PURPOSE
To enable design of optimum palliative care for women with cervical cancer, we studied the most common types of suffering and their severity, prevalence, and duration.
METHODS
We first reviewed the literature on the major types, severity, prevalence, and duration of suffering associated with cervical cancer. We then conducted a modified Delphi process with experts in cervical cancer care to supplement the literature. For each type of suffering, we distinguished between decedents (those who die from cervical cancer in a given year) and nondecedents (those who have cervical cancer in a given year but do not die). By applying the suffering prevalence and duration estimates to the number of decedents, nondecedents, and family caregivers in 2017, we were able to estimate their palliative care needs and the intensity of palliative care needed to respond adequately to this suffering.
RESULTS
There is a high prevalence among decedents of moderate or severe pain (84%), vaginal discharge (66%), vaginal bleeding (61%), and loss of faith (31%). Among both decedents and nondecedents, there is a high prevalence of clinically significant anxiety (63% and 50%, respectively), depressed mood (52% and 38%, respectively), and sexual dysfunction (87% and 83%, respectively). Moderate or severe financial distress is prevalent among decedents, nondecedents, and family caregivers (84%, 74%, and 66%, respectively). More than 40% of decedents and nondecedents are abandoned by their intimate partners. Most patients experience some combination of moderate or severe physical, psychological, social, and spiritual suffering. In total, 258,649 decedents and 2,558,857 nondecedents needed palliative care in 2017, approximately 85% of whom were in low- and middle-income countries where palliative care is rarely accessible.
CONCLUSION
Among women with advanced cervical cancer, suffering is highly prevalent and often severe and multifaceted.
INTRODUCTION
Cervical cancer, a preventable disease, is one of the gravest threats to women's well-being and lives worldwide. It is the fourth most common cancer in women globally and disproportionately afflicts the poor. One woman dies from it every 2 minutes, and the limited available data suggest that women with cervical cancer typically experience suffering that is more complex and severe than that caused by other serious illnesses.1-4 To stop the unnecessary suffering and death from cervical cancer, the WHO developed the Global Strategy to Accelerate the Elimination of Cervical Cancer as a Public Health Problem, which was adopted by the 73rd World Health Assembly in August 2020.5 The strategy outlines a comprehensive roadmap toward elimination within the current century that entails achievement of the 90-70-90 targets associated with three main pillars of the strategy: (1) primary prevention through human papilloma virus (HPV) vaccination, (2) screening with high-precision tests and treatment of precancerous lesions, and (3) management of invasive cervical cancer, including palliative care. But while palliative care is an essential part of comprehensive cancer care, design and implementation of optimum palliative care for women with cervical cancer requires better understanding of the suffering it engenders.6
CONTEXT
Key Objective
Cervical cancer disproportionately afflicts the poor and appears to cause worse suffering than most other serious illnesses. We studied the major types, prevalence, severity, and duration of suffering associated with cervical cancer as a necessary prerequisite to designing optimum palliative care.
Knowledge Generated
Among women with cervical cancer in 2017, there was a high prevalence of moderate or severe pain, malodorous vaginal discharge, vaginal bleeding, anxiety, depressed mood, sexual dysfunction, and financial distress, and more than 40% experienced abandonment by intimate partners. Patients' primary family caregivers also experienced psychosocial distress. More than 3 million patients and primary family caregivers needed palliative care in 2017, 85% of whom were in low- or middle-income countries.
Relevance
Cervical cancer generates suffering that is highly prevalent, severe, and varied, especially among the global poor. It is medically and morally imperative to assure access by the global poor to cervical cancer prevention, early diagnosis and treatment, and appropriate palliative care.
In this paper, we identify the most common and severe types of suffering of people affected by cervical cancer, including patients and their primary family caregivers, most of whom are poor and live in low- or middle-income countries (LMICs) where access to palliative care remains rare.7 We also identify the prevalence and duration of this suffering using a method pioneered by the Lancet Commission on Palliative Care and Pain Relief.8 Our hypothesis was that moderate and severe suffering is more prevalent and multifaceted among women with cervical cancer than among people with other cancers or serious illnesses.9
Epidemiology
The International Agency for Research on Cancer (IARC) estimates that, in 2018, 570,000 women were diagnosed with cervical cancer and 311,000 women died of it. More than 85% of cases occurred in LMICs or among poor and marginalized communities in high-income countries (HICs), and it was the most common cause of cancer-related death in sub-Saharan Africa.10 Globally, in 2018, the average age at diagnosis of cervical cancer was 53 years, and the average age at death was 59 years. China and India together had more than a third of the global cervical cancer cases (106,000 in China and 97,000 in India) and deaths (48,000 in China and 60,000 in India).10
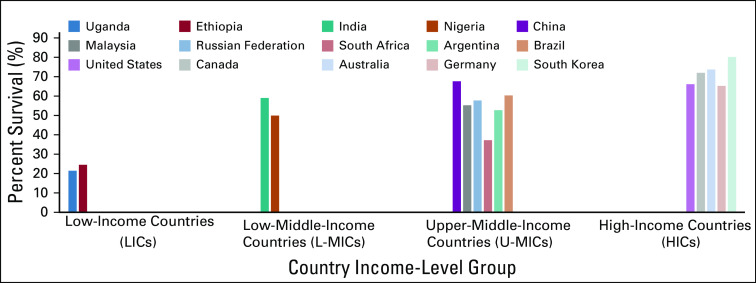
Five-year survival for women with cervical cancer varies widely by country income level (Fig 1). Although data on 5-year survival are scant from low-income countries (LICs) and lower-middle–income countries (L-MICs), it appears that a minority of patients survive for 5 years in these countries where 3.6 of the world's 7.7 billion people live.11,12 Available data indicate that 5-year survival in LICs may range from 3% to 23%. The differences in survival are due in part to the late diagnosis of cancer in these countries and the lack of access to adequate treatment including external beam radiotherapy and brachytherapy.13 Each increase in disease stage at diagnosis is known to decrease 5-year survival.12,14 But even in HICs, more than a third of patients die within 5 years.
