lock M, Brackstone M: Patient-perceived barriers to radiation therapy for breast cancer. Can J Surg 61:15716, 2017 [DOI] [PubMed] [Google Scholar]
- 27.Gill BS Lin JF Krivak TC, et al. : National cancer data base analysis of radiation therapy consolidation modality for cervical cancer: The impact of new technological advancements. Int J Radiat Oncol Biol Phys 90:1083-1090, 2014 [DOI] [PubMed] [Google Scholar]
- 28.Projecting the transmission dynamics of SARS-CoV-2 through the postpandemic period|Science. https://science.sciencemag.org/content/368/6493/860 [DOI] [PMC free article] [PubMed]