FIG 1.
Five-year survival with cervical cancer of any stage (%) by country income level. HIC, high-income country; LIC, low-income country; L-MIC, low-middle–income country; U-MIC, upper-middle–income country. Sengayi-Muchengeti et al.12 Arbyn et al,10 Allemani et al,11 Hong et al,32 National Cancer Institute,33 Cancer Australia,34 Canadian Cancer Society.35
Among cervical cancers, around 70% are squamous cell carcinomas, 25%-30% of carcinomas are adenocarcinomas, and there is a small percentage of noncarcinomas.5 Almost all cervical carcinomas are associated with chronic HPV infection, which is also associated with increased risk of vaginal and vulvar cancer in women, penile cancer in men, as well as anorectal cancer and oropharyngeal cancer in both men and women. Additional risk factors for cervical cancer include chronic immunosuppression, first- and second-hand exposure to tobacco smoke, prolonged use of oral contraceptives, increasing parity, as well as increased numbers of sexual partners or a single sexual partner who has multiple sexual partners. Women living with HIV infection are at increased risk for chronic HPV infection and are six times as likely to develop HPV-associated cervical cancer compared with HIV-negative women.15 This accounts in part for the high prevalence of cervical cancer in sub-Saharan Africa.13 Use of highly active antiretroviral therapy partially reduces the risk of HPV-associated neoplasia.16
Prophylactic HPV vaccination, given before onset of sexual activity, conveys almost 100% protection against HPV infection with the subtypes covered by the vaccine. However, as of 2020, less than a quarter of LICs and < 30% of L-MICs have introduced the HPV vaccine into their national immunization schedules, while more than 85% of HICs have done so.15 Screening for HPV-associated cervical neoplasia, followed by ablative or excisional treatment, has been shown to decrease the incidence of invasive cervical cancer. But striking disparities between countries of different income levels also exist in access to cervical cancer screening, diagnosis, and treatment services. Combined basic capacity for pathology, cancer surgery, radiotherapy, and chemotherapy is accessible only in about 13% of LICs. The other 87% of LICs lack one or more of these services.
METHODS
We first conducted a review of the literature on the major types, prevalence, and duration of suffering because of cervical cancer. We began with a PubMed search using the search terms uterine cervical cancer suffering, uterine cervical cancer pain, and uterine cervical cancer palliative care. All English-, French-, and German-language papers reporting quantitative or qualitative data on the types, severity, prevalence, or duration of suffering associated with cervical cancer, all meta-analyses of such reports, and all reviews of these topics were used for the study. Similar papers noted on the PubMed website and in the reference list of the downloaded papers were also used. For each paper, we also noted the World Bank country income classification of the country or countries from which data were obtained. All quantitative data on the types, severity, prevalence, or duration of suffering associated with cervical cancer were used to populate preliminary tables. In creating these tables, we adhered to the standard distinction in the palliative care literature between four categories of suffering: physical, psychological, social, and spiritual. Although these categories of suffering cannot be clearly distinguished in clinical practice, we do so heuristically here to better understand the ways women with cervical cancer suffer and thus what would constitute optimum palliative care. When there was more than one study reporting data on the prevalence or duration of any specific type of suffering, we calculated a mean for use in the preliminary tables.
In light of the dearth of quantitative data, especially from LMICs, on the specific types of suffering within each category and of prevalence and duration of each type of suffering, we also convened an expert panel of experienced providers of care for women with cervical cancer to review, comment on, and supplement our literature review. The expert panel consisted of two clinicians from each of the six WHO regions and included 10 medical doctors, one nurse, and one social worker. One member was from an LIC, five were from L-MICs, four were from upper-middle–income countries, and two were from high-income countries. We used a two-round modified Delphi Process to achieve consensus among members of the expert panel for refining and completing the preliminary tables on the types, prevalence, and duration of physical, psychological, social, and spiritual suffering experienced by women with cervical cancer and their primary family caregivers.17 Whereas the first round of a standard Delphi Process would have entailed asking each participant to identify the most common and severe types of suffering and their prevalence without providing any data or suggestions, we modified the first round by providing participants with the preliminary tables populated with available data from the literature on the most common and severe types of suffering, their prevalence, and their duration, to help inform their responses. For each type of suffering, we asked the participants to distinguish between decedents (those who die from cervical cancer in a given year) and nondecedents (those who have cervical cancer in a given year but do not die). We also asked participants to estimate the prevalence and duration of most types of psychological, social, and spiritual suffering of primary family caregivers.
To determine the total number of patients with cervical cancer per year who have one or more types of moderate or severe suffering and therefore require palliative care, we began with data on the number of deaths from cervical cancer in 2017 from the Institute for Health Metrics and Evaluation (IHME), the total prevalence of cervical cancer in 2017 from the IHME, and the 5-year prevalence data from IARC.18,19 The number of nondecedents was calculated as the sum of all patients with cervical cancer within 5 years of diagnosis and 50% of patients who survived longer than 5 years. We used the IHME data from 194 countries and territories. For the 16 countries for which no data from IARC were available, we imputed 5-year survival using the average from each country's World Bank income group. To calculate the number of family caregivers with moderate or severe psychological, social, or spiritual suffering and thus in need of palliative care, we assumed that each decedent had only one primary family caregiver at risk of some type of suffering.
By applying the suffering prevalence and duration estimates from the modified Delphi Process to the calculated number of decedents, nondecedents, and family caregivers, we were able to estimate the number of decedents, nondecedents, and family caregivers who experienced each type of suffering in 2017. We then also estimated the intensity of palliative care needed to respond adequately to this suffering, measured as the number of days when contact with a palliative care provider is needed either in inpatient or outpatient settings or in the home, to apply the essential package of palliative care recommended by WHO and described elsewhere.6,20,21 We generated estimates of the palliative care need by patients with cervical cancer and their family caregivers globally, regionally, for each country, and for each country income group.
RESULTS
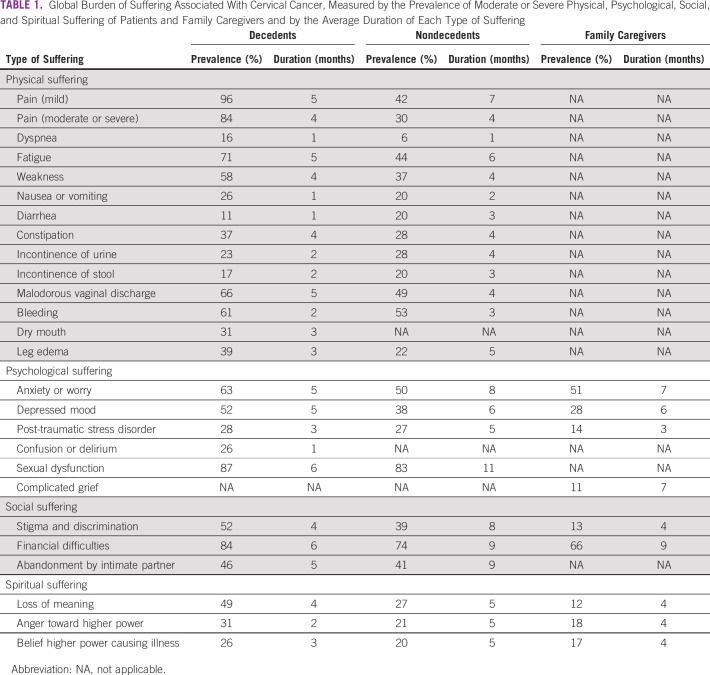
The results of the modified Delphi Process are shown in Table 1. Cervical cancer and its treatment result in an average prevalence of pain among decedents that is higher (mild 96%; moderate-severe 84%) than among patients with any other illness that commonly generates a need for palliative care, including malignant neoplasms in general.8 Nearly two thirds of decedents suffer from moderate or severe malodorous vaginal discharge (66%) and vaginal bleeding (61%). Among nondecedents, prevalence of mild pain is 42%, moderate or severe pain 30%, moderate or severe malodorous vaginal discharge 49%, and moderate or severe vaginal bleeding 53%. These symptoms contribute to a high prevalence of moderate or severe psychological suffering among both decedents and nondecedents, including anxiety (63% and 50%, respectively), depressed mood (52% and 38%, respectively), and sexual dysfunction (87% and 83%, respectively). Moderate or severe financial distress also is highly prevalent among decedents (84%) and nondecedents (74%) and it affects nearly two thirds of family caregivers (66%). More than half of the decedents and more than a third of nondecedents feel stigmatized or socially isolated (52% and 39%, respectively), and more than 40% are abandoned by their intimate partner (46% and 41%, respectively). Nearly half of the decedents experience loss of meaning in life (49%), and nearly one third suffer a loss of faith (31%). Most patients experience some combination of moderate or severe physical, psychological, social, and spiritual suffering.
TABLE 1.
Global Burden of Suffering Associated With Cervical Cancer, Measured by the Prevalence of Moderate or Severe Physical, Psychological, Social, and Spiritual Suffering of Patients and Family Caregivers and by the Average Duration of Each Type of Suffering
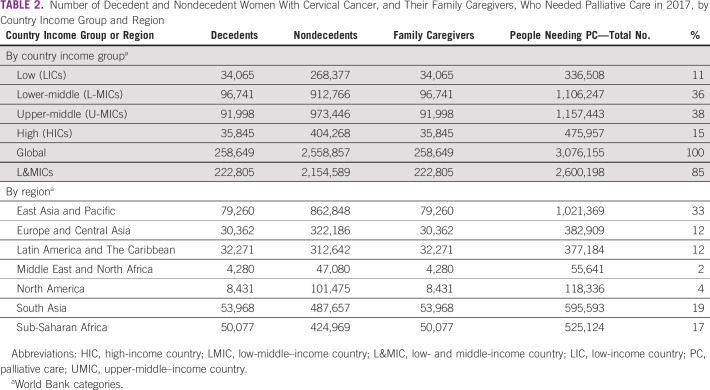
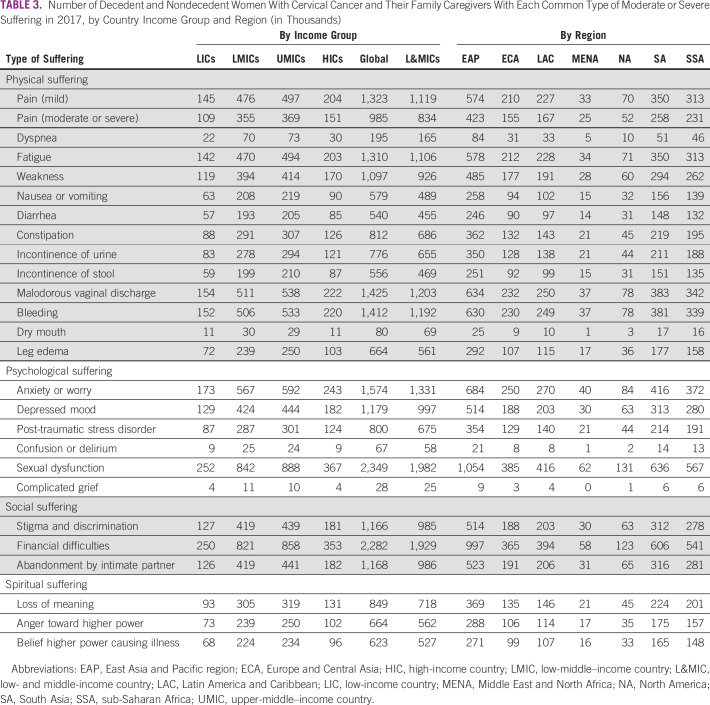
In total, more than 3 million people needed palliative care in 2017 because of the effects of cervical cancer: 258,649 decedent women with cervical cancer, an equal number of family caregivers, and 2,558,857 nondecedent women with cervical cancer (Table 2). L-MICs and upper-middle–income countries had the largest number of patients and family caregivers in need of palliative care, and 85% of people in need (more than 2.6 million) were in LMICs. Among the seven World Bank regions, the East Asia and Pacific region had the largest number of people (patients and their primary family caregivers) in need of palliative care (33% of the global total) followed by the South Asia and sub-Saharan Africa regions (19% and 17% of the global total, respectively). The number of people with each common type of suffering because of cervical cancer is shown in Table 3. Globally, nearly 1 million women with cervical cancer suffered from moderate or severe pain in 2017, 85% of whom were in LMICs. More than 1.4 million suffered from moderate or severe malodorous vaginal discharge, 84% of whom were in LMICs. Nearly 2 million women suffered from moderate or severe sexual dysfunction, and nearly 2 million patients and family caregivers combined suffered from moderate or severe financial difficulties associated with the patient's cervical cancer.
TABLE 2.
Number of Decedent and Nondecedent Women With Cervical Cancer, and Their Family Caregivers, Who Needed Palliative Care in 2017, by Country Income Group and Region
TABLE 3.
Number of Decedent and Nondecedent Women With Cervical Cancer and Their Family Caregivers With Each Common Type of Moderate or Severe Suffering in 2017, by Country Income Group and Region (in Thousands)
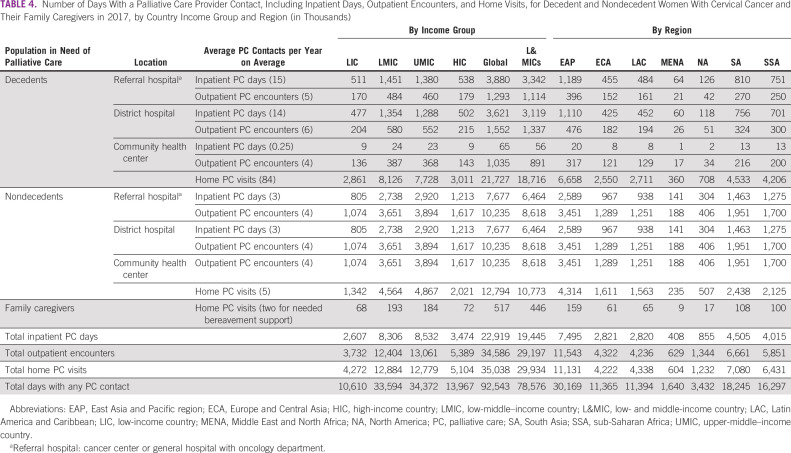
To provide adequate palliative care globally for women with cervical cancer, in 2017, using the WHO essential package of palliative care, we estimated that an inpatient palliative care encounter would have been needed on 22,919 days, an outpatient encounter on 34,586 days, and a home visit on 35,038 days (Table 4). Of the total of 92,543 days when a palliative care encounter would have been needed, 78,576 of these encounters (85%) were needed in LMICs.
TABLE 4.
Number of Days With a Palliative Care Provider Contact, Including Inpatient Days, Outpatient Encounters, and Home Visits, for Decedent and Nondecedent Women With Cervical Cancer and Their Family Caregivers in 2017, by Country Income Group and Region (in Thousands)
DISCUSSION
To our knowledge, ours is the first quantitative study of the major types, severity, prevalence, and duration of suffering associated with cervical cancer. Our data indicate that women with cervical cancer experience physical, psychological, social, and spiritual suffering that is more prevalent, complex, and severe than the suffering associated with most other serious illness.8 As a result of inadequate availability of primary prevention, early diagnosis and treatment of cervical cancer, and social problems such as poverty and stigmatization, a disproportionate percentage of patients with cervical cancer and family care givers in need of palliative care live in LMICs. Yet, access to palliative care to prevent and relieve this suffering also remains rare in LMICs.
Cervical cancer typically leads to multiple types of moderate and severe suffering for a variety of anatomic, physiologic, psychological, and social reasons. For purely anatomic reasons, pain due to cervical cancer and its treatment is more prevalent and severe than pain because of many other cancers. The pelvic region is highly innervated, and major nerves and nerve plexuses, including the sacral plexus and inferior hypogastric plexus, are located in or near the pelvis. Thus, invasive cervical cancer often injures nerves by invasion or compression resulting in neuropathic pain that is more difficult to control than nociceptive pain.22 Pelvic nerve injury and neuropathic pain also may result from surgery. In addition, peripheral neuropathic pain is a common adverse effect of paclitaxel and cisplatin, the chemotherapeutic agents used most commonly to treat cervical cancer. Radiotherapy to the pelvis may result in chronic inflammatory or nociceptive pain from vaginitis, cystitis, or proctitis as well as in sexual dysfunction, urinary incontinence, and diarrhea. Obstructive nephropathy and resultant end-stage kidney disease, common sequelae of cervical cancer, may result in dyspnea, pruritus, or delirium and may exacerbate edema and pain. Metal or hard plastic percutaneous nephrostomy drains, used in some places, severely limit patients' mobility and may increase risk of pain, leakage, dependence, and psychological distress. Fatigue and problems with memory and concentration often result from some combination of pain, chemotherapy, kidney disease, and depressed mood.
The high prevalence of psychological and social suffering among both decedents and nondecedents is due at least in part to the emotionally powerful meanings associated with the sex organs and sexual function, both of which are injured or ablated by invasive cervical cancer or its treatment. These meanings are informed by cultural values that often demean women deemed to have an unpleasant bodily odor and those whose sexual function does not reflect the cultural norm.3,23 In some East Asian cultures, for example, a young woman's status in society and personal identity may depend heavily on the ability to bear children, which often is destroyed by cervical cancer or its treatment.24 Women with both HIV infection and cervical cancer may be doubly stigmatized and at highest risk for psychological, social, or spiritual suffering.
WHO defines palliative care as care that improves the quality of life of patients and their families facing the problems associated with life-threatening illness, through the prevention and relief of suffering by means of early identification and impeccable assessment and treatment of pain and other problems, physical, psychosocial and spiritual.25 In our view, the essence of palliative care is prevention and relief of suffering, and the problems associated with life-threatening illness also may occur with non–life-threatening conditions. For example, women with early-stage, curable cervical cancer may suffer from abandonment, depression, or treatment-related acute pain, and long-term cervical cancer survivors may suffer from chronic pain. The specific types and severity of suffering vary by geopolitical situation, socioeconomic conditions, culture, and accessibility of disease prevention and treatment.26 People in LMICs typically experience less healthy social conditions and greater morbidity and mortality than people in HICs, yet they typically have less access to disease prevention, diagnosis, and treatment. Palliative care should never be considered a substitute for these, but it is imperative that palliative care be universally accessible.26-28
Our measure of necessary palliative care intensity (days-when-a-palliative-care-encounter-is-needed) refines the measure used by the Lancet Commission on Palliative Care and Pain Relief (days-in-palliative care).8 Some patients may require a palliative care encounter every day, whereas others may require only one encounter per month. By the previous measure, a patient receiving palliative care once per month for 1 year would have 365 days in palliative care but only 12 days with a palliative care encounter. Thus, days-in-palliative-care is an inaccurate measure of needed palliative care intensity and is not useful for estimating human resource needed. Days-with-a-palliative-care-encounter is a more accurate and useful measure.
Our study has several limitations. First, our literature review was limited to papers in English, French, and German that reported quantitative or qualitative data on the types, severity, prevalence, or duration of suffering associated with cervical cancer. However, among the English-language papers that met these criteria, 10 were from China and four were from countries whose official language is Spanish. In addition, our PubMed search revealed only five such papers in the other four official languages of the United Nations, three in Chinese, and one each in Russian and Spanish. Furthermore, our expert panel included members from countries whose official languages are Russian, Spanish, Arabic, French, Farsi, and Vietnamese. Thus, we believe that our research reflects the global situation. Our literature review revealed a large publication bias in that the majority of data on the types, severity, prevalence, and duration of suffering associated with cervical cancer came from HICs, whereas the majority of suffering patients are in LMICs. In addition, the studies used various methods, and although we did not systematically review each published study for bias, some contained various degrees of selection, recall, or other biases. We addressed these problems by conducting a modified Delphi process with an expert panel from each WHO region and from countries of all income classifications. Delphi studies themselves are limited in that they rely on expert opinion. But, we believe our method produced the most reliable data to date on the suffering of a highly vulnerable population.
The scarcity of quantitative data on the suffering of women in LMICs with cervical cancer and other gynecologic cancers reflects a morally indefensible neglect of this vulnerable population. Our study provisionally fills this massive gap in knowledge with expert opinion, but rigorous quantitative study of this palliative care need is crucial.8 As with all studies of highly vulnerable and seriously ill patients, short but clinically and ethically well-crafted, locally validated tools are needed to assess clinical outcomes of patients who receive any type of palliative care and those who do not. Although measures of outputs such as opioid accessibility and palliative care training programs are useful, they are never an adequate substitute for measures of patient outcomes such as quality of life, degree of pain control, or presence of depression. Because the specific types and severity of suffering vary, studies in different settings are needed to guide development of optimum palliative care services for any given population.6,20 Implementation science studies of integration of palliative care into healthcare systems at all levels, as urged by WHO, are necessary to make services for women with cervical cancer more integrated and people-centred.29 In light of the particularly high prevalence in this population of severe pelvic pain, humiliating malodorous vaginal discharge, anxiety, depression, sexual dysfunction, financial difficulties, and spiritual distress, these problems should be the focus of intensive research on optimum palliative care in LMICs. Further research on task shifting to improve access to mental health care, including treatment of depression and PTSD in patients with cervical cancer and other serious and severely troubling illnesses, is also needed.30,31
In conclusion, the suffering of women with advanced cervical cancer, an illness mainly of the global poor, has been largely ignored by scientific research. By reviewing the available literature and supplementing it with expert consensus, we found that the suffering of this population appears to be more prevalent, severe, and multifaceted than that associated with other cancers. Severe pelvic pain, malodorous vaginal discharge, sexual dysfunction, psychological distress, and financial insecurity are particularly prevalent. The high burden of suffering borne by women with cervical cancer makes it medically and morally imperative that there be universal access to HPV vaccination, screening, and treatment and that appropriate, effective, affordable, people-centered palliative care be integrated into all levels of systems of care for women with cervical cancer. This integration will require vigorous efforts from researchers, public health officials, oncologists, gynecologists, and primary care providers and should be part of the overall integration of palliative care into healthcare systems that is indispensable for achievement of universal health coverage.27
ACKNOWLEDGMENT
For helpful comments on the manuscript, the authors thank Sally Agallo Kwenda, Esther Cege-Munyoro, Lailatul Ferdous, Liliana de Lima, Rei Haruyama, Kim Hulscher, Elizabeth Mattfeld, Anastasia Merzlyakova, and Linda Van Le.
Eric L. Krakauer
Employment: Inform Diagnostics, Foundation Medicine
Xiaoxiao Kwete
Employment: Yaozhi Co Ltd
Stock and Other Ownership Interests: Expat Inc
Research Funding: Roche
Patents, Royalties, Other Intellectual Property: My husband Patrick Kwete has a granted patent called Personalized Medical Treatment Provision Software (https://patents.google.com/patent/US20130080425A1/en)
Travel, Accommodations, Expenses: Expat Inc
Annette Hasenburg
Honoraria: AstraZeneca, Med Update, Pfizer, Roche, StreamedupGmbH, Tesaro, MedConcept, LEO Pharma
Consulting or Advisory Role: PharmaMar, Tesaro, Roche, AstraZeneca, LEO Pharma, GlaxoSmithKline/MSD
Travel, Accommodations, Expenses: AstraZeneca, MedConcept, Roche, Streamedup!, Tesaro, MedUpdate, Pfizer
Cristiana Sessa
Consulting or Advisory Role: Basilea
Ted Trimble
Consulting or Advisory Role: Merck, GlaxoSmithKline, Inovio Pharmaceuticals
Research Funding: Frantz Viral Therapeutics
No other potential conflicts of interest were reported.
DISCLAIMER
Elena Fidarova, Cherian Varghese, and Eric Krakauer are staff members or consultants of the WHO. The authors alone are responsible for the views expressed in this article and they do not necessarily represent the decisions, policy, or views of the WHO.
SUPPORT
Supported in part by WHO, which contributed to study design, data analysis, data interpretation, and writing of the report. Dr Krakauer had full access to all the data and had final responsibility for the decision to submit the publication. Funding was provided by WHO and Unitaid.
AUTHOR CONTRIBUTIONS
Conception and design: Eric L. Krakauer, Xiaoxiao Kwete, Khadidjatou Kane, Gauhar Afshan, Danta Dona Ruthnie Bien-Aimé, Raimundo Correa, Mamadou Diop, Annekathryn Goodman, Quach Thanh Khanh, Dingle Spence, Cherian Varghese, Elena Fidarova
Administrative support: C. R. Beena Devi
Provision of study materials or patients: Khadidjatou Kane, Gauhar Afshan, Raimundo Correa, Quynh Xuan Nguyen Truong, Maryam Rassouli
Collection and assembly of data: Eric L. Krakauer, Xiaoxiao Kwete, Khadidjatou Kane, Nahla Gafer, Annette Hasenburg, Suresh Kumar, Diana Nevzorova, Maryam Rassouli, Elena Fidarova
Data analysis and interpretation: Eric L. Krakauer, Xiaoxiao Kwete, Khadidjatou Kane, Lisa Bazzett-Matabele, Sarah Byrne-Martelli, Stephen Connor, C. R. Beena Devi, Annekathryn Goodman, Surbhi Grover, Annette Hasenburg, Kelly Irwin, M. R. Rajagopal, Tom Randall, Cristiana Sessa, Julie S. Torode, Ted Trimble, Elena Fidarova
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated unless otherwise noted. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/go/authors/author-center.
Open Payments is a public database containing information reported by companies about payments made to US-licensed physicians (Open Payments).
Eric L. Krakauer
Employment: Inform Diagnostics, Foundation Medicine
Xiaoxiao Kwete
Employment: Yaozhi Co Ltd
Stock and Other Ownership Interests: Expat Inc
Research Funding: Roche
Patents, Royalties, Other Intellectual Property: My husband Patrick Kwete has a granted patent called Personalized Medical Treatment Provision Software (https://patents.google.com/patent/US20130080425A1/en)
Travel, Accommodations, Expenses: Expat Inc
Annette Hasenburg
Honoraria: AstraZeneca, Med Update, Pfizer, Roche, StreamedupGmbH, Tesaro, MedConcept, LEO Pharma
Consulting or Advisory Role: PharmaMar, Tesaro, Roche, AstraZeneca, LEO Pharma, GlaxoSmithKline/MSD
Travel, Accommodations, Expenses: AstraZeneca, MedConcept, Roche, Streamedup!, Tesaro, MedUpdate, Pfizer
Cristiana Sessa
Consulting or Advisory Role: Basilea
Ted Trimble
Consulting or Advisory Role: Merck, GlaxoSmithKline, Inovio Pharmaceuticals
Research Funding: Frantz Viral Therapeutics
No other potential conflicts of interest were reported.
REFERENCES
- 1.Kim YJ Munsell MF Park JC, et al. : Retrospective review of symptoms and palliative care interventions in women with advanced cervical cancer. Gynecol Oncol 139:553-558, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bates MJ, Mijoya A: A review of patients with advanced cervical cancer presenting to palliative care services at Queen Elizabeth Central Hospital in Blantyre, Malawi. Malawi Med J 27:93-95, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Maree JE, Holtslander L, Maree JE: The experiences of women living with cervical cancer in Africa: A metasynthesis of qualitative studies. Cancer Nurs 10.1097/NCC.0000000000000812[epub ahead of print on March 24, 2020] [DOI] [PubMed]
- 4.Fowler JM Carpenter KM Gupta P, et al. : The gynecologic oncology consult: Symptom presentation and concurrent symptoms of depression and anxiety. Obstet Gynecol 103:1211-1217, 2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Health Organization (WHO) : World Health Assembly Adopts Global Strategy to Accelerate Cervical Cancer Elimination. WHO, 2020. https://www.who.int/news-room/detail/19-08-2020-world-health-assembly-adopts-global-strategy-to-accelerate-cervical-cancer limination#:∼:text=The%20World%20Health%20Assembly%20has,detected%20early%20and%20managed%20effectively [Google Scholar]
- 6.Krakauer EL Kwete X Verguet S, et al. : Palliative care and pain control, in Jamison DT Gelband H Horton S, et al. (eds): Disease Control Priorities. Improving Health and Reducing Poverty, Volume 9 (ed 3). Washington, DC, World Bank, 2018, pp 235-246 [Google Scholar]
- 7.Connor SR. (ed): Global Atlas of Palliative Care (ed 2). London, UK, Worldwide Hospice Palliative Care Alliance. Geneva, Switzerland, World Health Organization, 2020 [Google Scholar]
- 8.Knaul FM Farmer PE Krakauer EL, et al. : Alleviating the access abyss in palliative care and pain relief: An imperative of universal health coverage. Lancet 391:1391-1454, 2018 [DOI] [PubMed] [Google Scholar]
- 9.Mishra K: Gynaecological malignancies from palliative care perspective. Indian J Palliat Care 17:S45-S51, 2011. (suppl) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Arbyn M Weiderpass E Bruni L, et al. : Estimates of incidence and mortality of cervical cancer in 2018: A worldwide analysis. Lancet Glob Health 8:e191-e203, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Allemani C Matsuda T Di Carlo V, et al. : Global surveillance of trends in cancer survival 2000–14 (CONCORD-3): Analysis of individual records for 37 513 025 patients diagnosed with one of 18 cancers from 322 population-based registries in 71 countries. Lancet 391:1023-1075, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sengayi-Muchengeti M Joko-Fru WY Miranda-Filho A, et al. : Cervical cancer survival in sub-Saharan Africa by age, stage at diagnosis and Human Development Index: A population-based registry study. Int J Cancer 147:3037-3048, 2020 [DOI] [PubMed] [Google Scholar]
- 13.Rudd P Gorman D Meja S, et al. : Cervical cancer in southern Malawi: A prospective analysis of presentation, management, and outcomes. Malawi Med J 29:124-129, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Grigsby PW Massad LS Mutch DG, et al. : FIGO 2018 staging criteria for cervical cancer: Impact on stage migration and survival. Gynecol Oncol 157:639-643, 2020 [DOI] [PubMed] [Google Scholar]
- 15.World Health Organization (WHO) : Global Strategy to Accelerate the Elimination of Cervical Cancer as a Public Health Problem. Geneva, Switzerland, World Health Organization, 2020 [Google Scholar]
- 16.Kelly H Weiss HA Benavente Y, et al. : Association of antiretroviral therapy with high-risk human papillomavirus, cervical intraepithelial neoplasia, and invasive cervical cancer in women living with HIV: A systematic review and meta-analysis. Lancet HIV 5:e45-e58, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sackman H: Delphi Assessment: Expert Opinion, Forecasting, and Group Process. Santa Monica, CA, Rand Corporation, 1974 [Google Scholar]
- 18.Institute for Health Metrics and Evaluation (IHME) Global Burden of Disease Collaborative Network : Global Burden of Disease Study 2017 (GBD 2017) Results. Seattle, WA, Institute for Health Metrics and Evaluation (IHME), 2018 [Google Scholar]
- 19.International Agency for Research on Cancer (IARC) : Cancer Today—IARC. Lyon, France, International Agency for Research on Cancer, 2018 [Google Scholar]
- 20.World Health Organization (WHO) : Integrating Palliative Care and Symptom Relief into Primary Health Care: A WHO Guide for Planners, Implementers and Managers. Geneva, Switzerland, World Health Organization, 2018 [Google Scholar]
- 21.Knaul FM Farmer PE Krakauer EL, et al. : Technical Note and Data Appendix for “Alleviating the Access Abyss in Palliative Care and Pain Relief—An Imperative of Universal Health Coverage: The Lancet Commission Report”. Miami, FL, University of Miami Institute for Advanced Study of the Americas, 2018 [DOI] [PubMed] [Google Scholar]
- 22.Rayment C Hjermstad MJ Aass N, et al. : Neuropathic cancer pain: Prevalence, severity, analgesics and impact from the European Palliative Care Research Collaborative–Computerised Symptom Assessment study. Palliat Med 27:714-721, 2012 [DOI] [PubMed] [Google Scholar]
- 23.Maree JE, Kaila I: Zambian women's experiences and understanding of cervical cancer: A qualitative study. Int J Gynecol Cancer 24:1065-1071, 2014 [DOI] [PubMed] [Google Scholar]
- 24.Lau KL, Yim PHW, Cheung EYW: Psychiatric morbidity in Chinese women after cervical cancer treatment in a regional gynaecology clinic. East Asian Arch Psychiatry 23:144-153, 2013 [PubMed] [Google Scholar]
- 25.World Health Organization (WHO) : WHO Definition of Palliative Care. 2002. https://www.who.int/cancer/palliative/definition/en/ [Google Scholar]
- 26.Krakauer EL: Palliative care, toward a more responsive definition. in MacLeod RD, Block L. (eds): Textbook of Palliative Care. Cham, Switzerland, Springer Nature, 2019 [Google Scholar]
- 27.World Health Organization (WHO) : World Health Assembly Resolution 67.19: Strengthening of Palliative Care as a Component of Comprehensive Care Throughout the Life Course. Geneva, Switzerland, World Health Organization, 2014 [Google Scholar]
- 28.Shulman LN Mpunga T Tapela N, et al. : Bringing cancer care to the poor: Experiences from Rwanda. Nat Rev Cancer 14:815-821, 2014 [DOI] [PubMed] [Google Scholar]
- 29.World Health Organization (WHO) : Framework on Integrated, People-Centred Health Services. Geneva, Switzerland, World Health Organization, 2016 [Google Scholar]
- 30.World Health Organization (WHO) : Task Shifting: Rational Redistribution of Tasks Among Health Workforce Teams. Global Recommendations and Guidelines. Geneva, Switzerland, World Health Organization, 2008 [Google Scholar]
- 31.Weobong B Weiss HA McDaid D, et al. : Sustained effectiveness and cost-effectiveness of the Healthy Activity Programme, a brief psychological treatment for depression delivered by lay counsellors in primary care: 12-month follow-up of a randomised controlled trial. PLoS Med 14:e1002385, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hong S Won YJ Park YR, et al. : Cancer statistics in Korea: Incidence, mortality, survival, and prevalence in 2017. Cancer Res Treat 52:335-350, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.National Cancer Institute: Cancer Stat Facts : Cervical Cancer. https://seer.cancer.gov/statfacts/html/cervix.html [Google Scholar]
- 34.Cancer Australia : National Cancer Control Indicators. https://ncci.canceraustralia.gov.au/ [Google Scholar]
- 35.Canadian Cancer Society: Cancer Information : Cervical Cancer. https://www.cancer.ca/en/cancer-information/cancer-type/cervical/prognosis-and-survival/survival-statistics/?region=on [Google Scholar]